3
ABDOMINOPELVIC ANATOMY
“Those who have dissected or inspected many [bodies] have at least learnt to doubt; while others who are ignorant of anatomy and do not take the trouble to attend it are in no doubt at all.”
GIOVANNI BATTISTA MORGAGNI DE SEDIBUS ET CAUSIS MORBORUM (1761)
DIGESTION & EXCRETION
The digestive and urinary systems constantly communicate to maintain a balance between absorbing nutrients and expelling waste. Both systems are regulated through input from the neuroendocrine system. The cardiovascular system is also linked on multiple levels with kidney and bowel function, and blood volume is tightly regulated by the kidneys, ensuring blood pressure is not too high or too low. The kidneys also work together with the respiratory system to make sure the concentration of blood is maintained within a tight range (not too acidic and not too alkaline). Each system on its own has a purpose: the digestive system to digest food and provide the body with nutrients, and the urinary system to remove toxins and fluids our body does not need. They rely on each other and their constant interplay keeps us well. Problems in one system can affect the other. If, for instance, the kidneys are malfunctioning, toxins arriving from the digestive system cannot be removed and recirculate through the body, leading to a buildup of toxins with subsequent harmful effects.
Our digestive journey
Our digestive tract extends from our mouth to our anus, connected by a series of interconnected tubes that are adapted for specialized functions along its course. Through this tract we take in food, break it down into molecules that can be used by the tissues and cells in our body, absorb nutrients we need, and get rid of waste. Several organs other than the gut partake in this process—the gallbladder, liver, salivary glands, and pancreas are all part of the digestive system. We take in food through our mouths, where our teeth grind it, our tongue manipulates it and moves it around our mouth, and saliva from three major salivary glands moisten this ingested material, all contributing to making it into a ball (bolus) that can slide down our throat (pharynx) into the food pipe (esophagus). Taste buds littered all over the surface of the tongue help us to quickly assess whether to enjoy the food or spit it out (if the taste suggests it may be harmful to us). Acceptable food is swallowed as the tongue pushes the bolus up against the hard palate and past the soft palate into the pharynx (throat), from where it is propelled downward by waves of contractions (peristalsis) via the esophagus into the stomach.
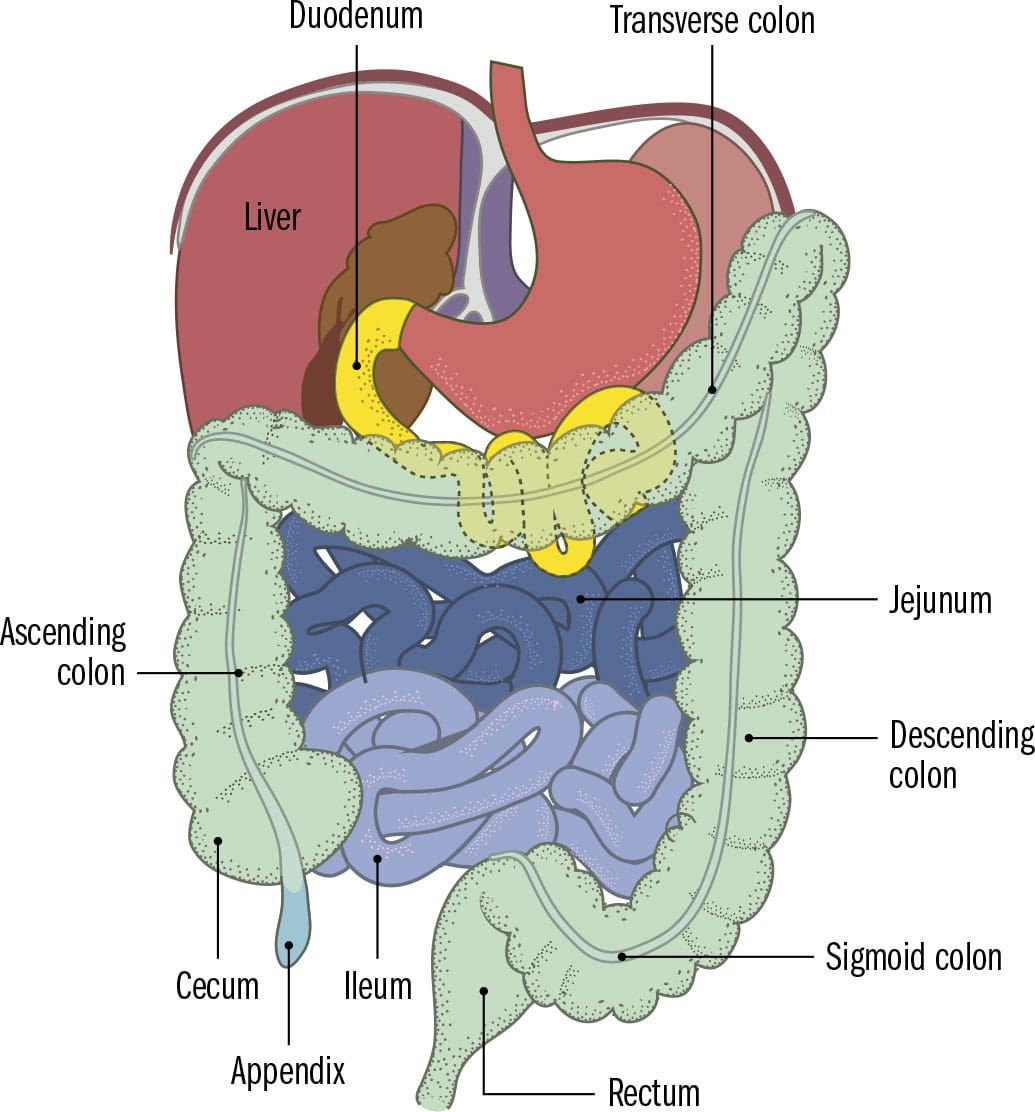
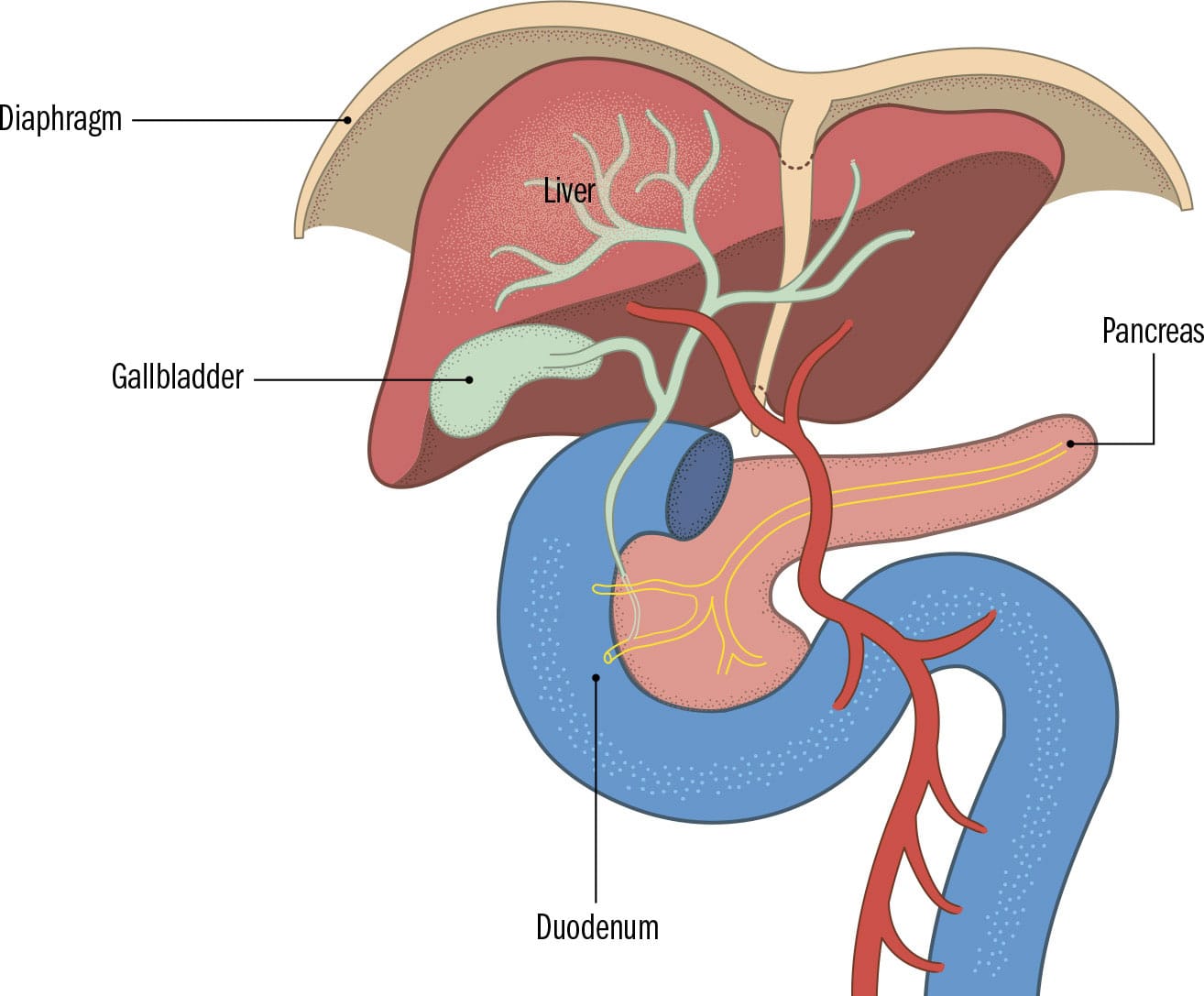
When food arrives in the stomach, it undergoes an “acid attack” to chemically break it down. It is also churned and then propelled into the start of the small intestine (duodenum). The duodenum is connected to the pancreas and liver by a series of tubes that bring in pancreatic enzymes and bile, all tailored to dissolve and digest carbohydrates, protein, fiber, and fat. The small intestine (duodenum, jejunum, and ileum) is coiled up in the middle of the abdomen and covered on its inner walls by tiny projections (microvilli). The microvilli increase the surface area of the small intestine for a very rich blood supply, and are connected to capillaries. It is through this interface that all digestible nutrients pass from the small intestine into the bloodstream and, from there, into the liver to be further processed. The majority of absorption happens in the small intestine, though alcohol (and some types of drugs) get partly absorbed from the stomach. Anything your intestines cannot break down (fiber, for instance), as well as bile and millions of bacteria, passes through the M-shaped large intestine and into the rectum for storage until they can be passed out.
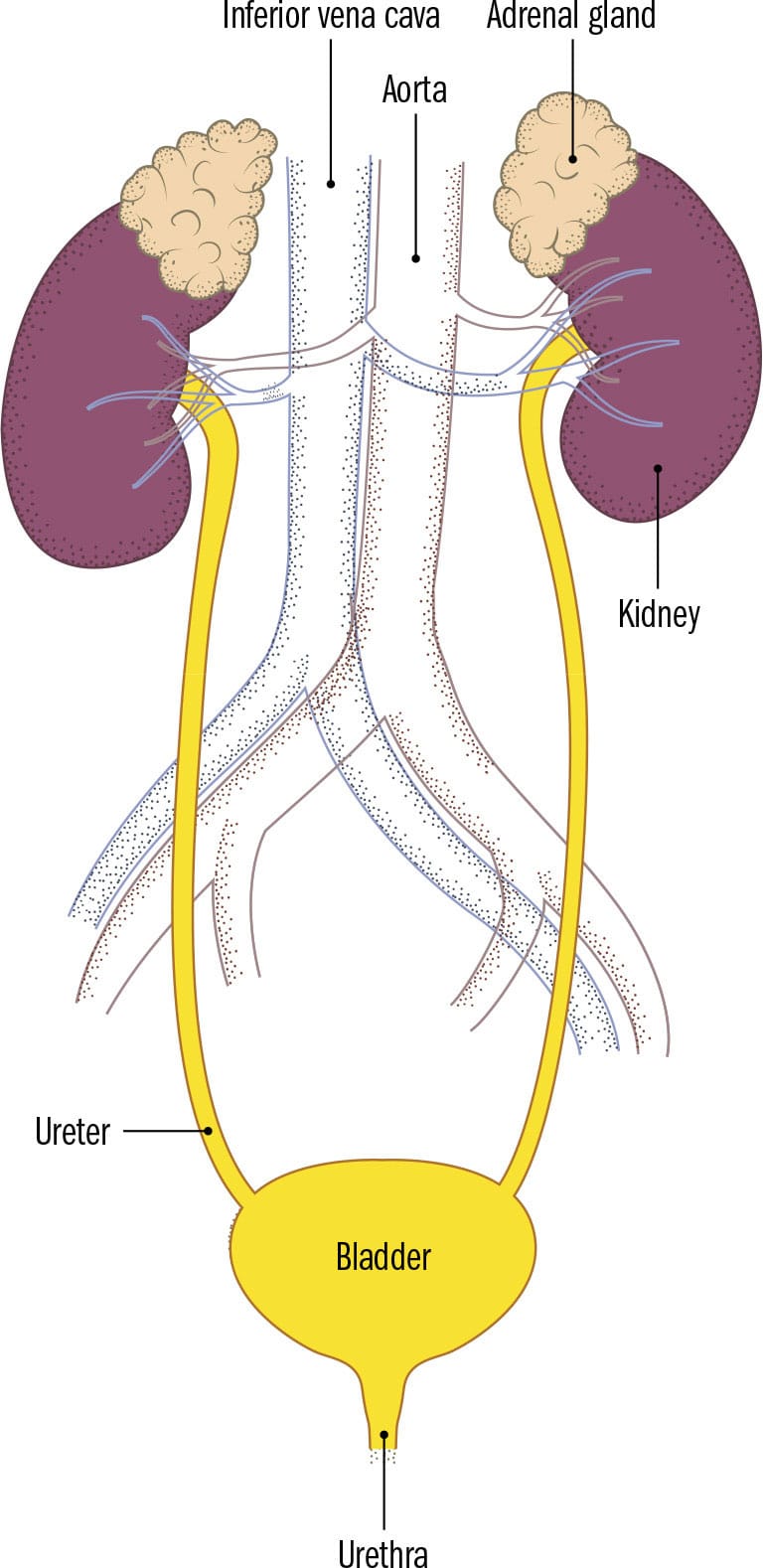
Journey from blood to urine
Our kidneys excete excess water and the end products of metabolism, which is essential to maintaining the correct concentration of substances within the body, and the correct water and electrolyte balance in tissue fluids. The nutrients from the watery mass in our small intestine make their way into our bloodstream (circulatory system) and from there into the liver via the portal system (all blood from the digestive system goes to the liver first for processing), and then via the circulatory system into the urinary system (kidney, ureters, bladder, and urethra). All blood passes through our kidneys, which sit high up on the back wall of the abdomen. The kidneys filter out waste products (particularly urea) from the blood as it passes through an intricate meshwork within them. The functional unit of the kidney is the nephron, and each kidney is composed of a million nephrons. Multiple sites along the course of a nephron reabsorb substances the body needs. Waste products and excess fluid are formed into urine. Urine then flows down ureters to the bladder, an expandible muscular bag that stores and then releases the urine through the urethra when it is full.
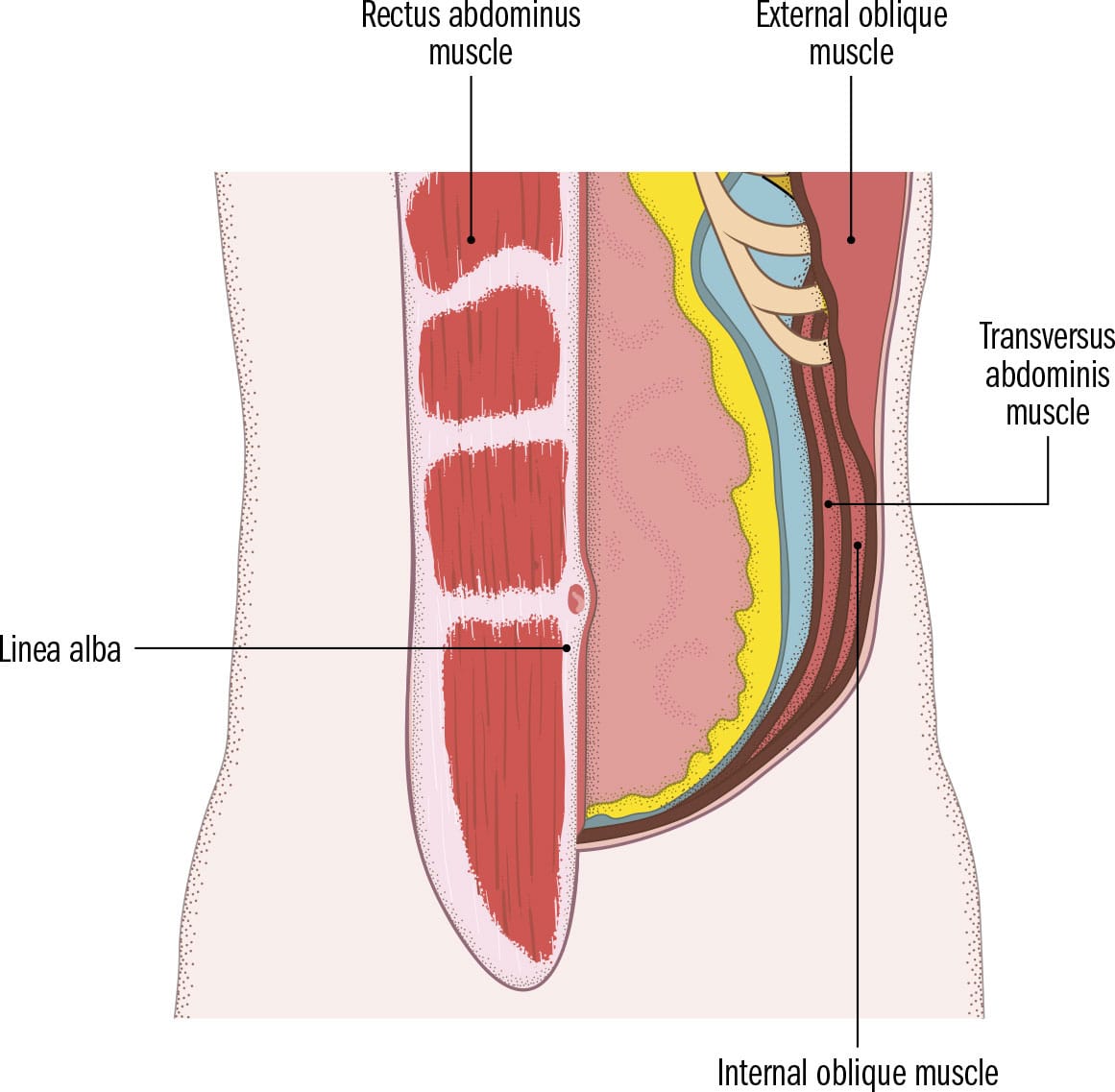
ANTEROLATERAL ABDOMINAL WALL
GROSS ANATOMY | Internal organs in the abdominal area have limited protection from the external world, as there is no underlying bony framework to shield them from damage at the front and the sides. Their protection is from a layered muscular wall, padded on the exterior by skin and fat and on the interior by sheets of thin membrane, the muscles of which can tense to form a rigid protective wall against any external onslaught. Three sheets of muscles—external oblique, internal oblique, and transversalis abdominis—emerge from the sides, and their fibers travel mainly in opposing directions, crisscrossing each other to provide strength to the wall. Their tendons flatten and merge just before they encounter two vertical strips of muscle on either side of the midline, the rectus abdominis or “six-pack” muscles in a toned abdomen. These thin sheets of muscles forming the anterolateral abdominal wall move the trunk, enabling twisting, sideways, and forward movement of the spine. They recoil passively when breathing out, pulling the ribcage down. The muscles help maintain posture and support the spine in the upright position when sitting or standing. Tensing them flattens the abdomen and raises the pressure inside the abdomen, allowing emptying of the bladder, defecation, vomiting, coughing, singing, childbirth, lifting heavy objects, and forcing air out of the lungs.
CLINICAL ANATOMY | The muscular abdominal wall is the access point for surgical procedures in the abdomen and pelvis; its anatomy is of great relevance to the surgeon aiming to avoid unnecessary blood loss and improve postoperative outcomes. Rapid access to the abdomen can be gained through a vertical incision in the midline, which is a virtually bloodless white line (linea alba) where the flattened tendons (aponeurosis) of the abdominal wall muscles meet below skin and fat. Incisions made a few inches parallel to the linea alba, and away from the midline rectus abdominis muscle, avoid damaging the muscles and the large blood vessels that run directly under it, and form an important anastomosis just below the umbilicus (bellybutton).
DISSECTION | Small, paired triangular abdominal wall muscles may overlie the lower end of the rectus abdominis muscles, although they vary in size, shape, and number. These pyramidalis muscles, when present, tense the midline of the abdominal wall, the linea alba, onto which they attach. It is still unclear what functional significance this has in humans.
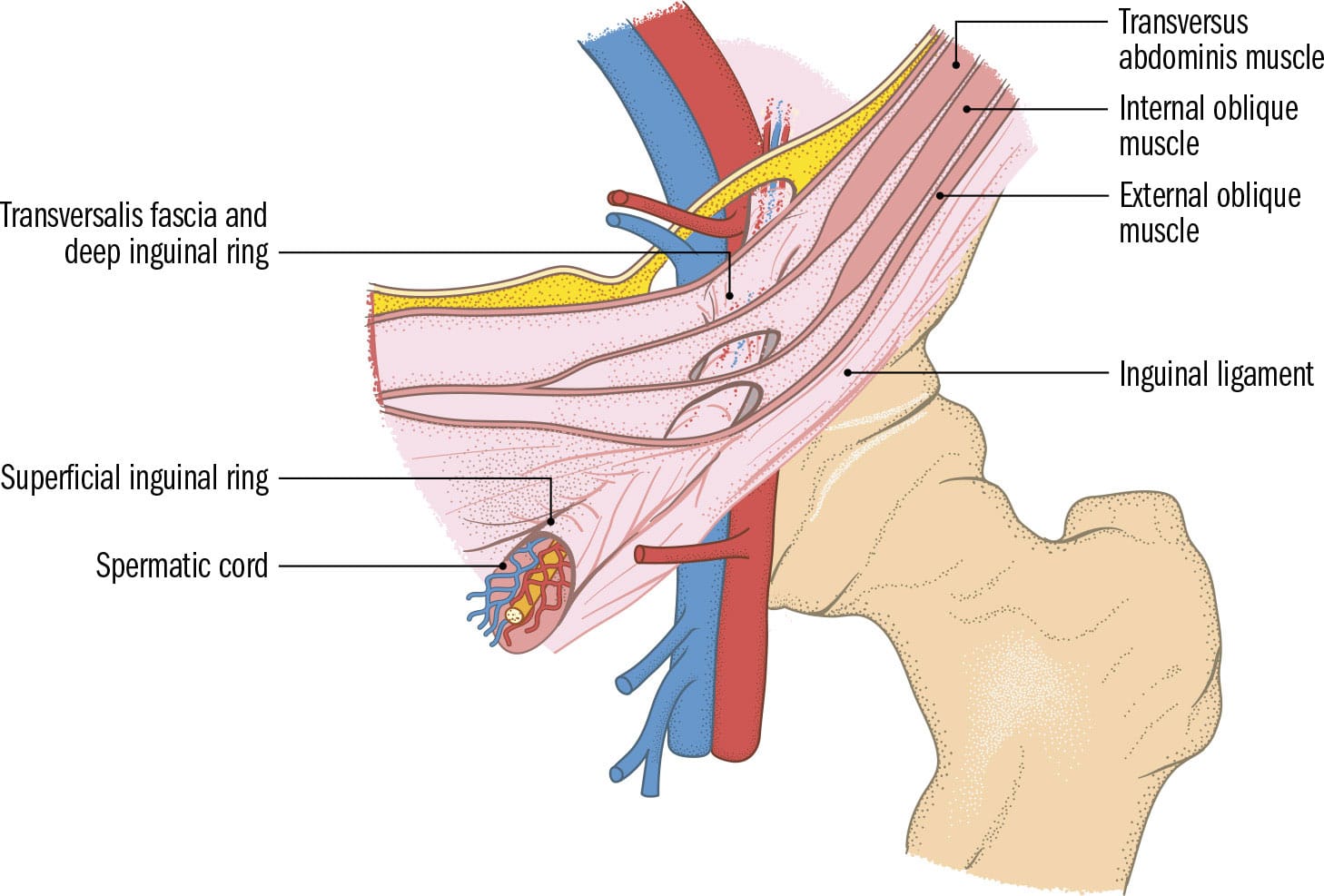
INGUINAL CANAL
GROSS ANATOMY | The transition zone where the trunk meets the thigh is an area known as the inguinal region. The lower part of the muscular anterolateral abdominal wall ends here, terminating in a ligament formed by tendinous folds of one of the broad flat muscles that comprises it. Overlying this inguinal ligament, on either side, is a 11/2 in. (4 cm) long cylindrical passageway tunneling through the layers of the abdominal wall. The inguinal canal allows structures to travel and communicate between the pelvis and outside the abdominal wall. Structures pass through the canal via small slit-like openings on the inside (deep inguinal ring) and outside (superficial inguinal ring) of the canal walls. The areas in front and behind these openings are reinforced to retain strength in the wall. In males, the spermatic cord carries numerous structures to and from the scrotum (sperm travels through the vas deferens from the scrotum into the urethra of the penis inside the pelvic region). In females, a ligament originating on the uterus (womb) runs into the inguinal canal and makes its way to the external genitalia, tethering the uterus to a position where it is facing forward.
CLINICAL ANATOMY | Even though both of the slits that form the entrance and exit to the inguinal canal are reinforced, they still represent a breach in the muscular wall that can widen as the wall weakens. Pressure on the wall from within can weaken the openings, and abdominal contents (intestines) can push through (hernia). Direct hernias push contents through the superficial ring closest to the midline in the groin area, while indirect hernias travel through the deep ring, along the inguinal canal and exit through the superficial ring. Usually, hernias can be pushed back but their contents can sometimes become trapped and their blood supply cut off.
DISSECTION | Inguinal stems from the Latin word “inguen,” the oblique depression between the abdomen and the thighs. To ancient Romans, inguen also signified one’s “privates” (sexual organs). The Middle English word “groin” (grynde) meant an abyss, hollow, or depression (in the ground). Crotch, used informally, is from Old French, meaning pitchfork or shepherd’s crook, i.e., the region where the body forks.
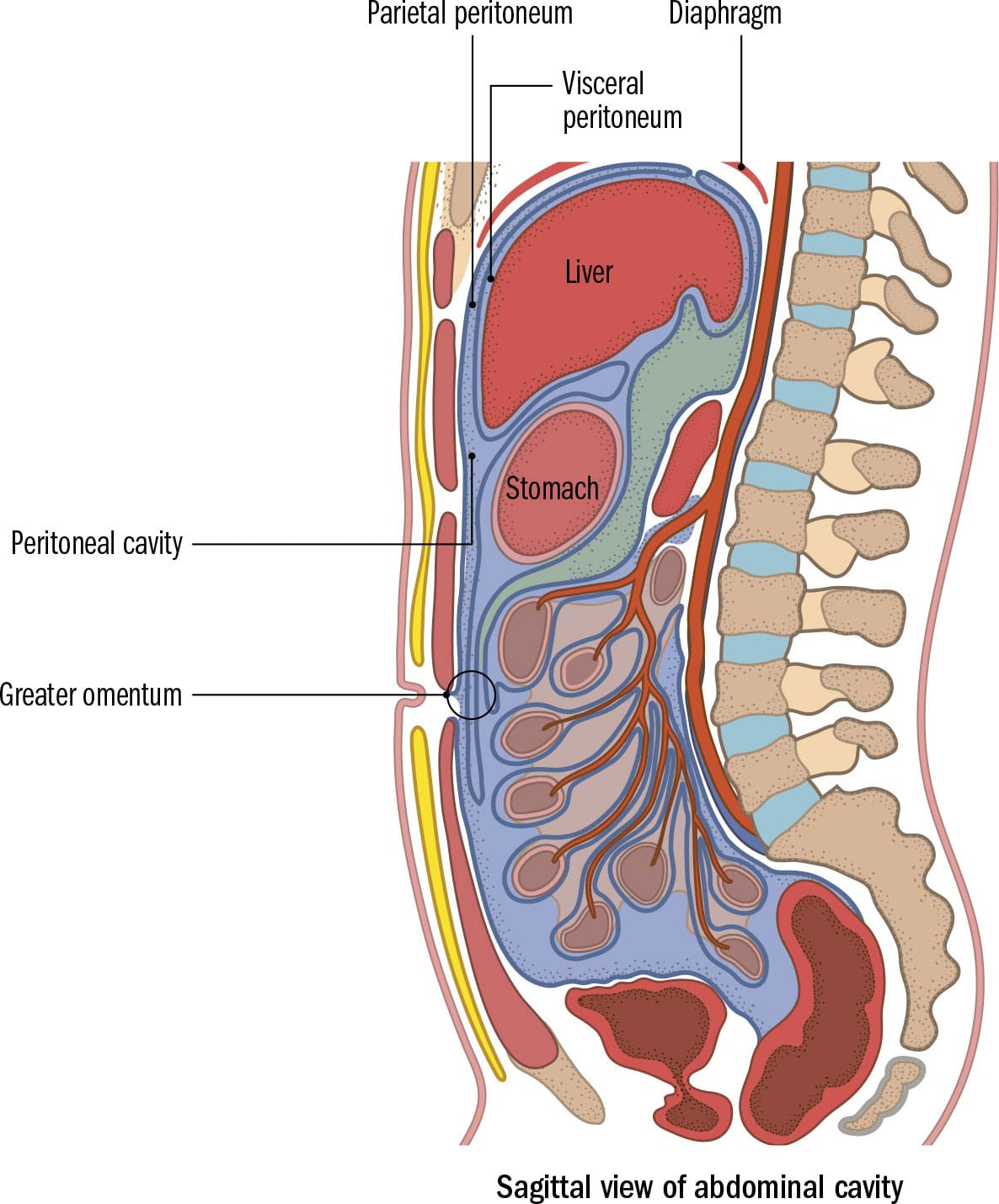
ABDOMINAL & PERITONEAL CAVITY
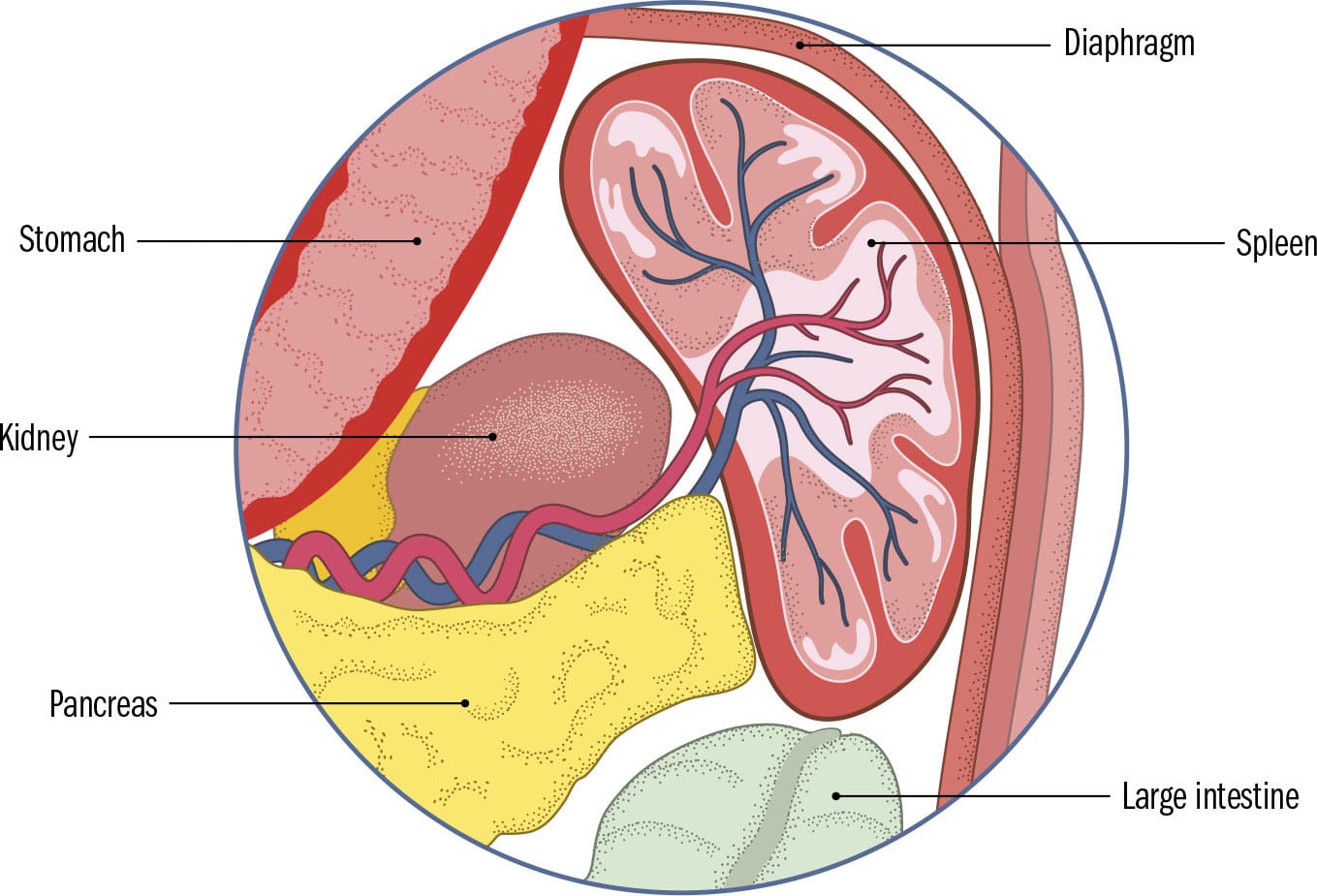
GROSS ANATOMY | The abdominal cavity is the largest hollow space within the body. It houses the liver, pancreas, kidneys, adrenal glands, the spleen, and the majority of the digestive tract. At the back, it is supported by the vertebral column, the lower part of the ribcage, the pelvic bone, and sturdy back muscles. The diaphragm separates it from the thoracic cavity above. Although there is no clear anatomical boundary between the abdominal cavity and the pelvis below, the pelvic contents are lined by a thin layer of membrane (peritoneum). Peritoneum surrounds most of the inside of the abdominal cavity (parietal peritoneum) and folds back on itself to cover every organ within (visceral peritoneum). A small amount of fluid lubricates the vacuum-like potential space between the two layers (peritoneal cavity), which stretches around the abdomen to envelop structures within. As the organs are packed together closely, the peritoneum provides a sliding surface that minimizes friction. It also holds organs in place and connects some organs with others. Two of its folds are of special relevance: the four-layered greater omentum hangs off the stomach, like an apron, and the small bowel mesentery, which gathers the long sausage-like loops of small intestine together and attaches them to the back of the abdomen. Blood vessels, lymphatics, and nerve supply run within these folds.
CLINICAL ANATOMY | Inflammation of the peritoneal cavity occurs when bacteria enter the sterile potential space, commonly from a rupture in the wall of the intestines or appendix. In life, intestines are filled with bacteria. The resulting widespread inflammation of the peritoneal cavity (peritonitis) is a surgical emergency. It requires immediate treatment with antibiotics and, if necessary, repairing the rupture. Peritoneal folds connecting structures contain blood vessels. Those running inside the edge of a fold known as the lesser omentum (between the stomach and liver) can be accessed if there is a liver bleed during an operation. In a procedure known as the Pringle maneuver, the fold is tightly squeezed for a short period to tackle the source of the blood loss.
DISSECTION | Dangling down like a fatty apron to cover the front of the internal organs, and known as the “policeman of the abdomen,” the highly mobile greater omentum can migrate and wrap around damaged or infected organs, containing infection and preventing spread. It provides an excellent place to store fat. Men are particularly susceptible to storage here (known as visceral fat), as evidenced by pronounced “beer bellies.”
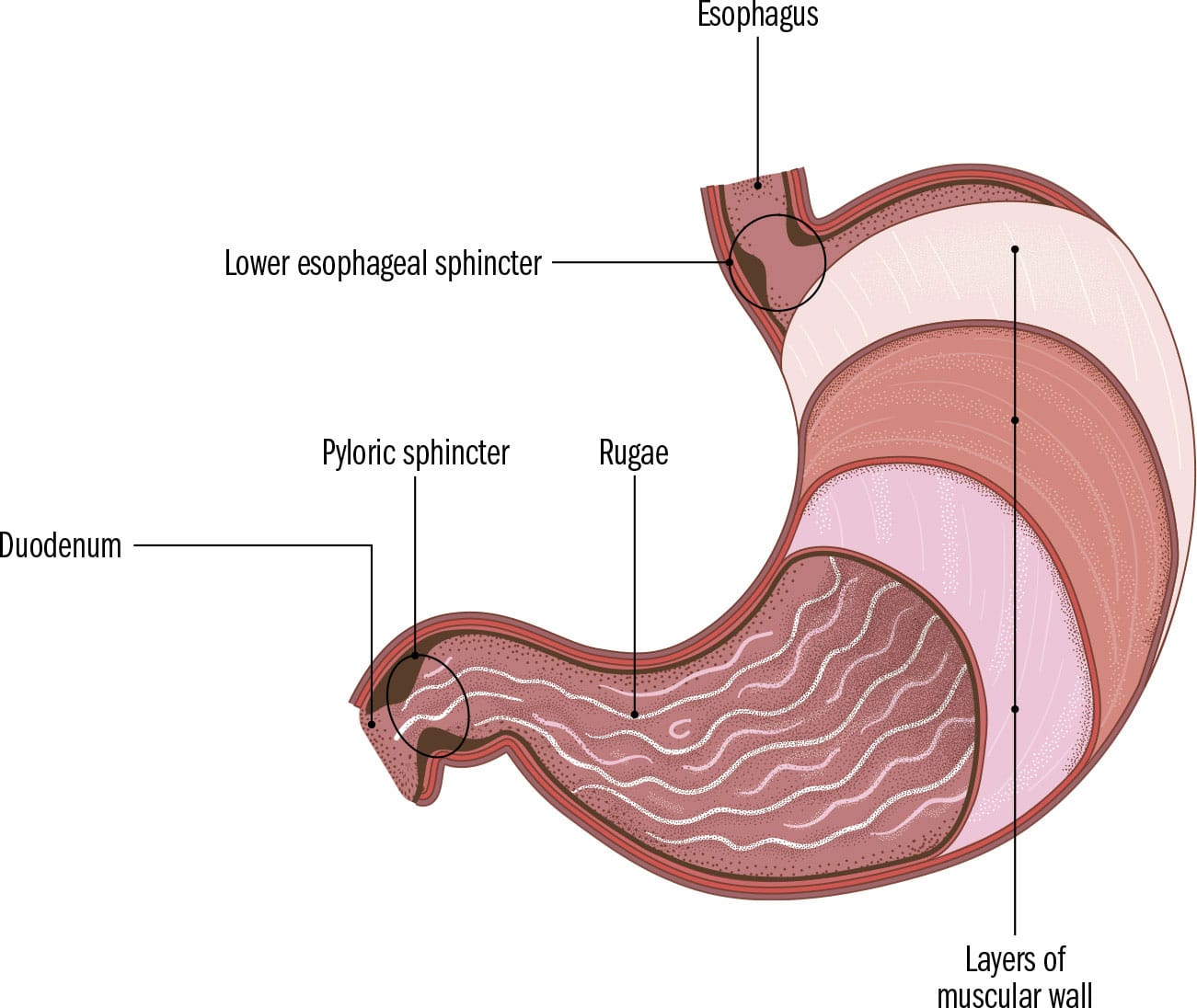
STOMACH
GROSS ANATOMY | The stomach is a somewhat J-shaped expandable muscular bag between the esophagus and the small intestine. Sat at the front of the upper left side of the abdominal cavity, it receives food from the esophagus. The process of digestion starts in the stomach. Food is exposed to a cocktail of powerful acids (hydrochloric acid) secreted from cells lining the main body of the stomach, and the contents are churned by the triple-layered muscular wall and then propelled into the small intestine. The stomach’s entrance (lower esophageal sphincter) and exit points (pyloric sphincter) are guarded by sphincters preventing back flow. They allow boluses of food to pass through at set intervals. Close to its exit point, the cells produce a more alkaline secretion, neutralizing the contents somewhat before they are emptied via the pylorus into the duodenum, the start of the small intestine. The inner lining of the stomach is folded into numerous wrinkles (rugae). As food fills the stomach, the wrinkles smooth out and the stomach expands. The shape, position, and size of the stomach varies greatly, depending often on whether it is empty or full. It tends to be elongated in tall and thin people but, in short and stout individuals, may lie high up and across the upper abdominal area.
CLINICAL ANATOMY | On an X-ray taken when a person is stood up, an air bubble (corresponding to gas in the stomach rising up to its highest point) is normally seen under the left side of the diaphragm. However, if even a small rupture occurs in the digestive tract, air (and bacteria-laden bowel contents) escapes into the sterile and vacuum-like peritoneal cavity. This is visible as a subtle line (air under the diaphragm) on an X-ray, requiring urgent surgical management. Stomach ulcers can sometimes erode through the muscular wall. If erosion occurs through the back wall, this can, very rarely, damage a large artery (splenic) behind it, leading to a catastrophic internal bleed.
DISSECTION | The pylorus has a thickened circular band of muscle that acts like the gatekeeper between the stomach and the small intestine. The Greek word means “band” or “anything that binds tight,” and was first used in the anatomical sense by the ancient anatomist, Galen. More than 60 sphincters are scattered around the human body, some minuscule and visible only under a microscope.
SMALL & LARGE INTESTINE
GROSS ANATOMY | Measuring about 23 feet (7 m) long, the three-part small intestine (duodenum, jejunum, and ileum) is the longest (though not the widest) section of the digestive tract. Its sausage-like coils are held together by peritoneal membrane, through which travels a wide network of blood vessels. Wavelike contractions (peristalsis) running through the entire digestive tract propel partly digested food from the stomach through the pyloric sphincter into the horseshoe-shaped duodenum, where pancreatic juices, bile, and sodium bicarbonate are added to the mix. These break down proteins, fat, and carbohydrates, and further neutralize the acidic contents. The majority of digested contents are taken up into the bloodstream through the lining of the small intestine, which is covered in microscopic finger-like velveteen protrusions which increase its surface area. These microvilli contain minute blood vessels (capillaries) that allow nutrients to enter the bloodstream. Food that cannot be digested passes through to the large intestine, where water is removed, hardening the contents to form feces. Peristaltic waves push fecal matter through the 5 ft (1.5 m) long colon (cecum and ascending, transverse, descending, sigmoid colon) and the rectum, from where it is excreted via the anus. The rectum and anus have sphincters that allow feces to pass through.
CLINICAL ANATOMY | The cecum is the pouch-like start of the large intestine into which the contents of the small intestine empty. Dangling from it, often behind it, is a wormlike 3–4 in. (8–10 cm) long hollow tube, commonly known as the appendix. While its function is still heavily debated, the appendix’s narrow opening into the cecum is prone to blockage (usually by hardened fecal matter); its mucous secretions cannot then be expelled and cause the organ to swell and enlarge. With its blood supply compromised, the tissue dies (necrosis). Filled with multiplying bacteria, a burst appendix can lead to these contents entering the sterile peritoneal cavity, causing severe infection (peritonitis).
DISSECTION | Around 15 minutes to an hour after eating or drinking, increased electrical activity from stretching of the stomach and small intestine triggers a physiological reflex known as the gastrocolic reflex. The resulting giant migrating contractions come in huge tidal waves, pushing contents out to make space quickly. This is experienced as the strong urge to defecate.
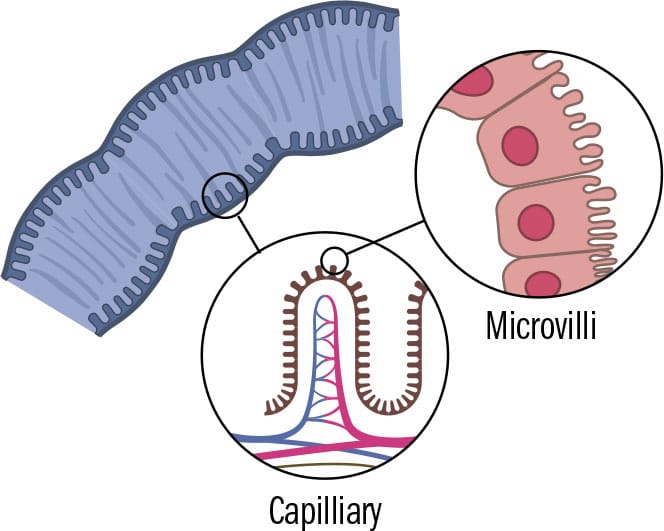
Small intestine under the microscope
LIVER, GALLBLADDER & PANCREAS
GROSS ANATOMY | The liver is the largest internal organ and fulfills numerous vital functions. A large vein (portal vein) carries nutrient-rich blood from the small intestine to the liver for processing. Specialized liver cells (hepatic cells) make up around 60 percent of liver tissue, converting most of the nutrients into forms the body can use. The liver converts and stores sugars, regulating blood sugar levels. It breaks down fats, produces cholesterol and detoxifies the body after drug and alcohol consumption. Importantly, it also produces blood-clotting factors that stop profuse bleeding after injury. A greenish-yellow, mildly acidic fluid (bile), which breaks down fats in the food, is produced by the liver but stored and concentrated (water is removed) in the gallbladder. The gallbladder is on the underside of the liver. Around a liter of bile is produced daily. Following a fatty meal, the gallbladder contracts and squeezes bile into the duodenum to break down the fat. The pear-shaped and light (only 23/4 oz /80 g) pancreas, sitting snugly in the C-shape of the duodenum and behind the stomach, is a gland that secretes digestive juices into the duodenum to break down carbohydrates, protein, and fats and neutralize stomach acid. It also secretes blood-sugar regulators, insulin, and glucagon directly into the blood.
CLINICAL ANATOMY | Yellow discoloration of eyes and skin (jaundice) indicates a damaged liver. It is caused by bilirubin, a yellow breakdown product of red blood cells, building up in the blood. Life is not possible without a liver. However, if part of it is removed, its tissue can regenerate over weeks. When insulin production in pancreatic cells is disrupted, high levels of sugar circulate in the blood, damaging vessels. Sugar cannot be taken up and stored in the liver. Without insulin replacement, this results in unquenchable thirst as sugar causes fluids to be removed from the body, as well as copious amounts of urine and a breakdown of fat and tissue. This is diabetes mellitus.
DISSECTION | Ancient Indian surgeon, Sushruta, (5th century BCE) observed ants gathering around the sickly sweet smelling and tasting urine of diabetics. It was only in the 17th century, in the Western world, that a doctor and neuroanatomist from Oxford, Thomas Willis, first coined the term “diabetes mellitus” from the Greek for “siphon” (a bent tube)—to pass through—and the Latin word meaning “honeyed.”
SPLEEN
GROSS ANATOMY | The soft and purple fist-shaped spleen sits in the upper left-hand corner of the abdominal cavity, wedged between the diaphragm and the stomach, and well-protected by the ribcage surrounding it. It is encased in a thick capsule. Weighing 51/4 oz. (150 g) in an average adult, the organ is very well supplied with blood and its mass is made up of two types of tissue that intermingle but have different functions. Red pulp acts as a blood filter, sifting out bacteria, viruses, and other debris. It also specializes in destroying tired red blood cells. The life span of a red blood cell is around 120 days, after which the spleen breaks it down and the breakdown products are transported elsewhere for recycling or removal. White pulp is like a massive lymph node, and produces lymphocytes, a type of white blood cell that helps fight off infection by initiating an immune response when a foreign substance (antigen) is encountered. As blood flows through the spleen, white blood cells remove foreign invaders, keeping blood clear of infectious agents. In the developing fetus the spleen produces red and white blood cells but loses this ability just before birth, after which the bone marrow takes over this task.
CLINICAL ANATOMY | Even though the spleen is well protected, in accidents its capsule can be damaged or the vessels supplying it can tear. Torrential blood loss may follow. While it is possible to live without a spleen, salvaging as much as possible is safest. A partly removed spleen may regenerate without any evident loss of function. A fairly normal life is still possible even if the spleen is completely removed, but problems may occur when the body encounters certain encapsulated bacteria and an overwhelming severe blood infection (sepsis) can follow. To prevent this, those who have had their spleen removed require a low dose of antibiotics for the rest of their life.
DISSECTION | The shape of the spleen ranges from a domed tetrahedron to a slightly curved wedge, determined by the structures pressing on it during fetal development. Its size and weight are determined by age and, partly, by the amount of blood within it. Curiously, when the spleen enlarges (for instance, as a consequence of infection or liver disease), it travels diagonally across the abdomen, past the belly-button, and may be felt in the lower-left hand corner.
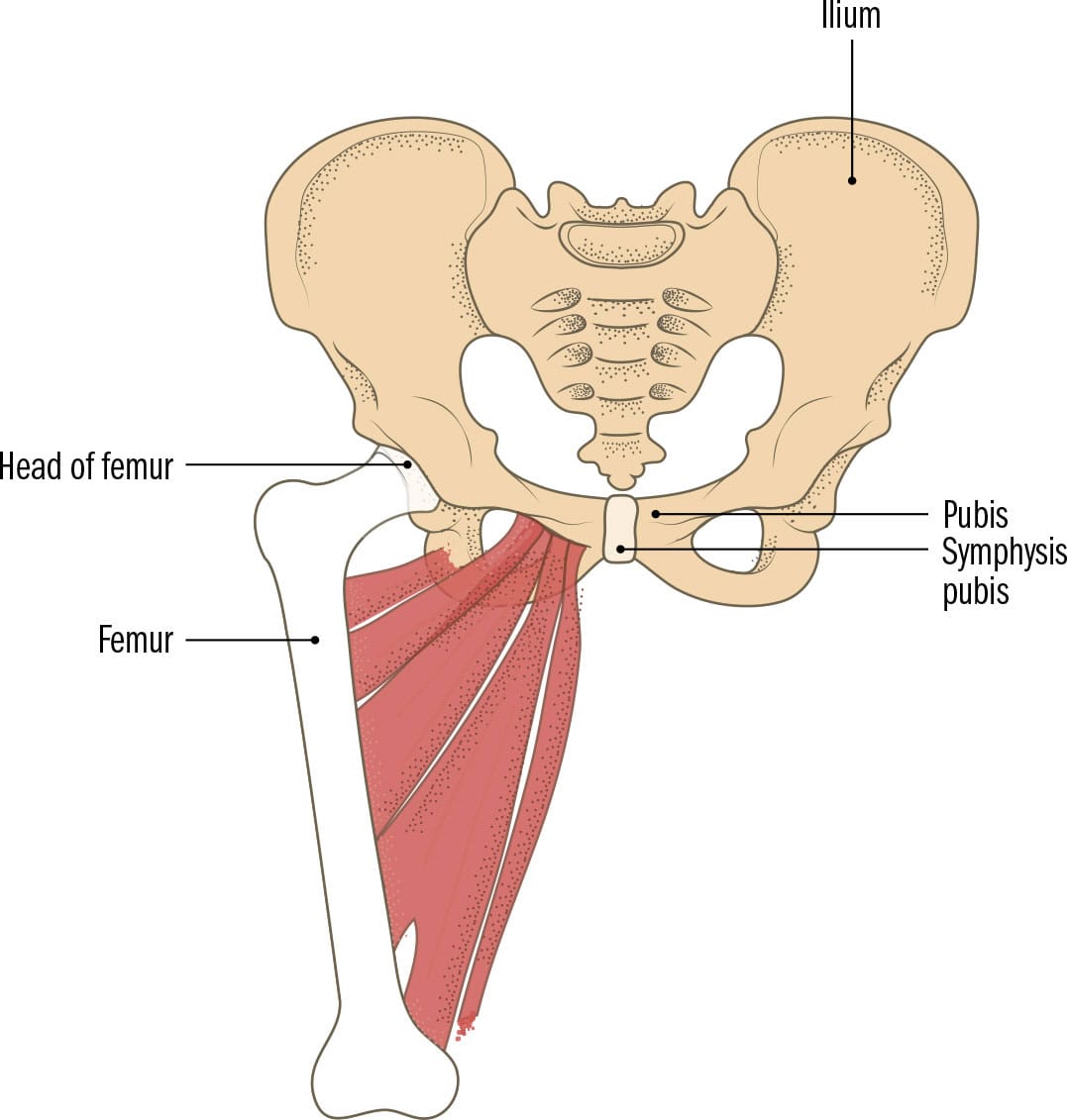
POSTERIOR ABDOMINAL WALL
GROSS ANATOMY | The posterior abdominal wall is not easily defined. It is the area at the back of the abdominal cavity that is not covered by the anterolateral abdominal wall. Behind it, and closer to the skin surface, are the back muscles covered by skin, fat, and fascia. The muscles forming this back wall move the lower limb or the spinal column and run inside the abdominal cavity. The bony pelvis and the vertebral column provide protection for the numerous organs overlying the muscles. The kidneys, adrenal glands, pancreas, duodenum, large intestine, ureters, nerves, and the aorta and inferior vena cava all reside in this tight space. These structures sit behind a double-layered membranous sac (peritoneal sac) enclosing the other abdominal organs. This is the retroperitoneal space (“retro” in this case meaning “behind”). The organs are sandwiched between the membranous sac in front of them and the muscular wall behind them. The region can be further divided into several spaces close to the kidneys and ureter based on layers of fascia splitting around these structures. Because the retroperitoneal space is so tightly packed, with little movement inside, small amounts of pus, blood, and fluid can be contained within them without spreading afar and causing widespread damage.
CLINICAL ANATOMY | The psoas major muscles (which bend the hip) originate from either side of the spinal column inside the abdomen, descend past the pelvis, and attach to the thigh bone (femur). The fascia covering them follows them into the upper thigh. Infections from the retroperitoneal area (or around the spine) that break through this fascial covering may track down with the muscle into the thigh, from where spread into large blood vessels can lead to widespread blood infection. Even large bleeds in the retroperitoneal region may go undetected. Bruising appearing in the flanks (between last rib and hip) may indicate severe inflammation of the pancreas or a bleed into the retroperitoneal area.
DISSECTION | Absent in around 40 percent of the population, a thin long slip of a muscle—psoas minor—overlies its chunky, muscular neighbor, the psoas major muscle. When present, it may assist in bending the trunk. Ancient Greek anatomists described each psoas muscle as being in the shape of a fox’s tail. This is particularly the case for the psoas major muscles.

URINARY SYSTEM
GROSS ANATOMY | Shaped like the beans that resemble them and bear their name are the two reddish-brown kidneys sitting high up at the back of the abdominal cavity overlying the posterior abdominal wall muscles. Well protected by the bottom of the ribcage and located on either side of the vertebral column, the kidneys are the start of the urinary system. They produce urine from waste products and excess water in the body, filter the blood, and help maintain stable blood pressure. They keep the delicate composition of blood at a constant, by monitoring and balancing water, pH, and salt levels. The bladder is an expandable hollow muscular reservoir sat behind the pelvic bone for storing urine. Urine is transported to the bladder via ureters, two long narrow tubes running in the retroperitoneal region. The bladder stretches as it fills up with urine and can hold around 10 fl. oz. (300 ml) quite comfortably. The signal to empty the bladder is conveyed in the need to urinate. This can become very painful if the bladder is not emptied. Urine leaves the body via the urethra, a tube of varying lengths in men (around 8 in/ 20 cm long with multiple bends) and women (around 11/2–2 in/4–5 cm) long, short, and very slightly curved). A sphincter keeps the junction between bladder and urethra closed until it is acceptable to urinate. The bladder then contracts, and urine is forced out through the urethral opening.
CLINICAL ANATOMY | The kidneys work nonstop to filter around 320 pt. (150 l) of blood every 24 hours. Every minute, 25 percent of circulating blood makes its way through them, producing more than 3 pt. (about 1.5 l) of urine per day. As efficient as they are, problems with the kidneys are difficult to detect in the early stages, and people can live without any clear symptoms for a long time. Just one functioning kidney is enough for survival. When around 90 percent of kidney function is lost, though, a dialysis machine (which replicates the blood-cleaning function of kidneys) is necessary for survival. If dialysis fails, organ donation is the only other option to ensure survival.
DISSECTION | The kidneys are thought to have several pacemaker sites in the smooth muscle cells of their walls. These trigger wave-like contractions (peristaltic waves) running through the ureters, making wriggly worm-like movements that push urine toward the bladder. Peristaltic waves continue even after partial removal of the kidney, allowing normal flow of urine out of the affected kidney.
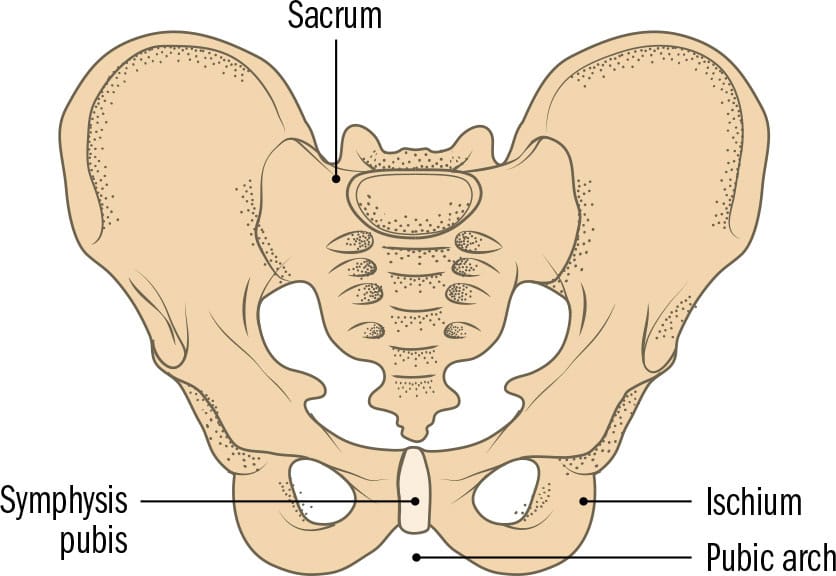
BONY PELVIS
GROSS ANATOMY | The bony pelvis is a ring of bones in the shape of a basin at the lower end of the trunk. It supports the weight of the body and cradles some reproductive and abdominal organs. It is formed by the fusion of paired hip bones (a further fusion of three smaller bones: ischium, ilium, and pubis) and the sacrum. These three smaller bones join together in puberty in a deep depression known as the acetabulum, forming a ball-and-socket joint with the head of the femur (thigh bone) that connects the hip with the thigh. The ilium fans upward in a wing-like expansion where one can easily rest one’s hands. The ischium is the bony protrusion on which one sits; strong hamstring muscles that move the thigh attach to it. The pubic bones fuse at the front via the symphysis pubis, a flexible cartilage bridge just in front of the bladder. The genitalia attach to an arch formed by the pubic bones (pubic arch). The greatest sex differences in the human skeleton are in the bony pelvis, as the female pelvis must accommodate a baby passing through during childbirth. To achieve this, the female pelvis is wider and shallower, with an oval-shaped rim where hip bones and sacrum meet, and a wider angle at the pubic arch. In a male, this pelvic brim is heart-shaped and narrower.
CLINICAL ANATOMY | Confusingly, hip fractures refer to breakages in the thigh bone and pelvic fractures to breakages in the ring of bones forming the hip bone. As bone in the aging body weakens and becomes more brittle, a simple fall may cause a pelvic fracture in the elderly. The pelvis is quite difficult to break, though. Serious fractures are mainly those that have occurred in a high-energy crash or a fall from a height. As these may cause huge invisible internal bleeds due to damage to the internal organs within, injured patients are always strapped in a pelvic binder to stabilize their pelvis and prevent further bleeding until a scan has given the all-clear.
DISSECTION | The Romans called the triangular large and heavy bone at the base of the spine (a fusion of five vertebra) os sacrum, Latin for “sacred bone.” In English, too, it was called “the holy bone.” The origins of “sacrum” are unclear and may stem from the ancient belief that this virtually indestructible bone, being very slow to decay, was where the soul resided.
Male pelvis
Female pelvis
PELVIS & PERINEUM
GROSS ANATOMY | The pelvic organs are separated from the abdominal organs only by a thin layer of membrane; the pelvic cavity and abdominal cavities are in essence just one large space (abdominopelvic cavity). The abdominal organs, however, sit on the wide wing-like bony protrusions above the rim formed by the hip bone and sacrum (false pelvis). The area below the pelvic brim is the true pelvis. It protects the bladder, rectum and, in females, the uterus (womb), uterine tubes, and ovaries. The pelvis is separated from the genital area (perineum) by a diaphragm-like levator ani muscle (a collection of several muscles known as the pelvic floor muscles) that holds up the pelvic organs and prevents them from protruding through the openings below. The pelvic floor and muscles regulating the opening and closing of the anus below are tethered to the perineal body in front of the anus. Maintaining good muscle tone in the pelvic floor ensures urinary and fecal continence. The perineal area below the pelvic floor contains the urethra, the vagina (in women), and the anal canal. Each has an opening in the groin. The external urethral meatus is at the front and the anus is at the back. In women, the vaginal orifice is between the two, for sexual intercourse and expelling a baby during childbirth.
CLINICAL ANATOMY | The pelvic floor muscles (levator ani) form a gutter shape where they unite in the midline. During childbirth, this shape guides the baby’s head into the correct orientation for exiting the uterus. These muscles stretch during pregnancy and childbirth, which can cause mild incontinence after childbirth. If the perineal body between the vagina and anus tears during a difficult labor, the results can be deeply disturbing for the woman, who may develop urinary and/or fecal incontinence. Laxity can also result in pelvic organs pushing through the pelvic floor into the perineum and genital area below. The resulting prolapse is extremely uncomfortable for the woman.
DISSECTION | The pudendal artery, vein, and nerve are all associated with the genital area, or the perineal area. A pudendal block, for instance, is used to numb the area around the vagina before a baby’s head passes through. The Latin word “pudens” means “to be ashamed,” suggesting that even in ancient times the private parts were considered something to be ashamed of and hidden away.
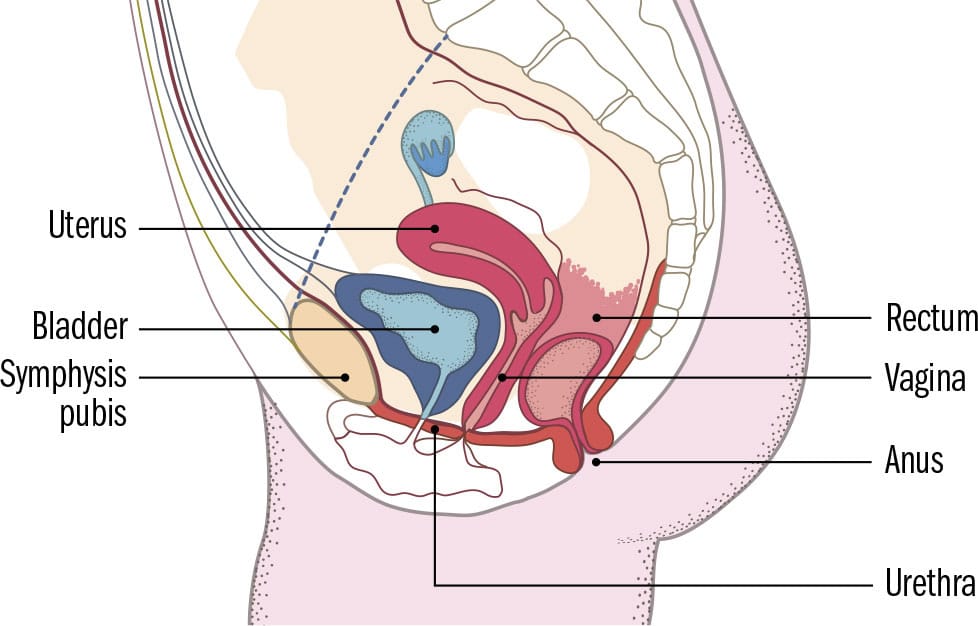
Sagittal view female pelvis
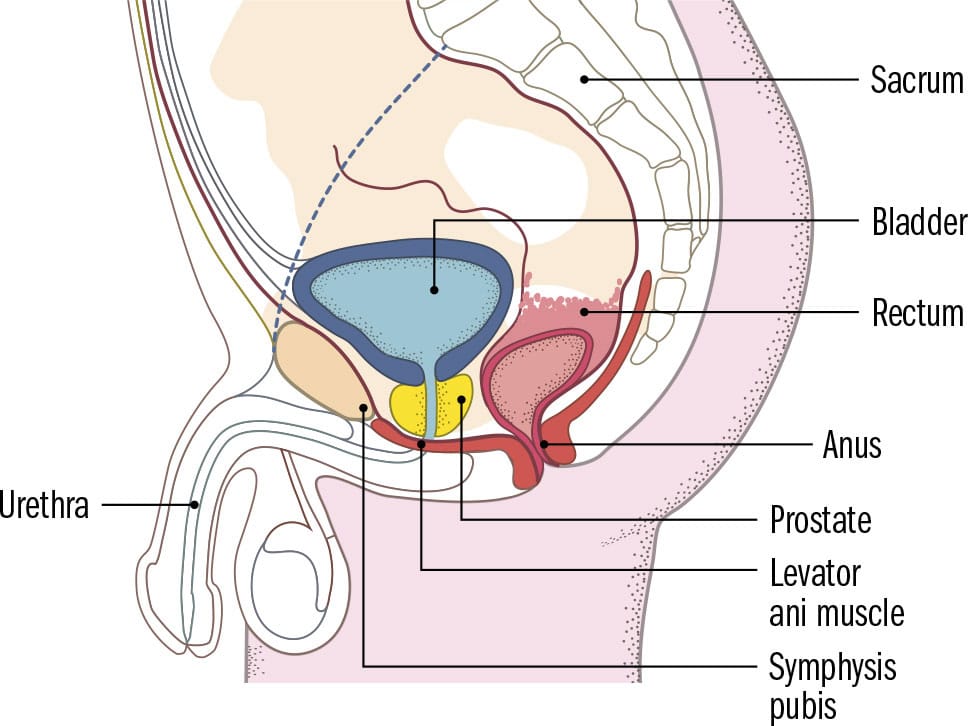
Sagittal view male pelvis
FEMALE REPRODUCTION
GROSS ANATOMY | The female reproductive tract has numerous functions. It secretes female sex hormones, produces and releases ova (plural of ovum, meaning “egg”), admits sperm and provides a safe place for implantation to take place and a haven for the growing baby until it is ready to be born. As a result, it has a complicated anatomical system with a feedback loop linking with the brain to maintain the delicate hormonal balance required for menstruation, pregnancy, and childbirth. It is composed of vagina, uterus, uterine tubes, and ovaries. The vagina is a thin-walled receptacle for the male penis. It leads into the uterus (womb), the entrance of which is a tight narrowing (the cervix). The uterus is thick-walled and muscular. It sits fully in the true pelvis (until pregnancy, when it expands into the abdominal region) and is held in place by numerous ligaments and a sheet of membrane overlying it (peritoneum). Fanning sideways and backward toward the ovaries are two funnel-shaped uterine tubes (commonly known as “Fallopian tubes”). Each month, when an ovum is released by the ovary, frond-like structures (fimbriae) at the end of the tubes lure it into the uterine tube to increase its chance of meeting a sperm and achieving impregnation. Breast development and the menstrual cycle are also controlled by the ovaries.
CLINICAL ANATOMY | The male and female gonads (testes and ovaries) originate on the back wall of the abdominal cavity, close to the aorta. The ovaries descend into the pelvis but remain within the peritoneal cavity. A small opening allows the ovum to enter the uterine tubes. Because of its existence in a different anatomical cavity, on very rare occasions sperm can travel through the opening, and impregnation and implantation can occur outside the safe environment of the uterus. This type of ectopic pregnancy (any pregnancy that implants outside the uterus is “ectopic”) can lead to rupture and severe internal bleeding, although there are some rare successful cases of abdominal pregnancies.
DISSECTION | Until the 19th century, it was thought that the uterus (Greek, hyster) could float around the body (almost with a mind of its own) causing typically female problems. The once respectable psychiatric diagnosis of “hysteria” was attributed to this ability of the womb to cause havoc by pressing on other structures. Smelling salts under the nose and vagina, as well as sneezing, were believed to return the “wandering womb” to its proper place.
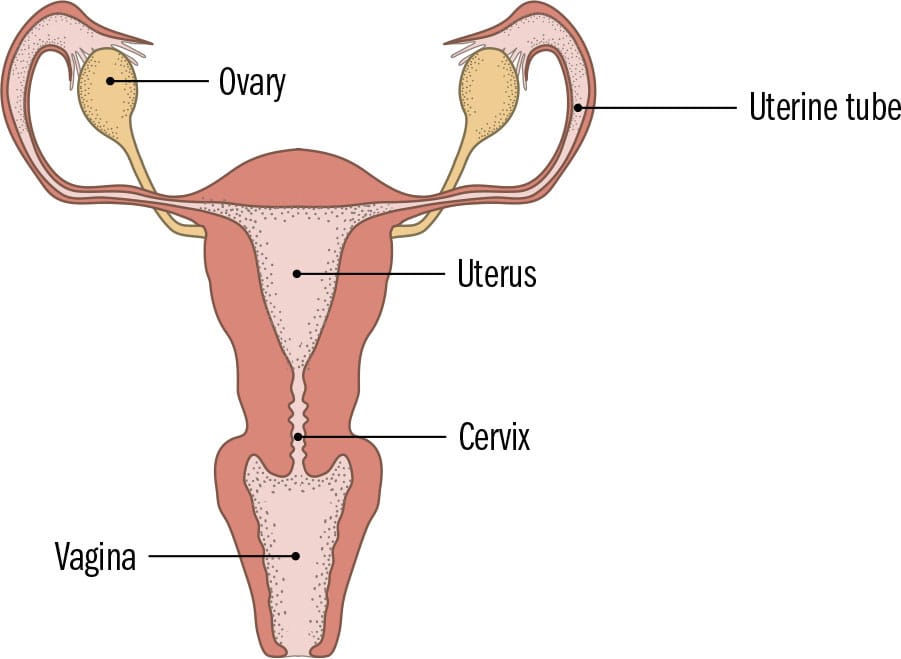
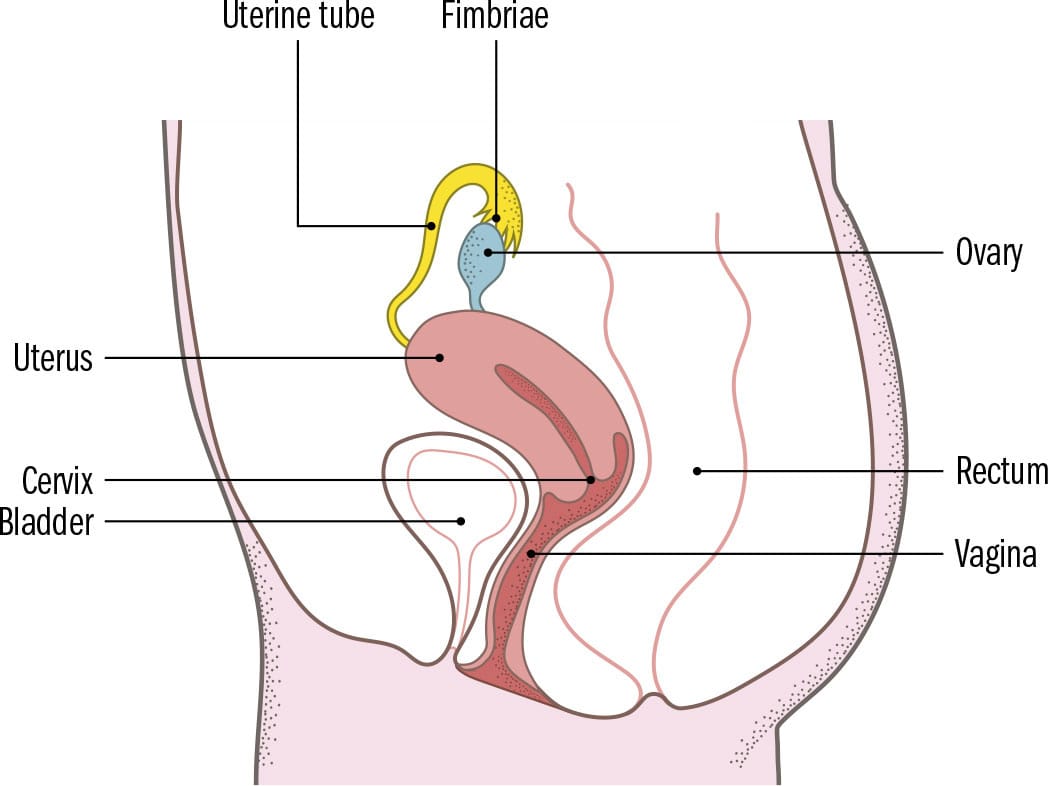
Sagittal view
MALE REPRODUCTION
GROSS ANATOMY | The male reproductive system lies below the bladder and between the legs. It consists of the plum-sized testes, an expandable sausage-like penis, the prostate gland, and seminal vesicles. Their combined function, after puberty, is to make and deliver sperm into the corresponding female reproductive system. The testes, lying in the scrotal sac on either side of the penis, produce sperm and male sex hormones. A long coiled tube (epididymis) attaches to each testis. It matures sperm passing through it on their way to the penis. The penis contains a very long urethra, the tube for expelling urine and semen. Covered by foreskin, a partly loose fold of tissue, it is very sensitive and made of spongy erectile tissue. During sexual arousal, the spongy tissue expands with blood, resulting in a rigid and enlarged penis (erection), whose role is to deliver sperm into a female vagina. Sperm are propelled out of the scrotum through the epididymis, along a duct (vas deferens) toward the penis. Fluids from the prostate gland and the seminal vesicles mix and dilute sperm, producing semen. This sticky, milky-white substance allows sperm to survive in the acidic female reproductive tract. Tiny bulbourethral glands secrete a lubricant into the urethra when a man becomes sexually aroused.
CLINICAL ANATOMY | Due to the long course the spermatic cord has to travel through in the scrotum and pelvis, it is vulnerable to twisting (torsion) along its course. When this happens, the blood supply to the testicles gets cut off and can lead to a permanently damaged testicle and infertility. Gently stroking the inside of the upper part of the thigh can trigger the cremasteric reflex, where the testicle on the same side lifts up due to a reflex arc involving a muscle within the scrotum. Its absence is a worrying clinical sign, which may signify twisting of the spermatic cord (testicular torsion). In young boys, the reflex is exaggerated and unreliable.
DISSECTION | The dartos muscle is a sheet of smooth muscle enveloping the scrotum. It helps maintain the fine balance of temperature regulation required for optimal sperm production either by crinkling the scrotal skin and reducing the surface area available to prevent heat loss or by expanding the skin to cool the testicles. The testicles lift up when exposed to sudden cold due to this shriveling effect.
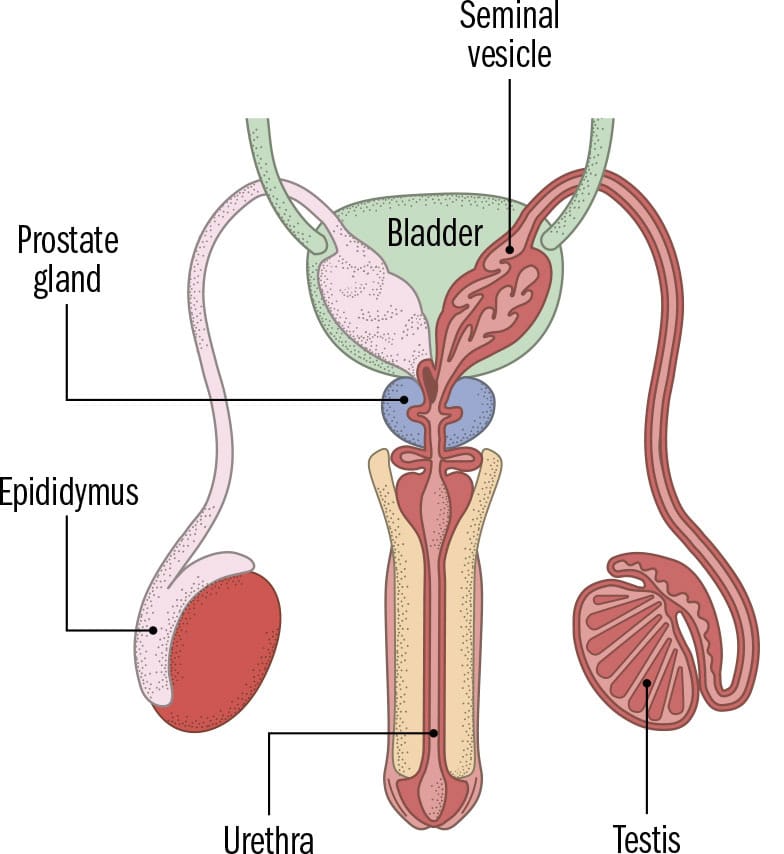
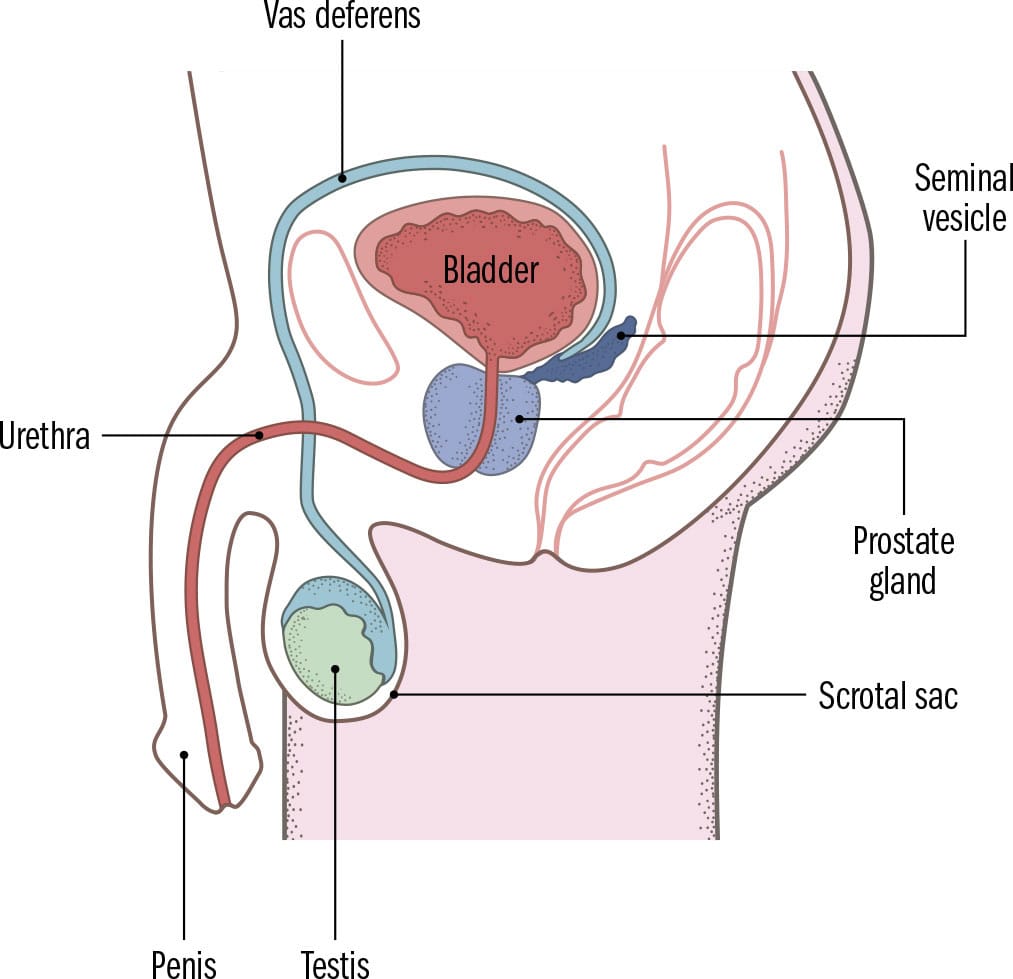
Sagittal view