
The aim of this chapter is to help you understand the medical aspects of heart disease. It is very important that you understand your illness, because only then will you be able to take an active role in healing yourself. It is important to know a bit about the circulatory system to be able to understand the illness.
In medicine, new discoveries are being made all the time. Therefore be prepared that your doctor may give you information at variance with what is written here. For example, new research may show that certain procedures are no longer as effective as they are made out to be. Safer procedure may be discovered, new drug discoveries may revolutionise the treatment of heart disease.
It is always a good idea to get a second opinion – especially if you are confused or have any doubts. It is always a good idea to get a second opinion before undergoing an angioplasty or bypass surgery. It is important you choose a doctor with whom you feel comfortable. Your doctor should be willing to discuss and explain things to you.
The blood supplies the body with nutrients and oxygen and carries away the waste products of metabolism to the organs of excretion. The blood is moved to the tissues through a network of intricate channels called blood vessels.
The heart is a pump that pumps blood along these channels through the body. The blood from the heart is first pumped into the aorta, the main blood vessel of the body. The aorta then divides into a network of increasingly smaller blood vessels that go on to supply various parts of the body. The small arteries further divide into smaller vessels called arterioles. These arterioles then divide into millions of thin-walled vessels called capillaries that supply blood to tissue and cells.

Fig. 1 - Circulation of Blood
The capillaries rejoin to form veins that carry back the blood from which the oxygen has been used, through the veins back to the right side of the heart. From here, the deoxygenated blood is pumped into the lungs where it is oxygenated and then sent into the left side of the heart.
Blood is supplied to the heart muscle by the coronary arteries which arise at the base of the aorta. There are three main coronary arteries that break up into smaller branches, each of which supplies a small area of the myocardium (heart muscle) with blood. The branches of the coronary arteries break up into smaller vessels called arterioles that finally divide into even finer vessels capillaries. It is through the walls of these capillaries that oxygen and nutrient substances diffuse into the heart muscle cells.
Each coronary artery supplies a particular part of the heart with small areas of overlap. In cases of sudden block of a coronary artery, the muscle supplied by it is damaged permanently. If the blockage develops slowly, often the capillaries from adjoining areas grow into the area starved of blood. This is called development of collateral circulation and is more commonly developed in elderly people who exercise moderately. When there is a total blockage to a coronary artery with a well developed collateral circulation the extent of damage to the heart muscle is minimised. Younger people usually have fewer collaterals and are more likely to die from a first infarct than an older person.
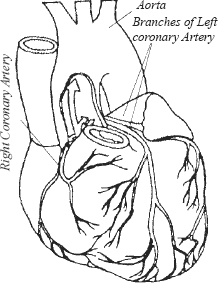
Fig. 2 - Coronary Arteries
While it may appear that modern medical science knows the real cause of heart disease, actually this is not true. So much is still being discovered so that anyone who studies the subject in any depth will realise that what is known is the pathology (changes in structure and functioning) but not the cause. Heart disease is a multi-factorial illness in the sense that there are a number of factors that come together to cause a problem.
There is little doubt that physical factors such as a high fat diet and/or the lack of exercise are contributory factors in coronary artery disease. One must remember that the emotional factors are equally if not more important. There are numerous epidemiological studies of groups of people who have a high fat diet, are sedentary and smoke but have much lower rates of heart disease than people from other communities with similar habits. The crucial factor that seems to protect these people is a Type B disposition, low levels of stress and a stable and close social network.
In most cases of coronary artery disease, it is the deposition of cholesterol, a fatty substance in the wall of the artery that causes the problem. The deposition of cholesterol in the arterial wall is called atherosclerosis or arteriosclerosis. The fatty deposits in the arterial wall are called plaque or atheroma. The fat deposits lead to a narrowing of the lumen of the artery and a reduction in the amount of blood that can flow through the vessel. More important the deposits of LDL cause inflammation and swelling in the walls of the artery and this leads to rupture of the plaque and formation of a clot at that point. The extent of blockage is not a very good indicator of the risk of having a heart attack in the near future as the incidence of heart attacks is high in people with 30-40% blockages. This is because the plaque may be soft and there may be greater inflammation, while the plaque in an artery with 90% block is likely to be harder and less likely to rupture if there is less inflammation. It is important you know this as some doctors use the fact of a high percentage of blockage to railroad people to have an angioplasty or bypass surgery immediately.

Fig. 3 - Atherosclerotic Artery
One should also be aware of the fact that some patients who have had a myocardial infarction do not have significant deposits of cholesterol in the walls of their coronary arteries, their problem is due to the artery going into spasm due to stress and psychological factors. Hence even if an angiography does not show any significant blockages, it is necessary to work on changing your response to stress, personality and other risk factors.
Any blockage to a coronary artery leads to damage and death of the muscle supplied by that artery. This is known as a myocardial infarction. Once the artery is blocked, the heart muscle in the area supplied by it dies within a short while due to lack of adequate oxygen and nutrients. The heart muscle does not regenerate after it has been damaged. Instead it is replaced by tough, fibrous, inelastic tissue. The total amount of contractile muscle is reduced and because of this, less blood can be pumped by the heart.
The blockage is usually due to the formation of a clot in the coronary artery. Sometimes the plaque can rupture and then block the artery. In certain cases an infarct is due to a spasm in the coronary artery due to stress or an emotional reaction. An artery can go into spasm in the absence of significant atherosclerosis but narrowed arteries are more likely to get blocked.
If a large portion of the muscle is destroyed following the infarction then the person may die immediately, as the heart is unable to pump enough blood to maintain the vital functions of the body. Generally the amount of muscle destroyed is not enough to cause death but may cause a reduction in the blood supplied for bodily functions. This leads to what is called cardiac failure and the other organs start giving way as they do not get enough blood. Sometimes there is enough reserve left to function while resting but there is no reserve capacity to deal with the increased demands of blood by the body during activity.
The first symptom is usually pain in the centre of the chest. This pain is often described as squeezing or vice-like, but in some cases the pain may be mild or even absent. The pain often radiates to the shoulder, back, neck or down the inner side of the left arm down to the little finger. Occasionally the pain may only arise in the epigastrium (the pit of the stomach) or in the shoulder, jaw, neck or arm and may be associated with sweating and/or nausea or vomiting. Occasionally profuse sweating may be the only sign of a myocardial infarction. In some cases, there are no symptoms: the so-called silent myocardial infarction that is only picked up on an electrocardiogram.
Usually the symptoms are diagnostic but your doctor will always confirm the diagnosis with an electrocardiogram (ECG). Following a heart attack certain diagnostic changes appear on the electrocardiogram, but in many cases it may take a few hours before changes appear.
In addition to an ECG, your doctor will also ask for some blood tests. Enzymes such as creatinine phosphokinase (CPK), SGPT enzymes are released into the blood when there is muscle damage. During an infarction, the muscle is damaged and the enzyme levels rise but again this may take some hours. So the test may be repeated if required.
As the confirmatory tests such as the enzyme levels and the ECG may take some time to become positive, your doctor will usually admit you to the ICU for observation if he suspects an infarction on the basis of your symptoms.
The important thing during this phase is to remain calm. Panic leads to the release of stress hormones in the blood and this raises the heart rate and risk of arrhythmias.
In the intensive care unit you will be connected to a monitor that records your heart rate and ECG that allows any abnormal rhythms of the heart to be detected immediately so that you can be given medicines to rectify them.
If you reach the hospital an hour or so after the onset of symptoms, clot busting drugs may be able to dissolve the clots completely and prevent muscle damage. An angioplasty at this stage is another option that may prevent muscle damage.
After a few days in the ICU, if there are no complications, your doctor will move you to an ordinary room in the hospital and then later discharge you. Post discharge it is important to continue your medication as prescribed by your doctor.
Usually you will be advised to walk around the house for about ten days and then over the next four to six weeks, gradually build to about a kilometre of slow walking. Always follow your cardiologist’s advice about exercise.
After six weeks if you want to restart vigorous exercise, you should have an exercise stress test. This will help determine your exercise tolerance.
In this condition one or more coronary arteries are partially blocked due to the fatty deposits (atheroma) within the wall of the artery. The atheroma restricts the amount of blood that can flow through the lumen of the artery. The diseased arteries are narrowed and hardened and cannot expand to allow more blood to flow to the heart muscle during exercise or times of increased oxygen demand. This leads to the heart muscle being starved of oxygen and nutrients and causes the pain during exertion. The pain is caused when the heart muscle’s demand for extra oxygen during exertion is not met. The anginal pain is a protective signal that warns the person that he has done enough and needs to rest.
Patients with angina pectoris are at a greater risk of having a myocardial infarction or developing irregular (potentially fatal) heart rhythms called arrhythmias. Because of this, it is important that you take anginal pains seriously. Angina is a warning that your heart is not getting enough blood and that the heart muscle has not suffered irreversible damage as in an infarction.
Chest pain that is brought on by exertion such as walking or running and relieved by rest is the commonest symptom of angina pectoris. The pain may extend into the neck, shoulder or the left arm and is usually described as a heaviness or crushing sensation. The pain of angina may be associated with feeling that the heart is beating very fast (palpitations) or breathlessness. In some cases, the pain may continue for hours and could indicate an imminent myocardial infarction.
The typical history of pain or exertion relieved by rest along with the ECG is often diagnostic. The ECG may show certain changes indicative of reduced oxygen supply to the heart called ischemia. In many cases of angina the resting ECG may be normal but an exercise stress test detects and confirms that the person has angina pectoris. This can then be confirmed by a C.T angiogram if your doctor thinks it is necessary.
If you have angina and start this programme soon, it is possible to reverse the blockage and prevent future infarction. Moreover it can prevent the need for bypass surgery or an angioplasty.
Remember that even a small decrease in the amount of blockage can lead to a substantial increase in the amount of blood flowing to the heart muscle. A 5% reduction in the amount of blockage, from 75% to 70%, allows a 100% increase in the amount of blood flowing through the artery and can lead to complete relief from symptoms. One can thus get a substantial amount of pain relief in a short period of time if one follows the programme.
One should not get frightened if an artery has a high percentage blockage because the plaque is likely to be harder and stable, therefore less likely to rupture in the near future, giving one enough time to start on a programme of diet and exercise. People with blockages as high as 90% have done well on the Ornish programme.
The heartbeat is co-ordinated by electrical impulses that are generated and transmitted across the heart by a specialised system of tissue. In the event that there is a reduction in the blood flow or damage to these tissues the heart starts beating irregularly, or may even stop.
This irregular heartbeat is known as an arrhythmia. There are various types of arrhythmias but what one must understand is that these arrhythmias can lead to a great reduction in the flow of blood and in some cases can even lead to death. Nicotine and caffeine can make arrhythmias worse or induce them in susceptible persons.
Emotion and stress can precipitate arrhythmias in vulnerable individuals. There are many cases of people dying suddenly in response to emotional stress and the most likely cause of sudden death in these circumstances is a type of arrhythmia called ventricular tachycardia. Your doctor may detect an arrhythmia while examining your pulse or it may show up on an ECG.
The first line of medical treatment for coronary heart disease is medication that dilates the coronary arteries (such as the Nitrates) thereby increasing the supply of oxygen to the heart. In addition other drugs reduce the oxygen consumption of the heart by slowing it down or reducing the resistance against which the heart beats and anti-arrhythmic medication, if required. It is important that blood pressure and diabetes be controlled aggressively.
In addition most patients with coronary artery will receive anti-clotting medication to prevent new clots forming. Small doses of Aspirin are commonly used for this purpose.
It is a good idea to read about the medication you take, become aware of how they work and of their benefits and side effects. There is a wealth of updated information available on the internet.
The introduction in the 1990s of the Statins, a group of cholesterol lowering drugs, has significantly lowered the disability and death rates in patients with coronary artery disease.
The statins rapidly and effectively reduce cholesterol levels, shrink the plaque and reduce inflammation in the arterial wall. Today it would be unusual for a cardiologist not to recommend these drugs for someone with CAD even if the person does not have elevated levels of cholesterol.
The Simvastatin Survival study by Dr Terje Pedersen, Head of the Coronary Care Unit at Aker University Hospital, Norway was one of the earliest studies using statins on 4444 men and women. He found a 30% reduction in heart attacks and 42% reduction in death rates and a 37% reduction in the need for invasive procedures such as angioplasty and bypass surgery.
While on cholesterol lowering medication you will be required to have frequent blood tests; you will need to have regular serum lipid levels regularly to determine that these medicines are working and tests to make sure that they are not causing any liver or muscle damage.
Many experts including Dr Ornish recommend that before getting onto cholesterol medication it is worth attempting to reduce cholesterol levels through dietary means. The Ornish, McDougal and Pritikin programmes have all been found to be effective and utilise a very low cholesterol and fat diet, with less than 10% of calories from fats (unlike most cardiologists who allow 20-30% of calories from fats).
They offer an option for people unwilling or unable to go on a fat free diet. Aggressive cholesterol lowering plus exercise and stress release and personality modification provides significant benefits.
Surgical procedures are becoming increasingly popular for treating patients with heart disease. In this procedure the blockage is bypassed by a graft from the veins of the legs, thus increasing the blood flow to the heart muscle. This is a major operation with mortality rates of 1-2%. In addition, high percentages (5-20%) of patients develop other complications such as infection. One of the major problems with a bypass operation is the fact that the graft closes down in a fairly high percentage of cases, up to 50%, in the first five years. To overcome this, surgeons have started using arterial grafts utilising the internal mammary arteries in the chest, they have a lower failure rate.
While CABG does improve quality of life, many studies have shown that there is not much difference in the death rates between patients who have undergone bypass surgery and those receiving conventional medical treatment. These studies revealed that only patients with the advanced CAD i.e. more than 90% blockage of the left coronary artery, or of three or more vessels with significant blockage with moderate or severe left ventricular dysfunction had improved survival for some years. One must balance this against the fact that some patients die as a consequence of the operation and many suffer non-fatal complications.
This is a less invasive and cheaper procedure than bypass surgery. The cardiologist inserts a thin catheter into an artery in the arm or groin and then guides it into the coronary artery, the area that is blocked. A small tube with a balloon at the end is inserted through the catheter. This tube is then inflated and as it expands it opens out the blockage by compressing the plaque and expanding the artery. There is a small risk of death and a small percentage of patients will have an infarction or ruptured artery during the procedure. A team of surgeons are usually standing by so that, in event of complications, emergency coronary artery surgery can be performed.
The major problem with an angioplasty is that in approximately 30% cases the arteries close down again within a few months necessitating bypass surgery. To overcome this problem various techniques have been developed, such as inserting a small metallic spring (stent) into the artery after the angioplasty to keep the artery open. They reduce the risk of immediate closure to less than 10%. Some years ago very expensive medicated stents have been introduced that have a special coating, which reduces the chances of immediate re-occlusion to less than 5% after an angioplasty. However in 2007 warnings were issued about the safety of these medicated stents and the jury is still out on them.
SURGERY AND ANGIOPLASTY VS LIFESTYLE CHANGES At the time of this edition (2007) there is still controversy about whether surgery or angioplasty alters the long term prognosis of patients with coronary artery disease. What it does, is to improve the quality of life and exercise tolerance. It is likely that in certain sub-groups of patients these procedures will prolong life, especially in those not willing or able to make lifestyle changes. But even here some patients who otherwise would have survived will die or suffer debilitating complications due to the intervention.
On the other hand, a programme of personality and lifestyle changes will prevent the progress of the disease and the clogging up (restenosis) of the arteries that plague these procedures.
Studies have shown that patients who have a Bypass or Angioplasty adopt a healthier lifestyle and diet, more so patients who have had surgery. Many researchers believe that this may explain the short term survival advantages of people with high risk CAD. If the patient does nothing to change his lifestyle and diet, bypass surgery may not prolong life very much.
Dr Ornish found that his programme did not prevent the 30% restenosis rate in the first few months after an angioplasty. Therefore it is preferable to attempt an intensive programme of diet and lifestyle changes before any traumatic procedure that may damage the endothelium and normal anatomy of the arteries. This is especially true if your doctor feels that it would be safe to wait for some time before having the operation or invasive procedures.
It may be possible to avoid surgery if one starts follows this programme seriously at an early stage as soon as one discovers that one has heart disease.
The prevention and screening for heart disease that starts in childhood. There is no doubt that a programme of inculcation of a healthy mental attitude, appropriate diet, exercise and non-smoking prevents the discomfort and suffering caused by coronary artery disease. One should also have regular screening for cholesterol, once in childhood and once every five years after the age of 20. After the age of 40 it is wise to have a full medical examination yearly.
