22. ACETAMINOPHEN
Acetaminophen (paracetamol) is an extremely popular over-the-counter pain reliever and fever reducer. By some accounts, it is the most widely used drug in the world. You have almost certainly taken it in some form. In the United States, the most popular brand name is Tylenol. However, there is no patent on the drug, and it is manufactured and sold by many different companies. One of the reasons acetaminophen is so popular is because it has long been considered very safe.
Originally discovered in the late 1800s, acetaminophen has been available in the U.S. since the 1950s. Acetaminophen is different from most over-the-counter pain medications in that it is not a nonsteroidal anti-inflammatory (NSAID) drug—it’s in the aniline family. Ibuprofen (Advil), naproxen (Aleve), and aspirin are all NSAIDs, which are more effective than acetaminophen at reducing pain but can have some nasty side effects such as gastric bleeding, heart attack, and stroke. Ibuprofen has been linked to birth defects, premature birth, and miscarriage. Aspirin should not be given to children because of the risk of Reye syndrome, a potentially fatal brain disease. Acetaminophen is superior to NSAIDs in all of these respects. In fact, acetaminophen was long considered to have virtually no side effects when used as recommended. This is why it is considered to be such a safe drug and why it is frequently prescribed and recommended as a first-line treatment.
Many people were surprised, therefore, when a panel of experts convened by the FDA in 2009 recommended that the maximum daily dose, as well as the maximum single adult dose, be lowered. The FDA later proposed that all products containing acetaminophen carry stronger warning labels. In 2013, the radio program This American Life produced an episode titled “Use Only as Directed” in collaboration with the nonprofit group ProPublica. The show drew attention to the fact that although many, if not most, consumers were unaware of it, taking a little more than the recommended dose of acetaminophen could cause acute liver failure. In fact, as the show pointed out, at least a few hundred Americans die of acetaminophen overdoses every year. Many people started to feel like acetaminophen was maybe not so safe after all.
This is probably a good thing, because it turns out there is a difference between “safe when used as directed” and “safe.” Acetaminophen is quite safe, as long as you don’t take too much of it (and as long as you aren’t allergic to it). But if you take too much of it, it will kill you. Acetaminophen is metabolized by the liver, so it can be eliminated in urine. This is just one of the important things your liver is quietly doing for you. There are a few different ways metabolism can happen. Acetaminophen is broken down into harmless by-products in two primary pathways. However, these pathways have a limited capacity, and when they are saturated, the drug is metabolized increasingly via a third pathway. Unfortunately, one of the by-products of this pathway is hepatotoxic—it binds to and kills liver cells. You might not spend a lot of time thinking about your liver, but you really need it. If your liver fails, you need to get a new one, or you’ll die.
So the biggest problem with acetaminophen is that people take too much of it. People have a tendency to take too much of other pain relievers too, which is also a problem. But taking too much acetaminophen is a much more immediate problem. The reason is that acetaminophen has a narrow therapeutic window. The difference between a safe dose and a lethal dose is small. This is not the case for ibuprofen, for example. Unfortunately, acetaminophen doesn’t work as well as ibuprofen, so people might be more inclined to take more of it. In addition, it is often included as a component of cough and cold medicines, allergy medicines, sleep aids, aspirin-based headache medicines, and opioid pain killers. The drug is so common that many people take it without even knowing it. That’s a problem, because all those sources can add up to a toxic dose. Liver damage can occur after a single large dose, or after sustained doses that moderately exceed the recommended limits. Contrary to what you might think, if prompt medical attention is sought, the prognosis for acute overdose is actually better than for a chronic overdose. This is because there is an antidote (N-acetylcysteine). So if you accidentally take too much acetaminophen, get to a doctor right away, even if you don’t have any symptoms.
As it turns out, even when taken as directed, acetaminophen is not as free of side effects as we once thought, especially when it is taken over a long time. Although it is considered safe during pregnancy, maternal consumption of acetaminophen has been tied to an increased incidence of asthma, ADHD, neurodevelopmental problems, and problems with the development of sexual organs in babies. But this evidence has not been strong enough to warrant a change in the established clinical recommendations.
If it surprises you that there are side effects, it shouldn’t. Acetaminophen is a drug. The only reason to take it at all is because it is biologically active. It is interacting with your body’s chemistry and, like most pharmaceuticals, it is doing so in a nonspecific way. There is no such thing as a perfectly safe drug. That doesn’t mean there is never a situation where acetaminophen use is warranted.
When you consider the safety of acetaminophen, you have to take into account not only the potential positive and negative effects of the drug but also the positive and negative effects of the alternatives. If you don’t take acetaminophen, you’re either going to take something else or live with the pain. In some cases, it might be worth trying to stick it out. Take a walk, or a bath, or a nap, or have a really good laugh. If your child is teething, you could try a cold washcloth and a little distraction. But in reality, this is not always going to cut it. Pain can be debilitating and fevers can be dangerous. Fevers can be especially problematic in some of the most vulnerable populations: young children and pregnant women—the very same populations for which the risk of NSAIDS is well established. There are many situations in which acetaminophen may be the most appropriate treatment; the key is to use it carefully.
Keep track of how much you’re using (write it down). Measure liquid doses carefully. Don’t use even a little bit more than the recommended amount. Pay attention to what’s in different products, and don’t take more than one acetaminophen-containing product at a time. Use as little as you can and don’t use it with alcohol. And, whatever you do, keep acetaminophen (and all other drugs) out of the reach of children.
SUMMARY
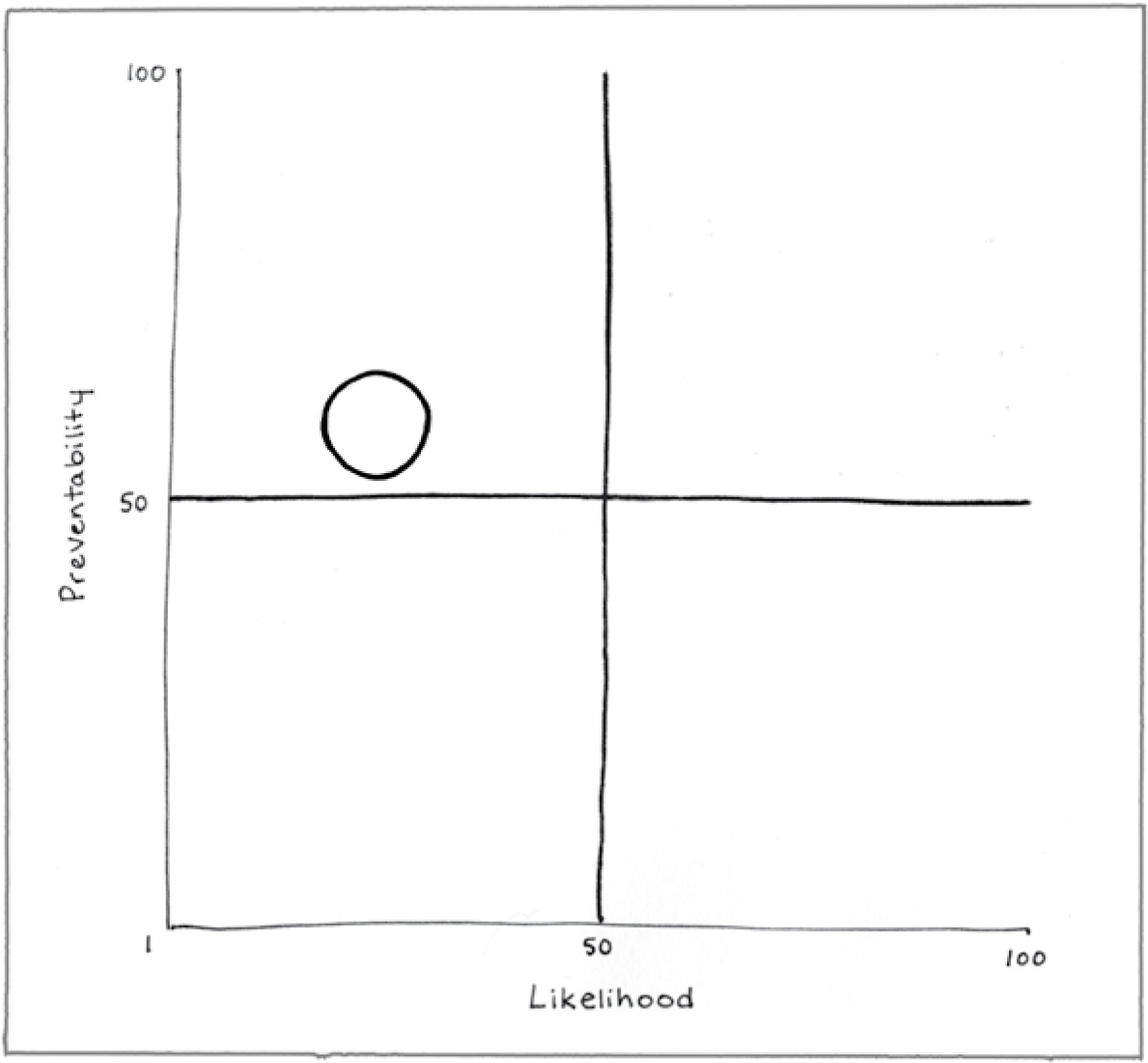
Preventability (60)
Sometimes you can choose to use another pain reliever or to use a product that does not have acetaminophen as an ingredient, but for some populations, acetaminophen is the safest choice.
Likelihood (22)
If you aren’t allergic to it, and if you use acetaminophen as directed, you are unlikely to experience a negative outcome. However, due to the narrow therapeutic range, it is surprisingly easy to take too much.
Too much acetaminophen can kill your liver, leading to a liver transplant or death.
REFERENCES
Aminoshariae, A., & Khan, A. (2015). Acetaminophen: Old drug, new issues. Journal of Endodontics, 41, 588–593.
Brune, K., Renner, B., & Tiegs, G. (2015). Acetaminophen/paracetamol: A history of errors, failures and false decisions. European Journal of Pain, 19, 953–965.
Gavura, S. (2011, August 4). Tylenol: Safe painkiller, or drug of hepatic destruction? Science-Based Medicine. Retrieved from https://sciencebasedmedicine.org/tylenol-safe-painkiller-or-drug-of-hepatic-destruction/
Gavura, S. (2013, October 10). Acetaminophen: Still the pain reliever you should trust? Science-Based Medicine. Retrieved from https://www.sciencebasedmedicine.org/acetaminophen-still-the-pain-reliever-you-should-trust/
Hall, H. (2014, February 18). Tylenol may not be as safe and effective as we thought. Science-Based Medicine. Retrieved from https://sciencebasedmedicine.org/tylenol-may-not-be-as-safe-and-effective-as-we-thought/
Kress, H. G., & Untersteiner, G. (2017). Clinical update on benefit versus risks of oral paracetamol alone or with codeine: Still a good option? Current Medical Research Opinion, 33, 289–304.
Prescott, L. F. (2000). Paracetamol: Past, present, and future. American Journal of Therapy, 7, 143–147.
U.S. National Library of Medicine. (2017, April 15). Acetaminophen. Retrieved from https://medlineplus.gov/druginfo/meds/a681004.html