50. PUBLIC TRANSPORTATION
Planes, trains, buses, and subways are inexpensive, safe, and usually convenient forms of public transportation. Millions of people use public transportation to get to work, school, or vacation. However, some people worry that when they disembark, they take along more than their luggage or baggage—they worry that they will pick up a germ that will make them sick. A survey of people from 12 different countries revealed that 12% of the respondents avoid public transportation because they are worried about becoming sick due to poor hygiene. Perhaps these people are concerned that crowded, enclosed, poorly ventilated public transportation systems provide a good environment for the transmission of pathogens from person to person. That doesn’t seem like such an unreasonable concern.
One heavily used public transportation system is the New York City subway system. Its subway cars and stations have never had a reputation for cleanliness. Indeed, when swabs from NYC subway turnstiles, exits, ticket kiosks, benches, handrails, doors, and seats were taken, researchers found hundreds of different species of bacteria. Most (57%) of these bacteria turned out to be harmless, but 12% of species were known to cause human disease. These dangerous pathogens included Yersinia pestis (bubonic plague), Bacillus anthracis (anthrax), and methicillin-resistant Staphylococcus aureus (MRSA). Contamination of the NYC subway system with fecal matter was also suspected because of the detection of E. coli bacteria. The London and Boston subway systems also get poor marks for cleanliness, because potentially dangerous bacteria have been found in their systems too.
One particular bacterium (Staphylococcus), often found on the skin, has received a good deal of attention because this microbe can spread disease, and some strains are resistant to antibiotics. For example, MRSA infections are difficult to treat and can cause life-threatening symptoms. MRSA has been found inside public buses in several cities, and researchers in Portland, Oregon, discovered six different strains of Staphylococcus in public buses and trains. The highest concentrations of Staphylococcus bacteria were found on bus and train floors (97.1 colonies/sample) and cloth seats (80.1 colonies/sample). Handrails (9.5 colonies/sample), seats and armrests at bus stops (8.6 colonies/sample), undersides of seats (3.8 colonies/sample), windows (2.2 colonies/sample), and vinyl seats (1.8 colonies/sample) had significantly fewer bacterial colonies by comparison. Although some of the bacteria were resistant to the antibiotics penicillin and ampicillin, the good news is that none of the bacteria were identified as MRSA. The bad news is that the strains of bacteria that were found on the buses and trains can still cause human illness. Surface areas inside mass-transit vehicles are not the only places where Staphylococcus can be found. Air samples taken from public metro stations in Shanghai found Staphylococcus strains that were resistant to antibiotics.
Tuberculosis is another bug with the potential to be passed from traveler to traveler. Active tuberculosis can be spread through the air when an infected person coughs or sneezes. Infections caused by the tuberculosis bacterium can result in respiratory problems and spread to other organ systems such as the kidneys and brain. People who use public buses and trains have been shown to be at risk for contracting tuberculosis.
People who use public transportation are also at a greater risk of getting sick with an acute respiratory infection. In fact, people who use public buses or trams were six times more likely to get sick five days after using the bus or tram than people who did not use these vehicles. Interestingly, occasional riders were slightly more susceptible to getting an acute respiratory infection than riders who used buses or trams regularly. Regular riders may develop immunity to viruses that make others ill.
Bus, train, and subway rides are relatively brief. On the other hand, on plane trips, passengers can be in close proximity to each other for several hours. High-efficiency particulate air (HEPA) filters installed on airplanes help reduce bacteria, fungi, and large viruses in the air, but low cabin humidity may make people more susceptible to getting sick. Aircraft passengers are many times more likely to catch a cold than those who do not fly. For example, catching a cold is estimated to be 15 times more likely after taking a flight between San Francisco and Denver than after staying on the ground. In addition to the common cold, tuberculosis, SARS, influenza, measles, malaria, dengue, and food poisoning have been spread on commercial airlines.
The spread of in-flight pathogens may take place directly by person-to-person contact or indirectly by contact when an infected passenger contaminates surfaces by coughing, sneezing, or touching objects. Armrests, seats, seatbelt buckles, air vents, headrests, pillows, entertainment touchscreens, tray tables, blankets, magazines, and pillows are a few of the possible landing spots for airborne microbes. Airplane bathrooms can harbor large numbers of pathogens too.
Each of us sheds millions of bacteria into the air every hour, and we are exposed to an assortment of microbes every day, so it is impossible to avoid other peoples’ germs. Yet we usually stay healthy, and even places like the New York subway have not been responsible for any epidemics (yet). Our immune system usually does a good job combating pathogens we encounter in our daily lives. Nevertheless, there are still ways to improve the odds of staying healthy. At the top of this list is to wash your hands with soap and warm water after you get off a bus, train, or plane. While traveling, it is especially important to wash your hands before you eat any food, such as that delicious in-flight meal. If you can’t wash your hands with soap and water, wear gloves or use an alcohol-based hand sanitizer or antibacterial gel to clean your fingers and palms. You can also use some hand sanitizers to wipe down the surfaces (e.g., armrests, tray tables, screens, windows) near your seat, although you should be prepared for some strange looks from other passengers. After you find your seat, make sure that it is clean. If your seat is not clean, ask to change to another location. Similarly, if the person sitting next to you appears ill, try to move to another seat. Finally, when you get to your destination, change your clothes and put them in the wash, because some pathogens can hitch a ride on your clothing.
SUMMARY
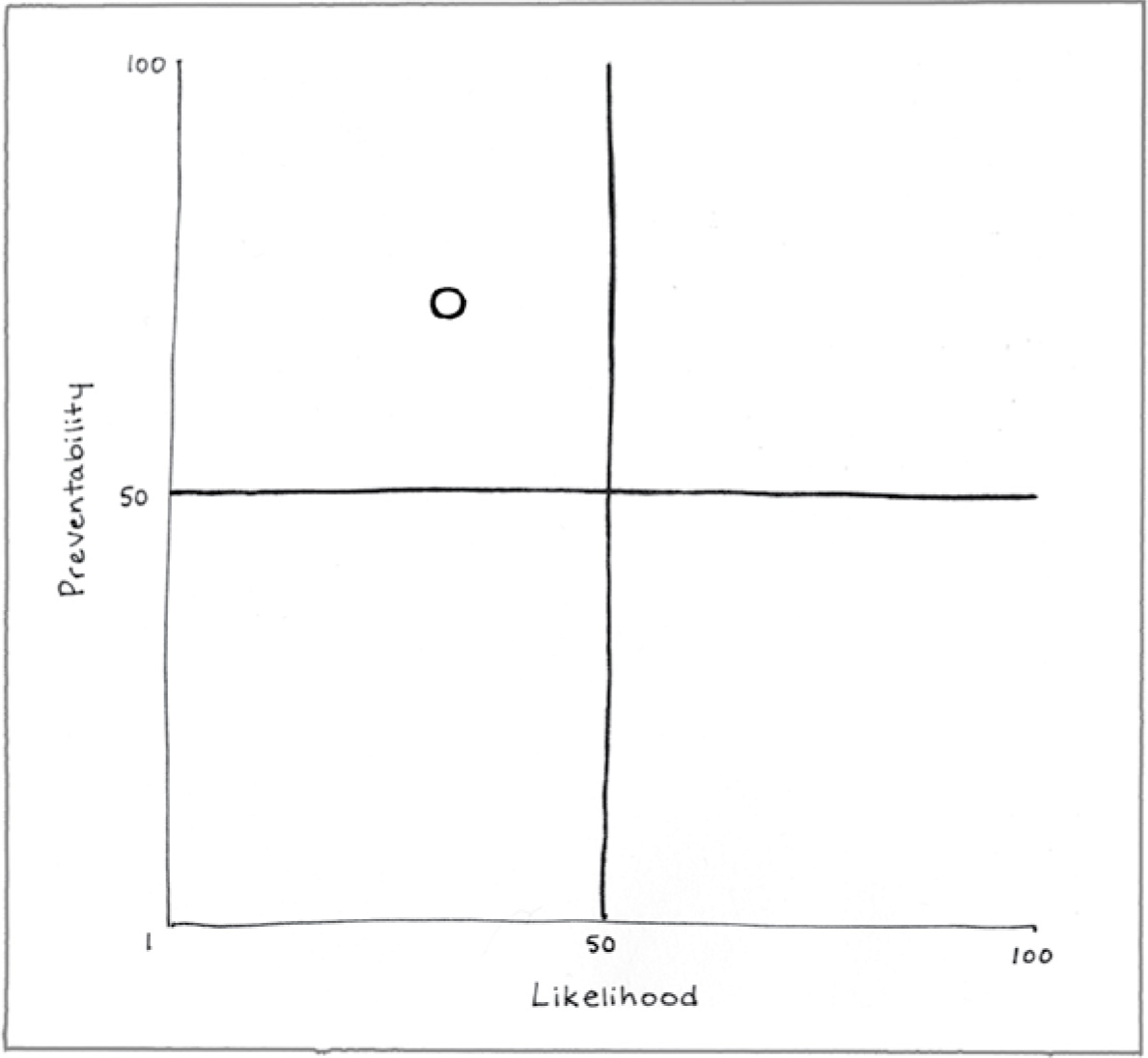
Preventability (76)
Many people rely on public transportation to get from place to place. Although riding on buses, trains, subways, and planes may be unavoidable, people can take steps to reduce their exposure to potentially dangerous microbes.
Likelihood (31)
People are not likely to encounter potentially dangerous pathogens on public transportation.
Consequence (26)
Most bacteria and viruses found on public transportation will not cause serious health problems.
REFERENCES
Afshinnekoo, E., Meydan, C., Chowdhury, S., Jaroudi, D., Boyer, C., Bernstein, N., . . . Mason, C. E. (2015). Geospatial resolution of human and bacterial diversity with city-scale metagenomics. Cell Systems, 1, 72–87.
Conceição, T., Diamantino, F., Coelho, C., de Lencastre, H., & Aires-de-Sousa, M. (2013). Contamination of public buses with MRSA in Lisbon, Portugal: A possible transmission route of major MRSA clones within the community. PLOS ONE, 8, e77812.
Edelson, P. J., & Phypers, M. (2011). TB transmission on public transportation: A review of published studies and recommendations for contact tracing. Travel Medicine and Infectious Disease, 9, 27–31.
Groth, M. (2016). Joining forces for progress. Hygiene Matters. Report 1016/17. Retrieved from http://reports.essity.com/2016-17/hygiene-matters-report/servicepages/downloads.html
Hocking, M., & Foster, H. D. (2004). Common cold transmission in commercial aircraft: Industry and passenger implications. Journal of Environmental Health Research, 3, 7–12.
Hsu, T., Joice, R., Vallarino, J., Abu-Ali, G., Hartmann, E. M., Shafquat, A., . . . Huttenhower, C. (2016). Urban transit system microbial communities differ by surface type and interaction with humans and the environment. mSystems, 1, e00018-16.
Lutz, J. K., van Balen, J., Crawford, J. M., Wilkins, J. R., Lee, J., Nava-Hoet, R. C., & Hoet, A. E. (2014). Methicillin-resistant Staphylococcus aureus in public transportation vehicles (buses): Another piece to the epidemiologic puzzle. American Journal of Infection Control, 42, 1285–1290.
Mangili, A., & Gendreau, M. A. (2005). Transmission of infectious diseases during commercial air travel. Lancet, 365, 989–996.
Staveley Head. (2017). London under the microscope. Retrieved from http://www.staveleyhead.co.uk/assets/under-the-microscope/index.html
Troko, J., Myles, P., Gibson, J., Hashim, A., Enstone, J., Kingdon, S., . . . Van-Tam, J. N. (2011). Is public transport a risk factor for acute respiratory infection? BMC Infectious Disease, 11, 16.
Yeh, P. J., Simon, D. M., Millar, J. A., Alexander, H. F., & Franklin, D. (2012). A diversity of antibiotic-resistant Staphylococcus spp. in a Public Transportation System. Osong Public Health and Research Perspectives, 2(3), 202–209.
Zamudio, C., Krapp, F., Choi, H. W., Shah, L., Ciampi, A., Gotuzzo, E., . . . Brewer, T. F. (2015). Public transportation and tuberculosis transmission in a high incidence setting. PLOS ONE, 10, e0115230.
Zhou, F., & Wang, Y. (2013). Characteristics of antibiotic resistance of airborne Staphylococcus isolated from metro stations. International Journal of Environmental Research and Public Health, 10, 2412–2426.