Chapter 2. Original 12 Points of Advice and Update
Matt Croughan
Answering questions from friends and family
As mentioned in Chapter 1 I posted points of advice on Facebook, to answer many questions I received from friends and family about COVID-19. There were two sequential posts, the first with 10 points of advice, the second with 2 more. With an update included below, as well as a few minor edits, these posts nicely summarize many of the key points of this book. Although they were originally written for my boomer friends, the message is valuable for any adult concerned about or suffering from COVID-19.
Ten points of advice for boomers with COVID-19
Posted on Facebook April 23, 2020
1. My wife and I both got exposed to the same relatively asymptomatic 20-somethings. She ended up with, at most, one night of mild chills. I had moderate illness for 12 days (like the flu), thought I was recovering, posted my Islay scotch taste test, but then have had 19 days of mostly severe disease since then. So now on day 31 and counting. No hospitalization. Hard to say where you personally will end up in terms of symptoms if you are exposed.
2. If you have symptoms like me, during the worst of it, you will likely spend 18-22 hours per day in bed. Turn your bedroom into a nest, with humidifiers, reading materials, snacks, drinks, and a local electric heater that you control. You will go in and out of awfully bad chills. Also have a humidifier in any other room where you will spend time, such as TV room.
3. You will wake up many mornings feeling pretty good, then Mr. Gorilla will visit, and throw you against the walls until you can barely stand. Then back to bed you go. Repeat this cycle daily.
4. If Mr. Gorilla fails to visit one day, go ahead and take naps, or he will come by for a double session the next day.
5. Hydroxychloroquine (HCQ) and Azithromycin did not provide an obvious benefit to me, maybe because I started them too late. Not sure. They are certainly nothing like a molecular-targeted,
FDA-approved cure, which we will not have for at least 18 months, probably much longer.
6. Good to have a pulse oximeter to monitor your oxygen levels, particularly when sleeping. The best one for that
purpose is the Garmin Vivosmart 4, pictured above. It is available at
Scheels.com
and elsewhere for about $130. Very cool device for health tracking
.
7. Fighting the disease draws a ton of energy. I am eating 1500-2000 calories per day or more and am still losing a half a pound a day. If you do not eat, the fatigue will get even worse, to the point of crushing.
8. To be able to handle the increased oxygen demand with somewhat messed up lungs, I would recommend you get in good enough shape beforehand to be able to aerobically sustain at least 6-8 METs for 30 minutes. I can sustain 9.5 METs at my house (5900 ft elevation) and was able to stay out of the hospital. [8 METS is roughly equivalent to jogging about 5 miles per hour].
9. If your COVID-19 infection moves to your lungs, you might also get a secondary bacterial lung infection and will need antibiotics, like me.
10. If you are really unlucky, you may eventually get bronchospasms, or lung spasms, like me. My first one came out of nowhere, lasted about 2 minutes before I had to Zen my way through it, and the experience was terrifying. I eventually got Albuterol, a wonder drug. You might want to get some in advance.
Some dear friends have done their best to help me through this. You know who you are. Thank you.
Personally, I think the virus has been mutating in my lungs to stay one step ahead of my immune system. Lots of data now coming out in line with that. It does not bode well for vaccines. Such as with HIV, vaccines typically do not work well under that scenario. Hopefully, I am wrong for COVID-19.
My asymptomatic, loving wife and I have things covered. Not sure what would have happened if we both got extremely sick. That would have been an awfully bad scenario.
I really hope you do not get it, or you have few or no symptoms if exposed.
Two more points of advice for boomers with COVID-19
Posted on Facebook, May 6, 2020
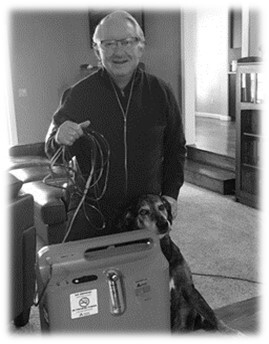
11. We have all seen many reports of hospitals being overwhelmed, with many bleary-eyed doctors and nurses not provided with adequate PPE (Personal Protective Equipment). Accordingly, many of us, including me, have been loath to go to the hospital. As it turns out, that was a huge mistake on my part. As my blood oxygen levels started plummeting about ten days ago, it was either go to the hospital or die (no joke). When we got there, they had plenty of staff, no one was overwhelmed or bleary-eyed, they all had on plenty of PPE and were happy to see me. They put me on oxygen, gave me some IV antibiotics, tested me for every possible complication, and sent me home after a couple days with the oxygen concentrator shown in the picture. It turns out the overwhelmed hospital story is unique to NYC and maybe a few other places. Your local community hospital almost certainly has plenty of room for you and will make sure you neither get infected, nor infect someone else, when you are there. Doctors, nurses, and other healthcare workers are always heroes to me, pandemic or not. That is just who they are. The worst you can do is not let them be a hero for you. That will just lead to lost hospital revenue, more suffering or possibly even death for you, and eventual layoffs of the heroes. Really stupid
12. As it turns out, Mr. Gorilla was well intentioned. After I got out of the hospital, he came by for one last visit. He noticed that my blood oxygen levels were back in the 90’s. He smiled, picked me up, cradled me to sleep, and gently laid me down in my bed. I woke up with a banana at my bedside. It turns out, all that throwing me around the room, when my blood oxygen levels were in the 80’s, were his attempts to make me go to the hospital. I just did not get the message. It would of course been simpler if he spoke English. But now you know the translation. If you are feeling very fatigued, or your blood oxygen levels are consistently below 90 or 92 percent (range of recommendations), you need to go the hospital, whether you have perceived shortness of breath or not.
So that is my final advice, my friends. I shuffle around the house in a starfish pattern, with my 50-foot cord attached to the concentrator and oxygen flowing into my nostrils at 3.5 liters per
min. I feel pretty good except when I get up to go to the bathroom, which is quite exhausting (pulse jumps above 130 bpm and breathing rate jumps to over 30 per minute). I have had a 100 F fever for weeks that seems to be breaking a bit today. My wife Kathy is happy to no longer see her husband marching toward the grave. She was the one that forced the hospital visit. My most common phrase is now “thank you, dear”, a reflection on my semi-helplessness and her love
❤
️
Thanks again for all the prayers, well wishes, as well as lots of great advice from my sister Mary, brilliant and ever-loving doctor friend Tom Stodgel, and many of you.
❤️
Update to Facebook posts with key message
The key message is illustrated in the graphic below. It shows the trend over time on my symptoms from COVID-19. Before I went to the hospital and started on oxygen therapy, I was losing my battle with COVID-19. With some ups and downs, my symptoms were progressively getting worse.
After starting oxygen therapy, I have been slowly winning my battle. With some ups and down, my symptoms have progressively diminished. For me and many people, oxygen is the wonder drug for COVID-19.
If you are starting to suffer substantial symptoms, do not delay going to the hospital, having your blood oxygen level checked, and starting on oxygen therapy if needed. Starting oxygen therapy early is important, so it can still be delivered through a simple nasal cannula or mask. You do not want to be so bad off you need to be put on a ventilator.
Oxygen therapy, as well as the use of pulse oximeters, will be covered in in Chapter 8.
With regard to the virus mutating in my lungs, as mentioned in my Facebook post, I no longer believe that was likely the case. I now believe I cleared the virus within 2-3 weeks of symptoms but then got a secondary case of bacterial pneumonia. This will be discussed further in Chapter 11.
With regard to hospitals being at capacity or overwhelmed, such situations have now occurred at more places beyond New York and New Jersey, but still only at certain locales (often urban) over limited periods of time. These situations are certainly of serious concern. The heroic activity of many staff has been impressive.
All that said, such situations have so far proven to be relatively rare among the many thousands of hospitals in the US. In the second quarter of 2020, there were far more scenarios wherein hospitals in the US did not have enough patients and potentially faced staff layoffs.
Many people avoided hospitals because they mistakenly thought their local hospital was at full capacity or overwhelmed. Even if their hospital was at full capacity, they may well have been rerouted to a hospital with available capacity. Many hospitals now have strong protocols to avoid cross-contamination of COVID-19 between
patients or between patients and staff.
If you do need oxygen but go to the hospital early on, with only moderate symptoms, you could well be out of the hospital quickly. You could be discharged possibly within a day or two, or even in the afternoon of that first day.
If, instead, you wait until you are quite bad off, you may be admitted directly to the Intensive Care Unit (ICU). If so, there is a good chance you will occupy one of those beds for many days, and thus contribute to any potential ICU overcrowding problems.
Wait too long and you may have a similar experience to the 41-year-old famous actor Nick Cordero. You may need to be quickly put on a ventilator and suffer similar fates as him, including leg amputation, over 90 days on a ventilator, and, very sadly, death.