In 2006, Merck introduced a remarkable vaccine that prevented several types of human papillomavirus (HPV), which are responsible for causing 70 percent of cervical cancers and 90 percent of genital warts. Both are transmitted by sexual intercourse. The vaccine is not effective in treating these conditions but can prevent them when given in three injections over a six-month period. Hence, the manufacturer and governmental health agencies in the United States and Europe recommended that the vaccine be administered before adolescence, to girls as young as nine years of age, before they potentially become sexually active, and until twenty-six years of age. In 2009, approval was also given to market the vaccine for use in males aged nine years and over.
The vaccine’s launch was initially accompanied by an apparent groundswell of political, medical, and public support, not only for its use but also for its mandatory administration in all eleven- and twelve-year-old girls as a condition for attending school. Texas governor Rick Perry was in the forefront of these discussions and, by executive order, in 2007 mandated vaccinations, bypassing the legislature. Months later, this action was overturned by his state legislature. In an effort to get state legislatures to pass such laws nationwide, Merck surreptitiously funded efforts by female state legislators but quickly terminated support after its involvement was disclosed.
GOOD MEDICINE, BAD POLITICS. Objections to mandatory vaccinations were soon voiced based on moral, political, financial, and health concerns. Socially conservative groups argued that the vaccine might encourage sexual activity in adolescent girls, who might think themselves now protected against sexually transmitted diseases. Some groups were opposed to all governmental mandates and interventions, regardless of how well intentioned. The series of shots cost around $360. Coverage by insurance companies is variable, and for many individuals, the out-of-pocket expense prohibitive.
Yet to be fully resolved are potential safety concerns associated with the vaccine and how long HPV protection lasts. Adverse reaction data and deaths have been subject to repeated analysis, and governmental health agencies in Europe and the United States have continued to conclude that Gardasil’s health benefits outweigh any possible risks.
SEE ALSO Smallpox Vaccine (1796), Polio Vaccine (1954).
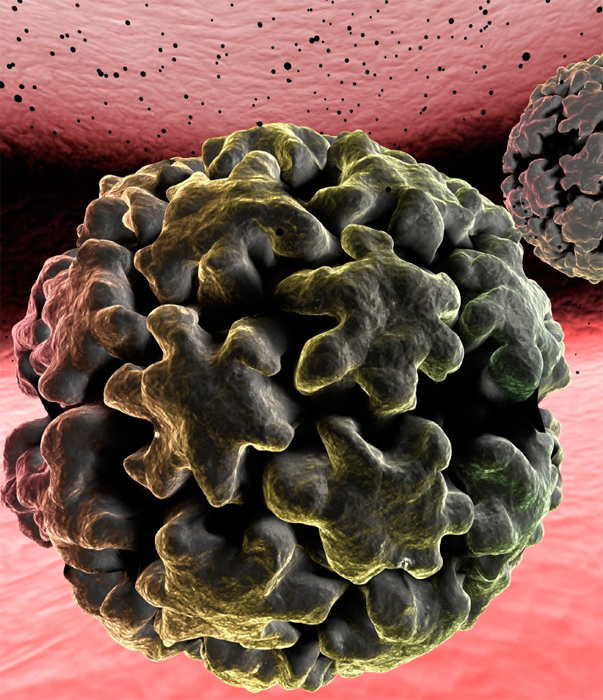
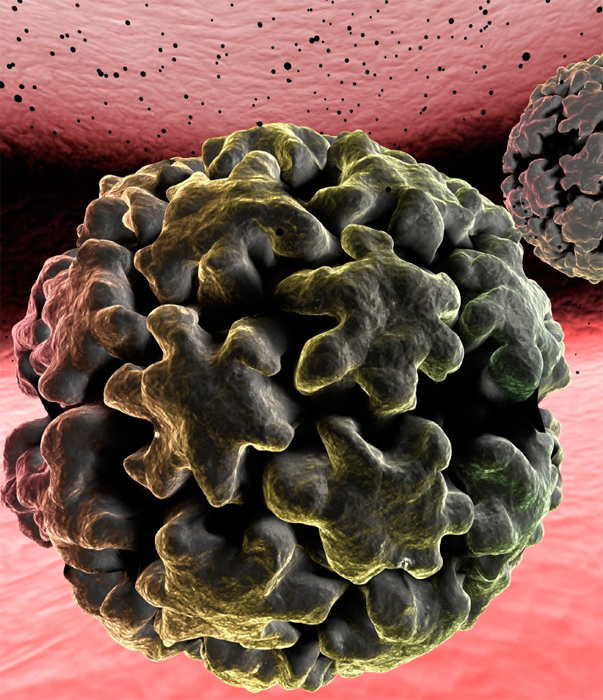
Out of the 150 to 200 types of HPV (pictured), 30 to 40 are transmitted through sexual contact, affecting about 80 percent of sexually active individuals. Most infections are temporary and cause no symptoms. In 5 to 10 percent of women, the infection persists and can progress to invasive cervical cancer over a 15- to 20-year period. Since the introduction of the Pap test in the 1940s, in which women are regularly screened, the death rate from cervical cancer has been reduced by 99 percent.