HEALTHCARE FOR A LIFETIME
When you own a dog, you become his healthcare advocate over his entire lifespan, as well as being the one to shoulder the financial burden of such care. Accordingly, it is worthwhile to focus on prevention rather than treatment, as you and your pet will both be happier.
Of course, the best place to have begun your program of preventive healthcare is with the initial purchase or adoption of your dog. There is no way of guaranteeing that your new furry friend is free of medical problems, but there are some things you can do to improve your odds. You certainly should have done adequate research into the Clumber Spaniel and have selected your puppy carefully rather than buying on impulse. Health issues aside, a large number of pet abandonment and relinquishment cases arise from a mismatch between pet needs and owner expectations. This is entirely preventable with appropriate planning and finding a good breeder.
Regarding healthcare issues specifically, it is very difficult to make blanket statements about where to acquire a problem-free pet, but, again, a reputable breeder is your best bet. In an ideal situation you have the opportunity to see both parents, get references from other owners of the breeder’s pups and see genetic-testing documentation for several generations of the litter’s ancestors. At the very least, you must thoroughly investigate the Clumber Spaniel and the problems inherent in the breed, as well as the genetic testing available to screen for those problems. Genetic testing offers some important benefits but is available for only a few disorders in a relatively small number of breeds and is not available for some of the most common genetic diseases, such as hip dysplasia, cataracts, epilepsy, cardiomyopathy, etc. This area of research is exciting and increasingly important, and advances will be made each year. In fact, recent research has shown that there is an equivalent dog gene for 75% of known human genes, so research done in either species is likely to benefit the other.

Dr. Roe Froman is a veterinarian who specializes in Clumber Spaniels. Here she is shown examining a four-week-old Clumber puppy to evaluate its general health.
We’ve also discussed that evaluating the behavioral nature of your Clumber Spaniel and that of his immediate family members is an important part of the selection process that cannot be underestimated or overemphasized. It is sometimes difficult to evaluate temperament in puppies because certain behavioral tendencies, such as some forms of aggression, may not be immediately evident. More dogs are euthanized each year for behavioral reasons than for all medical conditions combined, so it is critical to take temperament issues seriously. Start with a well-balanced, friendly companion and put the time and effort into proper socialization, and you will both be rewarded with a valued relationship for the life of the dog.
Assuming that you have started off with a pup from healthy, sound stock, you then become responsible for helping your veterinarian keep your pet healthy. Some crucial things happen before you even bring your puppy home. Parasite control typically begins at two weeks of age, and vaccinations typically begin at six to eight weeks of age. A pre-pubertal evaluation is typically scheduled for about six months of age. At this time, a dental evaluation is done (since the adult teeth are now in), heartworm prevention is started and neutering or spaying is most commonly done.
It is critical to commence regular dental care at home if you have not already done so. It may not sound very important, but most dogs have active periodontal disease by four years of age if they don’t have their teeth cleaned regularly at home, not just at their veterinary exams. Dental exams should be part of every annual physical examination.
DENTAL WARNING SIGNS
A veterinary dental exam is necessary if you notice one or any combination of the following in your dog:
• Broken, loose or missing teeth
• Loss of appetite (which could be due to mouth pain or illness caused by infection)
• Gum abnormalities, including redness, swelling and bleeding
• Drooling, with or without blood
• Yellowing of the teeth or gumline, indicating tartar
• Bad breath

Dental problems lead to more than just bad “doggy breath.” Gum disease can have very serious medical consequences. If you start brushing your dog’s teeth and using antiseptic rinses from a young age, your dog will be accustomed to it and will not resist. The results will be healthy dentition, which your pet will need to enjoy a long, healthy life.
Clumber Spaniels reach adulthood at about two or so years old and true maturity at around age five. Even individual dogs within each breed have different healthcare requirements, so work with your veterinarian to determine what will be needed and what your role should be. This doctor-client relationship is important, because as vaccination guidelines change, there may not be an annual “vaccine visit” scheduled. You must make sure that you see your veterinarian at least annually, even if no vaccines are due, because this is the best opportunity to coordinate healthcare activities and to make sure that no medical issues creep by unaddressed.
When your Clumber Spaniel reaches about three-quarters of his anticipated lifespan, or as deterimined by the vet, he is considered a “senior” and will require some changes to his healthcare routine. In general, if you’ve been taking great care of your canine companion throughout his formative and adult years, the transition to senior status should be a smooth one. Age is not a disease, and as long as everything is functioning as it should, there is no reason why most of late adulthood should not be rewarding for both you and your pet. This is especially true if you have tended to the details, such as regular veterinary visits, proper dental care, excellent nutrition and management of bone and joint issues.
At this stage in your Clumber Spaniel’s life, your veterinarian may want to schedule visits twice yearly, instead of once, to run some laboratory screenings, electrocardiograms and the like, and to change the diet to something more digestible. Catching problems early is the best way to manage them effectively. Treating the early stages of heart disease is so much easier than trying to intervene when there is more significant damage to the heart muscle. Similarly, managing the beginning of kidney problems is fairly routine if there is no significant kidney damage. Other problems, like cognitive dysfunction (similar to senility and Alzheimer’s disease), cancer, diabetes and arthritis, are more common in older dogs, but all can be treated to help the dog live as many happy, comfortable years as possible. Just as in people, medical management is more effective (and less expensive) when you catch things early.
SELECTING A VETERINARIAN
There is probably no more important decision that you will make regarding your pet’s healthcare than the selection of his doctor. Your pet’s veterinarian will be a pediatrician, family-practice physician and gerontologist, depending on the dog’s life stage, and will be the individual who makes recommendations regarding issues such as when specialists need to be consulted, when diagnostic testing and/or therapeutic intervention is needed and when you will need to seek outside emergency and critical-care services. Your vet will act as your advocate and liaison throughout these processes.
Everyone has his own idea about what to look for in a vet, an individual who will play a big role in his dog’s (and, of course, his own) life for many years to come. For some, it is the compassionate caregiver with whom they hope to develop a professional relationship to span the lives of their dogs and even their future pets. For others, they are seeking a clinician with keen diagnostic and therapeutic insight who can deliver state-of-the-art healthcare. Still others need a veterinary facility that is open evenings and weekends, is in close proximity or provides mobile veterinary services to accommodate their schedules. Your selection of a vet should be based on a combination of things: your trust and confidence in the vet’s expertise, knowledge and abilities, as well as his proximity to you. You should be comfortable with the entire staff and with the practice as a whole.
If possible, try to find a vet with Clumber experience. The shape of the Clumber’s eyelids is different, with a diamond-shaped lower lid. This sometimes leads to mistaken recommendations for surgical corrections, which may not be needed. Since the Clumber Spaniel is a relatively uncommon breed, vets who are familiar with them are often happy to consult with an owner’s vet if the latter is not experienced in the breed.
Just as we have different reasons for selecting our own healthcare professionals (e.g., covered by insurance plan, expert in field, convenient location, etc.), we should not expect that there is a one-size-fits-all recommendation for selecting a veterinarian and veterinary practice. The best advice is to be honest in your assessment of what you expect from a veterinary practice and to conscientiously research the options in your area. You will quickly appreciate that not all veterinary practices are the same, and you will be happiest with one that truly meets your and your Clumber’s needs.
There is another point to be considered in the selection of veterinary services. Not that long ago, a single veterinarian would attempt to manage all medical and surgical issues as they arose. That was often problematic, because veterinarians are trained in many species and many diseases, and it was just impossible for general veterinary practitioners to be experts in every species, every breed, every field and every ailment. However, just as in the human healthcare fields, specialization has allowed general practitioners to concentrate on primary healthcare delivery, especially wellness and the prevention of infectious diseases, and to utilize a network of specialists to assist in the management of conditions that require specific expertise and experience. Thus there are now many types of veterinary specialists, including dermatologists, cardiologists, ophthalmologists, surgeons, internists, oncologists, neurologists, behaviorists, criticalists and others to help primary-care veterinarians deal with complicated medical challenges. In most cases, specialists see cases referred by primary-care veterinarians, make diagnoses and set up management plans. From there, the animals’ ongoing care is returned to their primary-care veterinarians. This important team approach to your pet’s medical-care needs has provided opportunities for advanced care and an unparalleled level of quality to be delivered.
With all of the opportunities for your Clumber Spaniel to receive high-quality veterinary medical care, there is another topic that needs to be addressed at the same time—cost. It’s been said that you can have excellent healthcare or inexpensive healthcare, but never both; this is as true in veterinary medicine as it is in human medicine. While veterinary costs are a fraction of what the same services cost in the human healthcare arena, it is still difficult to deal with unanticipated medical costs, especially since they can easily creep into hundreds or even thousands of dollars if specialists or emergency services become involved. However, there are ways of managing these risks. The easiest is to buy pet health insurance and realize that its foremost purpose is not to cover routine healthcare visits but rather to serve as an umbrella for those rainy days when your pet needs medical care and you don’t want to worry about whether or not you can afford that care. There are also third-party medical financial lenders that can be very helpful.
Let’s discuss some of the diseases that create the need for vaccination in the first place. Following are the major canine infectious diseases and a simple explanation of each.
Rabies: A devastating viral disease that can be fatal in dogs and people. In fact, vaccination of dogs and cats is an important public-health measure to create a resistant animal buffer population to protect people from contracting the disease. Vaccination schedules are determined on a government level and are not optional for pet owners; rabies vaccination is required by law in all 50 states.
Parvovirus: A severe, potentially life-threatening disease that is easily transmitted between dogs. There are four strains of the virus, but it is believed that there is significant “cross-protection” between strains that may be included in individual vaccines.
Distemper: A potentially severe and life-threatening disease with a relatively high risk of exposure, especially in certain regions. In very high-risk distemper environments, young pups may be vaccinated with human measles vaccine, a related virus that offers cross-protection when administered at four to ten weeks of age.
Hepatitis: Caused by canine adenovirus type 1 (CAV-1), but since vaccination with the causative virus has a higher rate of adverse effects, cross-protection is derived from the use of adenovirus type 2 (CAV-2), a cause of respiratory disease and one of the potential causes of canine cough. Vaccination with CAV-2 provides long-term immunity against hepatitis, but relatively less protection against respiratory infection.
Canine cough: Also called tracheobronchitis, actually a fairly complicated result of viral and bacterial offenders; therefore, even with vaccination, protection is incomplete. Wherever dogs congregate, canine cough will likely be spread among them. Intranasal vaccination with Bordetella and parainfluenza is the best safeguard, but the duration of immunity does not appear to be very long, typically a year at most. These are non-core vaccines, but vaccination is sometimes mandated by boarding kennels, obedience classes, dog shows and other places where dogs congregate to try to minimize spread of infection.
Leptospirosis: A potentially fatal disease that is more common in some geographic regions. It is capable of being spread to humans. The disease varies with the individual “serovar,” or strain, of Leptospira involved. Since there does not appear to be much cross-protection between serovars, protection is only as good as the likelihood that the serovar in the vaccine is the same as the one in the pet’s local environment. Problems with Leptospira vaccines are that protection does not last very long, side effects are not uncommon and a large percentage of dogs (perhaps 30%) may not respond to vaccination.
Borrelia burgdorferi: The cause of Lyme disease, the risk of which varies with the geographic area in which the pet lives and travels. Lyme disease is spread by deer ticks in the eastern US and western black-legged ticks in the western part of the country, and the risk of exposure is high in some regions. Lameness, fever and inappetence are most commonly seen in affected dogs. The extent of protection from the vaccine has not been conclusively demonstrated.
Coronavirus: This disease has a high risk of exposure, especially in areas where dogs congregate, but it typically causes only mild to moderate digestive upset (diarrhea, vomiting, etc.). Vaccines are available, but the duration of protection is believed to be relatively short and the effectiveness of the vaccine in preventing infection is considered low.
There are many other vaccinations available, including those for Giardia and canine adenovirus-1. While there may be some specific indications for their use, and local risk factors to be considered, they are not widely recommended for most dogs.
VACCINATIONS AND INFECTIOUS DISEASES
There has never been an easier time to prevent a variety of infectious diseases in your dog, but the advances we’ve made in veterinary medicine come with a price—choice. Now while it may seem that this choice is a good thing (and it is), it also has never been more difficult for the pet owner (or the vet) to make an informed decision about the best way to protect pets through vaccination.
Years ago, it was just accepted that puppies got a starter series of vaccinations and then annual “boosters” throughout their lives to keep them protected. As more and more vaccines became available, consumers wanted the convenience of having all of that protection in a single injection. The result was “multivalent” vaccines that crammed a lot of protection into a single syringe. The manufacturers’ recommendations were to give the vaccines annually, and this was a simple enough protocol to follow. However, as veterinary medicine has become more sophisticated and we have started looking more at healthcare quandaries rather than convenience, it became necessary to reevaluate the situation and deal with some tough questions. It is important to realize that whether or not to use a particular vaccine depends on the risk of contracting the disease against which it protects, the severity of the disease if it is contracted, the duration of immunity provided by the vaccine, the safety of the product and the needs of the individual animal. In a very general sense, rabies, distemper, hepatitis and parvovirus are considered core vaccine needs, while parainfluenza, Bordetella bronchiseptica, leptospirosis, coronavirus and borreliosis (Lyme disease) are considered non-core needs and best reserved for animals that demonstrate reasonable risk of contracting the diseases.
NEUTERING/SPAYING
Sterilization procedures (neutering for males/spaying for females) are meant to accomplish several purposes. While the underlying premise is to address the risk of pet overpopulation, there are some medical and behavioral benefits to the surgeries as well. For females, spaying prior to the first estrus (heat cycle) leads to a marked reduction in the risk of mammary cancer and other serious female health problems. There also will be no manifestations of “heat” to attract male dogs and no bleeding in the house. For males, there is prevention of testicular cancer and a reduction in the risk of prostate problems. In both sexes there may be some limited reduction in aggressive behaviors toward other dogs, and some diminishing of urine marking, roaming and mounting.
GROWING PAINS
Eosinophilic panosteitis, often known as pano or eopan, is a condition similar to “growing pains.” It is frequently seen in adolescent pups between seven and fifteen months of age. It manifests as an intermittent, shifting leg lameness. That is, the dog will be lame on different legs at different times. Diagnosis of this condition by your vet is relatively straightforward, based on physical examination, clinical signs and sometimes x-rays (although typical lesions consistent with this diagnosis often are most noticeable in unaffected legs, making x-ray interpretation a bit more difficult). Although panosteitis can cause puppies to be quite lame, they typically feel fine otherwise, and eating and drinking habits remain normal. Mild pain-killing or anti-inflammatory medicines may bring some comfort, but the true cure for this condition is tincture of time (time itself).

While neutering and spaying do indeed prevent animals from contributing to pet overpopulation, even no-cost and low-cost neutering options have not eliminated the problem. Perhaps one of the main reasons for this is that individuals that intentionally breed their dogs and those that allow their animals to run at large are the main causes of unwanted offspring. Also, animals in shelters are often there because they were abandoned or relinquished, not because they came from unplanned matings. Neutering/spaying is important, but it should be considered in the context of the real causes of animals’ ending up in shelters and eventually being euthanized.
One of the important considerations regarding neutering is that it is a surgical procedure. This sometimes gets lost in discussions of low-cost procedures and commoditization of the process. In females, spaying is specifically referred to as an ovariohysterectomy. In this procedure, a midline incision is made in the abdomen and the entire uterus and both ovaries are surgically removed. While this is a major invasive surgical procedure, it usually has few complications because it is typically performed on healthy young animals. However, it is major surgery, as any woman who has had a hysterectomy will attest.
In males, neutering has traditionally referred to castration, which involves the surgical removal of both testicles. While still a significant piece of surgery, there is not the abdominal exposure that is required in the female surgery. In addition, there is now a chemical sterilization option, in which a solution is injected into each testicle, leading to atrophy of the sperm-producing cells. This can typically be done under sedation rather than full anesthesia. This is a relatively new approach, and there are no long-term clinical studies yet available.
Neutering/spaying is typically done around six months of age at most veterinary hospitals, although techniques have been pioneered to perform the procedures in animals as young as eight weeks of age. In general, the surgeries on the very young animals are done for the specific reason of sterilizing them before they go to their new homes. This is done in some shelter hospitals for assurance that the animals will definitely not produce any pups. Otherwise, these organizations need to rely on owners to comply with their wishes to have the animals “altered” at a later date, something that does not always happen.
There are some exciting immunocontraceptive “vaccines” currently under development, and there may be a time when contraception in pets will not require surgical procedures. We anxiously await these developments.
HEALTH ISSUES IN THE BREED
by Roe Froman, DVM
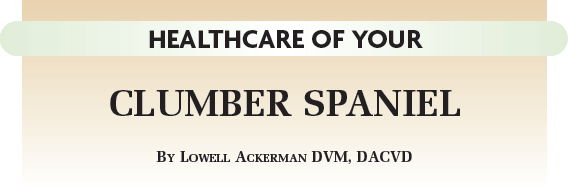
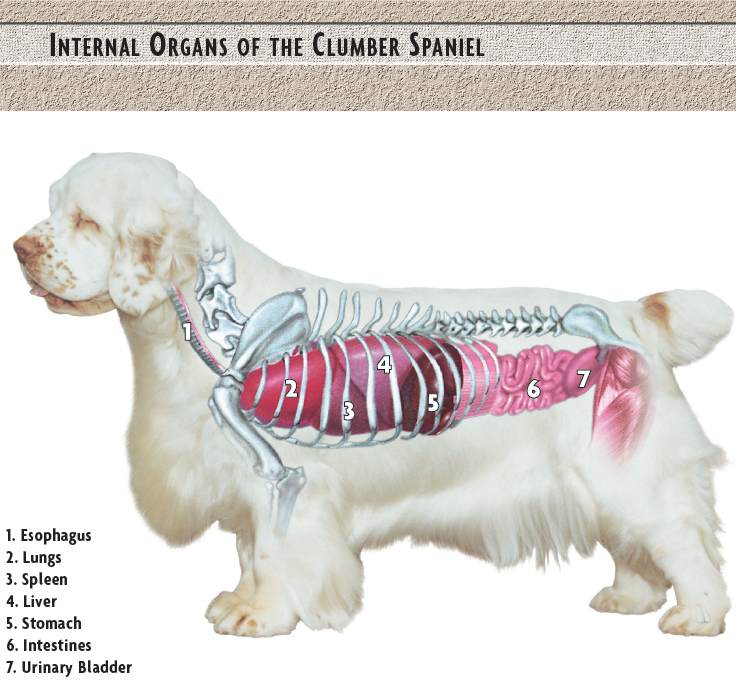
INTERVERTEBRAL DISC DISEASE
Long, low and heavy-set, Clumbers are anatomically, if not genetically as well, predisposed to disc disease. In this condition, the cushioning disc between adjacent vertebrae in the spine ruptures or herniates. This puts pressure on the spinal cord, leading to back pain, lameness, reluctance to turn or move the neck and, sometimes, paralysis. Two areas may be affected on Clumbers: the cervical region (neck) or the thoracolumbar area (back). Episodes often manifest as acute onset of pain (reluctance to move, inability to get up, reluctance to turn head or neck, lameness) with periods of remission between flare-ups.
Diagnosis is based upon clinical signs, physical examination, x-rays or myelography (the injection of dye into the spinal canal to identify the exact location of the problem). Treatment is either medical or surgical, depending on location. Cervical discs can respond very well to surgery performed by a practitioner qualified in the procedure. Thoracolumbar disc surgery is most often performed by neurosurgeons. Medical therapy consisting of corticosteroids and strict crate rest for three weeks during recovery is often very helpful.

Frolicking about is a most natural behavior for dogs. Sound vertebral health is essential to dogs’ being able to act like dogs.
IMMUNE-MEDIATED HEMOLYTIC ANEMIA (IMHA)
IMHA is a very serious, potentially fatal disorder in which the dog’s immune system begins attacking its own red blood cells. This can lead to a very sudden anemia. The dog may appear extremely fatigued, unable to rise and not interested in food. The mucous membranes (gums and tissues of the mouth, tissues around the eyes) will be extremely pale and sometimes jaundiced. This is an emergency situation that requires immediate veterinary attention. Aggressive treatment (sometimes necessitating blood transfusions and powerful immunosuppressive drugs) is needed.
THYROID DISEASE
Hypothyroidism is not uncommon in Clumber Spaniels. Hypothyroidism is best diagnosed with a complete thyroid panel (not just a T4 analysis), including thyroglobulin autoantibody levels. Michigan State University as well as some other veterinary labs can run these complete profiles. Some dogs with elevated autoantibody levels can be treated with low doses of thyroid supplementation, which can help stabilize their bodies’ thyroid levels. Clinically hypothyroid dogs are typically overweight, lethargic and heat-seeking, and often have non-itchy hair loss. These signs can be easily corrected with proper supplementation.
PYRUVATE DEHYDROGENASE DEFICIENCY
After an isolated letter to the editor describing four littermates with severe exercise intolerance in a British veterinary journal in the 1970s, this problem has been encountered a few times in various countries in Clumbers. Affected dogs suffer from a genetic deficiency that causes a lack of an enzyme that breaks down waste products produced during muscle activity. This causes a dog to become exhausted very easily, to the point that an affected dog can barely walk around the block. Research is being conducted to completely characterize this problem, to determine the inheritance pattern and to investigate possible therapies. A DNA test is under development for commercial usage at the time of this writing.
FOOD ALLERGIES
Dogs are allergic to many foods that are best-sellers and highly recommended by breeders and veterinarians. Changing the brand of food that you buy may not eliminate the problem if the element to which the dog is allergic is contained in the new brand.
Recognizing a food allergy is difficult. Humans vomit or have rashes when they eat a food to which they are allergic. Dogs neither vomit nor (usually) develop rashes. They react in the same manner as they do to an airborne or flea allergy: they itch, scratch and bite, thus making the diagnosis extremely difficult. While pollen allergies and parasite bites are usually seasonal, food allergies are year-round problems.
It is possible to handle food allergies and food intolerance yourself. This is often accomplished via hypoallergenic diets. It is important for these diets to be nutritionally balanced. They are based on novel carbohydrates and protein sources (ingredients the dog has never eaten before). These may include fish, venison, rabbit, duck and potato. Consult your veterinarian for advice before starting your dog on a new diet. Your vet may also be able to provide you with a completely balanced hypoallergenic diet, whether commercially manufactured or one that requires you to prepare food for the dog. It is also important to avoid incidental protein sources, such as treats or rawhides. Your vet also can advise you about healthy treats that should not cause an allergic reaction.
YOUR DOG NEEDS TO VISIT THE VET IF:
• He has ingested a toxin such as antifreeze or a toxic plant; in these cases, administer first aid and call the vet right away
• His teeth are discolored, loose or missing or he has sores or other signs of infection or abnormality in the mouth
• He has been vomiting, has had diarrhea or has been constipated for over 24 hours; call immediately if you notice blood
• He has refused food for over 24 hours
• His eating habits, water intake or toilet habits have noticeably changed; if you have noticed weight gain or weight loss
• He shows symptoms of bloat, which requires immediate attention
• He is salivating excessively
• He has a lump in his throat
• He has a lump or bumps anywhere on the body
• He is very lethargic
• He appears to be in pain or otherwise has trouble chewing or swallowing
• His skin loses elasticity.
Of course, there will be other instances in which a visit to the vet is necessary; these are just some of the signs that could be indicative of serious problems that need to be caught as early as possible
EXTERNAL PARASITES
FLEAS
Fleas have been around for millions of years and, while we have better tools now for controlling them than at any time in the past, there still is little chance that they will end up on an endangered species list. Actually, they are very well adapted to living on our pets, and they continue to adapt as we make advances.
The female flea can consume 15 times her weight in blood during active reproduction and can lay as many as 40 eggs a day. These eggs are very resistant to the effects of insecticides. They hatch into larvae, which then mature and spin cocoons. The immature fleas reside in this pupal stage until the time is right for feeding. This pupal stage is also very resistant to the effects of insecticides, and pupae can last in the environment without feeding for many months. Newly emergent fleas are attracted to animals by the warmth of the animals’ bodies, movement and exhaled carbon dioxide. However, when they first emerge from their cocoons, they orient towards light; thus when an animal passes between a flea and the light source, casting a shadow, the flea pounces and starts to feed. If the animal turns out to be a dog or cat, the reproductive cycle continues. If the flea lands on another type of animal, including a person, the flea will bite but will then look for a more appropriate host. An emerging adult flea can survive without feeding for up to 12 months but, once it tastes blood, it can survive off its host for only 3 to 4 days.
FLEA PREVENTION FOR YOUR DOG
• Discuss with your veterinarian the safest product to protect your dog, likely in the form of a monthly tablet or a liquid preparation placed on the back of the dog’s neck.
• For dogs suffering from flea-bite dermatitis, a shampoo or topical insecticide treatment is required.
• Your lawn and property should be sprayed with an insecticide designed to kill fleas and ticks that lurk outdoors.
• Using a flea comb, check the dog’s coat regularly for any signs of parasites.
• Practice good housekeeping. Vacuum floors, carpets and furniture regularly, especially in the areas that the dog frequents, and wash the dog’s bedding weekly.
• Follow up house-cleaning with carpet shampoos and sprays to rid the house of fleas at all stages of development. Insect growth regulators are the safest option.
It was once thought that fleas spend most of their lives in the environment, but we now know that fleas won’t willingly jump off a dog unless leaping to another dog or when physically removed by brushing, bathing or other manipulation. Flea eggs, on the other hand, are shiny and smooth, and they roll off the animal and into the environment. The eggs, larvae and pupae then exist in the environment, but once the adult finds a susceptible animal, it’s home sweet home until the flea is forced to seek refuge elsewhere.
KILL FLEAS THE NATURAL WAY
If you choose not to go the route of conventional medication, there are some natural ways to ward off fleas:
• Dust your dog with a natural flea powder, composed of such herbal goodies as rosemary, wormwood, pennyroyal, citronella, rue, tobacco powder and eucalyptus.
• Apply diatomaceous earth, the fossilized remains of single-cell algae, to your carpets, furniture and pet’s bedding. Even though it’s not good for dogs, it’s even worse for fleas, which will dry up swiftly and die.
• Brush your dog frequently, give him adequate exercise and let him fast occasionally. All of these activities strengthen the dog’s immune system and make him more resistant to disease and parasites.
• Bathe your dog with a capful of pennyroyal or eucalyptus oil.
• Feed a natural diet, free of additives and preservatives. Add a little fresh garlic and brewer’s yeast to the dog’s morning portion, as these items have flea-repelling properties.
Since adult fleas live on the animal and immature forms survive in the environment, a treatment plan must address all stages of the flea life cycle. There are now several safe and effective veterinary spot-on treatments that can be applied on a monthly basis. These include fipronil, imidacloprid, selamectin and permethrin (found in several formulations). Most of these products have significant flea-killing rates within 24 hours. However, none of them will control the immature forms in the environment. To accomplish this, there are a variety of insect growth regulators that can be sprayed into the environment (e.g., pyriproxyfen, methoprene, fenoxycarb) as well as insect development inhibitors such as lufenuron that can be administered. These compounds have no effect on adult fleas, but they stop immature forms from developing into adults. In years gone by, we relied heavily on toxic insecticides (such as organophosphates, organochlorines and carbamates) to manage the flea problem, but today’s options are not only much safer to use on our furry friends but also better for the environment.
TICKS
Ticks are members of the spider class (arachnids) and are bloodsucking parasites capable of transmitting a variety of diseases, including Lyme disease, ehrlichiosis, babesiosis and Rocky Mountain spotted fever. It’s easy to see ticks on your own skin, but it is more of a challenge when your furry companion is affected. Whenever you happen to be planning a stroll in a tick-infested area (especially forests, grassy or wooded areas or parks) be prepared to do a thorough inspection of your dog afterward to search for ticks. Ticks can be tricky, so make sure you spend time looking in the ears, between the toes and everywhere else where a tick might hide. Ticks need to be attached for 24–72 hours before they transmit most of the diseases that they carry, so you do have a window of opportunity for some preventive intervention.
Female ticks live to eat and breed. They can lay between 4,000 and 5,000 eggs and die soon after. Males, on the other hand, live only to mate and continue the process as long as they are able. Most ticks live on multiple hosts before parasitizing dogs. The immature forms typically reside on grass and shrubs, waiting for susceptible animals to walk by. The larvae and nymph stages typically feed on wildlife.
A TICKING BOMB
There is nothing good about a tick’s harpooning his nose into your dog’s skin. Among the diseases caused by ticks are Rocky Mountain spotted fever, canine ehrlichiosis, canine babesiosis, canine hepatozoonosis and Lyme disease. If a dog is allergic to the saliva of a female wood tick, he can develop tick paralysis.
If only a few ticks are present on a dog, they can be plucked out, but it is important to remove the entire head and mouthparts, which may be deeply embedded in the skin. This is best accomplished with forceps designed especially for this purpose; fingers can be used but should be protected with rubber gloves, plastic wrap or at least a paper towel. The tick should be grasped as closely as possible to the animal’s skin and should be pulled upward with steady, even pressure. It is important not to squeeze, crush or puncture the body of the tick or you risk exposure to any disease carried by that tick. Once the ticks have been removed, the sites of attachment should be disinfected. Your hands should then be thoroughly washed with soap and water to further minimize risk of contagion. The tick should be disposed of in a container of alcohol or household bleach.
Some of the newer flea products, specifically those with fipronil, selamectin and permethrin, have proven to be effective against some, but not all, species of tick. Flea collars containing appropriate pesticides (e.g., propoxur, chlorfenvinphos) can aid in tick control. In most areas, such collars should be placed on animals in March, at the beginning of the tick season, and changed regularly. Leaving the collar on when the pesticide level is waning invites the development of resistance. Amitraz collars are also good for tick control, and the active ingredient does not interfere with other flea-control products. The ingredient helps prevent the attachment of ticks to the skin and will cause those ticks already attached on the skin to detach themselves.
TICK CONTROL
Removal of underbrush and leaf litter and the thinning of trees in areas where tick control is desired are recommended. These actions remove the cover and food sources for small animals that serve as hosts for ticks. With continued mowing of grasses in these areas, the probability of ticks’ surviving is further reduced. A variety of insecticide ingredients (e.g., resmethrin, carbaryl, permethrin, chlorpyrifos, dioxathion and allethrin) are registered for tick control around the home.
MITES
Mites are tiny arachnid parasites that parasitize the skin of dogs. Skin diseases caused by mites are referred to as “mange,” and there are many different forms seen in dogs. These forms are very different from one another, each one warranting an individual description.
Sarcoptic mange, or scabies, is one of the itchiest conditions that affects dogs. The microscopic Sarcoptes mites burrow into the superficial layers of the skin and can drive dogs crazy with itchiness. They are also communicable to people, although they can’t complete their reproductive cycle on people. In addition to being tiny, the mites also are often difficult to find when trying to make a diagnosis. Skin scrapings from multiple areas are examined microscopically but, even then, sometimes the mites cannot be found.
Fortunately, scabies is relatively easy to treat, and there are a variety of products that will successfully kill the mites. Since the mites can’t live in the environment for very long without feeding, a complete cure is usually possible within four to eight weeks.
Cheyletiellosis is caused by a relatively large mite, which sometimes can be seen even without a microscope. Often referred to as “walking dandruff,” this also causes itching, but not usually as profound as with scabies. While Cheyletiella mites can survive longer in the environment than scabies mites, they too are relatively easy to treat, being responsive to not only the medications used to treat scabies but also often to flea-control products.
Otodectes cynotis is the canine ear mite and is one of the more common causes of mange, especially in young dogs in shelters or pet stores. That’s because the mites are typically present in large numbers and are quickly spread to nearby animals. The mites rarely do much harm but can be difficult to eradicate if the treatment regimen is not comprehensive. While many try to treat the condition with ear drops only, this is the most common cause of treatment failure. Ear drops cause the mites to simply move out of the ears and as far away as possible (usually to the base of the tail) until the insecticide levels in the ears drop to an acceptable level—then it’s back to business as usual! The successful treatment of ear mites requires treating all animals in the household with a systemic insecticide, such as selamectin, or a combination of miticidal ear drops combined with whole-body flea-control preparations.
Demodicosis, or red mange, can be one of the most difficult forms of mange to treat. Part of the problem is that the mites live in the hair follicles and they are relatively well shielded from topical and systemic products. The main issue, however, is that demodectic mange typically results only when there is some underlying process interfering with the dog’s immune system.
Since Demodex mites are normal residents of the skin of mammals, including humans, there is usually a mite population explosion only when the immune system fails to keep the number of mites in check. In young animals, the immune deficit may be transient or may reflect an actual inherited immune problem. In older animals, demodicosis is usually seen only when there is another disease hampering the immune system, such as diabetes, cancer, thyroid problems or the use of immune-suppressing drugs. Accordingly, treatment involves not only trying to kill the mange mites but also discerning what is interfering with immune function and correcting it if possible.
Chiggers represent several different species of mite that don’t parasitize dogs specifically, but do latch on to passersby and can cause irritation. The problem is most prevalent in wooded areas in the late summer and fall. Treatment is not difficult, as the mites do not complete their life cycle on dogs and are susceptible to a variety of miticidal products.
MOSQUITOES
Mosquitoes have long been known to transmit a variety of diseases to people, as well as just being biting pests during warm weather. They also pose a real risk to pets. Not only do they carry deadly heartworms but recently there also has been much concern over their involvement with West Nile virus. While we can avoid heartworm with the use of preventive medications, there are no such preventives for West Nile virus. The only method of prevention in endemic areas is active mosquito control. Fortunately, most dogs that have been exposed to the virus only developed flu-like symptoms and, to date, there have not been the large number of reported deaths in canines as seen in other species.
MOSQUITO REPELLENT
Low concentrations of DEET (less than 10%), found in many human mosquito repellents, have been safely used in dogs but, in these concentrations, probably give only about two hours of protection. DEET may be safe in these small concentrations, but since it is not licensed for use on dogs, there is no research proving its safety for dogs. Products containing permethrin give the longest-lasting protection, perhaps two to four weeks. As DEET is not licensed for use on dogs, and both DEET and permethrin can be quite toxic to cats, appropriate care should be exercised. Other products, such as those containing oil of citronella, also have some mosquito-repellent activity, but typically have a relatively short duration of action.
INTERNAL PARASITES: WORMS
ASCARIDS
Ascarids are intestinal roundworms that rarely cause severe disease in dogs. Nonetheless, they are of major public health significance because they can be transferred to people. Sadly, it is children who are most commonly affected by the parasite, probably from inadvertently ingesting ascarid-contaminated soil. In fact, many yards and children’s sandboxes contain appreciable numbers of ascarid eggs. So, while ascarids don’t bite dogs or latch onto their intestines to suck blood, they do cause some nasty medical conditions in children and are best eradicated from our furry friends. Because pups can start passing ascarid eggs by three weeks of age, most internal-parasite-control programs begin at two weeks of age and are repeated every two weeks until pups are eight weeks old. It is important to realize that bitches can pass ascarids to their pups even if they test negative prior to whelping. Accordingly, bitches are best treated at the same time as the pups.
HOOKWORMS
Unlike ascarids, hookworms do latch onto a dog’s intestinal tract and can cause significant loss of blood and protein. Similar to ascarids, hookworms can be transmitted to humans, where they cause a condition known as cutaneous larval migrans. Dogs can become infected either by consuming the infective larvae or by the larvae’s penetrating the skin directly. People most often get infected when they are lying on the ground (such as on a beach) and the larvae penetrate the skin. Yes, the larvae can penetrate through a beach blanket. Hookworms are typically susceptible to the same medications used to treat ascarids.
WHIPWORMS
Whipworms latch onto the lower aspects of the dog’s colon and can cause cramping and diarrhea. Eggs do not start to appear in the dog’s feces until about three months after the dog was infected. This worm has a peculiar life cycle, which makes it more difficult to control than ascarids or hookworms. The good thing is that whipworms rarely are transferred to people.
Some of the medications used to treat ascarids and hookworms are also effective against whipworms, but, in general, a separate treatment protocol is needed. Since most of the medications are effective against the adults but not the eggs or larvae, treatment is typically repeated in three weeks, and then often in three months as well. Unfortunately, since dogs don’t develop resistance to whipworms, it is difficult to prevent them from getting reinfected if they visit soil contaminated with whipworm eggs.
ASCARID DANGERS
The most commonly encountered worms in dogs are roundworms known as ascarids. Toxascaris leonine and Toxocara canis are the two species that infect dogs. Subsisting in the dog’s stomach and intestines, adult roundworms can grow to 7 inches in length and adult females can lay in excess of 200,000 eggs in a single day.
In humans, visceral larval migrans affects people who have ingested eggs of Toxocara canis, which frequently contaminates children’s sandboxes, beaches and park grounds. The roundworms reside in the human’s stomach and intestines, as they would in a dog’s, but do not mature. Instead, they find their way to the liver, lungs and skin, or even to the heart or kidneys in severe cases. Deworming puppies is critical in preventing the infection in humans, and young children should never handle nursing pups who have not been dewormed.
TAPEWORMS
There are many different species of tapeworm that affect dogs, but Dipylidium caninum is probably the most common and is spread by fleas. Flea larvae feed on organic debris and tapeworm eggs in the environment and, when a dog chews at himself and manages to ingest fleas, he might get a dose of tapeworm at the same time. The tapeworm then develops further in the intestine of the dog.
HOOKED ON ANCYLOSTOMA
Adult dogs can become infected by the bloodsucking nematodes we commonly call hookworms via ingesting larvae from the ground or via the larvae penetrating the dog’s skin. It is not uncommon for infected dogs to show no symptoms of hookworm infestation. Sometimes symptoms occur within ten days of exposure. These symptoms can include bloody diarrhea, anemia, loss of weight and general weakness. Dogs pass the hookworm eggs in their stools, which serves as the vet’s method of identifying the infestation. The hookworm larvae can encyst themselves in the dog’s tissues and be released when the dog is experiencing stress.
Caused by an Ancylostoma species whose common host is the dog, cutaneous larval migrans affects humans, causing itching and lumps and streaks beneath the surface of the skin.
The tapeworm itself, which is a parasitic flatworm that latches onto the intestinal wall, is composed of numerous segments. When the segments break off into the intestine (as proglottids), they may accumulate around the rectum, like grains of rice. While this tapeworm is disgusting in its behavior, it is not directly communicable to humans (although humans can also get infected by swallowing fleas).
A much more dangerous tapeworm is Echinococcus multilocularis, which is typically found in foxes, coyotes and wolves. The eggs are passed in the feces and infect rodents, and, when dogs eat the rodents, the dogs can be infected by thousands of adult tapeworms. While the parasites don’t cause many problems in dogs, this is considered the most lethal worm infection that people can get. Take appropriate precautions if you live in an area in which these tapeworms are found. Do not use mulch that may contain feces of dogs, cats or wildlife, and discourage your pets from hunting wildlife. Treat these tapeworm infections aggressively in pets, because if humans get infected, approximately half die.
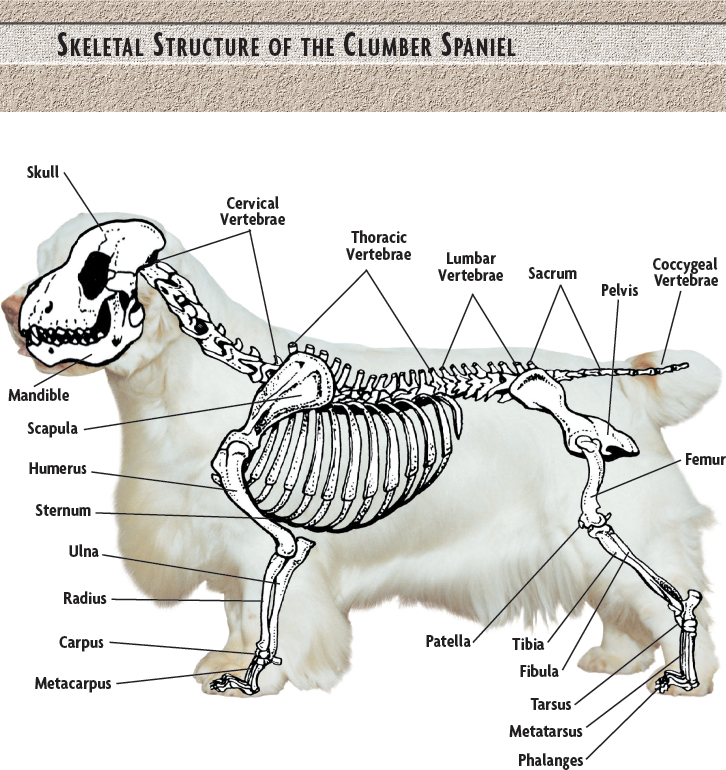
HEARTWORMS
Heartworm disease is caused by the parasite Dirofilaria immitis and is seen in dogs around the world. A member of the roundworm group, it is spread between dogs by the bite of an infected mosquito. The mosquito injects infective larvae into the dog’s skin with its bite, and these larvae develop under the skin for a period of time before making their way to the heart. There they develop into adults, which grow and create blockages of the heart, lungs and major blood vessels there. They also start producing offspring (microfilariae), and these microfilariae circulate in the bloodstream, waiting to hitch a ride when the next mosquito bites. Once in the mosquito, the microfilariae develop into infective larvae and the entire process is repeated.
When dogs get infected with heartworm, over time they tend to develop symptoms associated with heart disease, such as coughing, exercise intolerance and potentially many other manifestations. Diagnosis is confirmed by either seeing the microfilariae themselves in blood samples or using immunologic tests (antigen testing) to identify the presence of adult heartworms. Since antigen tests measure the presence of adult heartworms and microfilarial tests measure offspring produced by adults, neither are positive until six to seven months after the initial infection. However, the beginning of damage can occur by fifth-stage larvae as early as three months after infection. Thus it is possible for dogs to be harboring problem-causing larvae for up to three months before either type of test would identify an infection.
WORM-CONTROL GUIDELINES
• Practice sanitary habits with your dog and home.
• Clean up after your dog and don’t let him sniff or eat other dogs’ droppings.
• Control insects and fleas in the dog’s environment. Fleas, lice, cockroaches, beetles, mice and rats can act as hosts for various worms.
• Prevent dogs from eating uncooked meat, raw poultry and dead animals.
• Keep dogs and children from playing in sand and soil.
• Kennel dogs on cement or gravel; avoid dirt runs.
• Administer heartworm preventives regularly.
• Have your vet examine your dog’s stools at your annual visits.
• Select a boarding kennel carefully so as to avoid contamination from other dogs or an unsanitary environment.
• Prevent dogs from roaming. Obey local leash laws.
The good news is that there are great protocols available for preventing heartworm in dogs. Testing is critical in the process, and it is important to understand the benefits as well as the limitations of such testing. All dogs six months of age or older that have not been on continuous heartworm-preventive medication should be screened with microfilarial or antigen tests. For dogs receiving preventive medication, periodic antigen testing helps assess the effectiveness of the preventives. The American Heartworm Society guidelines suggest that annual retesting may not be necessary when owners have absolutely provided continuous heartworm prevention. Retesting on a two- to three-year interval may be sufficient in these cases. However, your vet will likely have specific guidelines under which heartworm preventives will be prescribed, and many prefer to err on the side of safety and retest annually.
It is indeed fortunate that heartworm is relatively easy to prevent, because treatments can be as life-threatening as the disease itself. Treatment requires a two-step process that kills the adult heartworms first and then the microfilariae. Prevention is obviously preferable; this involves a once-monthly oral or topical treatment. The most common oral preventives include ivermectin (not suitable for some breeds), moxidectin and milbemycin oxime; the once-a-month topical drug selamectin provides heartworm protection in addition to flea, some types of tick and other parasite controls.

Abrasions
Clean wound with running water or 3% hydrogen peroxide. Pat dry with gauze and spray with antibiotic. Do not cover.
Animal Bites
Clean area with soap and saline solution or water. Apply pressure to any bleeding area. Apply antibiotic ointment. Identify animal and contact the vet.
Antifreeze Poisoning
Induce vomiting and take dog to the vet.
Bee Sting
Remove stinger and apply soothing lotion or cold compress; give antihistamine in proper dosage.
Bleeding
Apply pressure directly to wound with gauze or towel for five to ten minutes. If wound does not stop bleeding, wrap wound with gauze and adhesive tape.
Bloat/Gastric Torsion
Immediately take the dog to the vet or emergency clinic; phone from car. No time to waste.
Burns
Chemical: Bathe dog with water and pet shampoo. Rinse in saline solution. Apply antibiotic ointment.
Acid: Rinse with water. Apply one part baking soda, two parts water to affected area.
Alkali: Rinse with water. Apply one part vinegar, four parts water to affected area.
Electrical: Apply antibiotic ointment. Seek veterinary assistance immediately.
Choking
If the dog is on the verge of collapsing, wedge a solid object, such as the handle of a screwdriver, between molars on one side of the mouth to keep mouth open. Pull tongue out. Use long-nosed pliers or fingers to remove foreign object. Do not push the object down the dog’s throat. For small or medium dogs, hold dog upside down by hind legs and shake firmly to dislodge foreign object.
Chlorine Ingestion
With clean water, rinse the mouth and eyes. Give the dog water to drink; contact the vet.
Constipation
Feed dog 2 tablespoons bran flakes with each meal. Encourage drinking water. Mix ¼-teaspoon mineral oil in dog’s food.
Diarrhea
Withhold food for 12 to 24 hours. Feed dog antidiarrheal with eyedropper. When feeding resumes, feed one part boiled hamburger, one part plain cooked rice, ¼- to ¾-cup four times daily. Contact vet if persists longer than 24 hours.
Dog Bite
Snip away hair around puncture wound; clean with 3% hydrogen peroxide; apply tincture of iodine. Identify biting dog and contact the vet. If wound appears deep, take the dog to the vet.
Frostbite
Wrap the dog in a heavy blanket. Warm affected area with a warm bath for ten minutes. Red color to skin will return with circulation; if tissues are pale after 20 minutes, contact the vet.
Heat Stroke
Partially submerge the dog in cold water; if no response within ten minutes, contact the vet.
Hot Spots
Mix 2 packets Domeboro® with 2 cups water. Saturate cloth with mixture and apply to hot spots for 15 to 30 minutes. Apply antibiotic ointment. Repeat every six to eight hours.
Poisonous Plants
Wash affected area with soap and water. Cleanse with alcohol. For foxtail/grass, apply antibiotic ointment. Contact the vet if plant is ingested.
Rat Poison Ingestion
Induce vomiting. Keep dog calm, maintain dog’s normal body temperature (use blanket or heating pad). Get to the vet for antidote.
Shock
Keep the dog calm and warm; call for veterinary assistance.
Snake Bite
If possible, bandage the area and apply pressure. If the area is not conducive to bandaging, use ice to control bleeding. Get immediate help from the vet.
Tick Removal
Apply flea and tick spray directly on tick. Wait one minute. Using tweezers or wearing plastic gloves, apply constant pull while grasping tick’s body. Apply antibiotic ointment.
Vomiting
Restrict dog’s water intake; offer a few ice cubes. Withhold food for next meal. Contact vet if vomiting persists longer than 24 hours.

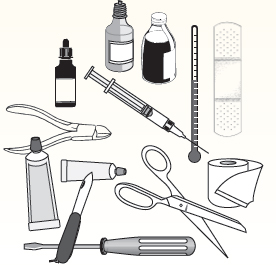
Use a portable, durable container large enough to contain all items.
DOG OWNER’S FIRST-AID KIT
 Gauze bandages/swabs
Gauze bandages/swabs
 Adhesive and non-adhesive bandages
Adhesive and non-adhesive bandages
 Antibiotic powder
Antibiotic powder
 Antiseptic wash
Antiseptic wash
 Hydrogen peroxide 3%
Hydrogen peroxide 3%
 Antibiotic ointment
Antibiotic ointment
 Lubricating jelly
Lubricating jelly
 Rectal thermometer
Rectal thermometer
 Nylon muzzle
Nylon muzzle
 Scissors and forceps
Scissors and forceps
 Eyedropper
Eyedropper
 Syringe
Syringe
 Anti-bacterial/fungal solution
Anti-bacterial/fungal solution
 Saline solution
Saline solution
 Antihistamine
Antihistamine
 Cotton balls
Cotton balls
 Nail clippers
Nail clippers
 Screwdriver/pen knife
Screwdriver/pen knife
 Flashlight
Flashlight
 Emergency phone numbers
Emergency phone numbers
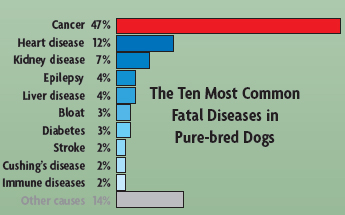
Number-One Killer Disease in Dogs: CANCER
In every age, there is a word associated with a disease or plague that causes humans to shudder. In the 21st century, that word is “cancer.” Just as cancer is the leading cause of death in humans, it claims nearly half the lives of dogs that die from a natural disease as well as half the dogs that die over the age of ten years.
Described as a genetic disease, cancer becomes a greater risk as the dog ages. Vets and dog owners have become increasingly aware of the threat of cancer to dogs. Statistics reveal that one dog in every five will develop cancer, the most common of which is skin cancer. Many cancers, including prostate, ovarian and breast cancer, can be avoided by spaying and neutering our dogs by the age of six months.
Early detection of cancer can save or extend a dog’s life, so it is absolutely vital for owners to have their dogs examined by a qualified vet or oncologist immediately upon detection of any abnormality. Certain dietary guidelines have also proven to reduce the onset and spread of cancer. Foods based on fish rather than beef, due to the presence of Omega-3 fatty acids, are recommended. Other amino acids such as glutamine have significant benefits for canines, particularly those breeds that show a greater susceptibility to cancer.
Cancer management and treatments promise hope for future generations of canines. Since the disease is genetic, breeders should never breed a dog whose parents, grandparents and any related siblings have developed cancer. It is difficult to know whether to exclude an otherwise healthy dog from a breeding program, as the disease does not manifest itself until the dog’s senior years.
RECOGNIZE CANCER WARNING SIGNS
Since early detection can possibly rescue your dog from becoming a cancer statistic, it is essential for owners to recognize the possible signs and seek the assistance of a qualified professional.
• Abnormal bumps or lumps that continue to grow
• Bleeding or discharge from any body cavity
• Persistent stiffness or lameness
• Recurrent sores or sores that do not heal
• Inappetence
• Breathing difficulties
• Weight loss
• Bad breath or odors
• General malaise and fatigue
• Eating and swallowing problems
• Difficulty urinating and defecating
“OLD-DOG” SYNDROME
There are many ways for you to evaluate old-dog syndrome. Veterinarians have defined canine cognitive dysfunction as the gradual deterioration of cognitive abilities, indicated by changes in the dog’s behavior. When a dog changes his routine response, and maladies have been eliminated as the cause of these behavioral changes, then canine cognitive dysfunction is the usual diagnosis.
More than half the dogs over eight years old suffer from some form of this syndrome. The older the dog, the more chance he has of suffering from it. In humans, doctors often dismiss the canine cognitive dysfunction behavioral changes as part of “winding down.”
There are four major signs of canine cognitive dysfunction: frequent potty accidents inside the home, sleeping much more or much less than normal, acting confused and failing to respond to social stimuli.
SYMPTOMS
FREQUENT POTTY ACCIDENTS
• Urinates in the house.
• Defecates in the house.
• Doesn’t signal that he wants to go out.
FAILURE TO RESPOND TO SOCIAL STIMULI
• Comes to people less frequently, whether called or not.
• Doesn’t tolerate petting for more than a short time.
• Doesn’t come to the door when you return home.
CONFUSION
• Goes outside and just stands there.
• Appears confused with a faraway look in his eyes.
• Hides more often.
• Doesn’t recognize friends.
• Doesn’t come when called.
• Walks around listlessly and without a destination.
SLEEP PATTERNS
• Awakens more slowly.
• Sleeps more than normal during the day.
• Sleeps less during the night.

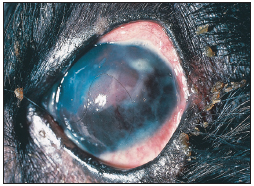
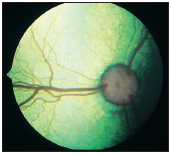
This is an example of a good eye on a Clumber Spaniel. The eyelids turn neither in nor out; the diamond-shaped lower lid is typical for the breed.
A PET OWNER’S GUIDE TO COMMON OPHTHALMIC DISEASES
by Prof. Dr. Robert L. Peiffer, Jr.
Few would argue that vision is the most important of the cognitive senses, and maintenance of a normal visual system is important for an optimal quality of life. Likewise, pet owners tend to be acutely aware of their pets’ eyes and vision, which is important because early detection of ocular disease will optimize therapeutic outcomes. The eye is a sensitive organ with minimal reparative capabilities, and with some diseases, such as glaucoma, uveitis and retinal detachment, early diagnosis and treatment can be critical in terms of whether vision can be preserved.
The causes of ocular disease are quite varied; the nature of dogs makes them susceptible to traumatic conditions, the most common of which include proptosis of the globe, cat scratch injuries and penetrating wounds from foreign objects, including sticks and air-rifle pellets. Infectious diseases caused by bacteria, viruses or fungi may be localized to the eye or part of a systemic infection. Many of the common conditions, including eyelid conformational problems, cataracts, glaucoma and retinal degenerations, have a genetic basis.
Before acquiring your puppy, it is important to ascertain that both parents have been examined and certified as free of eye disease by a veterinary ophthalmologist. Since many of these genetic diseases can be detected early in life, acquire the pup on the condition that he pass a thorough ophthalmic examination by a qualified specialist.

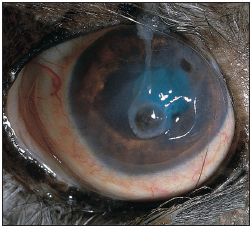
Lower entropion, or rolling in of the eyelid, is causing irritation in the left eye of this young dog. Several extra eyelashes are present on the lower lid, causing a condition known as distichiasis.
LID CONFORMATIONAL ABNORMALITIES
Rolling in (entropion) or out (ectropion) of the lids tends to be a breed-related problem. Entropion can involve the upper and/or lower lids. Signs usually appear between 3 and 12 months of age. The irritation caused by the eyelid hairs’ rubbing on the surface of the cornea may result in blinking, tearing and damage to the cornea.
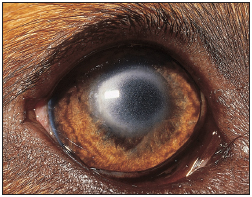
Keratoconjunctivitis sicca, seen here in the right eye of a middle-aged dog, causes a characteristic thick mucous discharge as well as secondary corneal changes.
Ectropion is likewise breed-related and is considered “normal” in hounds, for instance; unlike entropion, which results in acute discomfort, ectropion may cause chronic irritation related to exposure and the pooling of secretions. Most of these cases can be managed medically with daily irrigation with sterile saline and topical antibiotics when required.
EYELASH ABNORMALITIES
Dogs normally have lashes only on the upper lids, in contrast to humans. Occasionally, extra eyelashes may be seen emerging at the eyelid margin (distichiasis) or through the inner surface of the eyelid (ectopic cilia).

Prolapse of the gland of the third eyelid in the right eye of a pup.
CONJUNCTIVITIS
Inflammation of the conjunctiva, the pink tissue that lines the lids and the anterior portion of the sclera, is generally accompanied by redness, discharge and mild discomfort. The majority of cases are associated with either bacterial infections or dry-eye syndrome. Fortunately, topical medications are generally effective in curing or controlling the problem.
DRY-EYE SYNDROME
Dry-eye syndrome (keratoconjunctivitis sicca) is a common cause of external ocular disease. Discharge is typically thick and sticky, and keratitis is a frequent component; any breed can be affected. While some cases can be associated with toxic effects of drugs, including the sulfa antibiotics, the cause in the majority of the cases cannot be determined and is assumed to be immune-mediated.
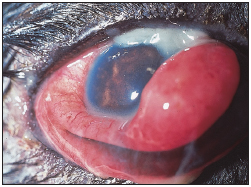
In this case, in the right eye of a young dog, the prolapsed gland can be seen emerging between the edge of the third eyelid and the corneal surface.
Multiple deep ulcerations affect the cornea of this middle-aged dog.
PROLAPSE OF THE GLAND OF THE THIRD EYELID
In this condition, commonly referred to as “cherry eye,” the gland of the third eyelid, which produces about one-third of the aqueous phase of the tear film and is normally situated within the anterior orbit, prolapses to emerge as a pink fleshy mass protruding over the edge of the third eyelid, between the third eyelid and the cornea. The condition usually develops during the first year of life and, while mild irritation may result, the condition is unsightly as much as anything else.
CORNEAL DISEASE
The cornea is the clear front part of the eye that provides the first step in the collection of light on its journey to eventually be focused onto the retina, and most corneal diseases will be manifested by alterations in corneal transparency. The cornea is an exquisitely innervated tissue, and defects in corneal integrity are accompanied by pain, which is demonstrated by squinting.
Corneal ulcers may occur secondarily to trauma or to irritation from entropion or ectopic cilia. In middle-aged or older dogs, epithelial ulcerations may occur spontaneously due to an inherent defect; these are referred to as indolent or Boxer ulcers, in recognition of the breed in which we see the condition most frequently. Infection may occur secondarily. Ulcers can be potentially blinding conditions; severity is dependent upon the size and depth of the ulcer and other complicating features.
Non-ulcerative keratitis tends to have an immune-mediated component and is managed by topical immunosuppressants, usually corticosteroids. Corneal edema can occur in elderly dogs. It is due to a failure of the corneal endothelial “pump.”
The cornea responds to chronic irritation by transforming into skin-like tissue that is evident clinically by pigmentation, scarring and vascularization; some cases may respond to tear stimulants, lubricants and topical corticosteroids, while others benefit from surgical narrowing of the eyelid opening in order to enhance corneal protection.
Lipid deposition can occur as a primary inherited dystrophy, or secondarily to hypercholesterolemia (in dogs, frequently associated with hypothyroidism), chronic corneal inflammation or neoplasia. The deposits in this dog assume an oval pattern in the center of the cornea.

Corneal edema can develop as a slowly progressive process in many breeds as a result of the inability of the corneal endothelial pump to maintain a state of dehydration.
UVEITIS
Inflammation of the vascular tissue of the eye—the uvea—is a common and potentially serious disease in dogs. While it may occur secondarily to trauma or other intraocular diseases, such as cataracts, most commonly uveitis is associated with some type of systemic infectious or neoplastic process. Uncontrolled, uveitis can lead to blinding cataracts, glaucoma and/or retinal detachments; aggressive symptomatic therapy with dilating agents (to prevent pupillary adhesions) and anti-inflammatories is critical.
Medial pigmentary keratitis in this dog is associated with irritation from prominent facial folds.
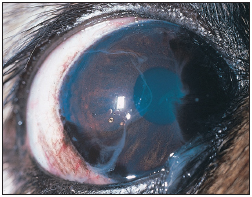
GLAUCOMA
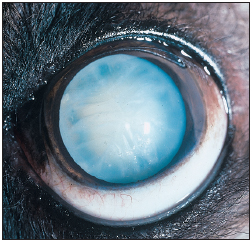
The eye is essentially a hollow fluid-filled sphere, and the pressure within is maintained by regulation of the rate of fluid production and fluid egress at 10–20 mm of mercury. The retinal cells are extremely sensitive to elevations of intraocular pressure and, unless controlled, permanent blindness can occur within hours to days. In acute glaucoma, the conjunctiva becomes congested, the cornea cloudy, the pupil moderate and fixed; the eye is generally painful and avisual. Increased constant signs of discomfort will accompany chronic cases.
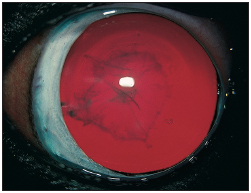
Glaucoma In the dog most commonly occurs as a sudden extreme elevation of Intraocular pressure, frequently to three to four tImes the norm. The eye of this dog demonstrates the common signs of episcleral injection, or redness; mild diffuse corneal cloudiness, due to edema; and a midsized fixed pupil.
Management of glaucoma is one of the most challenging situations the veterinary ophthalmologist faces; in spite of intense efforts, many of these cases will result in blindness.
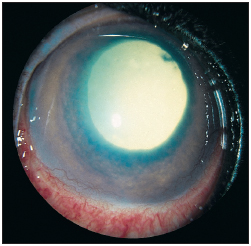
CATARACTS AND LENS DISLOCATION
Cataracts are the most common blinding condition in dogs; fortunately, they are readily amenable to surgical intervention, with excellent results in terms of restoration of vision and replacement of the cataractous lens with a synthetic one. Most cataracts in dogs are inherited; less commonly, cataracts can be secondary to trauma or to other ocular diseases, including uveitis, glaucoma, lens luxation and retinal degeneration, or secondary to an underlying systemic metabolic disease, including diabetes and Cushing’s disease. Signs include a progressive loss of the bright dark appearance of the pupil, which is replaced by a blue-gray hazy appearance. In this respect, cataracts need to be distinguished from the normal aging process of nuclear sclerosis, which occurs in middle-aged or older animals, and has minimal effect on vision.
The typical posterior subcapsular cataract appears between one and two years of age, but rarely progresses to where the animal has visual problems.
Lens dislocation occurs in dogs and frequently leads to secondary glaucoma; early removal of the dislocated lens is generally curative.
RETINAL DISEASE
Retinal degenerations are usually inherited but may be associated with vitamin E deficiency in dogs. While signs are variable, most frequently one notes a decrease in vision over a period of months, which typically starts out as a night blindness. The cause of a more rapid loss of vision due to retinal degeneration occurs over days to weeks is labeled sudden acquired retinal degeneration or SARD; the outcome, however, is unfortunately usually similar to inherited and nutritional conditions, as the retinal tissues possess minimal regenerative capabilities. Most pets, however, with a bit of extra care and attention, show an amazing ability to adapt to an avisual world and can be maintained as pets with a satisfactory quality of life.
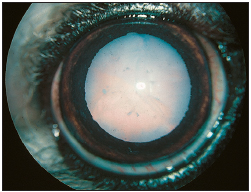
Inherited cataracts generally appear between three and six years of age and progress to the stage seen where functional vision is significantly impaired.
Anterior lens luxation can occur as a primary disease in some breeds, or secondarily to trauma. The fibers that hold the lens in place rupture and the lens may migrate through the pupil to be situated in front of the iris. Secondary glaucoma is a frequent and significant complication that can be avoided if the dislocated lens is removed surgically.
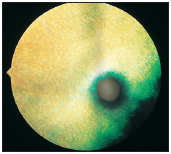
The posterior pole of a normal fundus is shown; prominent are the head of the optic nerve and the retinal blood vessels. The retina is transparent, and the prominent green tapetum is seen superiorly.
An eye with inherited retinal dysplasia is depicted. The tapetal retina superior to the optic disc is disorganized, with multifocal areas of hyperplasia of the retinal pigment epithelium.
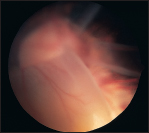
Severe collie eye anomaly and a retinal detachment; this eye unfortunately is blind.

Detachment of the retina—due to accumulation of blood between the retina and the underlying uvea, which is called the choroid—can occur secondarily to retinal tears or holes or tractional forces within the eye, or as a result of uveitis. These types of detachments may be amenable to surgical repair if diagnosed early.
OPTIC NERVE
Optic neuritis, or inflammation of the nerve that connects the eye with the brain stem, is a relatively uncommon condition that occurs usually with rather sudden loss of vision and widely dilated non-responsive pupils.