Chapter 6. COVID-19 and Well Being
Mary Flanigan and Dee Villarreal
There are so many unanswered questions regarding COVID-19, but what is known is that wellness is key in dealing with any illness a person may face. A healthy diet, exercise, proper rest, annual preventative health screenings, and good mental health cannot prevent COVID-19, but can certainly play their roles in a more favorable outcome.
As you may remember, carrying any of the underlying risk factors mentioned in Chapter 4, such as obesity, diabetes, and hypertension, can increase a COVID-19 patient’s risk of death over 10-fold. The topics covered in this chapter are aimed to help you reduce your risk of a severe infection or death. Even though you may not be able to remove those pre-existing conditions, staying healthy in other aspects of your health may help reduce their negative effects.
Additionally, it must be understood that there are both modifiable and non-modifiable risk factors to our overall health. For example, at this time, no one is able to modify our genetics. Perhaps that day will come soon or in a few decades.
For now, everyone must manage with the cards we are dealt. Fortunately, beyond diet and exercise, there is an ever-expanding toolbox of medicines available to help us overcome our genetic weaknesses, such as susceptibility to diabetes, high blood pressure, and high levels of low density (bad) cholesterol.
Vascular Disease
COVID-19 can impact many organs and systems in our body, including our blood vessels. According to the New England Journal of Medicine,
“Histologic analysis of pulmonary vessels in patients with covid-19 showed widespread thrombosis with microangiopathy. Alveolar capillary micro-thrombi were 9 times as prevalent in patients with covid-19 as in patients with influenza.” (Ackerman, 2020)
In other words, patients with COVID-19 were 9 times as likely to have some clotting in their blood vessels.
We (Mary and Dee) like to think of the vascular system as a pipe delivery system with our heart as the pump. Our blood carries nutrients, oxygen, disease-fighting cells, and much more through these pipes to every organ of our bodies. In this chapter, we will discuss ways in which we all can keep our “pipes” clean and strong for an efficient delivery system for everything our bodies need to thrive when healthy or ill. Before we do that, we shall first discuss the impact of exercise on our immune system.
Exercise and The Immune System
At this point and to our knowledge, there is no published data about the effects of exercise specifically for COVID-19. But we can make speculations from past studies involving exercise, the immune system, and other illnesses, such as influenza and other Upper Respiratory Tract Infections (URTIs).
Nieman provides an excellent and thorough review on exercise, the immune system, and infectious disease (Nieman, 2000). We summarize certain key messages from his chapter here.
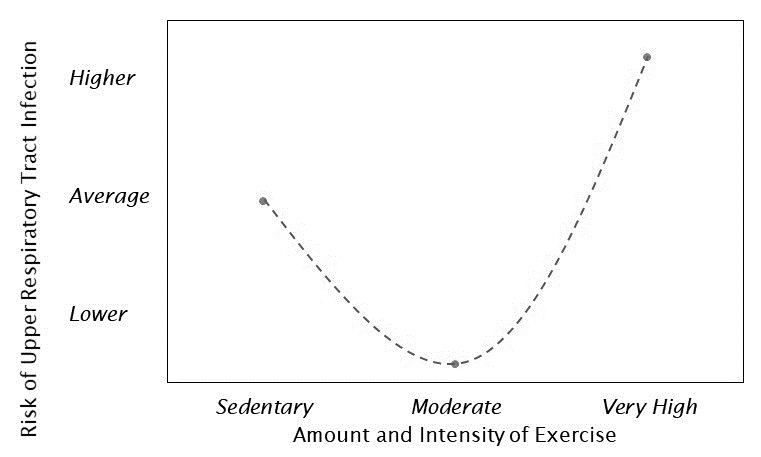
It has been proposed that the relationship between exercise and Upper Respiratory Tract Infections can be shown as a “J-curve”, as illustrated below.
In brief, moderate exercise provides the lowest risk of Upper Respiratory Tract Infections (URTI). The risk increases if you either have a sedentary lifestyle or have recently engaged in prolonged heavy endurance exercise. This ‘Very High’ intensity refers to something that would require a significant recovery period, such as a marathon. This would not apply to a person improving their health through a mix of moderate and vigorous exercise, as discussed further below.
Participation in competitive sports can potentially make you more susceptible to illness. This is due to close contact with other players, as well as any associated stress, increased travel, and calorie shortages.
These risks are additive with any immune suppression from the “Very High” exercise referenced above. Vigorous prolonged exercise while suffering from a strong viral infection can inhibit recovery and potentially cause death.
Some athletes suffer from post-viral fatigue syndrome. The associated symptoms can persist for up to several months. There are many symptoms, including lethargy and easy fatigability, made worse by prolonged endurance exercise. For further information on these topics, the reader is referred to the chapter by Nieman as well as his subsequent publications (Nieman, 2000).
Exercise and Vaccine Effectiveness
An important study to note is one performed by Dr. Jeffrey A.
Woods and his team at the University of Illinois at Urbana-Champaign. The study also reveals the effects of consistent exercise on the effectiveness of the influenza vaccine. When asked about the parallels between coronavirus and his previous work, Dr. Woods responded to the Journal of Sport Health Science:
“We also did a large study …in older adults, …We found that regular, moderate cardiovascular exercise could extend the protective effect of the annual influenza vaccination … throughout the entire influenza season” (Zhu, 2020)
In other words, older folks usually do not get the full effect of the flu vaccine, but they did with exercise! The results of this study likely extend to everyone, and they indicate that exercise can potentially reduce symptoms and/or improve the effects of any future vaccine.
Recommended Amount of Purposeful Exercise
According to the U.S. Department of Health and Human Services, 35% of all adult Americans have a preventable
chronic disease, influenced by lack of physical activity (USDHHS, 2020).
The physical activity they are referring to is exercise. Most of us know they should exercise to stay healthy, but exercise may not be what you think it is.
After years of working in Intensive Cardiac Rehab, we can’t tell you how many times we have heard things like “I exercised today…. I gardened for two hours pulling weeds”. Sorry, but gardening is not actually exercise. Exercise needs to go beyond
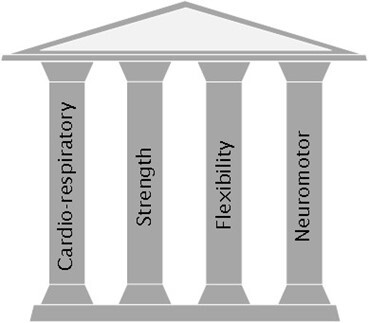
the activities of daily living and work on one of the main pillars of physical health, shown to the right.
The body adapts to the repetitive tasks we do daily, which is why you can see morbidly obese people who walk around all day. Simply put, being physically active is no replacement for purposeful exercise.
But how much is enough? The American Council of Sports Medicine recommends adults get at least 30 minutes of cardio-respiratory exercise a minimum of 5 days a week for a total of 150 minutes of such exercise per week.
Flexibility exercises are recommended at least 2 days per week. You might think you are exempt from these recommendations if you have a physical job, like lifting plants in a nursery all day. Unfortunately, you are out of luck. Do your best to find 20-30 minutes where you can exercise, to get in those 150 minutes per week (Garber, 2011).
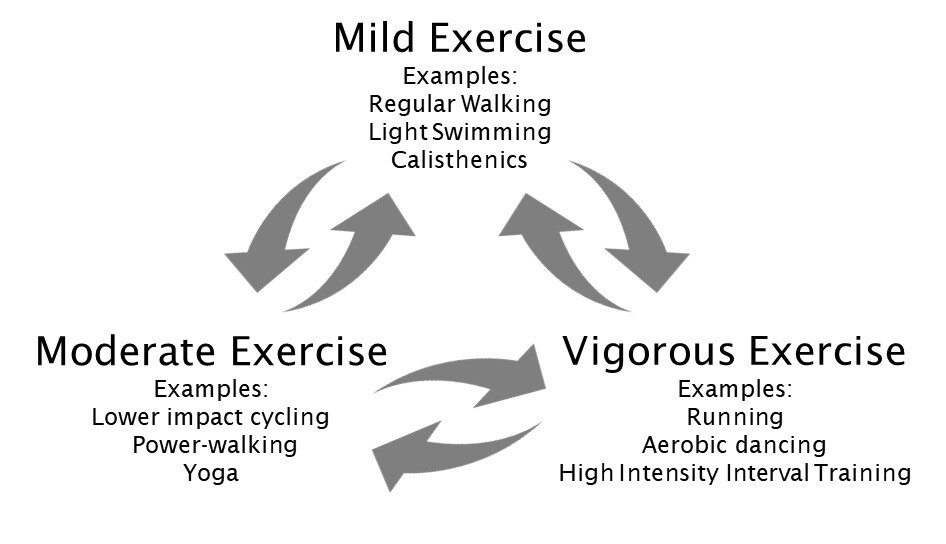
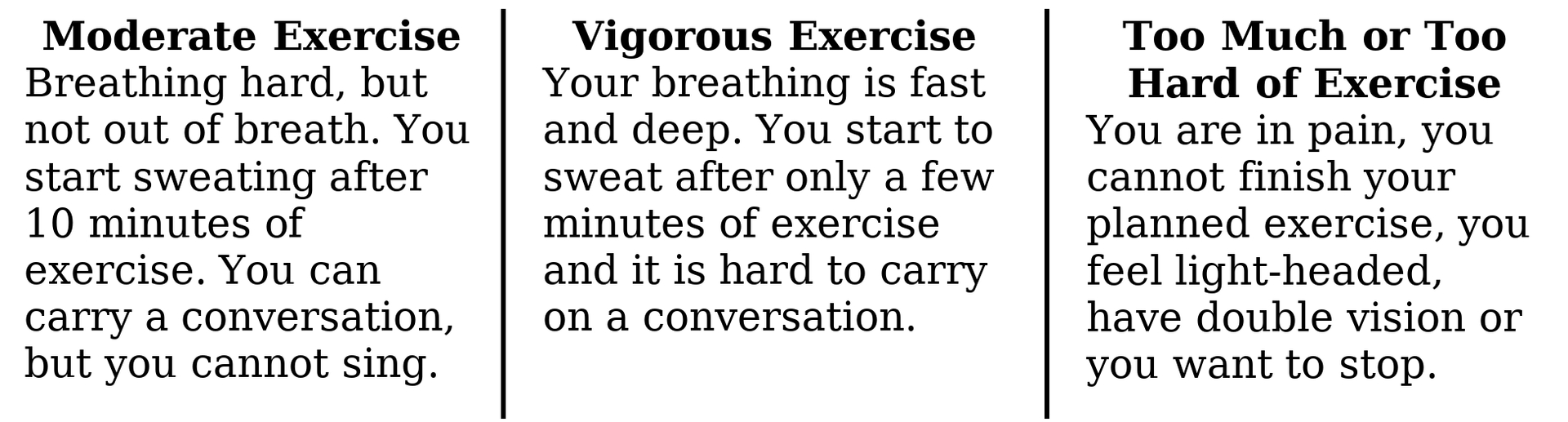
Appropriate Qualitative Level of Exercise
The American Heart Association generally recommends a moderate or vigorous intensity of exercise for maximum benefit. For weight loss, the more intense or longer your activity, the more calories you burn. For an extra benefit, someone could aim for 300 minutes a week of exercise.
Weight loss may be one of the largest benefits of exercise to improve COVID-19 outcomes. One study measured that over two times as many obese patients had severe COVID-19 infections than non-obese patients (Gao, 2020).
NOTE-ALWAYS CONSULT WITH YOUR PHYSICIAN PRIOR TO STARTING AN
EXERCISE PROGRAM.
Injuring yourself is counter-productive, so you need to know how to gauge your effort. If you are just starting an exercise routine, many people avoid injury by limiting themselves to just mild exercise for the first few sessions. Many such people then move up to moderate exercise and eventually to a mix of moderate and vigorous exercise.
On top of avoiding excessive exercise, you can reduce injuries by
utilizing mild exercises at the beginning and end of your routine. They allow your muscles to prepare and calm down, respectively. Lots of mild exercise to start and finish, along with stretching, are especially useful for those who are sore from prior workouts or for older folks, as these individuals are more prone to injury.
Appropriate Quantitative Level of Exercise
Another way to gauge your exercise, if you are more quantitative and adventurous, is to utilize your Target Heart Rate Zone (THR). A quick web-search can quickly teach you how to estimate your THR. THR can diverge strongly based on your personal health situation. THR is based upon a percentage of your estimated maximum heart rate (MHR).
NOTE-ALWAYS CONSULT WITH YOUR PHYSICIAN ABOUT YOUR MAXIMUM HEART RATE AND TARGET HEART RATE ZONE FOR EXERCISE.
Your maximum heart rate (MHR) can be estimated from the formulas:
MHR = 220 – your age
for most people
MHR = 210 – half of your age
for certain athletes
Once you know your MHR, you can use the guidelines from the American Heart Association to estimate your THR. As shown in the
graph below, your THR is a percentage of MHR: 50 to 70% for moderate exercise, 70 to 85% for vigorous exercise. Note however, that medications, such as those that affect your heart rate, can change your THR. Thus, as recommended above, you should always discuss your THR with your physician prior to starting an exercise program.
Things to remember about exercising
1. Exercise is different from physical activity. Exercise has a specific goal to increase one’s fitness and health.
2. There can be too much. Some studies have shown working out intensely for extended periods starts to lose the benefit of a stronger immune system (Simpson, 2016), as also expressed in the “J-curve” figure above.
3. Make a habit, mix up your routine and try things like prioritizing it in the morning, “Earn your shower”.
4. Keep it realistic and safe. Injuries are counter-productive and every baby-step towards better health is a success.
A Healthy Diet
Nutrition is complicated. Even the leading experts constantly debate on what is best. But they all agree diet can affect all aspects of your health, not just your weight. They also agree that certain things represent problem areas for almost all of us.
The best example is sugar. Sugar is a treat and should be considered as such, to be eaten on occasion and in moderation. Many studies have confirmed sugar causes inflammation and fat
build-ups that clog our arteries. These build-ups not only harm our vascular health, but also reduce our immune system’s ability to fight infections, such as COVID-19. Sugar can be tricky because it is snuck into foods that may seem healthy, like salsa and whole wheat fiber bread. Check those labels!
There are some useful examples though. Recently published nutrition information from, A Clinician’s Guide to Healthy Eating for Cardiovascular Disease Prevention
states
“The Dash Diet, Mediterranean Diet, and Vegetarian Diet are the most evidence based with regard to cardiovascular disease prevention and weight loss. Furthermore, a diet rich in healthful plant foods and fish is associated with low risk for CVD.” (Pallazola, 2019)
Because we are nurses working in Intensive Cardiac Rehabilitation, we have had the opportunity for a tremendous amount of training and education, including at the Pritikin Longevity Center (Exercise, Diet, and Stress Center). We have seen major improvements in energy, fasting glucose, lipids, and body mass index in our patients and in ourselves when following a healthy diet such as the Pritikin diet which is similar to the plant-based diets mentioned above.
The Pritikin Diet focuses on vegetables, fruits, unprocessed whole grains and small portions of lean animal proteins. We have seen and experienced how well the plan works for cardiovascular health. The Keto diet plan is another popular diet that you can consider, with your doctor.
“Dietary patterns focusing on low intake of carbohydrates at the expense of high intake of animal fat and protein may be associated with increased all-cause mortality when used for extended periods.” (Pallazola, 2019)
Having a healthy diet is essential when dealing with COVID-19 as it seems to affect those with comorbidities. A healthy diet can boost the immune system and can create a body that is more resilient when it comes across illness.
We like to think of food as a fuel. Take the time to look at your food and think about it.
•The animal that you are eating, was it a healthy strong animal?
•Is this food suspiciously salty and sweet, did you check the label?
•How fresh are these foods, are they bright in color? Think about what you are putting through your pipes, you owe that to yourself.
Getting Enough Sleep
Sleep is something that many people take for granted or overlook. Many of us do not get enough hours of sleep a day, or the hours we are trying to sleep are interrupted. Sleep is significant for our bodies, including our immune systems, to repair themselves, after the wear and tear of the day.
The Centers for Disease Control and Prevention (CDC) recommends that adults aged 18-60 get 7 or more hours of sleep a night (CDC, 2019). If you or someone you love has frequently interrupted sleep, excessive snoring, or never feels well rested upon waking, encourage them to see their Primary Care Physician.
There is plenty of evidence demonstrating the value of sleep in preventing and recovering from COVID-19. A 2012 study titled “Sleep and Immune Function” pointed out the illuminating data.
Intriguingly, the data consistently demonstrates that sleep enhances the adaptive immune response against an invading antigen (such as COVID-19). After 4 weeks, subjects who got enough sleep on just the first night after vaccination had twice as many antibodies (which your body uses to fight infection) as subjects who did not get enough sleep. This study shows us that a single night of normal sleep after vaccination strengthens our natural immune response against an invading antigen (such as COVID-19), to a clinically relevant extent (Besedovsky, 2011).
This data comes from a Hepatitis A vaccine study, but we can theorize that this would also be true when the SARS-CoV-2 (Coronavirus 2019) invades our systems and that sleep is the reinforcement our immune system needs to help us avoid or fight off any virus.
Mood and Mental Health
An important aspect in illness prevention and healing is having an awareness of our mental health, in other words, what are our thoughts and minds consumed with?
It is well known our bodies and minds are connected. If we are feeling stress, anxious-ness, and/or depression it can lead to making bad dietary choices, restlessness, poor sleep habits, and lack of motivation to exercise. These are all things we have talked about being significant to dealing with COVID-19. Chronic stress has also been shown to weaken almost our entire immune system (Segerstrom, 2006).
Basically, an unhealthy mind leads to an unhealthy body. It is important to seek out a positive environment: people who are uplifting and supportive to you, hobbies you enjoy, and some sort of stress outlet.
Activities like puzzles, playing cards, drawing, reading, deep breathing, prayer, meditation or taking a relaxing walk out in nature are just a few suggestions that could ease the tensions of your day. Additionally, try avoiding activities if they are causing you anxiety or stress, such as frequently monitoring the news.
If you have not heard about the “Blue Zone” study, we highly encourage you to discover it by looking it up. The study found that some of the longest living people on Earth shared the commonality of community, stress management, belonging and purpose, to just name a few. To treat your body right, you must first address your
mind (Buettner, 2016).
Deep Breathing
There is plenty of evidence that suggests that deep breathing is a healthy and essential practice that improves overall well-being. When discussing how deep breathing relates to COVID-19, it is all about overall wellness.
Anything we can do in our daily lives to keep our bodies healthy will increase our survivability when dealing with an illness. As part of how we help rehabilitate cardiac patients in Intensive Cardiac Rehab, we cover stress management. In this topic, we teach patients deep abdominal breathing techniques.
Deep breathing can relieve stress by decreasing the release of stress hormones. This can boost immunity, reduce the heart rate, and reduce blood pressure. As Dr. James Hoyt, a pulmonologist explains,
“Though it may feel unnatural to breathe deeply, the practice comes with various benefits. Deep breaths are more efficient: they allow your body to fully exchange incoming oxygen with outgoing carbon dioxide.”
When practiced regularly, deep abdominal breathing can lead to beneficial changes in health. An article from Harvard Health Publishing, Harvard Medical School (July 6, 2020) supports that:
“Deep abdominal breathing encourages full oxygen exchange — that is, the beneficial trade of incoming oxygen for outgoing carbon dioxide. Not surprisingly, it can slow the heartbeat and lower or stabilize blood pressure.”
There are several ways to practice deep breathing. You can count inhalations and exhalations, expanding how many seconds you can breathe in and out. While laying down, you can place one hand on the belly and one on the chest and practice inhaling till the hand on your abdomen rises well above the chest. You can follow a guided breathing exercise on YouTube or a phone app. James Nestor writes a great book named “BREATH” where he reveals years of breathing history through science and cultures.
Breathing is one of lowest effort the ways to boost our overall
health but is easily forgotten. You can start literally right now, and you can do it anytime and anywhere.
Regular Visits with Your Doctor
Last but certainly not least, you must regularly check-in and have a good relationship with your Primary Care Physician (PCP). You could well address everything we (Mary or Dee) have mentioned above, but the support and guidance of a good healthcare practitioner is also integral to your long-term health.
Your PCP can ensure that you are having your annual recommended health screenings such as blood work, mammograms, or colonoscopies. Remember those genes which you cannot control? Those tests make sure nothing sneaks up on you. Your PCP should be your coach and guide you in making decisions about your health, recommending supplements, and finding the right medication to use when necessary. You will want the help if you come down with a COVID-19 infection. Wellness is key when it comes to preventing disease, managing disease and/or treating disease.
Treat yourself well.