In 2000, the American Psychiatric Association (APA) published the revised criteria used in the diagnosis of alcohol dependence. According to this criteria, the single most defining aspect of alcohol dependence is the power of the relationship with alcohol: The stronger the relationship, the more likely the person will continue problematic drinking despite internal and external consequences.
Psychological dependence, where the person believes alcohol is necessary to get through daily activities, alleviate stress, and cope with problems, is a symptom of alcohol addiction. Tolerance and withdrawal are often present, but they alone are not sufficient for a diagnosis of alcohol dependence. Alcohol dependence is diagnosed behaviorally by these signs and symptoms:
Valdez and Koob (2004) state that physical withdrawal alone should not be used as a barometer of alcohol dependence because physical withdrawal is usually not the most powerful motivator for seeking alcohol. Instead, a separate component of withdrawal, consisting of the emotional or psychological component of withdrawal manifested as anxiety or depressed mood, is critical in the development of dependence.
This negative psychological state is called motivational withdrawal (Valdez and Koob 2004). In 2008, Kalivas and O’Brien concluded that the essential elements of dependence are the persistent and recurrent seeking and use of alcohol at the expense of the pursuit of normal rewards (Kalivas and O’Brien 2008). Also in 2008, Angres and Bettinardi-Angres stated that although the disease of alcohol or drug addiction represents a diversity of people, the end result is the same: compulsive behavior in the face of negative consequences.
This pattern of behavior is complicated by the presence of denial, a complex defense mechanism that typically accompanies addictive disease. Addiction is said to be the one disease where the affected individual is convinced he or she really doesn’t have it. Denial is reinforced both by the powerful reward of the alcohol or drug addiction, and by the deficits in learning, motivation, memory, and decision making that accompany the development of addiction (Angres and Bettinardi-Angres 2008).
The question of whether alcoholism is a disease has been debated for decades, if not centuries. The answer is vitally important to researchers, medical practitioners, and treatment providers, as well as to those who suffer from addiction and their family members. This is especially the case in light of absurd proclamations that alcoholism is a behavior choice and not a disease, that it represents a failure of willpower and a reflection of a maladapted and warped character formation, and therefore merits the assignment of judgment and blame. Of course the normal nondependent use of alcohol is a choice; it is alcohol dependence for which the designation of disease is appropriate.
History reveals many examples of illnesses for which the afflicted were held personally responsible until science and medicine were able to provide abundant proof that a biological disease process was responsible and not the weak will of the patients. Such illnesses have included leprosy, seizure disorders, cancer, and major depression. If addiction were really a choice, people would simply quit after the consequences exceeded the perceived benefits (Halpern 2002).
Addiction scientists have produced substantial evidence supporting the viewpoint that alcohol dependence is a chronic disease. Many aspects of alcohol dependence are similar to those of other recognized chronic illnesses, such as type 2 diabetes, diseases, and high blood pressure (McLellan et al. 2000). Alcohol dependence is fundamentally similar to other chronic diseases on several key dimensions:
Not all persons who experience alcohol problems inevitably progress to alcohol dependence. Some young persons experience alcohol use problems that are developmental and are outgrown in the successful transition from adolescence into adulthood. Others develop an alcohol use problem when experiencing difficult life events such as the death of a loved one, divorce, or job loss. Their problem is often resolved with time, emotional support, brief professional intervention, or peer-based intervention by others in recovery (Burman 1997; Granfield and Cloud 1999; Bien, Miller, and Tonigan 1993; Bernstein et al. 2005). Similarly, many persons will experience a period of high blood pressure that essentially resolves through lifestyle change, weight loss, and increased physical activity without developing chronic hypertension (White and McLellan 2008).
Although most adults have used alcohol, and some have abused alcohol, the recreational use of alcohol and alcohol abuse is obviously not considered an illness. Many persons drink heavily without developing an alcohol dependency syndrome. Only alcohol dependence is characterized by profound changes in the structure and function of key brain regions. These biological changes are what drives the symptoms of alcohol dependence, and are viewed as hallmarks of the disease of alcoholism. None of the patterns of nondependent drinking are associated with these profound and lasting changes to the brain.
Relapse is not inevitable, and not all persons suffering from alcohol dependence require multiple treatments to achieve stable, long-term recovery. Even among those who relapse following treatment, families, friends, and employers should not abandon hope that recovery is possible. Community studies of recovery from alcoholism report long-term recovery rates of 50% and higher (Dawson et al. 2005).
Viewing alcohol dependence as a chronic illness does not reduce or absolve the alcohol-dependent person of personal responsibility, any less than persons with diabetes or hypertension are absolved of the responsibility for continuous self-care because their condition is a recognized disease (White and McLellan 2008).
Comparing alcoholism with other chronic illnesses can arouse strong negative feelings. To some people, discussing alcohol dependence as a disease appears to communicate what they think is an inappropriate “medicalization” of addiction. Some believe that calling addiction a disease contributes to the denial of personal responsibility and creates a built-in excuse for treatment failure. Individuals with alcohol dependence who have achieved sobriety may also resent the idea that they have a continuing chronic illness (White and McLellan 2008). Therefore, care must be taken in how the chronic nature of addictive disease is communicated to the public, clients, family members, referral sources, and those working on the front lines of addiction treatment (White and McLellan 2008).
When we view alcohol dependence as a chronic illness, it helps explain the frequent and high rates of relapse following the completion of treatment. An important implication of alcohol and other drug dependence as a chronic illness relates to its treatment approach. Treatment of alcohol dependence is currently delivered in a manner more appropriate for acute illnesses, and there is growing belief that treatment of these patients should adapt the chronic care medical monitoring strategies currently used in the treatment of other chronic illnesses (McLellan et al. 2000; White and McLellan 2008).
Note:
Alcohol dependence shares many of the characteristics that define chronic diseases such as hypertension, asthma, and type 2 diabetes. These include an established set of signs and symptoms, a biological basis, a genetic component, the contributing role of behavior choices, treatment response, and high rates of relapse that are influenced by poor patient self-care and self-management. People with social or heavy nondependent alcohol use are not considered to have a disease. It is only alcohol dependence that has a disease basis, and this is because the symptoms and behavior are the direct reflection of abnormalities in brain structure and function. As with type 2 diabetes and high blood pressure, having the disease of alcohol dependence does not reduce or free the alcoholic of personal responsibility for managing the illness. Relapse following treatment for alcoholism is not inevitable, and if a relapse does occur, those close to the patient should remain hopeful that long-term recovery can still be achieved.
To understand how alcohol dependence is a brain disease, we must first understand the changes that occur in the brain as a drinker progresses from social drinking to alcohol abuse and ultimately to dependence (Cruz et al. 2008).
Alcohol and other drugs of abuse affect the brain in three major ways. They
All substances with addiction potential have strikingly similar effects on many of the same networks of brain cells and brain regions (Iacono, Malone, and McGue 2008). Even behavioral addictions—such as sex, gambling, and food (especially sweets) addiction—are driven by many of the same core brain processes that underlie alcohol and other drug addiction (Goodman 2008).
Neuroscience studies the relationship between brain function and behavior, which makes it an ideal discipline to study the biological basis of addiction. Neuroscientists have contributed enormously to our understanding of how the thoughts, feelings, and behaviors associated with addiction are actually a reflection of the changes in the structure and function of key brain regions (Winger et al. 2005).
The Basics
The human brain is made of billions of nerve cells, which are called neurons. Every thought, feeling, behavior, sensation, perception, and effect from alcohol or other drug that a person experiences is the result of a “conversation” between neurons. Neurons “talk” to other neurons, and these conversations take place when information passes between neurons in the form of a chemical message, called a neurotransmission. The molecule that makes up the chemical message passed between neurons is called a neurotransmitter.
When a neurotransmitter is released from one neuron, it travels across the small space between neurons called the synapse, to bind to an adjacent neuron that has a receptor for the specific type of neurotransmitter. Neurotransmitters bind to these receptors to either stimulate (excite) or slow (inhibit) the activity of the receiving neuron (Clapp, Bhave, and Hoffman 2008; Schuessler 2004).
Until recently, efforts to pinpoint the biological origin of addiction focused on isolated brain regions. The nucleus accumbens, a brain region with a high concentration of neurons that contain receptors for the neurotransmitter dopamine (simply termed dopamine receptors), was identified as the source of the euphoria and high produced by alcohol and other drugs. Therefore, the nucleus accumbens was believed to be the location where addiction developed (Dackis and Gold 1985).
Recent advances in brain science have produced a much broader and more complex understanding. We now understand that it is not a single brain region but multiple brain regions and neuron pathways that are involved in the addiction process.
Neural circuits or pathways are large and often widespread. The networks perform the brain’s essential functions, such as storing information, regulating basic body functions, and directing behavior. Neuron pathways link and coordinate communication between different brain regions. It is now believed that addiction develops from alterations to these neuron pathways within the mesolimbic dopamine system (MDS).
The MDS is a good example of how neuron pathways harness different brain regions so that together they can perform complex brain functions. The MDS neuron pathway connects brain regions that control
These different brain regions within the MDS relay information back and forth, using the neurotransmitter dopamine, the endogenous opioids, and several other neurotransmitters (Angres and Bettinardi-Angres 2008; Gonzales, Job, and Doyon 2004).
One of the essential functions of the MDS is to serve as a reward pathway. The MDS serves to motivate the behavior that is essential for survival, such as eating, loving, and reproducing. MDS releases dopamine and other neurotransmitters to produce pleasure that rewards these pro-survival behaviors. The same release of dopamine is achieved with alcohol and other drugs, but the effect is much more intense than what can be achieved by natural rewards (Comings and Blum 2000). All five classes of commonly abused drugs (stimulants, opiates, alcohol, cannabis, and nicotine) activate the MDS to produce euphoria and the high. Differences in the extent of MDS activation partially explain the differences in abuse liability among the various recreational drugs and alcohol (Pierce and Kumaresan 2006).
Note:
Brain cells or neurons are the most basic components of the brain. Neurons form extended networks with other neurons, called neuron pathways. These pathways link different parts of the brain together to perform the complex functions of the brain and body. Neurons communicate with adjacent neurons by using chemicals called neurotransmitters. These neurotransmitters either excite or slow the activity of the receiving neuron. One of the neuron pathways that is fundamental in the development of alcohol dependence is called the mesolimbic dopamine system, or MDS.
Any behavior is likely to be repeated when it is associated with the experience of pleasure. And one of the normal functions of the MDS is to produce pleasure when a person has sex, eats (especially sweets), or engages in other behavior that is conducive to survival. This pleasurable effect is caused by the temporary increase within the MDS of the neurotransmitter dopamine. Alcohol and drugs of abuse also stimulate dopamine release in the MDS. The intensity of the pleasurable effect from drugs is much greater than what can be achieved through natural rewards. The MDS is referred to as the reward pathway.
Alcohol and all other drugs of abuse have an immediate effect on neurotransmitters and the molecules that carry messages from one brain cell to another. Although every cell in the brain is affected by alcohol, dopamine is believed to be the primary neurotransmitter responsible for the pleasurable effect of alcohol. Dopamine is associated with feelings of well-being and euphoria.
Within the MDS, earlier called the reward pathway, alcohol causes dopamine cells in the ventral tegmental area to release dopamine into the prefrontal cortex, amygdala, and nucleus accumbens. Although dopamine is released in the MDS when we engage in pleasurable and rewarding activities such as eating (especially sweets) or sex (Blum et al. 2000), MDS dopamine release may be three to five times higher in response to alcohol (Di Chiara and Imperato 1988; Wise 2002). This is an important point.
As you can see, alcohol causes a release of dopamine and ensuing euphoria and high that is vastly greater and more intense than what any non-drug experience can deliver. Although nondrug experiences can produce some of the same feelings of euphoria, the dopamine response to nondrug experiences diminishes with successive exposures. In contrast, alcohol delivers the same powerful rewarding effect with every use (at least before addiction develops) (Kalivas and O’Brien 2008).
The highly pleasurable dopamine effect produced by alcohol is referred to as the positive reinforcing effect because it motivates the person to repeat the behavior. In other words, the behavior of drinking alcohol is reinforced through pleasure (Kalivas and Volkow 2005). This process of striving to recapture the euphoria from previous drinking experiences actually describes a learning effect that is based on reward, and reveals that dopamine release is a key event in the process of learned behaviors (Clapp, Bhave, and Hoffman 2008).
Other brain chemicals besides dopamine also contribute to the pleasurable effects of alcohol. A second neurotransmitter called serotonin also plays an important role in alcohol response. Individuals with dysfunctional serotonin activity may be more prone to developing alcoholism (Heinz et al. 2001; Hazelden July 2001).
Alcohol enhances the activity of the inhibitory neurotransmitter GABA (gamma-aminobutyric acid) and curtails the activity of the excitatory neurotransmitter glutamate. These two actions produce the sedating effect of alcohol (NIAAA 2004). Alcohol also activates the release of endogenous (produced within the body/brain) opioids, which contribute to the pleasurable effects of drinking (Kalivas and O’Brien 2008).
During the initial stage of alcohol use, changes in brain chemistry begin to occur that affect the normal balance of neurotransmitters, the receptors these neurotransmitters interact with, and various other molecules. Although these early changes are short-lived and are based on the initial effects of alcohol in the brain, repeated exposure of the brain to alcohol eventually creates longer-lasting changes in neuron and neurotransmitter function (Clapp, Bhave, and Hoffman 2008).
Note:
When a person drinks, changes occur in the activity of several neurotransmitters, which account for the short-term effects of alcohol. Alcohol stimulates the release of dopamine in the MDS, or the pleasure pathway, to produce the mood-altering effect of euphoria and high. Alcohol also (1) increases the release of serotonin and the endogenous (produced within the body/brain) opioids, (2) increases the activity of GABA, and (3) decreases the activity of glutamate. The combined effect of alcohol on GABA and glutamate produces the well-known sedating effect of alcohol.
Relatively short-lived changes in brain chemistry and brain function are thought to initially occur at the onset of alcohol dependence. Continued heavy and persistent alcohol use transforms these short-term changes into lasting changes by the functioning of several neuron pathways (Nestler 2005). Problem drinking progresses to alcohol dependence at different rates in different people. Some drinkers rapidly progress to very heavy, loss-of-control drinking within a short period of time; for other drinkers this escalation may take several decades.
Before the development of addiction, alcohol use is regarded as voluntary, while alcohol use after the onset of addiction is considered compulsive. For example, before the development of addiction, a parent may have to make a choice between helping a child with homework or drinking a glass of wine in the evening. At this stage the drinker will usually make the socially appropriate choice. With the development of alcohol dependence, the drinker may make a deliberate choice to drink and to neglect his or her obligations or responsibilities.
Using the same example, the dependent drinker may encounter other people, places, or things associated with alcohol use (environmental cues) that conflict with his or her wish to help the child with homework that evening. As a result, the parent may begin experiencing steadily increasing levels of anxiety, irritability, and feelings of unease since his or her last drink. Contact with environmental cues and increasing distress since the last drink can both intensify and trigger the overwhelming urge to drink.
The urge itself activates a powerful goal-directed drive to seek and consume alcohol. The intensity of this impulse to drink, and the inability to control the impulse (i.e., to not drink) directly stems not from a lack of will or moral judgment but from substantial neural changes beginning to occur to the structure and function of the brain (Leshner 1997).
Addiction to alcohol represents at its most basic level a dramatic and persistent change in brain structure and function. With the development of alcohol addiction come the establishment and strengthening of new memory pathways. These new pathways contribute to the distortions in thinking and behavior seen in alcoholics. These pathways are accompanied by the weakening of the brain process involved in planning, impulse control, and judgment. In time, the impulse to drink simply overwhelms the progressive loss of ability to resist (Kalivas and O’Brien 2008). It is this compulsive craving to drink alcohol—and the intensity of the craving that overwhelms all other motivations, such as feeling responsible to help the child with homework—that is the root cause of the enormous health and social problems created by alcoholism (Leshner 2001).
Earlier Theories of How Alcohol Addiction Developed
Earlier theories of addiction focused on the pleasurable effect or reward of drinking alcohol or using other drugs. Dependence was thought to stem solely from the intense and recurrent drive to experience the reward sensation (Wise 1980); in other words, addiction was driven by the positive reinforcement induced by the alcohol or other drug (Gill, Amit, and Koe 1988). Researchers also observed that alcohol or other drug dependence often resulted in unpleasant psychological and physical effects if the person stopped abruptly.
As a result, the addicted person often resumed drinking as a means to avoid the distressing symptoms of withdrawal (that is, negative reinforcement or behavior motivated to avoid or reduce an unpleasant experience or state). The positive and negative reinforcement theories provided some insight into the development and maintenance of alcohol and other drug dependence, but the theories were unable to fully account for many aspects, such as relapse after prolonged abstinence.
Current neuroscience discovery goes further by showing that addiction is a series of persistent changes in brain structure and function from prolonged heavy alcohol use that explains the nature of addiction, and the tendency to relapse even when abstinence has been achieved (Feltenstein and See 2008).
Many Alcohol Abusers Do Not Develop Alcohol Dependence
Although the risk factors for developing alcohol addiction have been identified, the exact mechanism by which some heavy drinkers progress to alcohol dependence while others do not has yet to be discovered. However, an important point is that many heavy drinkers do not develop alcohol dependence. Some actually abuse alcohol for decades without developing alcohol addiction (Vaillant 2003).
Individuals differ substantially in how easily and quickly they become addicted; these individual differences are the result of a combination of environmental and genetic factors (Leshner 2001). Also, many people who abuse alcohol or other drugs as teenagers or young adults either quit or moderate their use as they get older, a process referred to as “maturing out” (Chen and Kandel 1995). The process of maturing out may occur in tandem with major positive life events such as marriage, family, or career. This process is explained by a rewarding event or opportunity (positive reinforcer) that enters into the life of the drinker and is incompatible with alcohol use. At this point, the reinforcing properties of the alcohol or other drug, relative to those of the competing reinforcers (marriage, family, or career), diminish to the point where addictive alcohol or other drug abuse is no longer behaviorally sustainable.
People who do not mature out of heavy alcohol or other drug use may not have access to these alternative positive reinforcers, may not seek them out, or may find the reinforcement from alcohol or other drugs superior to these nonsubstance experiences (Winger et al. 2005). However, alcohol abuse in the absence of alternative reinforcers, or even heavy alcohol use in preference of other normally rewarding activities, does not in itself indicate alcohol dependence.
Brain Regions That Mediate the Process of Alcohol Dependence
During the development of alcohol dependence, neuron pathways are reorganized to establish the behaviors that are characteristic of addiction (Kalivas and Volkow 2005). The MDS, or reward pathway, is believed to be the primary brain location in the development of alcohol dependence. The role played by components of the MDS in the process of alcohol dependence involve the following three brain regions:
Examples of the medial prefrontal cortex in action include a person turning down an invitation to get drunk on a work night, or deciding not to pursue a sexual encounter with a co-worker or subordinate. The changes in the prefrontal cortex during the development of addiction have been described as an acceleration of “go” signals (to get drunk) and the impairment of “stop” signals (not on a work night), which contribute to uncontrolled alcohol use despite severe consequences (Clay, Allen, and Parran 2008).
All three of these brain regions linked by the MDS are involved in the activation and modulation of behavior. The nucleus accumbens and extended amygdala are involved in reward-motivated and fear-motivated behavior. The prefrontal cortex is involved in control over the behavioral response to the input from these other two brain regions (Kalivas and Volkow 2005).
Returning to the earlier example, the opportunity for a sexual encounter with an attractive subordinate at work may be intensely enticing to the normal nonaddicted person. However, the impulse to pursue the sexual encounter will not be acted on because activity in the normal, nonimpaired prefrontal cortex weighs the potential negative social and long-term consequences of the behavior against the short-term gratification. The person concludes the risks far outweigh the reward (Kalivas and Volkow 2005). Not so with an alcoholic.
The various processes and pathways that contribute to the development of addiction are very complex and sometimes overlapping. Another way to look at this process is to isolate some of the behavioral aspects of alcohol dependence and to identify the brain regions where these symptoms originate (Koob and Volkow 2010):
Changes in Brain Pathways Involved in Alcohol Reinforcement (i.e., Changes in the Motivation That Drives Alcohol Use)
As described earlier, alcohol or other drug dependence is much more likely to occur when adverse life experiences, genetics, or their combination alter brain function in such a way that predisposes the person to addiction.
For instance, during extreme stress such as emotional trauma or childhood neglect by one’s parent, the brain releases powerful stress hormones that over time can alter brain function to result in an abnormally intense sensitivity. It can result in a diminished capacity to delay gratification and an increased risk of impulsive behaviors.
In this case, the brain reward system also becomes sensitized so that a more powerful and intense experience of euphoria and pleasure may occur from the use of substances and behaviors that trigger and release dopamine in the MDS. The same chronic release of stress hormones can also result in a persistent negative emotional state of irritability, sadness, anxiety, distress, and poor affect regulation (the ability to calm oneself when emotionally upset, to control one’s thought response to an unsettling event, and to control emotion-based behavior). This can make the use of substances that calm or numb the emotional distress much more enticing (Goodman 2009).
Thus, the exact mechanism by which alcohol dependence develops in some but not most drinkers is unknown. However, persons with a heightened sensitivity to the pleasurable mood-altering effects and to the reduction in distressing emotions with alcohol use are most susceptible to developing alcohol dependence. Although these persons may possess altered brain reward pathways that came before their alcohol use, persistent alcohol abuse over time further alters these reward pathways to result in profound and lasting changes in the brain pathways involved in motivation. Some of these pathways mediate reward, while others mediate stress. These changes are the basis of the development of sensitization, tolerance, withdrawal, and dependence, and are described on the next pages.
Positive Reinforcement
Positive reinforcement describes behavior that is driven or motivated by the desire to achieve a pleasant or exhilarating state like euphoria. The positive reinforcing effects of alcohol are important factors that motivate the continued drinking before the onset of alcohol dependence (Gilpin and Koob 2008). However, the onset and progression of alcohol dependence is accompanied by impaired function of brain reward systems, including MDS dopamine and opioid function that produces the mood-altering euphoria with drinking. This loss of function in brain systems that produce reward and reinforcement occurs in tandem with the progressive activation of brain stress systems (Gilpin and Koob 2008).
Negative reinforcement describes behavior that is motivated or driven by the desire to reduce or remove an unpleasant state. With the development of alcohol dependence, an unpleasant emotional state begins to emerge during abstinence from alcohol that consists of dysphoria, anxiety, and irritability, and is distinct from the actual physical withdrawal from alcohol (described later). This negative emotional state is termed motivational withdrawal, and persons who have become alcohol dependent may drink to prevent or reduce the anxiety and distress they experience when they are not drinking (Gilpin and Koob 2008).
There are two factors that contribute to the development of negative reinforcement during alcohol dependence. The first involves the loss of normal MDS function. Impaired dopamine function in this system creates dysphoria (a state of dissatisfaction, unhappiness, and emotional distress). It is accompanied by impaired serotonin function that contributes to dysphoria, and decreased GABA activity that contributes to anxiety and irritability (Koob 2006). The second factor involves the recruitment of brain stress systems in the extended amygdala (CRF and NPY), which contribute to the negative emotional state (dysphoria, anxiety, and irritability) that drives compulsive alcohol use (Koob 2006).
Negative reinforcement often develops and intensifies during the course of addiction. However, some people, especially those who have experienced childhood trauma or severe and chronic stress, are more vulnerable to the powerfully rewarding and motivating effects of negative reinforcement. Such persons are very likely to possess impaired affect regulation and to experience painful and overwhelming emotions and emotional instability. If they find that alcohol provides temporary emotional relief, a powerful negative reinforcement is activated (Goodman 2008).
Neuroadaptation
Neuroadaptation is a term that describes the process by which the brain adapts to the constant presence of alcohol in order to keep performing the normal brain functions (NIAAA 2009). The function and activity of key neurotransmitters is altered with neuroadaptation, and several processes that occur during neuroadaptation serve to increase the compulsion to drink. These processes include
As mentioned earlier, an important effect of alcohol on neurotransmitter function is to reduce the activity of excitatory glutamate, and to increase the activity of inhibitory GABA. Now, an alcoholic doesn’t drink with that intention in mind, but the chronic stimulation of GABA and suppression of glutamate with chronic alcohol exposure cause the brain to attempt to regain a normal state by cranking up the activity of glutamate receptors (Vengeliene et al. 2008). As a result, intoxication begins to feel normal for a person dependent on alcohol.
When a drinker passes out or falls asleep, and alcohol use is abruptly stopped, this heightened glutamate receptor activity creates a state termed hyper-excitability, which is believed to account for many of the symptoms of physical alcohol withdrawal or hangover such as agitation, anxiety, insomnia, and potentially seizures or convulsions (Pulvirenti and Diana 2001; Gilpin and Koob 2008).
Three distinct types of alcohol craving have been identified below. Each type of craving is associated with a different stage in the development of alcohol dependence, and is a reflection of corresponding disruptions in different neurotransmitter systems and brain regions (Clapp, Bhave, and Hoffman 2008):
The transition to alcohol dependence is believed to occur in a sequence.
The first system to become altered is the MDS, followed by the ventral striatum, dorsal striatum, and orbitofrontal cortex, and eventually the prefrontal cortex, cingulate gyrus, and extended amygdala (Koob and Volkow 2010). The final significant brain alteration with alcohol dependence involves the development of a signaling pathway from the prefrontal cortex to the nucleus accumbens that transmits glutamate. This development has profound behavioral consequences.
It greatly diminishes the capacity of the drinker to respond to nonalcohol rewards; substantially decreases the ability to deliberate, plan, control impulses, and use judgment over the use of alcohol; and creates a hyper-response to people, places, and things associated with drinking, which intensifies the behavior directed toward obtaining and using alcohol (Kalivas and Volkow 2005).
The resultant state is termed impaired behavioral inhibition, which means that the person is much more likely to act on the urge for short-term reward or reinforcement (positive, negative, or both) despite longer-term consequences. An important point is that impaired behavioral inhibition is usually present in addicted persons to some degree before they develop an addiction, which also serves to heighten the risk for addiction (Goodman 2008).
The development of this excitatory glutamate pathway contributes to the two hallmarks of alcoholism: loss of control over alcohol use and continued drinking despite harmful consequences (Clapp, Bhave, and Hoffman 2008; Angres and Bettinardi-Angres 2008). Persons with the symptom of loss of control may not necessarily lose control of their alcohol use every time they drink, but instead, their attempts to control their drinking have often failed (Goodman 2008).
Note:
The progression to alcohol dependence is accompanied by profound changes in several brain regions and neuron pathways, which produce the symptoms and behavior changes that define alcoholism. During the development of alcohol dependence, the MDS reward pathway becomes impaired so that pleasurable effects from alcohol are diminished. This loss of function in the MDS pathway, and the growth and activation of other neuron pathways that produce emotional distress, result in the drinker experiencing anxiety, irritability, or depression during dry periods. The drinker is now compelled to resume drinking in order to avoid this unpleasant state, and to compulsively pursue the pleasurable effects of alcohol, which have become more difficult to recapture.
As the drive to consume alcohol intensifies, nondrinking activities and pursuits lose the ability to produce reward. Eventually, the motivation to drink overrides all other competing drives and motivations, leading to the abandonment of activities and pursuits that were formerly enjoyable and rewarding, such as family involvement, career, and hobbies.
With the increasing intensity in the urge to drink comes an increasing inability to control or put the brakes on this urge. This is due to loss in function of the prefrontal cortex, and accounts for such behaviors as drinking to intoxication when the drinker initially only intended to have one or two drinks. In addition, drinking despite predictably severe social, occupational, or legal consequences is another sign of dependence. To summarize it another way: continued drinking is positively reinforced and abstinence is negatively reinforced (Gorski 2001).
By the time the alcohol-dependent person has reached this stage, obtaining and consuming alcohol influences behavior to the point where the need for alcohol dominates the motivational hierarchy (Bozarth 1990). In other words, the need to drink eclipses all other obligations, relationships, and activities.
As described above, this progressively greater orientation of behavior toward alcohol use and the progressive loss of reward and reinforcement from nonalcohol experiences are the direct results of the profound changes in the brain motivational circuitry (Kalivas and O’Brien 2008). Alcohol has become the only potent reinforcer, and perhaps the only reinforcer at all, relative to competing rewards, such as family involvement and hobbies in the life of the alcoholic (Winger et al. 2005). Essentially, alcohol has “hijacked” the brain motivation and reinforcement pathways (Lubman, Yucel, and Pantelis 2004). These profound alterations in brain pathways can persist long after alcohol use has stopped (Kalivas and O’Brien 2008).
This loss of interest in previously gratifying and rewarding relationships, obligations, and leisure activities can result in child neglect and abandonment, the disintegration of marriages and business partnerships, and professional irresponsibility and misconduct. It is not surprising that the behavior and conduct of persons in this stage of addiction can resemble elements of psychiatric disorders such as antisocial personality disorder (ASPD) or narcissistic personality disorder (NPD). The overlap in behavior is considerable.
ASPD is characterized, in part, by a chronic pattern of failure to meet important financial and family obligations, employment instability and the abandonment of multiple jobs, impulsivity, pursuit of illegal activities and occupations, little regard for the truth, and the absence of guilt or remorse. NPD is characterized, in part, by a chronic pattern of extreme self-centeredness and the inability to experience empathy for others (APA 2000).
However, while the symptoms of ASPD and NPD typically emerge during adolescence to early adulthood and remain stable throughout adulthood, persons with chronic alcohol or other drug dependence, in the absence of a pre-existing personality disorder, are usually able to regain the ability to fulfill their financial and family obligations when they have stopped drinking. Then, they can re-enter into meaningful relationships that do not revolve around alcohol use and find enjoyment from nondrinking activities and pursuits. And unlike persons with ASPD and NPD, individuals who have stopped drinking are often intensely remorseful over the suffering endured by others as a consequence of their addiction.
For others, the capacity to experience pleasure or reward from ordinary nondrinking or nondrug experiences remains grossly impaired. The powerful drive to alter one’s distressing emotional state may persist long after alcohol or other drug use has stopped and physical withdrawal has ended. Such persons may begin the compulsive pursuit of activities that are not necessarily harmful and that provide a degree of symptom relief. These activities may be physical in nature and include running, martial arts, or yoga. Although these activities may be labeled as substitute addictions, they serve a positive purpose of introducing an intense non-substance reward that is sustainable, and in doing so can help the person transition from active drinking to ongoing abstinence.
However, in other cases the intense drive to alter one’s feeling or emotional state unfolds destructively with the development of a sex, food, or gambling addiction. They are often driven by the same dynamics as alcohol and other drug dependence:
These shared dynamics are the reflection of a common underlying biological and psychological basis (Goodman 2008; Goodman 2009).
Neurodegeneration
Chronic ingestion of high doses of alcohol can lead to profound changes in the structure, growth, and survival of neurons. Researchers have found substantially reduced volumes of many brain structures in alcoholics, particularly the prefrontal cortex and cerebellum, although this is at least partially reversed with prolonged abstinence. As described above, deficits in the prefrontal cortex can affect motivational circuits and impair the ability to control impulsive behavior, further contributing to alcoholic drinking (Jentsch and Taylor 1999). Alcohol-dependent persons also possess smaller amygdala volumes than nondependent individuals, which is associated with risk of alcohol relapse (Wrase et al. 2008; Gilpin and Koob 2008).
Relapse to Alcohol Use during Abstinence
The cardinal behavioral feature of alcohol addiction is the persistent vulnerability to relapse after physical withdrawal from alcohol has ended. This risk of relapse persists even after years of abstinence, and arises from an intense desire for alcohol and a diminished capacity to control that desire (Kalivas and Volkow 2005; Wolffgramm and Heyne 1995). Intense alcohol cravings, even after years of abstinence, can be provoked by emotional distress; exposure to people, places, or things (cues) associated with drinking; or changes in mood (Vengeliene et al. 2008). As mentioned earlier, alcohol addiction is caused, in part, by a learning process involving the lasting memories of powerful alcohol experiences, and in this context, relapse occurring from cue exposure may be understood as a response to learned behavior (Kauer and Malenka 2007).
The brain of addicted persons is altered and responds very differently to stress than the brains of nonaddicted persons in ways that increase relapse risk (Cleck and Blendy 2008). Studies examining the well-established relationship between stress and relapse have found that exposure to stress activates brain reward pathways, possibly explaining why craving for alcohol or other drugs is triggered when recovering alcoholics and addicts are under stress (Sinha et al. 2000; Cleck and Blendy 2008).
Researchers have found that relapse occurring from exposure to people, places, or things associated with drinking may be mediated by the endogenous opioid system. These findings have important implications for the development of pharmacological therapies to prevent relapse in alcoholics (Gilpin and Koob 2008).
The summary of a scientific conference addressing the interactions between stress, craving for alcohol or other drugs, and relapse during abstinence was published (Breese et al. 2005). Some of the key findings included
The results presented at this conference provide the rationale for the support of research efforts to reduce stress-induced alcohol craving through pharmacological or psychosocial interventions. They also underscore the powerful effect of people, places, and things associated with alcohol use on increasing the risk of relapse.
Summary of the Biological Basis of Relapse Vulnerability
Several factors related to altered brain chemistry and function contribute to the high risk of relapse among alcoholics trying to remain sober. Alcoholism can alter normal dopamine and serotonin function, especially within the MDS, and enhance stress pathways to increase the release of CRF. These effects may persist well into abstinence, leading to difficulties in experiencing pleasure from nonalcohol activities and the emergence of a restless irritability, anxiety, mood instability, and feelings of emptiness. Other factors that contribute to relapse risk include the conditioning process that has occurred throughout active alcohol addiction.
Conditioning refers to the deeply ingrained learning and memory process where people, places, and things (environmental cues) become strongly associated with alcohol use and intoxication. A poor stress tolerance, where stress can emotionally overwhelm the abstinent alcoholic, is another factor that reflects the altered brain chemistry with alcoholism. Abstinent alcoholics can experience intense urges to drink when under high levels of stress. Poor stress tolerance can also interact with exposure to environmental cues to overwhelm the ability of the alcoholic to resist drinking (Goodman 2008; Weiss et al. 2001).
In conclusion, several factors contribute to the very high risk of relapse in the recovering alcoholic. These include biological changes in the brain; the behavioral choices made by the alcoholic in recovery, such as whether or not to avoid old drinking associates and environments; and the degree (or lack of) self-care, such as involvement in a recovery program like AA.
Note:
The profound changes in the brain that occur during alcohol dependence can persist long after drinking has stopped and physical withdrawal has ended. These persistent alterations account for the vulnerability to relapse even years after the alcoholic has quit drinking. This vulnerability is explained by the impaired ability to experience pleasure and reward from nondrinking experiences, ongoing emotional distress, and reduced capacity to resist acting on impulses and urges. The impulse to drink can be triggered by contact with people, places, or things that were associated with drinking experiences, and stress can also trigger the urge to drink, increasing the risk of relapse.
Neurotoxic Effects of Alcohol on Cognitive Function
Alcohol can damage brain cells by impacting the structure, function, and production (i.e., neurogenesis) of neurons, ultimately resulting in cognitive impairment (Crews 2008).
Alcoholism is the second-leading cause of dementia, after Alzheimer’s disease (Eckardt and Martin 1986). Wernicke-Korsakoff’s syndrome (commonly known as “wet brain”) is a type of dementia associated with long-term alcohol use and the malnutrition that often accompanies alcoholism. This syndrome is characterized by the inability to learn new information. Often, the person with Wernicke-Korsakoff’s syndrome will make up or create scenarios to fill in the missing information (Beeder and Millman 1997). In addition to eroding cognitive function, chronic alcohol dependence may produce personality changes. Damage to the frontal lobe of the brain, for example, reduces impulse control, which can result in impulsive or violent behavior (NIAAA 2000; Hazelden July 2001).
Brain impairment from chronic alcoholism may reveal itself in the following areas:
Brain science has recently provided us with a greater understanding of how alcoholism can result in deficits in cognitive function:
Some people may be more susceptible to alcohol’s effects. Women generally experience the negative physical consequences of alcoholism sooner than men, given the same number of years of drinking. This phenomenon, known as telescoping, accounts for earlier onset of liver and heart damage among alcoholic women, and is very likely to occur in the brain as well (Mann et al. 1992; Mann et al. 2005). Adolescents may be especially vulnerable to the neurotoxic effects of alcohol because their brain is still active and developing (Barron et al. 2005; Goldstein and Volkow 2002; Hazelden Nov. 2006).
Note:
Alcohol dependence is associated with damage to brain cells, brain regions, and neuron pathways, resulting in persistent problems in thinking and memory function for some persons. The specific functions most likely to be impaired from chronic alcohol use include short-term memory; judgment, planning, and anticipating the consequences of one’s actions; and the learning and recall of visual information.
Cognitive Impairment and Recovery
Between 50% and 80% of individuals with alcohol use disorders experience some degree of neurocognitive impairment. There has been a persistent belief among clinicians that neurocognitive impairment plays an important role in determining treatment outcome (Bates, Bowden, and Barry 2002).
For most people, the brain heals itself given abstinence and time. Abstinent alcoholics show improvements in cognitive function within a few months of their last drink (Nixon and Crews 2004). Brain imaging (MRI scans) has shown increases in brain volume during abstinence as gray and white matter increase.
Neuropsychological tests reflect improvements in functioning in abstinence that correspond to normalization of brain structure (Rosenbloom, Pfefferbaum, and Sullivan 2004). Neurogenesis begins to resume, and is associated with increases in positive mood and the ability to learn. In turn, recovery tasks become easier and the resulting abstinence makes continued cognitive improvement possible, creating a spiral of continued progress (Crews et al. 2005).
These positive changes take place over a variable timeline. Some improvements occur within the first month of recovery and shortly thereafter, particularly in short-term memory and visuospatial tasks (Sullivan et al. 2000). Interestingly, patients with a diagnosis of antisocial personality disorder have a slower rate of recovery in deficits involving executive functioning. Age alone is not a factor in the rate of cognitive recovery, and persons of all ages who quit substance abuse are capable of some degree of short-term cognitive recovery (Bates et al. 2005). While some gains come early in recovery, other subtle cognitive improvements in executive control functioning may take several years. As one group of researchers concluded after reviewing longitudinal results, “… the message emerging from these studies is clear: Abstinence contributes to recovery, and longer abstinence contributes to greater recovery …” (Rosenbloom, Pfefferbaum, and Sullivan 2004).
Persons with substantial cognitive impairment do not have a worse chance for recovery. One MRI study found that those with the greatest impairment showed, with abstinence, improvement (Sullivan et al. 2000), reflecting not only the obvious greater room for improvement but also the resiliency of the brain. Also, the extent of cognitive impairment does not predict treatment success. However, motivation may be a critical component, and the relatively simple strategies of using support systems and avoiding alcohol-related situations may be the most important tools in early recovery. The Twelve Step approach may be especially helpful because of the repetition and social network it provides, and because it reinforces breaking complex tasks into smaller ones (Hazelden Nov. 2006).
Note:
Impairments in memory, learning, and thinking that are caused by alcohol dependence are in most cases reversed if the drinker remains abstinent. Recovery in cognitive function occurs at different rates in different people, and some areas of function recover more rapidly than other areas. Contrary to popular belief, persons with more extensive cognitive impairment do not have a worse chance for successful recovery from their addiction. One of the reasons for this is that motivation is a crucial element of success in treatment and recovery.
Earlier in this chapter we looked at the brain process that forms the basis of the development as well as the progression of alcohol dependence. We also saw how these changes in the brain account for the symptoms of alcohol dependence that are described by the DSM-IV-TR, which include loss of control over drinking, continued drinking despite consequences, preoccupation with alcohol use, tolerance, physical withdrawal, and the foregoing of important social and recreational activities in favor of alcohol use (APA 2000). Although core symptoms representing alcohol dependence are generally agreed upon, not all persons with a serious drinking problem exhibit the same pattern of symptoms.
Alcoholism is a complex disease with a development that is influenced by genetic, environmental, psychological, and behavioral factors. For more than sixty years, researchers and clinicians have recognized distinct differences in the pattern of symptoms that manifest among alcoholic patients. This recognition resulted in efforts to classify alcoholics into meaningful subgroups in the belief that identifying subtypes of alcoholic patients could increase the effectiveness of treatment selection, treatment outcome prediction, and prediction of the future disease course (Pombo et al. 2008; Moss, Chen, and Yi 2007).
The history of modern alcoholic subtyping systems actually began with the Big Book of Alcoholics Anonymous, first published in 1939. On page 31 there is reference to the moderate drinker, the problem drinker, and the “real alcoholic” (Alcoholics Anonymous 1939). This unscientific observation was the catalyst for the first scientific investigations into various types of problem drinking. E. M. Jellinek began the scientific investigation of alcoholism in the late 1930s, and devised a classification system consisting of what he termed “species” of alcoholism primarily influenced by responses to a questionnaire from the Alcoholics Anonymous newsletter called the Grapevine (Fingarette 1989). The following are brief descriptions of the species identified by Jellinek (Jellinek 1960).
Alpha Alcoholism
Alpha alcoholism is marked by a purely psychological dependence on alcohol, but without loss of control or the inability to abstain. There is a powerful reliance on alcohol to self-medicate stress and life problems, but progression is not inevitable. Jellinek notes that other writers may refer to this species as problem drinkers.
Beta alcoholism is identified by medical problems resulting from alcohol use, such as cirrhosis or gastritis, in the absence of psychological or physical dependence. It is more likely to occur in persons from cultures with widespread heavy drinking and inadequate diet.
Gamma Alcoholism
This species exhibits tolerance to alcohol, physiological changes leading to withdrawal symptoms, and loss of control over drinking; undergoes a progression from psychological to physical dependence; and experiences the most devastating physical and social consequences. According to Jellinek this is the most common species in the U.S. and in AA.
Delta Alcoholism
Very similar to the gamma variety, delta alcoholism exhibits psychological and physical dependence but without loss of control, and persons are likely to suffer from withdrawal when abstaining for even brief periods.
Epsilon Alcoholism
This species has not been studied in depth, but it is fundamentally different from other species. Jellinek called this periodic alcoholism as it is characterized by binge drinking.
Recently Identified Alcoholism Subtypes
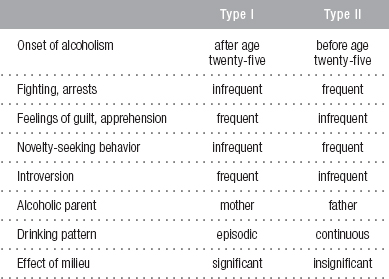
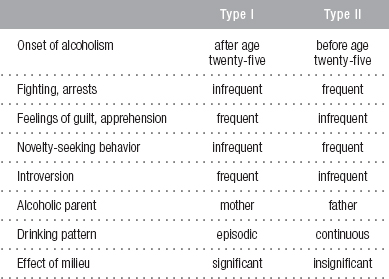
A study of Swedish adoptees and their biological and adoptive parents resulted in identifying two distinct alcoholism subtypes, Type I and Type II. These two subtypes differ by the age of onset of alcoholism, the relative contributions of genetic and environmental factors, gender and personality traits, and whether co-occurring psychiatric disorders (such as antisocial personality disorder) are present (Cloninger, Sigvardsson, and Bohman 1996).
C. Robert Cloninger, M.D., identified Type I alcoholism as characterized by later onset of dependence (25 years or older), few sociopathic features, drinking that is motivated by the desire for stress and anxiety relief, and fewer alcohol-related problems and childhood risk factors. Type II alcoholism was characterized by early age of onset, character pathology with antisocial and impulsive features, childhood risk factors, and more severe alcohol-related problems (Kenna, McGeary, and Swift 2004). Further research revealed three traits that most readily identified type: harm avoidance, reward dependence, and novelty (thrill) seeking. Different brain systems are believed to underlie these traits, an example being dopamine involvement in the trait of novelty seeking (Cloninger 1987).
The following table highlights the differences between Cloninger Type I and Type II alcoholics (Henderson 2000).
The Lesch typology integrates biological, social, and psychological factors in one classification (Lesch et al. 1990; Lesch and Walter 1996) and identifies four subtypes:
Perhaps the most-studied alcoholism typology is that of Babor et al. (1992). Relative to type A alcoholics, type Bs are characterized by greater severity, earlier onset, stronger family history of alcoholism, more childhood risk factors such as conduct disorder, and greater frequency of co-occurring psychiatric and substance use disorders (Bogenschutz, Tonigan, and Pettinati 2009).
Several of the typologies share common features, such as the Cloninger and Babor systems. The most widely recognized subtyping of alcoholics separates alcoholics who have a later onset of problem drinking and less severe alcohol dependence and alcohol-related problems from alcoholics with an early age of onset of problem drinking, a strong family history of alcoholism problems, pre-existing disorders such as conduct disorder, and severe alcohol dependence and alcohol-related problems. The age of onset of problem drinking and disease progression are also partially determined by genetics (Babor and Caetano 2006).
The recognition of these differences in disease pattern has been critically important in the discovery of differences between subgroups of alcoholics in treatment response, reflecting the genetic differences between these subgroups (O’Brien 2005). Several types of medications that act on brain serotonin systems have been found to be helpful in some subtypes and not in others. The two FDA-approved medications, acamprosate and naltrexone, are more effective in certain subtypes of alcoholics than in others (Pombo and Lesch 2009).
The different subtypes in Lesch’s typology have corresponding differences in neurobiology that may have practical implications for clinicians. One of these is related to differences in how glutamate transmission is regulated by the NMDA (N-methyl-D-aspartate) receptor, which has important implications for treatment response to acamprosate and naltrexone (Hillemacher and Bleich 2008). This approach to studying how medication response is influenced by genetic makeup is referred to as pharmacogenetics or pharmacogenomics, and is further described below (Hillemacher and Bleich 2008).
Note:
For many decades, workers in the field of alcoholism have noticed pronounced differences among their patients in the patterns of alcohol use, co-occurring problems, and family histories. These observations led to efforts to identify distinct subgroups of alcoholics in order to better match alcoholism subtype with treatment and to optimize outcome and improve the prediction of disease course. More recently, researchers have used their understanding of the genetics of alcoholism, the role of environmental factors, and the interaction of genetics with environment to identify and define several subtypes of alcoholism. Although several classification schemes have been published, two subtypes have been consistently identified. The two differ by
These differences between subtypes are believed to reflect differences in the underlying neurobiology. Numerous studies have found important differences in how subtypes of alcoholics respond to treatment.
Alcoholism, like other addictions, is a brain disorder. Research has shown that genes help shape how an individual experiences alcohol—how intoxicating, pleasant, or sedating it is—and helps influence how susceptible the drinker is to developing an alcohol problem. Research has also shown that alcohol dependence causes long-term—and perhaps permanent—changes in the way the brain responds to alcohol. These parallel insights from neuroscience research are paving the way for new medications that will improve alcoholism treatment and relapse prevention (NIAAA 2004).
Based on neuroscience research, scientists are developing medications that could potentially target both the acute response to alcohol and the adaptation of the brain to constant alcohol exposure (neuroadaptation) that occurs with alcohol dependence. Potential medications may target specific receptor types, the series of chemical reactions set off by receptor activation, or the production of critical protein enzymes involved in these processes within the brain cells. To use these strategies effectively and safely, however, researchers must first understand in detail where and how alcohol produces its effects (NIAAA 2004).
The age of initial use and regular use of alcohol, and the age of onset of alcohol dependence, are influenced by environmental and genetic factors, as are the adaptive changes in the brain that occur with chronic alcohol exposure. It is likely that differences between alcoholics in the brain process of adaptation will be found in the near future, and that this discovery will further help researchers understand the differences in response to medication treatment (Spanagel and Kiefer 2008).
Enormous ground has been covered by neuroscience in explaining the development of addiction, and in describing how the persistent changes in brain structure and function continue to place the recovering alcoholic at risk of relapse long after abstinence has been achieved. Many prominent researchers in the field of alcoholism and addiction are also looking to neuroscience to address key issues related to recovery from alcohol and other drug addiction. It will be this focus on the neurobiology of recovery that represents the new frontier of addiction research. Among the questions that remain to be answered by neuroscience include the following (White 2007):
Note:
Neuroscience has contributed enormously to a greater understanding of many aspects of alcoholism. These include the vulnerability to developing alcohol addiction, how changes in brain structure and function influence the change in behavior as one’s drinking progresses into alcohol dependence, and how these changes in brain structure and function persist into abstinence to heighten relapse risk. This information is now being used to develop interventions that more accurately target the functional abnormalities in brain chemicals and neuron pathways. However, many questions remain unanswered and will be the focus of ongoing future investigation by neuroscientists and addiction researchers. Especially important areas for future research include the process of recovery from addiction, restoration of normal brain function, and factors that influence the ability or inability to achieve recovery from addiction.