Chapter 3. First-Hand Advice for Caregiver and Update
Kathy Croughan
Introduction from Jess Croughan, Co-Editor
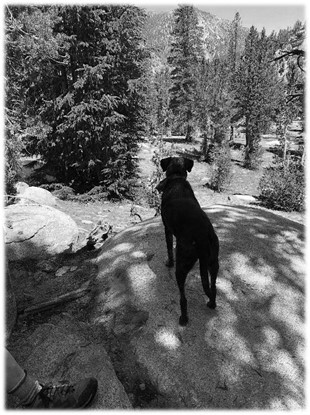
The following passage is a social-media post made by Kathy Croughan, Matt’s wife and my mother. Kathy served as Matt’s primary caregiver throughout his COVID-19 ordeal. The post below was made partly to provide advice for other caregivers and partly to as a cathartic way to help Kathy move past this difficult time. As you can see from the photos, Kathy and our dog Cookie have a mutual caregiver relationship
This chapter serves two purposes. One, to provide useful advice for caregivers. Two, to show you a snapshot in time of a caregiver going through this experience. Through these twelve points of advice, we hope you will see just how much of a family disease COVID-19 can be and how it takes a whole family to get through it well.
Some of this advice is no longer as relevant today as it was then. For instance, tests are far easier to access now than they were. Most of the advice though, can be applied to all caregivers. Even if you are not a caregiver, we believe this chapter will demonstrate the importance of being prepared. If you do not prepare or act properly, the consequences could fall on not just you, but the people you care about.
Twelve points of advice of the caregiver
Posted on Facebook May 28, 2020
As a follow-up to my husband’s advice for boomers with COVID-19, this is the other side…the Spouse’s or other Significant Other’s survival tips for caring for/living with someone with extended COVID-19 symptoms and its possible aftermath. By the way this is 5 weeks after Matt’s original post and 10 weeks into the disease.
1. The still unanswered question is why some people are asymptomatic. If you are, when are you “hot” and for how long? I am one of the lucky ones to not have the disease, but have had the opportunity to be a caregiver, without much advice to go on. Fortunately, I never stopped being able to smell, so never stopped enjoying scotch, or my nightly “Tequila Time”.
2. In the beginning, as there is no advice as to what to do because no one knows anything, you just hope that the patient will weather the COVID-19 storm, and it will all go away. The patient, mine at least, had a few days of grouchy old man syndrome, chills and extreme fatigue. He was starved, but mainly wanted to eat carbs - usually some form of potatoes. He went from anosmia (couldn’t smell) to being super sensitive to smell, especially normal things like soy sauce and tomato sauce. Now some smells can trigger bronchial or lung spasms. So much for the creative-cooking-during-quarantine project!
3. You do start to get a little paranoid as there are horrible rumors (not necessarily wrong) that they could asphyxiate. I relocated to one of our guest bedrooms so that we wouldn’t disturb each other. Unfortunately, if something bad happened during the night I might not know. So I would get up in the morning, waiting for the coughing sessions to begin, relieved at first because then I knew he was still breathing. But then there were the hacking sessions, which were heart wrenching. I really did think he was hacking up a lung. Repeat every morning. Did I mention we’re in week 10?
4. If you have a patient that is in this state, my best advice is to not let them have work video chats or any other contact with humans that takes any energy at all. Because they, and you, will lose precious ground you have gained. This is particularly challenging for an extrovert like my dear husband.
*Also, and this is extremely specific, if you take your nearly deaf dog on an off-leash hike, keep close track of her. I lost track of Cookie, and nearly had a nervous breakdown, because on top of Matt having taken a turn for the worse that morning, I thought I had lost her. She was waiting for me at home, but my imagination took me to a dark place in the meantime. This is not the time for random risk taking. (The dog and I keep better track of each other now)
5. There may be people who recommend various cures. At least, at this time, there are no miracle drugs. Once you are “fortunate” enough to move onto regular pneumonia you are in more familiar territory for doctors, but advanced pneumonia takes time to recover from.
6. While Matt has various scientific devices to track his status, we failed to have a working thermometer, as it had been so long since we needed one. If you don’t have one, start looking for one now!
7. Yes his appetite increased greatly, but he was very picky about what he wanted to eat and couldn’t eat a lot at once. So… to avoid calorie crashing, encourage them to eat every 2-3 hours, in order to avoid running out of calories. He ate a lot of bananas. As the caregiver of an adult male it is impossible to know exactly what he ate and when… so good luck managing that. In Matt’s case he craves all the things a 17-year-old would, which isn’t heart healthy or nutrient dense, but is calorie dense. Anemia is a problem, so steak is back in the dinner line-up.
8. As with general adult success, it doesn’t hurt to be in shape.
9. Yes. Maybe the pneumonia could have been avoided by earlier intervention by doctors. But here is the “Schrodinger’s Cat”
problem. (It’s a physics thing). Doctors can’t treat you for COVID-19 until you have a positive COVID-test, and you have to make the case with the appropriate symptoms to merit having a test done. If you do have COVID-19, there isn’t much they can do, except manage the symptoms, but if they aren’t too bad, and you know for sure you are not short on oxygen (hypoxic), you might as well stay home. Also, by the time you’ve convinced “them” you might have COVID-19, you may have cleared it, so your test is negative. But now “thankfully” you have pneumonia, and THAT they can treat.
10. Bronchial or lung spasms are a red flag it may be time to go the hospital.
11. Don’t be afraid to go to the hospital. We tried to manage things at home which meant phone calls to doctors and many trips to 4 different pharmacies, (some were stocked out of certain drugs). Ultimately hospitals, even if they are overwhelmed, have many more resources at their disposal – monitors, drugs, oxygen, testing labs, medically trained staff on duty 24/7. No, they don’t have all the answers about COVID-19, but if they deem you stable and send you home, you got a bit of a stamp of approval that you won’t die. As a spouse it’s a little nerve wracking not being able to visit or talk directly to the doctors, and rely on your somewhat brain-foggy spouse to give you all the information you need, but it is reassuring they don’t want your loved one there because someone else could use the hospital bed more. Also most hospitals outside of dense urban areas are underwhelmed. When we went to the ER, staff met us at the door and promptly escorted Matt in.
12. Finally, take care of yourself, whatever that means for you. For me I worked through a fabulous Bible study I was supposed to do with my Women’s group. I danced when I could, did A LOT of gardening around our beautiful house in the forest, kept the fountain and feeders going for the local birds, photographed the deer and bear, took the dog out on her daily walk or hike, and prayed a lot. It was wonderful watching spring emerge, as birds and wildlife returned, and plants came out of dormancy. Nature
wasn’t on lock down. I limited my exposure to media, social and otherwise. Media exists on fear, making things seem as bad as they can possibly be, focusing on horror stories. I didn’t hear one story about people who had COVID-19 symptoms and just got better. Social media at first was positive, but then turned darker as quarantine wore on. (Sorry to those of you who offered me a challenge that I didn’t accept.)
One thing my husband did, being the extrovert that he is, was to send out a plea to my social network to call me. I heard from many friends I don’t see often, and that was a huge help and comfort. COVID-19 is evil and will mess with your head if you let it, even if you’re not the one with symptoms- maybe especially if you’re not the one with symptoms.
The happy ending here is that we are living through it! Unfortunately, 100,000+ did not.
I am grateful my lungs work, and just enjoy breathing. I am grateful for having a supportive church (actually two prior churches were in the prayer mix), loving friends, and a big beautiful house in gorgeous surroundings. Also for Cookie who makes sure we get out every day, and my son James who stayed for three weeks at the beginning, and was here last week. And for a loving spouse who is still alive. As always it’s good to count your blessings, of which I have an abundance.
Hopefully none of you will need this advice, I pray. If you are unfortunate enough to get it, I hope your recovery is quick. If not this in my best advice from what I’ve learned. Good luck.
I will add one final word not included in my original post. You are fighting a battle here and it is important to manage expectations.
This disease is cyclical, there are bad days and better days. Matt didn’t expect to be sick for 6 months or more, so when he started feeling better, he assumed he was finally on the mend and wanted to do things, like have Mother’s Day dinner with me, or exercise.
You need to protect them from a relapse and yourself from disappointment. So, discourage them from “pushing it”. Live in the moment and be happy for whatever progress is made. Once again, don’t be afraid to take them to the hospital.
And remember, Cookie is rooting for you.
Part 2. What to Expect and How to Prepare