
If you have PCOS, you are probably insulin resistant, especially if you are overweight. Additionally, you may have the insulin resistance syndrome, in which your insulin resistance interacts with other risk factors to increase your vulnerability to diabetes and heart disease. As mentioned in chapter 2, insulin resistance and the insulin resistance syndrome are two different things. The insulin resistance syndrome—referred to by the perhaps alarmingly familiar initials IRS—is also known as the metabolic syndrome and syndrome X. It can be defined as a cluster of abnormalities and clinical syndromes that are much more likely to occur in people who are insulin resistant. With IRS, such people, as well as being insulin resistant, usually have high blood pressure, a high triglyceride level, and a low HDL level.
Most women with PCOS are insulin resistant and have IRS. Because a woman with PCOS is so likely to be insulin resistant and consequently have a high insulin level, the American Association of Clinical Endocrinologists (AACE) recommends that all women with PCOS be evaluated for IRS. Unfortunately this is equivalent to saying that if you have PCOS, you may have a higher risk for heart disease and type 2 diabetes.
I’m not trying to alarm you, but I do want to encourage you to start treatment—including a weight management program— as soon as possible. Cosmetic and fertility problems can cause a lot of suffering, both emotional and physical, but they cannot make you ill or shorten your life span. Heart disease and diabetes can do just that.
In this chapter, we will look at what it means for a woman with PCOS to have IRS. In chapter 4, we will discuss the major health risks involved.
Doctors don’t all agree on criteria for diagnosing IRS. Some pare the criteria down to the bare essentials; others look for more signs. Taking the former approach, we can say that the following are the four essential criteria of IRS. Having any one, and certainly two, of them is strongly indicative of IRS.
• Triglyceride level of 150 mg/dL or higher
• HDL cholesterol level of less than 50 mg/dL in women (less than 40 in men)
• Blood pressure of 130/85 mmHg or higher
• Insulin resistance and increased tendency toward type 2 diabetes, as evidenced by:
(i) fasting glucose of 110-125 mg/dL
(ii) two-hour post-75-gram glucose challenge of 140 to 199 mg/dL (considered to be impaired glucose tolerance)
IRS is a huge health problem for all women, not only for those with PCOS. Your likelihood of having it increases with age:
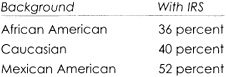
For Americans, ethnicity counts too:
Since it’s complicated for even the best professionals to accurately assess your insulin sensitivity, my advice is this: If you are twenty or more pounds overweight, you need to assume that you are likely to be insulin resistant and at risk for IRS. If you are of normal weight and know that you have PCOS, you need to make the same assumption and have a glucose tolerance test, blood lipid tests, and inflammatory marker tests (such as C-reactive protein).
Women with PCOS often have atherosclerosis-promoting blood lipid abnormalities, among them unhealthy triglyceride levels. Triglycerides, like cholesterol, are a lipoprotein, a combination of lipid and protein. These levels may be caused by insulin resistance or from genetic predisposition, ethnicity, obesity, or lifestyle. Having a high triglyceride level is characteristic of IRS. Your triglyceride level is measured, along with cholesterol levels, in a lab test on a blood sample that you give in a doctor’s office. Because your triglyceride level is highly responsive to food in-take, be careful to fast for ten to twelve hours before giving your blood sample.
Fat is stored in the body in the form of triglycerides. Having a high triglyceride level means that you have too many fat particles circulating in your bloodstream and presumably excess fat stored elsewhere in your body, including your liver.
Factors That Raise Your Triglyceride Level
Alcohol in excess
Beta blockers in high doses
Carbohydrate-abundant diet (more than 60 percent of calories)
Corticosteroids
Estrogen
Genetic lipid abnormalities
Nephrotic syndrome
Overweight or obesity
Physical inactivity
Renal failure, chronic
Smoking
Type 2 diabetes
People with IRS who have a high triglyceride level are particularly vulnerable to cardiovascular disease, as are people with a low HDL cholesterol (”good” cholesterol) level. As you already know, a triglyceride/HDL ratio of more than 3 is an indicator that you are insulin resistant and likely to have IRS. These two independent cardiac risk factors, together in IRS, accelerate the atherosclerosis process. These two risk factors can work with a third—small, dense LDL cholesterol particles—to create an even greater threat to the heart. Add to all this the elevating effect that obesity has on the triglyceride levels of women with PCOS and you start to understand how anxious I am about getting my patients on a sustainable weight loss program immediately.
If your triglyceride level is too high, how can you lower it? Of all the blood lipid levels, your triglyceride level is the most responsive to lifestyle changes. Eat food that is more healthful, lose a few pounds, and exercise or at least be more active and your triglyceride level will probably drop. If you’re serious about these lifestyle changes and stick with them, you may not need drugs to reach and maintain a healthy triglyceride level.
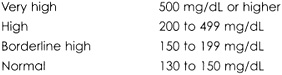
• A very high triglyceride level (500 mg/dL or more) requires immediate treatment because of the health threat to your pancreas. You need to eat a very low-fat diet (15 percent or fewer calories from fats), lose weight, exercise, and usually take a fibrate (Tricor) or nicotinic acid.
• A high triglyceride level (200 to 499) usually responds to any diet that lowers LDL cholesterol, along with weight loss and exercise.
• A moderately high triglyceride level (150 to 199) is usually lowered by weight loss and increased physical activity.
Lowering your LDL cholesterol level is the most effective way to bring down your triglyceride level. If your triglyceride level does not respond to lifestyle changes, ask your doctor about medications. Try lifestyle changes first.
The problem with lowering your low density lipoprotein (LDL or “bad”) cholesterol level is that doing so can also lower your high density lipoprotein (HDL or “good”) level. If your HDL is already at a low or borderline low level, this is a valid health concern. It can happen when you reduce the fats in your diet and replace them with carbohydrates, without also reducing your calorie intake. This kind of diet change can lower your HDL level by as much as one-fifth.
Factors That Lower Your HDL Level
Anabolic steroids used by athletes
Beta-blockers
Carbohydrate-abundant diet (more than 60 percent of calories)
Excess weight
Physical inactivity
Fertility drugs
Smoking
High triglyceride level
Type 2 diabetes
Researchers first paid major attention to HDL levels in the Framingham Heart Study. They saw that among study participants with the same LDL level, those with higher HDL levels were less likely to develop cardiovascular disease than those with lower HDL levels. LDL particles, with white blood cells and cellular debris, help build plaque in artery walls. HDL particles help remove such LDL particles from the blood by carrying them to the liver, where they are broken down. You can think of your HDL as functioning like a predator that helps keep the vermin count under control. More specifically, HDL carries antioxidants that probably combat LDL oxidation in plaque buildup.
Women with PCOS, of an average age of only twenty-six, were found to have more of their LDL cholesterol in the form of small dense particles than similar women without PCOS. LDL as small dense particles is regarded as its most dangerous form. Women with PCOS have higher levels of LDL than women without PCOS, independent of weight. They have higher LDL and lower HDL levels than similar women without PCOS up to about the age of forty-five, while after that age, both groups have similar levels. The early prolonged exposure of women with PCOS to unhealthy blood lipid levels presumably leads to cardiovascular problems.
Cardiovascular Risk and Cholesterol Level
(from the National Cholesterol Education Program)
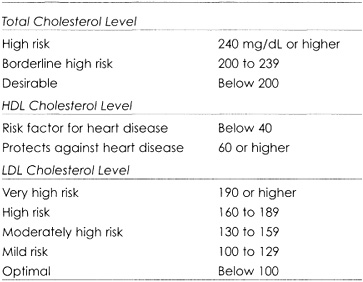
The third edition of the National Cholesterol Education Program (NCEP)’s guidelines suggests two main cardiovascular disease prevention strategies:
1. If you are healthy, you can help prevent cardiovascular disease by reducing your intake of saturated fats and cholesterol, increasing your physical activity, and controlling your weight.
2. If you already have cardiovascular disease, you can help prevent further problems by keeping your LDL cholesterol level below 100.
It’s debatable which category you fit in if you have PCOS and IRS, and have never had a cardiac event. I suggest that you play it safe by keeping your HDL well above 50 and your LDL between 80 and 100.
Later recommendations from the National Cholesterol Education Program suggest that people at very high risk for cardiovascular disease should aim for an LDL level below 70, and high-risk people who have high triglyceride or low HDL levels should consider combining a fibrate or niacin with their LDL-lowering drug.
Your heart beats about 100,000 times a day, pumping blood through the 60,000 miles or so of blood vessels in your circulatory system. Each time your heart beats, it builds the pressure needed to drive the blood through the intricate network of vessels. When your blood pressure becomes too high, you have an increased risk for heart disease and stroke. Even moderate rises in pressure greatly increase the risk. For example, in people forty to seventy years old, each 20/10 mmHg rise in blood pressure doubles the risk. The first number of your blood pressure reading is your systolic pressure, measured as your heart contracts, driving blood into your arteries. The second number is your diastolic pressure, measured as your heart relaxes.
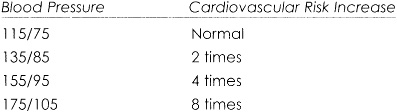
As women with PCOS reach age forty-five, they have a higher incidence of high blood pressure (hypertension) than women without PCOS. Typically, women with PCOS have increased daytime systolic pressure. Elevated blood pressure has also been associated with high insulin levels, regardless of weight.
High blood pressure can cause turbulent blood flow. This turbulence can affect the delicate cells of artery wall linings in the same way that turbulent water damages riverbanks. An injury site on an artery wall attracts white blood cells and clotting factors—the beginning of plaque buildup.
High blood pressure can threaten your cardiovascular health in more complex ways and can interact with other cardiac risk factors. For example, cigarette smoking and high blood pressure are a well known high-risk combination of cardiac risk factors. This combination is even more deadly in people with abnormal lipid levels and among women on oral contraceptives. High blood pressure is also often responsible for worsening diabetic complications, including kidney abnormalities through reduction in blood flow.
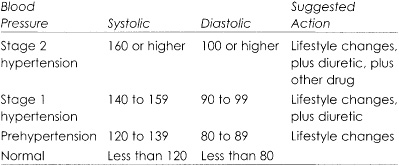
Less than half of the 50 million Americans who have high blood pressure have it under control. It seems only half the people on prescription medications for high blood pressure actually take them regularly. To make some changes for the better, the National High Blood Pressure Education Program (NHBPEP) suggests that people starting drug therapy begin with a low-cost diuretic, such as hydrochlorthiazide, instead of a more expensive medication. The program also encourages a renaming of the upper “normal” range of blood pressure to prehypertension, in order to serve as a warning. Additionally, you need to be aware that some over-the-counter and prescription medications for other complaints (for example, decongestants) can increase your blood pressure. Ask your doctor for details if you take them.
The lifestyle changes needed to lower your blood pressure usually involve weight loss, more exercise, a low-fat diet including more vegetables and fruit, markedly reduced salt intake, no smoking, and no more than moderate alcohol intake.
Salt helps raise blood pressure. Someone with normal blood pressure should not eat more than about 2,400 milligrams of sodium a day (about a heaping teaspoon of salt). Most Americans eat about 4,000 milligrams of sodium a day (about two teaspoons of salt), most of it from processed foods and restaurant meals. That’s almost double the recommended intake. Among my patients, those who try not to eat any salt bring their actual intake down to a healthy level—it’s hard to eliminate salt completely! Salt is, of course, essential to good health, even when you have high blood pressure, but most of us indulge in too much of this good thing.
SEVEN SUGGESTIONS FOR HIGH BLOOD PRESSURE
1. If you need to, lose some weight.
2. Be active at least half an hour every day.
3. Eat heart-healthy food.
4. Have no more than one alcoholic drink a day.
5. Quit smoking now.
6. Try to manage things that cause you stress.
7. Ask your doctor if any of your medications (decongestants and so forth) might be increasing your blood pressure.
Blood lipid levels and high blood pressure are serious health risk factors that combine with insulin resistance in IRS. Jointly they present a bigger health threat than one of them acting alone. How PCOS interacts with them to further increase the risk of diabetes and heart disease is not fully understood, but we do know they’re related. Type 2 diabetes commonly makes the health situation of women with PCOS and IRS even more precarious, because diabetes also interacts with other symptoms and health risks. Impaired glucose tolerance, an intermediate step toward type 2 diabetes, interacts with similar consequences (more on this in the next chapter).
Women with PCOS who understand the real importance of IRS know that as well as combating infertility and hair or skin symptoms, it’s essential they take action to protect themselves from diabetes and heart disease. In the next chapter we will look at the major health threats to women with PCOS.