APOCALYPSE COW: THE ORIGINS OF BSE
Unfortunately, the custom of consuming human flesh, like exotic sexual practices, polygamy, and other alien habits, raises violent, unintellectual passions in the Western scholars who study them.
Brian Fagan, The Aztecs
IN THE 1980S researchers in the United Kingdom, like those in New Guinea, were also seeking to explain how a strange form of spongiform encephalopathy was being transmitted, and where it had come from. Also like their southern counterparts, they struck lucky after making a connection to diet – in this case, after examining the diets of dairy cows.
In order to maximise milk production, farmers typically supplemented livestock diets with protein – most often in the form of soya bean products. However, in the 1940s meat and dairy industries in the UK came up with an alternative, rendering the waste products of livestock slaughter into an innocent-sounding material they called ‘meat and bone meal’. Noting the cost-saving benefits, the US and other nations followed suit. In addition to ingredients like bones, brains, spinal cords, heads, hooves, udders and viscera, meat and bone meal also called for the bodies of sick animals (including poultry, pigs, sheep and so-called ‘downer cattle’1) that had been deemed unfit for human consumption. This was then sent off to the knacker’s yard. During the rendering process, the above-mentioned were ground, cooked and dried into a greyish, foul-scented powder which was sold as a source of dietary protein, calcium and vitamins for dairy cows, beef cows, pigs and poultry.
Although a comparison of livestock feeding practices with the ritualised consumption of relatives by the Fore seems to be a bit of a stretch, in reality there is an important similarity. In the case of the Fore, ritual cannibalism of kuru victims exposed practitioners to a deadly infective agent. And although nobody knew it at the time, beginning in the 1940s, livestock were exposed to similar pathogens after being forced to consume dietary supplements derived (at least partially) from sickened members of their own species.
But why had the bovine spongiform encephalopathy (or BSE) epidemic struck so suddenly four decades later? The livestock industry had been using meat and bone meal for forty years and nothing like this had ever happened before.
In searching for answers, the British government enlisted epidemiologist John Wilesmith, who examined the records of rendering plants across the UK. He soon determined that several modifications related to the rendering process had been instituted in the early 1980s. The first was that most of the plants had discontinued the separation of tallow (a creamy fat used to made candles and soap) from the material being converted into meat and bone meal. Previously, dangerous solvents had been used to extract tallow during the rendering process, but after a massive industrial explosion in 1974 safety measures were introduced regarding the handling of solvents in the workplace. Rather than deal with the expensive modifications mandated by the new rendering industry regulations, all but two of the plants chose to abandon the tallow-extraction process altogether. As a result, substances that had once been removed by the solvent extraction process now remained in the meat and bone meal. Presumably, these substances included the still-unidentified infective agent causing BSE.
Additionally, Wilesmith and his team learned from herdsmen that several recent changes had been made to livestock diets. The first was a significant increase (from 1 per cent to 12 per cent) in the amount of meat and bone meal added to dairy cow feed. Calves were also receiving the protein supplement at an earlier age. As in other spongiform encephalopathies, there appeared to be a direct correlation between the amount of contaminated material ingested and the likelihood of contracting BSE. Similarly, the incubation period for BSE was apparently shorter in younger animals. In theory, then, before industry-wide changes in diet were implemented, calves received less of the contaminated supplement and did not start ingesting it until later in their lives. As a consequence, infected animals would have been slaughtered before they had a chance to get sick.
The results of Wilesmith’s epidemiological study were presented to ministry officials in May 1988. He told them that the BSE problem could be traced to the popular nutritional supplement that had been contaminated with sheep scrapie. This material had subsequently been fed to cows, making them ill in turn.
BACK IN THE USA in 1963, Gajdusek realised that his fellow researchers had been correct about the striking similarities between kuru-infected brains, brains from victims of Creutzfeldt-Jakob disease, and those from sheep with scrapie. The puzzle was just beginning to come together when yet another piece was discovered – and this one was several decades old.
In 1947 an outbreak of what would become known as transmissible mink encephalopathy (TME) in farm-raised mink led investigators to search for links between the ranches where infected animals had been identified. They discovered that it was a common practice for adjacently located ranches to share animal feed. In these instances, when mink from one ranch came down with TME, invariably so did those on the adjacent ranch. The feed itself was a vile mess composed of cereal, fish, meat-packing-plant by-products like sheep entrails and other internal organs, and flesh from downer cattle. By the time another outbreak of TME occurred in 1963, veterinary researchers suspected that something very strange had happened – the disease had been transmitted across species, in this case from sheep to mink.
By September 1963, similarities in kuru, scrapie and TME-infected brain tissue, coupled with the discovery that TME and scrapie could be transmitted within and between species, led Gajdusek and NIH researcher Joe Gibbs to an important experiment. At the Patuxtent, Maryland, lab they inoculated a trio of chimpanzees with liquefied brain tissue from kuru victims. If the chimps came down with the disease, it would prove once and for all that kuru was not a genetic abnormality or a stress-related psychosis, but an infectious or transmissible agent. As Gajdusek left the US for another field season in New Guinea, he worried about the long, symptom-free incubation period for scrapie, which sometimes extended up to five years post-exposure. What if his experimental animals didn’t get sick for five years or more?
Gajdusek need not have worried. Less than two years after being inoculated, two of the chimps, Georgette and Daisy, began showing the telltale signs of kuru – at first a drooping lower lip in Georgette, and then changes in behaviour as both primates became more lethargic. Eventually the apes began to show even more clear symptoms of the disease: occasional unsteadiness and trembling followed by a gradual loss of balance.
On 28 October 1965 Georgette was euthanised by the heartbroken researchers. Her entire body was deconstructed, fixed and preserved and her brain was sectioned for microscopic analysis. The results were conclusive. Slides of Georgette’s cerebellum were indistinguishable from those of human kuru victims.
Gajdusek and his colleagues had discovered a brand-new disease.
Meanwhile, Michael Alpers, who had been studying kuru since 1961 and who had taken time out from his own fieldwork to collaborate with Gajdusek and Gibbs on the NIH primate study, waded through six years of Gajdusek’s epidemiological data on the Fore. After examining hundreds of Fore genealogies, Alpers and Gibbs came up with a remarkable observation: instances of kuru were beginning to decline in children, starting with the youngest age group. Their question was, why? Shortly after conferring with Glasse and Lindenbaum, Alpers came up with a hypothesis.
According to information gathered from interviews with the Fore, kuru victims were favoured at mortuary feasts because the physical inactivity that characterised the latter stages of the disease left the stricken individuals with a tasty layer of subcutaneous fat. Starting in the 1950s, though, government authorities in New Guinea began cracking down on the practice of ritual cannibalism and with mortuary feasts now forbidden by law, fewer people were eating infected tissue. As a result, incidences of the disease were decreasing. Additionally, since kuru had a shorter incubation period in children than it did in adults, the reduced occurrence of ritual cannibalism translated swiftly into a decreased incidence of kuru in the young.
In a February 1966 article in Nature, Gajdusek, Gibbs, and Alpers described the experimental transmission of a ‘kuru-like syndrome’ to their chimpanzees although the identity of the disease-causing agent was still unknown. Gajdusek, who still believed that they were dealing with a slow virus, was also reluctant to attribute the transmission of kuru to the consumption of infected flesh. Instead, he supported the view that, during the process of handling and cutting up the dead, the agent was transmitted via cuts or across the thin mucous membranes that line the human mouth, eyes and nose (a form of exposure known as inoculation).
By 1973, however, Gajdusek had come around to the idea that inoculation and consumption were both viable routes for kuru transmission.
The mechanism of spread of kuru is undoubtedly contamination of the population during their ritual cannibalistic consumption of their dead relatives as a rite of respect and mourning. They did the autopsies bare-handed and did not wash thereafter; they wiped their hands on their bodies and in their hair, picked sores, scratched insect bites, wiped their infants’ eyes, and cleaned their noses, and they ate with their hands …
Other researchers such as Joe Gibbs stuck to the hypothesis that Fore mortuary practices, rather than the actual consumption of infected flesh, were the primary routes of kuru transmission. In a radio interview, the NIH researcher admitted that initial attempts to transmit kuru to chimps via a gastric tube (which modelled the consumption of infected flesh by humans) had failed, and that it was only after the animals were injected with liquefied brain material from kuru victims that they came down with the disease. As for how kuru was transmitted to the Fore, Gibbs explained that the Fore had multiple routes of inoculation, including their eyes and mouths, as well as skin lesions caused by leeches, mosquito bites and the razor-sharp blades of puni grass.
Today, in regions of West Africa, the Ebola virus is often spread because of ritual practices that involve handling of recently deceased victims. For example, some Muslims believe that family members should wash the bodies of the dead, a practice that also includes the elimination of certain bodily fluids. When performed under less than sanitary conditions, this ritual can place individuals in grave danger if they come into contact with infectious body fluids like blood, vomit and diarrhoea – all of which characterise advanced Ebola.
I asked Lindenbaum if she thought that Fore mothers had encouraged their children to handle the dead during mortuary ceremonies.
‘Mothers handed food to their small children to eat,’ she said. ‘Since people eat with their hands, most children would touch the food given to them by their mothers and other female relatives. Children would not have been involved in the cutting of bodies, though one of my interpreters remembered sitting with others watching his mother being cut [up] and eaten. So, just as with adults, handling the food was one possible one route of infection, but as I recall, this depended on cuts and scrapes that allowed the infectious agent to enter the bloodstream – which the rest of us agree could not explain the dimensions of the epidemic [1,100 deaths between 1957 and 1968]. That would require a lot of cuts and scrapes, an unlikely scenario.’
In October 1976, fifty-three-year-old Daniel Carleton Gajdusek shared the Noble Prize for Medicine for his research on kuru. Although he was still attributing the disease to an unidentified ‘slow virus’, other scientists had their doubts. By now, with cases of kuru dwindling to a few per year and confined to a ‘Stone Aged society’ few outsiders had ever seen, research on the disease was winding down. Interest in kuru appeared to have run its course, and with it funding for research. Fortunately for the researchers (but unfortunately for a lot of shepherds), scrapie, a disease that mimicked kuru’s destruction of the central nervous system, was beginning to attract more significant attention.
Considering the importance of the European sheep industry it was no surprise that by the early 1970s many researchers, including Gajdusek, were pressing to understand the mechanism behind scrapie. At the forefront of the mystery was the observation that whatever the scrapie-causing agent was, it could not be killed or inactivated by disinfectants like formalin or carbolic acid. Additionally, extracts from scrapie-infected brains lost none of their lethality after being heated, frozen or dried. In another set of experiments, South African radiation biologist Tikvah Alper and her colleagues bombarded the mystery agent with an electron beam from a linear accelerator. Although the beam was strong enough to disrupt the molecular structure of any known pathogenic cell or virus, there was no change in the infectivity of the scrapie extract. The researchers also tried mega-doses of ultraviolet light, a proven disruptor of viral DNA and RNA – all to no avail. The extracts retained their lethality. Alper’s research team soon reached a couple of conclusions about scrapie: (1) it was far smaller than any known virus, and (2) it could replicate without nucleic acids – the chemical rungs of the helical ladder that became Watson and Crick’s model for DNA. This last finding appeared to contradict one of the central tenets of biology – the fact that all organisms require nucleic acids to reproduce.
After reading Alper’s work, English mathematician J. S. Griffith came up with an unusual hypothesis. Perhaps, he suggested, the agent that caused scrapie wasn’t a virus at all but a self-replicating protein. Griffith proposed that this mutant protein could function as a template for the production of additional mutants, each in turn taking on its own role as a template.
Researchers from competing labs scoffed at Griffith’s idea and Tikvah Alper was ridiculed as a female version of virologist/biochemist Wendell Stanley, who had won a Nobel Prize in 1946 for determining that the infectious agent in tobacco mosaic virus was actually a self-propagating protein – a fact that was disproved only after he won the award.
But Stanley Prusiner, a young biochemist from the University of California at San Francisco, read the papers by Alper, Griffith and others, saw an opportunity and jumped into the fray. In the early 1970s Prusiner moved to Montana, where his work with scrapie expert William Hadlow confirmed Alper’s findings about the absence of nucleic acids. Prusiner and Hadlow’s results also indicated that when exposed to substances like enzymes that could destroy or denature proteins the disease-transmitting ability of the scrapie extract was eliminated.
Prusiner tried to tell Gajdusek and the other NIH researchers about what he had found but he was rebuffed. Among the kuru researchers, who were now mostly working on other projects, only Michael Alpers was supportive, inviting the American to the Goroka Institute in New Guinea, where Prusiner studied a group of nine kuru sufferers.
In 1982 Prusiner published his lab findings on scrapie in the journal Science. He coined the name prion (pronounced ‘pree-on’) to describe an aberrant form of protein, which he claimed was responsible for the suite of neurodegenerative disorders known as transmissible spongiform encephalopathies (TSEs). Prusiner claimed that, unlike viruses, prions were not biological entities, but they could be infectious – transmitted orally or through contact with infected material. They could also be inherited or spontaneous in origin.
When asked about why the body’s immune system didn’t appear to mount a defence against them, Prusiner explained that, unlike viruses or bacteria, prions weren’t foreign invaders, they were an altered form of one of the body’s own proteins. Because of this, the body never recognised them as a threat. As a result, prions would spread through the body of a TSE victim unchecked.
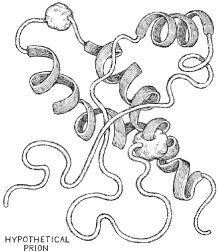
Prusiner hedged his bets by stating that current knowledge did not exclude the potential existence of a small core of nucleic acid within the prions – which might explain how they replicated. Nevertheless, he co-opted Griffith’s protein-as-template model, with his misfolded prion proteins (which were too small to see with even the most powerful microscopes) building up into the amyloid plaques that characterised fatal TSEs like kuru, Creutzfeldt-Jakob disease, TME and scrapie.
For his work on prions, Prusiner won the Nobel Prize for Medicine in 1997, an achievement that provoked a cannibalism-related controversy of a very different form. Some have argued that he should have shared the award with other researchers, pointing to the fact that several people had been bumped out or worse by the American. In his book Deadly Feasts, Pulitzer Prize-winning writer Richard Rhodes wrote that Prusiner ‘invaded and colonized the work of others in his apparent pursuit of a Nobel Prize’. According to Rhodes, Prusiner’s list of enemies grew even longer after accusations that he had used the peer review process to stonewall publication of another researcher’s results while submitting his own paper on a similar topic.
Footnote
1 A US Department of Agriculture term for cows that have become too sick to walk or die before being slaughtered.