24. MEDICAL IMAGING
Skin is opaque, concealing from view all of the inner workings of our bodies. So for most of human history, there was only one way to know what was going on inside the human body: open it up and have a look. Medically, this is what we would refer to as exploratory surgery. Obviously, this method has a number of undesirable side effects. This all changed when Wilhelm Roentgen, a German physicist, made the first X-ray of his wife’s hand in 1895. This ushered in the age of medical imaging, when doctors could visualize internal structures without ever using a scalpel. Our current medical imaging technology is far more advanced than those first blurry images. It is now possible to record high-resolution three-dimensional images of the body and even to create movies of physiological processes like the heart beating. It is now standard to capture the first pictures of our children before they are born.
The pioneers of X-rays used them with wild abandon. They quickly found that too high a dose could cause burns, but it wasn’t until later that the more insidious, long-term effects of X-ray imaging were discovered. As most people are already aware, X-rays, like gamma rays, can cause cancer. This is because X-rays are a form of ionizing radiation. They are energetic enough to knock electrons off atoms or molecules, including the molecules that make up your DNA. Your body has a mechanism for recovering from these insults, but it is imperfect. The higher the dose of radiation, the more damage there is, and the more likely it is that there will be a mistake that ends in cancer. This makes X-rays somewhat less appealing, and it might put you off medical imaging in general. But not all imaging was created equal, in terms of either risks or diagnostic value.
X-ray imaging is used in a few different contexts, and the way it is used changes the overall risk it presents. A plain X-ray, for example, uses much less radiation than a computed tomography (CT) scan. A chest CT scan exposes a patient to an effective dose that is 3,500 times higher than a standard posterior-anterior chest X-ray. On the other hand, a CT scan provides much higher resolution and three-dimensional spatial localization. The risks of exposure to ionizing radiation are usually estimated based on the health outcomes of the survivors of the two atomic bomb explosions in Japan at the end of World War II. These survivors showed a small but significant increase in radiation-attributable cancer risk. They were exposed to between 5 and 20 mSv of radiation (a millisievert is a unit of effective dose), which is not so much greater than the effective dose from a single CT procedure, which ranges from 1 to 10 mSv. The mention of atomic bombs might scare your pants off, but remember that the increase in probability, estimated to be about 0.05% for a single CT scan, is much less than the odds that you would get cancer anyway, which are about one in five. You’ll have to decide for yourself whether that is good news or bad news. In any case, the risk from radiation is not negligible, so it pays to think about it and discuss your options with your doctor. As you consider these options, you might want to bear the following points in mind. First, exposures add up. Second, some populations are more sensitive to radiation damage, like women and, especially, children. Finally, there are situations when a CT scan is medically necessary and might even safe your life.
Positron emission tomography (PET), like CT, relies on ionizing radiation to produce images. In this test you actually ingest a radioactive molecule—a sugar that is absorbed into cells when they require energy. The radioactivity that is emitted from these molecules acts like a beacon, effectively marking the location of the cells that absorbed them. PET is primarily used for cancer imaging. Rapidly dividing cancer cells require more metabolic energy than other cells in the body and therefore absorb more of the radioactive sugar. The effective dose of a PET scan is about 14 mSv, which exceeds the range of CT.
Like CT, magnetic resonance imaging (MRI) can create detailed three-dimensional images of your insides. Unlike CT, MRI does not use ionizing radiation and is not known to cause cancer. MRI relies on a combination of applied magnetic fields and radio waves. In order to get this type of imaging you have to lie in the bore of a magnet, which is usually a small tube. MRI also takes much longer than CT, which means you need to keep very still for a long time in a small space. This can be difficult for people who are claustrophobic as well as for children. Because very strong magnetic fields are involved, it is very important not to have any metal on or in your body, or even in the room with you when the magnet is on. This means people with artificial joints, bone plates or screws, pacemakers, deep brain stimulators, and other metallic devices should not get MRI scans. Metal implants can heat up and move, which is obviously not great when they are inside your body. Metallic objects can also cause distortions in the field that destroy the images. In addition, it is worth noting that just because magnetic fields do not alter DNA, it doesn’t mean that they have no biological effect. Our bodies, and especially our brains, rely heavily on electrical potentials to carry out business. Applying a strong magnetic field may throw this ongoing business out of whack. Nevertheless, MRI is considered a very safe procedure for people who don’t have any metal implants. There isn’t a lot known about how magnetic fields might impact a fetus, so MRIs are not recommended for pregnant women unless there is a strong medical indication, for either the woman or her unborn child.
Many people associate ultrasound with babies because at least one ultrasound is now part of the standard of care for most pregnancies. It can reveal structural abnormalities in the fetus, show a breech presentation, and expose other problems, like placenta previa. Ultrasound produces images based on the reflection of mechanical waves, or pressure waves. These waves are similar to sound waves but are out of the auditory perceptible range (which is why they are called ultrasound). Ultrasound does not involve any ionizing radiation and is considered very safe, which is why it is used during pregnancy. However, it does have some effects on tissue. Notably, it produces heat, which is generally bad, especially for a developing fetus. For this reason, ultrasound is recommended only when it is medically necessary. One study has linked the severity of autism in autistic children (not the incidence of autism in the general population) to the number of first-trimester ultrasound scans, but this connection is controversial. Nevertheless, getting a high-resolution fetal ultrasound image at the mall for souvenir purposes is discouraged. Ultrasound has many applications beyond fetal ultrasound. Because it is especially useful for capturing movement, cardiac ultrasound is very common.
Medical imaging represents a huge diagnostic benefit, and there is no question that it has saved many lives as well as relieved a great deal of pain and suffering. At the same time, as with almost everything in life, it is wise to proceed with caution, consideration, and information.
SUMMARY
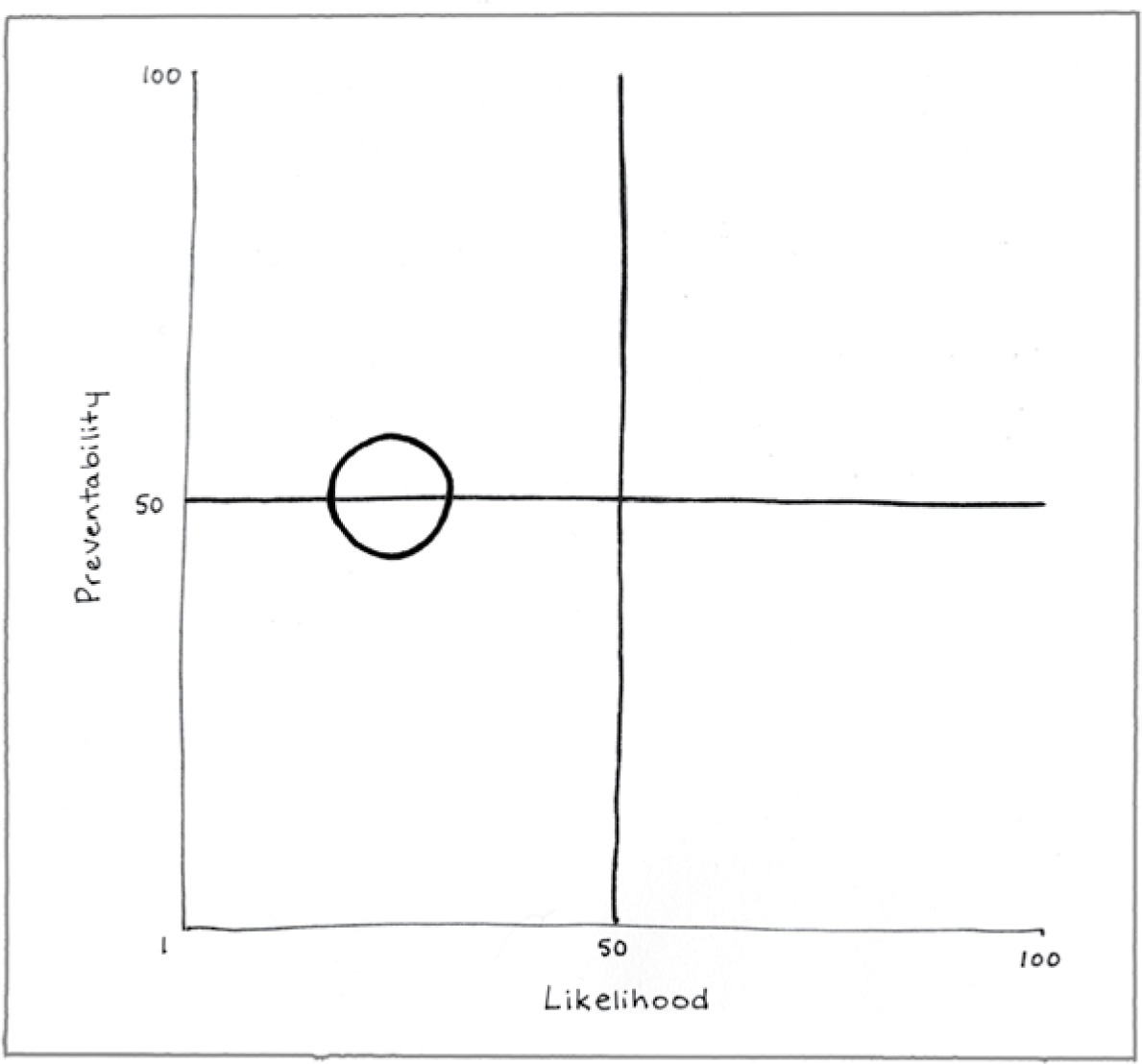
Preventability (51)
You can be cognizant of the risks of medical imaging and try to minimize the number of imaging procedures you have, and you certainly can avoid souvenir ultrasounds. But medical imaging is often necessary and appropriate.
Likelihood (25)
For adults, and especially men, medical imaging does not increase the risk of cancer or other negative health outcomes much. In children, the risks associated with exposure to ionizing radiation are a greater concern.
Consequence (97)
Ionizing radiation is known to cause cancer, so the potential consequences of too many head CTs can be grim.
American Cancer Society. (2015, February 24). Do x-rays and gamma rays cause cancer? Retrieved from https://www.cancer.org/cancer/cancer-causes/radiation-exposure/x-rays-gamma-rays/do-xrays-and-gamma-rays-cause-cancer.html
Health Physics Society. (2010, January). Radiation exposure from medical exams and procedures. Retrieved from http://hps.org/documents/Medical_Exposures_Fact_Sheet.pdf
Mayo Clinic. (2017, December 30). MRI. Retrieved from https://www.mayoclinic.org/tests-procedures/mri/home/ovc-20235698
McLennan, A. (2016). Ultrasound and autism spectrum disorder. Australian Journal of Ultrasound Medicine, 19, 131–132.
National Cancer Institute. (2013, July 16). Computed tomography (CT) scans and cancer. Retrieved from https://www.cancer.gov/about-cancer/diagnosis-staging/ct-scans-fact-sheet
National Institute of Biomedical Imaging and Bioengineering. (2016, July). Ultrasound. Retrieved from https://www.nibib.nih.gov/science-education/science-topics/ultrasound
Nikolić, L., Bataveljić, D., Andjus, P. R., Nedeljković, M., Todorović, D., & Janać, B. (2013). Changes in the expression and current of the Na+/K+ pump in the snail nervous system after exposure to a static magnetic field. Journal of Experimental Biology, 216, 3531–3541.
U.S. Food and Drug Administration. (2017, December 5). Computed tomography (CT). Retrieved from https://www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/MedicalX-Rays/ucm115317.htm
U.S. Food and Drug Administration. (2017, December 5). What are the radiation risks from CT? Retrieved from https://www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/MedicalX-Rays/ucm115329.htm
Webb, S. J., Garrison, M. M., Bernier, R., McClintic, A. M., King, B. H., & Mourad, P. D. (2017). Severity of ASD symptoms and their correlation with the presence of copy number variations and exposure to first trimester ultrasound. Autism Research, 10, 472–484.