CHAPTER 2
Cartilage: Helping Us Move
 Most people know cartilage as gristle. It’s the blob on the bone of a T-bone steak, the globs on chicken drumsticks, and nearly the entire skeleton of man-eating sharks.
Most people know cartilage as gristle. It’s the blob on the bone of a T-bone steak, the globs on chicken drumsticks, and nearly the entire skeleton of man-eating sharks.
Human beings, too, are blessed with cartilage. Without cartilage, we couldn’t wiggle our ears, scrunch up our noses, swallow with ease, or move our joints. Tough, elastic, spongy, and springy, cartilage has many vital roles: It acts as a framework, works as a shock absorber, and reduces the friction between moving parts.
The Many Roles of Cartilage
No bones about it, cartilage is a fascinating substance. There’s nothing else quite like it in the body. Unlike its cousins connective tissue and bone, it contains no nerves, blood vessels, or lymph system. Nutrients needed to maintain it are not transported via blood or lymph fluid but by synovial fluid, which flows into every nook and cranny when pressure is applied to the joint and released.
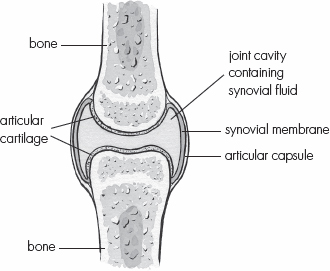
Figure 2: Shown here is a typical joint with the locations of bone, articular cartilage, a synovial membrane, and the joint cavity containing synovial fluid.
Synovial fluid is a transparent, raw egg white–like substance that contains albumin, fat, mineral salts, and a large organic molecule called hyaluronic acid in addition to water. Indeed, water is the chief constituent of healthy cartilage—65 to 85 percent. Health experts like to say it is possible for us to starve our cartilage in two easy ways: by not drinking enough water and by not exercising. But water is not nearly as helpful as broth, a substance that includes not only water but the amino acids, collagen, and other components the body needs to manufacture healthy cartilage.
The remarkable resilience of cartilage comes from its gelatinous matrix. Jiggly but not amorphous, this matrix is highly structured with the complex combinations of proteins and sugars known as proteoglycans, whose principal job is to get and hold water. The most prominent proteoglycans in cartilage are the sulfur-containing molecules chondroitin sulfate and keratan sulfate. These molecules carry negative charges and repel each other, creating space for the water they need to attract and hold.
The most common type of cartilage in the human body is hyaline cartilage, a hard, gristly, bluish translucent material, which—when healthy—is also pliable. Its strength comes from a dense, crisscrossing ropey network of collagenous fibers. Its resilience derives from the gel-like matrix into which these fibers are embedded. The fibrils found on the outside of cartilage are so tough and densely packed that they are known as the “armor plate layer.”
Chondrocytes Build Cartilage
Living within the matrix are the cartilage cells themselves. Known as chondrocytes, these cells reside in little isolation chambers known as lacunae, where they regulate cartilage metabolism, manufacture proteoglycan molecules and collagenous fibers, and build new cartilage as necessary. To do so, the chondrocytes need the right nutrients delivered in the right proportions to them by the water and synovial fluid. In addition, they require twenty to thirty different enzymes, without which the complex sugars cannot be properly synthesized and coupled to the core proteins.
During childhood and adolescence, chondrocytes regularly build new cartilage matrix, which can ossify into bone. In this way, nature designed our skeletons to grow to full size. In adulthood, the construction slows down and the chondrocytes lay new deposits of cartilage only on the surface of existing cartilage. Although for most adults the rate of cellular reproduction and repair is slow, individuals with healthy cartilage manage to maintain equilibrium between the creation of new cartilage and decomposition of the old.

A Change in Proportion
If we compare the cartilage of young healthy mammals with old and sick ones, we see different proteoglycan formation. In young ones, the chondroitin sulfate chains are considerably longer than the keratan sulfate ones. Studies done on old folks and old cows, however, show shorter chondroitin sulfate chains and longer keratan sulfate chains. With aging, the two components of cartilage become about equal in length, which results in hunched-over little proteoglycans that are less able to hold and attract water. According to Arnold I. Caplan, PhD, of Case Western Reserve University, “This difference may be responsible, at least in part, for the development of some forms of osteoarthritis in older people. After all, if the proteoglycans made in cartilage by aging chondrocytes have a lessened capacity to structure water, the resilience of the cartilage must be compromised, and with it the cushioning of bones in the joints.” This finding suggests the ideal broth for cartilage regeneration might come from young animals.


Can We Regenerate Our Cartilage?
While common sense tells us “like can feed like,” most people believe cartilage regeneration is improbable if not impossible. However, the late John F. Prudden, MD, DSci (1920–1998), known as the “father of cartilage therapy,” liked to explain how cartilage regeneration could work by comparing it to “the mesenchyme in a growing fetus.”
Mesenchyme is a tissue derived from the mesoderm, the layer of primordial tissue in the embryo from which muscles, bones, cartilage, tendons, ligaments, fat, and bone marrow develop. Mesoderm, endoderm, and ectoderm are the three primary germ layers from which all cells and tissues in the body derive.
Like cartilage itself, mesenchyme consists of a gelatinous matrix with fibers. Because its germ cells are the prototypes for healthy tissue, it comes rigged with maturation factors or biodirectors that tell the body not only how to create cartilage, bone marrow, the dermis of skin, the dentin of teeth, and other tissues, but also how to correct abnormalities.
Standard anatomy and physiology texts discuss mesenchyme primarily in terms of babies growing in the womb, but Dr. Prudden explained that we should consider what happens every time the human body mends a broken bone. First, the circulatory system cleans up the bony wreckage. Next, undifferentiated (meaning unspecialized) cells that are remarkably similar to mesenchyme settle in, multiply, and develop into the specialized cartilage cells known as chondrocytes. These chondrocyte cells, in turn, produce the cartilage matrix that is needed to fill the gaps and bind the bone fragments together. As the cartilage calcifies, new bone forms.
This scenario suggests adults can rebuild cartilage, though it is rare indeed for it to happen spontaneously in the case of people with osteoarthritis and other rheumatoid diseases. Dr. Prudden, however, accomplished it with many of his patients using bovine tracheal cartilage supplements, and he published the results in major medical journals. The cartilage Dr. Prudden used was taken from the tracheas of young healthy calves and not from humans, but the match was close enough. He furthermore discovered that cartilage could reverse diseases such as psoriasis and cancer that would not seem to be cartilage-related at all. We’ll discuss his pioneering work curing incurables with arthritis, autoimmune disorders, and cancer later in this book. For now, the commonsense principle of “you are what you eat” suggests the wisdom of consuming at least one cup of cartilage-rich broth daily for optimum health and longevity, more if you are dealing with degenerative disease.

Chondroitin sulfates play other important roles: They inhibit enzymes that like to chew up cartilage, and they interfere with enzymes that would hijack the transport of nutrients. Both types of enzymes seem to be gluttonous in the cartilage of aging mammals.
Changes in chondroitin sulfate and keratan sulfate accompany other changes in aging or unhealthy joints as well. It seems that if one part of the cartilage system breaks down, another is sure to follow. If, for any reason, the collagen and elastic network loses its shape and its strength, the gelatinous matrix growing on and around it will suffer the loss of support as well. Once cartilage is unable to attract and hold water, the chondrocytes lose their source of nourishment and their much-needed ability to reproduce and repair. And so it goes. However the problems begin, the unhappy result is the decomposition of old cartilage at a faster pace than the creation of new cartilage.
Once this happens, it is only a matter of time before the cartilage that was once plump and resilient becomes painfully thin, dried out, worn down, stiff, cracked, and inflamed. Then the bones that the cartilage was designed to protect start rubbing each other the wrong way, causing bone spurs, bone hardening, inflammation, and pain (see the illustration comparing a normal joint to one with osteoarthritis on here).
Conventional medical opinion holds that joint problems are inevitable with aging and that damage is irreparable and irreversible. But it appears the human body can revert to the “young” type of cartilage and regenerate young healthy cartilage if provided with the right tools. And it’s undoubtedly even easier to prevent the damage to begin with. That means providing the right constituents of cartilage—glycine, proline, glutamine, proteoglycans, and other nutrients found in cartilage-rich bone broth. The larger cartilage molecules may not be absorbed intact, but the components certainly are.