

Breaking Down
When balance is disrupted, stress and inflammation are created—the role of our central nervous system.
We now know that imbalance in our bodies can cause illness. Now, let’s understand which factors create imbalance in the first place.
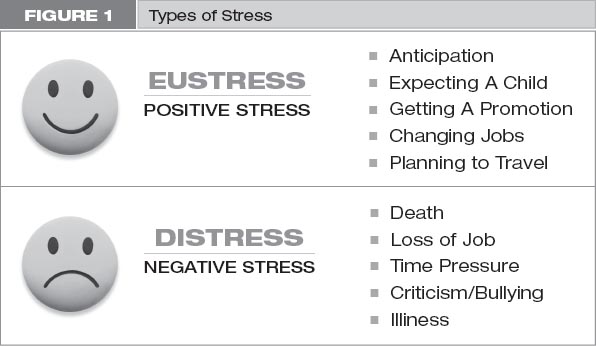
Imbalance is prompted by stress and can be brought on by an injury, anxiety, toxins we ingest, lack of activity, and many more triggers. The powerful effect of stress on your body is the most important concept that we will relay to you, because if you recognize how stress works, you can then start the healing process. The term “stress” was coined in the 1950s by Hans Seyle, MD, a pioneer in the field of endocrinology.1 Some consider him the first researcher to examine the biological impacts of stress and the connections between the mind and body. He defined stress as a body’s response to a demand for change. Stress can be emotional, mental, physical, chemical, or environmental. It can be a physical reality or created in our minds, but in either case it sets off a fixed reaction in our bodies. Seyle broke down stress into eustress and distress.
Eustress is good stress driven by positive anticipation, such as when we are expecting a child, starting a new job, or planning a vacation. It refers more to the way our body reacts to stress. It gives us good coping skills and makes our senses hyperacute. Distress, on the other hand, is negative stress and triggers inflammation and oxidative stress. Distress occurs when we suffer the loss of a child or spouse, termination of a job, or divorce. Both situations demand that the body change. (See figure 1 and Consider 1.)
CONSIDER 1
Dr. Seyle was a pioneer because he saw the connection the mind has over the body. He formed our current thinking around general adaptation syndrome, the ways in which our bodies cope with stress. During times of changing environment or a perceived threat, our acute stress response is adaptive and allows us to cope and respond appropriately to survive the stress. An acute stress response in healthy individuals is a good thing. It is a normal process, and it is protective.1 In acute stress response, we see activation of the nervous system and the cardiovascular, endocrine, and immune systems. The goal of the stress response is to release resources for the body to make energy for immediate use. The body also starts to allocate these resources to specific organs and shuts down resources to other organs to help conserve energy.
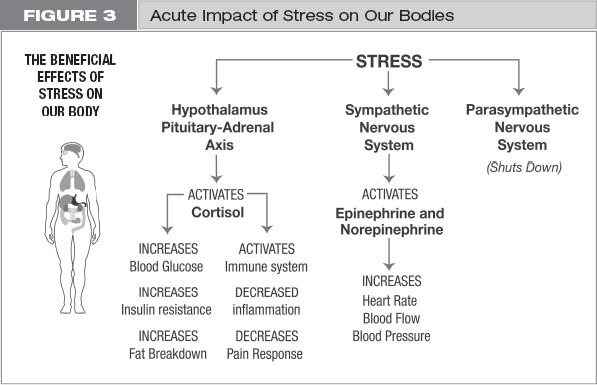
When our senses perceive a threat, the autonomic nervous system is triggered. The two major components of the autonomic nervous system are referred to as the sympathetic and the parasympathetic nervous systems. These systems are regulated by neurotransmitters, or chemical signals, which communicate to the nervous system to set off a chain of responses. They work in balance to affect many systems of the body, such as the heart, eyes, stomach, and genitals. The sympathetic nervous system (SNS) is also called our fight-or-flight system. The SNS triggers the release of neurotransmitters, such as epinephrine and norepinephrine, which then signal the cardiovascular system to increase blood pressure and heart rate. The heart pumps faster and gets blood to all essential organs more quickly, so the body is ready for whatever comes its way. It also suppresses gut motility and the urge to urinate so that we aren’t hungry when we are running and do not have the urge to urinate or defecate. The SNS also increases blood flow to our skeletal muscles and our brain. Our eyes dilate so we can see better in the dark. All of our senses become keener, we are more alert, and our muscles can endure. Simultaneously, the parasympathetic (PNS), our rest and digestive system, is suppressed. This system is responsible for lowering blood pressure, lowering heart rate, and improving gut motility. When there is an acute stressor, activities not essential for immediate survival, such as digestion, growth, and reproduction, are suspended.2
Another major pathway that becomes activated when stress is perceived comes when a signal in our brain triggers the release of cortisol (from the adrenal gland, the stress response center). Cortisol has two main jobs. The first is to help make energy. It is responsible for breaking down fat (lipolysis) and making sugar from storage sources (glycogenolysis). It also mobilizes fat from the periphery to the center to prepare it for use.3 (See figure 2 on the next page.)
Its second role is to regulate the immune system. Without overwhelming ourselves here with how immunology works, the role of cortisol is to balance inflammation with anti-inflammation. Our acute stress response allows for an increase in white cells—the infection fighters (macrophages and natural killer cells) that go into tissues, such as our skin or other organs, and act as protection against those cells most likely to suffer damage during an insult. Our immune system recruits chemicals in our blood to help fight against new trauma, infection, or injury.
One of the benefits of cortisol in acute stress is that it suppresses our pain response. When we are being chased, we cannot worry about the pain in our muscles or minor injuries. This is a protective benefit. It allows us to run despite injury. Cortisol is also known to be a catabolic hormone, which means it breaks down parts of our body, such as our muscle and bone, to provide nutrients to help us weather a stressful time. Again, when we are running from a tiger, we need all of the energy we can muster to save our lives. Cortisol is responsible for keeping us moving in times of stress. (See figure 3.)
People often ask whether cortisol is good or bad. Cortisol levels are a measure of stress. They are cyclic in the body. When we first wake up in the morning, our cortisol levels are at their highest. It is believed that those high amounts are needed then to mobilize our bodies for the day.3 A way to think about cortisol is that it gives us our “get-up-and-go” and allows us to be prepared for whatever the day holds. In a healthy state, these levels gradually decrease during the day.
However, in times of external stress, cortisol levels shift, and they become elevated at times when they would normally decline. This is necessary to activate our fight-or-flight response, to mobilize energy, and to allow us to meet the demands of a stressful day. Imagine a mother watching her child in a park and she witnesses him falling from the monkey bars. She sees her child on the ground, crying in pain and unable to walk. Her alarm phase kicks in, and she is mobilized to get her child help. We can see then that the stress response is extremely important.
Chronic Stress Response
When is stress detrimental to our health? If stress becomes persistent, our cortisol levels become chronically high. With the case of the mother who watches her child fall from the playground equipment, she learns her child has a broken bone in his leg, and she must fully care for him for six weeks while he is in a cast. This results in persistent high cortisol levels with constant activation of her fight-or-flight response. Her heart rate and blood pressure are continuously elevated. Her muscles are broken down, and fat is pulled from the periphery. (See figure 4.)
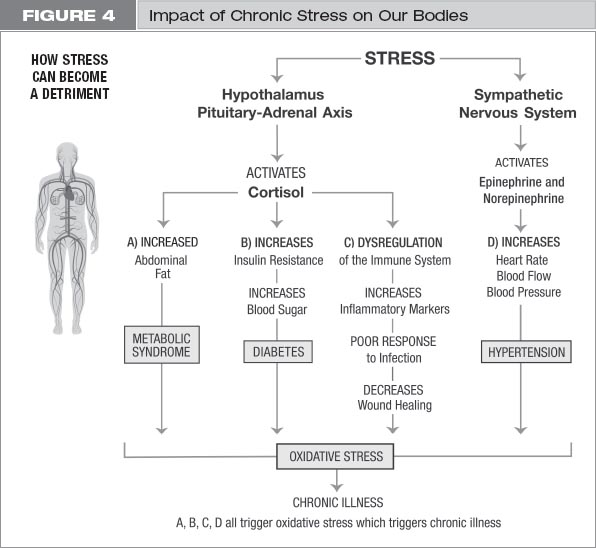
People with high cortisol levels often have trouble with excessive abdominal weight (apple shape). Their sugar levels are also chronically elevated. The immune system becomes overactivated and this can lead to suppression of key immune functions. This suppression can lead to increased risk for infections. Have you noticed, in times of stress that you are more prone to getting a cold? If the stress is ongoing, exhaustion sets in, preventing us from adjusting to the stressful situation. This is where the stress response takes the form of burnout, overtraining, or exhaustion. In the case of our mother from the playground, she has poor sleep, poor support, and poor nutrition, which can leave her burned out after six weeks of constantly caring for her child.
In times of burnout, there is significant imbalance in the immune response. We see more inflammatory markers, decreased wound healing, and poorer response to infection.2 Further, it has been shown that with chronic stress there is overactivation of the hormonal systems and subsequent formation of disease-causing free radicals. Free radicals are toxic to our cells. Their formation and injury to cells is called oxidative stress.4 Inflammation and oxidative stress can then cause chronic fatigue, depression, and excessive weight gain. In addition, persistent elevation of cortisol can lead to insulin resistance, which can cause chronic disease states, such as diabetes and cardiovascular disease. Chronic stress can lead to higher levels of anxiety, increased depression, and insomnia. Other functions, such as cognition, memory, and reproduction, are also adversely affected.4 (See Consider 2.)
CONSIDER 2
Remember that cortisol is about the balance between inflammation and anti-inflammation. In chronic stress, that balance is disrupted, and even with high levels of cortisol, the body becomes resistant and the balance with anti-inflammation is lost.5 This can cause a marked increase in inflammatory cells and can trigger an autoimmune disease in which the body actually starts attacking itself.6
Cortisol plays a role in aging as well. First, let’s discuss how aging affects the body. Aging is defined as the process of growing old, and this involves every cell in our bodies. Chronologic age is the number of years we are alive, but a person’s biological age may be different, depending on different insults to their systems. That is why we see so-called age-related illnesses at different ages in different people.
All cells in the body are continually dividing. It is a necessary function of life. All cells have genetic material (genes) in them that assign the cells their jobs. The genetic material defines who we are and how we think. Our genes are carried in our chromosomes. Chromosomes have caps on the ends called telomeres, whose job is to protect genetic material and promote chromosomal stability. Each time a cell divides, chromosomes are split, but the telomeres shorten because they cannot replicate with each splitting. Telomere shortening has been correlated with the aging of cells. Ultimately, without telomeres, our cells stop dividing. Without cell division, the body cannot repair and is prone to illness and dysfunction. This expedites biologic aging. Chronic stress is associated with shorter telomere length, which can then cause cells to stop dividing, and, ultimately, is associated with increasing biological age. In other words, chronic stress may be associated with premature aging and the onset of age-related illness. This is an area of great interest right now.7
Consider what age-related illnesses can do to us. With age, lung capacity is reduced, digestive enzymes in our guts decrease, brain size can shrink, and the cushions between the disks in our spines can grow smaller, causing us to actually lose height. Functionally, as we age, cognitive function diminishes. Vision weakens, as well as other senses, such as smell and hearing. The fat-to-muscle ratio grows, causing metabolism to slow down. Collagen in the skin dwindles and the skin thins. Our immune systems become weakened, and sleep disturbances increase. Stress can exaggerate the rate of our physical decline. In general, as we age, the risk of chronic disease grows. We desperately need tools to help lower our stress responses if we want to slow aging of our cells. (See Consider 3.)
CONSIDER 3
With constant stimulus, are we at our most efficient? Consider a cheetah who runs to pursue its prey. After it catches the prey, it spends time resting and recharging. That rest-and-recharge time is the counterbalance to the fight-or-flight response and is essential for healing the body. It is during this time that the parasympathetic nervous system is activated and blood pressure and heart rate slow down. Our hunger response returns, and digestion returns to normal. Our pain response comes back, and we can spend time healing our wounds. Our cortisol levels drop as well, so we stop breaking down muscle and fat; we can again build our fat and muscle stores. We return to having a normal immune response to insults.
Now, in our current day-to-day lives—with constant motion, work stress, and overstimulation from our electronic devices and poor nutrition that causes body aches, lack of activity, and lack of sleep—our bodies are under constant stress. Imagine if your phone battery showed a 7 percent charge rate; you would panic. Your primary mission would be to find a charger. Think of your body that way. It needs a battery charger, and if you don’t have time to rest and recharge, you are prone to an inflammatory state that cannot recover from injury. You cannot heal. This is the state within which most of us lead our lives. When you read Dr. A’s personal story, you will see that she certainly was overstressed. And with that condition came illness, as it often does. Most of us don’t see how stress and overstimulation affect us until we have suffered real injury.
YOUR PRESCRIPTION