Chapter 2
It’s the Glucose and the Hemoglobin A1c
In This Chapter
 Seeing how glucose works in the body
Seeing how glucose works in the body
 Identifying chronic high blood glucose with the hemoglobin A1c
Identifying chronic high blood glucose with the hemoglobin A1c
 Reviewing the warning signs of prediabetes
Reviewing the warning signs of prediabetes
 Testing for diabetes
Testing for diabetes
 Getting to know actual patients and their stories
Getting to know actual patients and their stories
The Greeks and Romans knew about diabetes. The way they tested for the condition was — prepare yourself — by tasting people’s urine. In this way, the Romans discovered that the urine of certain people was mellitus, the Latin word for sweet. (They got their honey from the island of Malta, which they called Mellita.) In addition, the Greeks noticed that when people with sweet urine drank, the fluids came out in the urine almost as fast as they went in the mouth, like a siphon. The Greek word for siphon is diabetes. Thus we have the origins of the modern name for the disease, diabetes mellitus.
In this chapter, I cover some not-so-fun stuff about diabetes — the big words, the definitions, and so on. If you really want to understand what’s happening to your body when you have diabetes — and I know I would — then you won’t want to skip this chapter.
Realizing the Role of Glucose
The body has three sources of energy: protein, fat, and carbohydrates. I discuss the first two sources in greater detail in Chapter 8, but I tackle the third one now. Sugar is a carbohydrate. Many different kinds of sugars exist in nature, but glucose, the sugar that has the starring role in the body, provides a source of instant energy so that muscles can move and important chemical reactions can take place. Table sugar, or sucrose, is actually two different kinds of sugar — glucose and fructose — linked together. Fructose is the type of sugar found in fruits and vegetables. Because fructose is sweeter than glucose, sucrose (the combination of fructose and glucose) is sweeter than glucose alone as well. Therefore, your taste buds don’t need as much sucrose or fructose to get the same sweet taste of glucose.
In order to understand the symptoms of diabetes, you need to know a little about the way the body normally handles glucose and what happens when things go wrong. A hormone called insulin finely controls the level of glucose in your blood. A hormone is a chemical substance made in one part of the body that travels (usually through the bloodstream) to a distant part of the body where it performs its work. In the case of insulin, that work is to act like a key to open a cell (such as a muscle, fat, or liver cell) so that glucose can enter. If glucose can’t enter the cell, it can provide no energy to the body.
With this fine-tuning, your body keeps the level of glucose pretty steady at about 60 to 100 mg/dl (3.3 to 6.4 mmol/L) all the time.
Your glucose starts to rise in your blood when you don’t have a sufficient amount of insulin or when your insulin is not working effectively (see Chapter 3). When your glucose rises above 180 mg/dl (10.0 mmol/L), glucose begins to spill into the urine and make it sweet. Up to that point, the kidneys, the filters for the blood, are able to extract the glucose before it enters your urine. The loss of glucose into the urine leads to many of the short-term complications of diabetes. (See Chapter 4 for more on short-term complications.)
Understanding the Hemoglobin A1c
Your blood glucose level is the level of sugar in your blood, a key measure of diabetes. Individual blood glucose tests are great for deciding how you’re doing at that moment and what to do to make it better, but they do not give the big picture. They are just a moment in time. Glucose can change a great deal even in 30 minutes. What you need is a test that gives an integrated picture of many days, weeks, or even months of blood glucose levels. The test that accomplishes this important task is called the hemoglobin A1c.
Hemoglobin is a protein that carries oxygen around the body and drops it off wherever it’s needed to help in all the chemical reactions that are constantly taking place. The hemoglobin is packaged within red blood cells that live in the bloodstream for 60 to 90 days. As the blood circulates, glucose in the blood attaches to the hemoglobin and stays attached. It attaches in several different ways to the hemoglobin, and the total of all the hemoglobin attached to glucose is called glycohemoglobin. Glycohemoglobin normally makes up about 6 percent of the hemoglobin in the blood. The largest fraction, two-thirds of the glycohemoglobin, is in the form called hemoglobin A1c, making it easiest to measure. The rest of the hemoglobin is made up of hemoglobin A1a and A1b.
The more glucose in the blood, the more glycohemoglobins form. Because red blood cells carrying glycohemoglobin remain in the blood for two to three months, glycohemoglobin is a reflection of the glucose control over the entire time period and not just the second that a single glucose test reflects.
Hemoglobin A1c has a number of advantages over the variety of glucose tests for diagnosing diabetes, which I discuss in the later section “Diagnosing diabetes through testing.” Hemoglobin A1c is now as well standardized as glucose testing, and it has the following benefits:
 A1c reflects chronic high blood glucose rather than a few seconds in time.
A1c reflects chronic high blood glucose rather than a few seconds in time.
 A1c has been found to reflect future complications (see Chapter 5) better than fasting glucose.
A1c has been found to reflect future complications (see Chapter 5) better than fasting glucose.
 Fasting isn’t necessary, and acute changes like diet and exercise don’t affect A1c.
Fasting isn’t necessary, and acute changes like diet and exercise don’t affect A1c.
 A1c is not as affected by sample delays on the way to or in the lab.
A1c is not as affected by sample delays on the way to or in the lab.
 A1c is also used to follow the course of diabetes, so the level of treatment needed is immediately understood.
A1c is also used to follow the course of diabetes, so the level of treatment needed is immediately understood.
 A1c is cost-effective, because no further testing is immediately necessary when results are abnormal (whereas an abnormal glucose test requires another glucose or A1c as the next test).
A1c is cost-effective, because no further testing is immediately necessary when results are abnormal (whereas an abnormal glucose test requires another glucose or A1c as the next test).
Following are some disadvantages of hemoglobin A1c:
 Abnormal glucose after eating is a better predictor of heart disease than A1c.
Abnormal glucose after eating is a better predictor of heart disease than A1c.
 Some subjects with anemia, a recent blood transfusion, and abnormal hemoglobin types (there are several types of hemoglobin) produce an unreliable A1c result.
Some subjects with anemia, a recent blood transfusion, and abnormal hemoglobin types (there are several types of hemoglobin) produce an unreliable A1c result.
 Different ethnic groups have different levels for their abnormal A1c.
Different ethnic groups have different levels for their abnormal A1c.
According to one study, in the United States, hemoglobin A1c detects that diabetes is present in one in every five people admitted to a hospital for any reason without a diagnosis of diabetes.
Getting a Wake-Up Call from Prediabetes
Diabetes doesn’t suddenly appear one day without previous notification from your body. For a period of time, which may last up to ten years, you may not quite achieve the criteria for a diagnosis of diabetes but not be quite normal either. During this time, you have what’s called prediabetes.
A person with prediabetes doesn’t usually develop eye disease, kidney disease, or nerve damage (all potential complications of diabetes, which I discuss in Chapter 5). However, a person with prediabetes has a much greater risk of developing heart disease and brain attacks than someone with entirely normal blood glucose levels. Prediabetes has a lot in common with insulin-resistance syndrome, also known as the metabolic syndrome, which I discuss in Chapter 5. The following two sections take the mystery out of whether you may have prediabetes by giving you some guidelines on when to get tested as well as explaining what testing for prediabetes involves.
Knowing whether you should get tested
Approximately 80 million people in the United States have prediabetes, although most of them don’t know it. Testing for prediabetes is a good idea for everyone over the age of 45. I also recommend getting tested if you’re under 45 and overweight and have one or more of the following risk factors:
 A high-risk ethnic group: African American, Hispanic, Asian, or Native American
A high-risk ethnic group: African American, Hispanic, Asian, or Native American
 High blood pressure
High blood pressure
 Low HDL (“good” cholesterol)
Low HDL (“good” cholesterol)
 High triglycerides
High triglycerides
 A family history of diabetes
A family history of diabetes
 Diabetes during a pregnancy or giving birth to a baby weighing more than 9 pounds
Diabetes during a pregnancy or giving birth to a baby weighing more than 9 pounds
Testing for prediabetes
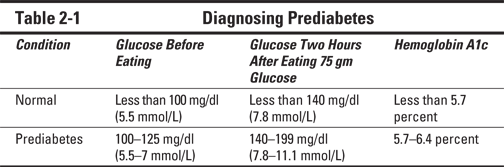
Testing for prediabetes involves finding out your blood glucose level, the level of sugar in your blood. Prediabetes exists when the body’s blood glucose level is higher than normal but not high enough to meet the standard definition of diabetes mellitus (which I discuss in the section “Diagnosing diabetes through testing,” later in this chapter). Testing is done by measuring a random capillary blood glucose. If the level is greater than 100 milligrams per deciliter (mg/dl), a fasting plasma glucose or oral glucose tolerance test is performed. As of 2010, the American Diabetes Association recommends that the hemoglobin A1c (see the next section) can also be used for the definition. Table 2-1 shows the hemoglobin A1c and glucose levels that indicate prediabetes:
 If the glucose before the test (the fasting plasma glucose) is between 100 and 125 mg/dl, the person has impaired (abnormally high) fasting glucose, the glucose before eating (see Table 2-1). The glucose in the fasting state (no food for eight hours) is not normal, but it’s not high enough to diagnose diabetes.
If the glucose before the test (the fasting plasma glucose) is between 100 and 125 mg/dl, the person has impaired (abnormally high) fasting glucose, the glucose before eating (see Table 2-1). The glucose in the fasting state (no food for eight hours) is not normal, but it’s not high enough to diagnose diabetes.
 If the glucose is between 140 and 199 mg/dl at two hours after eating 75 grams of glucose, the person has impaired glucose tolerance. Both impaired fasting glucose and impaired glucose tolerance may be present.
If the glucose is between 140 and 199 mg/dl at two hours after eating 75 grams of glucose, the person has impaired glucose tolerance. Both impaired fasting glucose and impaired glucose tolerance may be present.
 A hemoglobin A1c between 5.7 and 6.4 percent suggests prediabetes.
A hemoglobin A1c between 5.7 and 6.4 percent suggests prediabetes.
After a diagnosis of prediabetes is made, all the techniques described in Chapters 7 through 12 can help prevent the onset of clinical diabetes. If patients with prediabetes are left untreated, large numbers of these patients will develop diabetes over time. Preventing diabetes saves a person almost $10,000 in costs for the treatment of diabetes. And properly responding to a diagnosis of prediabetes prevented almost 20 percent of people with prediabetes from becoming diabetic.
Detecting Diabetes
When prediabetes becomes diabetes, the body’s blood glucose level registers even higher. In this section, I discuss the evidence for diabetes and the symptoms you may experience with diabetes.
Diagnosing diabetes through testing
The standard definition of diabetes mellitus is excessive glucose in a blood sample. For years, doctors set this level fairly high. The standard level for normal glucose was lowered in 1997 because too many people were experiencing complications of diabetes even though they did not have the disease by the then-current standard. In November 2003, the standard level was modified again. In 2009, the International Expert Committee on Diagnosis and Classification of Diabetes Mellitus recommended using the hemoglobin A1c as a diagnostic criterion for diabetes, and the American Diabetes Association subsequently accepted the recommendation.
After much discussion, many meetings, and the usual deliberations that surround a momentous decision, the American Diabetes Association published the new standard for diagnosis, which includes any one of the following four criteria:
 Hemoglobin A1c equal to or greater than 6.5 percent.
Hemoglobin A1c equal to or greater than 6.5 percent.
 Casual plasma glucose concentration greater than or equal to 200 mg/dl, along with symptoms of diabetes. Casual plasma glucose refers to the glucose level when the patient eats normally prior to the test. I discuss symptoms in the section “Examining the symptoms of diabetes” later in this chapter.
Casual plasma glucose concentration greater than or equal to 200 mg/dl, along with symptoms of diabetes. Casual plasma glucose refers to the glucose level when the patient eats normally prior to the test. I discuss symptoms in the section “Examining the symptoms of diabetes” later in this chapter.
 Fasting plasma glucose (FPG) of greater than or equal to 126 mg/dl or 7 mmol/L. Fasting means that the patient has consumed no food for eight hours prior to the test.
Fasting plasma glucose (FPG) of greater than or equal to 126 mg/dl or 7 mmol/L. Fasting means that the patient has consumed no food for eight hours prior to the test.
 Blood glucose of greater than or equal to 200 mg/dl (11.1 mmol/L) when tested two hours (2-h PG) after ingesting 75 grams of glucose by mouth. This test has long been known as the oral glucose tolerance test. Although this time-consuming, cumbersome test is rarely done, it remains the gold standard for the diagnosis of diabetes.
Blood glucose of greater than or equal to 200 mg/dl (11.1 mmol/L) when tested two hours (2-h PG) after ingesting 75 grams of glucose by mouth. This test has long been known as the oral glucose tolerance test. Although this time-consuming, cumbersome test is rarely done, it remains the gold standard for the diagnosis of diabetes.
Following is another way to look at the criteria for diagnosis:
 FPG less than 100 mg/dl (5.5 mmol/L) is a normal fasting glucose.
FPG less than 100 mg/dl (5.5 mmol/L) is a normal fasting glucose.
FPG greater than or equal to 100 mg/dl but less than 126 mg/dl (7.0 mmol/L) is impaired fasting glucose (indicating prediabetes).
FPG equal to or greater than 126 mg/dl (7.0 mmol/L) gives a provisional diagnosis of diabetes.
 2-h PG less than 140 mg/dl (7.8 mmol/L) is normal glucose tolerance.
2-h PG less than 140 mg/dl (7.8 mmol/L) is normal glucose tolerance.
2-h PG greater than or equal to 140 mg/dl but less than 200 mg/dl (11.1 mmol/L) is impaired glucose tolerance.
2-h PG equal to or greater than 200 mg/dl gives a provisional diagnosis of diabetes.
 Hemoglobin A1c equal to or greater than 6.5 percent gives a provisional diagnosis of diabetes. As the hemoglobin A1c rises from normal, the occurrence of diabetes rises with it. If the hemoglobin A1c is equal to or greater than 5.6, the patient has a threefold chance of developing diabetes in the next six years.
Hemoglobin A1c equal to or greater than 6.5 percent gives a provisional diagnosis of diabetes. As the hemoglobin A1c rises from normal, the occurrence of diabetes rises with it. If the hemoglobin A1c is equal to or greater than 5.6, the patient has a threefold chance of developing diabetes in the next six years.
Examining the symptoms of diabetes
The following list contains the most common early symptoms of diabetes and how they occur. One or more of the following symptoms may be present when diabetes is diagnosed:
 Frequent urination and thirst: The glucose in the urine draws more water out of your blood, so more urine forms, making you feel the need to urinate more frequently. As the amount of water in your blood declines, you feel thirsty and drink much more frequently.
Frequent urination and thirst: The glucose in the urine draws more water out of your blood, so more urine forms, making you feel the need to urinate more frequently. As the amount of water in your blood declines, you feel thirsty and drink much more frequently.
 Blurry vision: As the glucose level shifts from normal to very high, the lens of the eye swells due to water intake. This swelling prevents the eye from focusing light at the correct place, and blurring occurs.
Blurry vision: As the glucose level shifts from normal to very high, the lens of the eye swells due to water intake. This swelling prevents the eye from focusing light at the correct place, and blurring occurs.
 Extreme hunger: Inability to get energy in the form of glucose into the muscle cells that need it leads to a feeling of hunger despite all the glucose that is floating in the bloodstream. Such hunger is called “starvation in the midst of plenty.”
Extreme hunger: Inability to get energy in the form of glucose into the muscle cells that need it leads to a feeling of hunger despite all the glucose that is floating in the bloodstream. Such hunger is called “starvation in the midst of plenty.”
 Fatigue: Without sufficient insulin, or with ineffective insulin, glucose can’t enter cells (such as muscle and fat cells) that depend on insulin to act as a key. (The most important exception here is the brain, which does not need insulin to extract glucose from the blood.) As a result, glucose can’t be used as a fuel to move muscles or to facilitate the many other chemical reactions that have to take place to produce energy. A person with diabetes often complains of fatigue and feels much stronger after treatment allows glucose to enter his or her cells again.
Fatigue: Without sufficient insulin, or with ineffective insulin, glucose can’t enter cells (such as muscle and fat cells) that depend on insulin to act as a key. (The most important exception here is the brain, which does not need insulin to extract glucose from the blood.) As a result, glucose can’t be used as a fuel to move muscles or to facilitate the many other chemical reactions that have to take place to produce energy. A person with diabetes often complains of fatigue and feels much stronger after treatment allows glucose to enter his or her cells again.
 Weight loss: Weight loss occurs among some people with diabetes because they lack insulin, the builder hormone. When the body lacks insulin for any reason, the body begins to break down. You lose muscle tissue. Some of the muscle converts into glucose even though the glucose can’t get into cells. It passes out of your body in the urine. Fat tissue breaks down into small fat particles that can provide an alternate source of energy. As your body breaks down and you lose glucose in the urine, you often experience weight loss. However, most people with diabetes are heavy rather than skinny. (I explain why in Chapter 3.)
Weight loss: Weight loss occurs among some people with diabetes because they lack insulin, the builder hormone. When the body lacks insulin for any reason, the body begins to break down. You lose muscle tissue. Some of the muscle converts into glucose even though the glucose can’t get into cells. It passes out of your body in the urine. Fat tissue breaks down into small fat particles that can provide an alternate source of energy. As your body breaks down and you lose glucose in the urine, you often experience weight loss. However, most people with diabetes are heavy rather than skinny. (I explain why in Chapter 3.)
 Persistent vaginal infection among women: As blood glucose rises, all the fluids in your body contain higher levels of glucose, including the sweat and body secretions such as semen in men and vaginal secretions in women. Many bugs, such as bacteria and yeast, thrive in the high-glucose environment. Women begin to complain of itching or burning, an abnormal discharge from the vagina, and sometimes an odor.
Persistent vaginal infection among women: As blood glucose rises, all the fluids in your body contain higher levels of glucose, including the sweat and body secretions such as semen in men and vaginal secretions in women. Many bugs, such as bacteria and yeast, thrive in the high-glucose environment. Women begin to complain of itching or burning, an abnormal discharge from the vagina, and sometimes an odor.

A study in the November 2007 issue of Diabetes Care, however, showed that in a group of over 15,000 people being treated for diabetes, 44 percent of people with type 2 diabetes reported not one of the symptoms above in the previous year when given a questionnaire. It is no wonder that a third of people with diabetes don’t know they have it.
Tracing the History of Diabetes Treatment
More than 2,000 years ago, people writing in China and India described a condition that must have been diabetes mellitus. The description is the same one that the Greeks and Romans reported — urine that tasted sweet. Scholars from India and China were the first to describe frequent urination. But not until 1776 did researchers discover the cause of the sweetness — glucose. And it wasn’t until the 19th century that doctors developed a new chemical test to actually measure glucose in the urine.
Later discoveries showed that the pancreas produces a crucial substance that controls the glucose in the blood: insulin. Since that discovery was made, scientists have found ways to extract insulin and purify it so it can be given to people whose insulin levels are too low.
After insulin was discovered, diabetes specialists, led by Elliot Joslin and others, recommended three basic treatments for diabetes that are as valuable today as they were in 1921:
 Diet (see Chapter 8)
Diet (see Chapter 8)
 Exercise (see Chapter 9)
Exercise (see Chapter 9)
 Medication (see Chapter 10)
Medication (see Chapter 10)
Although the discovery of insulin immediately saved the lives of thousands of very sick individuals for whom the only treatment had been starvation, it did not solve the problem of diabetes. As these people aged, they were found to have unexpected complications in the eyes, the kidneys, and the nervous system (see Chapter 5). And insulin didn’t address the problem of the much larger group of people with diabetes now known as type 2 (see Chapter 3). Their problem was not lack of insulin but resistance to its actions. (Fortunately, doctors do have the tools now to bring the disease under control.)
The next major leap in the effort to treat diabetes, occurring in 1955, was the discovery of the group of drugs called sulfonylureas (see Chapter 10), the first drugs that could be taken by mouth to lower blood glucose levels. But even while those drugs were improving patient care, the only way to know if someone’s blood glucose level was high was to test the urine, which was entirely inadequate for good diabetic control (see Chapter 7).
Around 1980, the first portable meters for blood glucose testing became available. For the first time, doctors and patients could relate treatment to a measurable outcome. This development has led, in turn, to the discovery of other great drugs for diabetes, such as metformin, exenatide, and others yet to come.
If you are not using these wonderful tools for your diabetes, you are missing the boat. You can find out exactly how to use portable meters in Part III.
Explaining the Obesity (and Diabetes) Epidemic
Many changes explain the epidemic of obesity and diabetes that began to explode in the 1950s and ’60s. Here are some of them:
 The availability of fast-food restaurants and vending machines
The availability of fast-food restaurants and vending machines
 The frequency of television commercials for foods filled with fats and sugar
The frequency of television commercials for foods filled with fats and sugar
 The large number of screens watched passively all day, from TVs to smartphones
The large number of screens watched passively all day, from TVs to smartphones
 The larger, higher-calorie meals that tend to be eaten, both at home and at restaurants
The larger, higher-calorie meals that tend to be eaten, both at home and at restaurants
 The dependence on vehicles for much movement
The dependence on vehicles for much movement
 The huge increase in mass-produced, high-calorie convenience foods
The huge increase in mass-produced, high-calorie convenience foods
What steps can people take to reverse this trend? Some of the ideas developed to reverse the high rate of cigarette smoking can be recycled, but the process takes years for the whole population. What you can do immediately is contained in Part III. Some of the population-wide measures include the following strategies:
 A tax on low-nutrition foods like sweetened beverages
A tax on low-nutrition foods like sweetened beverages
 Better labeling of foods; for example, a red label for low-nutrition, high-calorie foods; a yellow label for intermediate foods; and a green label for low-calorie, high-nutrition foods
Better labeling of foods; for example, a red label for low-nutrition, high-calorie foods; a yellow label for intermediate foods; and a green label for low-calorie, high-nutrition foods
 A ban on or reduction of advertising of junk foods
A ban on or reduction of advertising of junk foods
 School-based programs promoting healthier eating and elimination of soft drinks and sugared juices
School-based programs promoting healthier eating and elimination of soft drinks and sugared juices
 A low, fixed amount of screen time for children
A low, fixed amount of screen time for children
Putting Faces to the Numbers: Sharing Some Real Patient Stories
The numbers that are used to diagnose diabetes don’t begin to reflect the human dimensions of the disease. People end up with test results after days, months, or even years of minor discomforts that reach the point where they can no longer be tolerated. The next few stories of real (though renamed) patients can help you understand that diabetes is a disease that happens to real people — people who are working, relaxing, traveling, sleeping, and doing many other things that make life so complex.
Debby O’Leary’s active sex life with her husband was continually being interrupted by vaginal yeast infections, which resulted in an unpleasant odor, redness, itching. Over-the-counter preparations promptly cured the condition, but it always rapidly returned. Finally, after three of these infections in two months, she decided to see her gynecologist. The gynecologist told her she needed a prescription drug. The cure lasted a little longer this time, but the infection promptly returned. On a return visit, the gynecologist did a urinalysis and found glucose in her urine. A random blood test showed a glucose of 243 mg/dl (13.5 mmol/L). He sent her to an internist, who ordered a variety of tests including a fasting blood glucose, which was 149 mg/dl (8.3 mmol/L). The doctor told her she had diabetes and recommended exercise and diet change to start with. She followed his advice, and as a result she not only lowered her blood glucose to the point that she no longer developed yeast infections but also lost weight and increased her energy, making her sex life with her husband even more satisfying.
 Insulin is essential for growth. In addition to providing the key to entry of glucose into the cell, insulin is considered the
Insulin is essential for growth. In addition to providing the key to entry of glucose into the cell, insulin is considered the  Diagnosing prediabetes can be the best thing that ever happened to a person! It could be the wake-up call that he or she needs. The diagnosis may motivate a person to make crucial lifestyle changes, especially in diet and exercise, which have been shown to prevent the onset of diabetes in people with prediabetes. And for people whose prediabetes doesn’t respond to lifestyle changes, medication may accomplish the same thing.
Diagnosing prediabetes can be the best thing that ever happened to a person! It could be the wake-up call that he or she needs. The diagnosis may motivate a person to make crucial lifestyle changes, especially in diet and exercise, which have been shown to prevent the onset of diabetes in people with prediabetes. And for people whose prediabetes doesn’t respond to lifestyle changes, medication may accomplish the same thing. Sal Renolo was a 46-year-old black-belt judo instructor. Despite his very active lifestyle, he was not careful about his diet and had gained 16 pounds in the last few years. He was more fatigued than he had been in the past but blamed this fatigue on his increasing age. His mother had diabetes, but he assumed that his physical fitness would protect him from this condition. However, he could barely get through a one-hour class without excusing himself for a bathroom break. One of his new students had diabetes, and he suggested to Sal that he ought to have the problem checked, but Sal insisted that he could not possibly have diabetes with all his activity. The symptoms of fatigue and frequent urination got worse, and Sal finally made an appointment with the doctor. Blood tests revealed a random blood glucose level of 264 mg/dl (14.7 mmol/L). The following week, another random blood glucose was 289 (16.0 mmol/L). The doctor told Sal he had diabetes, but Sal refused to believe it. He left the doctor’s office angry but vowed to lose weight and did so successfully. On a repeat visit to the doctor, a random glucose was 167 mg/dl (9.3 mmol/L). Sal told the doctor that he knew he didn’t have diabetes, but his resolve to eat carefully didn’t last, and he was back six weeks later with a glucose of 302 mg/dl (16.8 mmol/L). Finally, Sal accepted the diagnosis and started treatment. He rapidly returned to his usual state of health, and the fatigue disappeared.
Sal Renolo was a 46-year-old black-belt judo instructor. Despite his very active lifestyle, he was not careful about his diet and had gained 16 pounds in the last few years. He was more fatigued than he had been in the past but blamed this fatigue on his increasing age. His mother had diabetes, but he assumed that his physical fitness would protect him from this condition. However, he could barely get through a one-hour class without excusing himself for a bathroom break. One of his new students had diabetes, and he suggested to Sal that he ought to have the problem checked, but Sal insisted that he could not possibly have diabetes with all his activity. The symptoms of fatigue and frequent urination got worse, and Sal finally made an appointment with the doctor. Blood tests revealed a random blood glucose level of 264 mg/dl (14.7 mmol/L). The following week, another random blood glucose was 289 (16.0 mmol/L). The doctor told Sal he had diabetes, but Sal refused to believe it. He left the doctor’s office angry but vowed to lose weight and did so successfully. On a repeat visit to the doctor, a random glucose was 167 mg/dl (9.3 mmol/L). Sal told the doctor that he knew he didn’t have diabetes, but his resolve to eat carefully didn’t last, and he was back six weeks later with a glucose of 302 mg/dl (16.8 mmol/L). Finally, Sal accepted the diagnosis and started treatment. He rapidly returned to his usual state of health, and the fatigue disappeared.