Before we dive into the science on exercise and the gut, it will be helpful to establish a base of knowledge on the anatomy and function of the digestive system. Thus, we begin by taking a stepwise journey through the gut, from the mouth to (you guessed it!) the anus. As you’ll come to see, the alimentary canal is not 30 feet of tubular uniformity. Rather, each section of the gut was designed (or, more precisely, has evolved) to carry out distinct aspects of the digestive process. To put it another way, the gut is sort of like an automobile assembly line, in that each section carries out a unique task and all of these sections need to function properly for a car to come out right. A Ferrari that has no wheels won’t be able to hit 200 miles per hour no matter how well the rest of the car is put together. Similarly, a malfunction occurring in any part of your gut can dramatically change what gets digested and absorbed and how your body functions, usually for the worse.
The purpose of this chapter isn’t to detail every function of the gut. Instead, my goal is to strike a balance of providing enough information so that you understand how nutritional and other choices impact your gut’s function while also avoiding so much detail that you’re bored to tears. Even with this simplified overview of the digestive system, some of the information gets technical, though hopefully not pedantic. Don’t fret if you find it challenging to follow each and every detail; the most important takeaway is a general sense of how your gut is structured (in terms of order; see Figure 1.1) and how the basic processes of digestion and absorption work.
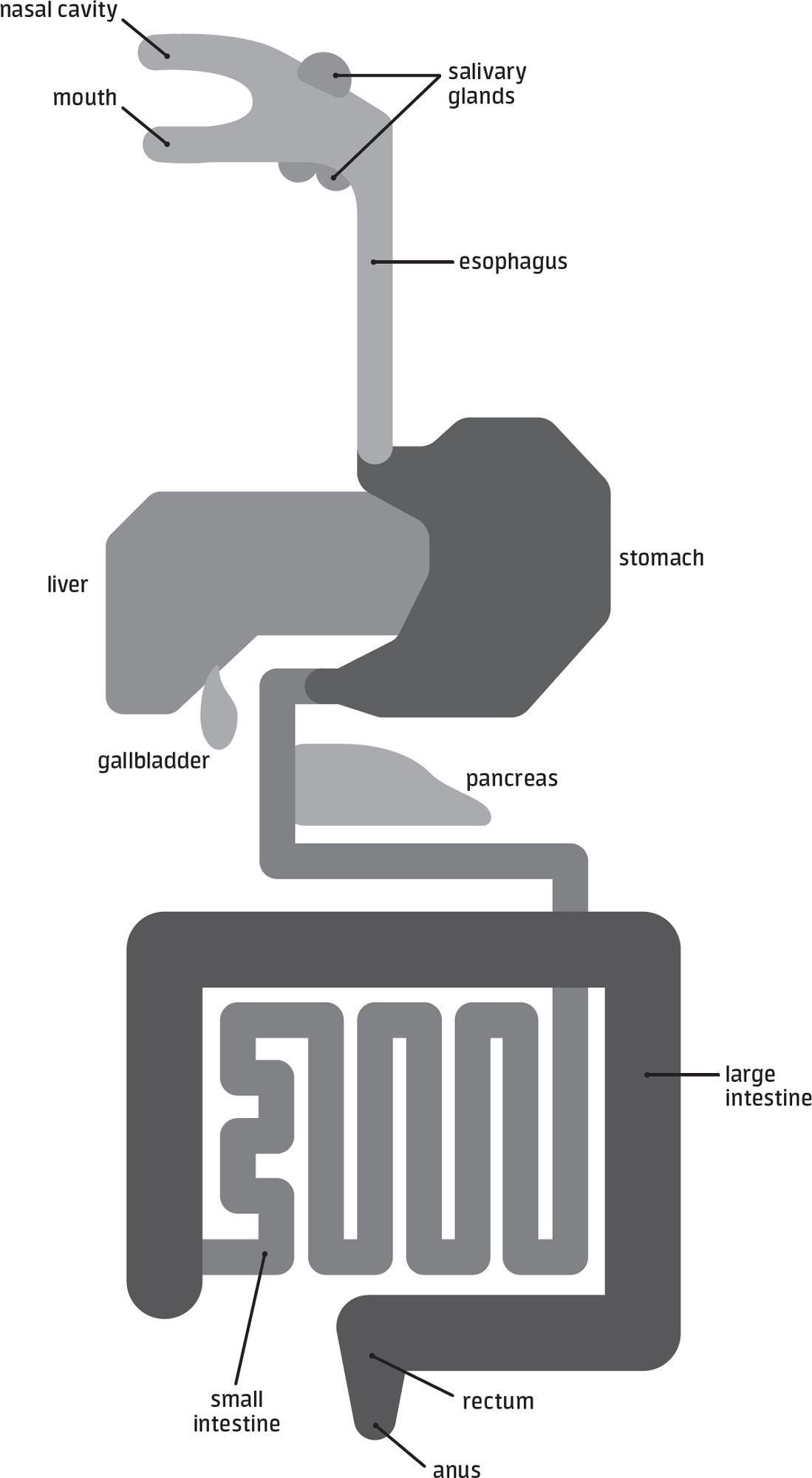
figure 1.1ANATOMY OF THE GUT

This roughly 30-foot-long system is responsible for digesting and absorbing the foods you eat.
If facts about digestion really aren’t your jam, you could consider skipping ahead to subsequent chapters, as the majority of the practical information presented later on isn’t dependent on having an in-depth knowledge of digestive processes. However, if you do jump ahead, bear in mind that you’ll be missing out on references to Mick Jagger, Shaquille O’Neal, Muggsy Bogues, blue whales, a shark movie, anacondas, hot dog eating contests, Sir Michael Caine, and Meryl Streep!
THE MOUTH
The first stop on our alimentary journey is the mouth. Although there are several techniques for quantifying mouth size, one way is to have people suck as much fluid into their mouths as humanly possible without swallowing, which is precisely what one 2012 study asked volunteers to do.1 The average adult was able to hold approximately 2 ounces of fluid in their mouth, which is about the size of a chicken egg, though the best of the best were able to hold more than 3 ounces. Interestingly, researchers found a correlation between external facial measurements and volumes that participants could keep in their mouths. To put that in layman’s terms, Mick Jagger and Steven Tyler (of the Rolling Stones and Aerosmith, respectively, for my non-rock ’n roll-literate readers) probably have larger capacities for holding grub in their pieholes than most other front men, though you probably didn’t need a scientific study to tell you that.
When it comes to function, the most important job of your mouth is to mechanically break apart solid foods you eat, from fruits and vegetables to head-sized burritos (no judgment here . . .). The grinding and chewing that occurs in your mouth is a bit like the process of crushing grapes before they’re made into wine, and this physical breakdown of food makes the process of chemical digestion easier by increasing the surface area where enzymes work their magic. Amylase is one of the first enzymes your body deploys to get this process of chemical digestion rolling. It’s released from your salivary glands into your lumen, which is just jargon for the hollow space by which food passes through you. Salivary amylase’s job is to attack the bonds that hold large carbohydrate molecules together, breaking them apart into shorter chains. Another enzyme, lingual lipase, is also secreted in the mouth and initiates fat digestion. While lingual lipase is an important enzyme in animals such as mice (and human babies), adult humans secrete it in only small amounts, and, consequently, little fat digestion takes place in your mouth.
Once you’ve finished masticating (chewing), the next step in the digestive process is swallowing. While a seemingly simple task, swallowing requires all the precision and coordination of a championship-caliber dance team. Most of us take for granted that this intricate feat of physiology occurs almost flawlessly five hundred to a thousand times every day, including several dozen times while we sleep.2 In the first step, your tongue holds and presses the semispherical mass of food (called a bolus) against the roof of your mouth, at which point it sends the bolus to your oropharynx, the section of throat behind your oral cavity. Sensory receptors detect this bolus, triggering the base of your tongue to drop and your uvula—that punching bag of flesh at the back of your mouth—to elevate, opening a path for the bolus to travel through. To prevent choking, several automatic actions kick in, including the covering of your airway by your epiglottis, a stiff flap of tissue at the base of your tongue. These and other steps need to occur in a coordinated, sequential manner for a successful swallow to occur. Aberrations in swallowing contribute to a multitude of health issues, including several thousand cases of death by choking every year in the US alone.3
THE ESOPHAGUS
The next stop on our enteral voyage is the esophagus, or as our vowel-happy Brit friends like to spell it, the oesophagus. Your esophagus serves chiefly as a transport tube between your mouth and your stomach.
An average adult’s esophagus is roughly 41 centimeters long (measuring from the incisors to the esophagogastric junction),4 although lengths vary based on a number of factors, most importantly one’s vertical prowess. At 7'1", Shaquille O’Neal’s esophagus is expected to be 54 centimeters long, while at just 5'3", Muggsy Bogues (the shortest basketball player in NBA history) is estimated to have an esophagus right around the average of 41 centimeters. And coming in at staggering 8'11", the tallest human in recorded history, Robert Pershing Wadlow, would have had an esophageal length of 68 centimeters, which, if you’re curious, is about the length of an alligator snapping turtle or a smallish bobcat.
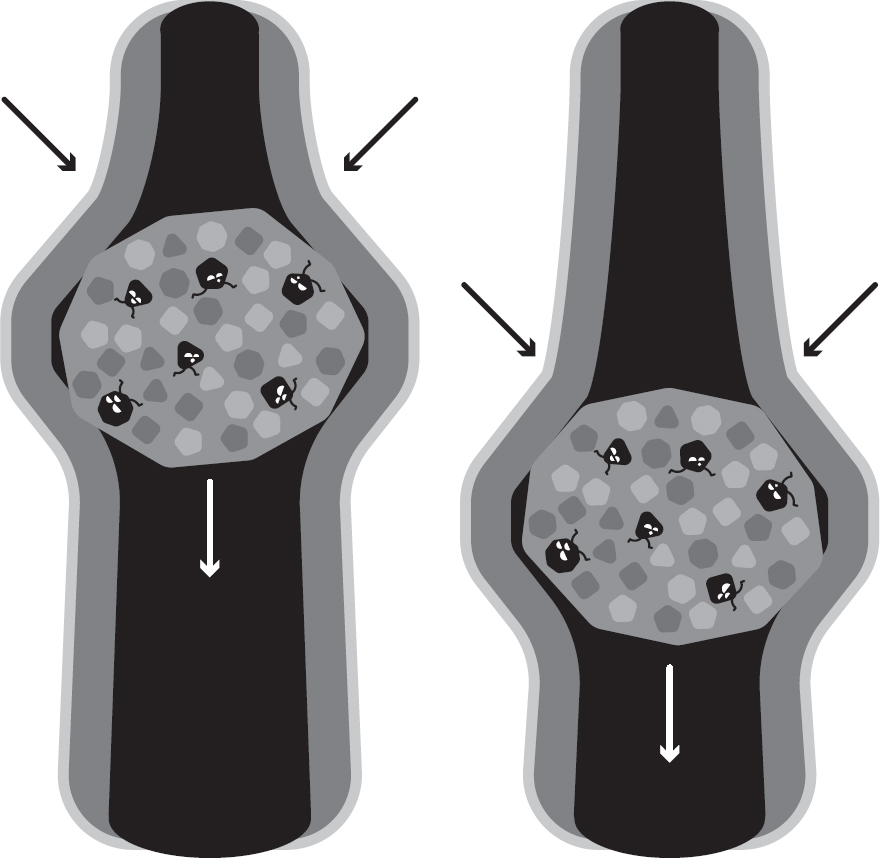
figure 1.2PERISTALSIS

This wavelike motion propels foodstuffs forward through the constriction and relaxation of your gut’s walls.
Regardless of whether your esophagus is like Shaquille O’Neal’s or more like that of Muggsy Bogues, its ability to regulate the movement of foodstuffs is impressive. In fact, the passage of a bolus through your esophagus is so well coordinated that you could, in Count Dracula–style, swallow blood (or any non-vampire sustenance of your choice) while hanging upside down from the ceiling. This also explains why astronauts are able to eat and drink in zero-gravity environments. Your esophagus achieves these gravity-defying feats via a process called peristalsis, which is a wavelike motion in your gut’s walls created by the constricting and relaxing of smooth muscles. In very simplistic terms, peristalsis is a better-coordinated version of squeezing toothpaste out of its tubing or squeezing ketchup out of a packet. Once the swallowing process is initiated, it takes about 5 to 10 seconds for peristaltic waves to transport a bolus through the entirety of a normally functioning esophagus5 (see Figure 1.2).
The entry and exit of a bolus into and out of your esophagus is regulated by sphincters, your gut’s security gates. Sphincters are specialized rings of muscle that open and close based on input from your nervous system; thankfully, most of your sphincters open and close without conscious input. (For those of us inept at multitasking, having to consciously regulate our sphincters would spell disaster for general life productivity.) Entry of a food bolus into your esophagus is controlled by your upper esophageal sphincter, while at the bottom end of your esophagus, your lower esophageal sphincter controls entry into your stomach. Dysfunction of these sphincters—particularly the lower sphincter—contributes to disorders such as gastroesophageal reflux disease (GERD), which is discussed in subsequent chapters.
THE STOMACH
Compared to the other portions of your gut, your stomach has an enormous capacity for expansion. The stomach is kind of like the puffer fish of the gut; it’s about the size of a fist when empty, but at max capacity it can hold 2 to 4 liters of foodstuffs, representing a 50-to-75-fold increase in volume. While that may seem like a lot of chow, it’s by no means anywhere close to the largest capacity for mammals, as it’s been estimated that it takes over a ton of krill to fill a blue whale’s stomach.6
Interestingly, the maximum volume of food that people can tolerate in their stomachs depends on their typical eating behaviors. In essence, if you’re a regular at Old Country Buffet, you can almost certainly tolerate greater volumes of foodstuffs before feeling uncomfortably full. In one illustrative study, three groups of women had balloons placed into their stomachs that were gradually inflated to the point of maximum discomfort.7 The first to sense discomfort were women with normal body weights, who were only able to tolerate about 0.75 liter of inflation before tapping out. As you might expect from people who habitually eat enough food to gain excess body weight, the obese women tolerated a higher volume (about 0.9 liter), but this was almost entirely driven by a subset of women who binge ate. Specifically, obese women who regularly binged were able to tolerate close to 1.0 liter of inflation, while obese women who didn’t regularly binge responded on par with the women with normal body weights. Finally, the most impressive tolerance to stomach distension, coming in at a whopping 1.2 liters of balloon inflation, was found in women with bulimia (a hallmark of bulimia is recurrent binge eating).
Obviously, inflating a balloon in the stomach isn’t eating, but these results suggest that the stomach can be trained to hold large volumes of stuff, including food. The most extreme example of this stomach trainability concept comes from the world of competitive eating. The world record (set in 2018) in hot dog eating, for example, is 74 franks in 10 minutes, which is held by Joey Chestnut, the LeBron James of the competitive eating world. (If you’re curious, 74 hot dogs and buns adds up to over 20,000 kilocalories, which is about 7 to 10 days’ worth of food for us mere mortals.)
Unfortunately, there’s scant research on how competitive eating changes the structure and function of the stomach over time, but fascinatingly, researchers at the University of Pennsylvania did get an opportunity to evaluate a competitive eater during a simulated hot dog eating contest. For the study, the eater (later reported to be first-class eater Tim Janus) and a control subject the researchers reported as having “a hearty appetite” consumed hot dogs along with barium, a substance that, when mixed with water, coats the gut and allows the size and shape of components of the digestive tract to be visualized with fluoroscopy, a sort of X-ray movie. What happened to Janus’s stomach was described in the researchers’ 2007 article:
“Intermittent fluoroscopy revealed progressive accumulation of an ever-increasing volume of hot dog pieces outlined by residual barium in the stomach. . . . At 6 minutes, the stomach had become a dilated, flaccid sac. . . . At 10 minutes, the speed eater had eaten a total of 36 hot dogs. His stomach now appeared as a massively distended, food-filled sac occupying most of the upper abdomen.”8
Images of Janus’s stomach shown in the article are almost unrecognizable, looking more like a fireball explosion than a portion of a human being’s alimentary canal. Bear in mind that he ate “only” 36 hot dogs without buns, which is roughly half of the current world record of 74 red-hots with buns. In case you’re wondering, the fellow with the “hearty appetite” that served as the control subject managed to down a measly seven dogs before saying he was about to be sick.
Undeniably, competitive eaters and individuals with bulimia prove the stomach is more than capable of accommodating sizeable quantities of food. You would think that these extreme binging episodes would rupture the stomach on occasion, but that sort of catastrophic injury is very rare. Still, there are a few case reports of individuals dying or experiencing major harm from gorging themselves. In one report published in The Lancet, a 23-year-old model with bulimia perished after eating 19 pounds of food in one sitting—among a host of items, she ate two pounds each of carrots, plums, grapes, and kidneys.9 In another case, a woman died after overindulging on two loaves of bread, three sweet buns, two packs of instant noodles, 4.3 liters of carbonated water, and 1.4 liters of beer.10 Somehow her stomach withstood this onslaught of carby goodness without bursting, but her luck ran out when her distended stomach compressed her inferior vena cava (a large vein) and heart as she lay on a hospital examination table. Remarkably, the occlusion of major blood vessels after extreme binges has been documented in similar cases, including a man whose aorta was blocked after reportedly scarfing down 10 meals’ worth of food at lunch11 and a woman whose aorta was obstructed after gorging on an unknown quantity of food (though 15 liters of gastric contents were emptied from her stomach).12
Now that we’ve established some facts (including a few macabre ones) about the stomach’s capacity to act as a food depot, let’s return to the actual process of digestion. Mechanical digestion continues via peristalsis and strong, coordinated muscle contractions that churn and mix food boluses. However, churning and mixing only go so far, so your body turns loose its chemical warriors, acid and enzymes. Gastric lipase is one of these chemical warriors, and in contrast to the low amounts of lingual lipase in your mouth, the stomach version contributes substantially to fat digestion. Carbohydrate digestion continues as salivary amylase accompanies food boluses into your stomach, but with time, it’s deactivated in the stomach’s acidic environment, leaving a substantial proportion of carbohydrate digestion to be handled in your small intestine.
Protein is also a target of digestion in your stomach, perhaps more so than fat and carbohydrate. The stomach is a hostile place for proteins, thanks in large part to the secretion of caustic hydrochloric acid from so-called parietal cells (see Figure 1.3). Hydrochloric acid has a couple of jobs as it relates to breaking down protein. First, it unravels the three-dimensional structure of proteins through a process called denaturation. This unraveling allows enzymes to attack the peptide bonds that keep proteins together. Denaturing a protein is sort of like removing your clothes on a cold winter’s day, in that it leaves you entirely vulnerable to the elements. In the case of proteins, denaturation leaves them defenseless against enzymes. The second thing that hydrochloric acid does is activate a protein-digesting enzyme, pepsin. The inactive version of this enzyme (pepsinogen) is secreted from a different set of specialized cells known as chief cells. Pepsinogen itself doesn’t digest protein, but in the presence of hydrochloric acid, pepsinogen transforms to pepsin. (Pepsinogen is like the hapless Clark Kent while pepsin is like Superman.) Activated pepsin then splits apart proteins into smaller molecules such as peptones and polypeptides, which are chains of amino acids, the basic building blocks of proteins.
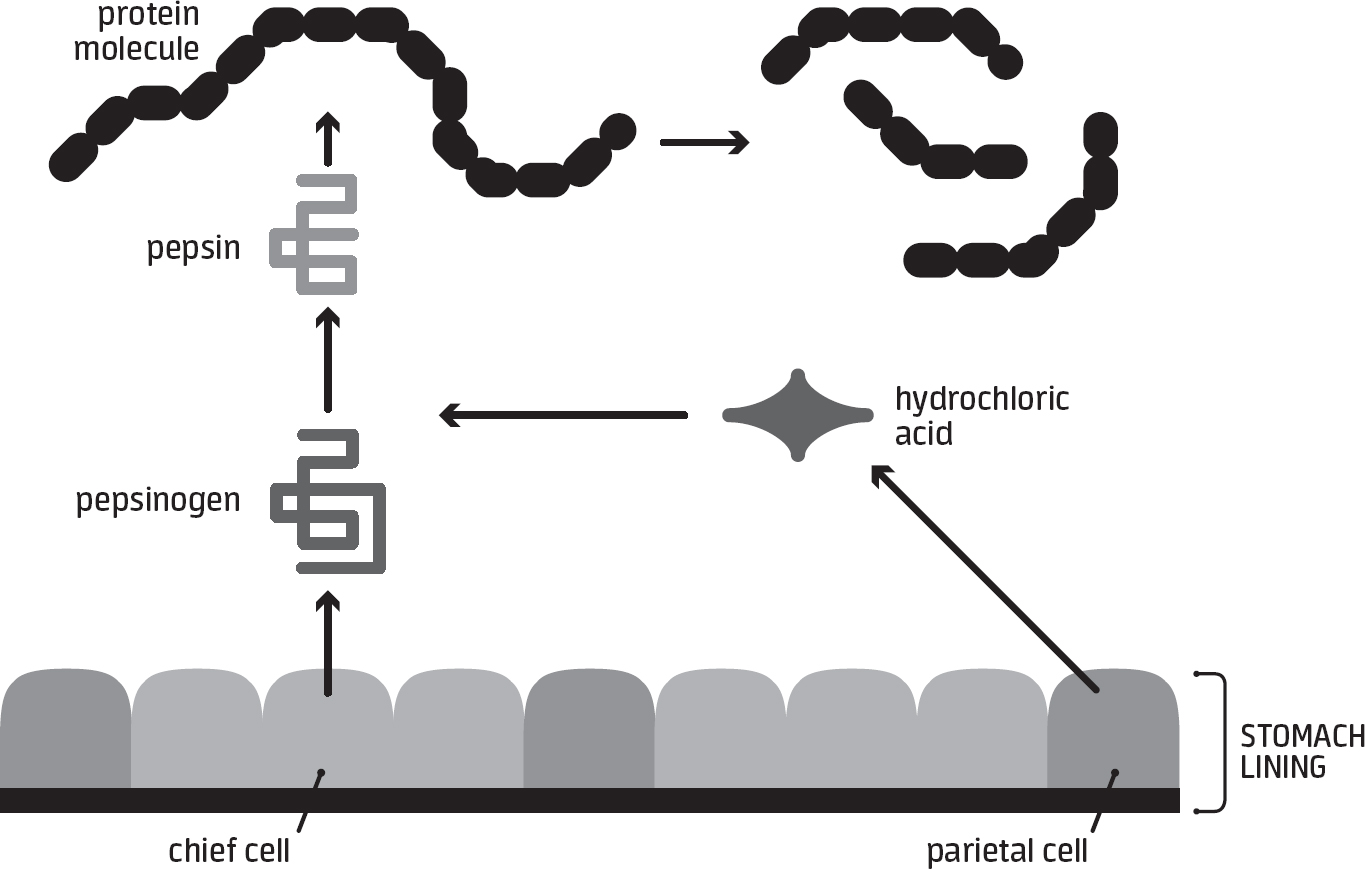
figure 1.3PROTEIN DIGESTION

The stomach is a major site of protein digestion, which is facilitated through the release of hydrochloric acid and activation of pepsinogen to pepsin.
The fact that your stomach is a hot spot of protein digestion has several implications. Logically, upping the protein in a meal should increase the time required for hydrochloric acid and pepsin to break down that protein. Indeed, including a substantial amount of protein in a meal—say, from a half-pound burger or an entire turkey leg—is known to lengthen the time it takes for a meal to empty from the stomach, which is one reason high-protein diets seem to blunt hunger more than other diets.13 In addition, the slowed emptying that accompanies a protein-rich meal means it isn’t a wise choice to eat a thick, juicy steak an hour before commencing intense exercise.
Another vital job of your stomach is to regulate the flow of substances into your small intestine. If semidigested food—referred to as chyme—passes from your stomach to your small intestine too quickly, it can overwhelm your small intestine, which, in turn, can trigger symptoms like abdominal cramping, flatulence, and diarrhea. To prevent this, your gut has evolved an elegant feedback system that tells your stomach to step on the metaphorical brake pedal if your small intestine detects too much of certain substances. This feedback is analogous to engineers reducing the flow of water through a mountain dam after getting reports of heavy water flows down in the valley below.
There are a variety of substances that, when detected in your small intestine, inhibit stomach emptying. For example, when hydrochloric acid, polypeptides (products of protein digestion), sugars (particularly glucose), or free fatty acids enter your small intestine, contractions in your stomach are curtailed, which ultimately retards the emptying of chyme.14 Likewise, fluids that are hypertonic or hypotonic (i.e., well above or well below the concentration of your blood) hinder emptying. Sports beverage makers have long known this, which is why most sports drinks are concocted to contain roughly 6 percent carbohydrate (ensuring that the osmolality doesn’t deviate extremely from that of your blood). Most drinks markedly above 6 percent carbohydrate hinder fluid emptying from the stomach. You can calculate the carbohydrate concentration of a sports beverage by dividing the grams of carbohydrate in one serving (listed on the Nutrition Facts panel) by the volume of one serving in milliliters. (There are roughly 30 milliliters in 1 ounce, so as an example, a 20-ounce bottle is equivalent to about 600 milliliters.)
The emptying of chyme is also regulated by the opening and closing of your pyloric sphincter, which serves as the gateway between the world of the stomach and the world of the small intestine. (Pylorus is from the Greek word for “gatekeeper.”) Your pyloric sphincter is essentially a bouncer that works the door at Club Small Intestine, preventing too many partygoers from entering all at once and ruining an otherwise enjoyable evening. A visual representation of these feedback responses (which are regulated through connections between your gut and nervous system) is shown in Figure 1.4.
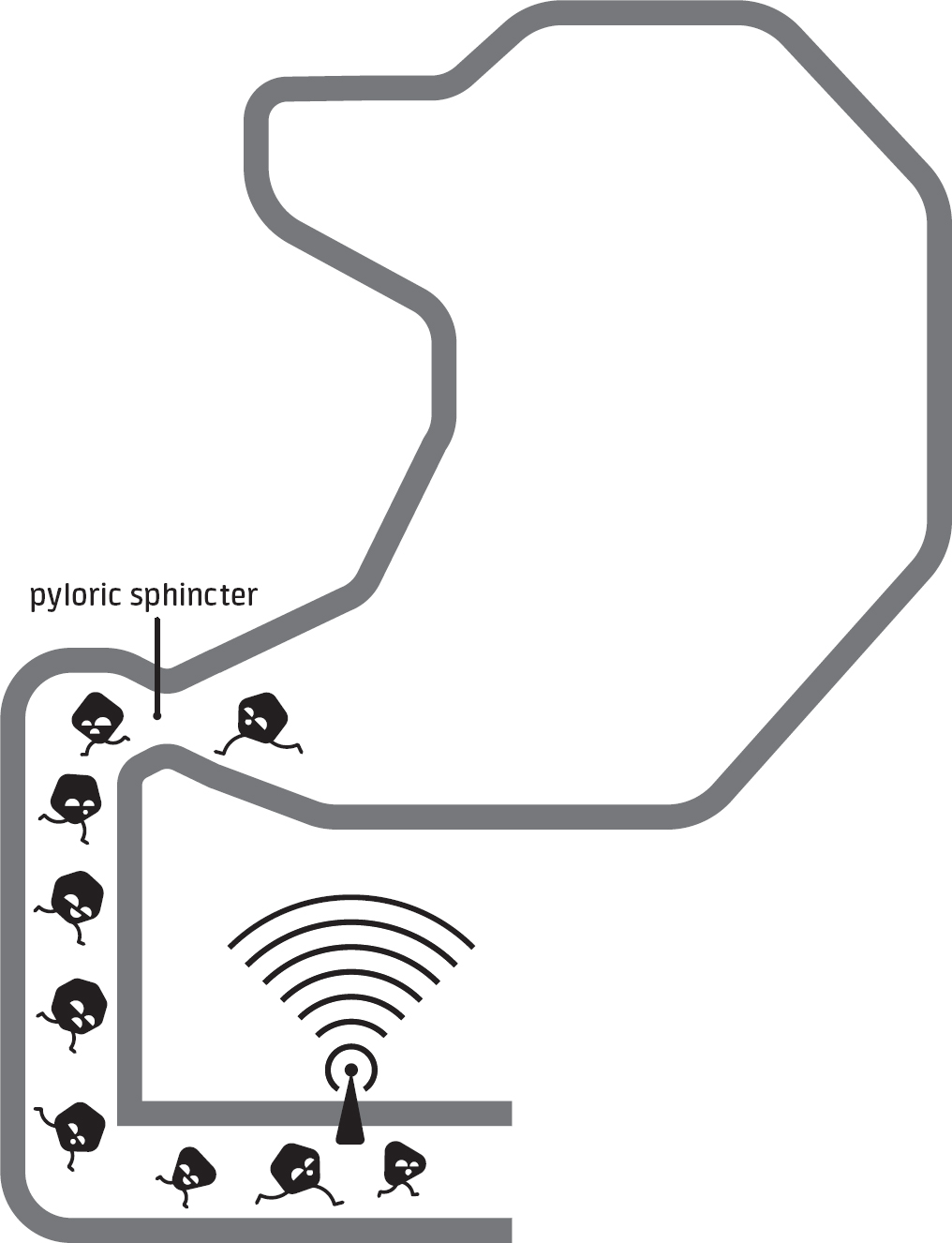
figure 1.4REGULATION OF GASTRIC EMPTYING

The rate of emptying from your stomach is regulated, in part, by the activation of sensory tissue in your small intestine that communicates with the stomach via the nervous system.
THE SMALL INTESTINE
The small intestine is by far the longest portion of the gut, so to be able to fit all of this tissue in your abdominal cavity, your small intestine takes on a coiled orientation. Though lengths vary based on how the measurements are taken (and whether they’re taken from a corpse or a living, breathing human), the typical small intestine is 3 to 7 meters long.15 To give you some perspective, that’s the same length as a female green anaconda snake. Yes, you heard that right, there’s the equivalent of an anaconda—albeit a skinny, hollow version—residing inside your abdomen.
Your small intestine is made up of three segments with odd-sounding names: in sequential order, they are the duodenum, jejunum, and ileum. The name duodenum comes from a Latin translation of an old Greek phrase that meant “12 finger widths.” (While conducting autopsies at the Mouseion of Alexandria, the Greek anatomist Herophilos of Chalcedon observed that the first part of the intestine was 12 finger widths in length.)16 As chyme enters your duodenum, the digestive process for carbohydrates, fats, and proteins is taken over by your pancreas. Putting out an estimated 2.5 liters of juices per day, the pancreas is the workhorse of your digestive system.17 To use a pop culture reference, I like to think of the pancreas as the Michael Caine of the digestive tract—it just keeps working. According to the website IMDb.com, Sir Caine had 175 acting credits as of 2020, including a role as carefree pilot Hoagie Newcombe in Jaws: The Revenge, widely thought of as one of the worst movies of all time. (As awful as the film is, it’s worth checking out the ending on YouTube if you’re in need of a good laugh.) To be fair to Caine, he also owns two Oscars for Best Supporting Actor.
This flow of pancreatic juices is stimulated by stomach acid (and other substances) coming into contact with the cells lining your duodenum. In turn, this leads to the secretion of hormones (secretin and cholecystokinin, for example) into your bloodstream. These hormones then travel to your pancreas and tell it to dump its juices into your small intestine (see Figure 1.5). One of the most important substances discharged from your pancreas is bicarbonate, an acid buffer. Unlike your stomach (which protects itself by producing a mucus that acts as a defensive barrier), your small intestine isn’t equipped to deal with chronic exposure to strong acids, so your pancreas secretes bicarbonate. In addition to acid-squelching bicarbonate, your pancreas releases several enzymes that target fat, protein, and carbohydrate molecules. Pancreatic lipase acts on fat molecules (triglycerides and diglycerides), while pancreatic amylase continues to split apart starch and other carbohydrates. The process of protein digestion is continued through the release of precursor enzymes known as trypsinogen and chymotrypsinogen, which end up being fully activated to trypsin and chymotrypsin. Like other parts of the gut, your small intestine relies on peristalsis to keep chyme and these digestive juices moving forward.
Apart from your pancreas, your liver also plays an instrumental role in the digestion that occurs in your small intestine. Bile is produced in your liver, temporarily stored in your gall bladder, and ultimately released into your small intestine lumen. It acts to emulsify globs of fat, downsizing them into smaller fat droplets. Emulsification of fat is necessary because pancreatic lipase is water-soluble, meaning it can’t effectively penetrate large globs of fat to do its job. Thus, transforming these fat globs into smaller droplets dramatically increases the area where lipases can work.
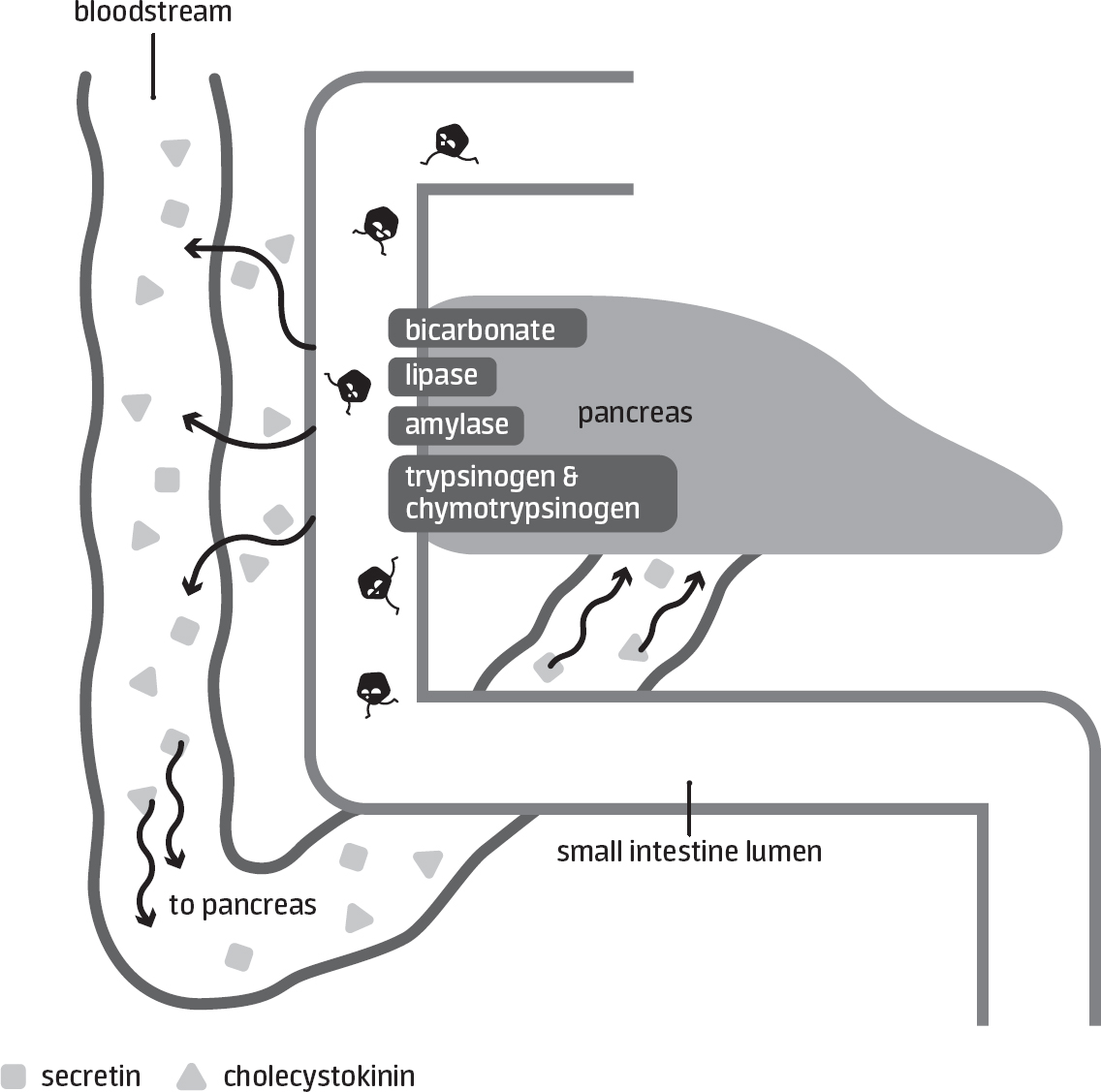
figure 1.5DIGESTION IN THE SMALL INTESTINE

The entry of chyme into the small intestine triggers the secretion of hormones (secretin and cholecystokinin) from specialized gut cells. These hormones travel to the pancreas via the bloodstream and cause pancreatic juices (water, enzymes, and bicarbonate) to be dumped into the small intestine lumen.
In addition to serving as a location for digestion, your small intestine is the alimentary canal’s most important site of absorption. Over the course of adulthood (say, from 18 to 80 years of age), people in industrialized societies can consume the equivalent of a female rhinoceros’s mass worth of protein, a male hippo’s mass worth of fat, an elephant’s mass worth of carbohydrate, and 15,000 to 20,000 gallons of water. Even more astonishing are the consumption totals of serious athletes; a runner who trains heavily and runs marathons for 30-plus years might consume a triceratops’s mass worth of carbohydrate and 25,000 to 30,000 gallons of water over their adult life. The vast majority of these ingested nutrients get absorbed somewhere in your small bowel. If you need further proof of its importance, keep in mind that surgical removal of large sections of the small intestine leads to severe health consequences in comparison to when other parts of the gut are excised.18 To return to pop culture analogies, if the pancreas is the Michael Caine of the gut, then the small intestine is the Meryl Streep—always doing vital work. (As of 2020, Streep had received a staggering 21 Oscar nominations.)
Your small intestine’s immense capacity for absorption is a product of its anatomy. On a gross level, it has numerous circular folds that increase the area where absorption occurs. If you zoomed in on these folds, you’d see that the epithelial cells lining your small intestine are arranged in such a way that they form small projections called villi. If you zoomed in even closer, you’d see tiny hairlike structures called microvilli protruding from the outer cell membrane of the epithelial cells; this membrane is often referred to as the brush border because it resembles a brush under a microscope (see Figure 1.6). Just like how bristles of a paintbrush provide a large surface area for applying paint to a wall, the villi and microvilli increase the surface area where absorption of nutrients occurs. Although some references put the surface area of the small intestine at 100 square meters, recent estimates are closer to 30 square meters,16 which is about the size of the standard American living room.
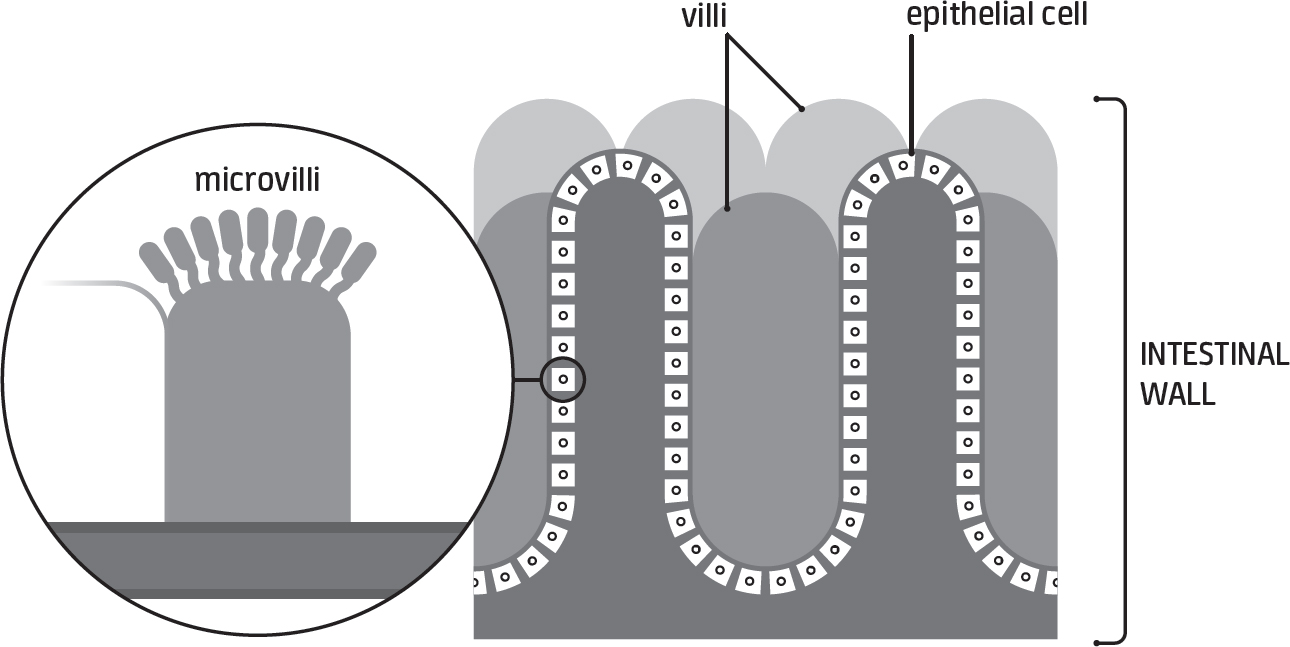
figure 1.6INTESTINAL VILLI AND MICROVILLI

These finger- and hairlike projections dramatically increase the area where absorption occurs in the small intestine.
After your pancreatic enzymes finish attacking carbohydrates, proteins, and fats, the remaining products of digestion still need to cross the cellular barrier that protects you from the nasty outside world. Products of protein digestion—amino acids and small peptides (two to three amino acids joined together)—pass through carriers located at the brush border, and the speed by which they’re absorbed depends on their structure and chemical properties. For example, branched-chain and essential amino acids (i.e., the type your body can’t make) tend to be absorbed more rapidly than nonessential amino acids.
Before carbohydrates are absorbed, enzymes at your brush border must first split any remaining longer-chain molecules into short chains of glucose or individual glucose molecules. Similarly, disaccharides such as sucrose (table sugar), lactose (milk sugar), and maltose (two glucoses bound together) are enzymatically split into single sugar molecules. The resulting single sugar molecules (glucose, fructose, galactose) are absorbed into your intestinal cells through protein-based transporters, the two most important being SGLT1 and GLUT5. These specific transporters are discussed more in Chapter 4, as they have important implications for how much carbohydrate you can tolerably ingest during exercise. Figure 1.7 presents a simplified overview of carbohydrate digestion.
In contrast to the absorption of carbohydrates and amino acids, fat absorption occurs mostly through simple diffusion. Small emulsified fat droplets made of fatty acids and monoglycerides are carried to the brush border, where they diffuse across the cell membrane, which is fat-soluble itself. Once inside your intestinal cells, fatty acids and monoglycerides get repackaged into triglycerides, and these triglycerides combine with other fat-soluble substances (e.g., cholesterol, fat-soluble vitamins) to form chylomicrons, which are conglomerations of protein, cholesterol, triglycerides, and phospholipids. Chylomicrons are then dumped out of your intestinal cells into your lymphatic system and join up with blood circulating in your chest.
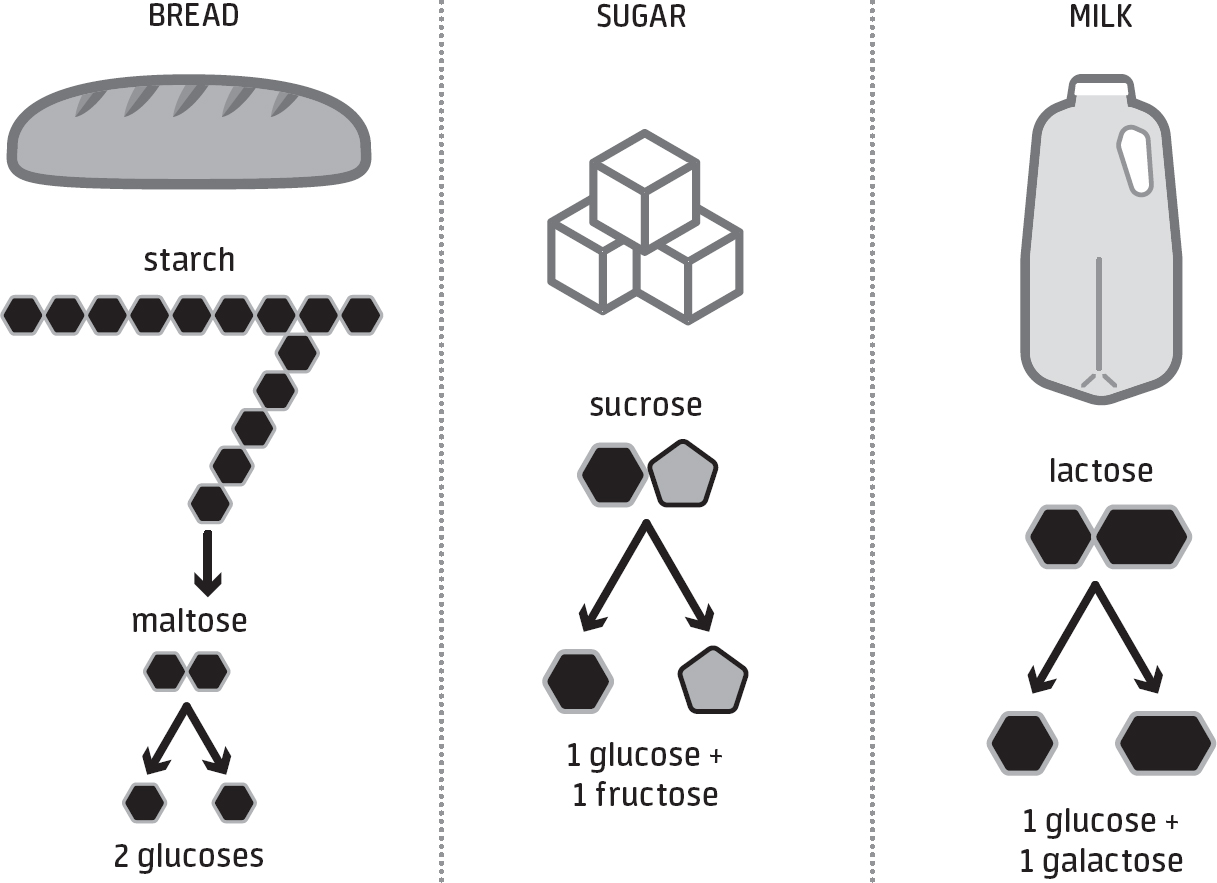
figure 1.7CARBOHYDRATE DIGESTION

In order to absorb carbohydrate, your body must break down chains of carbohydrate into single sugar molecules.
Vitamins and minerals are also readily absorbed in your small intestine, mostly via specialized carriers or transport systems. Your entire small bowel is capable of absorbing vitamins and minerals, but the highest rates of absorption occur in your duodenum and the first half of your jejunum. One notable exception is vitamin B12, which is primarily absorbed near the very end of your small intestine, in your distal ileum.19
A final essential nutrient that’s absorbed in your small intestine is water. Most couch potatoes living in temperate environments need to consume 2–3 liters of fluid per day to balance water losses from pooping, peeing, and sweating. In contrast, an athlete exercising for multiple hours in sweltering conditions may need to consume two to three times that amount to compensate for sweat loss. Clearly, your gut is part and parcel of maintaining hydration because of its role in absorbing water from the fluids and foods you eat. However, the volume of water you consume doesn’t actually represent the total water absorption load of your gut because you also secrete approximately 7 liters—or almost an entire case of beer’s worth—of fluid into your lumen each day. This fluid secretion occurs for digestive purposes (e.g., release of gastric and pancreatic juices) as well as to reduce the osmolality of any highly concentrated fluids that enter your intestines (as will be explained shortly). Instead of letting this secreted fluid pass through you as watery stool, your gut reabsorbs more than 95 percent of it—at least when it’s functioning normally. This recycling system is a favorable adaptation that dramatically reduces the amount of water you need to consume on a daily basis.
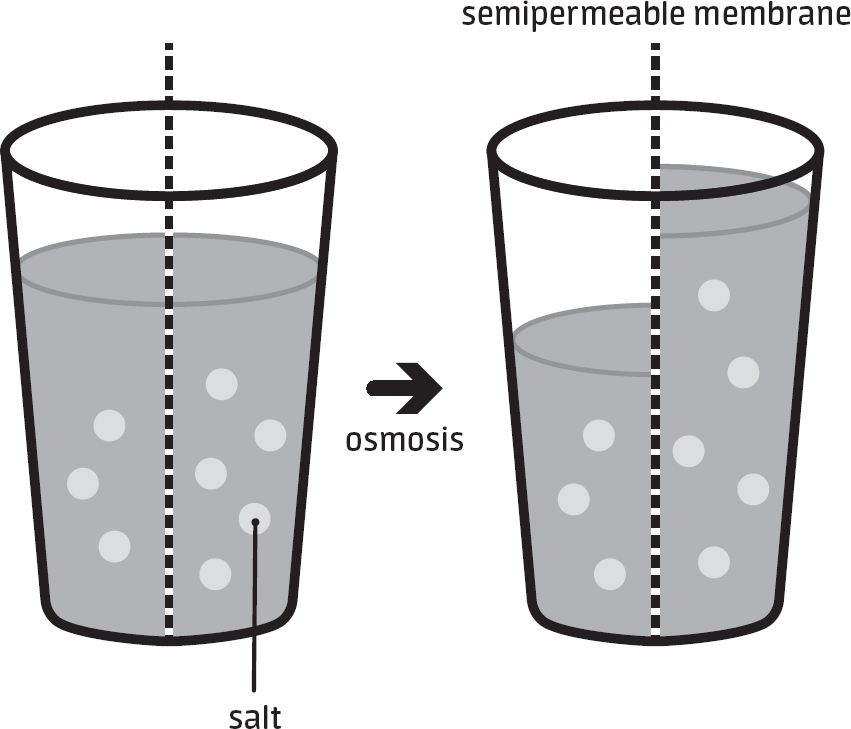
figure 1.8OSMOSIS

Fluid movement in and out of the gut is largely driven by the concentrations of solutes (sodium, sugar, etc.) in the lumen and in the body.
The bulk of water absorption—perhaps up to 80 percent—takes place in your small intestine20 and occurs via osmosis. If you slept through most of your science schooling as a youth, let me remind you how osmosis works. Osmosis means that water movement is based on the concentration of molecules on each side of a semipermeable membrane. Water passes from the side with a lower concentration to the side with a higher concentration of molecules, ultimately leading to an equilibration on both sides. (The technical jargon used to describe the concentration of molecules in a fluid is osmolality.) A simple experiment you can do to illustrate how osmosis works is to place two slices of a potato into separate dishes that contain different solutions: one with tap water and one with saltwater. After several hours, the slice in the saltwater should weigh less because water from the potato has moved into the saltwater solution. If you’re not a fan of home-based potato experiments, you can refer to Figure 1.8, which illustrates the process of osmosis.
What, you might be justifiably wondering, is the practical value of knowing this information? Ultimately, it means that chugging a beverage loaded with carbohydrate and/or electrolytes will cause a net movement of water from your blood into your small intestine lumen, which is the opposite direction of what you want when exercising. Beverages with osmolalities that are higher than your blood plasma are said to be hypertonic, and examples of these sorts of libations include apple juice, soft drinks, and pickle juice. With that in mind, avoiding extremely hypertonic beverages is a prudent choice when you want to optimize the speed of fluid absorption in your small intestine, as these hypertonic drinks cause an initial net movement of water into your small intestinal lumen and delay water absorption (see Figure 1.9).
It’s worth noting that beverage osmolality is most important to consider during exercise, as this is when the speed of hydration is critical. In other situations (throughout the day), there’s less need to worry about beverage osmolality because most of the water secreted into the first part of your small intestine eventually gets reabsorbed farther down in the intestinal tract.
If extremely hypertonic beverages aren’t the speediest hydration choice during exercise, then consuming hypotonic beverages (i.e., those well below the osmolality of blood plasma) like plain water must be, right? Although hypotonic beverages create a large osmotic gradient that drives water absorption, there’s actually an advantage to choosing a beverage with a bit more sodium and carbohydrate in it. For example, drinks that contain 10–25 grams of glucose and 1,000 milligrams of sodium per liter are slightly hypotonic (which creates an osmotic drive for water absorption), and as an added benefit, additional water is dragged along for the ride as the sodium and sugar in these beverages get absorbed. Unfortunately, plain water doesn’t benefit from this cotransport of water from sodium and glucose absorption, which is precisely why modern-day therapeutic rehydration solutions (e.g., Pedialyte, Hydralyte, Dioralyte) contain modest amounts of carbohydrate and sodium and are often formulated to have an osmolality that’s slightly below or right around blood levels.21
One thing to keep in mind is that, in contrast to these therapeutic rehydration solutions, sports beverages like Gatorade and Powerade are mildly hypertonic because they contain extra sugar (50–70 grams per liter) for fueling purposes. Even though fluid absorption may be optimal with carbohydrate concentrations of 10–25 grams per liter, it turns out that carbohydrate absorption and delivery to the muscle is increased at higher concentrations. In essence, sports beverages were designed to find the right balance between fluid and fuel delivery during prolonged exercise.
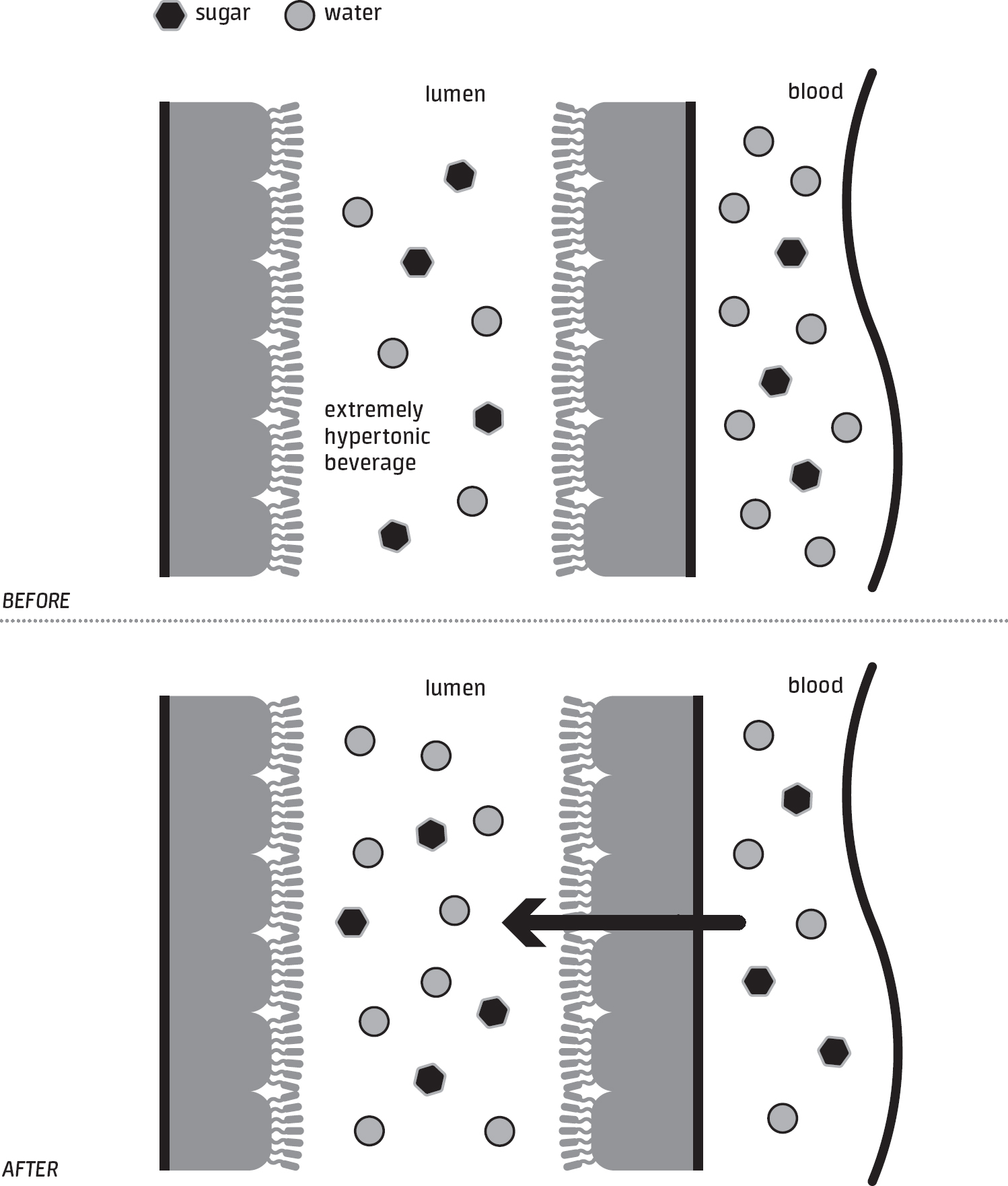
figure 1.9EFFECTS OF BEVERAGE OSMOLALITY ON FLUID MOVEMENT IN THE INTESTINES

A hypertonic beverage can cause fluid to move from your blood to your gut lumen, slowing the overall process of fluid absorption.
If all of this sounds a bit convoluted, it’s because the dynamics of fluid absorption are fairly complicated. In the end, one simple message you can take from all of this information is that, when you want to prioritize the speed of fluid absorption, beverages with osmolalities on the extreme ends of the spectrum (especially on the high end) are not the quickest to be absorbed. As with many things in life, the Goldilocks principle applies well to the concept of osmolality and fluid absorption.
Almost all of the nutrients absorbed in your small intestine pass into your capillary blood and are transported to your liver. (Long-chain fats are an exception because they must first enter your lymphatic system due to their insolubility in water.) Once in your bloodstream, these nutrients are channeled through various veins that merge to form your portal vein, which ultimately leads to your liver. This gives your liver, the body’s chemical processing plant, a first shot at metabolizing most nutrients, and it takes full advantage by extracting significant quantities of sugars, amino acids, and other nutrients. I like to think of the liver as the Paul Giamatti of the gut, a strong character actor who takes on a diverse set of roles. Whatever isn’t extracted by your Paul Giamatti (er, I mean liver) travels to other organs, such as your skeletal muscles, heart, and brain, where it can be used for the production of energy or other critical processes. As its journey through your small intestine ends, any unabsorbed chyme ends up at your ileocecal valve, a sphincter controlling passage into the shorter but wider segment of your bowels, the large intestine.
THE LARGE INTESTINE
The 0.5 to 2.5 liters of chyme reaching your large intestine each day is a mixture of undigested food residue, fiber, water, and electrolytes, and your 5-foot-long large intestine (also referred to as your colon) is responsible for downsizing that to 100 to 200 grams of stool,22 or, as it’s known in more colloquial language, poo. While 200 grams is on the high end of the daily poo production spectrum for Westerners, daily stool output is up to two times as much in some parts of the world.23 The differences in production, as you might expect, are primarily due to variances in the intake of fiber, a type of non-digestible carbohydrate.24
The primary method your large intestine relies on to turn chyme into fully formed fecal matter is the absorption of water and electrolytes. Although your small intestine is responsible for the lion’s share of water absorption, your large bowel is also an important player in this process and ultimately absorbs 90 percent of the fluid that passes into it.25 Like its smaller sibling, your large intestine absorbs water via osmosis. However, this big brother differs from the small intestine in a couple of ways: (1) the movement of chyme (or stool) is slower, and (2) it consists of saclike pouches that facilitate the absorption of water. Both features allow your large bowel to efficiently absorb water and make poo.
Apart from serving as a crap factory, your colon is home to an almost countless number of microscopic critters, especially bacteria. Your large intestine is essentially the jungle of your gut—everything grows there. In stark contrast, your stomach and small intestine are unwelcoming homes for the microorganisms present in the foods and beverages you eat. If your colon is a jungle, then the environment of your stomach is akin to the hostile conditions of a desert. “Growing conditions” are marginally better in your small intestine, but it’s still hard for most microorganisms to thrive there. The reason for this desertlike environment is that gastric acid, bile, and pancreatic secretions all function as antimicrobial agents. On top of that, food passes through these segments relatively expeditiously, limiting the amount of time available for microbes to take up residence there.
To put hard estimates on it, there are perhaps 40 trillion bacterial cells in the average man’s colon, vastly outnumbering the few million residing in said average man’s stomach.26 Even if you assume that some people have only half as many bacteria in their large intestine, their colonic bacteria will still far outnumber the bacteria living in any other part of their gut. Because there are so many bacteria in your colon, it means you have at least as many bacterial cells in your body as you have of your own cells. However, because microbial cells are only a fraction of the size of animal cells, the bacteria within the average human weigh only about half a pound despite their enormous numbers. (A commonly cited number is closer to 3 pounds, but that’s likely an overestimate.) These gut microorganisms—along with their genes and the metabolites they produce—are referred to collectively as the gut microbiome.
As recently as a few decades ago, most people—among the public, anyway—believed that nearly all bacteria were detrimental to health. However, there’s been a growing awareness that some of these microbugs keep our bodies in tip-top condition. In terms of the digestive process, colonic bacteria play an important role in breaking down foodstuffs that are otherwise indigestible by humans. Ultimately, foodstuffs that are invulnerable to your body’s attempts at digestion go unabsorbed in the small intestine and pass into the colon. At that point, certain species of bacteria metabolize some of these unabsorbed nutrients, the most prominent being fibers and other poorly digested carbohydrates.27 The end products of this metabolism of carbohydrates are gases (hydrogen, carbon dioxide, methane) and short-chain fatty acids (acetate, propionate, butyrate).
Interestingly, some of these short-chain fatty acids are absorbed in your gut and serve as fuel for your intestinal cells. There’s also mounting evidence that the types and amounts of short-chain fatty acids produced in the bowel are linked to health conditions such as obesity, celiac disease, colorectal cancer, and even brain disorders.28, 29 Specific to athletes, recent research suggests that exercise training may increase butyrate-producing bacteria,30 which are thought to promote gut health.
THE RECTUM AND ANUS
Technically, your rectum and anus are part of your large intestine, but they have functions that make them unique and noteworthy parts of your gut. Your rectum makes up the final inches of your colon, and its main function is to receive and briefly store stool before it exits your body forever. In contrast to the twisted nature of the rest of your intestines, your rectum is straight, which makes sense when you learn the word comes from the Latin intestinum rectum (“straight intestine”).
As stool or gas enters your rectum, receptors that are responsive to stretching get activated, and this sends signals to your brain that are ultimately interpreted as discomfort, an urge to defecate, or a need to let one rip. Nerve endings in your rectum and anus allow you to distinguish between solids, liquids, and gases, ensuring that you don’t soil your trousers when you simply intend to pass a little flatus. When you finally decide that it’s time to break wind (hopefully not in a crowded elevator) or do your duty, the opening of your anus allows stool and flatus to exit your body. The opening and closing of your anus is controlled by your anal sphincters, which, as a reminder, are rings of muscle that constrict and relax to control the flow substances (boluses, chyme, stool) between sections of your gut.31 You have internal anal sphincters that are controlled involuntarily by your autonomic nervous system, as well as external anal sphincters that are, to a large extent, under conscious control. Damage to the nerves that connect and communicate with these sphincters can lead to an inability to control one’s bowels.
THE ENTERIC NERVOUS SYSTEM
Your gut has a seemingly impossible job. Each day you consume several pounds of food containing an almost incalculable assortment of nutrients, nonnutrient molecules, and microorganisms—and if you trust a recent report, also thousands of bug bits from meal-worms, maggots, roaches, and the like.32 Not only is your gut responsible for identifying, digesting, and absorbing the nutrients you need to survive, but it’s also tasked with protecting your body from toxins and from being infected by the trillions of microorganisms that live in and pass through it day after day. The mucosal lining of your gut is the largest surface of your body exposed to the outside world, with an area that’s many times greater than your skin.33 The job of your gut is analogous to defending the Great Wall of China from hostile invaders while also allowing the flow of goods required to sustain an immense dynasty. This is no easy task.
Given the complex interface between your gut and the outside world, it shouldn’t be overly surprising to learn that your gut is home to one of the largest networks of nerve cells in your body. Although estimates vary, your gut houses somewhere between 100 million and 600 million neurons,33, 34 roughly equivalent to what you’d find in the brain of your pet dog or cat.35 Practically the entire length of your gut’s walls—from mouth to anus—is embedded with neurons, and this network of neurons is so vast that it’s often referred to as the body’s second brain (it’s also commonly called the enteric nervous system). This second brain is officially part of your autonomic nervous system, the branch of your peripheral nervous system that acts primarily on an unconscious level.
There are a couple of important things to know about how your second brain works. First, many of the actions your gut takes are controlled reflexively without instruction from your central nervous system (i.e., your brain and spinal cord).36 Other bodily reflexes—such as the muscle stretch reflex that your doctor tests by tapping below your kneecap—require signals to be sent to your spinal cord or brain before an appropriate action is taken. In contrast, sensory neurons within your gut are able to detect mechanical or chemical stimuli and reflexively cause an action—smooth muscle contraction, changes in blood flow, secretion of a substance—without ever communicating with your spinal cord or brain.
One prominent example of this type of intrinsic reflex is the control of peristalsis, the wavelike motion that propels boluses through your gut. Peristalsis begins with the stimulation of sensory neurons embedded in your gut, and this stimulation can occur through physical distension or through changes in the chemical environment of the lumen. These sensory neurons then communicate with motor (action) neurons housed entirely within your gut’s walls, causing smooth muscle to contract above and relax below a food bolus. This reflex was documented well over a century ago in experiments conducted by British physiologists William Bayliss and Ernest Starling, who showed that elevating pressure within the lumen of a dog’s intestine caused reproducible peristaltic contractions even when connections to nerves outside of the gut were severed.37 This isn’t to say that peristaltic movements are free of influence from extrinsic nerve activity (e.g., from the vagal nerve), as research has shown dual regulation through intrinsic and extrinsic nervous system control. Regardless, it’s clear that many of your gut’s actions aren’t wholly dependent on input from your central nervous system.22 So while your gut can’t learn a language or write poetry, it does seem to have a mind—albeit a primitive one—of its own.
Another interesting fact about your second brain is that it sends more signals to your central nervous system than it receives. Your brain and spinal cord are usually thought of as the command centers that run your entire nervous system, hence most of us assume that the flow of information tends to move in a downstream manner from the brain and spinal cord to the gut. On the contrary, much of this communication occurs in a bottom-up fashion, with up to 90 percent of the fibers in your vagal nerve sending information from your gut to your central nervous system.38 These messages include information about the overall activity of the gut and the presence of certain microbes, immune components, and chemicals, which may help the body respond to changes in the environment.
Intriguingly, studies in animals and humans show that these upstream messages impact mood and emotions.39, 40 In one innovative study, volunteers underwent several brain scans while being given either fatty acids or a placebo made of saline.40 Instead of having participants consume the treatments orally, the investigators shrewdly chose to infuse them directly into the participants’ stomachs so that they were unaware of what they were being given. This ensured that participants’ responses were due to gut-to-brain signaling and not from the taste, smell, or visual properties of the treatments. A few minutes after the investigators began infusing the treatments, they attempted to induce a sense of melancholy in the participants by showing them sad facial expressions and playing sad classical music. (If I had designed this study, I would have made them stare at photos of Kit Harington from Game of Thrones, who seems to always have resting sad face.) The study ultimately revealed that reductions in mood were less pronounced with fatty acid infusion, and these effects also showed up as blood flow changes in regions of the brain involved in mood regulation.
The take-home message of this research is that the composition of what a person eats can impact their mood and emotions, and these changes may be mediated by upstream messages traveling from the gut to the brain. While much is still to be learned about the interconnections between the gut, brain, and mood, it’s obvious that these links are bidirectional (both upstream and downstream) and that they are likely to have implications for our health and physical function.