
After Chapter 7.3, you will be able to:
In addition to knowing the psychological and sociological components of these diagnoses, the MCAT also expects you to know the biological basis of a few mental disorders. These disorders include schizophrenia, depression, Alzheimer’s disease, and Parkinson’s disease. Research into how to stop the progression of the biological component of these diseases is widespread and will also be something to stay apprised of as a medical student and a physician.
Schizophrenia is an area of active research, though some biological factors have been isolated. Most potential causes are genetic, but trauma at birth, especially hypoxemia (low oxygen concentrations in the blood), is also considered to be a risk factor. Other exposures may also play a role; excessive marijuana use in adolescence is associated with increased risk. There is significant data to indicate that schizophrenia is partially inherited. If a person has this disorder, the risk that his or her first-degree relatives will also have the disorder is ten times that of an unrelated person in the general population; this measurement controls for environmental effects.
Schizophrenia may be associated with structural changes in the brain, but more research is needed to determine their significance and prevalence within the affected population. Schizophrenia is highly associated with an excess of dopamine in the brain; many medications used to treat schizophrenia, such as neuroleptics, block dopamine receptors. The term neuroleptic (also referred to as antipsychotic) arises from the side effects of these medications, which tend to include sedation.
There are a host of markers associated with depression:
It has been found that both these neurotransmitters and their metabolites are decreased, meaning that their actual production is decreased (rather than production staying the same and their degradation increasing).
For bipolar disorders, there exists a different set of biological factors and genetic corollaries that contribute to the disease:
Alzheimer’s disease is a type of dementia characterized by gradual memory loss, disorientation to time and place, problems with abstract thought, and a tendency to misplace things. Later stages of the disease are associated with changes in mood or behavior, changes in personality, difficulty with procedural memory, poor judgment, and loss of initiative. Now, each of these symptoms alone doesn’t necessarily point to Alzheimer’s; however, when all or almost all of these symptoms are seen in one person, and especially when the symptoms end up inhibiting normal daily function, this points to Alzheimer’s disease. This disease is most common in patients older than 65, and women are at greater risk than men. Family history is a significant risk factor and, interestingly, there is a lower risk of developing disease with higher levels of education.
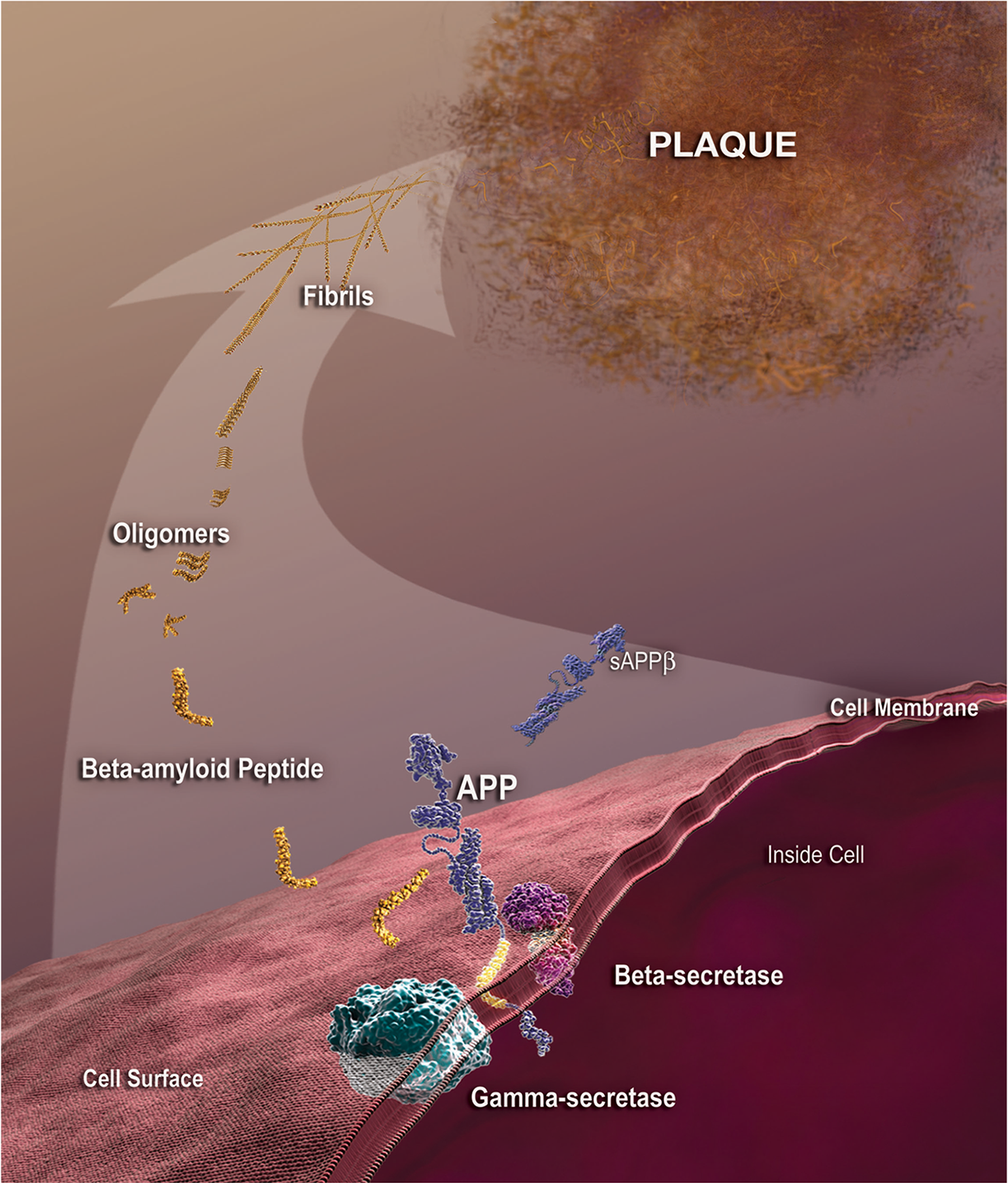
There is a genetic component to Alzheimer’s disease. Research shows that mutations in the presenilin genes on chromosomes 1 and 14 contribute to having the disease, and mutations in the apolipoprotein E gene on chromosome 19 can also alter the likelihood of acquiring the disease. Finally, the β-amyloid precursor protein gene on chromosome 21 is known to contribute to Alzheimer’s disease, explaining the much higher risk of Alzheimer’s in individuals with Down syndrome.
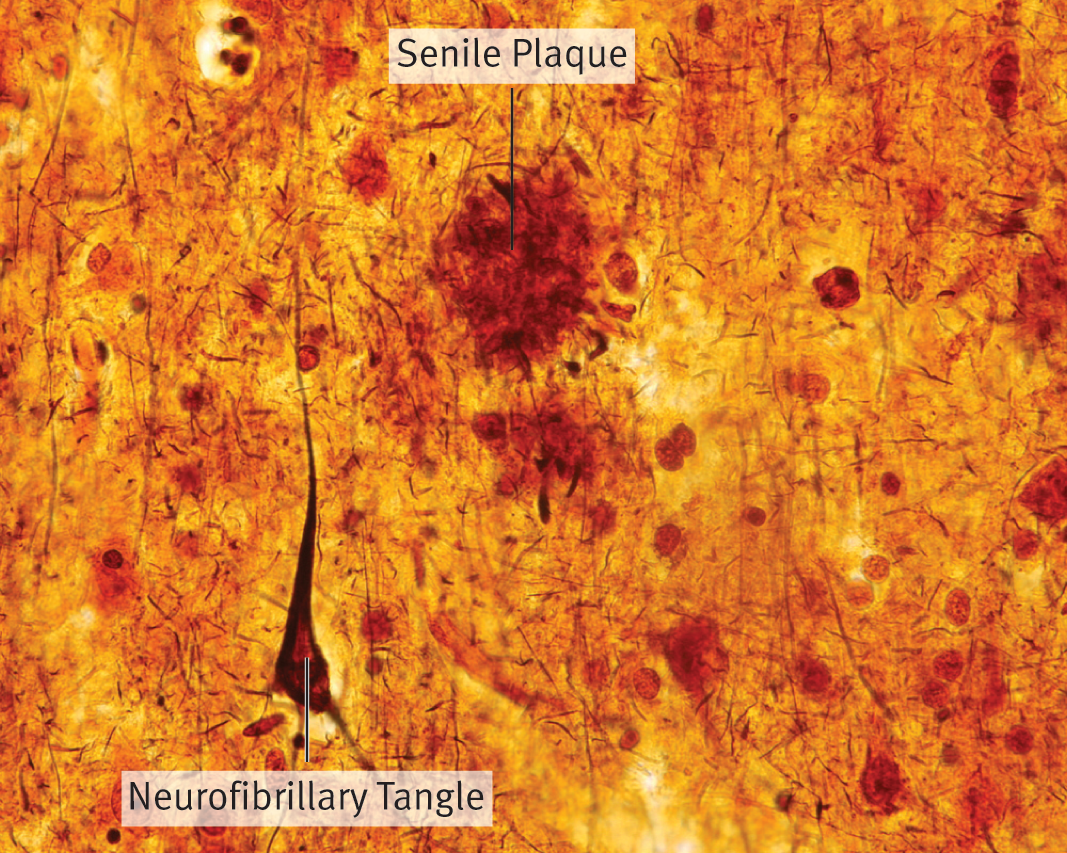
While the precise biological cause of Alzheimer’s disease is unknown, there are many biological markers that are found in patients with the disease. Don’t worry about understanding each of these markers in depth, but rather be able to recognize these factors if you see them on the MCAT:

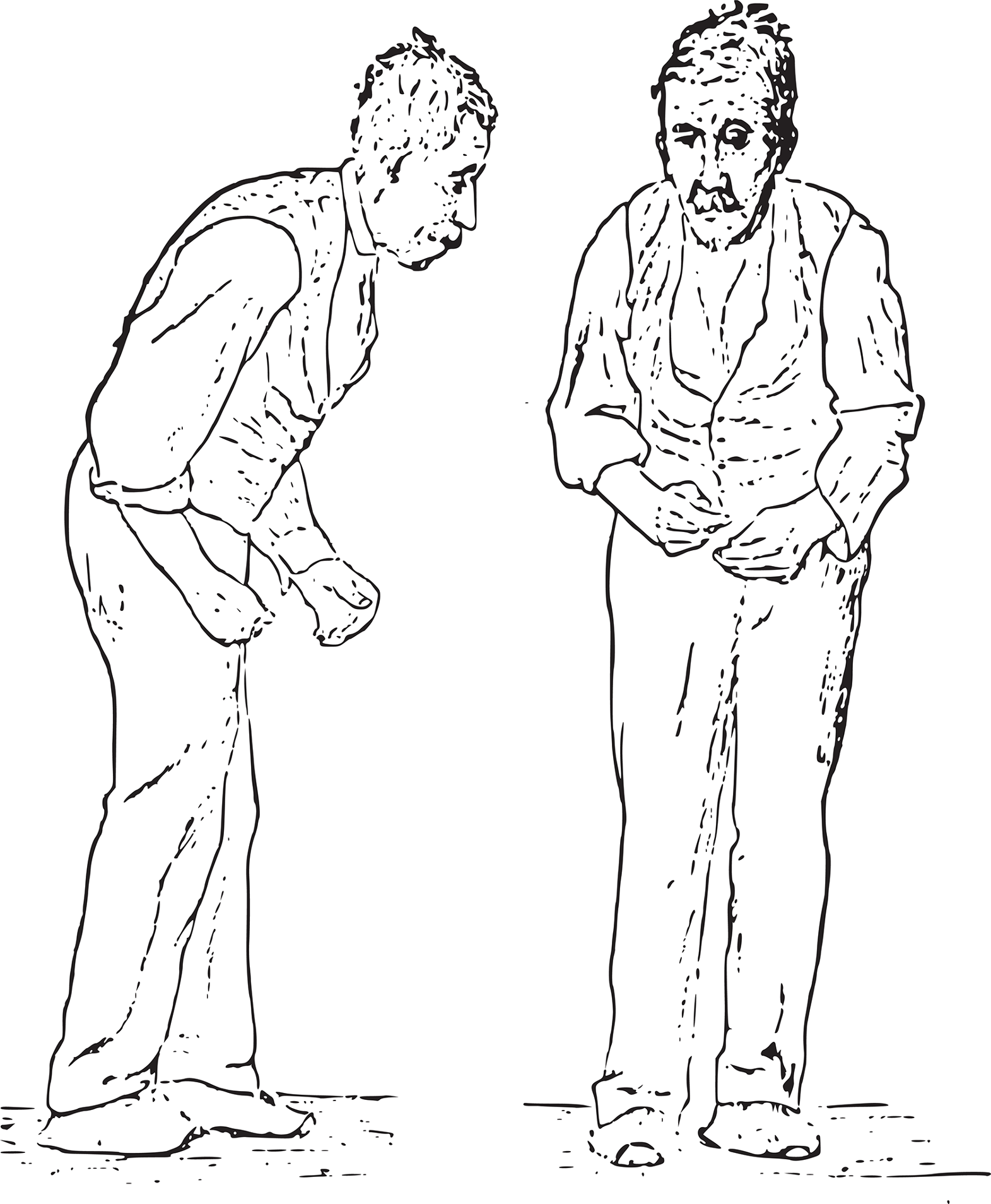
Parkinson’s disease, demonstrated in Figure 7.5, is characterized by bradykinesia (slowness in movement), resting tremor (a tremor that appears when muscles are not being used), pill-rolling tremor (flexing and extending the fingers while moving the thumb back and forth, as if rolling something in the fingers), masklike facies (a facial expression consisting of static and expressionless facial features, staring eyes, and a partially open mouth), cogwheel rigidity (muscle tension that intermittently halts movement as an examiner attempts to manipulate a limb), and a shuffling gait with stooped posture. A common but not characteristic symptom is depression. Dementia is also common in Parkinson’s disease.
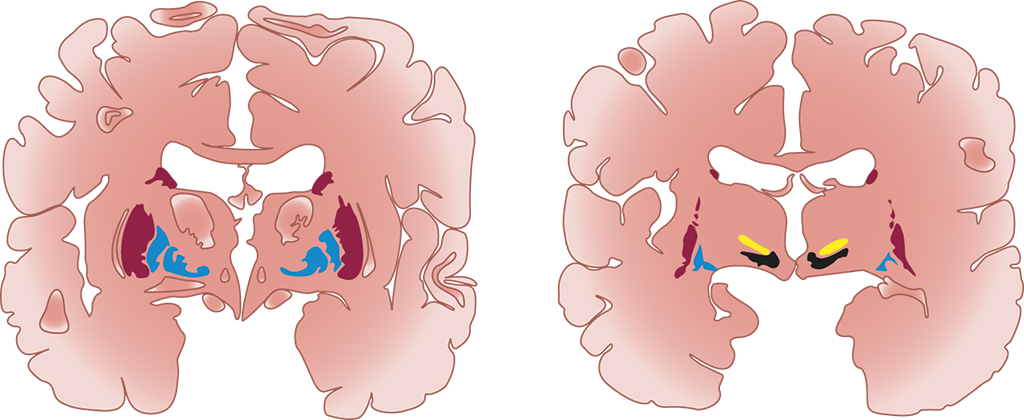
The biological basis of this disease is decreased dopamine production in the substantia nigra, a layer of cells in the brain that functions to produce dopamine to permit proper functioning of the basal ganglia, as shown in Figure 7.6. The basal ganglia are critical for initiating and terminating movements, as well as sustaining repetitive motor tasks and smoothening motions; thus, the symptoms of Parkinson’s disease flow logically from its underlying cause. This condition can be partially managed, therefore, with L-DOPA, a precursor that is converted to dopamine once in the brain, replacing that which is lost due to Parkinson’s disease. There have also been attempts to regenerate dopaminergic neurons in the substantia nigra using stem cells placed into the central nervous system. Similar stem cell-based therapies have been used in other contexts, such as after a spinal cord injury or stroke to attempt to regenerate function in the central nervous system, with limited results.
Note the connection between schizophrenia and psychosis (caused by an excess of dopamine) and Parkinson’s disease (caused by a deficit of dopamine). Antipsychotic medications often lead to “parkinsonian” side effects, like muscle rigidity and flattened affect. Medications used in Parkinson’s disease often lead to psychotic side effects, such as hallucinations and delusions.