The practice of medicine began long before the advent of written records. Prehistoric people in every culture had ideas on the causes of illness, often placing responsibility on gods, evil spirits, or angry ancestors. To cope with pain and disability, they tried various remedies, ranging from magical incantations to rational strategies.
More than 10,000 years ago people practiced trepanation: a hole was made in the skull bone, possibly in hopes of alleviating the effects of head injuries or symptoms of mental illness. Otzi, the Iceman, who lived some 5,300 years ago and whose mummified body was discovered in the Italian Alps in 1991, appears to have been familiar with a natural antibiotic. He was carrying the fruit of the fungus Piptoporus betulinus, which contains oils toxic to the parasitic whipworm Trichuris trichiura. An autopsy of the Iceman’s body revealed that his intestine was infested with Trichuris eggs. The history of medicine is the story of innovation emerging from the human desire to extend life and eliminate physical suffering.
Medicine in Antiquity
Beginning around the time of the Iceman, civilizations formed in the Middle East and people started to use numbers, pictures, and words to record information. The scientific study of medicine began as slowly information was disseminated from one healer to another and from one civilization to another.
Mesopotamia Clay tables from early civilizations in Mesopotamia contain diagnostic treatises with subsections covering gynecology, pediatrics, and convulsive disorders. Skin lesions, venereal disease, and fevers were described, and some of the described treatments were similar to modern treatments for the same conditions. Surgeries were performed and the earliest known legal code, the Code of Hammurabi, composed by the ruler of Babylon around 1700 B.C., included laws pertaining to the liability of physicians who “used the knife.”
Egypt Papyruses from ancient Egypt, dating from 3000 B.C. to 1200 B.C., include methods for diagnosing pregnancy and the sex of a fetus, accurate descriptions of diseases, and rational treatment of various diseases. Particularly well known are the Ebers Papyrus (ca. 1550 B.C. but possibly based on papyri dating back to 3000 B.C.), which describes a wide range of diseases plus more than 700 remedies, and the Edwin Smith Papyrus (also ca. 1550 B.C.), which details 48 surgical cases of wounds of the head and upper body, showing particularly astute knowledge of fractures.
Greece In Greece, nonmagic medicine based on empirical knowledge emerged around 500 B.C. Hippocrates (ca. 460–ca. 377 B.C.), today often referred to as the “father of medicine,” is credited with establishing medicine as a scientific undertaking. He wrote the first clinical description of diphtheria, recognized that tuberculosis occurs most commonly between the ages of 18 and 35, and stated “those naturally very fat are more liable to sudden death than the thin.” The Hippocratic Oath, dating from around the time of Hippocrates, pledges physicians to do their best for patients, to avoid doing harm, and to keep secret information about their patients; it continues to serve as a code of conduct for today’s physicians.
Around 300 B.C., the Greek physician Herophilus (ca. 335–280 B.C.), who practiced in Alexandria, Egypt, where dissections of human corpses were permitted, founded the first school of anatomy. He differentiated between sensory and motor nerves and established that the brain is the center of the nervous system. He made important observations about organs such as the liver and ovaries, and he invented a water clock to measure the pulse of arterial blood.
Rome By the beginning of the Christian era, the Romans had created a widespread empire that included lands from Gaul (France) through Greece and as far east as Syria. But the center of their empire, Rome, was crowded, dirty, and the frequent victim of epidemics of smallpox, bubonic plague, and other diseases. The Romans adopted important public health measures, building aqueducts to bring freshwater into the city and sewers to carry away wastes. Public baths were established to encourage personal hygiene and special buildings were set aside for care of the sick. War injuries advanced surgery: Roman surgeons could surgically
reduce limb fractures, tie ligatures around blood vessels, and cauterize wounds to stop bleeding.
The most influential physician of ancient Rome was a Greek, Galen of Pergamum (ca. 129–ca. 216). He used pulse readings in diagnosing problems, showed that different parts of the spinal cord control different muscles, and demonstrated that arteries contain blood, not air as had been believed. But his misconceptions were many. For instance, he stated that pores connect the two sides of the heart and the liver is the main organ of the blood system. In his 300 known writings on physiology, anatomy, disease, and drugs, over half of which have survived, Galen brought together his ideas and those of predecessors and contemporaries. For more than 1,400 years, these writings were considered infallible and were the basis of medical education in Europe.
Medicine During the Dark Ages
Following the collapse of the Roman Empire in the fifth century, medical knowledge withered in Europe. Religious teachings about the causes of disease—and about other knowledge—were paramount; questioning these teachings risked charges of heresy and blasphemy. Dissections of human corpses were forbidden and experimental investigations suppressed. The great pestilences of the period were considered the will of God. Infirmaries were founded, but they were crowded, unsanitary places where care consisted of little more than kindness to the dying.
Arabic Contributions Meanwhile, Arab physicians preserved, adopted, and expanded on the rational ideas of the ancient Greeks and Romans. Persian scholar ar-Razi (Rhazes: ca. 860–ca. 925) was the first to write a scientific paper on infectious diseases and the first to describe smallpox; he used opium as an anesthetic, plaster of Paris for casts, and animal guts for sutures. His multivolume al-Hawi (Comprehensive Book) included all the medical knowledge of the time, including work handed down from earlier times. Beginning in the late eighth century, hospitals providing both medical care and medical apprenticeships were opened in major cities in the Empire. Another vast encyclopedia of medical information, the Qanum (Canon of Medicine) was written by another Persian polymath, Ibn Sina (Avicenna, 980–1037), who recognized that tuberculosis is a contagious disease and that some diseases are spread through water or soil. In the Islamic empire, medicinal plants were avidly collected; the number of drugs used to treat illness increased greatly and pharmacy became a separate vocation.
The Renaissance Through the 18th Century
In the 12th century, the first medical school in Europe was established in Salerno, Italy, and was so influential that the Holy Roman Emperor Frederick II decreed that anyone who wanted to practice medicine had to be approved by the masters of Salerno. A revival of learning took place in Europe beginning in the early 13th century. Classical medical texts as well as works by Razi, Ibn Sina, and other Islamic scholars were translated from Arabic or Greek into Latin, and physicians such as Taddeo Alderotti (1223–95) urged their colleagues to read these texts. Major centers for the study of medicine opened in Paris and Montpellier in France and Bologna in Italy.
By the end of the 1400’s the Renaissance was well under way. The invention of printing in Europe led to books on surgery and medicinal plants. Experimentation became more common, as did dissection of human corpses. Seafaring explorations also influenced medical history—for instance, a monk who accompanied Christopher Columbus described for Europeans how Native Americans smoked tobacco for medicinal purposes; sailors introduced smallpox to the Americas and brought syphilis into Europe.
Anatomy In the 16th century, as religious prohibitions against human dissection were lifted, the modern study of anatomy began, allowing scientists to distinguish between abnormal and normal anatomical features. Andreas Vesalius (1514–64), a Belgian physician, dissected human and animal cadavers, demonstrating that Galen’s descriptions of human anatomy were based on the dissection of animals whose structure differs markedly from that of humans. In 1543 Vesalius published De Humani corporis fabrica (“On the Structure of the Human Body”), the first work to accurately illustrate human anatomy.
Gabriele Falloppio (1523–62), a student of Vesalius, described the tubes between the ovary and the uterus, now called Fallopian tubes, as well as previously unknown structures in the skull and inner ear. Bartolomeo Eus tachio (1513–74) described tooth structure at different ages and the tube that connects the middle ear to the back of the nasal cavity, today known as the Eustachian tube. Hieronymus Fabricius (ca. 1533–1619) helped found embryology. He compared the anatomy of embryos of dogs, cats, horses, and humans, and was the first to describe the placenta. He also provided detailed descriptions of the semilunar valves in blood veins. This led to the
discovery of blood circulation by his student William Harvey (1578–1657). Harvey’s Anatomical Study on the Movement of the Heart and Blood in Animals, published in 1628, accurately explained that the heart pumps blood into arteries, the arteries carry the blood throughout the body, and the veins return the blood to the heart.
This new understanding of human anatomy allowed surgery to emerge as a separate discipline. Previously surgery was performed by barber-surgeons, and was considered a less dignified occupation than medicine. This perspective was changed by Ambroise Paré (1510–90) the leading surgeon in the 16th century, who served four kings and earned the reputation as the “father of modern surgery.” Using the experience he gained on the battlefield, Paré pioneered the use of ligatures and dressings to stop bleeding instead of the painful practice of cautery. Paré is credited with originating the use of prostheses—artificial replacements for a missing part of the body—and popularized the use of the truss for treating hernias, which were previously often “cured” by castration.
One of the most important medical tools, helping physicians understand anatomy and identify signs of disease, was the compound microscope, invented in 1590 by Zacharius Janssen, a Dutch optician. News of this invention traveled quickly, and curious people began studying ever-tinier structures. Marcello Malpighi (1628–94) discovered blood capillaries and nephrons (structures in the kidney where urine is formed). In 1655 Robert Hooke (1635–1703) discovered cells. In the 1670’s, using single-lens microscopes he made himself, Antoni van Leeuwenhoek (1632–1723) became the first person to see blood cells, sperm cells, and one-celled organisms.
Understanding normal anatomy led to the scientific study of diseased organs. This field of pathological anatomy was founded by Giovanni Morgagni (1682–1771), who carefully related his postmortem findings to detailed clinical records of patients’ symptoms. Symptoms came to be viewed as “the cry of the suffering organs” and people with a technical bent looked for ways to detect organ abnormalities in living patients. In a 1761 paper, Leopold Auenbrugger (1722–1809), who recognized that the sounds of lungs full of air differ from those of lungs containing fluid, introduced percussion—tapping on a patient’s chest and listening to the resulting sounds. In the early 1800’s René Laënnec (1781–1826) invented the stethoscope to detect abnormal heartbeats and other chest sounds.
Study of Disease Interest in epidemiology—the causes of disease—developed, nurtured by the epidemics of plague and other diseases that killed huge numbers of Europeans during this period. Paracelsus (Theophrastus Bombastus von Hohenheim, 1493–1541), a German-Swiss physician and alchemist, attacked the widely held belief, handed down from ancient Greece, that disease results from internal disturbances of four bodily “humors” (blood, phlegm, yellow bile, and black bile). He stated that external agents cause disease; for example, in his On Diseases of Miners—the earliest book on occupational diseases—he wrote that inhaling metallic dust causes silicosis (“miner’s disease”). Paracelsus also pioneered the use of chemicals to fight diseases, advocating the use of specific medicines for specific diseases.
The 1546 work De contagione et contagiosis morbis (“On Contagion and Contagious Diseases”) by Girolamo Fracastoro (1483–1553) proposed that epidemic diseases are spread by tiny particles, with contagion occurring by either direct contact, indirect contact via infected items, or without contact from a distance. Fracastoro also identified typhus and gave syphilis its name.
Physiology Modern physiology began with Harvey’s discovery of blood circulation. Also in the 17th century, men such as Thomas Wharton (1614–73) and Regnier de Graaf (1641–73) initiated the study of glands and their secretions. Around 1670 Thomas Willis (1621–75) was the first to recognize diabetes mellitus when he noted that patients whose urine has a sweet taste suffer from fatigue and other symptoms. Later, Luigi Galvani (1737–98) showed that nerves conduct electricity and that electric stimuli cause muscle contractions. Antoine Lavoisier (1743–94) studied breathing, proving that muscles need less oxygen at rest than when working.
Improved Treatment People with a technical bent looked for ways to detect organ abnormalities in living patients. Traditionally, physicians used a collection of basic tools—to deal with patients. In the 1620’s, Santorio Santorio developed the pulsilogium, originally conceived by Galileo, to measure the beats of a man’s pulse. Later, John Floyer (1649–1734) invented a special watch for measuring the pulse. Leopold Auenbrugger (1722–1809) introduced percussion—tapping on a patient’s chest and listening to the resulting sounds—as a way of determining if their lungs were filled with fluid. New medical practices also emerged. Dominique Amel (1679–1730)
invented the fine-point syringe. James Lind (1716–94) discovered that ingesting lemon juice could prevent and cure scurvy, and William Withering (1741–99) discovered the value of digitalis in treating edema and heart disease.
It was in this period that one of the most far-reaching advancements in the fight against disease occurred. In 1796, Edward Jenner, an English surgeon (1749–1823), developed a vaccination against the virus that caused smallpox. Subjects were inoculated with a serum containing material from cowpox—a bovine form of the disease—and were found to be immune from smallpox when they were exposed to it later. Although it took another 50 years to find an effective method of producing this antiviral medication in volume, Jenner’s early work was responsible for eradicating the disease.
In the 18th century, physicians created the foundation for modern hospitals, where treatment and restored health, rather than containment and death, were attainable goals, and the first medical school was established at the University of Pennsylvania, in what would become the United States. At the same time, Philippe Pinel (1745–1826), a French physician, pioneered the humane treatment of the mentally ill, discarding the long-held belief that mental illness was caused by demonic possession.
19th-century Contributions
Medical advances occurred on many fronts during the 19th century. Of fundamental importance was the growing effect on medicine of the scientific method: observing a phenomenon, forming a hypothesis or possible explanation of the phenomenon, designing experiments to test the hypothesis, carefully observing and studying the experimental results to determine if they support the hypothesis—and if not, why not. As a result, many long-used remedies were found worthless or too harmful and were discarded; the use of addictive opium to soothe pain and the use of poisonous mercury to cure syphilis are examples.
The connection between filth and disease was firmly established, leading to improved sanitation and other public health measures. John Snow (1813–58) traced a number of cholera cases to a specific water pump in London—the first time that water pollution was proven to cause illness. More and more communities began treating water supplies with chlorine, first used to purify water in 1800.
The germ theory of disease, which holds that bacteria and other microbes (“germs”) cause infectious diseases, was established independently by Louis Pasteur (1822–95) and Robert Koch (1843–1910) in the 1870’s. In 1879, Pasteur accidentally discovered that bacteria could be weakened, which prevents them from causing disease but still enables them to trigger immunity in infected individuals. Using weakened anthrax bacteria taken from the blood of diseased animals, Pasteur developed the first artificially produced vaccine in 1881. This soon led to isolation of the causative agents of diphtheria, gonorrhea, tuberculosis, cholera, and other scourges—and sounded the death knell for theories that ascribed disease to such factors as spontaneous generation and alien spirits.
In 1892 came the first indication that some agents of disease are smaller than bacteria—indeed, so small that they cannot be seen with light microscopes. The discovery was confirmed in 1898 by Martinus Beijerinck (1851–1931), who named the agents “filterable viruses.”
Diagnostic Advances Diagnoses became more accurate as physicians applied new knowledge of human anatomy and physiology. In the 19th century scientists recognized that all organisms are composed of cells. Charles Bell (1774–1842) discovered the functions of nerves and showed that a nerve is not a single unit but a collection of filaments within a common sheath. William Beaumont (1785–1853) experimentally studied digestion in the exposed stomach of a wounded man, greatly advancing understanding of the process. Thomas Addison (1793–1860) helped found endocrinology when he reported that a form of anemia (now called pernicious anemia) was related to a fatal disease of the adrenal glands—the first time that anyone demonstrated that the adrenals are necessary for life. Jean Pierre Flourens (1794–1867) discovered the functions of the cerebellum and Paul Broca (1824–80) discovered the part of the brain that controls speech.
Claude Bernard (1813–78), often considered the founder of experimental medicine, investigated carbohydrate metabolism, discovering the ability of the liver to change glycogen to sugar and showing that blockage of the pancreatic duct prevents digestion of fats. Bernard also found that oxygen is not carried in solution in the blood but is bound to the red blood cells. He also proposed that in order to survive, a body maintains a stable internal environment even though external conditions change, a concept later termed homeostasis.
Numerous diseases, both acute and chronic, were carefully described for the first time: “shaking palsy” by James Parkinson (1755–1824), for whom the disease is now named; the facial paralysis now known as Bell’s palsy, by Charles Bell; hemophilia, by Johann Schonlein (1793–1864); Hodgkin’s disease, a cancer of the lymph nodes, by Thomas Hodgkin (1798–1866); and so on.
New Tools New tools included the stethoscope, invented by René Laënnec (1781–1826) in 1816 and used to investigate the lungs and heart, allowing physicians to hear for the first time “the cry of the suffering organs.” The invention of other influential tools soon followed, including the ophthalmoscope, invented independently by Charles Babbage (1792–1871) and Herman Helmholtz (1821–94) in mid-century and used to view the interior of the eye; and the sphygmograph, the predecessor of the modern sphygmometer, used to measure blood pressure, invented by Etienne-Jules Marey (1830–1904) in 1863. Endoscopy, or passing an instrument into a hollow organ in order to view its interior, had its beginnings in 1877 with the invention of a cystoscope to view the urinary bladder; candlelight was its source of illumination.
Until the 1860’s, doctors used very long thermometers to take a patient’s temperature, a process that took about 20 minutes. In 1866 Thomas Allbutt (1836–1925) introduced the short, efficient clinical thermometer. Its use was advanced by Carl Wunderlich (1815–77), who showed that fever is a symptom, not a disease.
In 1895, as the century neared its end, Wilhelm Röntgen discovered x-rays and how the radiation could be used to create a “shadow picture” revealing bone structure. Medicine diagnosis was revolutionized, for doctors could now examine a patient’s insides without cutting into the body.
Modern surgery emerged in the 19th century as well. Physicians recognized the three major obstacles to successful surgery—pain, infection, and bleeding. Two American dentists, Horace Wells and William Morton, discovered anesthesia in the 1840’s. By reducing the trauma of surgery for patients, anesthesia allowed doctors to take more time over their work and to apply surgery to more ailments. In 1842 Crawford Long (1815–78) painlessly removed a tumor from a patient’s neck after the patient sniffed ether. James Young Simpson (1811–70) discovered the anesthetic properties of chloroform and began using the substance to relieve the pain women experienced during childbirth.
Illness and death in hospitals decreased markedly with the introduction of antiseptic practices. In 1847 Ignaz Semmelweiss (1818–65) ordered doctors to wash their hands in a chlorine solution before each examination of a patient. In the late 1860’s Joseph Lister (1827–1912) introduced the use of carbolic acid on surgical instruments, wounds, and bandages, decreasing the death rate in his surgery from 49 percent to about 15 percent. Around 1890 William Halsted (1852–1922) introduced the practice of wearing sterilized rubber gloves during surgery.
By the end of the 19th century, the age-old practice of bloodletting was finally abandoned. The modern blood-type classification system, used to replenish a patient’s blood through transfusions, began with the 1900 discovery of the A-B-O blood groups by Austrian scientist Karl Landsteiner.
Chewing willow bark had been a successful method of combating fever for more than 2,000 years. Starting in 1838, chemists tried to produce a safe derivative of the active ingredient. Success came in 1893, when Felix Hoffmann (1868–1946) found acetylsalicylate. His employer, the Bayer pharmaceutical company, named the new drug “aspirin” and began selling it in 1899. Other drugs in the physician’s medicine cabinet included digitalis for heart ailments, amyl nitrate for angina, quinine for malaria, and sedatives such as chloral hydrate and paraldehyde.
Not all of the milestones in medicine were achieved in laboratories and operating rooms. In 1849 Elizabeth Blackwell (1821–1910) graduated from Geneva Medical College in upstate New York, earning the designation as the first woman doctor in modern times. At roughly the same time, Elizabeth Garrett (1836–1917) circumvented Britain’s rigid opposition to medical training for women and received a medical degree in 1865. Blackwell and Garrett eased the way for other women, both professionals and patients, by establishing women’s medical colleges, and infirmaries which specialized in obstetrics and pediatrics.
In 1889, Sir William Osler (1849–1919) a renowned Canadian physician, now revered as the “father of modern medicine,” was appointed the first Physician-in-Chief at John’s Hopkins Hospital in Baltimore, where he revolutionized the way the medical curriculum was taught. Osler insisted that students learn at the bedside, implementing his belief that “the good physician treats the disease; the great physician treats the patient who has the disease.” Students took patient histories, conducted physical examinations, and studied laboratory results, leading to a more interactive and humane treatment of medical conditions.
Osler established the medical residency, in which doctors in training make up much of a hospital’s medical staff. This system remains in place today in most teaching hospitals. In 1907, Dr. Osler invited Maude Abbott (1869–1940), a Canadian doctor, to contribute a chapter on cardiac abnormalities to his renowned work, Systems of Modern Medicine, which established her as the leading authority on the topic. Abbott literally wrote the book on cardiac disease, when she published The Atlas of Congenital Heart Disease (1936), which remained the primary source on the subject for decades.
20th-century Advances
When the 20th century began, life expectancy in the United States was 47 years. By 2000 average length of life had increased to almost 77 years. This steady improvement was due largely to a decline in deaths during childhood, the development of drugs to combat infectious diseases, improved nutrition, and better environmental sanitation. Public health measures, including pasteurization, inspection of food supplies, and fluoridation of water supplies, also were of great value.
Basic Discoveries Enormous strides in basic biological sciences—microbiology, biochemistry, genetics, and so on—coupled with technological advances led to explosive growth of pharmaceuticals and the development of new surgical techniques. For instance, the first indication that viruses can cause disease in humans came in 1901, when Walter Reed (1851–1902) and an associate proved that a virus causes yellow fever. Development of electron microscopes in the 1930’s gave scientists their first glimpse of viruses, and tissue culture techniques enabled researchers to grow viruses in the laboratory, for drug testing, preparation of vaccines, and other purposes.
Another type of disease-causing agent was first isolated in 1982 by Stanley Prusiner (b. 1942). Called prions, these particles consist solely of a protein. For reasons not yet understood, they can be transformed into abnormal shapes capable of destroying cells. Prions cause spongiform encephalopathies, fatal diseases characterized by the breakdown of brain tissue. These diseases include bovine spongiform encephalopathy, popularly called “mad cow disease,” and Creutzfeldt-Jakob disease in humans.
In 1901 Jokichi Takamine (1854–1922) became the first scientist to isolate a hormone, adrenalin. Isolation and, subsequently, synthesis made it easier to identify the roles played by hormones in diseases and led to improved treatments. The therapeutic use of hormones began in 1921, when Frederick Banting (1891–1941) and colleagues injected insulin, a hormone produced by certain pancreatic cells, into a person with diabetes.
Perhaps the most significant contribution in the field of endocrinology came 50 years later, with the creation of the birth control pill. In the early 1950’s, Gregory Pincus, an American biologist and researcher (1903–1967) discovered that injections of the hormone, progesterone, would inhibit ovulation and prevent pregnancy. Seed money for this effort was provided by Margaret Sanger, a lifelong advocate for women’s rights. At the same time, working independently, Carl Djerassi (b. 1923) created an orally effective form of synthetic progesterone. It was another decade before “the Pill” received F.D.A. approval and became commercially available, ushering in both a medical and social revolution.
In the first decade of the 20th century, scientists realized that certain “accessory food factors” are essential for good health. In 1911 Casimir Funk (1884–1967) found the first of these factors, B, and in a 1912 paper proposed the factors be called vitamins. The discovery of vitamins A (1913), D (1922), E (1922), C (1928), and K (1934) followed; it was shown that vitamin B actually is a complex of several vitamins, and synthesis led to widespread availability of the substances.
Rise of Genetics Nineteenth-century developments in genetics went largely unnoticed until 1900, when three botanists independently rediscovered basic laws of heredity published by Gregor Mendel (1822–84) in 1866. In 1902 Walter Sutton (1877–1916) correctly suggested that chromosomes—discovered and named in the late 19th century—carry Mendel’s “hereditary units,” later named genes.
By 1911 Thomas Hunt Morgan (1866–1945) had discovered that mutations could occur in the hereditary material; by the 1940’s scientists had established that all organisms as well as viruses can mutate. Meanwhile, other research demonstrated that exposure to x-rays, radioactive materials, and various chemicals increases the mutation rate. Scientists began identifying the connections between genes and disease. Today it is known that many diseases are triggered by altered genes. Some of these diseases are inherited while others result from random mutations that develop in body cells during one’s lifetime. Genetic abnormalities have been linked to illnesses from Alzheimer’s disease to osteoporosis to Tay-Sachs disease; scientists have identified more than thirty genes that cause different types of muscular dystrophy,
and nearly 400 cancer-related genes have been identified.
Genetic engineering, the deliberate alteration of an organism’s genetic material, began in 1973. By inserting specific human genes into bacteria or yeast, it became possible to manufacture large quantities of important human compounds: insulin, for people who have diabetes; erythropoietin, for treating anemia; tissue plasminogen activator (TPA), for dissolving blood clots; and so on. Researchers also took the first steps in gene therapy, transferring normal genes into the cells of people who suffer from diseases caused by defective genes. In 1990 a 4-year-old girl became the first person to undergo gene therapy, receiving a blood transfusion containing billions of cells with copies of the gene that would enable her body to made adenosine deaminase, an enzyme essential for a healthy immune system.
New Medications At the beginning of the 20th century, pneumonia and tuberculosis were the leading causes of death in the United States. By the century’s end, thanks to modern drug development, these and most other common bacterial infections had been brought under control, at least in the United States and other developed nations. Paul Ehrlich (1854–1915) helped found modern chemotherapy (the use of chemicals to fight disease) when he synthesized Salvarsan and in 1910 successfully used it to cure syphilis. In 1932 Gerhard Domagk (1895–1964) discovered that the red textile dye Prontosil protected against deadly Staphylococcus and Streptococcus bacteria. Prontosil was the first drug that could be used against a variety of bacteria; later, more powerful drugs, called sulfonamides or sulfa drugs, were derived from Prontosil. They would eventually be largely replaced by safer and more effective antibiotics.
Medicine was revolutionized in 1928 when Alexander Fleming (1881–1955) discovered the antibiotic properties of penicillin, but he was unable to produce it in a form pure enough to use on patients. Ten years later, Howard Florey and others at Oxford University, solved this problem, and by World War II, techniques were developed in the United States for the commercial production of the drug. Its disease-fighting potential was recognized in the early years of World War II, and it saved the lives of countless wounded soldiers. Today a number of penicillins are available, including ampicillin, amoxicillin, and oxacillin, and they are among the most widely used antibiotics. Other antibiotics include cephalosporins (for example, cephalothin), tetracyclines (tetracycline), macrolides (erythromycin), aminoglycosides (streptomycin), quinolones (ciprofloxacin), and glycopeptides (vancomycin). Unfortunately, bacteria evolve rapidly, developing strains resistant to one or more antibiotics and requiring researchers to search for new drugs to combat the “super-bugs.”
Other drugs added to the pharmaceutical arsenal included corticosteroids, to treat rheumatoid arthritis; antabuse, to prevent alcoholics from drinking; cyclo-sporine, to prevent rejection of transplanted organs; antidepressants and antipsychotics, for mental problems; and thrombolytic drugs to dissolve blood clots. Some new offerings actually were ancient drugs in new form. In 1950, for instance, reserpine was introduced for treatment of high blood pressure; the drug had long been used in India in the form of snakeroot.
Beginning in 1944, Gertrude Elion, along with her colleague, George H. Hitchings joined Burroughs Wellcome Laboratories (now GlaxoSmithKline), and using innovative new research techniques, developed an array of drugs that were effective against leukemia, autoimmune diseases, malaria, and viral herpes. They were awarded the Nobel Prize in Physiology or Medicine in 1988 for their discoveries. Elion later participated in the development of azidothymidine (AZT), the first drug used in the treatment of AIDS.
Advances in Surgery In the early 20th century, surgeons began to specialize and new fields emerged, building on the efforts of a few extraordinary individuals. Not for the first time, the theater of war made an enormous contribution to the progress of medicine. In 1914, Harold Gillies (1882–1960) a New Zealand-born, British Red Cross doctor in World War I, saw that while soldiers could survive their battle wounds, surgeons had neither the skill nor the time to deal with their often dramatic disfigurements. Gillies devoted himself to the study and practice of plastic surgery, founding Queen’s Hospital in Kent, England where more than 10,000 reconstructive surgeries were performed. The techniques he invented, including skin grafts, were adopted by surgeons around the world and ushered in the era of reconstructive and, ultimately, cosmetic surgery.
Working in some of America’s finest hospitals, including John’s Hopkins Hospital in Baltimore and Peter Bent Brigham Hospital in Boston, Harvey Cushing
(1869–1939) is recognized today as the first true neurosurgeon. Among his many innovations, Cushing created a way to stem the flow of blood with clamps and cuffs, allowing for a better visual field, and minimizing the possibility that the patient would bleed to death. He pioneered the use of the “electric scalpel,” and demanded that his team work with masks and gloves to minimize infection. His patients were the first to receive around-the-clock nursing care after surgery, and this type of post-operative treatment was the forerunner of intensive-care units. Taken together, Cushing’s contributions made brain surgery safer and more effective.
There were other surgical milestones during this period. The first successful appendectomies were performed in Davenport, Iowa in 1885 by Dr. William West Grant, and at roughly the same time by Dr. H. Hancock, in England. In 1932, American surgeon Michael E. DeBakey developed a roller pump that became an essential component of the heart-lung machine, and in 1944, Dr. Helen Taussig (1898–1980), an American cardiologist, developed an operation to correct the congenital heart defect that causes “blue baby” syndrome, an operation which has prolonged the lives of many children, and which was an important step in the development of adult open-heart surgery, successfully performed for the first time by John H. Gibbon, Jr. in 1953. In 1954, a team of physicians at Peter Bent Brigham Hospital transplanted a kidney from a young man into his identical twin.
In 1966, DeBakey implanted the first mechanical heart in a human, and other successful transplantations soon followed: liver (1963), lung (1963), pancreas (1966), intestine (1966). In 1967, Dr. Christiaan Barnard performed the first successful human heart transplant. Bone marrow transplants (in which blood-forming stem cells are used to treat certain cancers and blood disorders) began in 1964 when the first successful transplant took place, between identical twins. Today, stem cell transplants represent one of the most exciting—and controversial—frontiers in modern surgery. In 1990, the so-called laparoscopic technique was perfected, allowing surgeons to make much smaller incisions in the patient’s abdomen, and remove small organs through the navel.
New Technologies Twentieth-century technologies such as computers, electronics, fiber optics, lasers, and ultrasound were all incorporated into medicine, making diagnoses much more accurate and treatments safer and more effective. Mammography for diagnosing breast cancer was introduced in 1913, the electroencephalogram (EEG) for recording brain waves in 1929. The heart can be monitored by recording electrical activity via skin electrodes with the electrocardiography (EKG) machine, and the implantable pacemaker for regulating heartbeat was developed in 1958. The CT scan for producing three-dimensional images of internal organs was developed in 1972, balloon angioplasty for unclogging diseased arteries in 1977, and the lithotripter for breaking up kidney stones in 1980.
Great advances also occurred in the construction of artificial body parts. Aluminum, titanium, plastic resins, and three-dimensional computer modeling were used to build sophisticated limbs and joints. An artificial kidney was first used in 1943 and artificial skin was introduced in 1981. As the century neared its end, artificial blood vessels were being successfully tested in dogs.
Alternative Therapies Modern Western medicine has not been without its critics. Patients complain about assembly-line atmospheres in doctors’ offices, improper or ineffective treatments, botched operations, the debilitating side effects of many drugs, and health care costs that spiral higher and higher. In recent decades factors such as these helped fuel interest in alternative forms of medicine.
Acupuncture the insertion of needles into specific points on the body to stimulate and balance the flow of energy through the body, has been used in China for more than 2,000 years.
Ayurvedic medicine which focuses on natural diet, herbs, exercise, and such therapies as massage, has been practiced in India for at least 4,000 years.
Biofeedback learning to detect and consciously control physiological functions, developed in the mid-1900’s.
Chiropractic manipulation of the spine to treat spinal and nervous disorders, began in 1895.
Herbalism the use of potions derived exclusively from plants, has been practiced in China, India, and other places for thousands of years.
Homeopathy treating a disease with minuscule doses of the natural substances that in larger amounts would bring on the disorder, was developed in the early 1800’s.
New scientific evidence supported the effectiveness of some alternative therapies. For example, acupuncture
was found to ease chronic back pain and arthritic pain in some patients; migraine sufferers who learned relaxation techniques had fewer migraines and needed less medication to cope with their headaches. Physicians began integrating certain alternative therapies with conventional medicine—recommending biofeedback and stress-management techniques to heart patients, offering hypnosis programs to people who wanted to quit smoking, and referring patients to chiropractors and acupuncturists.
Current and Future Developments Humans continue to face major health challenges. Many infectious diseases have been brought under control in developed countries but remain huge epidemics elsewhere. Some of these diseases, such as malaria, tuberculosis, and dengue fever, actually are increasing and spreading to new regions. AIDS, Lyme disease, and other emerging diseases discovered only in recent decades have created new medical battlefields. So, too, has the growing resistance of ever-mutating germs to antibiotics; physicians have few weapons to combat once-treatable organisms such as Streptococcus pneumoniae, a major cause of bacterial pneumonia and MRSA (methicillin-resistant Staphylococcus Aureus), an infection often contracted in hospitals and nursing homes.
People are living longer, resulting in a growing incidence of arthritis, Alzheimer’s disease, congestive heart failure, and other diseases of the elderly. High-risk behaviors such as illicit drug use and limited access to health care are additional issues. Preventable illnesses kill many millions of people annually. Worldwide, tobacco use causes approximately 4.2 million premature deaths annually, a number expected to increase to 10 million by 2030. Obesity, a major contributor to chronic disease and disability, has also reached epidemic proportions globally, with more than 1 billion adults overweight, at least 300 million of them clinically obese. Also, more than 7 million children under age five die every year from diarrhea, pneumonia, and other preventable diseases; they could be saved if malnutrition and poor sanitary conditions were eradicated and basic medical treatments, including prenatal and neonatal care, were provided.
On a positive note, there is hope that some of the world’s worst diseases are being brought under control. Under the auspices of the World Health Organization (W.H.O.) and other governmental and private organizations, elimination and eradication programs are in place for polio, measles, leprosy, guinea-worm disease (dracunculiasis), river blindness (onchoceriasis), and Chagas’ disease. Results have been encouraging. After the Global Polio Eradication Initiative was launched in 1988, the number of polio cases fell by over 99 percent—from an estimated 350,000 cases in 1988 to 1,900–2,000 cases in the mid-2000’s; the number of countries in which polio was endemic decreased from more than 125 to four.
Better understanding of human biology, genetics, and psychology are leading to improved preventive measures, diagnostic tools, and therapies. Genetic engineering, computerization, miniaturization, and other technological advances also will continue to improve people’s health and medical care.
Medical researchers are particularly excited about the potential benefits of research on stem cells, undifferentiated cells that can develop into specialized cells. Embryonic stem cells, found only in embryos, give rise to all the different kinds of cells in the body. It appears that adult stem cells, found in children and adults, are only able to develop into a limited number of cell types; for example, adult stem cells in the skin develop into different kinds of skin cells. The best-known stem-cell therapy to date is the bone marrow transplant, in which blood-forming stem cells are used to treat certain cancers and blood disorders. Work with embryonic stem cells is still in its early stages, but many scientists believe these cells may provide entirely new treatments for heart disease, diabetes, Parkinson’s disease, and other ailments. Another area that may one day benefit is the development and testing of new medicines.
Through past millennia, human life span has increased as people have learned how to prevent and treat illness. By the beginning of the 21st century, average life span had exceeded 80 years in some countries. There is much reason to believe that future medical advances will increase not only life span but also quality of life.
Disease can be defined as a disturbance or abnormality in which part of the body is not functioning properly, thereby making a person physically or mentally ill and possibly leading to death. The most common types of diseases include:
Infectious diseases, which are caused by viruses, bacteria, fungi, and other organisms, and transmitted from person to person—or from animal to person. Examples: common cold, influenza, chickenpox, measles, tuberculosis, AIDS.
Hereditary diseases, which are transferred from parent to child via the genes. Examples: Down syndrome, hemophilia, sickle cell anemia.
Degenerative diseases, which result from a general breakdown of body structures and natural aging processes. Examples: certain types of arthritis and cardiovascular disease.
Hormonal disorders, resulting from an insufficiency or excess of hormones—chemicals that act as messengers in the body. Examples: diabetes, hypoglycemia, hypothyroidism, Graves’ disease.
Environmental diseases, caused by chemical and physical agents such as radiation, smoke, drugs, and poisons. Examples: allergies, asbestosis, bysinosis, lead poisoning.
Deficiency diseases, caused by the lack of vitamins or other essential nutrients. Examples: beriberi, scurvy, pellagra, rickets.
Mental and emotional illnesses, caused by chemical, genetic, and environmental factors. Examples: anxiety, bipolar disorder, dementia, schizophrenia.
The etiology (origins) of some ailments, such as chronic fatigue syndrome, fibromyalgia, and irritable bowel syndrome, has not yet been clarified. It is possible that two or more factors are responsible for each of these diseases or for its progression, as is true for many other diseases. For instance, when a person who smokes and is a heavy drinker develops throat cancer, it is probable that the cancer was caused by both tobacco and alcohol. A study in India reported in 2003 found that smokers are four times as likely as nonsmokers to die of tuberculosis.
The most common disease is cardiovascular disease. The World Health Organization (W.H.O.) estimated that 17.5 million people died from cardiovascular disease in 2005, representing approximately 20 percent of all global deaths. In the U.S., cardiovascular disease accounts for about 36 percent of all deaths.
Some diseases, such as bone cancers, tuberculosis, and stomach ulcers, have plagued humans since prehistoric times. Others are new. West Nile virus, spread by mosquitoes, was unknown in the United States prior to 1999. By 2006 the virus had spread to every state except Alaska and Hawaii; it had caused 4,261 cases of disease, including 174 fatalities. An avian influenza (“bird flu”) caused by the H5N1 virus was identified in 1997. It is highly contagious among birds, but usually only infects humans who have direct or close contact with infected poultry or virus-contaminated surfaces. By early 2007 there had been 291 laboratory-confirmed cases worldwide, with 172 deaths. Health officials fear that the H5N1 virus could mutate into a form that spreads easily from person to person. Should this occur, a worldwide flu pandemic, infecting and killing millions of people, could result.
Discovery Dates and Effects of Human Pathogens
| Year | Pathogen | Disease |
|---|---|---|
| 1975 | Human parvovirus B19 | Erythema infectiosum (fifth disease), chronic hemolytic anemias |
| 1976 | Cryptosporidium parvum | Acute and chronic diarrhea |
| 1977 | Ebola virus | Ebola hemorrhagic fever |
| 1977 | Legionella pneumophilia | Legionnaire’s disease |
| 1977 | Hantaan virus | Hemorrhagic fever with renal syndrome |
| 1977 | Campylobacter jejuni | Enteric diseases |
| 1980 | Human T-lymphotropic virus 1 (HTLV-1) | T-cell lymphoma-leukemia |
| 1981 | Toxin-producing strains of Staphylococcus aureus | Toxic shock syndrome |
| 1982 | Escherichia coli O157:H7 | Hemorrhagic colitis; hemolytic uremic syndrome |
| 1982 | HTLV-II | Hairy cell leukemia |
| 1982 | Borrelia burgdorferi | Lyme disease |
| 1983 | Human immunodeficiency virus (HIV) | AIDS (acquired immune deficiency syndrome) |
| 1983 | Helicobacter pylori | Peptic ulcer disease |
| 1988 | Hepatitis E | Enterically transmitted non-A, non-B hepatitis |
| 1992 | Vibrio cholerae O139 | Epidemic cholera |
| 1992 | Bartonella henselae | Cat-scratch disease (bacillary angiomatosis) |
| 1995 | Hepatitis G virus | Parenterally transmitted non-A, non-B hepatitis |
| 1997 | Avian influenza, type A (H5N1) | Influenza |
| 2003 | SARS virus | SARS (severe acute respiratory syndrome) |
Leading Causes of Death, Worldwide, 20041
| Number (ooo’s) | Percent | |
|---|---|---|
| World total deaths | 58,772 | 100.0% |
| Communicable diseases | 17,971 | 30.6 |
| maternal/perinatal conditions; nutritional deficiencies | ||
| Infectious and parasitic diseases | 9,519 | 16.2 |
| Diarrheal diseases | 2,163 | 3.7 |
| HIV/AIDS | 2,040 | 3.5 |
| Malaria | 889 | 1.5 |
| Childhood cluster diseases | 847 | 1.4 |
| Respiratory diseases | 4,259 | 7.2 |
| Respiratory infections | 4,177 | 7.1 |
| Noncommunicable conditions | 35,017 | 59.6 |
| Cardiovascular diseases | 17,073 | 29.0 |
| Cancers | 7,424 | 12.6 |
| Injuries | 5,784 | 9.8 |
| Intentional | 1,642 | 2.8 |
| Note: 1. Estimates. Source: World Health Organization, The Global Burden of Disease, 2004. | ||
In World Health Report 2002, W.H.O. identified the top 10 health risks in terms of the burden of disease they cause. These risks are responsible for more than one-third of all deaths worldwide. They are: underweight, unsafe sex, high blood pressure, tobacco consumption, alcohol consumption, unsafe water, sanitation and hygiene, iron deficiency, indoor smoke from solid fuels, high cholesterol, and obesity.
Common Diseases
AIDS Acquired immune deficiency disease (AIDS) is caused by human immunodeficiency virus (HIV). The disease was discovered in 1981 and the causative agent was identified in 1983. By 2009 an estimated 33.3 million people were infected worldwide and more than 25 million had died of the disease. Sub-Saharan Africa has been the region hardest hit by the HIV/AIDS pandemic; more than two-thirds of all people with HIV/AIDS are in this region. In the United States, more than 1 million people were living with HIV/AIDS, with an estimated 25 percent unaware of their infection.
Leading Causes of Death, United States, 20091
| Number | Death Rates per 100,000 Population | |
|---|---|---|
| Deaths, all causes | 2, 436,682 | 793.7 |
| Cardiovascular diseases | 598,607 | 195.0 |
| Cancer | 568,668 | 185.2 |
| Chronic lower respiratory disease | 137,082 | 44.7 |
| Cerebrovascular diseases | 128,603 | 41.9 |
| Accidents | 117,176 | 38.2 |
| Alzheimer’s disease | 78,889 | 25.7 |
| Diabetes | 68,504 | 22.3 |
| Influenza and pneumonia | 53,582 | 17.5 |
| Kidney diseases | 48,714 | 15.9 |
| Suicide | 36,547 | 11.9 |
| Septicemia | 35,587 | 11.6 |
| Chronic liver diseases | 30,444 | 9.9 |
| Hypertension and hypertensive renal disease | 25,651 | 8.4 |
| Parkinson’s disease | 20,552 | 6.7 |
| Homicide | 16,591 | 5.4 |
| Note: 1. Preliminary data based on estimate. Source: Center for Disease Control and Prevention. | ||
HIV is spread through contact with infected body fluids such as blood and semen. Infected people may harbor the virus within their bodies for several years or even longer before developing symptoms of AIDS. Though symptomless, they can still infect others. Worldwide, most HIV transmission occurs during sexual relations between heterosexual partners. In the United States, the majority of transmission has been between homosexual partners. Transmission among drug addicts who share infected needles is another significant route of transmission in many countries.
In the body, HIV invades immune system cells called T-helper lymphocytes. The viruses reproduce in the cells and send out new viruses to attack additional T-helper lymphocytes. Eventually, the lymphocytes are destroyed, leaving
the patient vulnerable to Pneumocystis carinii and other “opportunistic” pathogens.
No cure for AIDS is known. Researchers are working on preventative AIDS vaccines, but none are expected to be ready for market in the near future. Antiretroviral drug therapies introduced in the mid-1990’s have been extremely effective in controlling AIDS progression for some patients. However, the medications are expensive; without comprehensive programs and sustained financial support, they are beyond the reach of the vast majority of the world’s HIV-positive people.
Allergies Allergies are overreactions of the immune system to foreign substances. Any substance that triggers an allergic reaction is called an allergen. Pollen, mold spores, dust mites, foods, alcohol, medications, chemicals, and animal dander are common allergens. Allergens cause the body to produce and release histamine and other “mediator” compounds. These compounds affect local tissues and organs, causing symptoms of the reaction.
Symptoms may include itchy or blistering skin, stuffy or runny nose, sneezing, shortness of breath, red or swollen eyes, headache, swelling of the lips or tongue, nausea, vomiting, or diarrhea. If the release of mediator compounds is sudden or extensive, the allergic reaction may be severe, resulting in anaphylactic shock. U.S. incidence of allergic diseases has grown dramatically in recent years. An estimated 60 million Americans suffer from allergies; more than 700 die each year due to allergies, about half of them due to drug allergies from penicillin.
Measures such as staying away from poison ivy and eliminating certain foods from the diet can prevent many problems. Medications such as antihistamines and corticosteroids are helpful in treating allergic reactions. Prompt injection of the hormone epinephrine (adrenaline) can stop anaphylactic shock, saving the person’s life.
Alzheimer’s disease This progressive degenerative condition is characterized by forgetfulness in early stages and, as the disease progresses, increasingly severe debilitating symptoms that create demanding care-giving needs. As life expectancy has increased, so has the incidence of Alzheimer’s disease. In the U.S., more than 5.1 million people, most of them elderly, are estimated to have the disease, and it causes about 79,000 deaths annually. These figures are expected to rise in the coming years.
The cause of Alzheimer’s disease is unknown, but genetic abnormalities appear to play a role. There is a gradual degeneration of brain tissue. Areas involved with memory are damaged first, then structures involved with emotion and control of behavior. No cure yet exists. Treatment consists of alleviating symptoms and providing long-term care. Death usually occurs 10 to 15 years following onset of the disease.
Amyotrophic lateral sclerosis (ALS) ALS is a fatal disorder of the nervous system. Its cause is not known. It involves the progressive deterioration and death of the nerve cells that control the muscles. In its early stages, weakness in the limbs is the primary symptom. Gradually, cramping and twitching develop and the person has difficulty walking and carrying out everyday tasks. Weakening of muscles in the throat make speaking and swallowing difficult. When the diaphragm and chest muscles involved in breathing become affected, the person may require a ventilator. There is no cure for ALS; treatment consists of relieving symptoms and using physical therapy to slow muscle atrophy.
An estimated 30,000 Americans have ALS; about 50 percent die within three years of the first symptoms. ALS is also known as Lou Gehrig’s disease because the New York Yankee star was one of its most famous victims.
Anthrax This infectious disease is caused by the bacterium Bacillus anthracis. People contract it by inhaling bacterial spores, touching infected animals or animal parts (infected cattle hide, for example), or eating infected meat; the disease does not spread from one person to another.
Early symptoms vary depending on the source of infection. Anthrax bacteria that colonize the skin form a dark sore. Intestinal anthrax induces vomiting and abdominal pain. Inhaled spores are the most dangerous; they cause breathing difficulties, change into actively dividing cells, and pass quickly from the lungs into the lymph and blood. Swift diagnosis and treatment with antibiotics are critical in preventing death.
Arthritis Arthritis is a generic term that encompasses more than 100 different diseases, all of which cause pain, stiffness, and usually swelling in the joints. According to the National Arthritis Foundation, arthritis affects nearly 46 million Americans and is the leading cause of physical disability. Although it affects people of all ages, it most commonly develops as people get older.
The causes of most types of arthritis are unknown, although certain factors—particularly excess weight and joint injuries caused by accidents or overuse—increase risk. Genetic factors can increase risk for some types of arthritis. The most common types of arthritis include osteoarthritis, rheumatoid arthritis, and gout.
Osteoarthritis is a degenerative disease that involves the breakdown of cartilage and bone, particularly in the fingers and weight-bearing joints such as the spine, hips, and knees. Treatments include regular exercise, medication, and if a joint is seriously deformed, surgery.
Rheumatoid arthritis, the most severe form of arthritis, is an autoimmune disorder in which the immune system attacks joint tissues, causing inflammation that can eventually lead to serious damage, including bone erosion and dislocated joints. In some cases, the heart, lungs, and eyes also are affected. Effects of the disease can be limited by regular exercise during periods of remission and by rest and anti-inflammatory medications during attacks. Juvenile rheumatoid arthritis is the most common type of arthritis in children. It often is mild, disappearing after several years, but serious cases can last a lifetime.
Gout results from an accumulation of uric acid in the blood, which leads to deposits of uric acid crystals in a joint. Typically, the first joint to be affected is the one in the big toe; other joints of the extremities—fingers, wrist, knee, and ankle—often become affected as well. Attacks, which last for days, can be extremely painful. Fortunately, gout generally can be successfully controlled. Uric acid is a waste product of the digestion of compounds called purines; avoiding alcohol, organ meats, legumes and other foods rich in purines prevents or reduces the severity of attacks. During attacks, anti-inflammatory and corticosteroid drugs counteract joint inflammation and pain.
Asthma Some 20 million Americans are estimated to have asthma, an immune disorder that affects the muscles around the bronchial tubes leading to the lungs. In a reaction to certain stimuli, the muscles tighten, narrowing the airways and causing them to become inflamed and clogged. The person finds breathing difficult, and wheezes and coughs. In severe episodes, the person finds it almost impossible to breathe and requires immediate medical attention.
Most asthma attacks are caused by allergies to inhaled substances such as pollen, dust, and animal dander. Food allergies, infections, and emotional stress also can cause attacks. There is no cure for asthma, and proper management is essential. People with the disease can avoid substances and situations that act as triggers. They also can learn to recognize early warning signs and take medications to reduce underlying inflammation and prevent or relieve narrowing of the airways.
Autoimmune diseases Several dozen known diseases result from immune system malfunctions that cause disease-fighting cells to attack the body’s own tissues. What initiates such autoimmune diseases is usually not known. However, their incidence appears to be increasing, particularly in industrialized nations. In the United States, 14 million to 22 million people are believed to be affected. About twice as many women as men developed autoimmune diseases.
Symptoms of an autoimmune disease can vary widely, as can the disease’s course. Some patients develop mild cases, while in others the disease causes severe damage and can be fatal. Mild symptoms may be treated with nonsteroidal anti-inflammatory drugs (NSAIDs). Stronger anti-inflammatory compounds, including corticosteroids, are prescribed for severe symptoms. Common autoimmune diseases include:
Addison’s disease Affects adrenal glands; causes a deficiency of adrenal hormones, which can be life threatening if not treated.
Crohn’s disease Affects intestinal wall; causes chronic diarrhea, abdominal pain, rectal bleeding; increases risk of colon cancer.
Graves’ disease Affects thyroid; most common cause of hyperthyroidism, or overactive thyroid.
Multiple sclerosis Affects brain, spinal cord; causes partial or complete paralysis and muscle tremors.
Myasthenia gravis Affects synapses between nerves and muscles, causing muscle weakness.
Psoriasis Affects skin, forming red patches covered with white scales.
Rheumatoid arthritis Affects connective tissue, joints; characterized by pain, stiffness, inflammation, swelling.
Systemic lupus erythematosus (lupus) Affects connective tissue, joints, kidneys, blood vessel walls, mucous membranes (such as those surrounding the lungs); causes joint pain, skin rashes, chest pain, enlarged lymph nodes.
Cancer This group of diseases is characterized by the unrestrained growth of cells. Physicians describe the extent or spread of a cancer using a process called staging. This aids in determining the most appropriate treatment and in assessing the prognosis. One system widely used for many types of cancer classifies cancers into four stages. In this system, stage I is early stage cancer with no involvement of lymph nodes and no spread of the cancer from its original site (metastases); stage IV is advanced cancer, with both lymph node involvement and distant metastases.
Times focus
Rise Seen in Number of Survivors of Cancer
About one in every 20 adults in the United States has survived cancer, including nearly one-fifth of all people over 65, according to new federal data.
The numbers, released Thursday by the Centers for Disease Control and Prevention and the National Cancer Institute, indicated that the number of cancer survivors increased by about 20 percent in just six years, to 11.7 million in 2007, the latest year for which figures were analyzed, from 9.8 million in 2001. In 1971, the number of cancer survivors was three million.
“There’s still a concept that cancer is a death sentence,” said Dr. Thomas R. Frieden, director of the Centers for Disease Control. But, he said, “for many people with cancer there’s a need for them and their families and caregivers to recognize that this is a stage. They can live a long and healthy life.”
About 65 percent of cancer survivors have lived at least five years since receiving their diagnosis, 40 percent have lived 10 years or more, and nearly 10 percent have lived 25 years or longer.
The implications, Dr. Frieden said, are that many cancers are treatable and that it is just as important for people who have had cancer not to assume that they will necessarily die early.
“You might think, ‘I’ve had cancer—I don’t have to worry about eating right, quitting smoking, exercising,’” Dr. Frieden said. But people with cancer “need to be just as concerned about heart disease and other risks as they would otherwise,” he said.
The study defined a survivor as anyone who ever received a diagnosis of cancer who was alive on Jan. 1, 2007, and it did not indicate if the person was cured, undergoing treatment, afflicted with a chronic cancer-related illness, or in the process of dying at that time.
And the numbers tell only a piece of the cancer story. Some cancers, like lung cancer, are aggressive and difficult to treat. And the death rate from cancer, an indicator that many health experts consider a more accurate measure of progress in fighting the disease, has stayed virtually the same as it was in 1950—about 200 deaths per 100,000 people a year, and about 1,000 deaths annually per 100,000 people over 65.
Dr. Frieden said the increase in cancer survivors was due to several factors, some of which varied by type of cancer. In some cases of breast cancer and colon cancer, for example, improved treatment and increased follow-up after treatment have helped increase survival. In others, like prostate cancer, an explosion in screening has identified many men with the disease, but the cancer is often so slow-growing that they would be unlikely to die from it. And other cancer diagnoses are simply the consequence of the country’s aging population and improved care for other diseases—in other words, people are living long enough to develop cancer.
About a million more of the survivors were women than men, partly because women live longer than men, and partly because breast and cervical cancers are often diagnosed and treated at younger ages. About 22 percent of the survivors had breast cancer, about 19 percent had prostate cancer, and about 10 percent had colorectal cancer.
The study identified only the type of cancer first diagnosed in each person; additional tumors or cancer diagnoses were not recorded. Health authorities urged families and physicians to be aware of the health needs of cancer survivors. “Having cancer may be the first stage, really, in the rest of your life,” Dr. Frieden said. “We need to continue to scale up” the services available for cancer survivors.
Cancer afflicts people of all ages and races, although about 77 percent of all cases are diagnosed at ages 55 and above. Cancers vary greatly in cause, symptoms, response to treatment, and possibility of cure.
W.H.O. estimated that there were 7.9 million cancer deaths worldwide in 2007. Deaths from cancer worldwide are projected to continue rising, with an estimated 12 million deaths in 2030. A healthy, non-smoking U.S. male has slightly less than a 1 in 2 lifetime risk of developing cancer; a female slightly more than 1 in 3.
Bladder cancer Smoking is the main risk factor for cancer of the urinary bladder; exposure to certain hazardous chemicals in the workplace also places people at risk. Warning signs include blood in the urine, pain during urination, and frequent urination. Early stage cancer can often be removed surgically. Additional treatment may include chemotherapy and radiation.
Breast cancer The most common, though not the deadliest, cancer among women is breast cancer. Risk factors include advancing age, obesity, physical inactivity, alcohol use, hormone replacement therapy, a family history of breast cancer, and inherited susceptibility genes, particularly mutated BRCA1 or BRCA2 genes. Early detection of the tumor—typically by breast self-examination or, more effectively, by mammography—is critical in improving a person’s survival rate. Treatment options include removal of the tumor (lumpectomy) or the entire breast (mastectomy), radiation, chemotherapy, and hormone therapy.
Cervical cancer Sexually transmitted diseases (STDs), particularly genital warts, appear to be the major cause of cancer of the cervix (the lower opening of the uterus). Tobacco use and obesity also increase risk. The first noticeable symptom generally is abnormal bleeding or discharge from the vagina. Treatment may include surgical removal of the tumor, cyrotherapy (freezing the cancerous cells), radiation, and chemotherapy. A vaccine introduced in 2006 protects against four human papilloma viruses (HPV) that are a major cause of genital warts and cervical cancer. The vaccine is recommended for girls and women before they become sexually active.
Colorectal cancer Major factors that increase the risk of cancer of the rectum and colon include increasing age, inflammatory bowel disease, and familial history of colorectal cancer. Obesity, smoking, physical inactivity, alcohol consumption, and high-fat or low-fiber diets also increase risk. Symptoms include rectal bleeding, blood in the stool, and lower abdominal cramps. Because symptoms generally are not noticeable until the disease is advanced, people age 50 or more are advised to have periodic fecal occult blood tests and sigmoidoscopies or colonoscopies. Surgery is the most common treatment; chemotherapy and radiation may also be used.
Leukemia Leukemia affects bone marrow, the lymph system, and other tissues involved in forming white blood cells, resulting in excessive production of abnormal white blood cells. The cause is unknown, though exposure to viruses, radiation, and certain hazardous chemicals (benzene, for example) increase risk. Common symptoms include fatigue, fever, weight loss, swollen lymph nodes, a tendency to bleed, and pain in the bones and joint. Treatment options include chemotherapy, radiation, and bone marrow transplants.
Lung cancer The leading cause of cancer deaths in the United States and worldwide is lung cancer. The great majority of these deaths could be prevented if people did not use tobacco. Initial symptoms often are not noticeable until the lung cancer has grown for five to 10 years; they include chronic coughing, shortness of breath, wheezing, and chest or shoulder pain. Treatment may include surgical excision of part or all of the affected lung, radiation, and chemotherapy.
Lymphoma Cancers that develop in lymph tissue fall into two main categories: Hodgkin’s disease and non-Hodgkin’s lymphoma. Risk factors are unclear, though viruses or other infectious agents are believed to play a role in at least some cases. The first noticeable symptom of lymphoma usually is a swelling of lymph glands; fever, night sweats, itching, fatigue, and weight loss also are common symptoms. Treatment may involve chemotherapy, radiation, and, in advanced stages, bone marrow transplants.
Melanoma This is the deadliest type of skin cancer, and it may also occur in the eyes and in other areas where melanocytes (pigment-producing cells) are found. The major risk factors include certain inherited characteristics (light-colored skin, blond or red hair, blue eyes) and exposure to natural and artificial sunlight. Most often, the first noticeable sign of melanoma is a mole that has one or more ABCD characteristics: Asymmetry, Border irregularity, Color variation, and Diameter greater than that of a pencil. If caught early, before it has penetrated deeper levels of the skin or spread to other parts of the body, melanoma is very treatable. Treatment options include surgical excision of the melanoma and, if the cancer has spread, chemotherapy, radiation, and immunotherapy.
Ovarian cancer Major risk factors for cancer of the ovaries include advancing age, familial history of breast or ovarian cancer, and the use of fertility drugs and hormone
replacement therapy. The most common symptom is an enlarged abdomen due to accumulation of fluid. Treatment options include surgical removal of the ovaries and other female sex organs, radiation, and chemotherapy.
Pancreatic cancer Risk factors for cancer of the pancreas include tobacco use, advancing age, and obesity; pancreatitis, diabetes, and cirrhosis may also be factors. Symptoms usually are not noticeable until the disease has metastasized. Surgery, chemotherapy, and radiation may help ease pain and prolong survival.
Prostate cancer Increasing age is a leading risk factor for cancer of the prostate gland. Other risk factors are a family history of the disease and ethnicity—African-American men have the world’s highest incidence rates of prostate cancer. Noticeable symptoms generally develop after the disease has advanced, and include difficulty urinating, pain during urination, and pain in the lower back, pelvis, or upper thighs. Treatment may include surgery, hormone therapy, chemotherapy, and radiation.
Uterine cancer Cancer of the uterus (other than cervical cancer) typically begins in the lining, or endometrium. The major risk factor is exposure to the hormone estrogen; obesity, diabetes, and hypertension also increase risk. The first noticeable symptom generally is abnormal bleeding or discharge from the vagina. Treatment involves removal of the uterus and perhaps other female sex organs. If metastasis has occurred, radiation and chemotherapy may also be used.
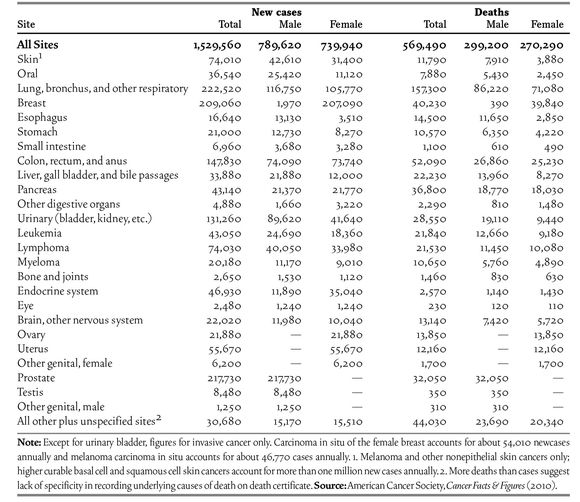
Estimated New Cancer Cases and Deaths by Site and Sex, United States, 2010
Times focus
The Hard Facts of Hypertension
Over the course of their remaining lives, Americans now 55 or over face a 90 percent chance of developing high blood pressure, or hypertension, a major risk factor for heart attacks, strokes, congestive heart failure, circulatory failure, kidney disease, and loss of vision. This finding emerged from a 22-year follow-up study of 1,298 residents of Framingham, Mass., who were from 55 to 65 in 1976.
If applied to the whole population, the risk of developing hypertension represents a huge public health burden, in addition to the costs to the health of those affected. Hypertension is a primary or contributing cause of more than 10 percent of American deaths each year. Complicating the picture is more bad news: of the 50 million Americans with hypertension, only 27 percent are receiving treatment that restores blood pressure to normal.
What Is Normal? Despite three decades of efforts to educate physicians and the public, there is still profound ignorance about what is normal blood pressure. And many physicians seem reluctant to provide adequate treatment and guidance. Your blood pressure should be measured at every visit to a health professional, regardless of the reason for the visit.
In most cases, hypertension is a silent disease, producing either no symptoms or symptoms readily attributed to other causes—headaches, ringing in the ears, lightheadedness, fatigue. The only way to be sure your pressure is normal is to have it taken.
The test is fast, cheap, noninvasive and painless. A cuff is wrapped around your upper arm, inflated to temporarily stop blood flow and then slowly deflated as the examiner listens through a stethoscope to your blood flowing through an artery just above the elbow, recording the number when a pulse noise is first heard and the number when the noise stops.
The two numbers, expressed in millimeters of mercury, represent the force of blood pushing against the walls of your arteries when your heart pumps, the systolic pressure, and when your heart rests between beats, the diastolic pressure. The final reading is the systolic pressure (the higher number) over the diastolic. Hypertension is defined as a systolic blood pressure of 140 or more, a diastolic pressure of 90 or more, or both. Both numbers are important; when either is elevated, so is the risk of developing heart and blood vessel disorders. Contrary to the practice of some physicians, bringing only the diastolic pressure down to normal is not enough to protect against complications.
Further, when a person already has a disease affected by hypertension, like heart or kidney disease, current medical guidelines call for lowering blood pressure even more, well below the 140-over-90 cutoff.
Finally, Some Good News How people live can make a big difference in their risk of becoming hypertensive. Several factors have already proved effective in controlling blood pressure. Other minor influences that can help keep blood pressure under control are continually being discovered.
First, the main actors: diet, weight control and exercise. In a major collaborative study sponsored by the National Heart, Lung and Blood Institute, the so-called DASH diet rich in fruits, vegetables and low-fat dairy products and moderate in fat, saturated fat, red meat, sweets and sugar-containing drinks not only lowered blood pressure, it lowered blood levels of L.D.L. cholesterol and homocysteine, each increasing the risk of heart disease. In a second study, a reduction in dietary sodium combined with the DASH diet was even more effective in lowering blood pressure than DASH alone. The DASH diet can also help prevent another major contributor to hypertension: being overweight. The third main factor in preventing hypertension, regular physical activity, can also help control the second, being overweight. Even among those who already have hypertension, aerobic activities like brisk walking, jogging, lap-swimming and cycling at least five days a week can reduce blood pressure. If nondrug measures are not enough to bring high blood pressure under control, there are now numerous effective and safe drugs that can drastically reduce the risks associated with this condition.
For more information, see the booklet “High Blood Pressure: What You Should Know About It and What You Can Do to Help Your Doctor Treat It,” available on the Web at www.hypertensionfoundation.org.
Cardiovascular disease Diseases of the heart and blood vessels kill more than 17 million people worldwide and account for 30 percent of the total number of deaths each year. Additional millions are disabled, frequently in their prime years. In the U.S., an estimated 79.4 million adults live with cardiovascular disease. Heart disease and stroke, the main cardiovascular diseases, account for one-third of all deaths in the nation.
Decades of research show that lifestyle, beginning in childhood, is the main cause of cardiovascular disease. The major risk factors are high blood pressure, tobacco use, poor dietary habits, especially the intake of saturated fat, elevated blood cholesterol, lack of physical activity, obesity, and diabetes.
Lifestyle changes are the first line of prevention and treatment of cardiovascular disease. Medical interventions range from drugs to surgery. For example, a bypass operation may be performed to reduce a person’s risk of a heart attack. In this operation, a blood vessel from elsewhere in the body is used to reroute blood around a blocked coronary artery (one of two arteries that arise from the aorta and supply the tissues of the heart with blood).
Atherosclerosis This condition is characterized by the deposition of fatty material called plaque on the inner walls of the arteries. As plaque builds up, the arterial channel narrows and blood flow is reduced. Usually there are no noticeable symptoms until plaque buildup is significant. Indeed, the first symptoms may be those of a heart attack or stroke. Treatment options include lifestyle changes, drugs to lower blood pressure or cholesterol, and surgery.
Heart attack A heart attack, or coronary event, occurs when the blood supply to the heart muscles is blocked. An uncomfortable pressure, fullness, squeezing, or pain in the center of the chest that lasts for two minutes or more may be a sign of a heart attack. Sweating, dizziness, nausea, fainting, or shortness of breath may also occur.
Many people who have heart attacks go into sudden cardiac arrest, in which the heart stops beating and begins to fibrillate (quiver). Unless its rhythm is rapidly restored by a defibrillator, the patient’s oxygen-starved brain will begin to die.
Heart failure In this disease, the heart’s pumping power is weaker than normal. Blood moves through the heart and body sluggishly, and pressure in the heart increases. The muscles surrounding the chambers of the heart respond by stretching, which keeps the blood moving but gradually weakens the muscles. The kidneys may then cause the body to retain water and sodium, resulting in fluid buildup in arms, legs, feet, or other organs—a condition known as congestive heart failure. Important warning signs of heart failure include swollen feet and ankles, fatigue, dizziness, rapid or irregular heartbeats, and shortness of breath. Heart failure often is a progressive condition, worsening over time and ultimately fatal. Treatment options include lifestyle changes, medication, and surgery.
Hypertension The pressure of blood against the walls of arteries is recorded as two numbers—the systolic pressure (as the heart beats) over the diastolic pressure (as the heart relaxes between beats). Normal blood pressure is less than 120 milliliters of mercury systolic and less than 80 milliliters mercury diastolic.
About 74.5 million people in the United States age 20 and older have high blood pressure. If left untreated, high blood pressure can lead to strokes, heart attacks, and kidney failure. Conversely, controlling elevated blood pressure can cut strokes 35 to 40 percent and heart attacks 20 to 25 percent. Often, dietary and other lifestyle changes are sufficient to keep blood pressure controlled. If not, if maybe necessary to add blood pressure medications such as diuretics, ACE inhibitors, beta blockers, or calcium channel blockers.
Stroke A stroke occurs when the blood supply to the brain is blocked, usually by a clot. The primary signal of a stroke is a sudden, temporary weakness or numbness of the face, arm, or leg on one side of the body. Other signals include temporary loss of speech, difficulty in speaking or understanding speech, temporary vision problems (particularly in one eye), unsteadiness, sudden severe headache, or unexplained dizziness.
Prompt medical attention may increase a person’s chances of survival and limit the amount of disability. Treatment, involving drugs or surgery, is aimed at stopping the stroke and preventing another stroke.
Blood Pressure Guidelines for Adults*
| Category | Systolic Pressure** | Diastolic Pressure** | |
|---|---|---|---|
| Normal | Less than 120 | and | Less than 80 |
| Prehypertension | 120 to 139 | or | 80 to 89 |
| Stage 1 hypertension | 140 to 159 | or | 90 to 99 |
| Stage 2 hypertension | 160 or greater | or | 100 or greater |
| * Age 18 and older. **Millimeters of mercury. Source: National Heart, Lung and Blood Institute, 2003. | |||
Cerebral palsy This disorder is characterized by damage to the areas of the brain that regulate movement. It results from damage to the brain before, during, or soon after birth. Poor oxygen supply to the brain, trauma, severe dehydration, and maternal infections such as rubella are among the factors that may result in cerebral palsy, but often the precise cause of the damage cannot be identified.
The most common form of the disorder is spastic cerebral palsy, in which the arm and leg muscles become stiff and weak. In the ataxic form, the sense of balance and depth perception are affected, resulting in coordination difficulties and unsteady movements. The choreoathetoid form is characterized by abrupt, jerky, spontaneous movements. Some individuals have symptoms of more than one of these forms, indicating damage to more than one area of the brain; this is called mixed cerebral palsy. The severity of cerebral palsy varies greatly. There is no cure. Drugs, surgery, and therapy are used to minimize its effects.
Cholera The bacterium Vibrio cholerae causes this infectious disease, which is typically spread via contaminated food and drinking water. Cholera is rare in the United States but common in Asia, Africa, and Latin America. For example, an epidemic in Latin America during the 1990’s infected 1.3 million people, killing 12,000.
Symptoms include severe diarrhea and vomiting. Without treatment, the person becomes dehydrated, which can lead to kidney failure, shock, and death. Treatment consists of antibiotics and rapid replacement of fluids. Cholera vaccines are available, but they provide only limited protection; they are not available in the United States.
Common cold More than 200 different viruses, about one-third of them rhinoviruses, cause contagious respiratory illnesses known as the common cold. Generally, an infection is short-lived, lasting about a week. Symptoms include a runny nose, sore throat, sneezing, and occasional coughing. There are no proven preventative measures and no known cure; over-the-counter cold remedies may relieve symptoms.
Cold viruses often spread as infected individuals cough or sneeze, releasing virus-laden droplets in the air. People become infected by breathing in the viruses or touching contaminated items (furniture, clothing, and so on) and rubbing their contaminated hands against their mouth, nose, or eyes. Frequent hand washing and keeping one’s hands away from the mouth, nose, and eyes—where the viruses thrive—help reduce one’s risk of catching a cold.
Congenital problems Congenital disorders are defects or malformations that are present at birth. In many cases, the cause is unknown. However, some factors are associated with an increased chance of developing certain congenital disorders. For example, alcohol or drug abuse during pregnancy or maternal viral infection can increase the risk of congenital heart disease. Down syndrome may cause congenital malformations of the heart or gastrointestinal system.
Treatment is based on the severity of the problem. Mild problems may not require any treatment; others may be treated with medication or surgery.
Dengue fever This infectious disease is caused by four different dengue viruses and transmitted by certain Aedes mosquitoes. Infection with one type of virus produces immunity only to that type; a person may later become infected by another dengue type. Symptoms include fever, headache, vomiting, and severe joint and muscle pain. Symptoms typically disappear within a week, and the disease is rarely fatal. There is a form known as dengue hemorrhagic fever which is much more dangerous and causes bleeding as capillaries burst. No cure for the diseases have yet been developed; treatment is mostly palliative—making patients as comfortable as possible and encouraging them to drink large amounts of fluids.
Worldwide, an estimated 50–100 million cases of dengue fever and up to hundreds of thousands of cases of dengue hemorrhagic fever occur each year. Most cases are in tropical and subtropical regions, particularly Southeast Asia. Cases in the United States are usually brought in from other countries.
Diabetes Diabetes mellitus is a group of diseases characterized by high blood sugar levels that result from the body’s inability to make or use insulin, a hormone produced by the pancreas that plays a vital role in metabolism. Symptoms include increased thirst and urination, hunger, weight loss, fatigue, and blurred vision. Diabetes can lead to debilitating and life-threatening complications including blindness, memory problems, kidney disease, heart disease, nerve damage, and amputations.
The most common type is type 2 diabetes, previously called adult-onset diabetes. It usually develops because the body fails to use insulin properly. It occurs in people, including children, who are overweight; other risk factors include high cholesterol, high blood pressure, ethnicity, and a family history of diabetes. Treatment includes a healthy diet, weight loss, and regular exercise. Many patients require daily insulin injections.
Times focus
Vast Gene Study Yields Insight on Alzheimer’s
The two largest studies of Alzheimer’s disease have led to the discovery of no fewer than five genes that provide intriguing new clues to why the disease strikes and how it progresses. Researchers say the studies, which analyzed the genes of more than 50,000 people in the United States and Europe, leave little doubt that the five genes make the disease more likely in the elderly and have something important to reveal about the disease’s process. They may also lead to ways to delay its onset or slow its progress. The discoveries double the number of genes known to be involved in Alzheimer’s, to 10 from 5, giving scientists many new avenues to explore. The two studies were published in the journal Nature Genetics in April 2011.
For years, there have been unproven but persistent hints that cholesterol and inflammation are part of the disease process. People with high cholesterol are more likely to get the disease. Strokes and head injuries, which make Alzheimer’s more likely, also cause brain inflammation. Now, some of the newly discovered genes appear to bolster this line of thought, because some are involved with cholesterol and others are linked to inflammation or the transport of molecules inside cells.
An estimated 5.4 million Americans have Alzheimer’s disease, most of whom are elderly. According to the Alzheimer’s Association, one in eight people over age 65 have the disease. Its annual cost to the nation is $183 billion.
By themselves, the genes are not nearly as important a factor as APOE, a gene discovered in 1995 that greatly increases risk for the disease: by 400 percent if a person inherits a copy from one parent, by 1,000 percent if from both parents. In contrast, each of the new genes increases risk by no more than 10 to 15 percent; for that reason, they will not be used to decide if a person is likely to develop Alzheimer’s. APOE, which is involved in metabolizing cholesterol, “is in a class of its own,” said Dr. Rudolph Tanzi, a neurology professor at Harvard Medical School and an author of one of the papers.
But researchers say that even a slight increase in risk helps them in understanding the disease and developing new therapies. And like APOE, some of the newly discovered genes appear to be involved with cholesterol.
Of the 10 genes now known to be associated with Alzheimer’s in old age, four were found in the past few years and are confirmed by the new studies. APOE may have other roles in the disease, perhaps involved in clearing the brain of amyloids that pile up in plaques, the barnacle-like particles that dot the brain of Alzheimer’s patients and are the one unique pathological feature of the disease.
It is known that one of the first signs of Alzheimer’s disease is an accumulation of beta amyloid, or a-beta, a protein that forms plaques.And it is known that later in the disease, twisted and tangled proteins—tau—appear in dead and dying nerve cells. But what is not known is why a-beta starts to accrue, why the brains of people with Alzheimer’s cannot get rid of its excess, or what is the link between amyloid and tau.
The American study got started about three years ago when Gerard D. Schellenberg, a pathology professor at the University of Pennsylvania, went to the National Institutes of Health with a complaint and a proposal. Individual research groups had been doing their own genome studies but not having much success, because no one center had enough subjects. So Dr. Schellenberg set out to gather all the data he could on Alzheimer’s patients and on healthy people of the same ages. The idea was to compare one million positions on each person’s genome to determine whether some genes were more common in those who had Alzheimer’s. He got what he wanted: nearly every Alzheimer’s center and Alzheimer’s geneticist in the country cooperated. Dr. Schellenberg and his colleagues used the mass of genetic data to do an analysis and find the genes and then, using two different populations, to confirm that the same genes were conferring the risk. That helped assure the investigators that they were not looking at a chance association.
Type 1 diabetes, formerly called juvenile diabetes, usually develops in childhood. It is caused by the inability of the pancreas to produce insulin. Genetic predisposition combined with exposure to viruses are the main risk factors. Treatment consists of carefully monitored insulin replacement, typically via needles or a special pump.
A small percentage of pregnant women develop gestational diabetes as a result of changing hormonal levels. Blood sugars often return to normal after delivery, but almost half of the women who experience gestational diabetes develop type 2 diabetes later in life.
The World Diabetes Foundation reported in 2010 that 285 million people worldwide had diabetes, mostly Type 2, with almost 80 percent of the total in developing countries. The number is expected to grow to 438 million by 2030, nearly 8 percent of the adult population.
Diphtheria The bacterium Corynebacterium diphtheriae causes this highly contagious infectious disease, which is spread mainly by coughing. Once a leading childhood disease, diphtheria is now rare in developed countries due to widespread vaccination.
Symptoms include sore throat, fever, coughing, and headache. As the disease progresses, tissues in respiratory passages may swell, making breathing difficult. The toxin produced by the bacteria may damage nerves and the heart muscle, leading to heart failure and death. Treatment consists of antibiotics to kill the bacteria and antibodies to neutralize the toxin.
Eating disorders Several mental health disorders are characterized by insufficient or excessive consumption of foods. These disorders are much more prevalent among females, particularly teenage girls and young women, than among males, although recent evidence suggests higher incidence in males than previously realized.
People who starve themselves because of a pathological fear of weight gain suffer from anorexia nervosa. Excessive weight loss and malnutrition result, and anorectics have many symptoms associated with chronic starvation, including low blood pressure, slow heartbeat, constipation, osteoporosis, weakened immunity, and failure to menstruate. Treatment is often difficult, and death occurs in about 5 percent of cases.
Bulimia nervosa is an abnormal, rapid consumption of large amounts of food (bingeing) followed by self-induced vomiting or the use of laxatives to get rid of the food (purging). The person may experience rapid fluctuations in weight, but the weight generally remains close to normal. Other symptoms may include swollen salivary glands, erosion of tooth enamel, dehydration, and electrolyte imbalances. Treatment generally includes psychiatric counseling to break the binge-purge cycle.
Some Food-borne Bacteria That Can Cause Serious Illnesses
| Bacteria | Serious illnesses that can result | Foods in which the bacteria may be found |
|---|---|---|
| Campylobacter | Arthritis; blood poisoning; Guillain-Barre syndrome (paralysis); chronic diarrhea; meningitis; inflammation of the heart, gallbladder, pancreas, and colon | Poultry, raw milk, meat |
| E. coli O157:H7 | Kidney failure, neurologic disorders | Meat, especially ground beef; raw milk; produce |
| Listeria | Meningitis, blood poisoning, stillbirths | Soft cheese and other dairy products; meat, including poultry; seafood; fruits and vegetables |
| Salmonella | Arthritis, blood poisoning; inflammation of joints, heart, thyroid, pancreas, spleen, gallbladder, and colon | Meat, including poultry; eggs; dairy products; seafood; fruits and vegetables |
| Shigella | Kidney failure, neurologic disorders, pneumonia, blood poisoning, inflammation of the joints and spleen | Salads, milk and other dairy products, fruits and vegetables |
| Vibrio vulnificus | Blood poisoning | Seafood |
| Yersinia enterocolitica | Pneumonia; inflammation of the joints, vertebrae, lymphatic glands, liver, and spleen | Pork, dairy products |
Binge eating disorder is characterized by eating abnormally large amounts of food, which leads to significant weight gain. People with this problem tend to be older than anorectics and bulimics, and their numbers are more evenly divided among men and women. Treatment consists of behavior therapy.
Emphysema This debilitating, often fatal disease is characterized by the enlargement and destruction of alveoli—the tiny air sacs that make up the lungs. This obstructs the exchange of oxygen and carbon dioxide with the blood, leading to coughing, breathing difficulties, rapid heartbeat, and—in advanced cases—mental problems. Smoking is the most important cause of emphysema. Air pollution also increases the risk.
Damage caused by emphysema cannot be reversed. However, regular exercise, medication, and giving up smoking can slow progression of the disease. A lung or heart/lung transplant may be used in certain severe cases.
Encephalitis Encephalitis is a viral inflammation of the brain. While some infections are mild, with few if any specific symptoms, others can be deadly. Early symptoms often include headaches, fever, and nausea. If the disease progresses, the person may suffer seizures, paralysis, mental confusion, and coma. Often the disease is accompanied by viral meningitis.
Mosquitoes carry some of the most dangerous types of encephalitis, including equine encephalitis, West Nile encephalitis, and St. Louis encephalitis. In other cases, encephalitis develops as a secondary complication of other viral diseases, including chickenpox, herpes, mumps, polio, and rubella. Treatment depends on the type and severity of the disease. It may include antiviral drugs and steroids to combat brain swelling.
Food-borne illnesses An estimated 76 million illnesses caused by food poisoning occur in the United States each year. Generally, the result is diarrhea and other temporary disorders of the digestive tract. But the illnesses can lead to more serious consequences, including about 325,000 hospitalizations and 5,000 deaths in the United States each year. People most at risk are pregnant women, children, those with compromised or suppressed immune systems, and the elderly.
Most food-related illnesses can be avoided—by washing fresh fruits and vegetables, cooking meat thoroughly, drinking only pasteurized milk, and common-sense hygiene.
Microbial contamination is the most common cause of food-borne illnesses. Pesticides, heavy metals, and other chemical agents that enter the food supply can also cause gastrointestinal, as well as neurologic and respiratory, symptoms.
(See also “Prion diseases” and “Worms and disease.”)
Genetic diseases Hundreds of diseases are due wholly or in part to genetic errors—mutations in genes that result in physical, chemical, or mental abnormalities. Genes work in pairs; in many cases, one form of the gene is stronger, or dominant, while another form is weaker, or recessive. If an individual inherits a mutated dominant gene or two copies of a mutated recessive gene, the result may be an inherited disease or increased susceptibility to disease. For example, Tay-Sachs disease is caused by a single recessive gene; the recessive gene must be inherited from both parents for the disease to develop. Although genetic diseases usually are inherited from parents, they also can appear as a result of a new mutation in either the mother’s egg or father’s sperm.
Abnormal genes on the X chromosome cause x-linked diseases. A female inherits two X chromosomes, one from each parent. A male inherits an X chromosome from his mother and a Y chromosome from his father. If the male inherits an abnormal gene on the X chromosome, the gene will express itself. Hemophilia is a well-known example. The genes responsible are located on the X chromosome. A female must inherit two copies of a recessive form to develop hemophilia, but a male need inherit only one.
In some cases, genetic disease occurs because an individual receives an abnormal number of chromosomes (the structures on which genes are located). For example, in Klinefelter syndrome, a male is born with an extra X chromosome.
Often, multiple genes may be involved in any one disease. For example, scientists have identified nearly 400 cancer-related genes plus evidence that multiple genes may contribute to development of Parkinson’s disease. Many disorders are believed to have a genetic component even though this has not yet been proven.
Hemorrhagic fevers These dangerous viral infections are characterized by bleeding (hemorrhaging). Each is commonly linked to a specific geographic region. For instance, outbreaks of Lassa fever have been limited to West Africa, while hantavirus pulmonary syndrome occurs mostly in the western United States. As a group, they are most common in tropical regions. The diseases spread to humans in various ways. Lassa fever and hantavirus are carried by rodents and spread in their droppings and saliva. Ebola, an exceptionally virulent African disease, is usually
spread via the blood or secretions of an infected person.
The first symptoms of hemorrhagic fevers are flulike, including fever, headache, nausea, and fatigue. The symptoms may be mild and taper off after several days or become increasingly severe. Not all cases progress to hemorrhaging. Fatality rates vary with the disease. Treatment is mostly palliative; maintaining appropriate fluid balance, blood pressure, and oxygen status is often critical.
Hepatitis Inflammation of the liver, called hepatitis, can be caused by excessive alcohol use or the use of certain medications. However, hepatitis usually results from one of several unrelated viruses. In the United States, hepatitis viruses A, B, and C are most prevalent. Hepatitis E occurs mostly in tropical regions, causing large epidemics on the Indian subcontinent, in Central and Southeast Asia, in the Middle East, and in parts of Africa. Hepatitis can be acute (short-term) or chronic (long-term).
Hepatitis A is spread primarily by fecal contamination of food and water and through person-to-person contact. Inflammation lasts only a few weeks and may be asymptomatic, which makes its frequency difficult to estimate. People who have had the disease do not get it again. Vaccines can prevent the disease; since their introduction there has been an 84 percent decline in reported cases.
Hepatitis B is generally transmitted via contact with the blood of an infected person during sex, during birth, or through contaminated needles and syringes. It can cause a chronic infection leading to cirrhosis of the liver, liver cancer, liver failure, and death. A vaccine is available, and medical groups recommend that all newborns be vaccinated. W.H.O. estimates that more than 350 million people worldwide are chronically infected with hepatitis B.
Well-known Genetic Diseases
| Disease | Cause | Symptoms |
|---|---|---|
| Cystic fibrosis | Mutated recessive gene | Glands produce abnormal secretions, resulting in lung inflammation, infection, and damage. |
| Down syndrome | Extra copy of chromosome 21 | Physical abnormalities, mental retardation. |
| Fragile-X syndrome | Mutated recessive gene on X chromosome | Mental retardation. |
| Hemophilia | Mutated recessive gene on X chromosome | Blood does not clot properly; excessive bleeding from small wounds and increased susceptibility to bruising. |
| Huntington’s disease | Mutated dominate gene | Deterioration of nerve cells in the brain, interfering with mental abilities and control of muscles. |
| Klinefelter syndrome | Extra copy of X chromosome in male | Problems with speaking and language skills. |
| Muscular dystrophy | Depends on the form; the two most common, Duchenne muscular dystrophy and Becker muscular dystrophy, are caused by a mutated recessive gene on the X chromosome. | Progressive weakening and deterioration of muscles. |
| Polycystic kidney disease | Depends on the form; the more common inherited form is caused by a mutated dominant gene. | Formation of numerous clusters of cysts on the kidneys reducing kidney function and resulting in kidney failure. |
| Sickle cell anemia | Mutated recessive gene | Misshapen (“sickled”) red blood cells, causing insufficient oxygen delivery to cells. |
| Tay-Sachs disease | Mutated recessive gene | Inability to produce a vital enzyme, resulting in progressive damage to the nervous system. |
| Von Willebrand’s disease | Mutated dominant gene | Abnormal blood clotting, with excessive bleeding from small wounds and increased susceptibility to bruising. |
| Wilson’s disease | Mutated recessive gene | Inability to process copper, resulting in progressive damage to the liver and other organs |
Hepatitis C is spread through exposure to infected body fluids. Major risks include unprotected sex and sharing contaminated needles. No vaccine is available. W.H.O. estimates that 170 million people are chronic carriers. In the United States, hepatitis C is the leading cause of chronic liver disease and the main reason for liver transplants.
Influenza Several types of viruses cause this highly contagious disease, commonly called the flu. The viruses are spread from one person to another via airborne droplets released during coughing and sneezing. They lodge in the lungs and breathing passages, causing fever, chills, sore throat, coughing, headache, fatigue, and weakness. Most symptoms subside in several days, but complications, particularly pneumonia, can occur. Treatment consists of bed rest and plenty of fluids; antiviral drugs may be prescribed.
Vaccination to avoid infection is strongly recommended for children age 6 months to 5 years; people age 50 and older; people with heart disease, diabetes, or immune system problems; residents of nursing homes; family members and caregivers of such individuals; and health care workers. Unfortunately, the flu vaccine only protects against certain viral strains; evolution of a new strain can result in a worldwide epidemic. One of the worst such epidemics, the 1917–18 “Spanish flu,” killed some 20 million people. An even deadlier epidemic is feared if the virulent H5N1 avian influenza virus mutates into a form able to spread easily among humans.
Leprosy (Hansen’s disease) Known since ancient times, leprosy is a chronic disease caused by the bacterium Mycobacterium leprae. Once widespread, the number of infected people has declined rapidly since the early 1990’s. According to WHO, improved diagnosis and treatment sharply reduced the number of leprosy cases in recent years, to about 212,000 at the beginning of 2010. However, as many as 2 million people were disabled due to past and present leprosy. Of the approximately 100 new cases of leprosy identified in the United States each year, the vast majority develop among immigrants who acquired the disease in their home countries.
Although infectious, leprosy is not very contagious. In most people, the immune system easily fights off the bacteria. Leprosy primarily damages the skin, peripheral nerves, eyes, and mucous membrane of the upper respiratory system, resulting in numbness, muscle weakness, blindness, and internal damage to the nose. Left untreated it can cause permanent disfigurement, especially of the face, hands, and feet, which historically cause people to fear the afflicted and expel them from society. Today, the disease is easy to treat with a combination of antibiotics.
Lyme disease Named after Lyme, Connecticut, where it was first reported, Lyme disease is caused by the spirochete bacterium Borrelia burgdorferi. It is transmitted to humans through the bite of ticks, including the deer tick Ixodes dammini. Its symptoms often mimic those of other diseases, and may include pain, diarrhea, nausea, swollen glands, difficulty swallowing, and coughing. A rash may appear several days after infection; the hallmark of Lyme disease is a bull’s-eye rash—a round ring with a central clearing. As the disease advances, it may produce a painful joint condition known as Lyme arthritis.
Prevention includes performing tick checks after walking in woods and other areas infested with ticks. Vaccines are available, but they are not completely effective. Antibiotics usually cure the illness.
Malaria This infectious disease is caused by single-celled Plasmodium protists, including P. falciparum, P. vivax, P. malariae, and P. ovale. The parasites are usually transmitted from infected to noninfected people via the bite of female Anopheles mosquitoes; about 60 species of Anopheles can serve as vectors. The parasites take up residence in the victim’s red blood cells.
The disease is characterized by episodes of chills and fever followed by profuse sweating; shaking and fatigue are other common symptoms. Repeated bouts can result in severe anemia, dehydration, and death. Infants, children, and pregnant women are at greatest risk of severe illness and death.
Treatment with chloroquine or other drugs that kill the Plasmodium has become more difficult in recent years. The parasites have become resistant to the drugs, and the Anopheles mosquitoes have become resistant to insecticides. Several candidate vaccines are being developed and show promise in early trials.
Malaria is most common in tropical and subtropical lands, particularly sub-Saharan Africa and Southeast Asia. It is both a cause of poverty and a result of poverty. Each year, between 350 million and 500 million acute cases are diagnosed and at least 1 million people, mostly African children younger than 5 years old, die of the disease. Almost all of the approximately 1,000 Americans who contract malaria each year get the disease while traveling abroad.
Measles (rubeola) An itchy rash consisting of small, reddish raised spots characterizes this highly contagious viral disease. Measles epidemics were once common, afflicting thousands of people, particularly young children, annually. Since the 1960’s vaccination has greatly reduced its incidence, to 100 or fewer cases a year in the United States. People who contract measles develop a natural immunity to the disease.
Initial symptoms include fever, coughing, a runny nose, and red eyes. Several days later the rash begins, usually on the face and neck and then spreading to the trunk and limbs. The rash typically fades in about a week. Treatment is palliative, keeping the patient comfortable while his or her immune system combats the virus.
In some cases, secondary bacterial infections or viral encephalitis develop. As a result, measles is sometimes, though rarely, fatal.
Meningitis This is an inflammation of the membranes (called meninges) that envelop the brain and spinal cord. It can result from a broad variety of bacterial, viral, fungal, and protozoan infections, including AIDS, brucellosis, cat-scratch disease, chickenpox, herpes, Lyme disease, malaria, mumps, rubella, syphilis, toxoplasmosis, trichinosis, and tuberculosis. The viruses that cause encephalitis can also infect the meninges.
Early symptoms include headache if the meninges around the brain are infected, and back pain if the spinal cord is infected. If the disease progresses, the patient may experience fever, vomiting, confusion, paralysis, and coma. Treatment depends on the causative agent and disease severity; it may include antibiotics (bacterial meningitis) or other medications.
Meningitis can also have noninfectious causes: brain disorders (cancer, multiple sclerosis, stroke), medications (including nonsteroidal anti-inflammatory drugs such as ibuprofen and naproxen), lead poisoning, and adverse reactions to antibiotics, chemotherapy, and certain vaccines. These cases usually are mild and do not require treatment.
Mental illness Among the commonest illnesses are those characterized by impaired psychological functioning and a significantly decreased ability to cope with emotions, thinking, and other basics of everyday life. According to the National Institute of Mental Health, four of the 10 leading causes of disability in the United States and other developed countries are mental disorders: major depression, bipolar disorder, schizophrenia, and obsessive-compulsive disorder. The institute has indicated that an estimated 22 percent of Americans age 18 and older—more than 44 million people—suffer from a diagnosable mental disorder in a given year. (See also “Psychology.”)
The causes of mental illness are gradually being identified. Some illnesses involve abnormal brain chemistry, such as an excess or deficiency of the neurotransmitter dopamine. Others develop after great trauma, such as that caused by child abuse, rape, or war. Genetics appears to play an important role and viruses are suspected of triggering or causing at least some problems.
Treatment generally involves medications, psychotherapy, or some combination of the two.
Anxiety disorders Excessive, chronic apprehension, tension, or uncertainty resulting from imagined or unreal threats are the hallmarks of anxiety disorders. The illnesses include general anxiety disorder, obsessive-compulsive disorder, panic disorder, phobias, and post-traumatic stress disorder.
Attention deficit/hyperactivity disorder (ADHD) ADHD, characterized by inattention and hyperactivity, is the most treated childhood-onset mental disorder in the United States, where it affects 3 to 5 percent of school-age children. Boys are two to three times more likely than girls to have ADHD. Many children with ADHD retain symptoms into adulthood. Additionally, many adults with attention-deficit disorder (ADD) probably had the illness when young but its symptoms weren’t obvious or the problem wasn’t correctly diagnosed.
Autism Evidence of this developmental disorder appears by the age of three. Autistic individuals have difficulty relating emotionally to other people, difficulty in communicating with others, and poor cognitive and language skills. They exhibit compulsive, ritualistic behavior and are easily upset by even slight changes in their surroundings or daily schedule.
Asperger’s syndrome is a comparatively mild autistic disorder characterized by normal intelligence and language development but impaired social and non-verbal communications skills.
Depression Depression is marked by feelings of extreme sadness, hopelessness, and inadequacy. Individuals often experience disturbed sleep and weight change. Most people who commit suicide suffer from depression.
Bipolar disorder, formerly known as manic depression, is characterized by alternating periods of abnormally intense elation and depression, with episodes lasting a week or longer.
Dissociative disorders Individuals separate, or dissociate themselves from, their identity and other aspects of their personality. They may have multiple personalities,
each with its own set of temperaments, responses, and even memories. Dissociation is believed to be a mechanism for coping with physical abuse or other severe trauma.
Schizophrenia A loss of contact with reality, irrational fears, delusions, hallucinations, bizarre behavior, and a restricted range of emotions characterize schizophrenia. Both genetic and environmental factors appear to be involved in causing the disorder, with severity varying significantly among individuals.
Oral diseases A normal person’s mouth harbors some 400 species of bacteria, which combine with saliva to form a sticky, colorless film called plaque. The plaque accumulates on teeth and gums, as does its hardened product, tartar. This leads to tooth decay and periodontal (gum) disease. Many of these problems can be prevented by good oral hygiene, including daily brushing and flossing as well as regular checkups in which the dentist or dental hygienist removes plaque. Proper diet and avoidance of tobacco also help keep teeth and gums healthy.
Periodontal disease is the most frequent cause of tooth loss in adults. It is progressive; the earlier it is treated, the less the damage. In its early form, called gingivitis, plaque builds up along the gum line; toxins released by the bacteria cause the gums to become red, swollen, and prone to bleeding. In the advanced stages of the disease, called periodontitis, the bacterial toxins deepen the openings between the gums and the roots of the teeth, and corrode the bone and ligament that anchor the teeth in the jaw.
In addition, periodontal disease can easily release bacteria into the bloodstream. This can exacerbate problems in other parts of the body. For instance, people with periodontal disease are more likely to suffer a stroke or fatal heart attack than those without periodontal disease.
Other common oral diseases include small sores called cankers and cold sores. Cankers, of unknown cause, form singly or in clusters and generally heal by themselves. Cold sores, caused by the Herpes simplex virus, are highly contagious; acyclovir ointment fights the virus and aspirin or ointment containing benzocaine may help relieve pain. Trench mouth is a painful inflammation of the gums caused by bacteria whose rapid growth is triggered by stress, poor diet, smoking, or other factors. Treatment options include careful cleaning of teeth, painkillers, and antibiotics.
Osteoporosis This condition is characterized by a progressive decrease in bone density. The person may experience back pain, stooped posture, increased curvature of the spine, and an ever-greater likelihood of fractures. Aging, physical inactivity, poor nutrition, smoking, and genetics are major risk factors. The disease is particularly common in post-menopausal women, partly because women start out with lower bone mass. An estimated 44 million Americans have osteoporosis. Millions more have low bone mass and thus are at risk of developing the disease.
Prevention should begin in childhood, with a diet containing sufficient calcium and vitamin D, both critical for building strong bones. Weight-bearing and strength-building exercises are important throughout life. Calcium and vitamin D supplements help build and maintain bone mass. Certain medications, including alendronate and raloxifene, slow bone loss and may help increase bone density.
Parkinson’s disease This degenerative disease, which usually begins between ages 45 and 65, is characterized by the gradual deterioration of brain cells that control muscles. The cells stop producing the chemical dopamine, which serves as a messenger to transmit impulses from one nerve cell to the next. As dopamine production is reduced, the person experiences tremors in a hand. Tremors may gradually appear in the other hand as well as the arms and legs. As the disease progresses, muscle stiffness, difficulty walking, stooped posture, reduced sense of smell, and decreased facial expression become noticeable. About 50 percent of the people develop dementia.
The cause of Parkinson’s disease is unknown. Nor is there a known cure. Treatment is designed to slow progression and reduce the severity of tremors.
Parkinsonism is a disorder with similar characteristics except that its causes are known. These include viral encephalitis, head injury, brain tumors, use of the illicit drug MPTP, and certain medications that interfere with the action of dopamine. Treating the underlying problem may result in a cure.
Pneumonia Various bacteria, viruses, and fungi cause this inflammatory lung disease. Common symptoms include coughing that produces sputum, which may contain blood; fever; chills; and chest pain. Severity ranges from mild to life threatening. For example, so-called walking pneumonia is a mild form of bronchial pneumonia that infects a relatively small area of the bronchi. In contrast, double pneumonia involves inflammation of both lungs. More than 54,000 Americans die from pneumonia each year; worldwide it is a leading cause of death in young children.
Vaccines are available to prevent certain types of pneumonia and are recommended for people who are particularly
susceptible to the disease, including individuals age 65 and older. Antibiotics are used to treat bacterial pneumonia but are not effective against viral pneumonia. Antifungal drugs are used to fight pneumonia caused by fungi.
In addition to microscopic organisms, pneumonia can be caused by inhaling food, liquids, or toxic chemicals. A common form of such aspiration pneumonia develops after a person inhales stomach acid during vomiting.
Poliomyelitis “Polio” is an infectious disease caused by three types of polioviruses that attack the central nervous system. The great majority of people who are infected are asymptomatic or experience only mild flulike symptoms that disappear in a few days and require no medical intervention. They are, however, a potential threat for others because polioviruses are excreted in their feces.
A small percentage of people develop major polio, with weakness or paralysis developing in certain muscles. Permanent disability can result, though often may be prevented or limited through an intensive program of physical therapy, to rebuild and maintain strength and muscle tone.
Polio is highly contagious and was once widespread in the United States. Vaccines introduced beginning in 1955 eradicated polio in the United States and the rest of the Western Hemisphere and are now part of routine childhood immunizations. Since 1988 the World Health Organization has led a worldwide vaccination effort to eliminate polio completely. The number of cases has been reduced from an estimated 350,000 in 1988 to 1,300 in 2010.
Prion diseases Misfolded proteins called prions appear to be the cause of a group of degenerative diseases of the central nervous system known as transmissible spongiform encephalopathies (TSEs). Prions are not organisms; they have no cell structure and no genetic material (DNA or RNA). They are infectious, however; prions can pass to humans and certain animals that eat the remains of infected organisms. The prions may incubate for years before beginning to destroy brain tissue, leaving parts of the brain porous and spongy and leading to dementia and loss of muscle control.
The best-known TSE is bovine spongiform encephalopathy (BSE)—so-called mad cow disease. In 1996 it was discovered that BSE can pass from infected meat to humans. The humans develop a disease similar to the TSE Creutzfeldt-Jakob disease (CJD), called variant CJD (vCJD). Other human TSEs are kuru, Gerstmann-Straussler syndrome, and fatal familiar insomnia. All are rare but fatal.
Rocky Mountain spotted fever Caused by the bacterium Rickettsia rickettsii and spread by ticks, Rocky Mountain spotted fever causes high fever, headache, fatigue, and a rash that spreads across most of the body. Some 2,500 cases were reported in the United States in 2008. If treated early with antibiotics, a patient usually recovers without serious problems. But if treatment is delayed, complications may include damage to the heart, lungs, liver, and kidneys.
Rubella Also known as German measles, rubella is a contagious viral disease that prior to the introduction of a vaccine in 1969 was very common among children. Its symptoms are mild and include low fever, swollen lymph nodes, and a rash. Treatment includes rest, fluids, and painkillers. Rubella infection poses serious problems for women in the early stages of pregnancy. The virus can pass through the placenta to the fetus, causing miscarriage, stillbirth, or permanent mental and physical disabilities in the infant.
Sexually transmitted diseases (STDs) The United States has the highest rates of STDs in the industrialized world, some 50 to 100 times higher than in other industrial nations. An estimated 15.3 million new cases of STDs are reported each year in the United States, with roughly half of these incurable. STDs are difficult to track, in part because many infected people do not have symptoms and remain undiagnosed, though able to infect other individuals.
The most prevalent STD in the United States, infecting some 45 million people, is genital herpes, caused by a virus. It is followed by human papillomaviruses (HPV), which cause genital warts and cervical cancers; chlamydia, caused by a bacterium; trichomoniasis, caused by a protozoan; and gonorrhea, caused by a bacterium. Syphilis is another STD caused by a bacterium; the number of cases has declined significantly but the disease remains a significant problem in certain areas.
People who have STDs have a significantly increased risk of becoming infected with HIV, the virus that causes AIDS, in part because they may have open sores that provide the virus with an easy route of entry to the body.
Prevention—practicing safe sex—is of critical importance in controlling the spread of STDs. Most STD cases caused by bacteria can be treated with antibiotics, although strains of gonorrhea bacteria resistant to common antibiotics have increased greatly in recent years. There is no known cure for viral STDs but a vaccine that protects against four HPV types that together cause 70 percent of cervical cancers and 90 percent of genital warts,
was introduced in 2006; it is recommended for girls and women before they become sexually active.
In addition to STDs, some other diseases can be sexually transmitted. These include amebiasis, giardiasis, hepatitis, salmonellosis, scabies, and shigellosis.
Shingles This is a very common and intensely painful skin rash caused by the same varicella-zoster virus that causes chicken pox. After a case of chicken pox, the virus may reside in sensory nerves; it remains dormant for decades but may then emerge as shingles, usually in people age 50 or older whose immune system begins to weaken. The disease is treated with antiviral drugs such as acyclovir. A vaccine for shingles was introduced in 2006; in clinical trials it prevented shingles in about 50 percent of people age 60 and older.
Smallpox This is a highly contagious, deadly disease caused by Variola viruses. Its symptoms include high fever, headache, muscle pain, and a rash that develops into oozing pustules that contain viruses able to infect others. People who recover have permanent scars from the pustules.
Smallpox once caused deadly epidemics. In the 20th century alone, experts estimate, it took up to a half billion lives. But by 1979, due to worldwide vaccination programs, smallpox had been eradicated in nature. By 2002 the only known stocks of Variola were kept in research laboratories in the United States and Russia, although there are fears that samples may have slipped into the hands of other countries or terrorists.
Tuberculosis (TB) TB, which usually infects the lungs, is caused by the bacterium Mycobacterium tuberculosis. Except for young children, few people become ill soon after M. tuberculosis enters their body. Their immune system kills most of the bacteria. The rest of the bacteria are confined by white blood cells, not causing problems but remaining alive in a state of dormancy. In most cases, these bacteria do not cause any problems. But if a person’s immune system is compromised by poor nutrition, unhealthy living conditions, aging, cancer, or certain infections, the bacteria may start to multiply; the person becomes sick and can spread the germs when he or she coughs or sneezes.
Left untreated, TB gradually destroys the lungs. Treatment consists of at least six months of daily antibiotic therapy; generally, this results in a complete cure. However, many patients stop taking the drugs after several weeks because their symptoms disappear. Not only do they risk developing active TB in the future, but they increase the likelihood that the TB they develop, and pass on to others, will be drug-resistant and difficult to treat. Since the mid-1990’s, W.H.O. has recommended “directly observed treatment strategy” (DOTS), in which health care workers watch patients take their medications to ensure the antibiotics are taken as instructed.
Approximately 11,000 cases of TB are reported in the United States each year, more than half of them among foreign-born individuals. About 98 percent of the world’s new TB cases occur in developing countries, and each year nearly 2 million people die from the disease. Incidence has surged in Africa, taking advantage of the vulnerability of people with HIV/AIDS.
Typhoid Also known as enteric fever, typhoid is caused by the bacterium Salmonella typhi. It is spread via food or liquids contaminated with the feces and urine of infected people. The disease causes flulike symptoms, including headache, joint pain, and prolonged fever. If untreated, complications such as pneumonia and internal bleeding may occur. Treatment consists of antibiotics. Although rare in developed nations, it is estimated that each year there are 17 million typhoid cases worldwide, with 600,000 deaths. Multidrug resistant strains of S. typhi have been reported in parts of Asia, Latin America, and the Middle East, where the disease is common.
Vitamin-related diseases Consuming too little or too much of a vitamin can interfere with cell building and other basic physiological processes, resulting in potentially fatal disease. For instance, a lack of biotin (a B vitamin) causes skin problems, nausea, and depression. Too much vitamin A can cause liver and nerve damage, dry skin, hair loss, blurred vision, and birth defects.
Vitamin deficiency diseases are most common in poor lands where proper nutrition is difficult to achieve. However, these diseases are not unknown in the United States and other developed countries. For instance, alcoholics are at high risk of vitamin B1 and folic acid deficiencies. Also, certain diseases such as cystic fibrosis and Crohn’s disease interfere with absorption of some vitamins; this problem, like other vitamin deficiencies, can be resolved with vitamin supplements.
Worms and disease A variety of parasitic worms can take up residence in the human body. They commonly enter through the skin or via contaminated food and water. Depending on the parasite and the number of worms present, an infected person may be asymptomatic, have mild symptoms, or experience life-threatening difficulties.
Guinea worms The worm Dracunculus medinensis causes guinea worm disease, or dracunculiasis. People become infected by drinking water contaminated with Dracunculus larvae. In the body, the worms grow to adults up to 3 feet (90 centimeters) long. The worms migrate to the surface of the body and a blister and ulceration develop on the skin where each worm emerges. The person typically experiences painful swelling, fever, nausea, and vomiting. Ulcers often become infected with bacteria, which causes disabling complications. A worm can be removed surgically or by slowly pulling it out—a process that can take months. No medication is available to prevent or treat infection.
People in poor communities in remote parts of Africa are most commonly affected by Guinea worm disease. An international effort to eradicate the disease was begun in 1986. By 2002, as a result of educating and encouraging people to make the behavioral changes necessary to stop disease transmission, the number of infected individuals was reduced by 98 percent, from 3.5 million to fewer than 3,200 reported cases in 2010.
Hookworms Almost 1 billion people who live in moist tropical and subtropical areas where sanitation is poor are infected with small roundworms of the genera Necator and Ancylostoma. Worm larvae present in the soil can penetrate the skin and travel to the intestines, where they mature; the adult worms produce huge numbers of eggs that are excreted in feces. Abdominal pain and diarrhea are common symptoms; however, many infected people are symptomless. Oral medications are available to treat the infection.
Selected Vitamin-Deficiency Diseases
| Disease | Cause | Major Symptoms |
|---|---|---|
| Beriberi | Vitamin B1 (thiamine) deficiency | Muscle cramps, nerve or heart abnormalities; in advanced cases, coma and death. |
| Night blindness | Vitamin A deficiency | Difficulty seeing in dim light; can cause blindness. |
| Pellagra | Niacin (a B vitamin) deficiency together with a deficiency of the amino acid tryptophan | Rash and other skin abnormalities, diarrhea, nausea; in advanced cases, mental problems and death. |
| Rickets | Vitamin D deficiency | Abnormal bone growth, weakened bones. |
| Scurvy | Vitamin C deficiency | Swollen gums, loose teeth, infection, irritability, bleeding, anemia. |
Pinworms Pinworm infection, or enterobiasis, is caused by certain roundworms that live in the intestine. Infections are common among children, who typically ingest the worms when sucking their thumbs or eating food contaminated with fecal matter. Itching in the anal or vaginal area is the most common symptom. Infections can be cured with medication, but children are often reinfected.
Schistosomiasis Also known as bilharziasis, schistosomiasis is caused by several species of the flatworm Schistosoma. People become infected by swimming or bathing in contaminated freshwater. Once established in a person’s body, the worms produce great numbers of eggs, which elicit an immune system response. This eventually results in internal bleeding and irreversible tissue damage. Globally, an estimated 200 million people are infected, mainly in the tropics and subtropics. About 120 million show symptoms of schistosomiasis, with 20 million suffering severe consequences of the infection. Treatment consists of daily doses of an oral medication, either praziquantel or oxamniquine.
Tapeworms Several species of parasitic flatworms known as tapeworms can infect humans. The most common are the beef tapeworm, Taenia saginata; pork tapeworm, Taenia solium; and fish tapeworm, Diphyllobothrium latum. Infection—rare in North America but common in Asia, eastern Europe, and Latin America—can be prevented by prolonged freezing or thorough cooking of meat and fish. In the human body, the tapeworms attach themselves to the intestinal wall, where some species may attain lengths of 25 feet (7.6 meters) or more. Common symptoms include abdominal pain and diarrhea, but many infected people are symptomless. Treatment consists of praziquantel.
Trichinosis Larvae of the tiny roundworm Trichinella spirali live in the muscle tissue of many mammals. A person becomes infected by eating undercooked or poorly smoked meat, especially pork, from infected animals. The larvae mature into adult worms in the person’s intestines. When the adult worms reproduce, new larvae move into the blood and to the muscles, where they form cysts. Swollen upper eyelids, muscle pains, fever, fatigue, and weakness are common symptoms. Treatment consists of antiparasitic medicines. The disease is rare in the United States.
Whipworms Whipworm infection, also known as trichuriasis, is caused by the small roundworm Trichuris trichiura. It is most common in subtropical and tropical regions where sanitation is poor; an estimated 800 million people are infected worldwide. Whipworm eggs are ingested orally, via contaminated food or unclean hands. The eggs develop into worms in the intestines. Most people have no noticeable symptoms but if a large number of worms are present, abdominal pain and diarrhea may occur. Treatment consists of antiparasitic medicines.
Yellow fever A virus transmitted by mosquito bites causes this infectious disease. Initial symptoms are flulike and disappear after a few days. In some cases, the fever returns, accompanied by nausea, vomiting, bleeding, jaundice, and delirium. There is no cure; treatment is palliative. However, a highly effective vaccine is available; people visiting tropical areas of Africa and Latin America where the disease is a problem should be vaccinated prior to travel.
Health care professionals rely on a broad variety of diagnostic tests to look for the presence of disease or injury, to pinpoint its cause, and to monitor its course. Diagnostic tests also help determine the appropriate treatment and, subsequently, the effectiveness of therapy. Some tests are invasive, requiring at least minor surgery, while others are noninvasive. Common diagnostic tests include:
Amniocentesis This common prenatal test usually performed between 15 and 20 weeks of pregnancy, involves insertion of a needle through the mother’s abdomen and into the amniotic sac that surrounds the fetus. A sample of fluid, which contains fetal cells, is removed from the sac. The fetal cells are then tested for genetic defects such as Down syndrome. The procedure also can be used to identify the sex of the fetus. Chorionic villus sampling (CVS) provides similar information but can be performed earlier in the pregnancy.
Angiography In this procedure, a thin tube, or catheter, is passed through the skin into a blood vessel and a contrast dye is introduced into the bloodstream, allowing visualization of blood vessels. Angiography is commonly used to examine the coronary arteries of the heart and arteries that carry blood to the brain. It also is used to view blood vessels in the lungs, liver, kidney, spleen, and legs.
Biopsy In a biopsy, a tissue sample is extracted and examined microscopically. Depending on the site, the sample may be removed surgically or through a needle. Biopsies are performed to look for abnormal cells damaged by injury or disease. Biopsy is a standard procedure for confirming a diagnosis of cancer.
Blood tests Numerous laboratory tests can be performed on blood. Which tests are performed depends on what the physician wishes to check. For example, enzyme-linked immunosorbent assay (ELISA) looks for the presence of antibodies to HIV in the blood; positive results indicate that the person is infected with HIV, the virus that causes AIDS. For the most common blood tests, such as those for cholesterol levels and red blood cell count, laboratories establish a so-called normal result range. Typically, 95 percent of healthy patients fall within a laboratory’s normal range. This means that 5 percent of healthy patients fall outside the normal range. Results may also be outside the normal range for non-illness-related factors such as age, dietary habits, physical activity, pregnancy, use of prescription and nonprescription drugs, and alcohol intake. It is therefore critical that the physician carefully evaluate results.
Bone density tests These imaging techniques are used to measure bone density—an important aid in detecting osteoporosis, a disease characterized by brittle, easily fractured bones. The best-known test is dual-energy x-ray absorptiometry (DEXA), which uses photons given off by x-rays to measure photon absorption by the bone. The more radiation absorbed, the denser the bone.
Bone scan In this imaging technique, a radioisotope (radioactive material) that concentrates in bones is injected into the patient’s bloodstream. After an hour or more, during which the bones pick up the radioisotope, special equipment is used to detect radiation emissions and translate them into images. These bone scans can be used to detect abnormalities such as stress fractures, arthritis, tumors, and infection (osteomyelitis).
Colonoscopy This endoscopic procedure allows examination of the interior of the entire large intestine and sometimes the lower part of the small intestine. A thin, flexible tube is passed through the anus and into the large intestine. Colonoscopy is commonly used to screen for colon cancer and to detect polyps, infectious bowel disease, and other abnormalities. (Most polyps found during colonoscopy can be completely removed during the procedure.) Colonoscopy can also be done to obtain tissue samples for biopsies or stool samples for microscopic examination. A related endoscopic procedure is sigmoidoscopy, in which the lower 10 to 12 inches (25–30 centimeters) of the large intestine are inspected.
Common Blood Tests
| Substance | Test Description | Result Indications |
|---|---|---|
| Blood Urea Nitrogen (BUN) | Measures the concentration of nitrogen in the form of urea in the blood; used to evaluate the rate at which blood is filtered across blood vessels in the kidney. | Elevated levels may indicate kidney dysfunction. |
| Cholesterol: high density lipoprotein (HDL) | Measures “good” cholesterol: HDL helps prevent cholesterol buildup in arteries. | Elevated levels may counteract the negative effects of high LDL levels. |
| Cholesterol: low density lipoprotein (LDL) | Measures “bad” cholesterol: LDL is the primary source of cholesterol buildup and blockage in arteries. | Elevated levels are a major risk factor for cardiovascular disease. |
| Cholesterol, total | Measures blood levels of cholesterol, a fatlike substance found in all cells. Total blood cholesterol is the sum of HDL and LDL. | Elevated levels suggest an increased risk of cardiovascular disease. |
| C-reactive protein | Measures the amount of a protein linked to artery disease. | The lower the level the better; elevated levels are associated with increased risk of heart attack or stroke. |
| Creatinine | Measures the amount of creatinine, a waste product of muscle breakdown that is excreted by the kidneys. | Elevated levels, especially accompanied by high BUN levels, may indicate renal failure or other kidney problems, dehydration, or hyperthyroidism. |
| Glucose | Measures the level of sugar in the blood. | Elevated levels are associated with diabetes, medications such as steroids, and eating before the test. |
| Hemoglobin (Hgb) | Measures the amount of oxygen- carrying hemoglobin contained within the red blood cells (RBCs). | Low levels suggest anemia, which can be due to a variety of causes. High Hgb may indicate lung disease or excessive production of RBCs; living at high altitudes elevates Hgb. |
| Iron | Measure blood levels of iron. Iron is essential for the formation of red blood cells. | Abnormal results may indicate bleeding, anemia, malabsorption, malnutrition, liver disease, cancer, infection, or other problems. |
| Platelets (PLT) | Estimates the number of platelets (cell fragments critical in initiating blood clotting). | Elevated levels may indicate bleeding or excessive production by the bone marrow. Low levels may result from acute blood loss, infections, bone marrow failure, or usage of certain drugs. |
| Potassium | Measures blood levels of potassium. Potassium regulates muscle activity, including contraction of heart muscles. | Abnormal levels may indicate kidney disease. |
| Prothrombin time (PT), Activated partial thromboplastin time (APTT) | Measure the time needed for a clot to form after certain reagents are added to the blood sample. | Abnormalities may indicate problems with anticoagulant drug therapy. |
| Sodium | Measures the amount of sodium in the blood. | Elevated levels may result from dehydra tion, diabetes, or excessive salt intake. Low levels may result from heart or kid ney dysfunction, use of diuretic or dia betes drugs, vomiting, or diarrhea. |
| Thyroid hormones | Measure the blood levels of thyroxine (T4) and triiodothyronine (T3), hormones that regulate body metabolism. | Elevated levels suggest an underactive thyroid; low levels suggest an overactive thyroid. |
| Triglycerides | Measures trigylcerides, a form of fat carried in the blood on very-low density lipoprotein (VLDL). | Elevated triglycerides, usually accompanied by low HDL cholesterol levels, may be associated with heart disease and pancreatitis. |
| Uric acid | Measures the blood levels of uric acid, a breakdown product of building blocks of DNA and RNA. | Elevated levels are associated with gout, kidney problems, and the use of certain diuretics. |
| White blood cells (WBC) | Measures the number of white blood cells in a unit of blood. A WBC differential count measures the different types of white blood cells (lymphocytes, monocytes, and so on). | A high WBC may be a sign of infection. A low WBC may indicate bone marrow disease or an enlarged spleen. |
CT Computer tomography is an imaging technique that uses X rays to take pictures—tomograms or, more commonly, CAT scans—of the body. The pictures are reconfigured by a computer to produce 3-D images. CT is particularly helpful in locating tumors, organ injuries, abscesses, and fluid accumulation.
Culture To identify bacteria or other disease-causing agents, samples of blood or other fluids or tissues are placed in laboratory dishes containing special culture media that encourage the growth of microorganisms. For example, if cholera is suspected, a stool sample or a swab from the patient’s rectum is cultured. The diagnosis is confirmed by isolation of the organism Vibrio cholerae from the culture.
Electrocardiogram For an ECG, small metal sensors are placed on the skin to record the electrical activity of the heart. The information is transmitted to a machine that creates a graph of the data. ECGs are used to diagnose heart attacks and other heart problems, to detect noncardiac problems such as potassium deficit, to monitor patients recovering from heart problems, to determine the effectiveness of pacemakers and certain heart medications, and in exercise stress tests to determine a person’s fitness for strenuous exercise. An echocardiogram is another test used for many of the same purposes. In this test, sound waves emitted from a device placed on the chest bounce off the heart; the echoes are then converted into images.
Electromyogram In electromyography, small needle sensors, or electrodes, are inserted into a selected muscle; they record the electrical activity of the muscle at rest and when contracting. The data are displayed on a screen or printed as a graphic record (electromyogram, or EMG) for study. Test results aid in diagnosing muscular, nerve, and neuromuscular diseases, including muscular dystrophy, amyotrophic lateral sclerosis, and myasthenia gravis.
Endoscopy An endoscope consists of a miniaturized camera mounted on a thin tube; the tube is inserted into the body to inspect the interior surface of a joint or other body part. High-definition technology may be used to improve clarity and visibility. Instruments may be passed through the tube to obtain fluid or tissues samples for laboratory examination. In some tests, the tube is inserted through a natural opening in the body. For instance, in a cystoscopy an endoscope called a cystoscope is passed through the urethra and into the urinary bladder. In other cases, endoscopy requires minor surgery. In arthroscopy, for example, an arthroscope is inserted through a small incision into a knee or other joint. See also Colonoscopy.
Fecal occult blood test In this test, samples of a person’s stool (feces) are examined microscopically and chemically to detect occult blood (“hidden” blood not visible to the naked eye). The test detects bleeding in the digestive tract, which may be caused by a variety of disorders such as hemorrhoids, ulcerative colitis, inflammatory bowel disease, and cancer. It is recommended that all individuals age 50 or older have the test annually, to screen the colon and rectum for premalignant growths and cancer.
Imaging Production of an image using X rays, sound waves or other signals. These techniques enable physicians to obtain highly detailed views of internal organs without surgery. (See “Bone density tests,” “Bone scan,”
“CT,” “MRI,” “Ultrasound,” and “X rays.”)
Mammogram Images of the internal tissues of the breasts (mammary glands) are produced by passing low-dose X rays through the breasts. Abnormalities show up as masses, shadows, and other distortions. The test is used to detect benign and malignant tumors and to monitor breast cancer patients during and following treatment. Women age 50 and older are urged to have a mammogram every year. A newer test is digital mammography, which records the X rays on digital film that can then be manipulated for more precise study of the images.
MRI Magnetic resonance imaging uses a combination of a strong magnetic field and radio waves to measure the distribution and chemical bonds of the protons in the body’s hydrogen atoms. A computer translates measurements into 3-D images. MRI is frequently used to view the brain and other soft tissues.
Myelogram The spinal column can by studied by injecting a dye into the cerebrospinal fluid that surrounds the spinal cord. X rays are used to track the flow of the dye and to identify abnormalities, including tumors, arthritic bone spurs, and herniated disks.
Pap smear For a Papanicolaou (Pap) test, a small sample of cells is scraped from the female patient’s cervix. The cells are examined microscopically for signs of cancer or inflammation. Women age 21 and older are urged to have regular Pap smears.
PSA test The prostate-specific antigen (PSA) test is a screening test for prostate cancer. It measures the blood level of the protein PSA, which is made by the prostate. PSA level fluctuates naturally over time, and cancer is not the sole factor that can raise the level. It is recommended that males over age 50 have the PSA test annually.
Pulmonary function tests These measure the lungs’ capacity to hold air and to inhale and exhale air. The patient is asked to do certain breathing exercises while breathing through a mouthpiece. The tests help diagnose and assess the severity of breathing ailments. They also are used to determine whether a patient has restrictive lung disease, which primarily interferes with breathing in, or obstructive lung disease, which primarily inhibits breathing out.
Scratch tests These tests are used to identify allergies—sensitivities to substances in the environment, called allergens. Scratches are made on the surface of the person’s skin, and a small amount of a suspected allergen is applied. If the person is allergic to the substance, the skin usually reddens and swells within about 15 minutes. Alternate techniques include pricking the skin or injecting the allergen between layers of the skin.
Spinal tap Also called a lumbar puncture, this procedure involves inserting a thin needle into the spinal canal and removing a sample of cerebrospinal fluid for analysis. The test helps diagnose disorders of the brain and spinal cord, including infections, tumors, bleeding, and multiple sclerosis. Spinal taps are also used therapeutically, to introduce medication into the cerebrospinal fluid.
Ultrasound Ultrasound imaging, or sonography, beams high-frequency sound waves at the body’s organs. The echoes that bounce back are translated into computer images. Because it doesn’t use X rays, sonography is recommended for use on pregnant women. It is well suited for examining soft tissue, such as the gall bladder, liver, heart, and thyroid gland. Doppler ultrasound images
blood flow in blood vessels, enabling the detection of blockages and aneurysms.
Upper GI series Sometimes referred to as the barium swallow, the upper gastrointestinal series is used to examine the esophagus, stomach, and upper part of the small intestine. It detects structural abnormalities, inflammation, tumors, hiatal hernia, and other problems. The patient swallows a liquid containing barium sulfate, a dye that coats the interior of the gastrointestinal tract. X rays are used to view the flow of the barium sulfate.
Urinalysis The chemical, physical, and microscopic analysis of urine often is a first step in diagnosing kidney disorders, urinary bladder infections, and certain metabolic diseases. For example, the presence of bacteria such as Escherichia coli or Proteus vulgaris signals a bladder infection (cystitis). Excessive glucose is a symptom of diabetes mellitus. Bilirubin—an orange-yellow pigment formed when red blood cells are broken down, and normally excreted in bile—suggests possible liver disease.
X-rays X-ray pictures, or radiographs, are two-dimensional images commonly used to detect bone fractures and displacements, dental problems, and tumors in certain organs. They are the most widely used diagnostic imaging technique.
Prescription drugs ease pain, combat infections, control blood pressure, relieve allergy symptoms, and play numerous other important roles in health care. They make up the fastest-growing health-care expenditure in the United States. In 1980 the nation spent $12 billion on drugs. By 2006 the nation’s pharmaceutical tab had risen to $274.9 billion, as retail pharmacies filled more than 3.2 billion prescriptions. An aging population and the introduction of new therapies for chronic conditions helped fuel the increasing demand for drugs. Additionally, newer drugs tended to be much costlier than older medications.
Side effects
Every medication has possible side effects. These can range from slight nausea or temporary drowsiness to kidney failure and other deadly conditions. The side effects can vary depending on the size of the dose and on the patient’s genetic makeup, body size, age, and overall health. People with one medical problem may not be able to take medication designed to treat another medical problem. For example, the cholesterol reducer simvastatin (Zocor) can lead to kidney failure in people with severe infections.
Side effects are among the most common causes of hospitalization in the United States. To avoid or limit such problems, it is important that patients know the common side effects of any medication, including over-the-counter medications, that they are taking. Medications should be taken as directed, problems should be reported promptly to the physician, and expired drugs should be discarded.
Some drugs interact with foods, causing side effects or inhibiting the effectiveness of the drugs. For example, antidepressants known as MAO inhibitors can cause severe headaches and potentially fatal increases in blood pressure in people who consume foods high in tyramine (many cheeses, yogurt, cured meats, red wine, and so on).
Additionally, drugs taken during the same time period can interact with one another, sometimes in deadly fashion. For instance, certain blood pressure medications can dangerously increase levels of lithium in people taking lithium drugs to combat manic depression. Pain relievers such as ibuprofen can reduce the effectiveness of diuretics. Alcohol consumption increases the risk of seizures among people taking the antidepressant bupropion hyudrochloride (Wellbutrin). Thus it is also important that patients inform all their doctors about all prescription and over-the-counter medications they are taking, including herbal remedies and weight loss pills.
Commonly Prescribed Medications
A medication has a chemical name that describes its molecular structure, a generic (nonproprietary) name, and a brand (proprietary) name. In the following list, which is by no means inclusive, the generic name is followed by a brand name in parentheses.
Acne therapy Substances used to treat a common skin condition characterized by pimples and pus-filled pockets on the face and upper torso. Isotretinoin (Accutane), antibiotics such as tetracycline and doxycycline.
Analgesics Substances that relieve pain. Prescription analgesics include both narcotics, such as Oxycodone (OxyContin) and hydrocodone/APAP, and non-narcotics, such as Sumatriptan succinate (Imitrex Oral) and
Tramadol (Ultram). The most widely used over-the-counter analgesics are nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen.
Antianxiety medications Substances used to treat panic, phobias, and other anxiety disorders. Alprazolam (Xanax), clonazepam (Klonopin), diazepam (Valium).
Antiarthritics Substances used to reduce symptoms of osteoarthritis. Celecoxib (Celebrex), rofecoxib (Vioxx).
Antibiotics Substances that destroy or inhibit the growth of bacteria. Amoxicillin/clavulanae (Augmentin), Azithromycin (Zithromax), Ciprofloxacin (Cipro), Levofloxacin (Levaquin).
Antidepressants Substances used to treat depression. There are three types:
Selective serotonin reuptake inhibitors (SSRIs) Fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft), Citalopram (Celexa).
Tricyclic antidepressants Clomipramine (Norpramin, Pertofrane), imipramine (Tofranil).
Monoamine oxidase inhibitors (MAOIs) Bupropion HCL (Wellbutrin SR), Venlafaxine (Effexor XR), Isocarboxazid (Marplan), phenelzine sulfate (Nardil).
Antihistamines Substances that interfere with the action of histamines, which play a critical role in allergic reactions. Loratadine (Claritin), fexofenadine (Allegra), cetirizine (Zyrtec).
Antihypertensives Substances used to combat high blood pressure. There are four types:
Angiotensin-converting enzyme (ACE) inhibitors Benazepril (Lotensin), captopril (Capoten), enalapril maleate (Vasotec), lisinopril (Zestril).
Beta blockers Acebutolol (Sectral), metoprolol (Lopressor), penbutolol (Levatol).
Calcium channel blockers Amlodipine (Norvasc), diltiazem (Dilacor), verapamil (Verelan).
Diuretics Thiazides such as chlorothiazide (Diuril) and chlorthalidone (Thalitone), potassium-sparing diuretics such as amiloride (Midamor) and spironolactone (Aldactone).
Antimanic medications Substances that treat bipolar disorder. Gabapentin (Neurontin), divalproex sodium (Depakote), lithium citrate (Cibalith-S).
Antiplatelet medications Substances that destroy or interfere with blood platelets, to prevent excessive blood clotting and help prevent strokes caused by blood clots. Clopidogrel (Plavix), ticlopidine (Ticlid), aspirin.
Antipsychotic Substances that alleviate the symptoms of schizophrenia and other psychotic states. Olanzapine (Zyprexa), quetiapine (Seroquel), risperidone (Risperdal), chlorpromazine (Thorazine).
Antiulcerants Substances that prevent or treat ulcers. Omepravole (Prilosec), Lansoprazole (Prevacid), Rabeprazole (Aciphex), Ranitidine (Zantac).
Asthma therapy Substances that prevent or treat asthma. Leukotriene modifiers such as montelukast sodium (Singulair), inhaled corticosteroids such as beclomethasone (Beclovent), beta-adrenergic agonists such as albuterol (Proventil), mast cell stabilizers such as cromolyn (Gastrocrom).
Bone density therapy Substances used to treat osteoporosis. Bisphosphonates such as alendronate (Fosamax), calcium and vitamin D supplements.
Bronchodilator Substances that relax and widen respiratory passages leading to the lungs, relieving wheezing and bronchial spasms. Albuterol (Proventil), salmeterol xinafoate (Serevent).
Cholesterol reducers Substances that lower cholesterol and trigylceride levels. Statins, including lovastatin, simvastatin (Zocor), pravastatin (Pravachol), and atorvastatin (Lipitor); fibric acid derivatives such as fenofibrate (TriCor); bile acid binders such as cholestyramine (Prevalite).
Contraceptives Medications that prevent fertilization of an egg by a sperm. Ethinyl estradiol (Ortho Tri-Cyclen).
Diabetes therapy Substances that lower blood sugar levels in people with type II diabetes. Metformin (Glucophage), pioglitazone (Actos), rosiglitazone maleate (Avandia).
Erythropoietins Substances that combat anemia by stimulating the bone marrow to produce red blood cells. Epoetin alfa (Epogen, Procrit).
Hormone therapy Substances used to treat endocrine gland disorders. For example, levothyroxine (Synthroid) is used to replace thyroid hormones in people with an underactive thyroid gland.
Proton pump inhibitors Substances that reduce gastric acid production in the stomach. Omeprazole (Prilosec), lansoprazole (Prevacid, Zoton), esomeprazole (Nexium), pantoprazole (Protonix), rabeprazole (Aciphex).
Sedatives Substances that calm or tranquilize, reducing anxiety and inducing sleep. Zolpidem (Ambien), temazepam (Restoril).
Sexual function therapy Substances used to treat impotence in men. Sildenafil citrate (Viagra), vardenafil HCl (Levitra).
Steroids Substances that treat inflammation by suppressing the immune system. For example, respiratory steroids such as fluticasone propionate (Flovent, Flonase) provide relief from allergy symptoms.
Immunization
When bacteria or viruses invade the body, they trigger a counterattack, or immune response. This response includes synthesizing antibody proteins that combine with antigen molecules on the surface of the invader, destroying the invader. Secondarily, the body forms long-lived “memory cells.” If again exposed to the same antigen at a later time, the memory cells immediately go into action, releasing antibodies. This is the basis for immunity to certain infectious disease and the basis for immunization programs that vaccinate against diseases.
Vaccines consist of dead or weakened bacteria or viruses. When a person is inoculated with a vaccine for a specific disease, the vaccine stimulates the production of antibodies without producing the disease. Some vaccines provide lifelong immunity. In other cases, immunity can begin to fade over time, requiring booster shots. The three most widely recommended vaccines for adults are:
Tetanus, diphtheria (Td) vaccine To combat tetanus and diphtheria. One dose booster every 10 years.
Influenza vaccine To combat the flu. One dose annually for individuals age 50 and older. For younger adults, one dose annually for those with medical or exposure indications. Medical indicators include chronic cardiovascular and pulmonary conditions, certain chronic metabolic conditions, and women who will be in the second or third trimester of pregnancy during influenza season.
Pneumococcal vaccine To combat pneumonia and other pneumococcal bacteria. For people age 65 and older; people with chronic lung (excluding asthma), heart, liver, or kidney disorders; and people with illnesses such as diabetes, sickle cell disease, alcoholism, or HIV/AIDS. For most people, one dose provides lifetime protection. Some people may need a booster shot after 5 years.
In 1998 a British doctor and his associates published a paper asserting that their research demonstrated a strong connection between a common childhood vaccine for measles, mumps, and rubella and of autism. Parents around the world were understandably alarmed and many decided not to have their children vaccinated, leaving them vulnerable to harmful illnesses.
In 2010, the C.D.C. reported that 40 percent of American parents with young children delayed or refused one or more of the 10 required vaccines for their child. After 12 years of intense research the medical community determined not only was the research poorly done it was, in the end, fraudulent.
Childhood and Adolescent Vaccines: Recommended Immunization Schedule, 2010
| Age | Vaccines |
|---|---|
| Birth | Hepatitis B |
| 2 months | Hepatitis B, polio, rotavirus, diph theria, tetanus, pertussis (DTaP), haemophilus B (Hib), pneumonia and other pneumococcal bacteria (PCV) |
| 4 months | Rotavirus, Polio, DTaP, Hib, PCV |
| 6 months | Rotavirus, DTaP, Hib, PCV |
| 6–18 months | Hepatitis B, polio |
| 6 months–18 years | Influenza (yearly) |
| 12–15 months | Hib; measles, mumps, rubella (MMR#1); chicken pox, PCV |
| 12–23 months | Hepatitis A series |
| 15–18 months | DTaP |
| 4–6 years | Polio, DtaP, MMR#2, chicken pox |
| 11–12 years | DTaP, human papillomavirus (HPV, 3 doses, females only), meningococcal (MCV4) |
| Note: It generally takes several doses of each vaccine for full protection. In some cases, there is a range of acceptable ages for vaccination. For example, the third dose of hepatitis B vaccine may be given between 6 and 18 months of age. Children who have not been vaccinated against Hepatitis B in infancy may begin the series during any childhood visit. For additional information, contact your physician. Sources: American Academy of Pediatrics; American Academy of Family Physicians; and U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention. | |
Times focus
Really?
Despite or perhaps because of the enormous amount of medical information now available on the Internet, everyone knows that medical myths and old wives’ tales about symptoms, treatments, etc. still hold a prominent place in everyday conversation. So every week The New York Times runs a small column devoted to affirming the validity of these “theories” or, more frequently, debunking them. Below are a few examples:
THE CLAIM: Lying on your left side eases heartburn.
THE FACTS For people with chronic heartburn, restful sleep is no easy feat. Fall asleep in the wrong position, and acid slips into the esophagus, a recipe for agita and insomnia.
Doctors recommend sleeping on an incline, which allows gravity to keep the stomach’s contents where they belong. But sleeping on your side can also make a difference—so long as you choose the correct side. Several studies have found that sleeping on the right side aggravates heartburn; sleeping on the left tends to calm it.
The reason is not entirely clear. One hypothesis holds that right-side sleeping relaxes the lower esophageal sphincter, between the stomach and the esophagus. Another holds that left-side sleeping keeps the junction between stomach and esophagus above the level of gastric acid.
In a study in The Journal of Clinical Gastroenterology, scientists recruited a group of healthy subjects and fed them high-fat meals on different days to induce heart-burn. Immediately after the meals, the subjects spent four hours lying on one side or the other as devices measured their esophageal acidity. Ultimately, the researchers found that “the total amount of reflux time was significantly greater” when the subjects lay on their right side.
“In addition,” they wrote, “average overall acid clearance was significantly prolonged with right side down.”
In another study, this one in The American Journal of Gastroenterology, scientists fed a group of chronic heartburn patients a high-fat dinner and a bedtime snack, then measured reflux as they slept. The right-side sleepers had greater acid levels and longer “esophageal acid clearance.” Other studies have had similar results.
THE BOTTOM LINE Lying on your right side seems to aggravate heartburn.
THE CLAIM: Humming can ease sinus problems.
THE FACTS Dealing with a cold is bad enough, but when it leads to a sinus infection, the misery can double. Some researchers have proposed a surprising remedy: channeling your inner Sinatra.
Sinus infections—which afflict more than 37 million Americans every year—generally occur when the lining of the sinuses becomes inflamed, trapping air and pus and other secretions, and leading to pain, headaches and congestion. Because the inflammation is often caused by upper-respiratory infections, people with asthma and allergies are more vulnerable than others to chronic sinusitis.
Keeping the sinuses healthy and infection-free requires ventilation—keeping air flowing smoothly between the sinus and nasal cavities. And what better way to keep air moving through the sinuses and nasal cavity than by humming a tune?
In a study in The American Journal of Respiratory and Critical Care Medicine, researchers examined this by comparing airflow in people when they hummed and when they quietly exhaled. Specifically, they looked to see if humming led to greater levels of exhaled nitric oxide, a gas produced in the sinuses. Ultimately, nitric oxides during humming rose 15-fold.
Another study a year later in The European Respiratory Journal found a similar effect: humming resulted in a large increase in nasal nitric oxide, “caused by a rapid gas exchange in the paranasal sinuses.” Since reduced airflow plays a major role in
sinus infections, the researchers suggested that daily periods of humming might help people lower their risk of chronic problems. But further study is needed, they said.
THE BOTTOM LINE Studies show that humming helps increase airflow between the sinus and nasal cavities, which could potentially help protect against sinus infections.
THE CLAIM: To reduce snoring, try sleeping on your side.
THE FACTS Chronic snoring can be more than a noisy nuisance. Up to three-quarters of nightly snorers also have sleep apnea, which causes breathing interruptions throughout the night. Sleep apnea raises the risk of heart disease, stroke and high blood pressure.
Snorers looking for a cure are often told to sleep on their sides, not on their backs, so that the base of the tongue will not collapse into the back of the throat, narrowing the airway and obstructing breathing. But for some snorers, changing sleep position may not make much of a difference.
Scientists say there are two types of snorers: those who snore only when they sleep on their backs, and those who do it regardless of their position. After sleep researchers in Israel examined more than 2,000 sleep apnea patients, for example, they found that 54 percent were “positional,” meaning they snored only when asleep on their backs. The rest were “nonpositional.”
Other studies have shown that weight plays a major role. In one large study, published in 1997, patients who snored or had breathing abnormalities only while sleeping on their backs were typically thinner, while their nonpositional counterparts usually were heavier. The latter group, wrote the authors, consequently suffered worse sleep and more daytime fatigue.
But that study also found that patients who were overweight saw reductions in the severity of their apnea when they lost weight. According to the National Sleep Foundation, in people who are overweight, slimming down is generally the best way to cure sleep apnea and end snoring for good.
THE BOTTOM LINE Sleeping on your side can help reduce snoring, though in people who are overweight, it may not make much difference without weight loss.
THE CLAIM: Eating local honey cures allergies.
THE FACTS Among allergy sufferers, there is a widespread belief that locally produced honey can alleviate symptoms—the idea being that the honey acts like a vaccine. Bees that jump from one flower to the next end up covered in pollen spores, which are then transferred to their honey. Eating that honey—just a spoonful a day—can build up immunity through gradual exposure to the local allergens that can make life so miserable for allergy sufferers.
Or at least that’s the thinking behind it. But when University of Connecticut Health Center researchers did a test, they found that the honey had no such effect.
In the study, published in the Annals of Allergy, Asthma and Immunology in 2002, the scientists followed dozens of allergy sufferers through the springtime allergy season. The subjects were randomly split into three groups. One consumed a tablespoonful daily of locally collected, unpasteurized and unfiltered honey; another ate commercial honey; and a third was given a corn syrup placebo with synthetic honey flavoring.
After tracking the subjects’ symptoms for months, the scientists found that neither of the honey groups saw improvements over the placebo group.
Dr. Stanley Fineman, president-elect of the American College of Allergy, Asthma and Immunology, said he has seen a growing number of patients ask about local honey. “Seasonal allergies are usually triggered by windborne pollens, not by pollens spread by insects,” he said. So it’s unlikely that honey “collected from plants that do not cause allergy symptoms would provide any therapeutic benefit.”
THE BOTTOM LINE There’s no evidence that local honey relieves allergy symptoms.