CHAPTER 1
Maternal heart health
Karen Sliwa1, John Anthony2, and Denise Hilfiker-Kleiner3
1 University of Cape Town, South Africa; University of the Witwatersrand, Johannesburg, South Africa
2 Department of Obstetrics & Gynaecology, Groote Schuur Hospital, Cape Town, South Africa
3 Department of Cardiology and Angiology, Medical School Hannover, Germany
1.0 Introduction
In this chapter, we first report upon a recent single-center prospective cohort study from Groote Schuur Hospital [13] in which the majority of maternal deaths observed were attributable to various forms of cardiomyopathy (CMO), with only two being related to complications of sepsis and thrombosis affecting prosthetic heart valves. Significantly, 8 out of the 9 deaths reported in this patient cohort of 152 patients with 6-month follow-up would not have been reported if the definition of death within 42 days had been applied, thereby underestimating the number of cardiac deaths related to pregnancy as a result of late presentation and deaths occurring among women with familial CMO or PPCMO.
The last decade has seen a steady increase in the institutional maternal mortality rate for cardiac disease in South Africa [14]. While the maternal mortality rate was 3.73 % per 100,000 live births during the period 2005 to 2007, this rose to 5.64 in 2008 to 2010 and further still to 6 % during 2011 to 2013. After nonpregnancy-related infections, cardiac disease is the second most common cause of indirect maternal death, with complications of rheumatic heart disease (RHD) and CMO being the most significant contributors to cardiac deaths. The fact that more than half of those cases occurred postpartum is noteworthy; it implies that the maternal death rate in South Africa—already estimated to be 176/100,000 [1]—is probably grossly underestimated, as death could only be reported until 42 days postpartum.
Valvular heart disease (VHD) in pregnant women, whether due to congenital or acquired etiologies such as RHD, poses a particular challenge to clinicians and their patients. Significant valve disease increases the risks associated with pregnancy to both mother and fetus and requires a careful preconception risk assessment as well as specialised care during gestation to minimize maternal and fetal morbidity and mortality. Ideally, all women with VHD would undergo preconception evaluation, including advice on risk prediction and contraception, by a joint cardiac–obstetric team seeking advice from other specialties [15]. Of note, recent findings from the Global Rheumatic Heart Disease Registry (REMEDY) (see Section 2) indicated that of 1,825 women with RHD in child-bearing age, only 3.6% were using contraception [16].
PPCMO is a disease particularly common in African women. It develops in previously healthy women peripartum and carries a mortality rate of approximately 15%. In a recent publication we summarize the prevalence, clinical presentation, and natural history of PPCMO treated with standard HF medication [17]. Close collaboration with basic scientists from Hannover University, Germany, gave rise to unique translational research involving several animal models and human biological samples, providing breakthrough evidence [18] on the pathogenesis of human PPCMO. Treatment of mice (which serve as a model for human PPCMO) with bromocriptine, a dopamine antagonist inhibiting prolactin, prevented the development of the disease. Figure 1.1 summarizes the possible metabolic events leading to PPCMO.

Figure 1.1 Basic mechanisms underlying peripartum cardiomyopathy.
Subsequent to this foundational research, a South African clinical trial in women with newly diagnosed PPCMO [19] was conducted. The trial showed significant clinical improvement in those treated with bromocriptine, compared to patients receiving only standard care. These initially positive results have since been confirmed via collaborative research in a German cohort [20], and this ongoing work was recently summarized in an invited review on this new treatment modality [21]. In conclusion, joint obstetric-medical-cardiac clinics will be the optimal approach for women presenting with cardiac disease in the peripartum period in sub-Saharan Africa. Appropriate guidance in referral to secondary and tertiary care hospitals with dedicated cardiac disease in maternity clinics should be implemented and is currently being explored in South Africa [13].
1.1 Spectrum of maternal cardiac disease in South Africa
Sliwa K, Libhaber E, Elliott C, Momberg Z, Osman A, Zühlke L, Lachmann T, Nicholson L, Thienemann F, Roos-Hesselink J, Anthony J. Spectrum of cardiac disease in maternity in a low-resource cohort in South Africa. Heart 2014; 100(24):1967–74. [13]
1.1.1 Background
Data focusing on the spectrum and characteristics of cardiovascular disease (CVD) among women in LMIC are limited, especially among those who are pregnant [22,23]. In sub-Saharan Africa this significant clinical research gap is exacerbated by a shortage of physicians and health care resources.
1.1.2 Study aims
The aims of this study were to examine the spectrum and characteristics of CVD presenting in the prepartum and postpartum period, as well as describe maternal and fetal outcomes, in a representative cohort of African women in Cape Town, South Africa.
1.1.3 Methods
1.1.3.1 Patient enrollment
During the period 1 July 2010 to 30 June 2012, 225 consecutive pregnant women with suspected or previously diagnosed CVD were assessed at their first visit to the joint cardiac–obstetric clinic, having been directed there via a referral algorithm from primary care and secondary care facilities in Cape Town and from within the tertiary hospital (see Figure 1.2). All referred patients were seen by a senior cardiology and obstetric consultant, and physicians from other disciplines (i.e., radiology, endocrinology, and anesthetics) were consulted. Patients were then assessed throughout their pregnancy, while those presenting postpartum were seen once at this clinic and subsequently managed at the general cardiac clinic or a dedicated CMO clinic, at Groote Schuur Hospital, Cape Town, South Africa. Patient appointments were scheduled according to standard management, which could entail a waiting period of up to 3 months. Patients with a history of CVD and a normal clinical inspection, along with minimal echocardiography changes, were seen only on one occasion early and subsequently referred to second-level obstetric care. Most patients were referred from peripheral hospitals; therefore, records were not available to document maternal and fetal outcomes. Those patients who presented with signs, symptoms, or a World Health Organization (WHO) classification stage of II–IV underwent clinical visits at <28 weeks (second trimester), 28 to 37 weeks (third trimester), onset of labor until hospital discharge (peripartum period), and at 6 weeks and 6 months postpartum.

Figure 1.2 Referral algorithm to joint Cardiac Maternity Clinic, Groote Schuur Hospital.
1.1.4 Results
As detailed in Table 1.1, patients of African ancestry were significantly more likely to present with advanced disease (WHO II–IV) than those of other ethnic groups (p < 0.0001). Patients in the modified WHO class II–IV exhibited significantly higher heart rate (p < 0.0001) and gravidity (p = 0.0002) than those in WHO class I. Comorbidity, including HIV infection, was associated with more severe cardiac disease (p < 0.0001). Overall, 73 (32.4%) patients were classified as WHO class I; of these, 27 (37.0%) had been referred for other reasons such as history of palpitations or the need for pre-conception counseling, 26 (35.6%) presented with minor or operated CHD and no significant residual structural abnormality, 16 (21.9%) had RHD, and 4 (5.5%) had chronic hypertension with no end-organ damage. The remaining 152 (67.6) patients were placed in WHO class II–IV and required close follow-up; of these, 21 (13.8%) presented with PPCMO, 15 (9.9%) with prior CHD surgical correction, 15 (9.9%) with prior surgery for RHD, 11 (7.2%) with idiopathic dilated CMO, 9 (5.9%) with hypertension-related CMO, 8 (5.3%) with atrial septal defect, 6 (4.0%) with ventricular septal defect, 5 (3.3%) with ventricular arrhythmias, 4 (2.6%) with Takayasu’s disease, 4 (2.6%) with Marfan’s disease, 3 (2.0%) with coarctation, and 3 (2.0%) with constrictive pericarditis. Notably, IHD was absent in this cohort. Figure 1.3 displays the distribution of patients per disease group.
Table 1.1 Patients’ demographic and clinical characteristics according WHO functional class.
| WHO I (n = 73) | WHO II–IV (n = 152) | All (n = 225) | |
| Age (years) | 28.8 ± 7.0 | 28.5 ± 6.1 | 28.6 ± 6.4 |
| Ethnicity | |||
| African ancestry | 23 (31.5%) | 79 (52.0%) | 101 (44.9%) |
| Mixed | 15 (20.6%) | 56 (36.8%) | 72 (32.0%) |
| Caucasian | 19 (26.0%) | 15 (9.9%) | 34 (15.1%) |
| Other | 16 (21.9%) | 2 (1.3%) | 18 (8.0%) |
| Medical history | |||
| Hypertension | 2 (2.7%) | 10 (6.6%) | 12 (5.3%) |
| Hypercholesterolemia | 0 (0%) | 3 (2.0%) | 3 (1.3%) |
| HIV infection | 2 (2.7%) | 36 (23.7%) | 38 (16.9%) |
| Syphilis | 0 (0%) | 1 (0.7%) | 1 (0.4%) |
| TB | 0 (0%) | 4 (2.6%) | 4 (1.8%) |
| Clinical history | |||
| Previously known CVD | 40 (54.8%) | 53 (34.9%) | 93 (41.3%) |
| Previous CVD operation | 27 (37.0%) | 30 (19.7%) | 57 (25.3%) |
| NYHA Class I–II | 73 (100%) | 120 (78.9%) | 193 (85.8%) |
| NYHA Class III–IV | 0 (0%) | 32 (21.1%) | 32 (14.2%) |
| Systolic BP (mm Hg) | 118 ± 13 | 119 ± 16 | 119 ± 15 |
| Diastolic BP (mm Hg) | 75 ± 10 | 74 ± 11 | 74 ± 11 |
| Heart rate (beats/min) | 78 ± 12 | 90 ± 19 | 86 ± 18 |
| Weight (kg) | 72.5 ± 12.5 | 72.1 ± 18.6 | 72.1 ± 16.8 |
| Obstetric history | |||
| <12 weeks | 3 (4.1%) | 4 (2.6%) | 7 (3.1%) |
| 12 to 24 weeks | 32 (43.8%) | 52 (34.2%) | 84 (37.3%) |
| >24 weeks | 31 (42.5%) | 66 (43.4%) | 97 (43.1%) |
| Median gravida (range) | 2 (1–6) | 2 (1–7) | 2 (1–7) |
| Median para (range) | 1 (0–4) | 1 (0–5) | 1 (0–5) |
| Nulliparous | 29 (39.7%) | 36 (23.6%) | 65 (28.9) |
| Twin pregnancies | 0 (0%) | 3 (2.0%) | 3 (1.3%) |

Figure 1.3 Case distributions according to disease categories.
As shown in Table 1.2, 122 (80.3%) patients presented prepartum, including 66 (54.1%) presenting for the first time with a gestational age entry at >24 weeks. Patients of African ancestry were more likely to present postpartum (p = 0.009). Overall, 30 (19.7%) patients presented in the postpartum period with severe functional impairment as measured by NYHA class (p < 0.001) and displayed significantly higher NTproBNP levels (p < 0.0001) and heart rate (p < 0.001). Patients presenting with developing symptoms of PPCMO had significantly larger LV dimensions and with a markedly lower left ventricular ejection fraction (LVEF) (44.7 ± 11.8% versus 54.5 ± 12.4%; p < 0.003). Of the women diagnosed with CVD prepartum, 27% received diuretics, 7.3% beta blockers, and 7.3% warfarin while pregnant.
Table 1.2 Patients’ demographic and clinical characteristics.
| Presenting Prepartum (n = 122) | Presenting Postpartum (n = 30) | All (n = 152) | |
| Age (years) | 28.2 ± 6.2 | 29.6 ± 5.8 | 28.5 ± 6.1 |
| Ethnicity | |||
| African ancestry | 55 (45.1%) | 24 (80.0%) | 79 (51.9%) |
| Mixed | 50 (41.0%) | 6 (20.0%) | 56 (36.8%) |
| White | 15 (12.3%) | 0 (0%) | 15 (9.9%) |
| Other | 2 (1.6%) | 0 (0%) | 2 (1.3%) |
| Language | |||
| Afrikaans | 40 (32.8%) | 3 (10.0%) | 43 (28.3%) |
| English | 29 (23.8%) | 4 (13.3%) | 33 (21.7%) |
| isiXhosa | 41 (33.6%) | 17 (56.6%) | 58 (38.2%) |
| isiZulu | 9 (7.4%) | 3 (10.0%) | 12 (7.9%) |
| Education level | |||
| Year 1–7 | 36 (29.5%) | 10 (33.3%) | 46 (30.3%) |
| Year 8–11 | 73 (59.8%) | 19 (63.3%) | 92 (60.5%) |
| Income per month (ZAR) | |||
| <300 | 39 (32.0%) | 17 (56.7%) | 56 (36.8%) |
| 300–999 | 31 (25.4%) | 7 (23.3%) | 38 (25.0%) |
| 1,000–9,999 | 48 (39.3%) | 6 (20.0%) | 54 (35.5%) |
| General medical history (%) | |||
| Hypertension | 10 (8.2%) | 0 (0%) | 10 (6.6%) |
| HIV infection | 26 (21.3%) | 10 (33.3%) | 36 (23.6%) |
| TB | 3 (2.5%) | 1 (3.3%) | 4 (2.6%) |
| CVD family history | 21 (17.2%) | 2 (6.7%) | 23 (15.1%) |
| PPCMO/CMO family history | 10 (8.2%) | 1 (3.3%) | 11 (7.2%) |
| Heart valve replacement | 16 (13.1%) | 0 (0%) | 16 (10.5%) |
| Obstetric history | |||
| Presenting with prepartum | |||
| 12 to 24 weeks | 52 (42.6%) | 0 (0%) | 52 (34.2%) |
| >24 weeks | 66 (54.1%) | 0 (0%) | 66 (43.4%) |
| Nulliparous | 32 (26.2%) | 4 (13.3%) | 36 (23.7%) |
| Parous | 90 (73.8%) | 26 (86.7%) | 116 (76.3%) |
1.1.4.1 Cardiac outcomes
Only one patient who was diagnosed with CVD prepartum had no postpartum visit. Therefore, follow-up data were available for 142 (93.4%) patients. Maternal mortality rate was 9 of 152 (OR 5.92%, 95% CI 2.15, 9.65%) within the 6-month postpartum follow-up period. Of these, 7 (77.8%) patients died due to familial CMO or PPCMO, with 2 cases of prosthetic valve complications. All patients who died had been assessed as WHO class III or IV. Significantly, 8 (88.9%) of 9 patients died 42 days postpartum. Overall, 30 patients had a poor outcome as predefined using a combined endpoint of death, low LVEF, or remaining in New York Heart Association (NYHA) Class III or IV. Of the women diagnosed with CVD prepartum, 41 (33.6%) developed signs and symptoms of heart disease while pregnant, leading to admission in 20% of cases. At the final follow-up, 13 (10.7%) of the patients were found to be in NYHA Class III or IV. Of the 30 patients diagnosed with CVD postpartum, 3 (10.0%) died before their 6-month visit. Of the remaining patients, 12 (44.4%) felt minimally to moderately better compared to their first presentation, 3 (11.1%) were unchanged, and 12 (44.4%) felt minimally or moderately worse.
1.1.4.2 Fetal and obstetric outcome
Mean gestational stage was 36.7 ± 4.2 years with a significantly longer gestational period in patients presenting with antenatal cardiac disease versus those presenting postpartum (p = 0.04). Eleven patients developed gestational hypertension during pregnancy. Overall, there was a high operative delivery rate, with 46 (30.3%) of 152 patients having received a cesarean section. No significant differences in obstetric outcome were revealed between the modified WHO Class II, III, and IV disease categories. Perinatal death occurred in 1 (0.7%) out of 152 patients (0.66; 95% CI 0.00, 1.94) due to one fetal death, translating to a perinatal mortality of 7/1,000 live births. In addition, there were two miscarriages and two medically indicated terminations. Mean birth weight for the entire cohort was 2850.8 ± 552.7 g, with 33/148 born weighing <2500 g and 46/148 born preterm (<37 weeks’ duration).
1.1.5 Study interpretation
Overall, this study revealed a pattern of disease that was markedly different from that of developed countries in terms of RHD, the CMOs, and CHD. Maternal mortality occurred in 9 of 152 (5.9%) patients. This was significantly higher than that reported in a recent study undertaken by the European Society of Cardiology [24]. Most deaths were due to forms of CMO, with only two deaths being related to complications attributable to sepsis and thrombosis affecting prosthetic heart valves. These data point to the need for care to be intensified covering the postpartum period, including earlier referral to the general cardiac or CMO clinic and adequate counseling about the risks of future pregnancy and contraceptive services. A recent systematic review of the burden of antenatal heart disease in South Africa reported a prevalence of heart disease ranging from 123 to 943 per 100,000 deliveries, with RHD being the most common abnormality, followed by CMO [25]. These data also revealed that 18% of women who survived and attended follow-up clinics experienced symptoms that were worse after the pregnancy, with 44% displaying moderate-to-severe disability. There were no stillbirths and only one neonatal death. Although 30% of the patients delivered before 37 weeks, the mean gestational age at delivery fell just short of 37 weeks and the mean birth weight was 2.85 kg. In the future, echocardiography-based screening of patients may further improve identification and referral of high-risk cases, although the cost-effectiveness of this intervention has yet to be established [26,27].
1.1.6 Study limitations
As with all observational studies of this kind, particularly when focused on a single center and community, the wider generalizability of observed associations (with the inherent caveat around inferring causality) and outcomes needs to be considered. Despite the study’s relatively large size and detailed clinical phenotyping, its data should still be interpreted with some caution.
1.1.7 Study conclusion
In conclusion, these data derived from a South African maternal cohort revealed a disease pattern markedly different from that seen in developed countries. Joint obstetric–cardiac care is related to the survival rates of pregnant mothers, even those with complex diseases, and their offspring. The greatest risk of adverse outcomes is attributable to late presentation and advanced cardiac failure, with death commonly occurring outside the 42-day maternal mortality reporting period. The perinatal outcome in an environment of intensive surveillance and management was found to be generally good.
1.2 Initial evaluation of bromocriptine treatment for PPCMO in South Africa
Sliwa K, Blauwet L, Tibazarwa K, Libhaber E, Smedema JP, Becker A, McMurray J, Yamac H, Labidi S, Struhman I, Hilfiker-Kleiner D. Evaluation of bromocriptine in the treatment of acute severe peripartum cardiomyopathy: a proof-of-concept pilot study. Circulation 2010; 121:1465–73. [28]
1.2.1 Background
As shown in recent studies focusing on PPCMO, only 23 to 54% of patients show recovery of cardiac function within 6 months [29–32]. Previous reports suggest that enhanced oxidative stress in a mouse model for PPCMO (mice with a cardiac-specific deletion for signal transducer and activator of transcription-3) triggers the activation of cathepsin D, a ubiquitous lysosomal enzyme that subsequently cleaves serum prolactin into its antiangiogenic and proapoptotic 16-kDa form [18]. This is associated with endothelial inflammation, impaired cardiomyocyte metabolism, and reduced myocardial contraction, suggesting that oxidative stress, inflammation, and prolactin may be interconnected and responsible for initiating PPCMO. Although these preliminary results suggesting beneficial effects of bromocriptine treatment in patients with acute PPCMO appear promising, concerns have been raised about the risk of thrombotic complications, including cerebral vascular incident and acute myocardial infarction (AMI) [33–36] and potential negative consequences for the children of these mothers, who are unable to breast-feed [37].
1.2.2 Study aims
The aim of this study was to initially assess the efficacy of bromocriptine on recovery of LV function, symptom status, and other clinical measures in patients presenting within the first month postpartum with new-onset symptomatic PPCMO and a LVEF <35%. A further aim was to identify prolactin, mainly its 16-kDa angiostatic and proapoptotic form, as a key factor in the pathophysiological development of PPCMO.
1.2.3 Methods
1.2.3.1 Patient enrollment
The study was conducted at the Chris Hani Baragwanath Hospital in Soweto, South Africa, where 93 pregnant patients suspected of having PPCMO were screened for confirmation. Patients were included in the study if they presented with a negative HIV status and CHF that developed during the final month of pregnancy or the first month postpartum. They were excluded if they presented with clinical conditions other than CMO that could increase plasma levels of inflammatory markers; a systolic blood pressure (BP) of <160 or <95 mm Hg or a diastolic BP of >105 mm Hg; significant liver disease; impaired renal dysfunction; a history of psychiatric disorder or peptic ulcer disease; or any other clinical conditions that in the opinion of the investigators precluded inclusion (e.g., IHD or malignancy). Clinical assessment, signs and symptoms, blood analysis, and echocardiography were recorded at baseline and at 6-month follow-up.
1.2.3.2 Pharmacotherapy
All patients received treatment with the loop-diuretic furosemide and the angiotensin-converting enzyme (ACE) inhibitor enalapril. Enalapril and carvedilol doses were titrated upward as tolerated during the first 4 weeks after diagnosis and then remained unchanged throughout the remainder of the study period. Carvedilol was added after resolution of overt HF. Patients who presented with LV thrombus or a LVEF of <25% received anticoagulation therapy with warfarin for 6 months. Furosemide dose was decreased as indicated according to clinical assessment during the 6-month study period. Ten patients were randomized to standard therapy (PPCMO-Standard) as described above, and the other 10 were randomized to standard therapy and received bromocriptine (PPCMO-Bromocriptine) 2.5 twice daily for 2 weeks followed by 2.5 mg daily for 6 weeks thereafter. After baseline visits, monthly outpatient visits were organized for medication response assessment and evaluation. Patients who were receiving bromocriptine underwent cardiac MRIs at 4 to 6 weeks after diagnosis to detect mural thrombi. All newborns of the study patients were assessed every 6 months with standard growth-monitoring charts issued by the South African Department of Health and maintained by primary physicians.
1.2.4 Results
Overall, 20 (21.5%) consecutive patients out of the 93 patients screened were enrolled in the study. As shown in Table 1.3, both the PPCMO-Standard and the PPCMO-Bromocriptine groups were found to have a similar age, parity, systolic and diastolic BP, heart rate, NYHA Class, LV end-diastolic diameter, and LV end-systolic diameter.
Table 1.3 Patients’ demographic and clinical characteristics.
| PPCMO-Standard n = 10 | PPCMO-Bromocriptine n = 10 | |
| Demographic characteristics | ||
| Age (years) | 28 ± 10 | 24 ± 6 |
| Parity | 2 (IQR 1–6) | 1.5 (IQR 1–3) |
| Clinical characteristics | ||
| Systolic BP (mm Hg) | 110 ± 19 | 116 ± 23 |
| Diastolic BP (mm Hg) | 76 ± 18 | 70 ± 16 |
| Heart rate (beats/min) | 108 ± 15 | 102 ± 13 |
| NYHA class | ||
| II/III | 5 (50.0%) | 5 (50.0%) |
| IV | 5 (50.0%) | 5 (50.0%) |
| Echocardiographic presentations | ||
| LV end-diastolic diameter (mm) | 59 ± 5 | 55 ± 10 |
| LV end-systolic diameter (mm) | 52 ± 6 | 46 ± 9 |
| LVEF (%) | 26.9 ± 7.6 | 27.2 ± 8.1 |
| Mitral regurgitation (grade) | 1.9 ± 0.6 | 2.1 ± 0.6 |
| Mitral effective regurgitant orifice (cm2) | 0.44 ± 0.18 | 0.45 ± 0.13 |
| Laboratory presentations | ||
| Hemoglobin (g/dL) | 11.8 ± 1.9 | 13.0 ± 2.2 |
| Creatinine (µmol/L) | 66 (IQR 5, 96) | 71 (IQR 6-109) |
| High-sensitivity C-reactive protein (mg/L) | 6.0 (IQR 4.0, 115) | 7.8 (IQR 1.1, 58) |
| Prolactin (µg/L) | 30.0 (IQR 5.1, 233) | 49.9 (IQR 3.8, 135) |
| Log N-terminal pro b-type natriuretic peptide | 8.54 ± 1.24 | 8.54 ± 1.24 |
1.2.4.1 Pharmacotherapy
At 6 months, the median daily enalapril dosage for the PPCMO-Standard group was 10 mg/day compared to 5 mg/day for the PPCMO-Bromocriptine group. Similarly, the median carvedilol dosage among the PPCMO-Standard group was 12.5 mg twice daily compared to 6.25 mg twice daily for the PPCMO-Bromocriptine group. For both groups, the median furosemide dosage was 80 mg/day (IQR 80, 120 mg).
1.2.4.2 Baseline and 6-month echocardiographic parameters
The study groups did not significantly differ in systolic and diastolic BP, heart rate, or LV end-diastolic and end-systolic dimension changes from baseline to 6 months. However, LVEF recovery was greater in the PPCMO-Bromocriptine group compared with the PPCMO-Standard group (31% versus 9%; p = 0.012), as was improvement of mitral regurgitation (MR) (p = 0.013), along with several other parameters shown in Table 1.4.
Table 1.4 Patients’ baseline and 6-month echocardiographic changes according to group.
| Baseline | 6 Months | |||
| PPCMO-Standard | PPCMO-Bromocriptine | PPCMO-Standard | PPCMO-Bromocriptine | |
| Clinical parameters | ||||
| Systolic BP (mm Hg) | 110 ± 19 | 116 ± 23 | 115 ± 9 | 118 ± 13 |
| Diastolic BP (mm Hg) | 76 ± 18 | 70 ± 16 | 73 ± 6 | 74 ± 9 |
| Heart rate (beats/min) | 108 ± 15 | 102 ± 13 | 79 ± 15 | 64 ± 7 |
| Echocardiographic parameters | ||||
| LV end-diastolic diameter (mm) | 59 ± 5 | 55 ± 10 | 56 ± 12 | 51 ± 9 |
| LV end-systolic diameter (mm) | 52 ± 6 | 46 ± 9 | 45 ± 11 | 34 ± 10 |
| LVEF (%) | 27 ± 8 | 27 ± 8 | 36 ± 11 | 58 ± 11 |
| MR (grade) | 1.9 ± 0.6 | 2.1 ± 0.6 | 1.5 ± 1.0 | 0.22 ± 0.44 |
| Mitral effective regurgitant orifice (cm2) | 0.44 ± 0.18 | 0.45 ± 0.13 | 0.34 ± 0.18 | 0.11 ± 0.03 |
| Left atrial diameter (cm) | 3.83 ± 0.62 | 3.54 ± 0.25 | 3.93 ± 0.83 | 3.36 ± 0.53 |
| Mitral E velocity (cm/s) | 89 ± 23 | 86 ± 19 | 85 ± 24 | 66 ± 24 |
| Mitral A velocity (cm/s) | 33 ± 6 | 32 ± 7 | 45 ± 12 | 48 ± 19 |
| Mitral E velocity/A velocity ratio | 2.73 ± 0.68 | 2.82 ± 0.76 | 1.94 ± 0.67 | 1.63 ± 1.13 |
| Deceleration time (ms) | 136 ± 30 | 118 ± 26 | 168 ± 36 | 197 ± 59 |
| Mitral medial annular (E') tissue Doppler imaging. velocity (cm/s) | 6.5 ± 1.1 | 7.0 ± 1.3 | 7.3 ± 2.5 | 12.4 ± 2.4 |
| E/E' (medial annular velocity) | 14.0 ± 4.6 | 12.5 ± 3.0 | 12.4 ± 6.4 | 5.4 ± 2.5 |
| Mitral lateral annular (E') tissue Doppler imaging. velocity (cm/s) | 6.6 ± 0.97 | 7.2 ± 1.1 | 7.3 ± 2.5 | 12.4 ± 2.5 |
| E/E' (lateral annular velocity) | 13.8 ± 4.2 | 12.0 ± 2.0 | 12.1 ± 3.9 | 5.4 ± 2.5 |
1.2.4.3 Natriuretic peptide levels
Log N-terminal pro b-type natriuretic peptide change was found to differ between the groups, with a borderline statistically significant (positive) difference present in the PPCMO-Bromocriptine group as compared with the PPCMO-Standard group (p = 0.05).
1.2.4.4 Outcomes and infant findings
In the PPCMO-Standard group, 4 patients died prior to the 6-month follow-up, due to HF (n = 3) and sudden cardiac death (n = 1). Alternatively, only 1 patient died in the PPCMO-Bromocriptine group at 7 days due to severe HF; all remaining patients survived to 6 months. Furthermore, all 9 surviving PPCMO-Bromocriptine patients were found to have recovered to NYHA Class I at the 6-month follow-up. In contrast, 3 PPCMO-Standard patients were assessed as NYHA Class II and 3 as NYHA Class III at 6 months. With respect to the infant outcomes, a total of 21 children were assessed throughout the study, all displaying normal growth curves when recorded on the WHO standard weight-for-age growth charts. Although all children were alive at the 6-month follow-up, weight-for-age data at 6 months were available for 13 children. However, there was no significant difference in the children’s growth curves at 3 months according to study group (see Figure 1.4).

Figure 1.4 Comparison of infant growth curves according to maternal treatment group.
1.2.5 Study interpretation
This key study showed that the addition of bromocriptine to standard HF therapy in women with PPCMO was associated with significantly greater improvements in NYHA functional class, LV systolic and diastolic function, and degree of functional MR than was observed with standard therapy alone. Moreover, bromocriptine appeared to be well tolerated with no thrombotic complications observed, and although its use prevented lactation and breast-feeding in the PPCMO patients, the growth and survival of their infants were normal. In addition, both forms of prolactin promote inflammation [38], a reaction that seems to be associated with PPCMO in this African cohort, given that most patients displayed increased serum levels of the inflammatory marker high-sensitivity C-reactive protein [30]. Positive effects of bromocriptine on BP, vascular resistance, and plasma norepinephrine levels have been described [39]. However, it has been shown to increase stroke volume index and to decrease LV filling pressure [39,40]. The mortality rate in the PPCMO-Standard group was higher than in the group receiving bromocriptine, a finding that diverges from data previously reported [29,30,41,42]. This difference may be due to variations in inclusion criteria, as patients in this study were enrolled within 24 hours after diagnosis.
1.2.6 Study limitations
This trial involved a number of limitations that require comment. First, as a pilot study, the cohort was small, albeit with sufficiently encouraging results to prompt larger and more definitive studies in the future. Second, blinding of the study was not possible as the PPCMO-Standard group continued to nurse their infants while the PPCMO-Bromocriptine group could not breast-feed due to bromocriptine-induced cessation of lactation. Although this was a small study with only short-term follow-up, these results suggest no disadvantage to the infant of a PPCMO patient who could not breast-feed for this reason. However, at the time of this report a larger study was currently underway in Germany testing this concept. The European Cardiac Society via the EURObservational Research Programme is currently collecting information on 1,000 patients with PPCM from >40 countries, which will also include a large number of women who have received bromocriptine.
1.2.7 Study conclusion
In conclusion, the addition of bromocriptine to standard HF therapy appeared to improve cardiac function in women presenting with PPCMO, with no ill effects evident in their infants. Despite the small sample size, which consequently cannot be taken as representative of the population at large, these results are very encouraging.
1.3 Health outcomes associated with PPCMO in South Africa
Blauwet LA, Libhaber E, Forster O, Tibazarwa K, Mebazaa A, Hilfiker-Kleiner D, Sliwa H. Predictors of outcome in 176 South African patients with peripartum cardiomyopathy. Heart 2013; 99(5):308–13. [17]
1.3.1 Background
As described above, PPCMO is known to cause HF among pregnant women several months before and 6 months after delivery. Even though most PPCMO patients experience a higher rate of recovery of LV function than observed in those with other forms of nonischemic CMO [43], only 23 to 54% patients are reported to recover at 6 months [29–31,43,44]. Case series have demonstrated that poor outcomes are predicted by LV dilation, LV thrombus, LV systolic dysfunction, and body mass index (BMI), as well as renal and liver dysfunction [31,44–48]. However, the association between HF and BMI, renal function, and liver dysfunction has not been previously assessed in patients with PPCMO.
1.3.2 Study aims
The aim of this study was to determine whether those variables previously linked to poor outcomes in PPCMO (outlined above) are indeed predictors of outcome in a large cohort of PPCMO patients in Soweto, South Africa.
1.3.3 Methods
1.3.3.1 Patient enrollment
Patients being referred to the Chris Hani Baragwanath Hospital in Soweto, South Africa, from local clinics, secondary hospitals, and the Department of Obstetrics at the same hospital were studied. Each patient underwent assessment for preexisting cardiac signs and symptoms during first presentation at the cardiac unit and at the 6-month follow-up; this was confirmed by examining the obstetric card carried by each patient. Blood analysis, echocardiography, and clinical assessment were also performed at baseline and at follow-up. Inclusion criteria comprised age between ≥16 and ≥40 years old, symptoms of CHF that developed during the last month of pregnancy or the first 5 months postpartum and no other identifiable cause of HF, LVEF ≥45% by transthoracic echocardiography, and sinus rhythm. Patients were excluded if they presented with significant organic VHD, a systolic BP >160 mm Hg or diastolic BP >100 mm Hg, clinical conditions other than CMO that could increase plasma levels of inflammatory markers, severe anemia (hemoglobin <9 g/dL), and/or IHD or malignancy. Of the 176 patients who were included in the study, 164 (93.2%) received treatment with furosemide, 141 (80.1%) were treated with ACE inhibitor, 113 (64.2%) were prescribed digoxin, and 100 (56.8%) were prescribed carvedilol after resolution of overt HF. ACE inhibitors and carvedilol doses were titrated upward as tolerated throughout the 6-month study period.
1.3.4 Results
1.3.4.1 Cohort profile
In total, 176 consecutive patients diagnosed with PPCMO and fulfilling the inclusion criteria were enrolled in the study. All patients were of African ancestry. The mean age was 30.7 ± 6.9 years, mean parity was 2 (range 1–7); mean BMI was 25.6 ± 5.2 kg/m2, and most of the women (82%) presented as NYHA Class III or IV. Table 1.5 compares the patients’ characteristics from baseline to 6-month follow-up, demonstrating that while the mean LV end systolic dimension decreased significantly from 51.3 ± 7.6 mm to 42.3 ± 9.5 mm (p < 0.0001), mean LVEF increased significantly from 27.3 ± 8.1 mm to 43.3 ± 12.5 mm (p < 0.0001). Over the same period, mitral inflow E/A decreased significantly from 2.01 ± 0.86 ms to 1.51 ± 0.65 ms, and mitral inflow deceleration time increased significantly from 140.0 ± 66.1 ms to 185 ± 67.9 ms (p < 0.0001 for both). Hemoglobin, renal function, and liver function test results had also improved at 6 months.
Table 1.5 Patients’ baseline and 6-month follow-up characteristics.
| Baseline (n = 176) | 6-Month Follow-up (n = 141) | |
| Age (years) | 30.7 ± 6.9 | — |
| Median parity (range) | 2 (1–7) | — |
| BMI (kg/m2) | 25.6 ± 5.2 | — |
| Systolic BP (mm Hg) | 111 ± 17 | 113 ± 17 |
| Diastolic BP (mm Hg) | 72 ± 13 | 72 ± 12 |
| Heart rate (beats/min) | 97.3 ± 19.1 | — |
| NYHA functional class | ||
| I/II | 33 (18.8%) | 128 (90.8%) |
| III/IV | 143 (82.3%) | 13 (9.2%) |
| Echocardiography | ||
| LV end-diastolic diameter (mm) | 59.5 ± 7.3 | 54.0 ± 8.6 |
| LV end-systolic diameter (mm) | 51.8 ± 7.6 | 42.3 ± 9.5 |
| LVEF (%) | 27.1 ± 8.1 | 43.3 ± 12.5 |
| E-velocity (ms) | 0.89 ± 0.25 | 0.80 ± 0.22 |
| A-velocity (ms) | 0.49 ± 0.20 | 0.57 ± 0.18 |
| E/A | 2.02 ± 0.89 | 1.51 ± 0.65 |
| Deceleration time (ms) | 134.5 ± 63.2 | 185.1 ± 67.9 |
| LV thrombus | 19 (10.8%) | 0 (0%) |
| Laboratory | ||
| Hemoglobin (g/dL) | 12.1 ± 1.8 | 12.8 ± 1.52 |
| Creatinine (mmol/L) | 84.1 ± 20.5 | 76.4 ± 23.5 |
| Urea (mmol/L) | 5.4 ± 2.9 | 4.4 ± 1.6 |
| Total protein (g/L) | 77.9 ± 11.4 | 82.2 ± 8.9 |
| Albumin (g/L) | 40.1 ± 18.5 | 43.7 ± 13.5 |
| Total bilirubin (µmol/L) | 17.3 ± 26.8 | 11.0 ± 8.6 |
| Direct bilirubin (µmol/L) | 9.2 ± 23.2 | 4.5 ± 4.9 |
| Indirect bilirubin (µmol/L) | 8.2 ± 7.3 | 6.1 ± 4.4 |
| Alkaline phosphatase (U/l) | 117.9 ± 51.0 | 97.4 ± 36.4 |
| Aspartate transaminase (U/l) | 45.0 ± 46.8 | 26.4 ± 12.9 |
| Alanine transaminase (U/l) | 54.7 ± 67.1 | 24.5 ± 14.0 |
| γ-glutamyl transpeptidase (U/l) | 72.4 ± 49.4 | 52.8 ± 40.8 |
1.3.4.2 Health outcomes
During 6-month follow-up, 9 (5.1%) patients were lost to follow-up, 3 (1.7%) moved to remote areas where follow-up could not occur, and 2 (1.1%) did not undergo echocardiographic assessment at 6 months. Of the remaining 162 (80.1%) patients, 45 (27.8%) met the prespecified combined endpoint of death, or (if still alive) remained in NYHA Class III/IV and/or had a residual LVEF <35% at 6 months. Univariate analysis of baseline profiling revealed that this prespecified composite endpoint was predicted by increased LV end systolic diameter, mitral inflow E/A, aspartate transaminase, and alanine transaminase; and decreased systolic BP, LVEF, mitral inflow deceleration time, and total cholesterol. Of the 141 patients who survived, 30 (21.3%) had fully recovered LV function (LVEF ≥55%) at 6 months. When comparing the baseline characteristics of the patients who fully recovered to those of the patients who did not, it was found that predictors of LV recovery included older age, increased hemoglobin levels, and decreased LV end systolic diameter, LV end diastolic dimension, and creatinine levels.
1.3.5 Study interpretation
These data confirm previous reports that a relatively high proportion of surviving patients with PPCMO (around 4 in 5 cases) have residually poor LV function (i.e., minimum cardiac recovery) at 6 months [31,47]. Baseline predictors of poor outcome in this series of patients included increased LV end systolic diameter, lower BMI, and lower total cholesterol levels. Older age appears to be a novel predictor of LV recovery, while younger age, lower BMI, increased LV end systolic diameter and LV end diastolic diameter, and higher NYHA class all seem to be predictors of mortality. As previously reported, increased LV end systolic diameter at diagnosis was a significant predictor of outcome, even when adjusted for other variables in multivariate analysis [44]. However, in contrast with previous reports, LVEF and LV end diastolic diameter at diagnosis, NYHA class, and presence of LV thrombus were not predictors of poor outcome [30,31,44,45,47,48]. Numerous studies have shown an association between cholesterol and mortality in patients with chronic HF [49–51]. As the cohort experienced a relatively low number of deaths, multiple logistic regression analysis of mortality was not performed. Future studies are therefore necessary to further clarify and validate predictors of mortality among this patient population. More awareness of CVD in pregnant women is urgently required. The team has developed a web-based data entry platform that contains a number of videos for women from low socioeconomic backgrounds providing information on common cardiac conditions in pregnancy. This data entry platform can be accessed under www.hedu-africa.org (Figure 1.5).
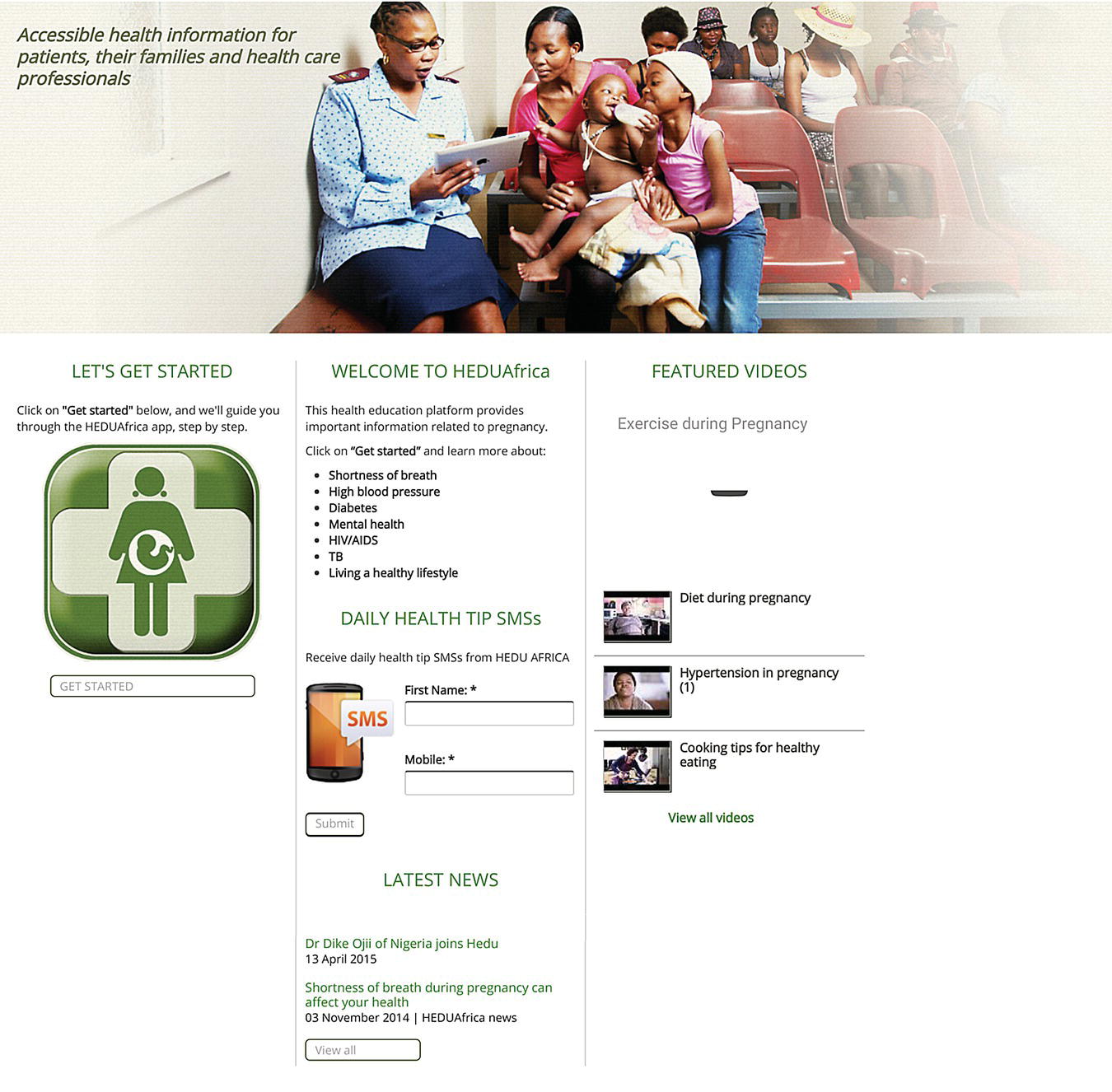
Figure 1.5 The Health Education (HEDU) Initiative to improve maternal health outcomes in South Africa.
1.3.6 Study limitations
As noted earlier, as in all observational studies of this kind, particularly when focused on a single center and community, the wider generalizability of observed associations (with the inherent caveat around inferring causality) and outcomes needs to be considered. In particular, this was a selected population attending a specialist program focusing on PPCMO, and there is a need to confirm observations in other parts of Africa—noting the creation of a prospective registry for this very purpose.
1.3.7 Study conclusion
In conclusion, high LV end systolic diameter and low total cholesterol were found to be associated with poor outcomes in a large cohort of African women with PPCMO. Conversely, lower LV end systolic diameter and older age were related to high levels LV function recovery.
S1.2 Maternal health in Africa: The way forward
Given residually high levels of maternal ill health and mortality, there is urgent need to refocus on this major health issue throughout the African continent; particularly given high mortality rates in the content of the relatively (to other African countries) well-developed maternal health care system in South Africa. Much of the death and disability at this stage of life is cardiac related and highly preventable with more structured surveillance and proactive management of underlying cardiovascular issues (particularly hypertension). In response to these data, ongoing research is focusing on harnessing information technology to provide important health messages to African women to improve their overall and maternal heart health. If successful, these will have a profound impact on maternal outcomes and, of course, on the short- and longer-term health prospects of the next generation of African children (see Section 2 below). More specific efforts are also underway to more actively quantify the distribution and number of cases of PPCMO via an Africa registry, along with ongoing efforts to better understand and treat this potentially devastating condition.