LILIACEAE
The Lily family
There are about 294 genera in the lily family throughout the world mainly in warm and tropical regions. It is the most typical monocot family of mainly perennial herbaceous plants. Many species contain alkaloids and are more or less toxic.
Characteristics
- Stems are often partly underground in the form of bulbs, corms or rhizomes
- Leaves are simple, usually narrow and with parallel veins, alternate and spirally arranged
- Flowers are usually regular, insect pollinated, solitary or in racemes, spikes, panicles or umbels
- Perianth—the calyx and corolla are not distinguishable with 6 tepals, free or united, arranged in two whorls of 3
- Stamens usually 6 in two whorls of 3
- Gynoecium—ovary superior with 3 united carpels divided into 3 loculi with numerous ovules in each loculus
- Fruit usually a capsule
Aletris farinosa
True unicorn root, colic root

Family Liliaceae
Description
A perennial growing from a stout rhizome, up to a 1 m tall in flower. Leaves in a basal rosette, lance shaped over 15 cm long, yellowish green. Flowers white, tubular swollen at the base and with a mealy surface grow in a long raceme up a tall, leafless stalk. Fruit shorter than the perianth. Flowers in late spring to summer.
Odour—faint; taste—sweet then bitter and soapy.
Habitat and cultivation
Aletris grows in grassy woods in dry or moist peat or sandy soils, throughout the eastern states of USA. It is grown commercially in North Carolina, Virginia and Tennessee.
Parts used
The dried roots and rhizomes harvested when flowering is over.
Active constituents
This herb is very poorly characterized.
1) A saponin has been suggested as the major constituent1—this could be the steroidal saponin, diosgenin,2 or it may be an additional constituent to it
2) Volatile oil
Also contains alkaloids.
Actions
1) Tonic
2) Bitter
3) Spasmolytic
4) Mild sedative
Scientific information
Aletris was an official medicine in the United States Pharmocopoiea and National Formulary until the mid 20th Century. It has been suggested that it was used interchangeably or in combination with False Unicorn Root (Chamaelirium luteum) in the treatment of the female reproductive tract, although they should not have been confused from their physical appearance.
The early American herbalists used the herb to treat a broad range of female issues including amenorrhoea, dysmenorrhoea, threatened and habitual miscarriage, uterine prolapse, uterine weakness for example due to “too frequent child bearing”, infertility, leucorrhoea and as a menstrual cycle regulator. Weiss too states that Aletris is a uterine tonic. However due to the confusion surrounding the purity of the herb and its common substitution, or contamination, by Chamaelirum it is possible that it is a digestive and not a female tonic (King's American Dispensatory).3 Although its chemistry would suggest it may have an influence on the reproductive tract.
The true value of Aletris may have to await future scientific study of its constituents and pharmacological actions. There has been no modern research.
Medicinal uses
Gastro-intestinal tract
The herb's actions would have given rise to one of its common names—colic root.
- flatulent colic
- anorexia
- dyspepsia
Pharmacy
| Three times daily | |
| Decoction of dried root/rhizome | – 0.3–0.6 g |
| Fluid Extract (45%) | – 2–4 m |
Precautions and/or safety
The fresh root in large doses can cause vomiting and diarrhoea and may be narcotic, in small doses it can cause hypogastric discomfort and vertigo.
Historical uses
See above. Also rheumatism; as a diuretic.
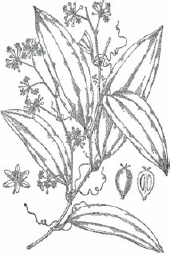
Allium sativum
Garlic
Description
A perennial bulb, ovoid or globose, usually divided into several cloves within the multi-layered membranous coat which later dries to form a protective papery layer. The cloves are swollen buds formed in the leaf axils at the base of the bulb. The cloves are pointed at the top, swollen in the middle and narrower and flat at the base. Scape to 60 cm with 4–6 flat leaves about 1–1.5 cm wide, which form a sheath from the base of the plant. Flowers are pedicellate, small and white or pinkish, borne in a terminal umbel, interspersed with bulbils. Seeds are not usually fertile but bulbils may be used as seed though garlic is usually grown from cloves.

Family Liliaceae
Odour—strong; taste—persistently pungent and acrid.
Habitat and cultivation
Originally native to Asia, garlic is now grown throughout the world for use in food and medicine. Garlic is usually grown from individual cloves and the larger the clove the bigger the mature garlic bulb will be. The cloves should be set, pointed end up, about 5 cm deep and 15 cm apart, in fertile, slightly alkaline soil with good drainage. The plot must be kept weed free. The cloves are usually planted in mid winter because garlic requires a period of chilling below 10°C before hours of long daylight and hot dry conditions in spring and summer. This means that it often does not grow well in wetter areas. It is frost resistant but drought tender.
It is generally harvested when the tops die back in late summer and should be dug with its stems left on and dried, being turned regularly. It must be protected from dew and rain while it is drying. Once properly dried it should keep until the following harvest. If it is not dug, garlic will continue to grow but the bulbs will become smaller.
Parts used
The bulb harvested in mid to late summer when leaves have died back. The bulb is divided into cloves.
Active constituents
1) Volatile oil (about 0.2%) including:
a) sulphur containing compounds (more than 90%) as S-alk(en)yl-L-cysteine sulphoxides (alliin, isoalliin, methiin and cycloalliin)4 and γ-glutamyl-S-allyl-L cysteines.5 Derivatives of vinyldithiin have recently been isolated in fresh garlic.6 Thiosulfinates arise from the sulphoxides once it is crushed, eg. allicin from alliin, they are not present in intact garlic5
b) other—citral, geraniol, linalool
2) Flavonoids including myricetin, quercetin and apigenin7
3) Steroidal saponins (based on erubroside and sativosides)5,8
Also scordinins which are sulphur containing glycosides, mucilage, adenosine, organo-selenium compounds, predominantly selenomethionine5,9,10 (when garlic is grown in soil rich in selenium it tends to replace sulphur),11 lignans,12 fructans13 and proteins including allivin14 and/or alliumin15 (the protein may vary with the sub-species of Allium sativum, of which three have been identified).16 Also contains a number of essential amino acids.16
The chemistry of garlic is complicated by the reactive and unstable nature of its main constituents and their conversions as the tissue cells are disrupted, a process which is influenced by the particular processing method used to achieve the end product.17 Even within the fresh, intact herb the chemistry is variable, alliin being present at higher levels in the outer cloves.18 Further alterations result from duration and temperature of storage.4
Alliin (S-allylcysteine sulfoxide) is itself stable but on crushing fresh garlic or adding water to garlic powder the enzyme allinase, which occurs in a separate compartment in the intact bulb, comes together with alliin which it converts to thiosulfinates. This process is rapid and occurs in about 10 seconds at room temperature.19 Of the thiosulfinates produced 70–80% is allicin, which is unstable, unless dried, and has a halflife of 2.5 days at room temperature.19 Allicin subsequently decomposes to form a number of other sulphur containing compounds including allyl sulfides—diallyl sulphide (DAS), diallyl disulfide (DADS) and diallyl trisulfide (DAT or allitridin)—vinyldithiins and ajoenes (isomers called E and Z) depending on the temperature and pH. These compounds are themselves very reactive and form complexes with cellular proteins and fatty acids.
The γ-glutamyl-S-allyl-L cysteines are converted to:
a) sulfoxides when bulbs are hydrolysed, oxidised or stored at low temperatures20 or to
b) S-allyl-cysteines via another enzyme conversion if the herb is extracted into water.
Commercially produced aged garlic is prepared by adding minced garlic to 15–20% alcohol, incubating for 20 months and then concentrating the resulting extract.21 Odourless garlic has had the allinase inactivated or is deodorised by the addition of chlorophyll.
Nutritional constituents
Vitamins: A, B1,22 B2, B6, nicotinic acid, biotin, C23 and E
Minerals: Selenium (good source),24,25 germanium, sulphur, calcium, magnesium, manganese, copper, potassium, zinc and some iron26,27
Actions
1) Antimicrobial
2) Anthelmintic
3) Anti-inflammatory
4) Hypolipidaemic
5) Spasmolytic
6) Diaphoretic
7) Expectorant
8) Hypocholesterolaemic
9) Antithrombotic
10) Hypotensive
Scientific information
The use of garlic dates back to our earliest history and written records of its medicinal use were found in ancient Egypt in the Codex Ebers ca. BC 1550. The herb has been, and still is, valued across many cultures not only as a medicine but as a food flavouring and preservative. In more modern times it was used as an antimicrobial during World Wars I and II and it is still an official medicine in a number of countries. In Europe where garlic is sold mainly as a powder 156 different garlic preparations are licensed.28 German Commission E has approved its use to aid the reduction of serum lipid levels and as a preventative for age-related vascular changes.
The investigation into garlic, its constituents and their therapeutic effects began in the mid-20th century and still continues at a rapid rate today. Where at one time many of garlic's actions were thought to relate to its allicin content it is now recognised that many of the constituents are biologically active. Alliinase appears to be irreversibly inactivated below pH 3.6 which has raised some doubt about the enzyme's ability to survive exposure to stomach acid and to enable allicin to be produced and absorbed further down the gastro-intestinal tract. Allicin also binds easily to protein and fatty acids so that it may be trapped in the cell membrane, being unavailable for absorption, a proposal borne out by the fact that allicin is not detectable in either blood or urine after consuming garlic or pure allicin.5 Moreover, when allicin is added directly to blood it is undetectable after a few minutes suggesting its rapid chemical alteration.29 However the body does seem to have some limited alliinase-like activity.30 It is probable that allicin alone is not responsible for the known medicinal benefits of the herb in vivo and that other constituents, in particular the organo-sulphur compounds that result from allicin's breakdown, are the pharmacological agents.
There is a lack of consensus on some aspects of garlic's medicinal benefits and effects and a number of significant reasons could explain these contradictory results:-
1) Chemical complexity. Constituents can vary with geographical origin,31 method of storage, age of the garlic and processing of the bulb e.g. allicin levels are lower in powdered garlic than in the fresh herb.32 As allicin has been assumed to be garlic's main active constituent preparations have been standardised on it. However it has been estimated that the amount of allicin released from the type of tablet most used in clinical trials from 1994–2000 varied between 14–18%,30 leaving the majority of the chemistry uncharacterised. In actual fact more than one hundred constituents have been isolated from garlic so far33 of which the organo-sulphur compounds have variable stability20
2) Biological complexity. A great many of the known constituents and their derivatives are biologically active. In addition the volatile constituents are inherently unstable and may change or react in vivo with the metabolites found within the cells or at the cell membrane. There are therefore a great many unknowns in garlic's activity and whilst some of the activities of particular metabolites have been assigned biological functions34 the whole preparation is too complex to be easily standardised. Clearly it becomes very difficult to unify one preparation on all of the active constituents let alone all the different commercial products that have been used in the multitude of trials. Therefore each clinical trial is really assessing a particular garlic product rather than garlic as a single entity
3) Bio-availability. Even within similarly prepared garlic products that may be expected to have similar chemical profiles e.g. garlic powders the bio-availability can be very different. For example enteric-coated garlic tablets designed to preserve allinase from stomach acid were tested for the bioavailability of their allicin, this was found to vary between 3–94% across 24 different brands.30,35,36 There are many other constituents for which this comparison has not yet been made
4) Experimental variability. Trials have varied from the baseline health of the subjects used, their gender, duration of treatment, experimental design and dosage, all of which may have influenced the trial outcomes37,38
There is a large volume of research and reviews into this herb and some of the older information has been superseded by more recent work. Research from the last decade has therefore provided the main basis of the information below but this in turn is based on earlier work.
The process used to produce aged garlic alters its chemistry and possibly its actions compared to the fresh or dried herb. Aged preparations have also been intensively researched but data cannot necessarily be extrapolated to the non-aged herb and has, therefore, not been included.
Anti-oxidant
Garlic exhibits a spectrum of strong anti-oxidant activity due to the polyphenols, tocopherol, protein and volatile oils within it.39–43 Cooking for less than 20 minutes does not diminish the activity of the non-volatile constituents significantly10 but microwave heating and pickling do significantly weaken it.44,45 Water extracts of the fresh bulb provide the strongest anti-oxidant preparations.46
Antimicrobial
In vitro—An extensive range of antimicrobial actions exists for the fresh herb, powder, water extract and/or its constituents with ethanol extracts having the strongest activity.47 Actions to date include:-
- antibacterial against a broad range of organisms, both Gram-positive and Gram-negative, some of which are antibiotic-resistant.48–52 These include Staphylococcus aureus, Escherichia coli, Salmonella typhi, Bacillus cereus,53,54 Neisseria gonorrhoeae,54 Enterococcus faecalis,54 Pseudomonas aeruginosa, Salmonella typhimurium, Klebsiella pneumoniae, Streptococcus pneumoniae, Helicobacter pylori,55–58 Bacillus anthracis,59 Clostridium spp., Mycobacterium tuberculosis,60 oral/periodontal pathogens61,62 and many others.63 Not only does garlic inhibit this great range of bacteria, it does not seem to induce resistance in them and can be effective against some bacterial toxins too.64 The antibacterial activity is apparently 10 times stronger against pathogenic bacteria than against gut flora47,64 the growth of the latter being additionally encouraged by the fructans present in the herb
Garlic works synergistically with some antibiotics65 but was found to increase the minimum inhibitory concentration of others (ampicillin and norfloxacin) when the two were co-administered.66
Powders are more effective antibacterials than oil extracts,67 powder from the fresh bulb being stronger than that derived from stored bulbs.68
- antifungal15,69 against a range of fungi including Candida spp. (C. albicans),49,63,70–72 Cryptococcus neoformans,60 Scedosporium prolificans73 (which is resistant to orthodox antifungals), Aspergillus spp.74 and other pathogenic fungal species.75–77 It also enhanced the activity of pharmaceutical antifungals against C. albicans,78 Aspergillus fumigatus79 and Trichophyton spp.80 Fresh garlic seems to be a better antifungal against Candida than garlic powder81
- antiviral against human cytomegalovirus,82–84 the enteroviruses coxsackie and ECHO virus;85 HIV in the early part of its life cycle,86 influenza A and B, HSV-1 and 2, parainfluenza virus type 3, vaccinia virus, vesicular stomatitis virus and human rhinovirus type 260
- antiprotozoal against Giardia lamblia,87 Entamoeba hystolytica,60 Trypanosoma spp.88 and Leishmania spp.89 and inhibitory to Plasmodium sporozoites (malaria)90
In vivo—The clinical trials conducted on garlic are limited given its broad spectrum of activity in vitro.
Topical preparations effectively treated:-
- oral candidiasis (paste), comparable results to clotrimazole91
- otalgia associated with acute otitis media (combined with other herbs) as ear drops, comparable benefits to orthodox therapy92,93
- tinea infections (ajoene)94,95
- recurrent mouth ulcers (powder)96
- warts (both aqueous and lipid fractions of fresh garlic, the latter being much more effective and faster acting).
Furthermore use of the preparation on larger warts resolved smaller untreated warts in the same vicinity97
Garlic's systemic antibacterial activity was epidemiologically assessed by checking the occurrence of Helicobacter pylori amongst regular garlic eaters compared with non-garlic eaters. Although its prevalence was not reduced by garlic,98 the bacterial population size was significantly lower99 suggesting its consumption may confer some protection. However garlic oil failed to reduce signs of H. pylori infection in a small group of dyspeptic patients.100
Other studies have shown that garlic:-
- reduced the incidence of the common cold and hastened recovery from infection when used daily101
- treated giardiasis successfully47
- reduced the incidence of acute viral infections of the respiratory tract102
The mode of action as an antimicrobial is not only one of immune stimulation (see below). It seems likely that the sulphur content disorders the cellular activity of pathogens without disturbing human cells which are protected by their glutathione content.87,103
Anticancer
In vitro—The herb and its sulphur constituents inhibit a number of cancer cell lines, the lipid soluble fraction being more effective than the water soluble one104 and the action of alliinase apparently playing a significant role in the development of this activity.105
Mechanisms contributing to the anticancer activity of the herb and/or its constituents probably involve:-
- anti-oxidant activity23,106,107
- direct anti-proliferative effects—many studies show increased apoptosis and arrest of division of cancer cells.15,106–112 Cell lines that have been inhibited include nasopharyngeal carcinoma,113 neuroblastoma,114 prostate115,116—including the unresponsive androgen-independent type,117–119 gastric120–123 lung,124,125 skin,126 melanoma,127 leukaemia,128–132 liver,133–135 colon,136–138 oesophageal,139 bladder140,141 and breast cancer cells whether hormone-dependent or not130,142,143
- induction and maintenance of detoxification enzymes against potentially damaging chemicals.23,106,107,144–146 This prevents damage to DNA (genotoxicity) including from asbestos,147–149 aflatoxin,150 chemical carcinogens151 or mutagens152–154 and radiation154–156
- increased immune activity23,107 (see below)
In addition research has shown that Allium and/or its constituents can induce some cancer cells to differentiate,157 inhibit their invasiveness,158 inhibit angiogenesis159,160 and can act synergistically with conventional chemotherapeutic drugs, increasing cancer cells susceptibility to them.161
In vivo—Epidemiological evidence indicates that garlic users may have protection against a range of cancers23,162,163—breast,164 ovarian,165 colorectal,166 oropharyngeal,162 laryngeal,162 oesophageal,167 stomach,166–170 prostate162,171 and renal cancers.162 Protection was linked to the consumption of garlic, either raw or cooked, more than three times a week.163
Garlic juice reduced levels of an endogenously produced chemical carcinogen derived from a high level of dietary nitrate172 and ajoene has been used with success in the topical treatment of basal cell carcinoma to reduce tumour size.173
Cardio-vascular effects
In vitro—Actions that have been demonstrated for garlic preparations and/or its constituents include:-
- inhibition of platelet aggregation21,174–177 the thiosulfinates are stronger than aspirin at equivalent doses.178 (Raw garlic is stronger than cooked179 and steam-distilled garlic oil and garlic oil macerates have a very much reduced activity. Aged garlic may be devoid of antiplatelet activity.)180
- protection of erythrocytes181 and neutrophils182
- reduced cytokine induced endothelial inflammation and monocyte adhesion—early factors in the development of atherosclerosis and atherothrombosis183—and decreased arteriosclerotic plaque formation184
- protection of LDL from oxidation185 and glycation186,187
- inhibition of cholesterol and fatty acids synthesis188–191 and reduced production and secretion of chylomicrons192
- activation of nitric oxide production—vasodilation21,160
- inhibition of angiotensin converting enzyme (γ-glutamylcysteines)
- reduced lipid accumulation in aortic cells derived from arteriosclerotic plaque193
At high enough doses garlic modulates the cytokines involved in pre-eclampsia in placental cells194 although to-date this effect has not been borne out in vivo—see below.
In vivo—Early work on garlic suggested it had hypolipidaemic and hypotensive activity however it is here that a lack of consensus on garlic's benefits is most apparent. Results of clinical trials have been reviewed over a number of years.21,37,195–199 The averaged results of the positive data showed a reduction in cholesterol of 9.9%, LDL 11.4% and triglycerides 9.9%.188 However less than half of the studies assessed in a 2006 critical review found garlic preparations lowered cholesterol.188
The hypotensive activity of garlic preparations have been tested in clinical trials—the majority of these were positive21,200 and a pilot epidemiological study also associated regular garlic consumption with lower systolic blood pressures.201 There are negative studies here too though.188,202
Other circulatory benefits that have been reported are188:-
- reduced oxidative stress200
- prevention and some reduction of arteriosclerotic plaque formation203,204
- protection of elasticity in aging blood vessels205
- inhibited platelet aggregation (garlic is a possible substitute for aspirin-intolerant patients)206,207
- increased peripheral blood flow21,208,209 with benefits for treating peripheral arterial occlusive disease21 (reviewed210)
- reduced incidence of myocardial infarction in men with a high risk for coronary heart disease21,211
- increased tolerance for exercise in patients with coronary artery disease212
- increased fibrinolytic activity in patients with atherosclerosis, this increases with regular use of the herb21
- improved arterial oxygen levels and reduced dyspnoea in cases of hepatopulmonary disease213–215
- improved skin temperature as well as reduced erythrocyte and thrombocyte aggregation in patients with systemic sclerosis216
A review of garlic's use to prevent pre-eclampsia, and its complications, concluded the herb was safe for pregnant women and may help reduce hypertension, but there was insufficient data to recommend its use to treat this condition.217,218
With the current discrepancies in clinical trials, the true and full extent of the benefits of garlic for cardiovascular problems must await further evaluation.
Immunomodulatory
In vitro—Garlic and its constituents have demonstrated potential benefits by:-
- increased activity and protection of macrophage and lymphocyte activity219 including against chemotherapeutic agents and UV radiation220
- increased levels of natural killer cells220
- cytokine modulation associated with inflammation and immune function221–226
- modulation of membrane-dependent immune cell functions227
- modulation of T-cell function associated with chronic inflammation228
Other
In vitro:-
- some of the sulphides are COX-2 inhibitors229
- the oil is a good solvent for gall stones230
- aqueous garlic extracts can immobilise sperm (membrane disruption)231
- garlic and/or its constituents have insecticidal activity232 and are anthelminitic against roundworms and hookworms21
- garlic has some phyto-oestrogenic potential (lignans)12
In vivo garlic:-
- with vitamins improved chronic atrophic gastritis233
- was carminative in patients with gastro-intestinal discomfort21
- was beneficial (anti-inflammatory) for patients with rheumatoid arthritis234
- decreased blood glucose by over 11%,206 in men only38 but not in non-insulin dependent diabetes21
- reduced apparent nephrotoxicity of cyclosporine in renal transplant patients235
- effectively treated corns (lipid fraction)97
- as a 1% topical application of garlic oil was a deterrent to sand flies (97% protection)236 but ingestion of a single dose did not reduce mosquito bites.237
Medicinal uses
Cardiovascular system
Because of the effects on serum lipids, platelet activity and hypotensive activity as well the action on the blood vessel walls themselves, it may be used for:
- hypertension
- hypercholesterolaemia
- hyperlipidaemia
- thrombosis
- varicose ulcers
- atherosclerosis (prophylaxis)
- atheroma
- phlebitis
Respiratory tract
- influenza
- whooping cough
- infections (lungs, throat and tonsils)
- asthma
- recurrent colds
- respiratory catarrh
- bronchitis (chronic and acute)
Gastro-intestinal tract
As an antimicrobial in the gut, it is effective in treating all infections in this area. It is believed to have a normalising effect on beneficial gut flora.
- typhoid
- food poisoning
- worms
- dysentery (amoebic and bacillary)
- cholera
- flatulence
- colic
- increased assimilation of vitamin B1
Externally
- infected wounds
- otitis (drops)
Pharmacy
| Dosage | – for long term maintenance 3–8 perles or 1 clove |
| – for acute infections 2–6 good sized cloves a day | |
| Daily (BHP) | – 4–12 mg of alliin (approximately 2–5 mg allicin) |
| – 400–1200 mg fully dried powder | |
| – 2–5 g fresh bulb | |
| – 0.0–30.12 mg garlic oil |
Tinctures may have very variable compositions due to the instability of the constituents.238
The macerated oil can be dropped into the ears to treat ear infections. The fresh clove can be swallowed whole, after cutting if necessary, crushed or chopped and added without cooking to food. Cooking will cause loss of at least some of the active, volatile constituents. Garlic should be taken with food to avoid gastro-intestinal problems.
CONTRAINDICATIONS—Warfarin and saquinavir users or those with an allergy to the herb or Allium family.
Pharmacokinetics
After consuming garlic a complex series of chemical transformations occur and many elements of the pharmacokinetics are still to be elucidated. Although allicin has been shown to diffuse easily through cell membranes in vitro,239 no allicin is detectable in serum, urine or stools in vivo even after the consumption of large amounts of raw garlic. It seems likely that allicin is converted by stomach acid to DAS and DADS240 and that these substances are further metabolised to produce the sulphur constituents found in the breath namely allyl mercaptan, methyl mercaptan and the predominant allyl methyl sulphide (AMS)—cooking garlic reduces these breath-detectable metabolites.241 (DADS has also been reported to occur in breath after eating garlic5 and in vitro it is converted by liver microsomes to allicin242). Apart from the sulphur containing compounds, non-toxic levels of acetone are also detectable on the breath which may result from increased triglyceride metabolism.32 Although the immediate breath odour is from sulphur constituents produced in the mouth these are subsequently replaced by AMS produced in the gut.243 Cysteine metabolites (S-allyl-cysteines) are excreted in urine after being further modified to S-allyl-mercapturic acid.244
Precautions and/or safety
Its use by breastfeeding mothers has not been associated with any adverse effects in their infants.245
In standard test constituents of garlic were strongly anti-mutagenic due to the induction of detoxifying enzymes.246 The most frequent side-effects is that of a perceptible odour on the breath and body that is not always acceptable. Raw garlic in particular can also cause flatulence, heartburn, diarrhoea247 and possibly stomach irritation if taken on an empty stomach.32 Skin contact with raw herb can cause burns.248,249
It has been established that there is a food allergy to members of the onion family and an enzyme has been isolated from them that evokes an immunoglobulin-E-mediated (type-1 hypersensitivity) response in sensitive individuals.250 Skin prick tests on patients with suspected food allergies found a 4.6% reaction in children and 7.7% reaction in adults to the herb.251
Other reported allergic reaction include urticaria,252 contact dermatitis,253–257 occupational rhino-conjunctivitis and asthma from exposure to garlic dust258 and one case of anaphylaxis in a patient with multiple allergies.259 However immediate allergic reactions, either by contact or ingestion, are considered to be rare.252
There is a suggested link between garlic consumption and the exacerbation of pemphigus,260 one case of surgical haemorrhage261 and one of spinal epidural haematoma.21
Interactions
In vitro—Garlic and its constituents can affect cytochrome P450 isozymes. These include CYP2C9*1, CYP2C19, CYP3A4,262 CYP3A5, CYP3A7263 and CYP2A6.264 Both the herb and allicin had low to moderate interaction with P-glycoprotein, a cell membrane transporter.262,265 Organo-sulphur constituents in garlic altered the transport of cisplatin (chemotherapeutic), suggesting a potential to either increase or decrease levels of this drug.266 It does not interfere with the activity of the antibiotic gentamicin.267
In vivo—Co-administration of garlic with the chemotherapeutic drug docetaxel found no interaction occurred however there is a possibility that it could decrease clearance of the drug.268
Garlic reduced levels/bioavailability of saquinavir a protease inhibitor when the two were taken together269 but did not significantly affect the level of another protease inhibitor, ritonavir.270 However two cases of gastro-intestinal toxicity have been reported where ritonavir and garlic were used together by HIV patients.
There are only two reports to-date of garlic and warfarin causing increased clotting time when used together271 and one of an interaction between garlic and the antithrombotic, fluindione.272
CYP3A4 activity was not affected by concomitant garlic use.273
CYP2E1 activity represented by chlorzoxazone (muscle relaxant) metabolism was reduced by garlic oil in elderly volunteers274 and by DAS in healthy volunteers (protective?) although no therapeutic interactions have been reported.275
No other interactions have been reported.276
Historical uses
As a treatment for worms; tumours; arthritis and heart disorders. An ancient heal-all; diuretic; emmenagogue; a cure for all poisons; removes spots and blemishes; jaundice; epilepsy. Bites of mad dogs and venomous creatures; cure for lethargy! Prophylactic for the plague; piles; smallpox; hoarseness; tuberculosis; rheumatism.
Aloe barbadensis [Formerly Aloe vera]
Aloe

Family Liliaceae
Description
A stemless, stoloniferous, drought-resistant succulent which forms a clump over time. First leaves upright growing in a fan shape. Older leaves spiral round the plant. Leaves narrowly lanceolate, 30–60 cm long, smooth, rubbery, succulent, glaucous green. They are flat on the upper surface, curved beneath and dotted with small white stripes. Margins armed with whitish-reddish teeth. A mature aloe has about 15 leaves forming a basal rosette and the leaves are held upright by the water pressure of the gel. Flowers yellow-red, tubular, about 2 cm long in a long raceme up to about 1 m tall, blooming intermittently throughout the year. Plants growing in full sun may be stunted and/or have pinkish-red leaves which curve at the tips or lack gel.
Latex odour—characteristic and unpleasant; taste—nauseating and very bitter. Gel—odourless; taste—slightly bitter.
Habitat and cultivation
Originally from southern and eastern Africa and introduced to the Mediterranean,291 it is cultivated throughout the world. It is usually propagated from “pups” or young suckers which grow from the main root stock. They may be easily separated and reset when they have some roots of their own. Aloes need a frost-free situation and well-drained soil. They do best in semi-shade with adequate water in hot weather when they are growing strongly. They need drier conditions in winter. When transplanting, it is important not to water them for 7–10 days or they will rot and die. They are best potted and brought inside for winter in frosty areas.
Parts used
There are two different fractions of the herb that are used medicinally. The latex or juice, known as aloes, is an exudate derived from the outer part of the leaves after they have been cut transversely near the base. It is collected for a period of 6 hours and evaporated to a yellow residue. Latex levels vary within the plant for instance younger leaves have more than older ones.277 The other fraction is the gel derived from the inner central part of the cut leaf, which is usually used or processed when fresh—the leaf automatically seals itself so may need to be cut again several times.
Active constituents278
Latex
1) Hydroxyanthracene derivatives (min. 28%) of anthrone type including barbaloin (15–40% consists of the isomers aloin A and B),279,280 emodin, aloe-emodin281 and chrysophanol282,283
2) Chromone derivatives284–286 including aloeresins of which up to 30% is aloeresin B or aloesin287
Also contains coumarins/dihydrocoumarins288 and a number of aromatic substances mainly aldehydes.289
Gel
1) Carbohydrates (0.3%)
a) polysaccharides (10%) consisting of units of mannose, glucose and galactose.290 Mannose, as mannose 6-phosphate,291 is the predominant one and gives rise to the name mannans.292–294 It includes the acetylated mannan, acemannan, which may have one or more polymers of various chain lengths.277 Other polysaccharides include aloeride which contains predominantly glucose units.295 The make-up is dependent on a number of variables such as subspecies, geographical location,290 growing conditions382 and extraction process296
b) glucans (malic acid acylated carbohydrates)297
2) Glycoproteins298 including lectins—aloctin I and II299
Also contains some hydroxyanthracene glycosides, triterpenoids including lupeol, phytosterols300 including β-sitosterol301 and campesterol, salicylic acid, prostanoids including arachidonic acid,302 cholesterol,302 choline,302 a phthalate303 and tannins. A number of amino acids291 and enzymes have been identified in the gel including a peroxidase,304 carboxypeptidase305 and superoxide dismutase isozymes.306
There are four main medicinal species of Aloe although A. barbadensis is considered the most potent.277
Nutritional constituents
Vitamins: A, C, E and B vitamins including thiamine, riboflavin, niacin and folic acid
Minerals: Zinc, sodium, copper, potassium, manganese, iron, calcium and traces of chromium307 and germanium308
Actions
Latex
1) Laxative
Gel
2) Vulnerary
3) Anti-inflammatory
4) Emollient
Scientific information
Aloe has been used for many centuries and in many different cultures, the latex as a purgative and food flavouring (bitters) and the gel for external healing. In recent times the gel has been of interest to the medical and cosmetic industries and this in conjunction with its widespread public use has generated a body of research. The gel has yielded contradictory results in the scientific literature and this may be explained by a number of factors as is the case with garlic. Firstly it is chemically complex, there are more than 75 biologically active constituents in the gel277 and over 200 in the leaf, some of which are volatile and oxidise/degrade very rapidly on exposure to air.309 In addition preparations may have varying levels of “contaminants” like hydroxyanthracene glycosides depending on the starting material and processing used,382 indeed some preparations are actually derived from the whole leaf and contain both fractions.277 Even though the gel is treated to stabilise it chemically (heated/treated with anti-oxidants), and keep it free of bacterial contamination, this does not necessarily ensure a stable product and new compounds may form during storage.310
Secondly the constituent(s) responsible for the pharmacological activity of the gel are uncertain and although acemannan has been assumed to be the main active there are a number of different constituents that have activity.309 In vitro the polysaccharides are immune modulatory and anti-inflammatory, the glycoproteins are vulnerary with possible antitumour and anti-ulcer effects, the hydroxyanthracenes are purgative, anti-inflammatory, anti-oxidant and anti-proliferative. This makes standardisation a very complex task and as yet there are no accepted protocols for the extraction, processing and stabilisation of the raw material so that the end-products are inconsistent.309,311 Not only has variable quality of commercial gel312,313 (and latex282) products been reported but adulteration of the gel also occurs.314
Finally the fresh gel is pharmacologically different from that produced by processing. Gel preparations lose their UV protection activity as early as one month after processing277 and whilst the fresh gel promoted cell growth and attachment, the processed gel was cytotoxic to normal as well as cancer cells.291
In vivo the mechanism behind the herb's actions is yet to be fully determined but it seems certain that the results of each trial product cannot easily be extrapolated to another due to their great variation. Currently there is greater interest in, and investigation into, the gel rather than the latex, particularly for topical use.
Immunomodulatory
In vitro—Different cells respond to the polysaccharide fraction, particularly acemannan,315 by releasing cytokines316 that stimulate immune function, However humans lack the necessary enzyme to break down acemannan277 and its seems to pass through the digestive tract unchanged. Whilst it may have a local effect in the digestive tract it is considered unlikely that acemannan is responsible for any immunomodulatory effects attributed to aloe.295 Aloeride, a potent immune stimulator/macrophage activator, although present at low concentration, possibly as a contaminant may in fact be responsible.295
Components of the gel activate complement and stimulate polymorphonuclear neutrophil activity whilst reducing the damage associated with free oxygen radicals.317 However low molecular weight constituents in the gel may be cytotoxic.318
Antimicrobial
In vitro—As well as stimulating macrophage activity the latex has direct activity against Leishmania spp.319 and the anthraquinones, aloin in particular, have antibacterial320 and antiviral properties.321 Aloin inhibits bacterial collagenase and may help moderate host cell damage during infection.322
The gel is active against Shigella flexneri, Streptococcus pyogenes323 and Trichomonas vaginalis324 and acemannan enhances macrophage destruction of Candida albicans.277
In vivo—Aloe was part of a preparation used to successfully treat HPV infections topically.325
Anticancer
In vitro—Constituents of Aloe (mostly hydroxyanthracene derivatives but also the phthalate) are anti-proliferative in a number of cancer cell lines,326–332 inhibit angiogenesis,333 are antimutagenic303,334 and may have anti-carcinogenic335 activity. However emodin and aloe-emodin are both potentially genotoxic.334
In vivo—Aloe tincture added to melatonin seemed to be a promising treatment for intractable solid tumours.336
Vulnerary
Aloe gel has been subject to a number of tests related to wound healing and skin protection.
In vitro—Vulnerary actions that have been established for the gel or its constituents include:-
- increased growth of various connective tissue cells, including those derived from healthy and diabetic sources337–341
- protection of cells from radiation damage342,343
- promote angiogenesis (new blood vessel growth)301
- anti-oxidant activity304
Whole leaf extracts and aloe emodin344 may however increase the potential for UVA light to cause oxidative damage to skin even though some of the anthraquinones are themselves anti-oxidants during irradiation.345
In vivo—Plant derived complex carbohydrates, including those of Aloe, protect the skin's immune system from UV damage.346 However Aloe's vulnerary and cell-protection activities have produced contrary results possibly for reasons highlighted above. Benefits from topical application include:-
- aid to prevention of skin ulcers due to impaired circulation347
- increased skin hydration i.e. it is an effective moisturiser348
- improvement in occupational irritant contact dermatitis using gel-coated latex gloves349
- anecdotal resolution of a case of lichen planus350
- improvement in healing time, with reduced infection, in burns treatment351,352
- improvement of psoriasis,353 (not corroborated)354
A preparation containing acemannan used topically after tooth extraction reduced the incidence of alveolar osteitis.355
Negative trials claim no clear benefit in treating aphthous ulcers,356 pressure ulcers357 or protecting or treating sunburn due to UVB light.358 One study found the gel apparently delayed healing of surgical wounds.359
Aloe gel's use for radiation burns dates back to the 1930s when its benefits were reported in a number of cases. Some recent attempt has been made to validate these protective effects against radiotherapy damage. Again results have been mixed ranging from success291,360 to no benefit either in topical form361–363 or orally for mucus membranes.364 These results have been reviewed.365,366
Anti-inflammatory
In vitro—Individual constituents of Aloe are anti-inflammatory—glucans,297 chromone,284 glycoprotein,367 carboxypeptidase (inactivation of bradykinin)305 and trace elements.368 The whole leaf extract also inhibits 5-LOX activity369 and the gel is anti-inflammatory in inflamed colorectal mucosal biopsy cells, through cytokine inhibition and antioxidant activity.370 In fact leaf extracts of plants older than 2 years have exhibited stronger anti-oxidant activity than vitamin E371—an activity linked to the chromones285 and dihydrocoumarins.288
In vivo—Aloe gel had no significant benefits for irritable bowel syndrome although it helped improve diarrhoea or alternating bowel habit whilst it was being taken.372 It did however give some improvement, with apparent anti-inflammatory effects, in ulcerative colitis.373
Other
In vitro—The whole leaf extract inhibits cholinesterase activity369 whilst the trace elements seem responsible for anti-spermicidal374 and anti-diabetic307 properties (this is a traditional use).375
In vivo—aloe gel preparations were found to:-
- slow down the rate but increase the level of absorption of vitamins C and E376
- increase excretion of precursors to kidney stone formation, so may be a prophylactic for lithiasis377,378
- reduce hyperlipidaemia particularly triglyceride levels379
- reduce blood sugar in diabetic patients379 (not corroborated.380 Reviewed381,382)
The laxative actions are associated with the hydroxyanthracene derivatives—see Cassia spp. (senna).
Medicinal uses
Gastro-intestinal
- constipation (latex)
Externally
- burns
- wounds
Pharmacy
| Once daily (latex) | |
| Powder | – 50–200 mg |
| Tincture 1:40 (45%) | – 2–8 ml383 |
The laxative effect of aloe is due to aloin which passes through the digestive tract unchanged until it reaches the bowel where it is transformed to aloe-emodin-9-anthrone by intestinal bacteria,277 an action that occurs 6–12 hours after ingestion. The laxative action involves increased water and electrolyte secretion in the colon which stimulates peristalsis384—(see Cassia).
Gel applied topically is best used fresh. The gel used orally to treat ulcerative colitis was a commercial product used at a dose of 100 ml twice a day but introduced at doses of 25–50 ml twice daily for 3 days to establish tolerability.373
CONTRAINDICATIONS—Intestinal obstruction and abdominal pain of unknown origin. Patients with haemorrhoids should rather be given bulk laxatives.
Precautions and/or safety
Latex—Should be combined with a carminative to reduce griping. This stimulating type of laxative should not be used for longer than 10 days. Possible minor side-effects are diarrhoea, pseudomelanosis coli (see Cassia), red coloured urine. More serious effects can result from overdose or chronic use such as hypokalaemia, electrolyte imbalance and renal damage. Steatorrhoea, hypoalbuminaemia and osteomalacia have also been reported.291
Gel—The incidence of contact allergy to aloe gel appears to be quite low385 but there are reports of hypersensitivity,386 disseminated dermatitis in a patient with stasis dermatitis,291 photodermatitis387 and severe dermatitis when used on skin that had been subjected to dermabrasion.388 Internal gel use has been reportedly associated with Henoch-Schonlein purpura,389,390 acute toxic hepatitis391,392 and thyroid dysfunction (topical and internal use).393
Aloe gel may have genotoxic properties but it is not cytotoxic and does not appear to cross cell membranes.394
Pregnancy and lactation—anthraquinone metabolites of Aloe are secreted in breast milk and should be used cautiously291 although more recent reviews have cleared Cassia and Rhamnus for use in this situation (see Cassia).
Interactions
There is a reported interaction between Aloe tablets taken prior to surgery and sevoflurane, an anaesthetic drug, which lead to increased bleeding during surgery.395
Other cautions are hypothetical rather than actually reported. One is the possibility that aloe may lower blood sugar and therefore care should be taken by those using hypoglycaemics. The other is that the latex may reduce the absorption of other drugs by decreasing intestinal transit time. Chronic use or abuse of Aloe latex which leads to hypokalaemia could potentiate the effect of cardiac glycosides, (like digitalis), or anti-arrhythmics and exacerbate potassium deficiency induced by thiazide diuretics or adrenocorticosteroids.
Historical uses
As for modern uses. Applied to fingernails to stop children biting them.
Chamaelirium luteum
Helonias root, false unicorn root

Family Liliaceae
Description
An erect, dioecious, perennial herb with tuberous roots, growing from 60–100 cm tall. Female plants taller and more leafy than male plants. Basal leaves spatulate to obovate, 7–15 cm long, in basal rosette. Stem leaves progressively reduced and narrowed upward along the stem. Flowers yellowish, in crowded spikes, usually drooping at the top, flowering from May to July in their native woods in North America.
Habitat and cultivation
Native to rich woods in West Massachusetts, New York to Florida, Arkansas to Illinois and Michigan. Also sometimes planted in shady places in American gardens.
Parts used
Rhizome and root, collected in autumn.
Active constituents
Little information is available as it is not a well studied plant.
1) Steroidal saponins, including diosgenin and its derivatives chamaelirin1 (9.5%), helonin.
Also contains starch, calcium oxalate and an oleoresin.
Actions
1) Uterine tonic
Scientific information
There are no modern investigations into this herb. Its western history is closely allied to that of Aletris farinosa for which it seems to have been used interchangeably.3 With the degree of confusion between the two and no scientific study into either herb it is difficult to know to what extent their actions have been confused and interchanged too. It is possible that Chamaelirium substituted for Aletris gave the latter herb its reputation for treating gynaecological problems. Likewise Chamaelirium's usefulness in treating gastro-intestinal problems may have been due to the presence of Aletris. This herb comes from the American Indian tradition.
Medicinal uses
Reproductive tract
The action is presumed to derive from the steroidal saponins:
- dysmenorrhoea†
- amenorrhoea
- infertility
- irregular menstruation
- leucorrhoea
- uterine prolapse
- pelvic congestion
- pelvic inflammatory disease
The herb is also reported to be useful for morning sickness in pregnancy and in threatened miscarriage, due to atony of the uterus.
Pharmacy
| Three times daily | |
| Decoction of dried root | – 1–2 g |
| Tincture 1:5 (45%) | – 2–5 ml |
| Fluid Extract (45%) | – 1–2 ml |
Precautions and/or safety
In large doses it can cause nausea and vomiting. Chamaelirin is suspected of being cardiotoxic, large doses of the herb should be avoided.1
Historical uses
Anthelmintic; tonic for urinary and reproductive tracts; emetic and diuretic. A liver remedy to improve anabolism. Also for dyspepsia, colic, indigestion. Purported to alkalinise urine.
Convallaria majalis [Restricted Herb]
Lily-of-the-Valley

Family Liliaceae
Description
A perennial with a creeping rhizome. Leaves usually 2, elliptic, glabrous, glossy green 8–20 cm topping stems with papery sheathing bracts. Flowers, 5–10, pure white, sweetly scented and pendulous growing on one side of the curved stem, above a pair of leaves. Perianth broadly bell-shaped 6–8 mm with short, recurved, triangular lobes. Fruit bright red, globular, poisonous berries. Flowers mid spring to early summer.
Habitat and cultivation
Native to most of Europe and Britain, growing in dry woods and thickets on calcareous soils. Naturalized in north eastern North America. Cultivated in gardens for its beauty and fragrance. Grown from separated crowns and forms large patches if undisturbed.
Parts used
Leaves or whole plant harvested in flower. The fresh leaves are, according to Weiss, the strongest medicine followed by the flowers. The berries are highly toxic.
Active constituents2
1) Cardioactive glycosides (0.1–0.5%) including the cardenolides convallatoxin, convalloside, convallatoxol396–399
2) Steroidal saponins—progesterone has been reported in the leaves400,401
3) Flavonoids402
Other constituents include an analogue of the amino acid, proline403 and chelidonic acid.404
Actions
1) Cardioactive
2) Cardiac tonic
Scientific information
Convallaria has been an official medicine in a number of countries.383 Its acts like Digitalis to increase the excitability of heart muscle and its force of contraction and slows ventricular contraction, these actions being effected through electrolyte changes. It is considered a much safer remedy than Digitalis. The main active constituent is convallatoxin but its bioavailability is aided by some of the apparently non-active constituents of the herb. Used in Denmark to treat epilepsy, an extract was shown to have some affinity for GABA receptors in animal tissue in vitro.405 It is now a restricted herb.
Medicinal uses
Traditional uses of the herb includes:-
- arrhythmia
- congestive heart failure†
- atrial fibrillation
- oedema of cardiac origin and cardiac asthma
- angina
- coronary insufficiency
- hypotension
Precautions and/or safety
Convallaria is apparently a common cause of plant poisoning in children.406 It can cause respiratory allergies due to the strong scent of the flowers.407 Its main side-effects in overdose include arrhythmias, nausea, vomiting, diarrhoea, intestinal colic, headache, lethargy and visual disturbances (it is reported to affect colour perception408). However the herb is not known to have caused any human fatalities.409
Interactions
It is likely to interact with other cardiac glycoside containing medicines.
Smilax ornata and spp.
Sarsaparilla
Family Liliaceae
Description
Evergreen vines to 4 m. Stems twining and trailing with paired tendrils growing from leaf axils. Leaves alternate, orbicular-ovate. Flowers small, greenish, in axillary umbels.
Taste—sweet and acrid, mucilaginous and almost odourless.
Habitat and cultivation
Native to tropical America in rich, moist soils in semi-shady, sheltered situations. Propagated from cuttings. The medicinal species are both drought and frost tender.
Parts used
Root and rhizome of spp. Those used are:
S. aristolochiaefolia (S. medica)—Grey or Mexico Sarsaparilla
S. febrifuga (S. officinalis)—Ecuador or Guayaquil Sarsaparilla
S. ornata—Jamaica, Costa Rica or Red Sarsaparilla
S. regelii—Honduras or Brown Sarsaparilla
Active constituents
1) Steroidal saponins (up to 3%) based on either smilagenin or sarsapogenin. Parillin and smilacin are glycosides of the latter, possibly formed as a by-product of processing1,410,411
2) Phytosterols including β-sitosterol and stigmasterol
3) Flavonoids including astilbin and its derivatives, smitilbin, resveratrol, dihydroxyquercetin and taxifolin412–416
Also contains proteins (smilaxin417 and a lectin418), essential oil, phenylpropanoids, resin, starch, calcium oxalate and sarsapic acid.
Nutritional constituents
Vitamins: A, B complex, C and D
Minerals: Potassium (approx. 1.25%), iron, manganese, sodium, silica, sulphur, copper, zinc and iodine
Actions
1) Alterative
2) Anti-inflammatory
3) Antipruritic
4) Diuretic
5) Antiseptic
6) Antirheumatic
Scientific information
S. ornata was part of the medical tradition in a number of countries including China and has been an official medicine throughout the world.383,410
Much of the chemical analysis of the steroidal saponins was undertaken many decades ago. However there is still ongoing research into the herb's constituents and their actions although this has comprised either in vitro or animal based studies. There are no modern clinical trials reported.
In vitro—Smilax was used traditionally to treat infectious conditions. It inhibits pathogenic dermatophytes419 and the steroidal saponins have some antifungal activity against Candida spp.410,411
A decoction of Smilax is cytotoxic to liver cancer cells420 (it has been used in combination with other herbs, to treat cancer in Sri Lanka).
Some of the constituents have been tested in vitro. Astilbin inhibits delayed type hypersensitivity and may reduce the inflammatory damage of auto-immune diseases414 whilst smilaxin attenuates HIV-reverse transcriptase417 and the lectin has antiviral activity against HSV-1 and respiratory syncytial virus.418
In vivo—Animal studies suggest Smilax may have hepatoprotective properties415,421 and that it is anti-inflammatory, modulating cytokine release.422
Other research is now somewhat dated but includes its use in a herbal combination to benefit patients with chronic hepatitis B423 and on its own to help in the treatment of leprosy424,425 and psoriasis.426
Chinese uses of Smilax include detoxification, relief of dampness and joint problems and it has also been used to treat and prevent syphilis, leptospirosis, acute bacterial dysentery, acute and chronic nephritis.414
Medicinal uses
Musculoskeletal
- gout
- arthritis
- rheumatoid arthritis
- chronic rheumatism
Skin
- psoriasis
- eczema
- skin conditions
Pharmacy
| Three times daily | |
| Decoction of dried root | – 2–4 g |
| Fluid Extract (50%) | – 2–4 ml |
Precautions and/or safety
May cause gastric irritation. It has been suggested the herb could lead to a temporary impairment of the kidneys although there is no apparent evidence to support this, it may relate to its calcium oxalate content. Contrary to this is the traditional understanding that it aids excretion of chlorides and uric acid (BHC), is a noted diuretic and is used in traditional Chinese medicine to treat nephritis.
Historical uses
As above. Also used in passive dropsy and venereal diseases. Asthma (smoke inhalation).
Trillium erectum
Bethroot, birthroot

Family Liliaceae
Description
A perennial with a short thick rootstock, growing to 60 cm tall in flower. Leaves sessile, triangular oval, to 12 cm long, 3 in a single terminal whorl, subtending a flower on a peduncle 10 cm long. Sepals 3, green; petals spreading from the base, brownish-purple or purple, sometimes white, yellow or green, to 5 cm long, nearly erect, ill-scented. Ovary purple, fruit a dark red 6-angled berry with 3 seeds. Flowers from April to June in North America.
Habitat and cultivation
Originally native to North America in rich woodlands from Nova Scotia to Georgia in mountainous regions, Florida, Tennessee to Michigan, and Ontario. It prefers rich, damp soils in protected shaded situations and may be grown from seed although germination is poor. It is generally transplanted from the wild after flowering and may also be grown from division. Grown in similar situations to Paeonia (peony). Frost resistant but drought tender.
Parts used
The roots and rhizomes.
Active constituents
1) Steroidal saponins including trillarin, trillin, kryptogenin and diosgenin427
2) Steroidal glycosides
3) Tannins
4) Fixed oil
Actions
1) Antihaemorrhagic
2) Mild expectorant
3) Astringent
Other actions ascribed to the herb include partus praeparator, antiseptic and tonic.
Scientific information
The herb, used by American Indians to facilitate childbirth, was an official medicine in the USA. The chemical analysis was carried out many decades ago and the pharmacology is largely unexplored but the steroidal constituents must account for its action on the female reproductive tract.
While its haemostatic properties are largely employed in the reproductive tract it was also used to staunch bleeding elsewhere e.g. in the urinary and respiratory tracts.
Medicinal uses
Respiratory tract
In the symptomatic treatment of:
- haemoptysis
Urinary tract
In the symptomatic treatment of:
- haematuria
Reproductive tract
Used in the treatment of uterine bleeding but also as a tonic and astringent:
- menorrhagia
- metrorrhagia
- leucorrhoea
BHP specific for menopausal menorrhagia with depression.
Externally
- leucorrhoea (douche)
- vaginal infections (douche)
- indolent ulcers (poultice/ointment)
Pharmacy
| Three times daily | |
| Decoction of dried herb | – 0.5–2 g |
| Tincture 1:5 (40%) | – 1–4 ml |
| Fluid Extract (25%) | – 0.5–2 ml |
Used in combination with Ulmus rubra and Lobelia inflata, as powders, for ulcers.
Historical uses
Internally used for diarrhoea and dysentery; bronchial problems—coughs—was called “cough root”, diabetes. Externally for halting gangrene; tumours, insect stings.
Urginea maritima
White squill
Description
A large perennial bulb 10–15 cm across, from which arise, in autumn, long, leafless, unbranched flower stems 1–1½ m tall, bearing spikes of numerous spirally arranged flowers in a cylindrical cluster about 30 cm or more long. Perianth 8 mm long, white, with green or purplish midveins; anthers short and greenish. Flower stalks spreading and 2–3 times as long as bracts. Leaves appear only after flowering and persist into the following summer. They are large, lance-shaped 15–30 cm × 2½–10 cm slightly fleshy, smooth, flat and glossy. Bulbs are often partly exposed. Flowers in autumn.

Family Liliaceae
Habitat and cultivation
Native to Mediterranean Europe, the Canary Islands and South Africa growing in sandy rocky places along the coast. Cultivated for medicine in Italy and Malta.
Parts used
The bulb collected soon after flowering, sliced and dried.
Active constituents
1) Cardiac glycosides of the bufadienolide type based on scillaren and scilliphaeosidin. There are also bufadienolides that are not glycosides428–430
2) Flavonoids based on quercetin and kaempferol and also glycosylflavones.431,432
Also contains mucilage, sinistrin (a fructan) and calcium oxalate.
Actions
1) Expectorant
2) Cardioactive
3) Diuretic
4) Cathartic
5) Emetic
Scientific information
This herb was known and used by ancient civilisations. The use of squill for treating coughs was supposed to have been discovered by Pythagoras in the 6th Century BC.433 It was also used in medieval times to treat dropsy/oedema.
The cardiac glycosides like those of Digitalis and Convallaria, increase the force of contraction of the heart (inotropic)434 thereby improving circulation and kidney function. However these glycosides are not well absorbed and the action of Urginea is much weaker than that of Digitalis.383
Its acts on the respiratory tract by reflex irritation of the gastric mucosa causing an increase in mucous secretions.383
Medicinal uses
It was used traditionally for treating:-
- chronic bronchitis
- pertussis
- mild cardiac insufficiency
- pulmonary catarrh
- asthma
- emetic (in large doses)
There is a variety of Urginea maritima, called red squill, which contains the toxin scilliroside, that was used at one time as a rat poison.383
CONTRAINDICATIONS—Hypokalaemia and impaired renal function.
Precautions and/or safety
The herb can cause nausea, vomiting, diarrhoea and reduced heart rate. In large enough doses it may be fatal435 although the emetic action should offer some protection against the cardio-toxicity that would occur from overdosing.
Interactions
Should not be used with Digitalis or other cardiac glycoside medications.
_______________
†Associated with a dragging sensation.
†Especially that associated with bradycardia.