Chapter 1

GERMS
ANY DISCUSSION about a sick child must begin with understanding the basics of germs.
There are two major groups of germs that typically infect healthy children: bacteria and viruses. Fungi and parasites can also lead to infection, but these groups are far less common, and not relevant to this general discussion.
Identifying the key differences between bacteria and viruses will help parents to understand when antibiotics are necessary, and when they are not. Antibiotics can trigger unwanted side effects such as diarrhea and allergic reactions. Thus, it is important to only use antibiotics when they are truly needed. This in turn helps parents to know when a child can be monitored at home, as opposed to when they need to be seen at the doctor’s office.
There are many different classes of antibiotics. Choosing the right one is dependent on what type of bacteria is suspected and where in the body the infection is occurring.
BACTERIA VS. VIRUS
The two major groups of germs that make children sick are bacteria and viruses.
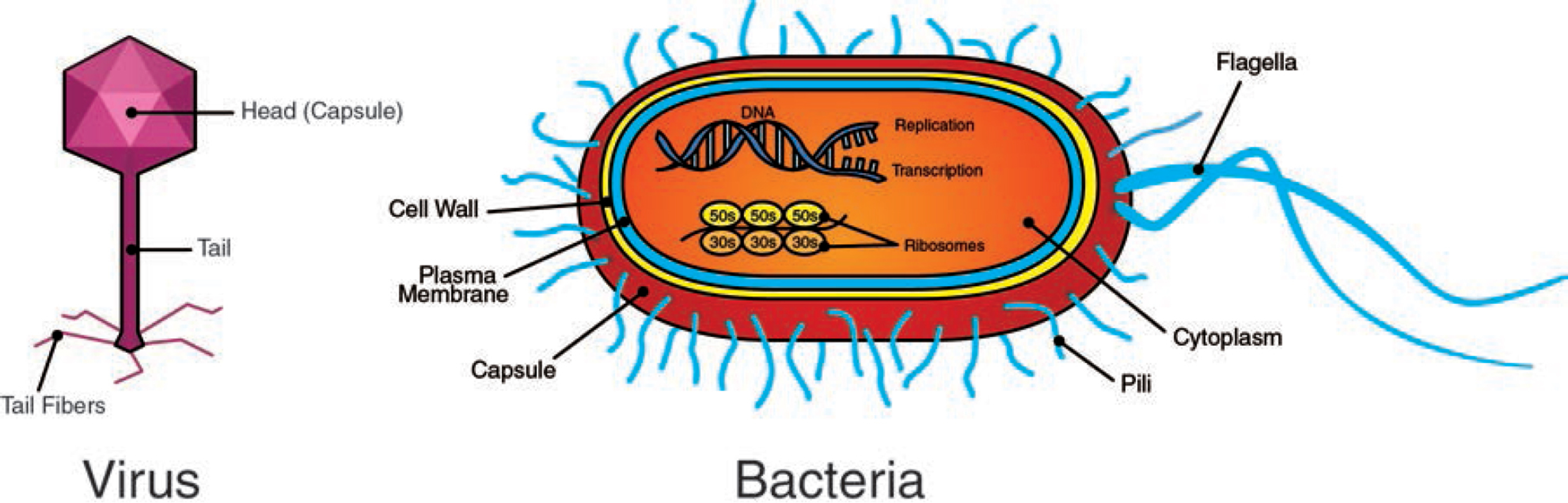
The illustration above demonstrates the significant difference in complexity between a virus and a bacterial cell. The picture is not drawn to scale; typical bacteria are generally 10 times bigger than typical viruses. Bacteria also have many organelles and cellular components that are not present in viruses.
This is important to understand, as antibiotics work by attacking different sections of a bacterial cell that simply do not exist in a virus. In other words, antibiotics work on bacteria, but do absolutely nothing against a virus. This is why antibiotics should never be prescribed for a child who is sick from a virus—it will not help!
And, as viruses are by far the most common source of illness, most infections do not require antibiotics.
But the word antibiotics itself can be confusing. Sometimes the term “antibiotics” is used (correctly) to describe a medication that treats viruses or fungi; however, it is more precise to refer to these medications as antivirals or antifungals, respectively. For the purposes of this book, antibiotics will refer to antibacterial medications, which are only used to treat bacterial infections; this is the more commonly utilized meaning of the word.
MANY DIFFERENT TYPES OF BACTERIA MAKE US SICK


Bacteria that can make people sick are called pathogenic. Only a small percentage of bacteria in the world actually cause disease in humans; even so, there are many different kinds of pathogenic bacteria. Not all bacteria are shaped like the one on the previous page, but all bacteria are similarly complex in structure and are built up of similar components.
The ideal environment for each species of bacteria is also different: some prefer to attack us in our digestive area, causing vomiting and diarrhea, while others prefer to attack us in our ears, causing middle ear infections. Still others prefer to attack our skin, forming painful boils and skin infections. There are also a small group of bacteria which can thrive in multiple different environments.
When bacteria are suspected as the source of illness, identifying the specific type of bacteria involved is the first step in deciding which antibiotic to use for treatment.
ANTIBIOTICS TARGET A SPECIFIC PART OF BACTERIA


In the majority of cases, when you have a bacterial infection, antibiotics should be administered to help fight the illness; while some bacterial illnesses will resolve without any medication, this should be carefully determined with the help of a doctor.
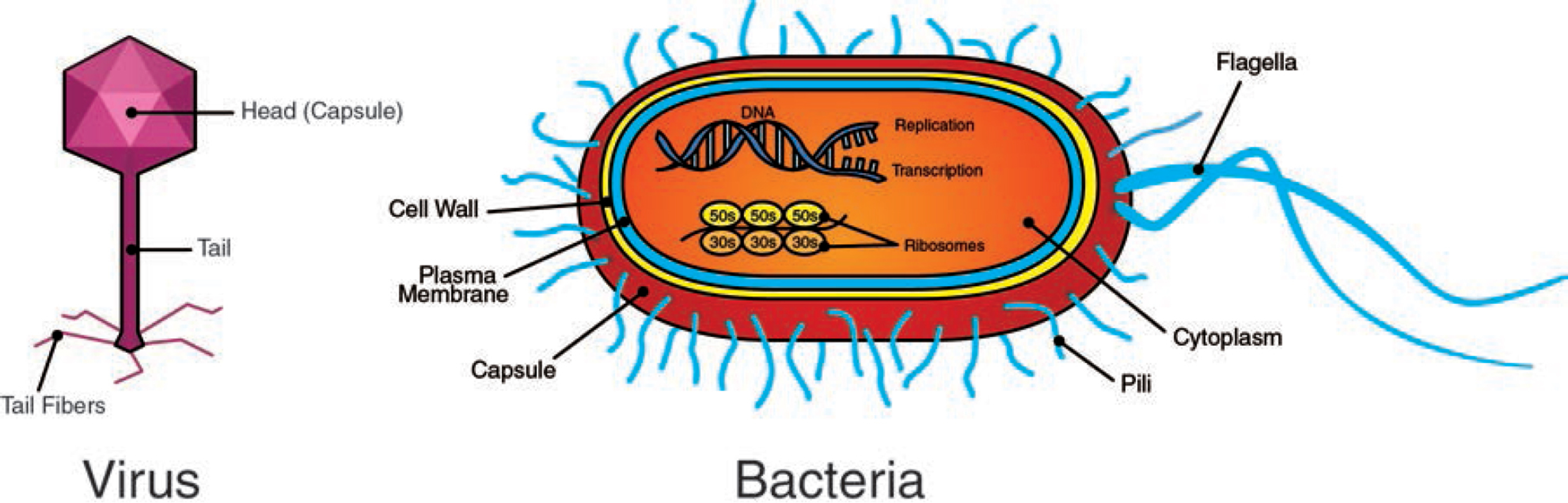
There are many different antibiotics available to treat bacteria. The picture above illustrates the many different classes of antibiotics, each targeting a different section of the bacteria. A single class of antibiotics may contain several different drugs, which all work very similarly.
Picking an antibiotic for treatment is not “one-size-fits-all.” Each time a child is infected with a bacterial illness, the doctor must choose the best antibiotic to match the type of bacteria suspected. Often, an antibiotic class that works well against one group of bacteria will not work at all on a different group of bacteria.
In general, the most cost-effective antibiotic that best targets the germ suspected with the lowest potential for side effects should be utilized.
YOUR BLOOD VESSELS ARE HIGHWAYS FOR GERMS
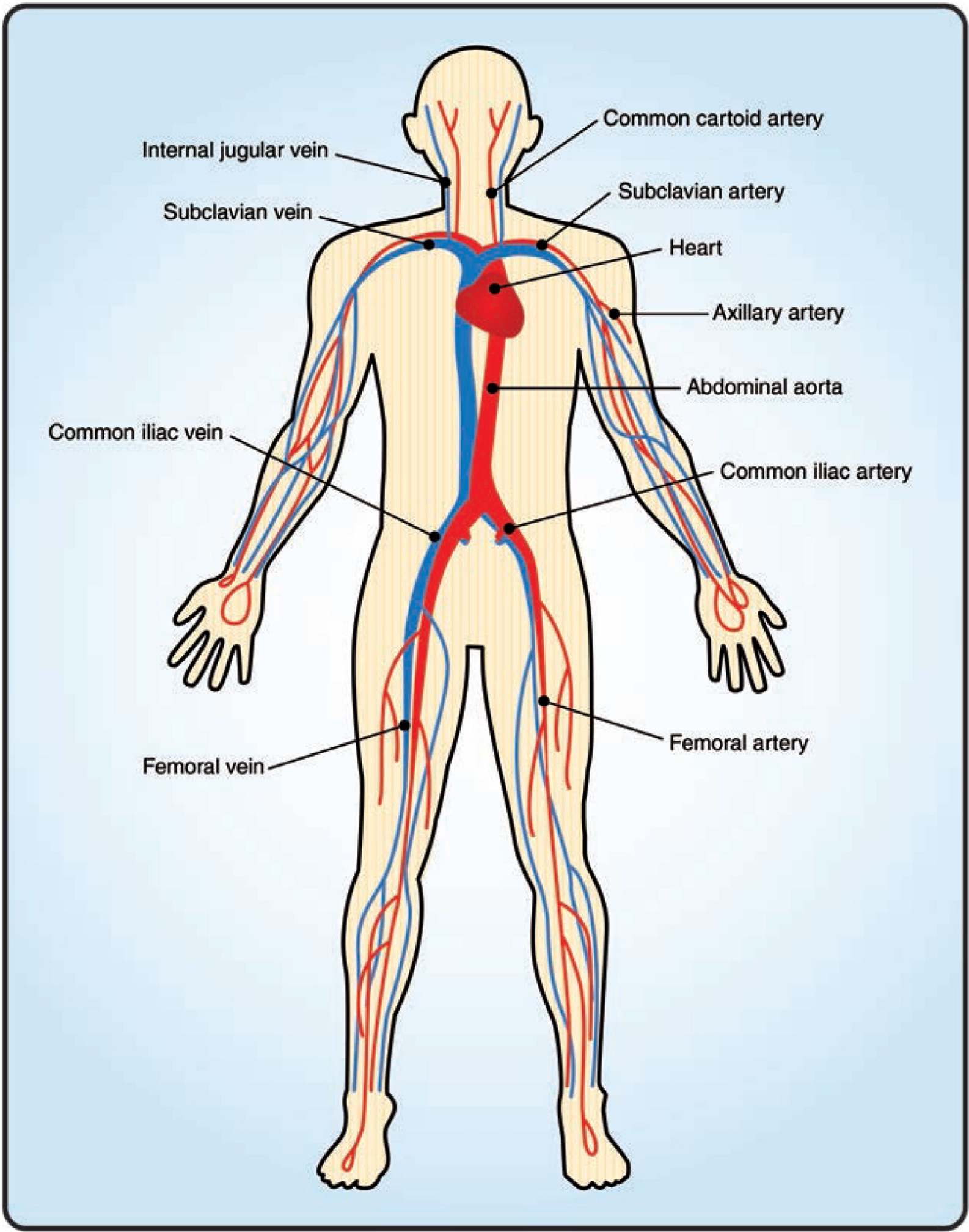
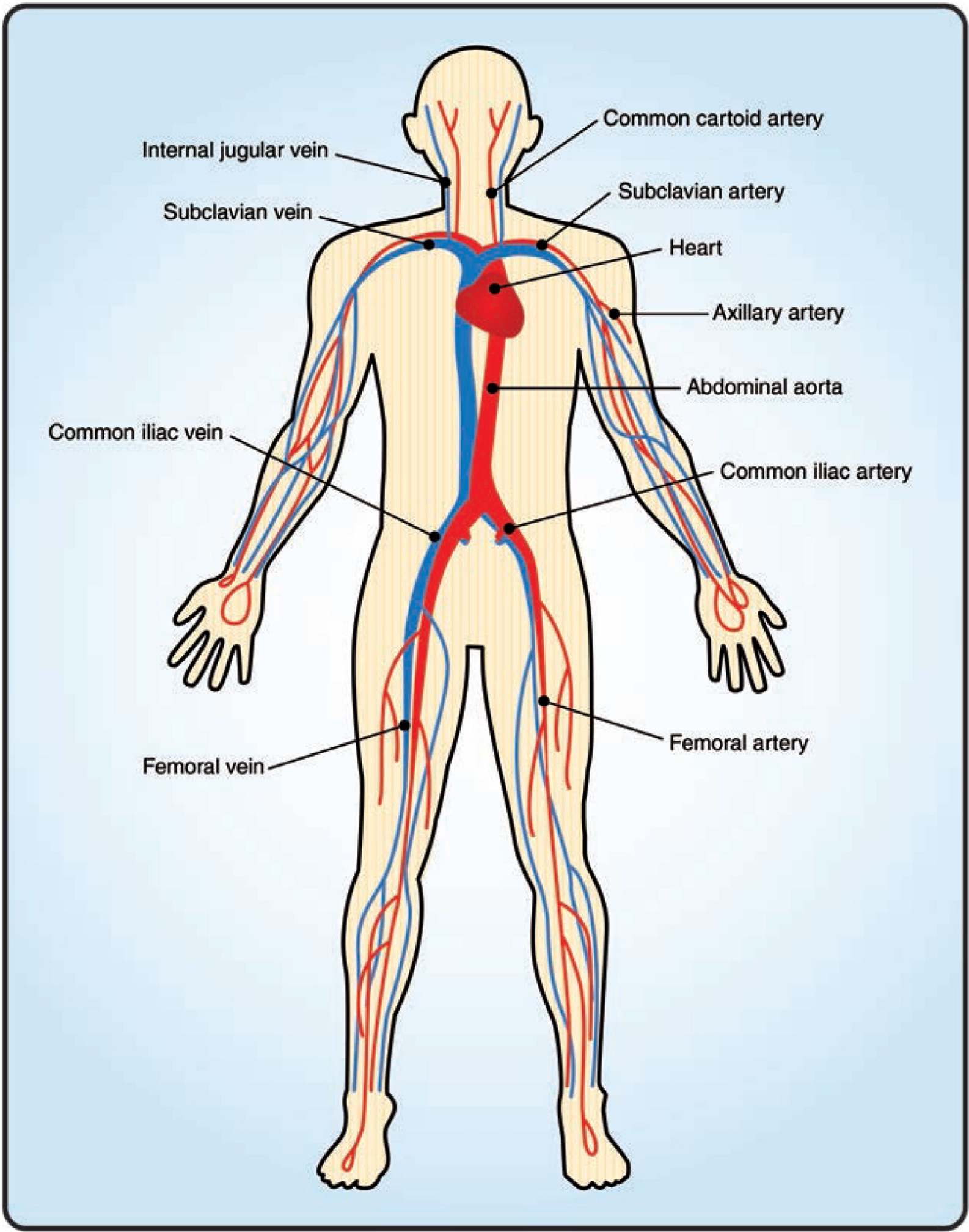
Another very important factor in treating kids is ascertaining where the infection is located. Your blood vessels provide a highway system for germs. A germ can enter the body from contact with animals, other people, infected surfaces, and even your own body. Once a germ enters your body, it can travel anywhere and infect virtually any organ in your body by following your bloodstream.
Knowing where in the body the infection is located can help determine what class of antibiotics should best be utilized, as certain antibiotics will better penetrate the specific organ that is infected. Germs can end up in different parts of the body, either transferred by external contact or by traveling through your blood vessels or other systems of your body.
THE SAME GERM CAN PRESENT IN MULTIPLE WAYS


Depending on where the germ lands and seeds itself, the same germ can manifest as many different types of infections.
For example, a staphylococcal bacterium can cause a pneumonia (infection of the lungs) if it seeds itself in the lungs. Alternatively, it can trigger several different types of skin infections (such as a wound infection, focal skin infection, or impetigo), depending on where it seeds itself in the skin. These are some of the more common examples in which the staphylococcal bacteria can infect an individual, but in reality almost any organ in the human body can be affected.
WE HAVE MANY HEALTHY BACTERIA ON OUR BODY


It is important to note that not all bacteria are bad. In fact, our bodies are teeming with good bacteria that help keep us healthy. Surprisingly, the number of overall bacterial cells (good and bad) in and on our bodies outnumbers our human cells tenfold.
Many of these good bacteria help maintain pH balance, crowd out bad bacteria, and assist with digestion and other bodily functions.
ANTIBIOTICS DESTROY HEALTHY BACTERIA THAT AID IN DIGESTION


Our intestines, in particular, have many healthy bacteria that aid in our digestive process. This is why one of the side effects of taking antibiotics is diarrhea. When you take antibiotics, in addition to killing off the bad bacteria that are causing the illness, you kill off healthy bacteria (for example, in the intestines). After taking antibiotics, the digestive process becomes disrupted until the healthy bacteria are able to repopulate themselves in your intestines.
Another common side effect of taking antibiotics is developing a fungal skin infection. When the healthy bacteria occupying your skin are killed off, it makes it easier for a fungus to then invade the “vacant” skin cells.
Antibiotics can be lifesaving, but because of the potential side effects, it is important that they be used judiciously.
DISPLACEMENT OF COLONIZED BACTERIA CAN LEAD TO INFECTIONS


Some bacteria colonize themselves in certain parts of our bodies and live harmoniously with us, but they still have the potential to create trouble when they move to a different part of the body. For example, our nose harbors bacteria that are harmless—if they remain in place.
However, should the colonized bacteria from the nose become displaced and move to a different part of the body (such as the middle ear space), an infection can occur. Bacterial infections often come from our own bodies when the germ “moves” from one part of the body to another.
Another example of this happening is a skin infection. Many times, the germ that triggers the skin infection is already colonized somewhere else on our body. A cut or break in the skin allows the germ to burrow underneath the skin and fester, leading to a skin infection.
Parents often ask how their child acquired the germ that triggered their infection. Although we can acquire bacterial infections from contact with animals, other people, or infected surfaces, a lot of the time, the infection comes from the child’s own body!
OVERUSE OF ANTIBIOTICS CAN LEAD TO ANTIBIOTIC RESISTANCE


Another complication of antibiotics is that resistant strains of bacteria can develop in your body over time. When you take the same antibiotic over and over, natural selection goes to work on many of the bacteria that are colonized on your body, eventually selecting out only the bacteria that are resistant to that antibiotic.
Consider the colonized bacteria in your nose. Let’s assume that 95 percent of the colonized bacteria can be killed with the antibiotic amoxicillin, while 5 percent of the colonized bacteria have resistance to amoxicillin, and as such, cannot be killed with amoxicillin (but can typically be killed with a stronger antibiotic*).
With every course of amoxicillin, the non-resistant strain of bacteria (the 95% which can be killed) will slowly decrease in population, while the resistant strain (the 5% which cannot be killed) will slowly increase in population, until your nose is completely colonized with only bacteria that are resistant to amoxicillin.
Should some of the colonized, antibiotic-resistant bacteria then “move” and create an infection in a different part of the body, the infection then becomes more difficult to treat because of its resistance to amoxicillin. Hence, a stronger antibiotic will be necessary, often carrying with it a larger potential for side effects.
The emergence of resistant strains of bacteria is why doctors must carefully choose the antibiotic that best targets the “bad” bacteria perpetrator, while minimizing the destruction of colonized bacteria that are not the cause of the acute infection being treated. In other words, when possible, it is always better to use a method with the least risk of collateral damage that can still get the job done.
TAKE-HOME POINTS

![]() Bacteria and viruses are different kinds of germs.
Bacteria and viruses are different kinds of germs.

![]() Antibiotics should only be used for bacteria, and do not work on viruses.
Antibiotics should only be used for bacteria, and do not work on viruses.

![]() Antibiotics are not “one-size-fits-all.”
Antibiotics are not “one-size-fits-all.”

![]() Judicious use of antibiotics can minimize unwanted side effects and curb the rise of antibiotic-resistant bacteria.
Judicious use of antibiotics can minimize unwanted side effects and curb the rise of antibiotic-resistant bacteria.
In summary, although antibiotics are powerful weapons that can be lifesaving when used in the right situations, inappropriate use of them can lead to unwanted side effects and antibiotic resistance.
Because they target specific parts of bacteria, antibiotics will not work on viruses. The majority of infections seen in children are caused by viruses, which will typically get better with time, and which neither require nor respond to antibiotics.
*Some strains of antibiotic-resistant bacteria are only resistant to one or two antibiotics. Alarmingly, however, there are a growing number of bacteria that are resistant to all antibiotics and have no known treatment. While new antibiotics are in development, at present, this is a global healthcare issue that will require the cooperation of all nations in working toward the judicious use of antibiotics.