The long, slow process of developing Type 2 diabetes can take years. The symptoms can develop so gradually that you don’t really notice them, at least not at first. In fact, many cases of diabetes are diagnosed only because the person went to the doctor for another ailment. Long before you might notice any symptoms of diabetes, your body may already be having trouble regulating your insulin and blood sugar levels.
UNDERSTANDING BLOOD SUGAR
We’ve already used the terms blood glucose and blood sugar a lot, and we’re going to use them a lot more in this book. Let’s take a closer look at glucose and how your body puts it to use. Glucose is a simple form of sugar that is one of your body’s primary fuels for energy; glucose is derived primarily from carbohydrates. (Fat is your body’s backup energy source.) Blood glucose,then,is the amount of sugar that’s in your bloodstream at any given time. That amount can vary quite a bit over the course of the day—it’s generally higher shortly after you eat something and lower between meals. Under normal circumstances, your body can also manufacture glucose from dietary protein so that your blood sugar level can be maintained.
Although the words blood glucose and blood sugar are often used interchangeably, glucose and sugar aren’t exactly the same thing. But because blood glucose and blood sugar are so commonly used to describe the same thing—the amount of glucose in your bloodstream—we’ll use the two terms interchangeably as well.
If your blood sugar mechanism is functioning normally and you eat a high-carbohydrate food such as a bowl of spaghetti, your body starts to break the starchy pasta down into glucose the moment it enters your mouth. (You can prove this to yourself by chewing a strand of plain cooked spaghetti and holding it in your mouth.As enzymes in your saliva start to break down the carbohydrate,you’ll notice a faintly sweet taste.) The carbohydrate continues to be broken down further in your digestive system, but some glucose enters your bloodstream almost immediately.
HOW IT SHOULD BE
As your blood sugar begins to rise, the pancreas releases enough insulin to handle it.The body likes to keep its glucose level within a fairly narrow range, so it quickly releases insulin to carry the glucose into your cells, where it can be converted into energy. If there’s more glucose than the cells can handle, the body can store the extra amount as glycogen in the liver and muscle cells for future energy needs.Once the glycogen storage areas are full, any glucose remaining is then stored as body fat.
Normally,after you eat a meal that contains protein,fat,and carbohydrates, you would expect that the glucose and insulin in your blood would first go up steadily within the proper range and then slowly go down again over the next several hours, without wide swings, which cause stress hormone release.
That’s how it should function. However, if you’re at risk for diabetes, your blood sugar and insulin balance can gradually start to get out of sync. It’s a slow process that happens in stages that almost imperceptibly merge into each other.
MILESTONES ON THE ROAD TO DIABETES
Though the progression to diabetes is slow and insidious, Dr. Atkins observed,through decades of evaluating patients with blood sugar abnormalities, that it can nonetheless be divided into six distinct stages. His observations are similar to those of other researchers in this area.1 The first four stages are milestones on the road to diabetes:
- Insulin resistance of cells
- Insulin resistance with hyperinsulinism (the production of large amounts of insulin)
- Insulin resistance with hyperinsulinism and reactive hypoglycemia (low blood sugar)
- Insulin resistance and hyperinsulinism with impaired glucose tolerance (now called prediabetes)
- Type 2 diabetes with insulin resistance and high insulin production
- Type 2 diabetes with low or virtually no insulin production
We’ll be discussing the six stages in more detail as we progress through this book, starting with the first three stages of insulin resistance as it gradually worsens and leads to excessive insulin production and hypoglycemia.
THE PROGRESSION OF INSULIN RESISTANCE
The first steps on the diabetes road usually begin with excessive consumption of carbohydrates (or a high-calorie diet) that leads to excess glucose being stored as fat. The result? Weight gain. As you put on the pounds, you gradually become insulin resistant—meaning your cells begin to be less responsive to the effects of insulin. Why? That’s a very good question,and despite its importance,it’s a question for which the medical profession still doesn’t have a good answer. (Today many researchers believe that one of the underlying causes is inflammation, but we’re just starting to understand what causes the inflammation.)2–4
As you gain fat, your insulin resistance increases. Though not everyone who is overweight is insulin resistant, the heavier you are, the more likely you are to become insulin resistant.On the other hand, in some people, insulin resistance begins at normal body weight and can worsen due to a high-carb diet even if their body weight stays normal. For these people, insulin resistance may be due to genetic factors or other factors not yet well understood. Fortunately, a controlled- carbohydrate lifestyle benefits just about everyone with insulin resistance, whether or not they are overweight. That’s because controlling carbs alone helps your cells regain their ability to respond properly to insulin, even if weight loss isn’t needed.5, 6
To compensate for insulin resistance, your pancreas pours out extra insulin in an attempt to force your cells to take in glucose and to maintain your blood sugar within the normal range. You now have what doctors call hyperinsulinemia or hyperinsulinism—meaning excess insulin in the blood. What happens then is that the smooth rise and fall of glucose and insulin in your bloodstream becomes unbalanced after a meal. To clear away the glucose, your pancreas produces a big spike of extra insulin.
As time goes on, your blood sugar and insulin production get increasingly out of sync. Your blood sugar rises, but now the insulin surge takes longer to occur, and when it does happen, you produce more insulin than is needed. When the insulin finally does kick in, your glucose then drops below its normal level, causing reactive hypoglycemia, or low blood sugar.
When hypoglycemia occurs,you may suffer from numerous symptoms, including ups and downs in energy level, shakiness, irritability, and even trouble thinking clearly.You’ll probably also feel cravings for your favorite carbs as your body instinctively tries to bring your blood sugar level back up—which puts you right back on the blood sugar roller coaster. A dramatic case of this among Dr. Atkins’ patients was Warren S.,a 35-year-old who came to him because blood sugar swings were causing panic attacks, dizziness, headaches, and an array of other unpleasant symptoms.Within two weeks of starting on the controlled- carb approach, he told Dr. Atkins, “I’m a different person.” And he was—his symptoms had improved almost immediately.
ONWARD TO PREDIABETES
The earliest three stages of the progression to diabetes can go on for months or even years before you move on to the next stage. After a while, however, even all that extra insulin can’t force enough glucose to enter your cells. The amount of sugar in your blood begins to peak at higher than the normal range. You now have reached the fourth stage: You have not only hyperinsulinemia but also hyperglycemia— elevated levels of blood sugar. What some people will then develop is what Dr.Atkins called a high-low curve.One to two hours after a high- carb meal, the blood sugar goes higher than it should, provoking symptoms such as sleepiness or a strong desire to nap. This is followed by the belated insulin spike, which causes hypoglycemia with the symptoms described above. This stage, in which the temporary elevation of blood sugar two hours after a glucose challenge during a glucose tolerance test goes above 140 mg/dL (milligrams per deciliter) but is still less than 200 mg/dL, is called impaired glucose tolerance. (We’ll explain more about how we measure blood sugar levels and what they mean in Chapter 6, Diagnosis: Diabetes.)
As the condition progresses, your fasting blood sugar (the amount of sugar in your blood after not eating for 8 to 12 hours) will slowly begin to rise. Once your fasting blood sugar hits a level of 100 mg/dL to 125 mg/dL, you have impaired fasting glucose, or prediabetes. Dr. Atkins observed that individuals with this condition could also have above-normal levels of blood sugar after eating a high-carbohydrate meal. Florence S. is a good example. At 61 years old and five feet three inches tall, she weighed 141 pounds. Florence had signs of metabolic syndrome and was taking a number of medications for high blood pressure and abnormal lipids. During her glucose tolerance test (GTT), her fasting blood sugar was 114, revealing prediabetes; at the half-hour point of the GTT, her blood sugar was 198; at one hour, 215; at two hours, 173; at three hours, 83; at four hours, 76; and at five hours, 89. As you’ll learn in a later chapter, this blood sugar pattern is the “high-low curve.”
If you have progressed to impaired glucose tolerance or if you have reached the point of impaired fasting glucose, you have what is called prediabetes. Now things are getting really serious—so serious that we’ll have to spend all of Chapter 5 discussing prediabetes and what it means for your health.
Unless action is taken to stop the underlying cycle of insulin resistance and hyperinsulinism, then the body’s compensatory mechanism of overproduction of insulin will continue. As your insulin resistance becomes more severe, your blood sugar levels become increasingly difficult to control and your pancreas becomes increasingly stressed. Without proper intervention, you’ll move from prediabetes to the next stage of full-blown Type 2 diabetes.
ARRIVING AT DIABETES
Stage 5 represents the early phase of true diabetes. In this stage, your fasting blood sugar is usually 126 mg/dL or higher, and your blood sugar after meals will consistently be even higher above the normal range. At this point, most people continue to have high levels of insulin production combined with severe insulin resistance.
Unless dramatic intervention occurs, the huge amounts of insulin your pancreas is forced to produce will eventually lead to a loss of pancreatic beta cell function.Indeed,you may lose so much beta cell function that your pancreas is making little or no insulin. By now, to survive,you will require the daily administration of insulin.When this happens, you have reached stage 6—insulin-dependent diabetes.
Oftimes, it is only when you have reached these last two stages that a diagnosis of Type 2 diabetes is finally made. Now the diagnosis is hard to miss. Your fasting blood sugar is in the diabetic range of 126 mg/dL or higher, and the classic symptoms of increased thirst, increased hunger, and increased urination occur. In some cases, unexplained weight loss and blurred vision also occur. By now, insulin resistance, hyperinsulinism, and hyperglycemia have been present for a long time, perhaps years, silently causing damage.
ARE YOU AN UNDIAGNOSED DIABETIC?
According to the American Diabetes Association, of the 18 million Americans with Type 2 diabetes, somewhere between 5 million and 8 million don’t know they have it. Here’s one reason that early diagnosis is so important: Retinopathy, blood vessel damage to the eyes, begins to develop at least seven years before clinical diagnosis of Type 2 diabetes is made based either on symptoms or standard blood tests.7, 8
Some undiagnosed diabetics will find out the hard way: when they end up in the emergency room with a heart attack, a stroke, kidney disease, or other vascular conditions. Others will learn the truth when they visit the doctor for something else and a routine blood test reveals their disease. Could you be one of them?
BLOOD SUGAR BY THE NUMBERS
According to the American Diabetes Association,the definitions of normal and impaired blood sugar are:
Normal Fasting Blood Sugar (FBS). Although there may be some variation among testing labs, normal FBS ranges from 65 to 99 mg/dL (milligrams per deciliter) after a fast of 8 to 12 hours. The measurement is accurate only if you haven’t eaten for at least 8 hours before your blood is drawn.
Impaired Fasting Glucose (IFG). A blood glucose level between 100 and 125 mg/dL (5.5 to 6.9 mmol/L [millimoles per liter]) after a fast of at least eight hours.If you have IFG,you have prediabetes. Impaired Glucose Tolerance (IGT). You have impaired glucose tolerance if two hours after eating a carbohydrate test meal your blood sugar has risen to above 140 mg/dL but stays below 200 mg/dL. If you have impaired glucose tolerance, you have prediabetes, whether or not you also have impaired fasting blood sugar.
Diabetes. Fasting blood sugar of 126 mg/dL or higher on two readings after fasting for at least eight hours indicates diabetes. An alternative measurement is a postprandial (after a meal) blood sugar of 200 mg/dL or higher two hours after a high-carbohydrate meal on two different days,or similar results at the two-hour point during an oral glucose tolerance test.9
Being diagnosed with high fasting blood sugar is like being told you’re a little bit pregnant—things will become more apparent very soon. That’s what happened with a patient named Donna G. Less than a year passed from the time her doctor told her she had high fasting blood sugar to the time she came to see Dr. Atkins to treat her full- blown Type 2 diabetes. If only she had started on the Atkins program when she was first diagnosed with high blood sugar, she might well never have gone on to that point. As it is, following the program has helped her quite a bit. Her fasting blood sugar over the past several years has always been steady at around 100 mg/dL.
Current medical guidelines say that if you have any of the risk factors for diabetes, your doctor should regularly check your fasting blood sugar level. But if you’ve been paying attention, you now know that by the time your fasting blood sugar is high, the damage has already started. (We’ll discuss tests to detect blood sugar abnormalities in Chapter 6, Diagnosis: Diabetes.)
The onward march toward diabetes and steadily worsening health might seem inevitable. Not so! At any point along the way it is possible to stop the progression. The sooner the better, of course, but even if you have reached stage 6 of diabetes, the Atkins Blood Sugar Control Program can help you manage the disease and help you to stave off some of its worst consequences.Please read on—that’s what the rest of this book is all about.
DO YOU HAVE A BLOOD SUGAR PROBLEM?
The effects of the blood sugar roller coaster on your health and well-being are fairly predictable. Compare your symptoms to the following list of the most common symptoms of abnormal blood sugar. Score each symptom according to how you experience it:
0 = never
1 = mild and/or rarely
2 = moderate and/or up to twice a week
3 = severe and/or more than twice a week
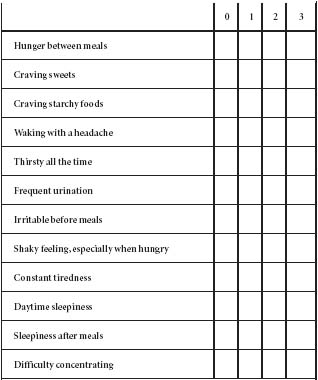
Add up each column and then multiply the sum by the number at the top of that column. Now add all the numbers together. Remember, all the answers in the 0 column = 0. If your score is 12 or more, you’re probably experiencing some blood sugar abnormalities. Please see your doctor to explore the issue further, especially if you also have any risk factors for diabetes.
A NEW PATH WITHOUT PILLS
After a 30-year hiatus, Ann McKay has returned to the very same program with which she initially experienced success. It is now helping her restore her health.
I’ve had a serious weight problem all my life. In fact, I did Atkins for the first time 32 years ago when Dr. Atkins’ original book, Dr.Atkins’Diet Revolution, was published. I am a registered nurse and, at the time, I was working on a surgical unit. Although I was doing well on Atkins—losing weight and feeling good—the surgeons I worked with were vehemently against it. They told me I was going to get sick and that it would ruin my kidneys.They were on me about it every day.Atkins was a brand-new concept at the time, and I thought, “Well, what if they’re right?” So I did go off the program after about 12 weeks. During the 30 years since then, I have been on every conceivable diet there is, never with any real success.
In 1996, I was placed on the drug Lupron and had a hysterectomy. From that point on, my weight problem only got worse. No mat ter how little I ate, no matter what diet I tried, I simply could not lose any weight.


NAME: Ann McKay
AGE:57
HEIGHT: 5 feet 0 inches
WEIGHT BEFORE:
247 pounds
WEIGHT NOW:
205 pounds
About two years ago, I found myself at a depressing 247 pounds—I’m only 5 feet tall—and wearing a size 26. I also discovered that my blood sugar level was going up—it was around 170 mg/dL. When I spoke to my primary-care doctor about it, he wanted me to go on a 1,500-calorie-a- day American Diabetes Association (ADA) diet. I told him, “Well, I’ve been on a 1,000-calorie diet pretty much my whole life, one way or another, and it hasn’t worked.”
I had even been hospitalized in the 1970s for my weight problem, where I was placed on a 700- to 800-calorie-a-day diet. I remember waiting for my eight o’clock snack of Tab soda and celery sticks. It was really sad. I was there for three and a half weeks and I gained 5 pounds.
All these years later, not wanting to be put on yet another low-calorie diet, I asked my doctor,“What about Atkins?”And he said,“Oh, I just lost 40 pounds on Atkins! But I don’t want you on it.” He was apparently concerned about my medical history—I’ve had some serious health problems. I don’t think he wanted to do the close monitoring that he thought would be necessary if I went on Atkins. So, he handed me the 1,500- calorie ADA diet and said, “Try this for two weeks and then come back and we’ll see what we’re going to start you on.” I knew what that meant: He was going to put me on diabetes medication.
When I got home, I was very upset. I knew I had the phone number for The Atkins Center somewhere in my house and began madly sifting through my papers to find it.When I called the number, a nurse answered the phone and I spilled my guts to her. “I just left my doctor’s office and I’m very angry and upset,” I said.“I know where’s he’s heading. He wants to put me on medication. Also, I’ve been seeing him for hypothyroidism, and I feel he’s not looking at it properly.All my hormone levels are normal but I know there’s something wrong with my thyroid. I was just wondering if Dr. Atkins still sees patients?” I was told he did. I breathed a sigh of relief. She faxed me a questionnaire that day, I filled it out and, three weeks later, I had my appointment. I did one day of lab work and then saw Dr. Atkins the very next day.
I liked Dr. Atkins right away. He reminded me of the old-time GP I had as a child. He was solid and confident.“You’ve got a complex medical situation here,” he said, “and it could have been straightened out years ago.” He asked me several questions, went through the eating plan with me, and told me I’d need to come to The Atkins Center once a month for follow-up. So for the next six months, I went every month—a big commitment when you have to drive three and a half hours to get there. Fortunately, my husband was willing to get up at six a.m. and drive with me each time.
When I first saw Dr. Atkins, my blood sugar level was 179, my cholesterol was 215, my triglycerides were 158, my HDL was 41 and my LDL was 142, and other lab results were also out of whack.As I’d suspected, my thyroid was not okay. Dr. Atkins took me off my medication and put me on natural alternatives. As of my last visit, my thyroid was normal, my cholesterol was down to 160, my blood sugar was within the normal range, and all of my other lab results had dropped from high-risk levels to within a normal range. My weight is 205 pounds—42 pounds less than I was—and I’m still losing about a quarter of a pound each week. I have lost 72 inches and am wearing a size 16 or 18. It’s a very slow process, but I have to look at the big picture. It’s not so much the change in my weight that matters, it’s the improvements in my blood sugar and my cholesterol. Recent labs measured a fasting blood sugar level of 96, cholesterol of 164, triglycerides of 72, HDL of 55, and LDL of 95. Dr. Atkins said that when I first came to him, I was three months away from a heart event.
Thanks to Atkins, I now exercise and can walk up and down the stairs of my house without becoming out of breath. Best of all, at age 57, I have a general, overall sense of well-being that I never had before. I also like what I see in the mirror. Recently, I was packing for a trip to Florida and I tried on a top that was a size 2X or something. I turned to my husband and said, “Look how big this is on me!” He smiled at me and said, “You just lit right up when you said that.” I’m going to save that top forever as a reminder to never go back to that size again.
Note: Your individual results may vary from those reported here.