4
BACK & LIMB ANATOMY
“It is the novel province of anatomy to tell the truth, the whole truth, and nothing but the truth about the structure, the origin and the history of man.”
HENRY FAIRFIELD OSBORN EVOLUTION AND RELIGION IN EDUCATION : POLEMICS OF THE FUNDAMENTALIST (1926)
MOVEMENT
We are bipedal, and move, stand, and walk upright. In this position, our trunk is erect, our knees are almost straight, and our feet are firmly planted on the ground (unlike larger mammals who stand and move on their toes, and ungulates who use hooves at the tips of their toes). Standing up straight and moving (locomotion) require coordinated movement of upper and lower limbs, the back, and buttocks.
We sway when we stand still
Simply standing up motionless creates a center of gravity just above the hip joints and in front of the spinal column, with the center of pressure approximately midway between the insteps of our feet. The main muscles we use are two muscles in the calf (soleus and gastrocnemius), with very little activity required by our thigh muscles. As we stand, we sway slightly, a factor that deteriorates with age when we may become less able to control our posture and may fall over as a result. If you decide to stand on one foot, the weight in the upper body requires the hip to be adjusted and the muscles in the buttocks region (gluteus medius, gluteus minimus, and tensor fascia lata on either side) need to be recruited to maintain balance.
Walking is a series of repeated gait cycles
Walking looks so simple but is really a complex biomechanical process requiring synchronized movement of hips, spinal column, arms, shoulders, and head to maintain balance and to get the feet to move across the ground. A child goes through a typical pattern of learning to sit (six months), crawl (nine months), walk supported (12 months), and unsupported (18 months). By the age of three, a child’s walk is similar to that of an adult.
Walking is somewhat like controlled falling: with each step, our body “vaults” itself over the limb that is not moving (inverted pendulum motion). The center of gravity fluctuates constantly, from being high in the middle of our stride to low when both our feet are on the ground. Our arms swing to stabilize our posture but, even today, how this happens is not fully understood. When we walk, we are striding through two repeating phases of the gait cycle. During one full round of the cycle, each foot is on the ground for about 60 percent of the time (stance phase) and lifted off the ground for the rest of the time (swing phase); in each of these phases, our gait goes through a single-support phase, when one foot is on the ground, and a double-support phase, when both feet are on the ground.
Three discrete things happen in the stance phase: the heel of the foot hits the ground (known as “heel strike”), then the rest of the foot hits the ground as the other foot makes contact with the ground, and, lastly, the foot leaves the ground (heel first and toes last, known as “toe-off”). Our knees are almost straight when our heels hit the ground, and bend only slightly before our toes lift off the ground. In the swing phase, two things happen: the leg lifts up and we are then propelled forward. This is how moving forward occurs, when the weight of the body is only on one limb. The knee is bent to a maximum of 60 degrees in the middle of this phase.
Muscles in the buttocks (gluteal region) tighten to stop the pelvis from dropping down toward the raised leg, as would happen if gravity took over. The gluteal, thigh, leg, and foot muscles are all in use during walking. The muscles in our calf propel us forward but this is enhanced by our foot arching and our toes flexing. The weight of the foot is balanced on the ball of the foot, the outer edges, and the heel; the toe muscles and lumbricals (small, worm-like muscles that simultaneously enable bending and straightening at three different joints in the foot) are important during walking, extending and balancing the toes so they do not buckle during toe-off.
We float a bit when we run
Running is analogous to being on a pogo stick, with our center of gravity shifting in the opposite direction to when we walk, from being low in the middle of the stride to high when we are “double-floating,” when neither of our feet is on the ground. During jogging, each foot is on the ground 40 percent of the time; when we break into a sprint, this is for only 27 percent of the time. The faster you run, the less time your feet spend in the stance phase of the gait cycle. In contrast to the walking gait cycle, during running the knee of the leg supporting our weight bends. During running, too, the leg muscles exert far more forces than during walking. Our foot is moving when the heel hits the ground, and is locked into a rigid structure so that the shock of the impact can be better absorbed. Our body now vaults itself over the foot and the foot passively stretches downward, becoming more flexible to adapt to the running surface. Just before it lifts off again, it tightens and lifts upward and backward, becoming a lever. Most of us hit our heels on the ground first when running; when we sprint, to get better leverage, our forefoot hits the ground first. Curiously, our knees never fully straighten when we run.
VERTEBRAL COLUMN & BACK
GROSS ANATOMY | The S-shaped vertebral column occupies a central position in the body. It provides a rigid supporting framework and protects the spinal cord running within it. While standing or walking, it transmits our weight. The curved linkage of 33 individual bones extends from atlas to coccyx (tailbone) in ever-increasing, then diminishing, size. The lowest vertebra is merely a pointy tip. Seven cervical vertebrae move the neck, twelve thoracic vertebrae help form the protective casing around the chest, five lumbar vertebrae move the lower back, five sacral vertebrae fuse to form the back wall of the pelvis, and four fused coccygeal vertebrae form the bottom of the column. There is limited flexibility between individual vertebrae but, due to cushioning intervertebral discs separating the vertebrae, the spine is very flexible. Strong back muscles, layered in the neck and lower back, attach to the spinal column, enabling movement and providing stability to allow posture. The muscles closest to the skin are the extremely broad latissimus dorsi and trapezius muscles. Below them are fleshy muscle bulks on either side of the spinal column known as the erector spinae muscles; they keep us in an upright position. Back muscles form a strong platform for limb movement and work together with abdominal wall and lower limb muscles.
CLINICAL ANATOMY | Spinal nerves emerging at each vertebral level are vulnerable to damage when the jelly-like pulp (nucleus pulposus) at the core of an intervertebral disc ruptures and pushes through the tougher outer rim (annulus fibrosis). This disc prolapse presses on the nerve below and pain, numbness, tingling, and weakness (the symptoms are known as “sciatica”) may radiate along the distribution of the muscles or muscle groups supplied by the nerve, usually in the area of the buttocks and/or lower limb. Most back problems, especially those in the lower back (the erector spinae and transversospinales muscle groups), can be resolved by improving core back muscle strength. Back surgery is rarely required.
DISSECTION | On average, a female vertebral column (231/2 in./60 cm) is 4 in. (10 cm) shorter than a male one (271/2 in./70 cm). Intervertebral discs, which make up a third of vertebral column height, swell with fluid absorbed during periods of rest. Weight-bearing activity squeezes fluid out, the result being that a 20 percent reduction in water content and vertebral column height takes place during the day. Three hours after rising, our full height has decreased by about half an inch (15 mm).

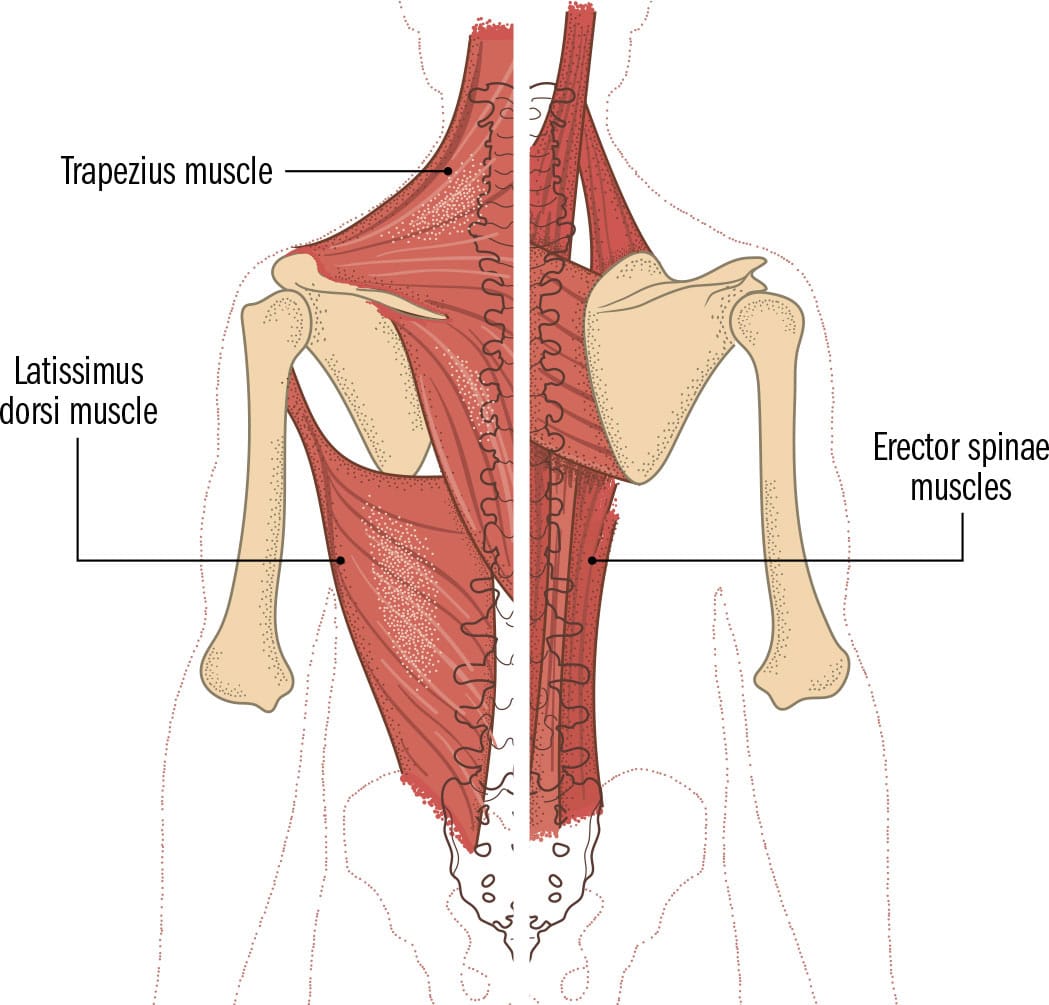
Posterior view back muscles
SHOULDER JOINT & AXILLA
GROSS ANATOMY | The upper limb is connected to the trunk via the scapula (shoulder blade) and clavicle (collar bone) meeting to form the pectoral (shoulder) girdle. They anchor the humerus (upper arm bone) to the chest via a ball-and-socket joint (glenohumeral or shoulder joint), forming the most mobile joint in the body. The scapula at the back floats over the ribcage through only muscular attachments. The ball-shaped head of the humerus nestles in a shallow cavity on the outer rim of the scapula, allowing it to freely move in multiple planes. The shoulder joint is dependent on muscles to stabilize and move it and requires several stabilizing mechanisms to prevent the head from popping out of its socket. A slice of cartilage deepens the cavity, a fluid-filled capsule surrounds it to tether the scapula to the humerus, fluid-filled sacs (bursae) pad the area outside the capsule to minimize friction, ligaments anchor bone to bone, and four small rotator cuff muscles and the biceps brachii muscle provide muscular stability. Movement is enabled by rotator cuff muscles and strong muscles (deltoid, trapezius, latissimus dorsi, serratus anterior, and pectoralis major) attaching to the shoulder complex. The axilla (armpit) is the anatomical space below the shoulder, between the arm and the trunk, filled with large vessels, nerves, and lymph nodes, all surrounded by fat.
CLINICAL ANATOMY | Mobility at the shoulder joint comes at a price: it is naturally unstable and dislocation happens relatively easily. A blow to the arm while it is raised may pop the head of the humerus forward and downward out of the socket (a ligament prevents upward dislocation) into the axilla, where nerves and vessels are at risk of damage. The deep rotator cuff muscles gripping hold of the humerus from several sites on the scapula are also prone to damage. The tendon of supraspinatus traveling within a narrow space (subacromial space) can become inflamed with overuse, and shoulder movement becomes painfully limited (impingement/painful arc syndrome).
DISSECTION | The collarbone (clavicle) links the sternum and scapula. It is the first bone in the body to harden into bone (ossify) and the most common to become fractured. Clavicle initially meant “small key” or “bolt,” perhaps because it bolts onto the shoulder. It acts as a prop to push the shoulder back and allow the free-swinging movement of the arm.

Anterior view pectoral girdle muscles

Posterior view left shoulder
ARM
GROSS ANATOMY | The arm is the anatomical region between the shoulder and elbow joints. It consists of just one long bone (humerus) surrounded by two groups of muscles that move it (the biceps and the triceps). The humerus is the largest and longest bone in the upper limb, with a hemispherical and expanded top end (head). When the arm is resting by the side, the smooth head points slightly backward and toward the midline to form the glenohumeral joint (shoulder). A small and large bony bump (lesser and greater tubercle) can be felt close to the top of the arm. Between them, a groove carries the long head of biceps brachii tendon to provide additional stability to the shoulder joint. The humeral shaft is somewhat cylindrical, curving forward at the lower end to form two knuckle-shaped expansions that help form the elbow joint. Arm muscles are arranged into two sets separated by deep fascia. Enclosed within each fascial compartment are muscles and their blood and nerve supply. Three muscles in the biceps compartment at the front (biceps brachii, brachialis, and coracobrachialis) move the arm forward at the shoulder joint and bend it at the elbow. The single three-headed triceps muscle in the compartment at the back moves the arm backward at the shoulder and straightens the elbow.
CLINICAL ANATOMY | Nerves running behind, along or in front of the humerus are at risk. At the narrowest part below the head, a fracture can damage the axillary nerve running behind the surgical neck, disrupting nerve supply to the deltoid muscle. A mid-shaft fracture can damage the radial nerve running in a spiral groove in contact with the bone, leading to an inability to straighten the wrist and hand. The biceps and triceps muscles may pull the bone fragments of a facture occurring just above the elbow in opposing directions. The jagged edge of the bone protruding forward can compress the median nerve and brachial artery; a claw-like deformity may form in the hands and fingers (Volkmann’s contacture).
DISSECTION | There are several bony condyles in the body. These are usually smooth rounded bumps at the end of bones (mandible, humerus, and femur) and form joints with other bones. The Greek word kondylos originally meant “knuckle,” entering the English language via Latin and French to mean “knob at the end of a bone.” Anatomical condyles are somewhat knuckle-shaped.

Anterior view right shoulder and arm

Anterior view right arm muscles
ELBOW & CUBITAL FOSSA
GROSS ANATOMY | The elbow is for shortening and lengthening the forearm and for reaching out and grasping objects. The lower end of the humerus forms a forward-sloping, double-knuckled expansion (the condyles) that meets the two forearm bones (the radius and ulna): the capitulum articulates with the radius on the thumb side, while the trochlea articulates with the ulna on the little finger side. They form a hinge joint that bends (flexes) and straightens (extends) the forearm, and produce a rotational movement with the radius and ulna that makes it possible to turn the palm of the hand upward (supination) or downward (pronation). The upper arm muscles act on the elbow to produce these movements (triceps straightens and brachioradialis and biceps brachii bends the elbow); only one muscle in the elbow region has a single function to bend it (brachialis). Muscles that flex and extend the forearm attach to two bony bumps above and on either side of the humeral condyles (lateral and medial epicondyles). A joint capsule and strong collateral ligaments stabilize the elbow. The cubital fossa is a triangular depression at the elbow joint within which the pulsation of the brachial artery can be felt. The median nerve supplying several muscles in the forearm and hand runs close to it. A network of veins is closest to the skin here, useful for taking blood.
CLINICAL ANATOMY | Some extensor muscles of the forearm attach to the lateral epicondyle of the humerus. Overuse of these muscles inflames their common origin, leading to pain and tenderness over the outer bump, common in tennis players (lateral epicondylitis or tennis elbow). Overuse of muscles in the flexor compartment attaching to the medial epicondyle results in symptoms on the inner aspect of the elbow; medial epicondylitis is common in golfers. The ulnar nerve runs on the inner aspect of the elbow joint, close to bone. Leaning too long on the elbows can produce numbness and tingling in the little finger and half of the ring finger, as the nerve supplies this area.
DISSECTION | The veins at cubital fossa were commonly used for bloodletting. A slip of a barber–surgeon’s knife could easily damage the underlying brachial artery and median nerve, if it were not for the “grâce à Dieu!” (grace of God) aponeurosis. Even today this flattened triangular tendon (aka bicipital aponeurosis) fans out to protect structures below the veins, providing reassurance for inexperienced clinicians taking blood samples from the area.

Anterior view right elbow

Front view right elbow
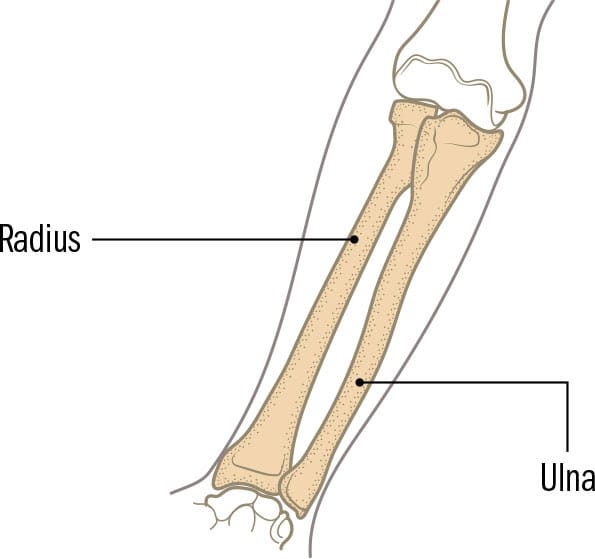
FOREARM & CARPAL TUNNEL
GROSS ANATOMY | The forearm is the area of the upper limb between the elbow and wrist. Two long bones, radius (thumb side) and ulna (little finger side), are bound together by joints at the ends of the bones, and by a thin flat sheet of ligament in the middle (interosseous membrane). This sheet divides the muscles on either side of the bones into sets: flexors at the front and extensors at the back. The 12 muscles in the extensor compartment straighten the fingers and wrist, and bend the wrist backward. The radial nerve supplies all the extensors of the upper limb. The eight muscles in the flexor compartment bend the wrist, hand, and digits (thumb and fingers) forward. The median and ulnar nerves travel with the flexors, and innervate them. The carpal tunnel is a U-shaped bony tunnel at the wrist covered by a strip of fascia (flexor retinaculum). Within it, nine tendons originating from three forearm flexor muscles (four each from flexor digitorum superficialis and profundus and one from flexor pollicis longus) tunnel their way into the hand to enable the hand’s powerful gripping movements. Flexor retinaculum holds them down, preventing bowstringing of the tendons when the wrist is bent forward.
CLINICAL ANATOMY | The compartments of the forearm have little space within them due to deep fascia enveloping them relatively tightly. After an injury or surgical procedure, accumulating fluid may squeeze the blood supply and nerves within so tightly that irreversible muscle death follows. Compartment syndrome is a surgical emergency. A long cut through skin and deep fascia is made to relieve the pressure. The median nerve travels through the narrow and congested carpal tunnel. If it gets squeezed tightly, pain, altered sensation, or numbness are felt within the thumb and next two and a half fingers (carpal tunnel syndrome). The flexor retinaculum can be cut through to release the pressure (carpal tunnel release).
DISSECTION | The palmaris longus muscle may be absent on one or both sides in 10 to 15 percent of the population. This spindle-shaped flexor inserts into the wrist, anchoring the overlying skin to the underlying fascia of the hand. Absence or presence is easily tested by opposing the little finger and thumb and flexing the wrist (known as Schaeffer’s test). A raised ridge running close to the midline on the front aspect of the wrist hints at its presence.
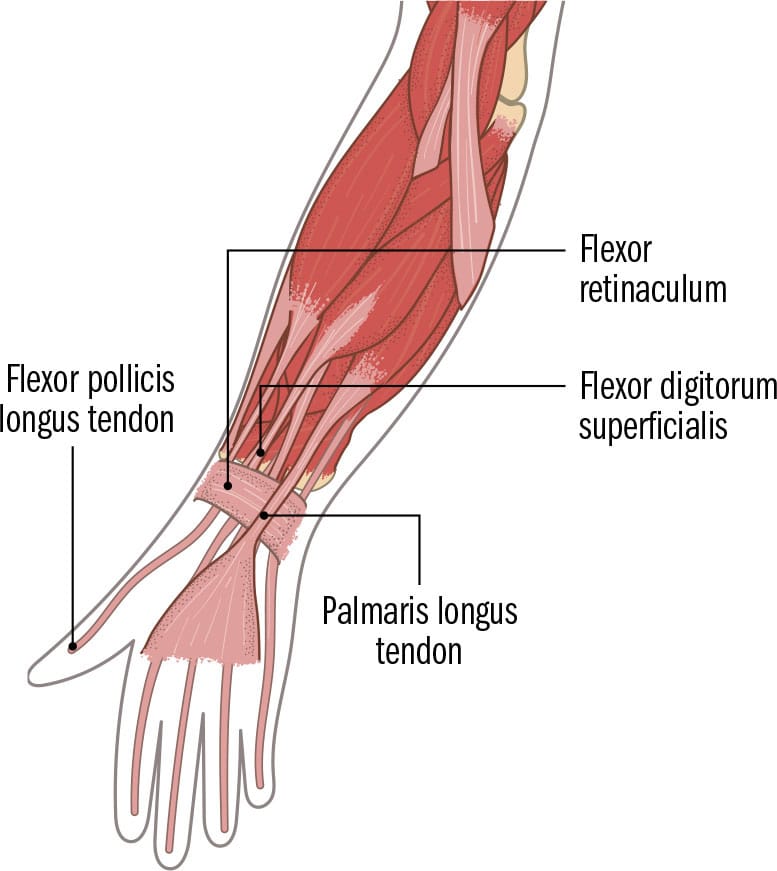
Anterior view (palms facing forward)

Posterior view (back of hand)
Right forearm and wrist
WRIST & HAND
GROSS ANATOMY | Grasping objects and opening the palm to release them both require simultaneous contraction of numerous individual hand muscles and are mechanically extremely complex actions. The 27 bones that form the framework for these actions are organized into rows of bone: the wrist (carpus), consisting of two rows of four bones, the five metacarpals (hand bones), and the 14 bones of the five digits (phalanx). At each meeting point between the bones, ligaments and capsules tether bones to each other, allowing movement at each joint. The joint between the wrist and the metacarpal of the thumb is exceptionally mobile, enabling us to touch the tips of each finger with the thumb. Numerous muscles enter the hand from the forearm (extrinsic) and several start and end within the hand (intrinsic). Extrinsic muscles enable strong powerful movements (grasping, gripping). Intrinsic muscles fine-tune, allowing intricate movement, and are arranged into bulging groups of muscles visible on the palm of the hand—those at the thenar eminence move the thumb and those at the hypothenar eminence move the little finger. Special muscles move just the fingers (lumbricals, interossei). The digits are supremely sensitive to touch and positioning, taking up a large area in the brain disproportionate to their size to interpret these senses.
CLINICAL ANATOMY | The wrist joint is formed between the radius and two nearest carpal bones (scaphoid, lunate). The mobility of the hand moving in relation to the forearm comes at a price: the wrist is unstable and fractures often occur here. A fall onto an outstretched hand can break the end of the radius, compromising the large radial artery (felt on the thumb-side at the wrist) and the nerves in the region. The boat-shaped scaphoid is the most commonly fractured bone in the wrist but fractures are easily missed, as they show up on X-ray often only after their blood supply (which travels through a narrow isthmus of bone that usually breaks) has been compromised.
DISSECTION | The Latin and Greek origins for phalanx (plural, phalanges) related to heavily armed soldiers in close ranks. The finger bones sit in close proximity to one another in a row, resembling a phalanx of infantry soldiers. The thumb has two phalanges, the other four digits have three each. The toe bones have a similar arrangement and are also called phalanges.

Posterior view right hand

Anterior view left hand
HIP JOINT
GROSS ANATOMY | The lower limb is attached to the spinal column via the hip bone (pelvic girdle). Compared to the shoulder, this is a far more stable arrangement, as the pelvis and lower limbs must be able to bear our weight when we move around or stand still. The hip joint is a ball-and-socket joint, similar but not identical to the shoulder joint. The compromise for stability comes at a reduction in the range of movement, although the joint is still capable of a wide variety of movement. Two large bones meet to form this joint: the innominate (hip or pelvic) bone and the femur (thigh bone). The ball-like head of the femur sits snugly in a deep socket in the hip bone (at the acetabulum), held there by a strong ligament (ligamentum teres femoris) that runs from inside the acetabulum to a small dip in the head of the femur (fovea). The joint is surrounded by a fluid-filled joint capsule (resembling a purse string) that runs from the rim of the acetabulum to a raised area (intertrochanteric line) between two bony bumps (greater and lesser trochanter) close to the neck. Three tough ligaments prevent forward and backward movement of the femoral head, and fluid-filled sacs (bursae) lubricate the area. Strong gluteal and thigh muscles move the hip.
CLINICAL ANATOMY | Of all the joints in the human body, the hip is most important in terms of the catastrophic consequences of any damage to it. It is susceptible to age-related changes, particularly weakening of the bone (osteoporosis) and wear and tear of the joint (osteoarthritis). Weakened bone makes it susceptible to fracture at the narrow neck, particularly in the elderly. The femoral head receives its blood supply from below the joint, and blood travels up to the head plastered, surprisingly, under the fibrous capsule along the neck. So, when the neck breaks as a result of a fall, the blood supply to the head is lost and the bone dies (avascular necrosis of the femoral head).
DISSECTION | The acetabulum is the socket into which the head of the femur fits. Its concave shape resembled a “small vinegar cup” commonly used in Roman times. The site is the fusion point of three bones forming the hip (innominate) bone. Fusion is completed between the ages of 16 and 25. In children, in whom the acetabulum (and hence the three parts forming the hip bone) is unfused, this is visible on X-ray as a Y-shape (or an inverted Mercedes Benz sign).
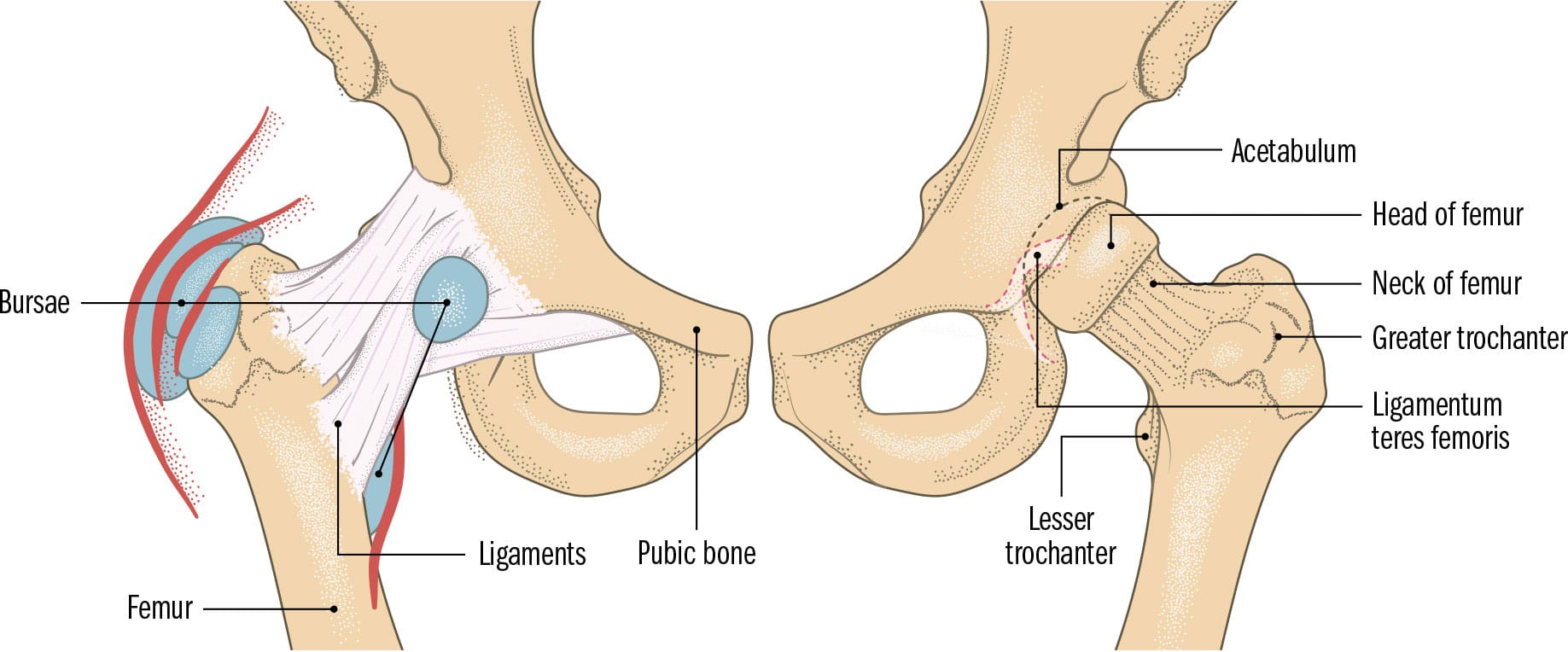
Anterior view pelvis and hip joint
GLUTEAL REGION
GROSS ANATOMY | The gluteal region is between the lower back and the upper thigh. The markedly rounded area is formed by the forward tilt of the pelvis, the fleshy mass of the largest (and, perhaps, most powerful) muscle in the body (gluteus maximus), and a considerable amount of fat. Two groups of gluteal muscles move the hip joint. The buttocks (gluteus is Latin for “rump” or “buttocks”) allow us to sit upright without needing to rest our weight on our feet in the way that four-legged animals do. Its bony framework is the back of the pelvis and vertebral column, the hip bones on the sides and the sacrum in the midline. At the top of this region, the rounded edges of the iliac crest on the hip bone can be felt on both sides. These serve as an attachment site for gluteus maximus, which allows us to stand in an upright position by virtue of its size and the power it has to stabilize the trunk (it prevents our trunks from leaning forward). Several deep muscles (piriformis, superior gemellus, inferior gemellus, obturator internus and quadratus femoris) rotate the hip. The two rounded muscles are separated in the midline by a deep cleft (natal cleft) in which the anus sits. The bottom of the gluteal region is marked on the surface by horizontal gluteal creases, below which the thigh begins.
CLINICAL ANATOMY | Immediately below the large gluteus maximus muscle are two smaller muscles—gluteus medius and minimus. Despite their smaller size, the role they play in maintaining the trunk in an upright position when the opposite side is raised (running or walking) is vital. As long as these two muscles are functional, there is little effect on walking or running, even if the other muscles acting on the hip joint are not fully functional. Paralysis of these glutei muscles, however, results in a curious lurching gait. Nerve damage can be tested by getting the person to stand on the affected side; the pelvis on the unaffected side will dip down (known as Trendelenburg sign).
DISSECTION | The dimples of Venus are two indentations in the lower back above the natal cleft. They are more prominent in women, in whom the dimples have been considered a sign of beauty (Venus being the Roman goddess of beauty). A short ligament tethers skin to a bony bump on the hip bone (posterior superior iliac spine), forming the dimples. They are used as surgical landmarks in spinal surgery.

Posterior view
THIGH & FEMORAL TRIANGLE
GROSS ANATOMY | Some of the largest and most powerful muscles move the hip and knee and reside within the thigh. They are mostly associated with the longest, heaviest, and strongest bone in the body; the femur measures, on average, 173/4 in. (45 cm). Its ball-shaped hemispherical head contributes to the hip joint, and its lower expanded end, with double-knuckled bumps, contributes to the knee joint. Deep fascia binds together the entire lower limb, wrapping round it like plastic wrap. Where it pushes inward to attach to bone, it forms two anatomical compartments in the thigh. The muscle groups are functionally organized into three compartments, each with its own nerve and blood supply. The posterior compartment has two groups of muscles: those that move the thigh inward and upward (adductor compartment) and those that move the hip backward and bend the knee (hamstring compartment). The anterior compartment has muscles that bend the hip and straighten the knee (quadriceps compartment). When viewed from the side, the front of the thigh appears to curve forward, reflecting the shape of the curved femoral shaft overlain by the fleshy mass of quadriceps femoris (containing rectus femoris, vastus lateralis/medialis/intermedius muscles). The outer side of the thigh is flattened by a tight band of fascia, from hip bone to below the knee (iliotibial tract), which stabilizes both joints.
CLINICAL ANATOMY | A triangular space at the top of the thigh, shaped like an inverted sail, is the femoral triangle. It is bounded by two muscles (sartorius and adductor longus) and the inguinal ligament. Within it, the femoral nerve, artery and vein sit side by side (outside to inside). The pulsating femoral artery is a landmark for accessing the artery or the vein in emergencies. The femoral artery lies close to the bone lower down, as it makes its way to the back of the thigh through an opening in a muscle (adductor hiatus). Shaft fractures that tear the artery here may be catastrophic, as the artery pumps the entire blood volume through it within minutes.
DISSECTION | The longest muscle in the body starts on a bony bump on the hip bone and travels obliquely across the thigh to insert below the knee. Sartorius (sartor is Latin for “tailor”) is known as the “tailor’s muscle,” as tailors in former times best illustrated the use of this muscle while working cross-legged on the floor. For similar reasons, it may sometimes be referred to, rather rudely, as the “honeymoon muscle.”

Anterior view
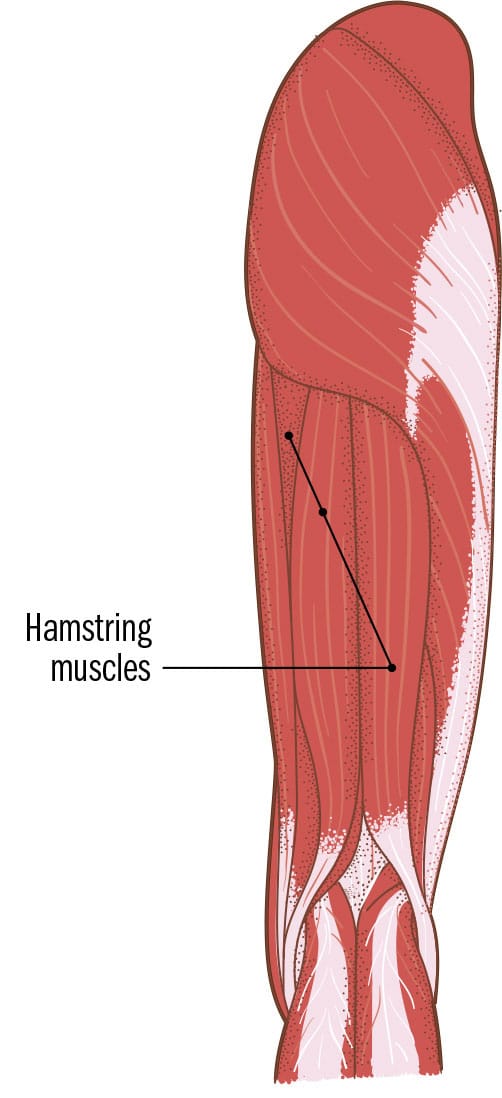
Posterior view

Cross section of thigh compartments
KNEE & POPLITEAL FOSSA
GROSS ANATOMY | The largest joint in the body is the knee joint. It carries the entire weight of the body above it and is subject to a significant amount of relentless stress. The knee is a modified hinge joint, consisting of two joints: one between the knuckle-shaped condyles on the femur and the shinbone (tibia), and the other between the kneecap (patella) and the femur. The space between the femur and the tibia is smooth and cushioned by crescent-shaped cartilages (menisci) on the tibial plateau (widened flat top). The femur and tibia are held together by extremely strong connecting ligaments that cross over in the midline (anterior and posterior cruciate ligaments) and prevent the tibia from moving too far forward or backward when the leg is bent. Sturdy ligaments on either side (lateral and medial collateral ligaments) also hold it in place, and an incomplete fluid-filled capsule surrounds it on the sides and at the back. The quadriceps femoris tendon travels over the knee, enclosing the patella, and attaches onto the tibial tuberosity (easily felt on the upper top end of the tibia). This arrangement allows the muscles of the anterior compartment of the thigh to straighten the knee. Other thigh and leg muscles do a combination of movements at the knee.
CLINICAL ANATOMY | The popliteal fossa is the large depression behind the knee through which the blood and nerve supply to the knee and lower leg travels. The popliteal artery is the deepest structure in this space. Bulges commonly occur in the fossa and can be anything from a cyst to a weakened and ballooning artery (aneurysm). Aneurysms of the popliteal artery were fairly common when tight-fitting riding boots were used for horse-riding. If present, aneurysms require surgical repair, and care must be taken to avoid damaging the structures closer to the surface (the nerves that supply the lower leg and the popliteal vein).
DISSECTION | The patella is the body’s largest sesamoid bone. From the Latin for “sesame seed,” sesamoid bones are usually very small and embedded within tendons. Their precise role is not known but they may lessen friction, and change the direction of muscle pull. Instead of patellae, babies have a soft cartilage that starts to harden into bone by their third year and is fully formed at puberty.

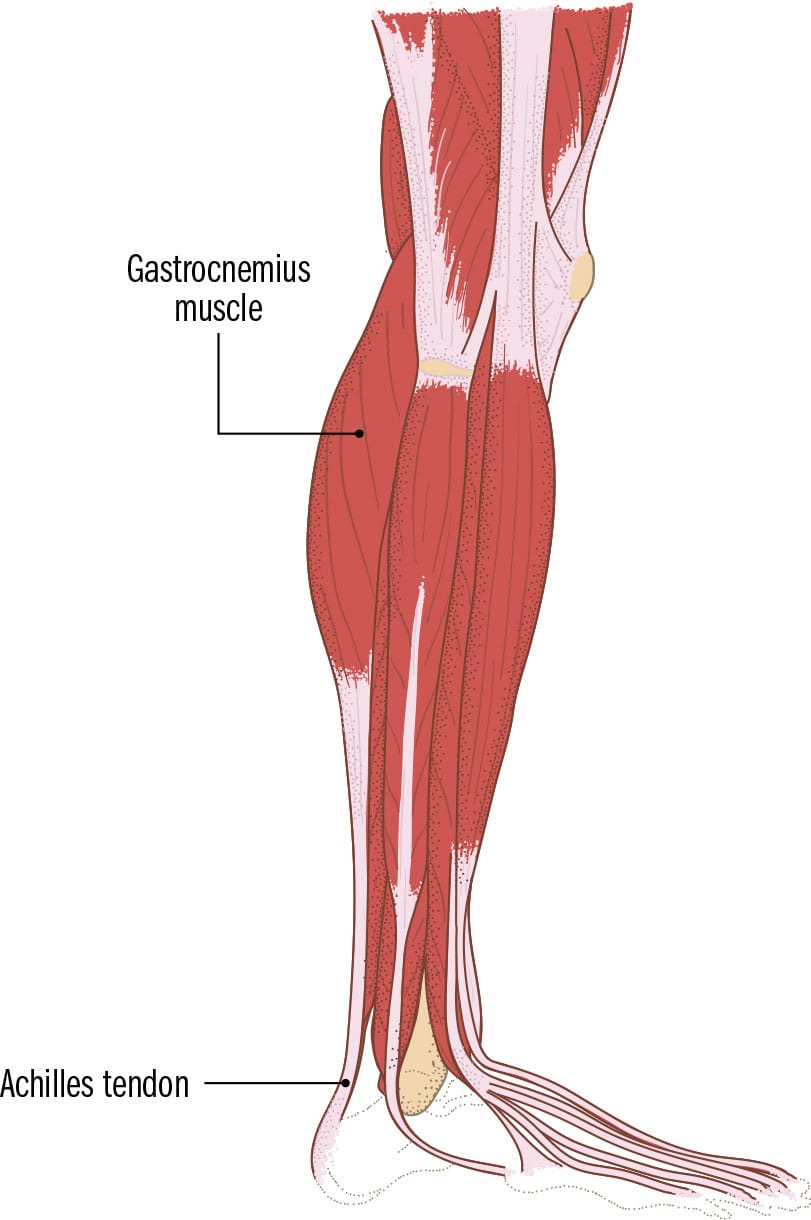
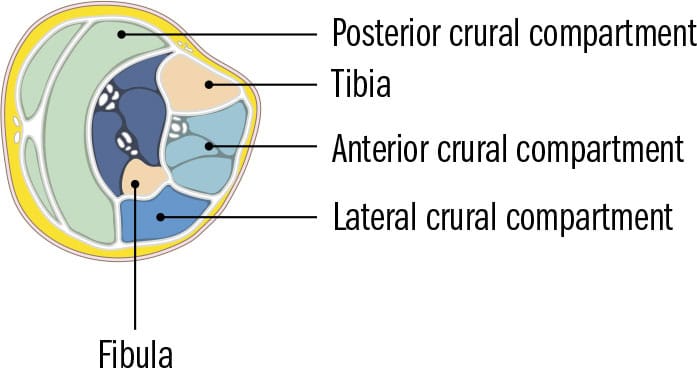
LEG
GROSS ANATOMY | The legs (crus/crura) are anatomically situated between knee and ankle. They allow a range of movement, and enable standing and dancing. As they bear the weight of the body above, the muscles and bones within are strong. The tibia (shinbone) is the second-largest and heaviest bone in the body. The back of the leg is the calf. Its bulk and shape come mainly from a large two-headed muscle resembling a cow’s belly (gastrocnemius). The front of the leg is formed by the tibia and fibula. These bones are held together by a thin flat sheet of interosseous membrane, with joints at the top and bottom. Muscles arise from both bones but mainly from the tibia. No muscles originate from the flattened front (the muscle-free zone is the shin) or lower third of the tibia. Four groups of muscles encircle the leg: the anterior crural compartment muscles pull the foot up toward the nose (dorsiflexion) and the inner foot edge upward (inversion), the posterior crural compartment muscles (in two compartments) point the foot and toes downward (plantarflexion) and bend the knee, and the lateral crural compartment muscles pull the outer edge of the foot upward (eversion). Three tendons from the posterior compartment muscles meet to form the Achilles (calcaneal) tendon that inserts into the heel bone (calcaneus).
CLINICAL ANATOMY | Some structures in the leg are vulnerable to damage. The fibular (peroneal) nerve wraps around the neck of the fibula, where it can get torn in more serious knee injuries but may also be damaged when a plaster cast is placed too tightly. The nerve supplies the ankle as well as the lateral and anterior crural compartments. Loss of innervation results in a characteristic steppage gait, where the foot hangs down and the toes scrape the ground while walking (foot drop). Tibial fractures in the lower third of the bone heal poorly. As no muscles attach to this area, the blood supply is limited, meaning bone healing is slower.
DISSECTION | The longest vein in the body is the great saphenous vein running from the big toe (hallux) to the top of the thigh along the inside of the lower limb. The origin of the word “saphenous” is shrouded in mystery. In Greek it meant “obviously visible,” whereas in Semitic languages (Arabic and Hebrew) it meant “hidden.” To complicate matters, it is visible at the ankle and hidden in the thigh.

ANKLE JOINT & TARSAL TUNNEL
GROSS ANATOMY | The leg (crus) meets the foot at the ankle bone (talus). The talocrural joint (ankle joint) allows the lower limb to interact with the ground and is vital for standing, gait, and other everyday functions. It is formed where two large bumps on the ends of the tibia and fibula (medial and lateral malleoli) leave a spanner-shaped space. The talus sits like a nut within the space. The simple hinge joint allows two movements: toes to the nose dorsiflexion) or toes pointing downward (plantarflexion). The talus is wedged between the malleoli when the ankle is dorsiflexed, a very stable position. When the ankle is plantarflexed, the joint is more lax and some degree of side-to-side movement can take place. The ankle is surrounded by a fibrous capsule and is weak at the front and back. On the sides, it is reinforced by strong ligaments. On the inner aspect, the deltoid or medial collateral ligament radiates to four places on the foot from the medial malleolus. Three bands of ligaments form the lateral collateral ligament from the lateral malleolus to areas on the foot, a much weaker arrangement than on the opposite side. The tarsal tunnel is a space behind the medial malleolus covered by a band of fascia (flexor retinaculum) containing the tibial nerve, artery, and vein and muscle tendons entering the foot.
CLINICAL ANATOMY | Sprains of the ankle are very common, with the ankle being the most commonly injured joint. The arrangement of the collateral ligaments means that the individual bands forming the outer reinforcement (lateral collateral ligaments) sprain more easily. This happens when the foot is inverted too much. When the ankle is plantarflexed, it is in a compromised position, and eversion in this position can result in the tough deltoid ligament getting sprained. Although the ankle is frequently injured and bears the entire weight of the body, wear and tear of this joint (and resulting osteoarthritis) is low when compared to the hip or knee.
DISSECTION | The talocrural joint is the only example of a true mortise joint in the body. In carpentry, a mortise and tenon joint is commonly used when a frame construction needs to be strong: the mortise is a depression cut into wood (in the ankle, a spanner-like arrangement formed by the two malleoli) and the tenon a tongue that fits into the mortise (in the ankle, the talus).

Medial view right ankle

Posterior view left ankle
FOOT
GROSS ANATOMY | The foot is a complex and very strong functional unit with a dual role: it creates a rigid support for the body when we are stood up but transforms into a mobile springboard when we are running or walking. It has 28 bones, (including the ankle joint and small sesamoids at the base of the big toe) and over 30 joints, numerous ligaments and muscles. The foot is traditionally divided into hindfoot (calcaneus and talus), midfoot (cuboid, navicular, and three cuneiform bones), and forefoot (five metatarsals and 14 phalanges). These are joined together by muscles, ligaments, and thickened fascia on the sole of the foot (plantar fascia). The foot muscles are arranged into those entering it from the leg (extrinsic) and those starting and ending within the foot (intrinsic). Two longitudinal arches and one transverse arch, formed by the interlocking of bones, act as shock absorbers. They allow some movement. When stood up, the arches sink slightly under the load: the bones lock together and the ligaments are tensed, so the foot is a rigid base. When the foot is raised during walking, the arches unlock and allow the spring-like actions of walking and running. The heel and the metatarsal heads bear the main weight of our bodies when we are stood up.
CLINICAL ANATOMY | The plantar fascia is a thick condensed fascial band from calcaneus to the base of the toes on the sole of the foot. Heel pain associated with the plantar fascia is common. The hallmark of plantar fasciitis (inflamed plantar fascia) is pain on weight-bearing after a period of rest. Its causes are still not properly understood and recovery can take a long time. A march fracture is a type of stress fracture that occurs as a result of strain through prolonged periods of standing or repeated, concentrated damage to the metatarsals, most commonly the second or third metatarsal. Such fractures are hard to diagnose as there may be no clear fracture line on the X-ray.
DISSECTION | Roman soldiers made the dice they used in games from sheep anklebones known as “knucklebones” (Latin taxillus or talus). We now use “talus” to indicate the second-largest bone in the foot, belonging to the group of foot bones known as the tarsal bones. Unusually, the blood supply to the talus travels past the bone then backward to supply the bone (like the scaphoid at the wrist). The bone has no muscles attaching to it.

Inner view right foot

Superior view right foot

Inferior view (sole) right foot