Psoriatic arthritis is a chronic inflammatory arthritis that affects 5–30% of persons with psoriasis. Some pts, especially those with spondylitis, will carry the HLA-B27 histocompatibility antigen. Onset of psoriasis usually precedes development of joint disease; approximately 15–20% of pts develop arthritis prior to onset of skin disease. Nail changes are seen in 90% of pts with psoriatic arthritis.
There are 5 patterns of joint involvement in psoriatic arthritis.
• Asymmetric oligoarthritis: often involves distal interphalangeal/proximal interphalangeal (DIP/PIP) joints of hands and feet, knees, wrists, ankles; “sausage digits” may be present, reflecting tendon sheath inflammation.
• Symmetric polyarthritis (40%): resembles rheumatoid arthritis except rheumatoid factor is negative, absence of rheumatoid nodules.
• Predominantly DIP joint involvement (15%): high frequency of association with psoriatic nail changes.
• “Arthritis mutilans” (3–5%): aggressive, destructive form of arthritis with severe joint deformities and bony dissolution.
• Spondylitis and/or sacroiliitis: axial involvement is present in 20–40% of pts with psoriatic arthritis; may occur in absence of peripheral arthritis.
• Negative tests for rheumatoid factor.
• Hypoproliferative anemia, elevated erythrocyte sedimentation rate (ESR).
• Hyperuricemia may be present.
• HIV infection should be suspected in fulminant disease.
• Inflammatory synovial fluid and biopsy without specific findings.
• Radiographic features include erosion at joint margin, bony ankylosis, tuft resorption of terminal phalanges, “pencil-in-cup” deformity (bone proliferation at base of distal phalanx with tapering of proximal phalanx), axial skeleton with asymmetric sacroiliitis, asymmetric nonmarginal syndesmophytes.
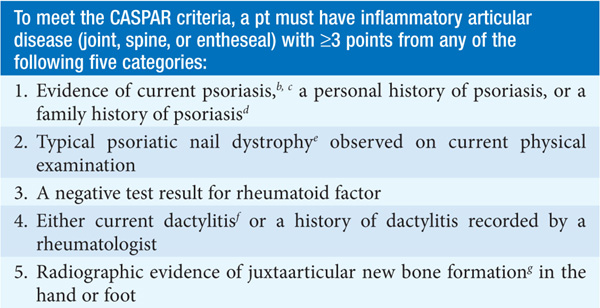
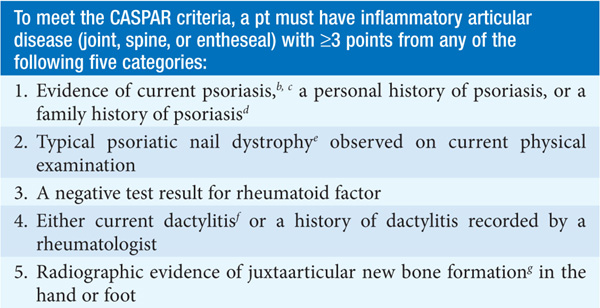
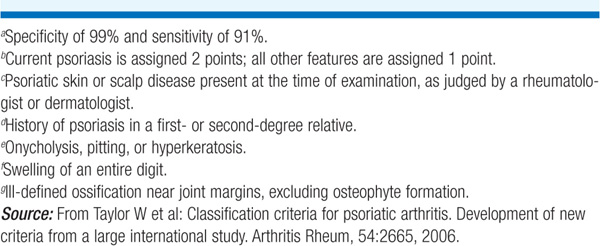
TABLE 172-1 THE CASPAR (CLASSIFICATION CRITERIA FOR PSORIATIC ARTHRITIS) CRITERIAa
TREATMENT Psoriatic Arthritis
• Coordinated therapy is directed at the skin and joints.
• Pt education, physical and occupational therapy.
• TNF modulatory agents (etanercept, infliximab, adalimumab, golimumab) can improve skin and joint disease and delay radiographic progression.
• Alefacept in combination with methotrexate can benefit skin and joint disease.
• NSAIDs.
• Intraarticular steroid injections—useful in some settings. Systemic glucocorticoids should rarely be used as may induce rebound flare of skin disease upon tapering.
• Efficacy of gold salts and antimalarials controversial.
• Methotrexate 15–25 mg/week and sulfasalazine 2–3 g/d have clinical efficacy but do not halt joint erosion.
• Leflunomide may be of benefit for skin and joint disease.

For a more detailed discussion, see Taurog JD: The Spondyloarthritides, Chap. 325, p. 2774, in HPIM-18.