Answers and Explanations
Practice Test
- The Answer is 3
The LPN/LVN is gathering data from a client who is receiving treatment for obsessive-compulsive disorder (OCD). Which of the following is the most important question the LPN/LVN should ask this client?
Reworded Question: What are the signs and symptoms of obsessive-compulsive disorder?
Strategy: “Most important” indicates there may be more than one correct response.
Needed Info: Obsessive-compulsive disorder is characterized by a history of obsessions and compulsions. Obsessions are recurrent and persistent thoughts, ideas, impulses, or images that are experienced as intrusive and senseless. The client may know that the thoughts are ridiculous or morbid but cannot stop, forget, or control them. Compulsions are repetitive behaviors performed in a certain way to prevent discomfort and neutralize anxiety.
Category: Data Collection/Psychosocial Integrity
- “Do you find yourself forgetting simple things?”—should be used to collect data for a client with suspected cognitive disorder
- “Do you find it difficult to focus on a given task?”—collects data for disorders that disrupt the ability to concentrate, such as depression
- “Do you have trouble controlling upsetting thoughts?”—CORRECT: one feature of obsessive-compulsive disorder is the client’s inability to control intrusive thoughts that repeat over and over
- “Do you experience feelings of panic in a closed area?”—appropriate for client with suspected panic disorder related to closed spaces or claustrophobia
- The Answer is 1
The LPN/LVN is caring for a client who states, “I just want to die.” The LPN/LVN should examine the client’s medical record for which of the following documents?
Reworded Question: What data does the LPN/LVN need to know?
Strategy: Determine the document that would address a client’s choice to die.
Needed Info: Advance directives: specific instructions by the client that are legally binding. Clients with advance directives must provide them in written form to the health care provider. Advance directives include the “do not resuscitate” instruction, living will, durable power of attorney/health care surrogate.
Category: Data Collection/Safe and Effective Care Environment/Coordinated Care
- Advance directives—CORRECT: advance directives specify the client’s wishes regarding health care decisions
- Power of attorney—surrogate or proxy if the client is incompetent to make decisions
- “Do not resuscitate” order—only one part of advance directives
- Living will—only one part of advance directives
- The Answer is 4
A newly admitted client with a history of seizures suddenly says to the LPN/LVN, “I hear drums.” Which of the following should the LPN/LVN do first?
Reworded Question: What does a sudden visual, olfactory, or auditory sensation often signal in a client with a history of seizures?
Strategy: Quickly review the most likely causes of the client’s unusual perception.
Needed Info: Aura: brief sensory alteration often preceding seizure or migraine, likely for client with history of seizures. Petit mal seizures: usually occur in children, not associated with an aura. Grand mal seizures: involve loss of consciousness and convulsions.
Category: Evaluation/Physiological Integrity/Physiological Adaptation
- Tell the client to ignore the drums—client is experiencing an auditory sensation that may signal the start of a seizure
- Place the client in a darkened room away from the nurses’ station—the client needs continued observation
- Continue to question the client—many adult clients experience unusual sensory perceptions (an aura) before the onset of a seizure; this client has a history of seizures
- Insert an oral airway in the client—CORRECT: an oral airway prevents the client from biting cheek or tongue during a seizure
- The Answer is 2
A client diagnosed with multiple myeloma is admitted to the unit after developing pneumonia. When the LPN/LVN enters the client’s room wearing a mask, the client says in an irritated tone of voice, “Why are you wearing that mask?” Which of the following responses by the LPN/LVN is best?
Reworded Question: What is the most therapeutic response?
Strategy: Remember therapeutic communication.
Needed Info: Multiple myeloma: a neoplastic disease that infiltrates bone and bone marrow, causes anemia, renal lesions, and high globulin levels in blood; pneumonia is inflammatory process resulting in edema of lung tissue and extravasion of fluid into alveoli, causing hypoxia.
Category: Data Collection/Safe and Effective Care Environment/Safety and Infection Control
- “The chest x-ray taken this morning indicates you have pneumonia.”—does not help determine what client knows; primary health care provider is responsible for telling client the medical diagnosis
- “What have you been told about the x-rays that were taken this morning?”—CORRECT: data collection; determines what client knows before responding; allows client to verbalize
- “You have been placed on contact precautions due to your infection.”—certain types of pneumonia require droplet precautions
- “I am trying to protect you from the germs in the hospital.”—certain types of pneumonia require droplet precautions
- The Answer is 1
A nursing team consists of an RN, an LPN/LVN, and a unlicensed assistive personel (UAP). The LPN/LVN should be assigned to which of the following clients?
Reworded Question: Which client is an appropriate assignment for the LPN/LVN?
Strategy: Think about the skill level involved in each client’s care.
Needed Info: LPN/LVN: assists with implementation of care; performs procedures; differentiates normal from abnormal; cares for stable clients with predictable conditions; has knowledge of asepsis and dressing changes; administers medications (varies with educational background and state nurse practice act).
Category: Planning/Safe and Effective Care Environment/Coordinated Care
- A client with a diabetic ulcer that requires a dressing change—CORRECT: stable client with an expected outcome
- A client with cancer who is reporting bone pain—requires assessment; RN is the appropriate caregiver
- A client with terminal cancer being transferred to hospice home care—requires nursing judgment; RN is the appropriate caregiver
- A client with a fracture of the right leg who asks to use the urinal—standard unchanging procedure; would be assigned to the UAP
- The Answer is 1
To determine the structural relationship of one hospital department with another, the LPN/LVN should consult which of the following?
Reworded Question: How does the LPN/LVN determine the relationship of one hospital department to another?
Strategy: Think about each answer.
Needed Info: The lateral lines on an organizational chart define the division and specializations of labor; the vertical lines explain the lines of authority and responsibility.
Category: Implementation/Safe and Effective Care/Coordinated Care
- Organizational chart—CORRECT: delineates the overall organization structure, showing which departments exist and their relationships with one another both laterally and vertically
- Job descriptions—focus is not on departmental relationships
- Personnel policies—defines policies for the organization’s employees
- Procedures manual—defines standards of care for an institution
- The Answer is 3
A client reports pain in the right lower extremity. The primary health care provider prescribes codeine 60 mg and aspirin grains X PO every 4 hours, as needed for pain. Each codeine tablet contains 15 mg of codeine. Each aspirin tablet contains 325 mg of aspirin. Which of the following should the LPN/LVN administer?
Reworded Question: What amount of medication should you give?
Strategy: Remember how to calculate dosages.
Needed Info: 60 mg = 1 grain.
Category: Implementation/Physiological Integrity/Pharmacological Therapies
- 2 codeine tablets and 4 aspirin tablets—inaccurate
- 4 codeine tablets and 3 aspirin tablets—inaccurate
- 4 codeine tablets and 2 aspirin tablets—CORRECT: 60/x = 15/1, x = 4; 10 grains = 600 mg; 325/1 = 600/x, x = 1.8 (round to 2)
- 3 codeine tablets and 3 aspirin tablets—inaccurate
- The Answer is 2
The LPN/LVN is caring for a client receiving paroxetine. It is most important for the LPN/LVN to report which of the following to the physician?
Reworded Question: What is a potential drug interaction?
Strategy: “Most important” indicates priority.
Needed Info: Paroxetine (Paxil) is a selective serotonin reuptake inhibitor (SSRI) used to treat depression, panic disorder, obsessive-compulsive disorder; side effects include palpitations, bradycardia, nausea and vomiting, and decreased appetite.
Category: Evaluation/Physiological Integrity/Pharmacological Therapies
- The client reports no appetite change—causes anorexia; monitor weight and nutritional intake; report continued weight loss
- The client reports recently being started on digoxin—CORRECT: may decrease effectiveness of digoxin
- The client reports applying sunscreen to go outdoors—appropriate action; prevents photosensitivity reactions
- The client reports driving the car to work—driving is acceptable after determining client’s response to drug
- The Answer is 2
A client with a “do not resuscitate” order experiences a cardiac arrest. Which of the following is the first action the LPN/LVN should take?
Reworded Question: What actions are appropriate for a client with a do not reus order who has no heartbeat?
Strategy: Determine which actions meet DNR standards.
Needed Info: “Do not resuscitate” requires a written primary health care provider order in the medical record: no extraordinary care given in the event of the client’s death. Extraordinary care after cardiac or pulmonary cessation: cardiopulmonary resuscitation (CPR), medications, ventilators, defibrillation.
Category: Data Collection/Safe and Effective Care Environment/Coordinated Care
- Administer lifesaving medications—"Do not resuscitate" means these medications are not given
- Assess the client for signs of death—CORRECT: client has signs of death and requires further data collection to confirm death
- Open the airway and give 2 breaths—CPR should not be initiated for clients with a “do not resuscitate” order
- Summon the emergency code team—CPR should not be initiated for clients with a “do not resuscitate” order
- The Answer is 1
An LPN/LVN is working in the newborn nursery. Which of the following client-care assignments should the LPN/LVN question?
Reworded Question: Which infant is outside the scope of practice for an LPN/LVN?
Strategy: Remember the ABCs (airway, breathing, circulation).
Needed Info: Need to meet client’s needs. Physical stability of client is LPN/LVN’s first concern. Most unstable client should be cared for by RN.
Category: Evaluation/Safe and Effective Care Environment/Coordinated Care
- A 2-day-old client lying quietly alert with a heart rate of 185 beats/minute—CORRECT: client has tachycardia; normal resting rate is 120–160 beats/minute; requires further investigation
- A 1-day-old client who is crying and has a bulging anterior fontanel—crying causes increased intracranial pressure, which normally causes fontanel to bulge
- A 12-hour-old client whose respirations are 45 breaths/minute and irregular while being held—normal respiratory rate is 30–60 breaths/minute with apneic episodes
- A 5-hour-old client whose hands and feet appear blue bilaterally while sleeping—acrocyanosis normally occurs for 2–6 hours after delivery due to poor peripheral circulation
- The Answer is 3
The LPN/LVN is inserting a nasogastric (NG) tube. The LPN/LVN should use which of the following personal protective equipment during NG tube insertion?
Reworded Question: What is the correct standard precaution?
Strategy: Think about each answer choice. How does each piece of equipment protect the LPN/LVN?
Needed Info: Mask, eye protection, and face shield protect against mucous membrane exposure; used if activities are likely to generate splashes or sprays. Gowns used if activities are likely to generate splashes or sprays.
Category: Planning/Safe and Effective Care Environment/Safety and Infection Control
- Gloves, gown, goggles, and surgical cap—surgical caps offer protection to hair but aren’t required
- Sterile gloves, mask, and gown—sterile gloves are used to protect the client during sterile procedures
- Gloves, gown, mask, and goggles—CORRECT: must use standard precautions on all clients; prevent skin and mucous membrane exposure when contact with blood or other body fluids is anticipated
- Double gloves, goggles, mask, and surgical cap—surgical cap not required for standard precautions; unnecessary to double glove
- The Answer is 2
The LPN/LVN is caring for clients in the outpatient clinic. Which of the following clients should the LPN/LVN see first?
Reworded Question: Who is the priority client?
Strategy: Think ABCs.
Needed Info: Need to meet client’s needs. Physical stability is LPN/LVN’s first concern. Client with most serious problem should be seen first.
Category: Planning/Safe and Effective Care Environment/Coordinated Care
- A client with hepatitis A who states, “My arms and legs are itching.”—caused by accumulation of bile salts under the skin; treat with calamine lotion and antihistamines
- A client with a cast on the right leg who states, “I have a funny feeling in my right leg.”—CORRECT: may indicate neurovascular compromise; requires immediate data collection
- A client with osteomyelitis of the spine who states, “I am so nauseous that I can’t eat.”—requires follow-up, but not highest priority
- A client with rheumatoid arthritis who states, “I am having trouble sleeping.”—requires data collection, but not a priority
- The Answer is 4
Which of the following client assignments should an LPN/LVN question?
Reworded Question: Which client is an inappropriate assignment for an LPN/LVN?
Strategy: Think about the skill level involved in each client’s care.
Needed Info: Determine nursing care required to meet clients’ needs; take into account time required, complexity of activities, acuity of client, and infection control issues. Consider knowledge and abilities of staff members and decide which staff person is best able to provide care.
Category: Planning/Safe and Effective Care Environment/Coordinated Care
- A client with a chest tube who is ambulating in the hallway—LPN/LVN can care for client
- A client with a colostomy who requires colostomy irrigation assistance—LPN/LVN can care for client
- A client with a right-sided stroke who requires assistance with bathing—LPN/LVN can care for client
- A client who is refusing medication to treat cancer of the colon—CORRECT: requires the assessment skills of the RN
- The Answer is 3
The LPN/LVN is caring for a client with hepatitis B. The client is to be discharged the next day. The LPN/LVN would be most concerned if the client made which of the following statements?
Reworded Question: What is an incorrect statement about care with hepatitis B?
Strategy: “Most concerned” indicates you are looking for an incorrect statement.
Needed Info: Hepatitis A (HAV): high-risk groups include young children, institutions for custodial care, international travelers; fecal/oral transmission, poor sanitation; nursing considerations include prevention, improved sanitation, treat with gammaglobulin early postexposure, no preparation of food. Hepatitis B (HBV): high-risk groups include drug addicts, fetuses from infected mothers, homosexually active men, transfusions, health care workers; transmission by parenteral, sexual contact, blood/body fluids; nursing considerations include hepatitis vaccine, immune globulin (HBIG) postexposure, chronic carriers (potential for chronicity 5–10%). Hepatitis C (HVC): high-risk groups include transfusions, international travelers; transmission by blood/body fluids; nursing considerations include great potential for chronicity. Delta hepatitis: high-risk groups same as for HBV; transmission coinfects with HBV, close personal contact.
Category: Evaluation/Safe and Effective Care Environment/Coordinated Care
- “I must not share eating utensils with my family members.”—prevents transmission; handwashing before eating and after toileting very important
- “I must use my own bath towel.”—prevents transmission; don’t share bed linens
- “I’m glad that I can have intimate relations with my partner.”—CORRECT: avoid sexual contact until serologic indicators return to normal
- “I must eat small, frequent meals.”—easier to tolerate than three standard meals; diet should be high in carbohydrates and calories
- The Answer is 2
The LPN/LVN is carrying out the plan for care of a client with anemia who reports weakness. Which of the following tasks could be assigned to the unliscened assistive personnel (UAP)?
Reworded Question: What is an appropriate assignment for the UAP?
Strategy: Think about the skill level involved in each task.
Needed Info: Unlicensed assistive personnel (UAPs): assist with direct client care activities (bathing, transferring, ambulating, feeding, toileting, obtaining vital signs/height/weight/intake/output, housekeeping, transporting, stocking supplies); includes nurse aides, assistants, technicians, orderlies, nurse extenders; scope of nursing practice is limited.
Category: Evaluation/Safe and Effective Care Environment/Coordinated Care
- Auscultate the client’s breath sounds—requires data collection; could be performed by LPN/LVN and reported to RN
- Set up the client’s lunch tray—CORRECT: standard, unchanging procedure; decreases cardiac workload
- Obtain client's dietary history—involves data collection; could be performed by LPN/LVN and reported to RN
- Instruct client how to balance rest and activity—instruction required; could be performed by LPN/LVN following established plan of care
- The Answer is 4
The LPN/LVN on the surgical floor is receiving hand-off report from the RN. Which of the following clients should the LPN/LVN see first?
Reworded Question: Which client is the least stable?
Strategy: Think ABCs.
Needed Info: Need to meet the client’s needs. Physical stability is the LPN/LVN’s first concern. Most unstable client should be seen first.
Category: Planning/Safe and Effective Care Environment/Coordinated Care
- A client admitted 3 days ago with a gunshot wound; 1.5-cm area of dark drainage noted on the dressing—does not indicate acute bleeding; small amount of blood
- A client who had a mastectomy 2 days ago; 23 mL of serosanguinous fluid noted in the wound drain—expected outcome
- A client with a collapsed lung due to an accident; no drainage noted in the previous 8 hours—indicates resolution
- A client who had an abdominal-perineal resection 3 days ago; client now reports chills—CORRECT: at risk for peritonitis; should be assessed by the RN for further symptoms of infection
- The Answer is 2
A client scheduled for a cardiac catheterization says to the LPN/LVN, “I know you were in here when I signed the consent form for the test. I thought I understood everything, but now I’m not so sure.” Which of the following responses by the LPN/LVN is best?
Reworded Question: Which response is most therapeutic?
Strategy: “Best” indicates that discrimination is required to answer the question.
Needed Info: Informed consent is obtained by the individual who will perform the test; explanation of the test and expected results, anticipated risks and discomforts, potential benefits, possible alternatives are discussed; consent can be withdrawn at any time.
Category: Evaluation/Safe and Effective Care Environment/Coordinated Care
- “Why didn’t you listen more closely to the explanation?”—“why” questions are nontherapeutic; does not respond to the client’s feelings or concerns
- “You sound as if you would like to ask more questions.”—CORRECT: directly responds to client’s statement by paraphrasing; implies encouragement of expression of client’s concern
- “I’ll get you a pamphlet about cardiac catheterization.”—may be helpful, but first the nurse needs to clarify the client’s concerns through discussion
- “That often happens during explanation of this procedure.”—does convey acceptance and lets the client know that the response is not abnormal; response is closed and does not allow client to express feelings or concerns
- The Answer is 2
A 1-day-old client diagnosed with intrauterine growth retardation has a high-pitched shrill cry and appears restless and irritable. The LPN/LVN also observes fist-sucking behavior. Based on this data, which of the following actions should the LPN/LVN take first?
Reworded Question: What do you do for a newborn client experiencing withdrawal?
Strategy: Determine the outcome of each answer.
Needed Info: Drug withdrawal may manifest from as early as 12 hours after birth up to 10 days after delivery. Symptoms: high-pitched cry, hyperreflexia, decreased sleep, diaphoresis, tachypnea, excessive mucus, vomiting, uncoordinated sucking. Nursing care: assess muscle tone, irritability, vital signs; administer phenobarbital as ordered; report symptoms of respiratory distress; reduce stimulation; provide adequate nutrition/fluids; monitor mother and newborn interactions.
Category: Implementation/Health Promotion and Maintenance
- Gently massage the client's back every 2 hours—may result in overstimulation of the client
- Tightly swaddle the client in a flexed position—CORRECT: promotes client’s comfort and security
- Schedule feeding times every 3 to 4 hours—small, frequent feedings are preferable
- Encourage eye contact with the client during feedings—may result in overstimulation of client
- The Answer is 2
The LPN/LVN visits a neighbor who is at 20 weeks’ gestation. The neighbor reports nausea, headache, and blurred vision. The LPN/LVN notes that the neighbor has tremors and appears nervous and diaphoretic. It would be most important for the LPN/LVN to ask which of the following questions?
Reworded Question: What is the priority data collection question?
Strategy: “Most important” indicates there may be more than one correct response.
Needed Info: Data collection: irritability, confusion, tremors, blurring of vision, coma, seizures, hypotension, tachycardia, skin cool and clammy, diaphoresis. Plan/implementation: liquids containing sugar if conscious, skim milk is ideal if tolerated; dextrose 50% IV if unconscious, glucagon; follow with additional carbohydrate in 15 minutes; determine and treat cause; client education; exercise regimen.
Category: Data Collection/Health Promotion and Maintenance
- “Are you having menstrual-like cramps?”—symptoms of preterm labor
- “When did you last eat or drink?”—CORRECT: classic symptoms of hypoglycemia; offer carbohydrate
- “Have you been diagnosed with diabetes?”—need to determine if she is hypoglycemic
- “Have you been lying on the couch?”—not relevant to hypoglycemia
- The Answer is 4
The LPN/LVN notes that a client newly admitted to the pediatric unit is scratching the head almost constantly. It would be most important for the LPN/LVN to take which of the following actions?
Reworded Question: What might head scratching indicate?
Strategy: Determine if data collection or implementation is appropriate.
Needed Info: Pediculosis (lice). Data collection: scalp—white eggs (nits) on hair shafts, itchy; body—macules and papules; pubis—red macules.
Category: Data Collection/Health Promotion and Maintenance
- Discuss basic hygiene with the parents—makes an assumption; must collect data first
- Instruct the child not to sleep with the dog—must first collect data to determine the problem
- Advise parents to contact an exterminator—not enough information to make this determination
- Observe the scalp for small white specks—CORRECT: nits (eggs) appear as small, white, oval flakes attached to hair shaft
- The Answer is 3
The client diagnosed with major depressive disorder who was admitted to the psychiatric unit for treatment and observation a week ago suddenly appears cheerful and motivated. The LPN/LVN should be aware of which of the following?
Reworded Question: What is the significance of sudden mood changes in a depressed client?
Strategy: Know the signs of impending suicide.
Needed Info: Data collection for suicidal ideation, suicidal gestures, suicidal threats, and actual suicidal attempt. Clients who have developed a suicide plan are more serious about following through, and are at grave risk. Clients emerging from severe depression have more energy with which to formulate and carry out a suicide plan (for which they had no energy before treatment). The LPN/LVN should determine risk for suicide; suspect suicidal ideation in depressed client; ask the client if he is thinking about suicide; ask the client about the advantages and disadvantages of suicide to determine how client sees his situation; evaluate client’s access to a method of suicide; and support the client’s reason to live.
Category: Planning/Psychosocial Integrity
- The client is likely sleeping well because of the medication—improved sleep patterns would not explain the client’s sudden mood change
- The client has made new friends and has a support group—support on the nursing unit would not explain the mood change
- The client may have finalized a suicide plan—CORRECT: as depressed clients improve, their risk for suicide is greater because they are able to mobilize more energy to plan and execute suicide
- The client is no longer depressed due to treatment—sudden cheerful and energetic mood does not indicate resolution of depression
- The Answer is 3
The LPN/LVN is caring for clients in the GYN clinic. A client reports an off-white vaginal discharge with a curdlike appearance and vulvar itching. It would be most important for the LPN/LVN to ask which of the following questions?
Reworded Question: What is a predisposing factor to developing candidiasis?
Strategy: “Most important” indicates there may be more than one correct response.
Needed Info: Candida albicans. Symptoms: odorless, cheesy white discharge; itching, inflames vagina and perineum. Treatment: topical clotrimazole, nystatin.
Category: Data Collection/Health Promotion and Maintenance
- “Do you routinely douche?”—not a factor in the development of candidiasis
- “Are you sexually active?”—candidiasis not usually sexually transmitted; predisposing factors include glycosuria, pregnancy, and oral contraceptives
- “What kind of birth control do you use?”—CORRECT: oral contraceptives predispose individuals to candidiasis
- “Have you taken any cough medicine?”—no relationship between cough medicine and candidiasis
- The Answer is 2
The primary health care provider orders application of an elastic wrap bandage for a client’s left leg from toes to mid-thigh. The LPN/LVN should do which of the following?
Reworded Question: What should an LPN/LVN do for a bandaged extremity?
Strategy: Think of what is most important for a bandaged extremity.
Needed Info: Quality of circulation: determined by observing the color, motion, and sensitivity of an affected body part, particularly distal to the bandage.
Category: Data Collection/Safe and Effective Care Environment/Safety and Infection Control
- Increase friction between skin and bandage surfaces—would cause skin breakdown
- Leave a small distal portion of the extremity exposed—CORRECT: enables the LPN/LVN to determine the color, motion, and sensitivity of a distal body part
- Use multiple pins to secure the bandage—unnecessary
- Position the left leg in abduction—unnecessary
- The Answer is 3
A client recovering from a laparoscopic laser cholecystectomy says to the LPN/LVN, “I hate the thought of eating a low-fat diet for the rest of my life.” Which of the following responses by the LPN/LVN is most appropriate?
Reworded Question: Is a low-fat diet required indefinitely?
Strategy: “Most appropriate” indicates discrimination may be required to answer the question.
Needed Info: Laparoscopic laser cholecystectomy is removal of the gallbladder by laser through a laparoscope; monitor T-tube if present; observe for jaundice; monitor intake and output; monitor for pain and encourage early ambulation to rid the body of carbon dioxide.
Category: Implementation/Physiological Integrity/Physiological Adaptation
- “I will ask the dietician to come speak with you.”—passing the reponsibility; LPN/LVN should respond to the client
- “What do you think is so bad about following a low-fat diet?”—does not respond directly to the client’s statement
- “It may not be necessary for you to follow a low-fat diet for that long.”—CORRECT: fat restriction is usually lifted as the client tolerates fat; biliary ducts dilate sufficiently to accommodate bile volume that was held by the gallbladder
- “At least you will be alive and not suffering that pain.”—nontherapeutic and judgmental
- The Answer is 2
The LPN/LVN is caring for clients in a pediatric clinic. The mother of a 14-year-old male privately tells the LPN/LVN that she is worried about her son because she unexpectedly walked into his room and discovered him masturbating. Which of the following responses by the LPN/LVN is most appropriate?
Reworded Question: What is the most therapeutic response?
Strategy: Remember therapeutic communication.
Needed Info: Male changes in puberty: increase in genital size; breast swelling; pubic, facial, axillary, and chest hair; deepening voice; production of functional sperm; nocturnal emissions. Psychosexual development: masturbation as expression of sexual tension; sexual fantasies; experimental sexual intercourse.
Category: Implementation/Health Promotion and Maintenance
- “Tell your son he could go blind doing that.”—false information
- “Masturbation is a normal part of sexual development.”—CORRECT: true statement provides opportunity for sexual self-exploration
- “He’s really too young to be masturbating.”—boys typically begin masturbating in early adolescence
- “Why don’t you give him more privacy?”—judgmental; doesn’t take advantage of opportunity to teach
- The Answer is 4
A client begins to breathe very rapidly. Which of the following actions by the LPN/LVN would be the most appropriate?
Reworded Question: What is the most appropriate action for a client experiencing tachypnea?
Strategy: “Most appropriate” indicates priority.
Needed Info: Tachypnea: rapid respirations, respirations greater than 20 breaths/minute. Changes in respiratory rate: gather additional data in order to provide complete information to the RN and primary health care provider.
Category: Data Collection/Safe and Effective Care Environment/Coordinated Care
- Auscultate the client's apical pulse rate—initial data collection should be directed at respiratory data
- Measure client's blood pressure and pulse—initial data collection should be directed at respiratory data
- Notify the primary health care provider—the primary health care provider will need more data to respond to client's condition change
- Obtain the client's oxygen saturation level—CORRECT: provides the LPN/LVN with data about the client’s oxygen saturation
- The Answer is 1
The LPN/LVN is planning morning care for a client hospitalized after a stroke resulting in left-sided paralysis and homonymous hemianopia. During morning care, the LPN/LVN should do which of the following?
Reworded Question: What should you do for morning care for this client?
Strategy: Think about the consequences of each answer choice.
Needed Info: Homonymous hemianopia: blindness in half of each visual field caused by damage to brain. Client cannot see past midline toward the side opposite the lesion without turning the head toward that side. Approach client from side that is not visually impaired. Reduce noise and complexity of decision making.
Category: Implementation/Physiological Integrity/Physiological Adaptation
- Provide morning care from the right side of the client—CORRECT: approach from side with intact vision
- Speak loudly and distinctly when talking with the client—no hearing loss
- Reduce the level of lighting in the client’s room to prevent glare—increase light to assist with vision
- Provide client’s care to reduce the client's energy expenditure—encourage independence
- The Answer is 1
A primigravid client at 32 weeks’ gestation comes to the clinic for her initial prenatal visit. The client reports periodic headaches and continually bumping into things. The LPN/LVN observes numerous bruises in various stages of healing around the client’s breasts and abdomen. Vital signs are: BP 120/80, pulse 72 beats/minute, respirations 18 breaths/minute, and fetal heart tones 142 beats/minute. Which of the following responses by the LPN/LVN is best?
Reworded Question: What might bruising indicate?
Strategy: Determine if it is appropriate to collect data or implement.
Needed Info: Symptoms of domestic abuse: frequent visits to physician’s office or emergency room for unexplained trauma; client being cued, silenced, or threatened by an accompanying family member; evidence of multiple old injuries, scars, healed fractures seen on x-ray; fearful, evasive, or inconsistent replies, or nonverbal behaviors such as flinching when approached or touched. Nursing care: provide privacy during initial interview to ensure perpetrator of violence does not remain with client; carefully document all injuries (with consent); determine safety of client by asking specific questions about weapons, substance abuse, extreme jealousy; develop with client a safety or escape plan; refer client to community resources.
Category: Data Collection/Health Promotion and Maintenance
- “Are you battered by your partner?”—CORRECT: evidence of injury should be investigated; assess head, neck, chest, abdomen, breasts, upper extremities
- “How do you feel about being pregnant?”—injuries take priority
- “Tell me about your headaches.”—injuries take priority
- “You may be more clumsy due to your size.”—assumption; need to collect data
- The Answer is 4
The LPN/LVN is providing care for a client with chronic lung disease who is receiving oxygen through a nasal cannula. The LPN/LVN should expect which of the following to occur?
Reworded Question: What physiological changes occur with chronic obstructive pulmonary disease (COPD) that affect oxygen usage?
Strategy: Note the guidelines for oxygen use for clients with COPD.
Needed Info: Clients with COPD retain carbon dioxide. Client’s respiratory drive may be controlled by the level of oxygen present in the arterial blood. Administration of oxygen at high-liter flows can suppress the respiratory drive. Humidification effective only for flow rates above 5 L.
Category: Planning/Physiological Integrity/Physiological Adaptation
- Arterial blood gases will be drawn q 2 hours—blood gases are not drawn that often unless the client is in acute distress
- The client’s oral intake will be restricted—fluids should be encouraged, not restricted
- The client will be maintained on bed rest—client should rest as needed: maintaining the client on bed rest is unnecessary
- The oxygen flow rate will be set at 3 L/minute or less—CORRECT: the respiratory drive for clients with COPD can be suppressed by high levels of oxygen
- The Answer is 1
The LPN/LVN is caring for a pediatric client in a leg cast for treatment of a right ankle fracture. It is most important for the LPN/LVN to reinforce which of the following activities after discharge?
Reworded Question: What is the priority action for a client in a cast?
Strategy: Determine the outcome of each answer choice.
Needed Info: Immediate nursing care for plaster cast: don’t cover cast until dry (48 hours), handle with palms not fingertips; don’t rest on hard surfaces; elevate affected limb above heart on soft surface until dry; don’t use head lamp; check for blueness or paleness, pain, numbness, tingling (if present, elevate area; if it persists, contact physician); client should remain inactive while cast dries. Intermediate nursing care: mobilize client, isometric exercises; check for break in cast or foul odor; tell client not to scratch skin under cast and not to put anything underneath cast; if fiberglass cast gets wet, dry with hair dryer on cool setting. After-cast nursing care: wash skin gently, apply baby powder/cornstarch/baby oil; have client gradually adjust to movement without support of cast; swelling is common, elevate limb and apply elastic bandage.
Category: Implementation/Physiological Integrity/Reduction of Risk Potential
- The client performs isometric exercises of the right leg—CORRECT: contraction of muscle without moving joint; promotes venous return and circulation, prevents thrombi; quadriceps setting (push back knees into bed) and gluteal setting (push heels into bed)
- The parent massages the client’s right foot with moisturizer—will help prevent dryness of foot but does not address skin under cast
- The parent cleans the leg cast with mild soap and water—unnecessary to clean cast
- The parent elevates the right leg on several pillows—unnecessary
- The Answer is 3
The LPN/LVN is caring for a client who had a thyroidectomy 12 hours ago for treatment of Graves’ disease. The LPN/LVN would be most concerned if which of the following were observed?
Reworded Question: What is a complication after a thyroidectomy?
Strategy: “Most concerned” indicates a complication.
Needed Info: Nursing care for Graves’ disease/hyperthyroidism: limit activities and provide frequent rest periods; advise light, cool clothing; avoid stimulants; use calm, unhurried approach; administer antithyroid medication, irradiation with I131 PO. Post-thyroidectomy care: low or semi-Fowler’s position; support head, neck, and shoulders to prevent flexion or hyperextension of suture line; tracheostomy set at bedside; observe for complications—laryngeal nerve injury, thyroid storm, hemorrhage, respiratory obstruction, tetany (decreased calcium from parathyroid involvement), check Chvostek’s and Trousseau’s signs.
Category: Data Collection/Physiological Integrity/Reduction of Risk Potential
- The client’s vital signs include: blood pressure 138/82 mm Hg, pulse 84 beats/minute, and respirations 16 breaths/minute—vital signs within normal limits
- The client supports the head and neck to turn head to right—prevents stress on the incision
- The client spontaneously flexes the wrist when the blood pressure is inflated during blood pressure measurement—CORRECT: carpal spasms indicate hypocalcemia
- The client becomes drowsy and reports a sore throat—expected outcome after surgery
- The Answer is 4
A client is admitted who reports severe pain in the right lower quadrant of the abdomen. Which of the following actions should the LPN/LVN take to assist the client with pain relief?
Reworded Question: What is an appropriate nonpharmacological method for pain relief?
Strategy: Determine the outcome of each answer choice.
Needed Info: Establish a 24-hour pain profile. Teach client about pain and its relief: explain quality and location of impending pain; slow, rhythmic breathing to promote relaxation; effects of analgesics and benefits of preventative approach; splinting techniques to reduce pain. Reduce anxiety and fears. Provide comfort measures: proper positioning; cool, well-ventilated, quiet room; back rub; allow for rest.
Category: Implementation/Physiological Integrity/Basic Care and Comfort
- Encourage rhythmic, shallow breathing—slow, rhythmic deep breathing promotes relaxation
- Massage the right lower quadrant of the abdomen—if appendicitis is suspected, massage or palpation should never be performed as these actions may cause the appendix to rupture
- Apply a warm heating pad to the client's abdomen—if pain is caused by appendicitis, increased circulation from heat may cause appendix to rupture
- Position the client for comfort using pillows—CORRECT: nonpharmacological methods of pain relief
- The Answer is 3
Which of the following actions by the LPN/LVN would be considered negligence?
Reworded Question: What is incorrect behavior?
Strategy: Think about the consequences of each action.
Needed Info: Negligence is the unintentional action or failure to act of an LPN/LVN that a reasonable person would or would not perform in similar circumstances; can be an act of commission or omission. Standards of care: the actions that other LPN/LVNs would take in the same or similar circumstances that provide for quality care. Nurse practice acts: state laws that determine the scope of the practice of nursing.
Category: Implementation/Safe and Effective Care Environment/Safety and Infection Control
- Administering heparin subcutaneously into a client’s abdomen without first aspirating for blood—correct procedure
- Crushing furosemide and adding to a teaspoon of applesauce for an elderly client—correct procedure
- Lowering the bed side rails after administering meperidine and hydroxyzine to a client preoperatively—CORRECT: bed side rails should be raised after administering preoperative medication
- Placing a used syringe and needle in a sharps container in a client’s room—correct procedure
- The Answer is 3
The LPN/LVN is teaching an elderly client with right-sided weakness how to use a cane. Which of the following behaviors by the client indicates that the teaching was effective?
Reworded Question: What is the appropriate technique used to ambulate with a cane?
Strategy: Determine the outcome of each answer choice.
Needed Info: Cane tip should have concentric rings (shock absorber for stability). Flex elbow 30 degrees and hold handle up; tip of cane should be 15 cm lateral to base of the fifth toe. Hold cane in hand opposite affected extremity; advance cane and affected leg; lean on cane when moving good leg. To manage stairs, step up on good leg, place the cane and affected leg on step; reverse when going down (“up with the good, down with the bad”); same sequence used with crutches.
Category: Evaluation/Physiological Integrity/Basic Care and Comfort
- The client holds the cane with the right hand, moves the cane forward followed by the right leg, and then moves the left leg—should hold cane with the stronger (left) hand
- The client holds the cane with the right hand, moves the cane forward followed by the left leg, and then moves the right leg—should hold cane with the stronger (left) hand
- The client holds the cane with the left hand, moves the cane forward followed by the right leg, and then moves the left leg—CORRECT: the cane acts as a support and aids in weight-bearing for the weaker right leg
- The clientn holds the cane with the left hand, moves the cane forward followed by the left leg, and then moves the right leg—cane needs to be a support and aid in weight-bearing for the weaker right leg
- The Answer is 4
The LPN/LVN is caring for client whose vital signs have been within normal limits. Now vital signs include: tympanic temperature 103.6° F (39.7° C), pulse 82 beats/minute, regular and strong, respirations 14 breaths/minute, shallow and unlabored, and blood pressure 134/88 mm Hg. What should the LPN/LVN’s next action be?
Reworded Question: What do you do first when you obtain a vital sign that represents a significant change in the client’s status and conflicts with other data?
Strategy: Think about what other vital sign changes occur with a significant temperature elevation.
Needed Info: Vitals in normal range: pulse 82 beats/minute, respirations 14 breaths/minute, BP 134/88 (slightly elevated likely due to age). Temperature significantly elevated: should result in a more rapid pulse rate and an increased respiratory rate due to increased cellular metabolism. Validation of the temperature reading with another thermometer is required to determine the accuracy of the initial temperature reading.
Category: Planning/Physiological Integrity/Physiological Adaptation
- Notify primary health care provider immediately—the LPN/LVN should take responsibility for gathering additional data before calling the physician
- Proceed with the client’s care—a temperature elevation to 103.6° F (39.7° C) is abnormal
- Record vital signs in medical record—the LPN/LVN should ensure the accuracy of reading before documenting them in a legal document
- Retake the temperature with a different thermometer—CORRECT: a temperature of 103.6° F (39.7° C) is abnormal without a corresponding increase in pulse and respiratory rate, the thermometer may be defective
- The Answer is 2
A client admitted to the hospital with right femur fracture is placed in balanced suspension traction with a Thomas splint and Pearson attachment. During the first 48 hours, the LPN/LVN should gather data related to which of the following complications?
Reworded Question: What complication of a fracture is seen in the first 48 hours?
Strategy: Be careful! They are asking for the complication that occurs during the first 48 hours. Later complications may be included.
Needed Info: Complications of fractures: (1) compartment syndrome (increased pressure externally [casts, dressings] or internally [bleeding, edema] resulting in compromised circulation); signs/symptoms (S/S): pallor, weak pulse, numbness, pain, (2) shock, (3) fat embolism, (4) deep vein thrombosis, (5) infection, avascular necrosis, (6) delayed union, nonunion, malunion of the bone.
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- Pulmonary embolism—obstruction of pulmonary system by thrombus from venous system or right side of heart; seen 2–3 days to several weeks after fracture
- Fat embolism—CORRECT: fat moves into bloodstream from fracture; formed by alteration in lipids in blood; fat combines with platelets to form emboli; S/S: abnormal behavior due to cerebral anoxia (confusion, agitation, delirium, coma), abnormal arterial blood gases (ABGs) (pO2 below 60 mmHg), increased respiratory rate; chest pain, dyspnea, pallor, hypertension, petechiae on chest, upper arms, abdomen; treatment: high Fowler’s position, high concentration O2 , ventilation with positive end expiratory pressure (PEEP) to decrease pulmonary edema, IV fluid to prevent shock, steroids
- Avascular necrosis—(seen later than 48 hours) bone loses blood supply and dies; seen with chronic kidney disease or prolonged steroid use; treatment: bone graph, joint fusion, prosthetic replacement
- Malunion—bone fragments heal in deformed position as a result of inadequate reduction and immobilization; treatment: surgical or manual manipulation to realign
- The Answer is 1
The LPN/LVN is helping an unlicensed assistive personnel (UAP) provide a bed bath to a comatose client who is incontinent. The LPN/LVN should intervene if which of the following actions is noted?
Reworded Question: What is an incorrect action?
Strategy: “Should intervene” indicates that you are looking for something wrong.
Needed Info: Standard precautions used with all clients: primary strategy for preventing exposure to blood or body fluids. Gloves are worn when exposure to blood, body fluids, secretions, excretions, or contaminated articles is likely; remove and discard promptly after use, and perform hand hygiene, before touching items and environmental surfaces to reduce the risk for pathogen transmission.
Category: Evaluation/Safe and Effective Care Environment/Safety and Infection Control
- The UAP answers the phone while wearing gloves—CORRECT: contaminated gloves should be removed and discarded, and then hand hygiene performed before answering the phone.
- The UAP log-rolls the client to provide back care—appropriate action, maintains proper body alignment
- The UAP places an incontinence pad under the client—appropriate for a client with incontinence
- The UAP positions the client on the left side, with the head of bed elevated—appropriate position to prevent aspiration and protect the client's airway
- The Answer is 3
A client is brought to the emergency department for treatment after being found on the floor by a family member. When comparing the legs, the LPN/LVN would most likely make which of the following observations?
Reworded Question: What is a symptom of a hip fracture?
Strategy: Think about each answer choice.
Needed Info: Symptoms of fracture: swelling, pallor, ecchymosis; loss of sensation to other body parts; deformity; pain, acute tenderness, or both; muscle spasms; loss of function, abnormal mobility; crepitus (grating sound on movement); shortening of affected limb; decreased or absent pulses distal to injury; affected extremity colder than contralateral part. Emergency nursing care: immobilize joint above and below fracture using splints before moving client; in open fracture, cover the wound with sterile dressings or cleanest material available, control bleeding by direct pressure; check temperature, color, sensation, capillary refill time distal to fracture; in emergency department, manage pain.
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- The client’s left leg is longer than the right leg and externally rotated—affected leg shortens due to contraction of muscles attached above and below fracture site
- The client’s left leg is shorter than the right leg and internally rotated—affected leg is usually externally rotated
- The client’s left leg is shorter than the right leg and adducted—CORRECT: affected leg shortens due to contraction of muscles attached above and below fracture site, fragments overlap by 1–2 inches (2.5 to 5 cm)
- The client’s left leg is longer than the right leg and is abducted—affected leg shortens and externally rotates
- The Answer is 3
The LPN/LVN is caring for a client with a cast on the left leg. The LPN/LVN would be most concerned if which of the following is observed?
Reworded Question: What is a complication of a cast?
Strategy: “Most concerned” indicates a complication.
Needed Info: Immediate nursing care for plaster cast: Don’t cover cast until dry (48 hours), handle with palms not fingertips; don’t rest on hard surfaces; elevate affected limb above heart on soft surface until dry; don’t use head lamp; check for blueness or paleness, pain, numbness, tingling (if present, elevate area; if it persists, contact primary health care provider); client should remain inactive while cast dries. Intermediate nursing care: mobilize client, isometric exercises; check for break in cast or foul odor; tell client not to scratch skin under cast and not to put anything underneath cast; if fiberglass cast gets wet, dry with hair dryer on cool setting. After-cast nursing care: Wash skin gently; have client gradually adjust to movement without support of cast; swelling is common, elevate limb.
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- Capillary refill time is less than 3 seconds—capillary refill time is within normal limits
- Client reports discomfort and itching—a casted extremity may itch or feel uncomfortable due to prolonged immobility
- Client reports of tightness and pain—CORRECT: pain and tightness may develop if swelling occurs and the cast becomes too tight; if left untreated compartment syndrome may develop
- Client’s foot is elevated on a pillow—newly casted extremity may be slightly elevated to help relieve edema; it should remain in correct anatomical position and below heart level to allow sufficient arterial perfusion
- The Answer is 2
The LPN/LVN is assisting with discharging a client from an inpatient alcohol treatment unit. Which of the following statements by the client’s wife indicates that the family is coping adaptively?
Reworded Question: What indicates that the client’s family is coping with the client’s alcoholism?
Strategy: Think about what each statement means.
Needed Info: Nursing care for alcohol use disorder: safety; monitor for withdrawal; reality orientation; increase self-esteem and coping skills; balanced diet; abstinence from alcohol; identify problems related to drinking in family relationships, work, etc.; help client to see/admit problem; confront denial with slow persistence; maintain relationship with client; establish control of problem drinking; provide support; Alcoholics Anonymous; disulfiram (Antabuse): drug used to maintain sobriety, based on behavioral therapy.
Category: Evaluation/Psychosocial Integrity
- “My husband will do well as long as I keep him engaged in activities that he likes.”—wife is accepting responsibility; codependent behavior
- “My focus is learning how to live my life.”—CORRECT: wife is working to change codependent patterns
- “I am so glad that our problems are behind us.”—unrealistic; discharge is not the final step of treatment
- “I’ll make sure that the children don’t give my husband any problems.”—wife is accepting responsibility; codependent behavior
- The Answer is 3
An LPN/LVN is caring for clients in the mental health clinic. A client reporting insomnia and anorexia tearfully tells the LPN/LVN about a personal job loss after 15 years of employment with the company. Which of the following responses by the LPN/LVN is most appropriate?
Reworded Question: What is the most therapeutic response?
Strategy: Remember therapeutic communication.
Needed Info: Nursing considerations, explore client’s understanding of the problem: focus on the present; emphasize client’s strengths; avoid blaming; determine how client handled similar situations; provide support; mobilize client’s coping strategies.
Category: Implementation/Psychosocial Integrity
- “Did you receive a severance package?”—yes or no questions are not therapeutic
- “Focus on your healthy, happy family.”—gives advice and dismisses the client's feelings
- “Explain what happened with your job.”—CORRECT: validates the client's concern and further explores situation; encourages the client to verbalize feelings
- “Job loss is very common these days..”—dismisses the client’s concern
- The Answer is 1
A client with a history of alcohol use disorder is transferred to the unit in an agitated state. The client is vomiting and diaphoretic, and states that it has been 5 hours since the last drink. The LPN/LVN would expect to administer which of the following medications?
Reworded Question: What is the best medication to treat acute alcohol withdrawal?
Strategy: Think about the action of each drug.
Needed Info: Alcohol sedates the central nervous system (CNS); rebound during withdrawal. Early symptoms occur 4–6 hours after last drink. Symptoms: tremors; easily startled; insomnia; anxiety; anorexia; alcoholic hallucinosis (48 hours after last drink). Nursing care: administer sedation as needed, usually benzodiazepines; monitor vital signs, particularly pulse; institute seizure precautions; provide a quiet, well-lit environment; orient client frequently; don’t leave hallucinating, confused client alone; administer anticonvulsants as needed, thiamine IV or IM, and IV dextrose.
Category: Planning/Psychosocial Integrity
- Chlordiazepoxide—CORRECT: antianxiety; used to treat symptoms of acute alcohol withdrawal; side effects (S/E): lethargy, hangover effect, agranulocytosis
- Disulfiram—used as a deterrent to compulsive drinking; contraindicated within 12 hours of alcohol consumption
- Methadone—opioid agonist; used to treat opiod withdrawal syndrome; S/E: respiratory depression, hyptension, dizziness, lightheadedness
- Naloxone—opioid antagonist used to reverse opiod-induced respiratory depression; S/E: ventricular fibrillation, seizures, pulmonary edema
- The Answer is 2
The LPN/LVN is caring for a client diagnosed with end-stage colon cancer. The spouse of the client says, “We have been married for so long. I am not sure how I can go on now.” What is the most appropriate response by the LPN/LVN?
Reworded Question: What is the most therapeutic response to the spouse of the person diagnosed with terminal colon cancer?
Strategy: Remember therapeutic communication.
Needed Info: The client in this interaction is the spouse of the client diagnosed with end-stage colon cancer; focus on the present; encourage verbalization of feelings; provide support.
Category: Implementation/Psychosocial Integrity
- “It sounds like your children will be there to help during your time of grieving.”—dismisses client’s concern; keep focus on client
- “I know this is difficult. Tell me more about what you are feeling now.”—CORRECT: acknowledges client’s feelings; allows client to express feelings
- “Think about the pain and suffering your spouse has endured lately.”—gives advice; discourages verbalization
- “I will call the hospice nurse to discuss to your spouse's condition with you.” —passes responsibility to the hospice nurse; instead the LPN/LVN should encourage the spouse to express feelings
- The Answer is 2
The LPN/LVN is reinforcing teaching with an elderly client about how to use a standard aluminum walker. Which of the following behaviors by the client indicates that the reinforcement of teaching was effective?
Reworded Question: What is the correct technique when ambulating with a walker?
Strategy: Determine the outcome of each answer choice.
Needed Info: Elbows flexed at 20- to 30-degree angle when standing with hands on grips. Lift and move walker forward 8–10 inches (20–25 cm). With partial or non-weight-bearing, put weight on wrists and arms and step forward with affected leg, supporting self on arms, and follow with good leg. Nurse should stand behind client, hold onto gait belt at waist as needed for balance. Sit down by grasping armrest on affected side, shift weight to good leg and hand, lower self into chair. Client should wear sturdy shoes.
Category: Evaluation/Physiological Integrity/Basic Care and Comfort
- The client slowly pushes the walker forward 12 inches (30 cm), then takes small steps forward while leaning on the walker—should not push the walker
- The client lifts the walker, moves it forward 10 inches (25 cm), and then takes several small steps forward—CORRECT: the client should pick up the walker, and then place it down on all legs
- The client supports weight on the walker while advancing it forward, then takes small steps while balancing on the walker—the client should not support weight on walker while trying to move it
- The client slides the walker 18 inches (46 cm) forward, then takes small steps while holding onto the walker for balance—client should pick up the walker, not slide it forward
- The Answer is 2
An LPN/LVN is providing care for a group of elderly clients in a long-term care facility. The LPN/LVN knows that the elderly are at greater risk of developing sensory deprivation for which of the following reasons?
Reworded Question: Why do the elderly have sensory deprivation?
Strategy: Think about each answer choice.
Needed Info: Plan/implementation: assist client with adjusting to lifestyle changes; allow client to verbalize concerns; prevent isolation; provide assistance as required.
Category: Implementation/Psychosocial Integrity
- Increased sensitivity to the side effects of medications—many medications alter GI function but do not cause decreased vision, hearing, or taste
- Decreased visual, auditory, and gustatory abilities—CORRECT: gradual loss of sight, hearing, and taste interferes with normal functioning
- Isolation from their families and familiar surroundings—clients are in contact with other residents and staff who provide stimulation
- Decreased musculoskeletal function and mobility—clients can be mobilized in wheelchairs, if necessary
- The Answer is 2
The LPN/LVN would expect which of the following clients to be able to sign a consent form for nonemergent medical treatment?
Reworded Question: Which of these clients can give consent for own medical treatment?
Strategy: Think about the requirements for informed consent in nonemergent medical situations.
Needed Info: Clients requiring consent by an agent: under 18 years of age unless emancipated, declared legally incompetent, under the influence of drugs or alcohol, unable to understand or respond to information. In emergency situations: assumption that clients would want to be treated.
Category: Planning/Safe and Effective Care Environment/Coordinated Care
- A school-age child with a right tibia and fibula fracture—this client requires the consent of the legal guardian in this nonemergent situation
- A client requiring surgery for acute appendicitis—CORRECT: this client can provide own informed consent
- A client who is confused after a motor vehicle accident —informed consent would be required from designate health care agent in this nonemergent situation
- A client who has been legally declared incompetent—consent is required from the designate health care agent in this nonemergent situation
- The Answer is 3
An LPN/LVN is assisting with the discharge of a client with a diagnosis of hepatitis of unknown etiology. The LPN/LVN knows that teaching has been successful if the client makes which of the following statements?
Reworded Question: What is a correct statement about hepatitis?
Strategy: Determine the outcome of each statement.
Needed Info: Hepatitis A (HAV): high-risk groups include young children, residents of institutions for custodial care, international travelers; transmission by fecal/oral route, poor sanitation; nursing considerations include prevention, improved sanitation, treat with gammaglobulin early postexposure, no preparation of food. Hepatitis B (HBV): high-risk groups include drug addicts, fetuses from infected mothers, homosexually active men, transfusions, health care workers; transmission by parenteral, sexual contact, blood/body fluids; nursing considerations include hepatitis vaccine, immune globulin (HBIG) postexposure, chronic carriers (potential for chronicity 5–10%). Hepatitis C (HVC): high-risk groups include transfusions, international travelers; transmission by blood or body fluids. Delta hepatitis: high-risk groups same as for HBV; transmission coinfects with HBV, transmitted through close personal contact.
Category: Evaluation/Physiological Integrity/Reduction of Risk Potential
- “I am so sad that I am not able to hold my baby.”—hepatitis not spread by casual contact
- “I will eat my meal after my family finishes eating.”—client can eat with family; cannot share eating utensils
- “I will make sure that my children don’t use my eating utensils—CORRECT: to hepatitis transmission, the client should not share eating utensils or drinking glasses, and should wash hands before eating and after using the toilet
- “I’m glad that I don’t have to get help taking care of my children.”—need to alternate rest and activity to promote hepatic healing; mothers of young children will need help
- The Answer is 2
The LPN/LVN checks the IV flow rate for a postoperative client. The client is to receive 3,000 mL of lactated Ringer’s lactate solution IV infused over 24 hours. The IV administration set has a drop factor of 10 drops per milliliter. The LPN/LVN would expect the client’s IV to infusing at how many drops per minute?
Reworded Question: What is the IV flow rate?
Strategy: Remember the formula to calculate IV flow rate: total volume × drop factor divided by the time in minutes.
Needed Info: Lactated Ringer’s: electrolyte solution used to expand extracellular fluid volume, and reduce blood viscosity.
Category: Implementation/Physiological Integrity/Pharmacological Therapies
- 18—incorrect
- 21—CORRECT: (3,000 × 10) divided by (24 × 60) = 30,000 divided by 1,440 = 20.8 = 21
- 35—incorrect
- 40—incorrect
- The Answer is 1
A client diagnosed with emphysema becomes restless and confused. Which of the following actions should the LPN/LVN take next?
Reworded Question: What should the LPN/LVN do to raise the oxygen levels of a client with emphysema?
Strategy: Determine the outcome of each answer choice.
Needed Info: Emphysema: overinflation of alveoli resulting in destruction of alveoli walls; predisposing factors include smoking, chronic infections, environmental pollution. Teaching includes breathing exercises; stop smoking; avoid hot and cold air or allergens; instructions regarding medications; avoid crowds or close contact with persons who have colds or influenza; adequate rest and nutrition; oral hygiene; influenza vaccines; observe sputum for indications of infection.
Category: Implementation/Physiological Integrity/Reduction of Risk Potential
- Encourage pursed-lip breathing—CORRECT: purse-lipped breathing helps the client control the rate and depth of breathing
- Measure the client’s temperature—confusion is probably due to decreased oxygenation
- Assess the client’s potassium level—confusion is most likely caused by poor oxygenation, not electrolyte imbalance
- Increase the client’s oxygen flow rate to 5 L/minute—should receive low flow oxygen to prevent carbon dioxide narcosis
- The Answer is 4
The LPN/LVN is caring for a client following cataract surgery on the right eye. The client reports severe eye pain in the right eye. Which of the following activities should the LPN/LVN do first?
Reworded Question: Is pain after cataract surgery normal?
Strategy: Remember what you know about cataract removal.
Needed Info: Cataract: change in the transparency of crystalline lens of eye. Causes: aging, trauma, congenital, systemic disease. S/S: blurred vision, decrease in color perception, photophobia. Treated by removal of lens under local anesthesia with sedation. Intraocular lens implantation, eyeglasses, or contact lenses after surgery. Complications: glaucoma, infection, bleeding, retinal detachment.
Category: Planning/Physiological Integrity/Reduction of Risk Potential
- Administer an analgesic to the client—mild discomfort treated with analgesics
- Recheck the client's condition in 30 minutes—action should be taken immediately
- Document finding in client's medical record—action should be taken immediately
- Report the finding to the supervising RN—CORRECT: ruptured blood vessel or suture causing hemorrhage or increased intraocular pressure; notify primary health care provider for restlessness, increased pulse rate, drainage on dressing
- The Answer is 4
The LPN/LVN is caring for a client 4 hours after intracranial surgery. Which of the following actions should the LPN/LVN take immediately?
Reworded Question: What is a priority after intracranial surgery?
Strategy: Determine the outcome of each answer choice.
Needed Info: Monitor vital signs hourly. Elevate head 30 to 45 degrees (as ordered) to promote venous return from brain, and prevent increased intracranial pressure (ICP). Avoid neck flexion and head rotation. Reduce environmental stimuli. Prevent the Valsalva maneuver by teaching the client to exhale when turning or moving in bed. Administer stool softeners. Restrict fluids to 1,200–1,500 mL/day. Administer medications: an osmotic diuretic, corticosteroid and anticonvulsant.
Category: Implementation/Physiological Integrity/Reduction of Risk Potential
- Instruct the client to deep breathe, cough, and expectorate into a tissue—coughing should be avoided because it increases ICP
- Position the client in a left lateral position with neck flexed—the head should be maintained in a neutral position to promote venous return and reduce risk for increased ICP
- Perform passive range-of-motion exercises every two hours—position changes required during range-of-motion exercises can increase ICP
- Use a turning sheet under the client's head to midthigh to reposition in bed—CORRECT: using a turning sheet under the client's head to midthigh helps move the client as a unit maintaining body alignment, and reducing the risk for increased ICP
- The Answer is 2
A pediatric client with a congenital heart disorder is admitted with heart failure. Digoxin 0.12 mg by mouth daily is ordered for the client. The bottle contains 0.05 mg of digoxin in 1 mL of solution. Which of the following amounts should the LPN/LVN administer to the client after validating the dose with the RN?
Reworded Question: How much of the medication should you give?
Strategy: Remember how to calculate dosages. Be careful and don’t make math errors.
Needed Info: Formula: dose on hand over 1 mL = dose desired.
Category: Implementation/Physiological Integrity/Pharmacological Therapies
- 1.2 mL—inaccurate
- 2.4 mL—CORRECT: 0.05 mg/1 mL = 0.12mg/x mL, 0.05x = 0.12, x = 2.4 mL
- 3.5 mL—inaccurate
- 4.2 mL—inaccurate
- The Answer is 4
The LPN/LVN is caring for a client diagnosed with chronic lymphocytic leukemia, hospitalized for treatment of hemolytic anemia. The LPN/LVN should expect to implement which of the following actions?
Reworded Question: What should you do for a client with anemia?
Strategy: Although the client has leukemia, he is admitted with anemia. You must focus on the anemia.
Needed Info: Lymphocytic leukemia: characterized by proliferation of lymphocytes. S/S: fatigue, weakness, hemolytic anemia, easy bruising, bleeding gums, epistaxis, fever, generalized pain. Diagnostic tests: CBC, bone marrow aspiration, lumbar puncture, x-rays, lymph node biopsy. Treatment: total body irradiation or radiation to spleen, chemotherapy. Nursing responsibilities: low-bacteria diet (no raw fruits or vegetables), institute bleeding precautions (soft toothbrush, don’t floss, no injections, no aspirin, pad bed rails, use air mattress, use paper tape), antiemetics, comfort measures. Hemolytic anemia S/S: jaundice, splenomegaly, hepatomegaly, fatigue, weakness. Treatment: O2, blood transfusions, corticosteroids.
Category: Planning/Physiological Integrity/Physiological Adaptation
- Encourage activities with other clients in the day room—does not meet need for rest
- Isolate the client from visitors and clients to avoid infection—no information given about white blood cell count; protective isolation for neutrophil count less than 500/mm3
- Provide a diet that contains foods that are high in vitamin C—needed for wound healing and resistance to infection; not best choice
- Maintain a quiet environment to promote adequate rest—CORRECT: primary problem activity intolerance due to fatigue
- The Answer is 3
The LPN/LVN is caring for a client with cervical cancer. The LPN/LVN notes that the radium implant has become dislodged. Which of the following actions should the LPN/LVN take first?
Reworded Question: What is the best action when a radium implant becomes dislodged?
Strategy: Think about the outcome of each answer choice.
Needed Info: Limit radioactive exposure: assign client to private room; place “Caution: Radioactive Material” sign on door; wear dosimeter film badge at all times when interacting with client (measures amount of exposure); do not assign pregnant health care worker to client; rotate staff caring for client; organize tasks so limited time is spent in client’s room; limit visitors; encourage client to do own care; provide shield in room. Client care: use antiemetics for nausea; consider body image; provide comfort measures; provide good nutrition.
Category: Implementation/Physiological Integrity/Reduction of Risk Potential
- Grasp the implant with a sterile hemostat and carefully reinsert it into the client—the implant should be picked up with long-handled forceps, not a hemostat, and deposited into a lead container in the room, not reinserted into the client
- Wrap the implant in a blanket and place it behind a lead shield until reimplantation—the implant should be picked up with long-handled forceps and put into a lead container in the room for disposal
- Ensure the implant is picked up with long-handled forceps and placed in a lead container—CORRECT: the priority is to secure the implant to prevent unwanted and dangerous radiation exposure; the implant should be picked up with long-handled forceps and then placed in a lead container; this equipment should be kept in the room of any client receiving this therapy so that it is readily available; institutional guidelines and procedures for managing dislodgement should be followed; radiology is usually involved as soon as dislodgement occurs
- Obtain a dosimeter reading on the client and report it to the primary health care provider—need to place implant in lead container
- The Answer is 2
The LPN/LVN comes to the home of a client with cellulitis of the left leg to perform a daily dressing change. The client tells the LPN/LVN that the unlicensed assistive personnel (UAP) changed the dressing earlier that morning. Which of the following actions by the LPN/LVN is best?
Reworded Question: What is the correct chain of command for reporting a problem?
Strategy: Think about the chain of command.
Category: Implementation/Safe and Effective Care Environment/Coordinated Care
- Tell the client that the new dressing looks fine—does not address the problem of the UAP performing the dressing change
- Notify the RN supervisor of the situation—CORRECT: correct follow the chain of command for reporting this problem
- Ask the client to describe the dressing change—does not address the problem of the UAP performing the dressing change
- Report the UAP to the home care agency—incorrect chain of command; should report problem to next person in direct line of authority in same area
- The Answer is 1
The LPN/LVN is caring for a client with pernicious anemia. The LPN/LVN reinforces teaching about the plan of care. The LPN/LVN should report which of the following statements to the RN?
Reworded Question: What is true about pernicious anemia?
Strategy: Determine the outcome of each answer choice.
Needed Info: Pernicious anemia is caused by failure to absorb vitamin B12 because of a deficiency of intrinsic factor from the gastric mucosa. Symptoms: pallor, slight jaundice, glossitis, fatigue, weight loss, paresthesias of hands and feet, disturbances of balance and gait. Treatment: vitamin B12 IM monthly.
Category: Evaluation/Physiological Integrity/Physiological Adaptation
- “In order to get better, I will take iron pills.”—CORRECT: pernicious anemia is due to vitamin B deficiency, not iron deficiency
- “I will attend smoking cessation classes.”—no reason to report
- “I will learn how to perform IM injections.”—many clients instructed how to give monthly IM B12 injection
- “I will make sure to eat a well-balanced diet.”—no reason to report
- The Answer is 2
The LPN/LVN is caring for clients on a general medical/surgical unit of an acute care facility. Four clients have been admitted in the last 20 minutes. Which of the admissions should the LPN/LVN see first?
Reworded Question: Who is the priority client?
Strategy: Think ABCs.
Needed Info: Factors to consider: chief complaint; age of client; medical history; potential for life-threatening event.
Category: Planning/Physiological Integrity/Reduction of Risk Potential
- A client reporting vomiting and diarrhea—airway issue takes priority
- A client with third-degree burns to face—CORRECT: face, neck, chest, or abdominal burns can cause severe edema that restricts the airway; airway issues take priority
- A client with a fractured left hip—airway issue takes priority
- A client reporting epigastric pain—airway issue takes priority
- The Answer is 4
The LPN/LVN is caring for a client with a diagnosis of chronic bronchitis. The client has audible wheezing, and an oxygen saturation of 85%. Four hours ago, the oxygen saturation was 88%. It is most important for the LPN/LVN to take which of the following actions?
Reworded Question: What is the best action for a client with COPD?
Strategy: Determine the outcome of each answer choice.
Needed Info: Chronic bronchitis: predisposing factors include smoking, chronic infections, environmental pollution. Teaching reinforcement includes breathing exercises; stop smoking; avoid hot and cold air or allergens; instructions regarding medications; avoid crowds or close contact with persons who have colds or influenza; adequate rest and nutrition; oral hygiene; influenza vaccines; observe sputum for indications of infection.
Category: Implementation/Physiological Integrity/Pharmacological Therapies
- Give beclomethasone, 2 puffs via metered-dose inhaler—administer brochodilator first to open passageways
- Auscultate the client's bilateral breath sounds—situation does not require further data collection
- Increase oxygen flow rate to 4L/minute via mask—increasing the client's blood oxygen level may cause respiratory depression
- Administer albuterol, 2 puffs via metered-dose inhaler—CORRECT: a brochodilator, such as albuterol relaxes bronchial smooth muscles and increases airflow to the lungs.
- The Answer is 4
The LPN/LVN is caring for a client hospitalized for observation following a fall. The client states, “My friend fell last year, and no one thought anything was wrong. She died 2 days later!” Which of the following responses by the LPN/LVN is best?
Reworded Question: What is the most therapeutic response?
Strategy: Remember therapeutic communication.
Needed Info: Therapeutic communication: using silence (allows client time to think and reflect; conveys acceptance; allows client to take lead in conversation); using general leads or broad openings (encourages client to talk, indicates interest in client); clarification (encourages description of feelings and details of particular experience; makes sure LPN/LVN understands client); reflecting (paraphrases what client says; reflects what client says, especially feelings conveyed).
Category: Implementation/Psychosocial Integrity
- “This happens to quite a few people.”—nontherapeutic; doesn’t address client’s concerns
- “We are monitoring you, so you’ll be okay.”—nontherapeutic; “don’t worry” response
- “Don’t you think I’m taking good care of you?”—nontherapeutic; focus is on the LPN/LVN
- “You’re concerned that it might happen to you?”—CORRECT: reflects client’s feelings
- The Answer is 2
The LPN/LVN is caring for clients on the pediatric unit. A client with second- and third-degree burns on the right thigh is being admitted. The LPN/LVN should expect the new client to be placed with which one of the following roommates?
Reworded Question: Who is the appropriate roommate for a client with burns?
Strategy: Think about the transmission of diseases.
Needed Info: Burns: increase the risk for infection; contact precautions to prevent spread of pathogens transmitted by direct contact or contact with items in the client's environment, such organisms as Clostridium difficile and methicillin-resistant Staphyococcus aureus; airborne and contact precautions required until chickenpox lesions become dry and crusted.
Category: Implementation/Physiological Integrity/Physiological Adaptation
- A client with chickenpox—infectious disease requires airborne and contact precautions
- A client with asthma—CORRECT: lowest risk of cross-contamination because client is not infectious
- A client who developed acute diarrhea after antibiotic—requires contact precautions because the client may have Clostridium difficile diarrhea
- A client with methicillin-resistant Staphylococcus aureus —requires resistant organism requires contact precautions
- The Answer is 2
To evaluate the effectiveness of a client’s heparin therapy, the LPN/LVN should monitor which of the following laboratory values?
Reworded Question: What blood work is done to monitor heparin therapy?
Strategy: Remember what information is most important for a client receiving heparin therapy.
Needed Info: Heparin: anticoagulant. Side effects: hemorrhage, thrombocytopenia. Antidote: protamine sulfate. When given subcutaneously, inject slowly; leave needle in place 10 seconds, then withdraw; don’t massage site; rotate sites. Nursing responsibilities: check for bleeding gums, bruises, nosebleeds, petechiae, melena, tarry stools, hematuria; use electric razor and soft toothbrush.
Category: Data Collection/Physiological Integrity/Reduction of Risk Potential
- Platelet count—evaluates platelet production; not altered
- Clotting time—CORRECT: or partial thromboplastin time; 1.5–2 times control, clotting time 2–3 times control
- Bleeding time—duration of bleeding after small puncture wound; detects platelet and vascular problems; not altered
- Prothrombin time—used to monitor warfarin therapy
- The Answer is 3
The LPN/LVN is reinforcing teaching with a client who is scheduled for a paracentesis. Which of the following statements by the client indicates that teaching has been successful?
Reworded Question: What is a correct statement about paracentesis?
Strategy: Determine the outcome of each answer choice.
Needed Info: Paracentesis: removal of fluid from the peritoneal cavity; 2–3 L may be removed. Preparation: informed consent; void, obtain vital signs; measure abdominal girth; weigh client. During procedure: frequently monitor vital signs. After procedure: document amount, color, characteristics of drainage obtained; assess pressure dressing for drainage; position in bed until vital signs stabilize.
Category: Evaluation/Physiological Integrity/Reduction of Risk Potential
- “I will be in surgery for less than an hour.”—not a surgical procedure
- “I must not void prior to the procedure.”—bladder is emptied prior to the procedure to prevent puncture
- “Two to 3 liters of fluid will be removed.”—CORRECT: primary health care provider slowly removes 2 to 3 liters of fluid to decrease ascites; in severe cases, can remove up to 6 liters
- “I will lie on my back and breathe slowly.”—positioned in an upright position with feet supported for the procedure
- The Answer is 2
The LPN/LVN is performing chest physiotherapy on a client with chronic airflow limitations (CAL). Which of the following actions should the nurse take first?
Reworded Question: What should the LPN/LVN do prior to beginning chest physiotherapy?
Strategy: Determine whether to collect data or implement.
Needed Info: Postural drainage: uses gravity to facilitate removal of bronchial secretions; client is placed in a variety of positions to facilitate drainage into larger airways; secretions may be removed by coughing or suctioning. Percussion and vibration: augments the effect of gravity during postural drainage; percussion: rhythmic striking of chest wall with cupped hands over areas where secretions are retained; vibration: hand and arm muscles of person doing vibration are tensed, and a vibrating pressure is applied to chest as client exhales.
Category: Data Collection/Physiological Integrity/Reduction of Risk Potential
- Perform chest physiotherapy prior to meals—prevents nausea, vomiting, aspiration
- Auscultate breath sounds before the procedure—CORRECT: helps identify areas of the lung that require drainage; auscultate breath sounds after the procedure to determine effectiveness
- Administer bronchodilators after the procedure—given before chest physiotherapy to dilate the bronchioles and to liquify secretions
- Percuss each lobe prior to asking the client to cough—may cause fractures of the ribs; percussion helps loosen thick secretions
- The Answer is 2
In which of the following situations would it be most appropriate for the LPN/LVN to wear a gown and gloves?
Reworded Question: Which of these clients poses the greatest risk for spreading disease, requiring the use of gloves and a gown?
Strategy: Note how microorganisms are most frequently spread.
Needed Info: Spread of microorganisms: contact directly with a source of infection, contact with surfaces contaminated with microorganisms, some airborne diseases, includes all bodily waste and fluids except sweat. Standard precautions: Centers for Disease Control and Prevention (CDC) recommends barrier techniques to prevent spread of microorganisms; common barriers include gloves, masks, goggles, and gowns; choose appropriate barrier for the situation.
Category: Implementation/Safe and Effective Care Environment/Safety and Infection Control
- Administering oral medications to a client with with human immunodeficiency virus disease—there is no contact with blood or other potentially infectious body fluids
- Assisting in the care of a motor vehicle accident victim who continues to bleed—CORRECT: blood from this client may contact the LPN/LVN’s skin when performing care or gathering data; gloves protect hands and gowns protect the skin from exposure to blood and body fluids
- Bathing a client with an abdominal wound infection—gloves provide adequate protection
- Changing the linen of a client with sickle-cell anemia—if bed is soiled, gloves should provide adequate protection; linen should not be in contact with the LPN/LVN’s uniform
- The Answer is 2
A client is receiving 1,000 mL of 5% dextrose in half normal saline solution IV to infuse over 8 hours. The IV administration set tubing delivers 15 drops per milliliter. The LPN/LVN should expect the flow rate to be how many drops per minute?
Reworded Question: What is the correct IV flow rate?
Strategy: Use the correct formula and be careful not to make math errors.
Needed Info: Formula: total volume × drip factor divided by the total time in minutes.
Category: Planning/Physiological Integrity/Pharmacological Therapies
- 15—incorrect
- 31—CORRECT: (1,000 × 15) divided by (8 × 60)
- 45—incorrect
- 60—incorrect
- The Answer is 3
A client is admitted to the hospital reporting seizures and a high fever. A positron emission tomography (PET) brain scan is prescribed. Before the PET brain scan, the client asks the LPN/LVN what position his necessary for the test. Which of the following statements by the LPN/LVN is most accurate?
Reworded Question: What is the proper position for a PET brain scan?
Strategy: Visualize the procedure.
Needed Info: PET brain scan: measures amount of uptake by the brain of radioactive isotopes. Damaged tissue absorbs more than normal tissue. Nursing care before: withhold medicationss (antihypertensives, vasoconstrictors, vasodilators for 24 hours). Test is painless. After test, force fluids to promote excretion of isotopes. Urine doesn’t need special handling.
Category: Implementation/Physiological Integrity/Reduction of Risk Potential
- “You will be in a side-lying position, with the foot of the bed elevated.”—incorrect
- “You will be in a semi-upright sitting position, with your knees flexed.”—incorrect
- “You will be lying on your back with a small pillow under your head.”—CORRECT
- “You will be flat on your back, with your feet higher than your head”—incorrect
- The Answer is 2
A client with a diagnosis of delirium is admitted to the hospital. Blood samples are sent to the laboratory to help determine the underlying cause. Laboratory test results include: sodium 156 mEq/L (156 mmol/L), chloride 100 mEq/L (100 mmol/L), potassium 4 mEq/L (4 mmol/L), bicarbonate 21 mEq/L (21 mmol/L), blood urea nitrogen (BUN) 86 mg/dL (30.7 mmol/L), glucose 100 mg/dL (5.5 mmol/L). Based on these laboratory results, the LPN/LVN would expect to see which of the following nursing diagnoses on the client’s care plan?
Reworded Question: What nursing diagnosis is appropriate?
Strategy: Determine if each laboratory test result is normal or abnormal. Decide what the abnormal laboratory test results indicate about the client and how it would influence the appropriate nursing diagnosis for that client.
Needed Info: Normal sodium: 135–145 mEq/L (135–145 mmol/L). Hypernatremia: dehydration and insufficient water intake. Normal chloride: 95–105 mEq/L (95–105 mmol/L). Normal potassium: 3.5–5 mEq/L (3.5–5 mmol/L). Normal bicarbonate: 22–26 mEq/L (22–26 mmol/L). Decreased levels seen with starvation, acute kidney injury, diarrhea. Normal: BUN 6–20 mg/dL (2.1–7.4 mmol/L). Elevated levels indicate rapid protein catabolism, kidney dysfunction, dehydration. Normal glucose: 70–100 mg/dL (3.9–5.5 mmol/L).
Category: Planning/Physiological Integrity/Reduction of Risk Potential
- Alteration in patterns of urinary elimination—would have altered potassium level
- Fluid volume deficit—CORRECT: elevated sodium level, decreased bicarbonate level, elevated BUN, other values are normal; elevated sodium and BUN levels seen with dehydration
- Nutritional deficit: less than body requirements—would have altered potassium level
- Self-care deficit: feeding—no information to support this
- The Answer is 3
A client is to receive 3,000 mL of normal saline solution IV to infuse over 24 hours. The IV administration set delivers 15 drops per milliliter. The LPN/LVN would expect the flow rate to be how many drops of fluid per minute?
Reworded Question: What should the IV flow rate be?
Strategy: Use the formula and avoid making math errors.
Needed Info: Total volume × the drop factor divided by the total time in minutes
Category: Planning/Physiological Integrity/Pharmacological Therapies
- 21—inaccurate
- 28—inaccurate
- 31—CORRECT: (3,000 × 15) divided by (24 × 60)
- 42—inaccurate
- The Answer is 4
The LPN/LVN is caring for a client diagnosed with asthma. The primary health care provider prescribes neostigmine IM. Which of the following actions by the LPN/LVN is most appropriate?
Reworded Question: Can neostigmine be administered to a client with asthma?
Strategy: “Most appropriate” indicates that discrimination is required to answer the question.
Needed Info: Neostigmine: parasympathomimetic used to treat myasthenia gravis and as an antidote for nondepolarizing neuromuscular blocking agents; potentiates the action of morphine; side effects include nausea, vomiting, abdominal cramps, respiratory depression, bronchoconstriction, hypotension, and bradycardia; nursing considerations include monitor vital signs frequently, have atropine injection available, take with milk.
Category: Evaluation/Physiological Integrity/Reduction of Risk Potential
- Administer the medication, as prescribed—causes bronchoconstriction; notify the primary health care provider
- Obtain the client's blood pressure and pulse—data collection; neostigmine causes hypotension and bradycardia; important to monitor vital signs, but priority is to notify the supervising RN or primary health care provider because medication can precipitate an acute exacerbation of asthma
- Ask pharmacist if the medication can be given orally—medication used cautiously for clients with asthma
- Notify the primary health care provider—CORRECT: cholinergics can cause bronchoconstriction in asthmatic clients; may precipitate an acute exacerbation of asthma
- The Answer is 4
The LPN/LVN is caring for a client with a history of Addison’s disease who has received steroid therapy for several years. The LPN/LVN would expect the client to exhibit which of the following changes in appearance?
Reworded Question: What changes are seen in a client after taking steroids long-term?
Strategy: All the options in an answer choice must be correct for the option to be right.
Needed Info: Medications: cortisone and hydrocortisone usually given in divided doses: 2/3 in morning and 1/3 in late afternoon with food to decrease GI irritation. Reinforce teaching to report S/S of excessive drug therapy (rapid weight gain, round face, fluid retention).
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- Buffalo hump, girdle-obesity, gaunt facial appearance—buffalo hump and girdle-obesity true with long-term steroid use; gaunt face seen with lack of steroids
- Skin tanning, mucous membrane discoloration, weight loss—tanning and weight loss seen with lack of steroids; mucous membrane discoloration not seen
- Emaciation, nervousness, breast engorgement, hirsutism—nothing to do with steroids; hirsutism: excessive growth of hair
- Truncal obesity, purple striations on the skin, moon face—CORRECT: effects of excess glucocorticoids
- The Answer is 1
The LPN/LVN is caring for a client with a history of pancreatic cancer who appears jaundiced. The LPN/LVN should give the highest priority to which of the following needs?
Reworded Question: What is the highest priority for a client with pancreatic cancer?
Strategy: Remember Maslow.
Needed Info: Medical treatment: high-calorie, bland, low-fat diet; small, frequent feedings; avoid alcohol; anticholinergics; antineoplastic chemotherapy
Category: Planning/Physiological Integrity/Reduction of Risk Potential
- Nutrition—CORRECT: profound weight loss and anorexia occur with pancreatic cancer
- Self-image—a client who appears jaundiced clients may be concerned about personal appearance, but physiological needs take priority
- Skin integrity—jaundice causes dry skin and pruritis; scratching can lead to skin breakdown
- Urinary elimination—obstructive process caused by pancreatic cancer darkens urine; kidney function is not affected
- The Answer is 1
An pediatric is seen in a clinic for treatment of attention-deficit/hyperactivity disorder (ADHD). Medication has been prescribed for the client along with family counseling. The LPN/LVN reinforces the teaching plan about the medication and discusses parenting strategies with the parents. Which of the following statements by the parents indicates that further teaching is necessary?
Reworded Question: What information is wrong for a child with ADHD?
Strategy: Be careful! You are looking for incorrect information.
Needed Info: ADHD: developmentally inappropriate inattention, impulsivity, hyperactivity. Treatment: medication, family counseling, remedial education, environmental manipulation (decrease external stimuli), psychotherapy.
Category: Evaluation/Psychosocial Integrity
- “We will give the medication at night so it doesn’t decrease appetite.”—CORRECT: incorrect information; stimulants used; side effects: insomnia, palpitations, growth suppression, nervousness, decreased appetite; give 6 hours before bedtime
- “We will provide a regular routine for sleeping, eating, working, and playing.”—true
- “We will establish firm but reasonable limits on behavior.”—true
- “We will reduce distractions and external stimuli to help concentraton.”—true
- The Answer is 4
The client diagnosed with anorexia nervosa is admitted to the hospital. Which of the following statements by the client requires immediate follow-up by the LPN/LVN?
Reworded Question: Which problem has the highest priority for this client?
Strategy: Remember Maslow’s hierarchy of needs.
Needed Info: Anorexia nervosa: a disorder characterized by restrictive eating resulting in emaciation, disturbance in body image, and an intense fear of being obese. Physical needs must be met first to maintain the client in stable condition. Adequate fluid and electrolyte balance are difficult to maintain.
Category: Planning/Psychosocial Integrity
- “My gums bled this morning.”—vitamin deficiencies may cause bleeding gums, but not the highest priority
- “I’m getting fatter every day.”—body image disturbance occurs in client's diagnosed with anorexia nervosa, but such psychosocial needs do not take priority
- “Nobody likes me, I’m so ugly.”—chronic low self-esteem commonly occurs with anorexia nervosa; this psychosocial need does not take priority
- “I’m feel dizzy and weak today.”—CORRECT: fluid volume deficit takes highest priority; dehydration, a common occurence with anorexia nervosa, could lead to irreversible kidney damage and vital sign instability
- The Answer is 4
A client is admitted to the hospital for treatment of Pneumocystis jiroveci pneumonia and Kaposi’s sarcoma. The client informs the LPN/LVN about a personal decision to become an organ donor. Which of the following responses by the LPN/LVN is best?
Reworded Question: Can this client be an organ donor?
Strategy: Think about each answer choice.
Needed Info: Criteria for organ and tissue donation: no history of significant disease process in organ or tissue to be donated; no untreated sepsis; brain death of donor; no history of extracranial malignancy; relative hemodynamic stability; blood group compatibility; newborn donors must be full-term (more than 200 g); only absolute restriction to organ donation is documented case of human immunodeficiency virus (HIV) disease. Family members can give consent. Nurse can discuss organ donation with other death-related topics (funeral home to be used, autopsy request).
Category: Implementation/Physiological Integrity/Physiological Adaptation
- “What does your family think about your decision?”—client has the right to make the decision
- “You will help many people by donating your organs.”—clients with documented HIV disease are prohibited from donating organs
- “Would you like to speak to the organ donor coordinator?”—passes responsibility for the discussion to the organ donor coordinator
- “Your illness prevents you from becoming an organ donor.”—CORRECT: clients with documented HIV disease are prohibited from donating organs
- The Answer is 3
The LPN/LVN is caring for a client 2 days after a pancreatectomy for cancer of the pancreas. The LPN/LVN observes minimal drainage from the nasogastric (NG) tube. It is most important for the LPN/LVN to take which of the following actions?
Reworded Question: What is the best action when an NG tube is not draining?
Strategy: Determine whether it is appropriate to collect data or implement.
Needed Info: Insertion of NG sump: measure distance from tip of nose to earlobe, plus distance from earlobe to bottom of xyphoid process. Mark distance on tube with tape and lubricate end of tube. Insert tube through nose to stomach. Offer sips of water and advance tube gently; bend head forward. Observe for respiratory distress. Secure with hypoallergenic tape or securement device. Verify tube position initially and before feeding. Aspirate for gastric contents and check appearance and pH.
Category: Data Collection/Physiological Integrity/Basic Care and Comfort
- Notify primary health care provider—should collect data first
- Monitor vital signs every 15 minutes—does not address lack of drainage
- Check the NG tube for kinking—CORRECT: collect data prior to implementing; maintain tubing in a dependent position to promote drainage
- Replace the NG tube immediately—collect data before implementing
- The Answer is 3
The LPN/LVN is planning to administer furosemide 20 mg PO to a client diagnosed with chronic kidney disease. The client asks the LPN/LVN the reason for receiving this medication. Which of the following responses by the LPN/LVN is best?
Reworded Question: Why is furosemide given to a client diagnosed with stage?
Strategy: Think about the action of furosemide.
Needed Info:Chronic kideny disease is progressive, irreversible kidney damage that can be caused by hypertension, diabetes mellitus, lupus erythematosus,or chronic glomerulonephritis; symptoms include anemia, acidosis, azotemia, fluid retention, and urinary output alterations; nursing care includes monitoring potassium levels, daily weight, intake and output, dietary teaching about regulating protein intake, fluid intake to balance fluid losses, and some restrictions of sodium and potassium.
Category: Implementation/Physiological Integrity/Reduction of Risk Potential
- “To increase the blood flow to your kidney.”—Furosemide is a loop diuretic that inhibits sodium and chloride reabsorption at the proximal and distal tubules and the ascending loop of Henle
- “To decrease your circulating blood volume.”—Furosemide used to treat fluid overload due to chronic kidney disease
- “To increase excretion of sodium and water.”—CORRECT: nursing considerations when administering furosemide include monitoring blood pressure, measuring intake and output, monitoring potassium levels; don’t give at hour of sleep
- “To decrease the workload on your heart.”—correcting the fluid overload will decrease the workload on the heart, but the primary reason furosemide is given to clients diagnosed with chronic kidney disease is to augment the kidney’s functioning
- The Answer is 1
The LPN/LVN is reinforcing discharge teaching for a client with Parkinson’s disease. To maintain safety, the LPN/LVN should make which of the following suggestions to the family?
Reworded Question: What is a correct client teaching for Parkinson’s disease?
Strategy: Determine the outcome of each answer choice.
Needed Info: Symptoms: tremors, akinesia, rigidity, weakness, motorized propulsive gait, slurred monotonous speech, dysphagia, drooling, mask-like expression. Nursing care: Encourage finger exercises. Administer antiParkinson's medications. Reinforce teaching of client ambulation modification. Promote family understanding of the disease (intellect/sight/hearing not impaired, disease progressive but slow, doesn’t lead to paralysis). Refer for speech therapy, potential stereotactic surgery.
Category: Implementation/Physiological Integrity/Basic Care and Comfort
- Install a raised toilet seat—CORRECT: helps client maintain independence
- Obtain a hospital bed—no indications that this is needed
- Instruct client to hold arms dependently during ambulation—client should swing arms to maintain balance when walking
- Participate in an exercise program during the late afternoon—activities should be scheduled for late morning when energy level peaks
- The Answer is 3
The LPN/LVN is reinforcing discharge teaching for a client with chronic pancreatitis. Which of the following statements by the client indicates that further teaching is necessary?
Reworded Question: What is an incorrect statement about pancreatitis?
Strategy: This is a negative question; you are looking for incorrect information.
Needed Info: Plan/implementation: nothing by mouth (NPO), gastric decompression. Medications: antacids, analgesics, antibiotics, anticholinergics. Maintain fluid/electrolyte balance. Monitor for signs of infection. Cough and deep-breathe; semi-Fowler’s position. Monitor for shock and hyperglycemia. Treatment of exocrine insufficiency: medications containing amylase, lipase, trypsin to aid digestion. Long-term: avoid alcohol; low-fat, bland diet; small, frequent meals. Monitor S/S of diabetes mellitus.
Category: Evaluation/Physiological Integrity/Reduction of Risk Potential
- “I do not have to restrict physical activity.”—no specific restrictions on activity
- “I should take pancrelipase before meals.”—pancreatic enzyme replacement should be taken before or with meals
- “I will eat three large meals every day.”—CORRECT: small, frequent feedings are most beneficial with chronic pancreatitis
- “I am not allowed to drink any alcoholic beverages.”—chronic pancreatitis requires complete abstinence from alcohol
- The Answer is 3
After a laparoscopic cholecystectomy, the client reports abdominal pain and bloating. Which of the following responses by the LPN/LVN is best?
Reworded Question: What is the best intervention for a client reporting free air pain?
Strategy: “Best” indicates there may be more than one response that appears correct.
Needed Info: Cholecystectomy: removal of gallbladder. T-tube inserted to ensure drainage of bile from common bile duct until edema diminishes. Check amount of drainage (usually 500–1,000 mL/day, decreases as fluid begins to drain into duodenum). Protect skin around incision from bile drainage irritation (use zinc oxide or water-soluble lubricant). Keep drainage bag at same level as gallbladder. Maintain client in semi-Fowler’s position after T-tube removal; observe dressing for bile; notify primary health care provider for significant drainage. Evaluate pain to check for other problems. Monitor for signs of potassium and sodium loss; flattened or inverted T-waves on electrocardiogram; muscle weakness; abdominal distension; headache; apathy; nausea or vomiting; jaundice.
Category: Implementation/Physiological Integrity/Physiological Adaptation
- “Increase intake of fresh fruits and vegetables”—no indication of constipation
- “I’ll give you the prescribed pain medication.”—laparoscopic procedure requires less pain medication than open cholecystectomy
- “Why don’t you take a walk down the hallway?”—CORRECT: carbon dioxide insufflated during laparscopic surgery causes pain; ambulation increases absorption and decreases pain
- “You may need an indwelling urinary catheter.”—carbon dioxide insufflated during laparscopic surgery causes pain; an indwelling urinary catheter does not relieve associated pain
- The Answer is 3
The nursing team consists of an RN, two UAPs, and an LPN/LVN. The LPN/LVN would expect to be assigned to which of the following clients?
Reworded Question: What is a correct client assignment for an LPN/LVN?
Strategy: Think about each answer.
Needed Info: LPN/LVNs care for stable clients with predictable outcomes. Unlicensed assistive personnel (UAPs) perform standard, unchanging procedures.
Category: Implementation/Safe and Effective Care Environment/Coordinated Care
- A client scheduled for an MRI of the brain—requires assessment and teaching; should be cared for by RN
- An unconscious client who requires a bed bath—bed bath for an unconscious client can be assigned to the UAP
- A client in balanced suspension traction—CORRECT: LPN/LVN must care for client; collect data on client airway, adequate respirations, and circulatory status
- A client with diabetes who needs help bathing—UAP can assist with bath
- The Answer is 125
The primary health care provider orders 1 L dextrose 5% in half normal saline solution IV to infuse over 8 hours. The drip factor stated on the IV administration set tubing is 15 gtt/mL. How many milliliters should the LPN/LVN expect to be infused every hour?
Reworded Question: How much fluid needs to infuse every hour to infuse 1,000 mL in 8 hours?
Strategy: Think about the question being asked. Note that there is unnecessary information provided.
Needed Info: One liter is equal to 1,000 milliliters. Dividing the total amount of fluids to infuse by the number of hours in which the infusion should be completed equals hourly fluid amounts.
Category: Planning/Physiological Integrity/Pharmacological Therapies
1 liter = 1,000 mL; 1,000 mL/8 hours = 125 mL/hour
The correct answer is 125.
- The Answer is 1
A client underwent vagotomy with antrectomy for treatment of a duodenal ulcer. Postoperatively, the client develops dumping syndrome. Which of the following statements by the client indicates to the LPN/LVN that further dietary teaching is necessary?
Reworded Question: What is contraindicated for the client with dumping syndrome?
Strategy: Be careful! You are looking for incorrect information.
Needed Info: Antrectomy: surgery to reduce acid-secreting portions of stomach. Delays or eliminates gastric phase of digestion. Dumping syndrome occurs in clients after a gastric resection. It occurs after eating and is related to the stomach's reduced capacity. Undigested food is dumped into the jejunum resulting in distention, cramping, pain, diarrhea 15–30 minutes after eating. Subsides in 6–12 months. S/S 5–30 minutes after eating: vertigo, tachycardia, syncope, diarrhea, nausea. Treatment: sedatives, antispasmodics, high-protein, high-fat, low-carbohydrate, dry diet. Eat in semirecumbent position, lying down after eating.
Category: Evaluation/Physiological Integrity/Reduction of Risk Potential
- “I should eat bread with each meal.”—CORRECT: incorrect information; should decrease intake of carbohydrates
- “I should eat smaller meals more frequently.”—true; 5 to 6 small meals
- “I should lie down right after eating.”—true; delays gastric emptying time
- “I should avoid drinking fluids with my meals.”—true; no fluids 1 hour before, with, or 2 hours after meal
- The Answer is 3
The LPN/LVN reinforces discharge teaching with a client with emphysema. Which of the following statements by the client indicates that teaching was successful?
Reworded Question: What is true about emphysema?
Strategy: Determine the outcome of each answer choice.
Needed Info: Emphysema: chronic progressive respiratory disease caused by destruction of alveolar walls. Complications: acute respiratory infections, heart failure or cor pulmonale, cardiac dysrhythmias. Symptoms: cough, dyspnea, wheezing, barrel chest, use of accessory muscles to breathe. Treatment: bronchodilators, corticosteroids, cromolyn sodium, oxygen, diaphragmatic and pursed-lip breathing maneuvers, energy conservation, diet therapy.
Category: Evaluation/Physiological Integrity/Physiological Adaptation
- “Cold weather should help my breathing problems.”—can exacerbate breathing problems by causing bronchospasms
- “I'll eat three balanced meals daily but limit my fluid intake.”—small, frequent meals should be consumed to increase caloric intake, limit shortness of breath caused by eating; fluids should not be limited because hydration liquefies secretions
- “I'll limit my outside activity when pollution levels are high.”—CORRECT: pollution acts as irritant by causing bronchospasms
- “Intensive exercise should help me regain strength.”—intensive exercise is not tolerated; a conditioning program can help conserve and increase pulmonary ventilation
- The Answer is 3
A client has been taking aluminum hydroxide daily for 3 weeks. The LPN/LVN should be alert for which of the following side effects?
Reworded Question: What is a side effect of aluminum hydroxide?
Strategy: Remember common side effects.
Needed Info: Aluminum hydroxide: antacid that reduces the total amount of acid in the GI tract and elevates the gastric pH level. May cause hypophosphatemia. Shake suspension well and give with milk or water.
Category: Data Collection/Physiological Integrity/Pharmacological Therapies
- Nausea—not common
- Hypercalcemia—seen with calcium-containing antacids; normal calcium 8.5–10.5 mg/dL (2.3–2.6 mmol/L)
- Constipation—CORRECT: may need laxatives or stool softeners
- Anorexia—not common
- The Answer is 3
The LPN/LVN is hearing a client call for help. The LPN/LVN enters the room and finds a client in bilateral wrist restraints with a cool, pale right hand and no palpable radial pulse. Which of the following would be the most appropriate action for the LPN/LVN to take first?
Reworded Question: What is the priority response to this situation?
Strategy: Think ABCs and about the risk restraints pose to circulation.
Needed Info: Loss of circulation: loss of all or part of a limb can occur in as little as 15 minutes when blood flow is absent.
Category: Planning/Safe and Effective Care Environment/Safety and Infection Control
- Leave to find the client’s nurse—this delays the immediate intervention required to protect the hand
- Massage the client’s wrist and hand—does not address the cause of the impaired hand circulation, delays intervention
- Remove the right wrist restraint—CORRECT: provides the most immediate and effective way to help return circulation to the wrist and hand; the LPN/LVN can call for help and turn on the client’s call light for further assistance and assessment
- Reposition the client to reduce pressure—does not address the cause of the impaired hand circulation, delays intervention
- The Answer is 4
The LPN/LVN is reinforcing discharge teaching for a client with a new colostomy. The LPN/LVN knows teaching was successful when the client chooses which of the following menu options?
Reworded Question: What is the appropriate diet for a client with a colostomy?
Strategy: Recall the type of diet required and then select the menu that is appropriate.
Needed Info: Diet: a low-residue diet for 4–6 weeks postoperatively, avoiding gas-forming, odor-producing, or excessively laxative or constipating foods.
Category: Evaluation/Physiological Integrity/Reduction of Risk Potential
- Sausage, sauerkraut, baked potato, and fresh fruit—sausage and sauerkraut are gas-producing and should be avoided with a new colostomy
- Cheese omelet with bran muffin and fresh pineapple—bran muffin and fresh fruit are high-fiber (residue)
- Pork chop, mashed potatoes, turnips, and salad—turnips are odor-causing and salad is high-residue
- Baked chicken, boiled potato, cooked carrots, and yogurt—CORRECT: provides balanced nutrition, high protein, low residue, low fat, and nonirritating foods
- The Answer is 4
A client is admitted to the unit wih suspected acute kidney injury. The LPN/LVN would be most concerned if the client made which of the following statements?
Reworded Question: What is a symptom of acute renal failure?
Strategy: “Most concerned” indicates you are looking for a symptom of acute kidney injury.
Needed Info: Symptoms of oliguric phase of acute kidney injury: urinary output less than 400 mL/day; irritability, drowsiness, confusion, coma; restlessness, twitching, seizures; hyperkalemia, increased blood urea nitrogen (BUN) and creatinine levels, hypercalcemia, hypernatremia, increased pH; anemia; pulmonary edema, heart failure, hypertension. Symptoms of diuretic or recovery phase: urinary output of 4–5 L/day; increased serum BUN; potassium and sodium loss in urine; increased mental and physical activity.
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- “My urine often appears pink-tinged.”—seen with urinary tract infections (UTI) or trauma; hematuria not usually a symptom of acute kidney injury
- “It is hard for me to start the flow of urine.”—urinary hesitancy seen with UTI, not usually seen with acute kidney injury
- “It is quite painful for me to urinate.”—dysuria seen with UTI, not with acute kidney injury
- “I urinate in the morning and again before dinner.”—CORRECT: symptoms of acute kidney injury include decreased urinary output (anuria or ologuria), hypotension, tachycardia, lethargy; normal output 1,200–1,500 mL/day or 50–63 mL/hr, normal voiding pattern 5–6 times/day and once at night
- The Answer is 2
The LPN/LVN is implementing the protocol for teaching a new mother how to breastfeed her newborn. The LPN/LVN knows that teaching has been successful if the client makes which of the following statements?
Reworded Question: What indicates that a newborn is receiving adequate nutrition when breastfeeding?
Strategy: Think about each statement. Is it true?
Needed Info: Breastfeeding is recommended for first 6–12 months of life; human milk is considered ideal food. Colostrum is secreted at first; clear and colorless; contains protective antibodies; high in protein and minerals. Milk is secreted after 2–4 days; milky white appearance; contains more fat and lactose than colostrum.
Category: Evaluation/Health Promotion and Maintenance
- “My baby’s weight should equal her birthweight in 5 to 7 days.”—breastfeeding infants should surpass birthweight in 10–14 days
- “My baby should have at least 6 to 8 wet diapers per day.”—CORRECT: indicates newborn adequately hydrated and therefore, ingesting adequate nutrition
- “My baby will sleep at least 6 hours between feedings.”—newborns feed approximately every 2 to 3 hours during the day and every 4 hours at night
- “My baby will feed for about 10 minutes per feeding.”—should feed for approximately 15–20 minutes per breast
- The Answer is 2
A client is admitted to the telemetry unit for evaluation of reported chest pain. Eight hours after admission, the client's cardiac monitor shows ventricular fibrillation. The primary health care provider defibrillates the client. The LPN/LVN understands that the purpose of defibrillation is to do which of the following?
Reworded Question: Why is a client defibrillated?
Strategy: Think about each answer choice.
Needed Info: Defibrillation: delivers an electrical current to the heart that depolarizes myocardial cells. When the cells repolarize, the sino-atrial (SA) node commonly recaptures its role as the heart's pacemaker.
Category: Implementation/Physiological Integrity/Physiological Adaptation
- Increase cardiac contractility, preload, and cardiac output—inaccurate
- Depolarize cells allowing SA node to recapture pacing node—CORRECT: electrical current delivered to the heart depolarizes myocardioal cells allowing the SA node to recapture its pacing role
- Reduce the degree of cardiac ischemia and acidosis—inaccurate
- Provide electrical energy for depleted myocardial cells—inaccurate
- The Answer is 3
The LPN/LVN is caring for a client who suddenly reports chest pains. The LPN/LVN knows that which of the following symptoms would be most characteristic of an acute myocardial infarction (MI)?
Reworded Question: What type of pain is characteristic in an MI?
Strategy: Think about the cause of each type of pain.
Needed Info: MI signs and symptoms: chest pain radiating to neck, jaw, shoulder, back, or left arm; unrelieved by nitroglycerin. Also fever, apprehension, dizziness, diaphoresis, palpitations, shortness of breath.
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- Intermittent, localized epigastric pain—indicates GI disorder
- Sharp, localized, unilateral chest pain—symptoms of pneumothorax
- Severe substernal pain radiating down the left arm—CORRECT: pain may be crushing; radiate; unrelated to emotion or exercise
- Sharp, burning chest pain moving from place to place—may be caused by anxiety
- The Answer is 1
The primary health care provider prescribes packing for a nonhealing open surgical wound. Which of the following is the first action by the LPN/LVN?
Reworded Question: Which first step is important prior to packing a wound?
Strategy: Determine what you need to know about the wound and dressing. “First action” indicates priority.
Needed Info: Must observe a wound to properly care for the wound and client. Observation allows the nurse to determine what materials are needed, whether another person will be needed to provided assistance, and whether the client will require pain medication prior to the dressing change. Open wounds require sterile technique.
Category: Planning/Safe and Effective Care Environment/Safety and Infection Control
- Identify wound size, shape, and depth—CORRECT: it is necessary to observe the wound to adequately prepare for a dressing change and select appropriate dressing materials
- Observe for wound drainage or discharge—this is necessary, but not the first step
- Plan to set up for clean technique—an open wound requires sterile, not clean, technique
- Select the proper dressing material—this is a safe and expected practice, but not the first step
- The Answer is 2
A client returns to the clinic 2 weeks after hospital discharge. The client is taking wafarin sodium 2 mg PO daily. Which of the following statements by the client to the LPN/LVN indicates that further teaching is necessary?
Reworded Question: What is contraindicated for warfarin?
Strategy: Think about what each statement means and how it relates to warfarin.
Needed Info: Warfarin sodium: anticoagulant. Side effects: hemorrhage, fever, rash. Prothrombin time (PT) used to monitor effectiveness; PT usually maintained at 1.5–2 times normal. Antidote: vitamin K (aquamephyton). Nursing responsibilities: check for bleeding gums, bruises, nosebleeds, petechiae, melena, tarry stools, hematuria. Use electric razor, soft toothbrush; provide green leafy vegetables (contain vitamin K).
Category: Evaluation/Physiological Integrity/Pharmacological Therapies
- “I take an antihistamine before bedtime..”—no contraindication
- “I take aspirin whenever I have a headache.”—CORRECT: inhibits platelet aggregation increasing the risk for bleeding; avoid use with warfarin
- “I put on sunscreen whenever I go outside.”—correct behavior
- “I take an antacid if my stomach gets upset.”—correct information
- The Answer is 3
To enhance the percutaneous absorption of nitroglycerin ointment, it would be most important for the LPN/LVN to select a site that is which of the following?
Reworded Question: What is the best site for nitroglycerin ointment?
Strategy: Think about each site.
Needed Info: Nitroglycerin: used in treatment of angina pectoris to reduce ischemia and relieve pain by decreasing myocardial oxygen consumption; dilates veins and arteries. Side effects: throbbing headache, flushing, hypotension, tachycardia. Nursing responsibilities: teach appropriate administration, storage, expected pain relief, side effects. Ointment applied to skin; sites rotated to avoid skin irritation. Prolonged effect up to 24 hours.
Category: Implementation/Physiological Integrity/Pharmacological Therapies
- Muscular—not most important
- Near the heart—not most important
- Non-hairy—CORRECT: skin site free of hair will increase absorption; avoid distal part of extremities due to less-than-maximal absorption
- Bony prominence—most important is that the site be non-hairy since hair interferes with absorption
- The Answer is 3
When assisting the RN in planning care for a postoperative client, which of the following should be the first choice of the LPN/LVN to reduce the client’s risk for pooled airway secretions and decreased chest wall expansion?
Reworded Question: What respiratory intervention is the easiest and most cost-effective to implement?
Strategy: Identify standards of care to prevent respiratory complications for all hospitalized clients.
Needed Info: Causes of respiratory complications in the hospital setting: decreased mobility or immobility of acutely ill clients. To prevent potential complications: frequently reposition clients from side to side, get clients out of bed to a chair, assist clients to ambulate. These actions are cost-effective, easy, and standard practice.
Category: Planning/Physiological Integrity/Basic Care and Comfort
- Chest percussion—not necessary for the majority of clients and requires nursing staff or respiratory therapy intervention
- Incentive spirometry—not necessary for the majority of clients, adds cost to care and requires a piece of equipment issued to the client
- Position changes—CORRECT: can be encouraged and accomplished easily for all clients without any additional expense for equipment or staff
- Postural drainage—not necessary for the majority of clients and requires nursing staff or respiratory therapy intervention
- The Answer is 2
Which of the following actions by the LPN/LVN would be most helpful in preventing injury to elderly clients in a health care facility?
Reworded Question: What is the most frequent cause of injury for the elderly in a health care facility?
Strategy: Think about the primary injury category for the elderly.
Needed Info: Statistically, falls are the most frequent cause of injury for the hospitalized or institutionalized elderly adult. Must protect clients/residents from falls.
Category: Planning/Safe and Effective Care Environment/Safety and Infection Control
- Closely monitor the temperature of hot oral fluids—necessary, but not the most frequent cause of injury
- Keep unnecessary furniture out of the way—CORRECT: falls are the most common cause of injury, and maintaining an uncluttered environment can help prevent falls
- Maintain the safe function of all electrical equipment—necessary, but not the most frequent cause of injury
- Use safety protection caps on all medications—necessary, but bottles of medication should not be accessible to clients
- The Answer is 4
Which of the following statements by a client during a group therapy session requires immediate follow-up by the LPN/LVN?
Reworded Question: Which statement indicates the possibility of impending danger?
Strategy: Think about which statement would make you question the client’s intentions.
Needed Info: In Tarasoff v. The Regents of the University of California (1976), the court established a duty to warn of threats of harm to others. Failure to warn, coupled with subsequent injury to the threatened person, exposes the mental health professional to civil damages for malpractice. Based on this and other rulings in many states, the mental health caregiver must take responsibility to warn society of potential danger.
Category: Implementation/Psychosocial Integrity
- “I know I’m a chronically compulsive liar, but I can’t help it.”—this statement is revealing, but does not indicate impending threat
- “I don’t ever want to go home; I feel safer here.”—this statement is a response to anxiety or fear, but does not indicate immediate danger
- “I don’t really care if I ever see my girlfriend again.”—this statement does not imply a threat or impending violence
- “I’ll make sure that doctor is sorry for what he said.”—CORRECT: under the Tarasoff Act, a threatened person, including health professionals, must be warned about threats or potential threats to personal safety
- The Answer is 4
A client newly diagnosed with major neurocognitive disorder (NCD) due to Alzheimer’s disease is admitted to the unit. Which of the following actions by the LPN/LVN is best?
Reworded Question: What is appropriate care for a client with Alzheimer’s disease?
Strategy: Determine whether to collect data or implement.
Needed Info: Alzheimer’s disease: chronic, progressive, degenerative, resulting in cerebral atrophy. S/S: changes in memory, confusion, disorientation, change in personality; most common after age 65. Nursing responsibilities: reorient as needed; speak slowly; place clocks and calendars in room; place bed in low position with side rails up.
Category: Data Collection/Psychosocial Integrity
- Place the client in a semi-private room away from the nurses’ station—should be in a semi-private room near nurses’ station; needs frequent monitoring
- Ask family members to wait in the waiting room during the admission process—familiar people decrease confusion of unfamiliar environment
- Assign a different nurse daily to care for the client—consistency is important
- Ask the client to state the current date—CORRECT: data collection is the first step in planning care
- The Answer is 3
A female client visits the clinic reporting right calf tenderness and pain. It would be most important for the LPN/LVN to ask which of the following questions?
Reworded Question: What is a predisposing factor to developing deep vein thrombosis (DVT)?
Strategy: Determine why you would ask each question.
Needed Info: Thrombophlebitis (phlebitis, phlebothrombosis, or DVT): clot formation in a vein secondary to inflammation of vein or partial vein obstruction. Risk factors: history of varicose veins, hypercoagulation, cardiovascular disease, pregnancy, oral contraceptives, immobility, recent surgery, or injury.
Category: Data Collection/Physiological Integrity/Pharmacological Therapies
- “Do you exercise excessively?”—excessive exercise could cause shin splints
- “Have you had any recent fractures?”—not relevant to client’s reported symptoms
- “What type of birth control do you use?”—CORRECT: increased risk of DVT with oral contraceptives
- “Are you under a lot of stress?”—should be concerned about possibility of DVT
- The Answer is 1
Which of the following should be the LPN/LVN’s first priority in providing care for a client who has end-stage ovarian cancer and has been weakened by chemotherapy?
Reworded Question: What is the most important information needed regarding this client?
Strategy: Think about basic needs of every client. Remember Maslow’s hierarchy of needs.
Needed Info: Maslow’s hierarchy of basic human needs: physiological needs must be met before higher-level needs of safety and security, love and belonging, self-esteem, and self-actualization. Untreated pain affects all other physiological needs: oxygenation, food and fluid intake, elimination, ability to rest and sleep, comfort, and activity level.
Category: Planning/Physiological Integrity/Basic Care and Comfort
- Collect data to see if client has pain—CORRECT: collecting data to see if the client has pain enables the LPN/LVN to plan for the client's pain management needs
- Determine if the client is hungry or thirsty—important physiological needs that are difficult to meet for a client in pain
- Explore the client’s feelings about dying—important psychological safety and security need that is difficult to meet for a client in pain
- Observe the client’s self-care abilities—important safety and security need that is difficult to meet for a client in pain
- The Answer is 2
The LPN/LVN in the postpartum unit is caring for a client who delivered her first child the previous day. The LPN/LVN notes multiple varicosities on the client’s lower extremities. Which of the following actions should the LPN/LVN perform?
Reworded Question: What is the best way to prevent thrombophlebitis?
Strategy: Think about what causes thrombophlebitis.
Needed Info: high-risk of developing thrombophlebitis during pregnancy and immediate postpartum period. Thrombophlebitis: inflammation of vein associated with formation of a thrombus or blood clot. Other risk factors: prolonged immobility, use of oral contraceptives, sepsis, smoking, dehydration, and heart failure. S/S: pain in the calf, localized edema of one extremity, positive Homans’ sign (pain in calf when foot is dorsiflexed). Treatment: bed rest and elevation of extremity, anticoagulant (heparin).
Category: Planning/Health Promotion and Maintenance
- Teach the client to rest in bed when the baby sleeps—not preventive; bed rest can cause thrombophlebitis
- Encourage early and frequent ambulation—CORRECT: facilitates emptying of blood vessels in lower extremities
- Apply warm soaks for 20 minutes every 4 hours—not a preventive measure but an intervention used to treat; must be ordered by primary health care provider
- Perform passive range-of-motion (ROM) exercises 3 times daily—early ambulation more effective; passive ROM retains joint function, maintains circulation; passive exercises: no assistance from client
- The Answer is 2
The LPN/LVN is caring for a client who sustained a left femur fracture in a bicycle accident. A cast is applied. The nurse knows that which of the following exercises would be most beneficial for this client?
Reworded Question: What exercise is best for a client in a cast?
Strategy: Picture the client as described. Imagine client performing each type of exercise. Also think about the key words “Most beneficial.”
Needed Info: Fracture: break in continuity of bone. Complications: hemorrhage (bone vascular), shock, fat embolism (long bones), sepsis, peripheral nerve damage, delayed union, nonunion. Treatment: reduction (closed or open), immobilization (cast, traction, splints, internal and external fixation). Cast allows early mobility. Nursing responsibilities: teach isometric exercises.
Category: Planning/Physiological Integrity/Reduction of Risk Potential
- Passive exercise of the affected limb—nurse moves extremity; unable to perform with cast in place
- Quadriceps setting of the affected limb—CORRECT: isometric exercise: contraction of muscle without movement of joint; maintains strength in the affected limb
- Active range-of-motion exercises of the unaffected limb—not best, doesn't strengthen affected limb
- Passive exercise of the upper extremities—need strengthening exercises, not passive exercises
- The Answer is: See Answers and Explanations
In preparation for a dressing change, the LPN/LVN puts on sterile gloves. Where should the LPN/LVN initially grip the first sterile glove?
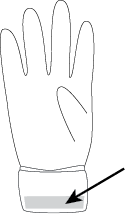
Reworded Question: What is the correct procedure for applying sterile gloves?
Strategy: Remember what part of the glove must remain sterile.
Needed Info: Absolutely necessary for the first glove of the pair to be donned in the proper fashion. Grasp the top end of the folded cuff without touching any part of the rest of the sterile glove to avoid contamination from nonsterile hands.
Category: Implementation/Safe and Effective Care Environment/Safety and Infection Control
- The Answer is 2
A client is being discharged from the hospital following a right total hip arthroplasty. The LPN/LVN reinforces discharge teaching. Which of the following statements by the client would indicate that teaching was successful?
Reworded Question: What should a client do after a total hip arthroplasty?
Strategy: Determine which movements bring the right hip toward the median plane of the body (adduction).
Needed Info: Adduction: movement toward the median plane or midline of the body. Adduction precautions implemented to prevent hip dislocation: legs may not be crossed at knees or ankles, knees must be separated (most often with a special pillow). No hip flexion beyond 90 degrees.
Category: Planning/Physiological Integrity/Basic Care and Comfort
- “I can bend over to pick up something on the floor.”—this describes flexion, not adduction. It is not allowed for total hip arthroplasty clients
- “I should not cross my ankles when sitting in a chair.”—CORRECT: even though the client is only crossing the legs at the ankles, the leg is adducted
- “I need to lie on my stomach when sleeping in bed.”—the prone position does not necessarily adduct the hip
- “I should spread my knees apart to put on my shoes.”—this movement abducts the hip
- The Answer is 725
The LPN/LVN is caring for a client with continuous bladder irrigation. At 7 a.m., the LPN/LVN notes 4,200 mL of normal saline solution left in the irrigation bags. During the next shift (7 a.m. to 3 p.m.), the LPN/LVN hangs another 3,000 mL and empties a total of 5,625 mL from the urine drainage bag. At 3 p.m., there are 2,300 mL of irrigant left hanging. What is the actual urine output for the client from 7 a.m. to 3 p.m.?
Reworded Question: After subtracting the irrigant, what is the client’s urinary output?
Strategy: Calculate irrigant used and subtract it from total fluid output to determine urinary output.
Needed Info: Accurate measurement of urinary output is critical. Subtract the irrigant used from the total fluid output to determine the urinary output.
Category: Implementation/Physiological Integrity/Basic Care and Comfort
The irrigant infused was 4,200 mL left at the beginning of the shift + 3,000 mL added − 2,300 mL remaining at the end of the shift = 4,900 mL infused as irrigant. Total output from the catheter bag was 5,625 mL − 4,900 mL of irrigant infused = 725 mL of urine as output.
The correct answer is 725.
- The Answer is 1
The LPN/LVN is observing activities on a medical/surgical unit. The LPN/LVN should intervene if which of the following is observed?
Reworded Question: What will cause the spread of infection?
Strategy: “Should intervene” indicates an incorrect action.
Needed Info: Standard precautions are used to prevent exposure to blood and body fluids infections; perform hand hygiene as soon as gloves are removed, between client contacts, between procedures or tasks with same client; wear gloves when touching blood, body fluids, or contaminated surfaces; masks, goggles, and gown if splashing is likely.
Category: Evaluation/Safe and Effective Care Environment/Safety and Infection Control
- A client’s family member disposes of the client's used tissue in the bedside container before opening the roommate’s milk carton—CORRECT: contaminated hands cause cross-contamination; instruct family about hand hygiene
- An UAP removes gloves and washes hands for 15 seconds after emptying an indwelling urinary catheter—perform hand hygiene after removing gloves
- An LPN/LVN puts on a gown, gloves, mask, and goggles prior to inserting a nasogastric tube—appropriate technique; splashes may occur
- A visitor talks with a client diagnosed with methicillin-resistant Staphylococcus aureus (MRSA) wound infection while eating lunch—client in isolation may develop sense of loneliness; visiting with client during meals increases sensory stimulation
- The Answer is 3
A client with a history of type 1 diabetes mellitus is admitted to the unit reporting nausea, vomiting, and abdominal pain. The client reduced the insulin dose four days ago when influenza symptoms prevented eating The LPN/LVN observes poor skin turgor, dry mucous membranes, and fruity breath odor. The LPN/LVN should be alert for which of the following problems?
Reworded Question: What do these symptoms indicate?
Strategy: Think about each answer choice.
Needed Info: Diabetes mellitus: disorder of carbohydrate metabolism: insufficient insulin to meet metabolic needs. Type 1 diabetes mellitus: insulin dependent, prone to diabetic ketoacidosis. Type 2 diabetes mellitus: controlled by diet and oral antidiabetic agents, not prone to ketosis. In ketoacidosis, the body becomes dehydrated from osmotic diuresis. The fruity breath odor develops from acetone, a component of ketone bodies. Rate and depth of respiration increase (Kussmaul) in attempt to blow off excess carbonic acid. Hyperosmolar nonketonic syndrome (HHNS)—lacks ketonuria.
Category: Planning/Physiological Integrity/Reduction of Risk Potential
- Rebound hypoglycemia—cause: too much insulin after a period of hyperglycemia; blood glucose level falls below 60 mg/dL (3.3 mmol/L); S/S: tachycardia, perspiration, confusion, lethargy, numb lips, anxiety, hunger
- Viral gastrointestinal illness—may produce similar symptoms, not best answer based on client history
- Diabetic ketoacidosis—CORRECT: cause: insufficient insulin; S/S: polyuria, polydipsia, nausea, vomiting, dry mucous membranes, weight loss, abdominal pain, hypotension, shock, coma
- Hyperglycemic hyperosmolar nonketotic syndrome— extreme hyperglycemia (800–2,000 mg/dL [44.4–111 mmol/L]) with absence of acidosis; some insulin production, don’t mobilize fats for energy or form ketones; usually with type 2 diabetes; cause: infections, stress, medications (steroids, thiazide diuretics), total parenteral nutrition; S/S: polyphagia, polyuria, polydipsia, glycosuria, dehydration, abdominal discomfort, hyperpyrexia, changes in level of consciousness (LOC), hypotension, shock; treatment: fluid and electrolyte replacement, insulin given IV
- The Answer is 1
The LPN/LVN is caring for a group of clients. The nurse knows that it is most important for which of the following clients to receive scheduled medications on time?
Reworded Question: Which medication, if given late, might cause harm to the client?
Strategy: Think about each answer.
Needed Info: Myasthenia gravis is deficiency of acetylcholine at myoneural junction; symptoms include muscular weakness produced by repeated movements that soon disappears following rest, diplopia, ptosis, impaired speech, and dysphagia.
Category: Planning/Physiological Integrity/Pharmacological Therapies
- A client diagnosed with myasthenia gravis receiving pyridostigmine bromide—CORRECT: Pyrostigmine bromide is a cholinesterase inhibitor, which increases acetylcholine concentration at the neuromuscular junction; early administration can precipitate a cholinergic crisis; late administration can precipitate myasthenic crisis
- A client diagnosed with bipolar disorder receiving lithium carbonate—Lithium carbonate is a mood stabilizer; targeted blood level = 1–1.5 mEq/L (1–1.5 mmol/L)
- A client diagnosed with tuberculosis receiving isonicotinic acid hydrazide—Isonicotinic acid hydrazide (INH) is given in a single daily dose; side effects include hepatitis, peripheral neuritis, rash, and fever
- A client diagnosed with Parkinson’s disease receiving levodopa—Levodopa is thought to restore dopamine levels in extrapyramidal centers; sudden withdrawal can cause parkinsonian crisis; priority is to administer pyrostigmine bromide
- The Answer is 3
An school-age client is admitted to the hospital for evaluation for a kidney transplant. The LPN/LVN learns that the client received hemodialysis for 3 years due to stage 5 kidney disease. The LPN/LVN knows that the illness can interfere with this client’s achievement of which of the following?
Reworded Question: What developmental stage is altered in a client due to this chronic disease?
Strategy: Picture the person described in the question. Think about his activities and interests. This helps eliminate incorrect answer choices. A school-age client may be thinking about homework, or doing chores at home.
Needed Info: Eric Erikson developed a theory of the stages of personality development that progressed in predictable stages from birth to death. Other stages: autonomy versus shame and doubt (task of 1–3 yrs); initiative versus guilt (task of 3–6 yrs).
Category: Planning/Health Promotion and Maintenance
- Intimacy—young adult: 20–40 yrs; achieving sexual and loving relationship with another; alternative: isolation
- Trust—infancy; results from consistent care by a loving caretaker; teaches that basic needs will be met; alternative: mistrust
- Industry—CORRECT: 6–12 yrs; aspires to be the best; learns social skills, how to finish tasks; sensitive about school expectations; may be impaired due to absences from school, growth retardation, and emotional difficulties
- Identity—adolescence; peer groups important; used to define identity, establish body image, form new relationships; alternative: role diffusion
- The Answer is 2, 3, 5, and 6
The LPN/LVN notes that a client has an unsteady gait. The LPN/LVN should do which of the following? Select all that apply.
Reworded Question: What safety measures are appropriate for a client who is unsteady on his or her feet?
Strategy: Identify nonrestrictive safety measures.
Needed Info: Safety measures to help prevent falls include: rubber-soled (nonskid) shoes, removal of obstacles and clutter, a method of summoning the help of the nursing staff, assistance when out of bed, adequate lighting, safety bars and hand rails, and adaptive equipment including walkers and raised toilet seats as appropriate.
Category: Implementation/Safe and Effective Care Environment/Safety and Infection Control
- Apply a chest or vest restraint at night—restrictive and false imprisonment without a primary health care provider's orders
- Help the client put on nonskid shoes for walking—CORRECT: a choice that decreases fall risk without restricting the client
- Keep the call light within the client’s reach—CORRECT: not restrictive and addresses the client’s need to call for assistance when getting out of bed
- Lower the bed and raise all four side rails—lowering the bed is appropriate, but raising all the side rails only increases the height from which a client may fall while climbing over the side rails
- Provide adequate lighting in room and bathroom—CORRECT: allows client to assess an unfamiliar hospital environment
- Remove obstacles and room clutter—CORRECT: provides clear access to room and bathroom
- The Answer is 2
Haloperidol 5 mg PO tid is prescribed for a client with schizophrenia. Two days later, the client reports “tight jaws and a stiff neck.” The LPN/LVN should recognize that these complaints are which of the following?
Reworded Question: Why does the client taking haloperidol have these symptoms?
Strategy: Think about each answer choice.
Needed Info: Haloperidol, antipsychotic agent used to treat psychotic disorders. High incidence of extrapyramidal reactions: pseudoparkinsonism (rigidity and tremors), akathisia (motor restlessness), dystonia (involuntary jerking, of muscles, acute muscular rigidity and cramping), tardive dyskinesia (abnormal movements of lips, jaws, tongue). Schizophrenia: retreat from reality, flat affect, suspiciousness, hallucinations, delusions, loose associations, psychomotor retardation or hyperactivity, regression. Nursing responsibilities: maintain safety, meet physical needs, decrease sensory stimuli. Treatment: antipsychotic medications, individual therapy.
Category: Evaluation/Physiological Integrity/Pharmacological Therapies
- Common side effects of antipsychotic medications that will diminish over time—gets worse, untreated, life-threatening
- Early symptoms of extrapyramidal reactions to the medication—CORRECT: dystonic reaction, airway may become obstructed
- Psychosomatic symptoms resulting from a delusional system—not accurate
- Permanent side effects associated with haloperidol therapy—reversible when treated with IV diphenhydramine hydrochloride
- The Answer is 4
A client is receiving a continuous gastric tube feeding at 100 mL per hour. The LPN/LVN checks for gastric residual volume and finds 90 mL in the client’s stomach. Which action should the LPN/LVN take?
Reworded Question: What are the standards and procedures for gastric residual volume from a gastric tube feeding?
Strategy: Think about electrolyte balance and gastric emptying.
Needed Info: Standard procedures for clients receiving continuous tube feedings: gastric residual volume and tube placement checked every 4 hours, position clients with head of bed elevated at least 30 degrees. To promote normal function: gastric residual volume with associated gastric enzymes and hydrochloric acid should be returned to the stomach when gastric residual volume measures under 150 mL, feeding should be stopped if the gastric residual volume is over 50% of the volume fed over the last 1 hour.
Category: Physiological Integrity/Basic Care and Comfort/Analysis
- Discard the gastric residual volumel and continue the tube feeding—gastric residual volume under 150 mL should be returned to the stomach to maintain electrolyte balance; the feeding should be stopped because the gastric residual volume exceeds 50% of the volume fed over 1 hour
- Discard the gastric residual volume and stop the tube feeding—return the gastric residual volume and stop the feeding
- Return the gastric residual volume and continue the tube feeding—return the gastric residual volume and stop the feeding
- Return the gastric residual volume and stop the tube feeding—CORRECT: residuals less than 150 mL should be returned to the stomach to maintain electrolyte balance; the feeding should be stopped because the gastric residual volume exceeds 50% of the volume fed over 1 hour
- The Answer is 4
The LPN/LVN opens several sterile gauze dressings on the client’s over-the-bed table. The LPN/LVN knows that the sterile dressings will be contaminated if she does which of the following?
Reworded Question: What is incorrect sterile technique?
Strategy: List the basic principles of sterile technique.
Needed Info: To maintain sterility of sterile objects: may only touch other sterile objects, must remain in the LPN/LVN’s view, must be above the LPN/LVN’s waist, cannot be exposed to air for prolonged periods, must be located inside the 1-inch (2.5 cm) border of a sterile field or within the dressing packaging borders, sterile fluids must not contact a nonsterile object when fluids flow with gravity. The client’s over-the-bed table is not sterile.
Category: Evaluation/Safe and Effective Care Environment/Safety and Infection Control
- Does not allow the dressings prolonged exposure to the air—a principle of sterile technique
- Keeps sterile dressings inside border of the sterile packaging—a principle of sterile technique
- Positions top of the over-the-bed table at or above waist level—a principle of sterile technique
- Pours sterile saline onto the opened sterile dressing on table —CORRECT: capillary action and gravity lead to contamination of the sterile object because of contact between the nonsterile over-the-bed table and the once-sterile fluid
- The Answer is 3
A client has adamantly refused hygiene measures over the past 3 days. Eventually the LPN/LVN was able to collaborate with the client to develop the hygiene goal: “self-administration of a complete bath daily while in the hospital.” To evaluate if this goal is achieved, the LPN/LVN should do which of the following?
Reworded Question: What is the most objective method to evaluate goal attainment of a psychomotor skill?
Strategy: Identify how you can best objectively determine if the client did bathe.
Needed Info: Goals and expected outcomes of nursing process provide the focus for the effectiveness of the planned nursing interventions. To validate that a goal has been met, measurable criteria are needed.
Category: Evaluation/Physiological Integrity/Basic Care and Comfort
- Ask the client whether self-bathing was accomplished—asking the client about bathing is not measurable and may not always be reliable
- Bathe the client to be sure the hygiene goal is met—this does not support the goal of a self-administered bath
- Observe the client performing portions of the daily bath—CORRECT: direct observation provides the LPN/LVN with objective measurable data that the client has met the goal
- Remind the client to bathe and provide the needed supplies—places all the responsibility on the client and does not actively create client compliance
- The Answer is 1
The LPN/LVN is caring for a client in labor. The primary health care provider palpates a firm, round form in the uterine fundus, small parts on the client’s right side, and a long, smooth, curved section on the left side. Based on these findings, where should the LPN/LVN anticipate auscultating the fetal heart tones?
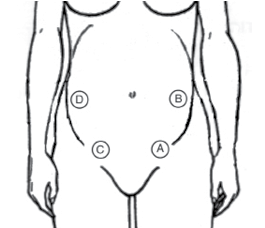
Reworded Question: If a fetus is LOA, where should the nurse listen for the fetal heart tone?
Strategy: Examine the diagram carefully. Know the woman’s right from left.
Needed Info: Fetal reference point: Vertex presentation—dependent upon degree of flexion of fetal head on chest; full flexion/occiput (O), full extension chin (M), moderate extension (military) brow (B). Breech presentation-sacrum (S). Shoulder presentation-scapula (SC). Maternal pelvis is designated per her right/left and anterior/posterior. Position = relationship of fetal reference point to mother’s pelvis; expressed as standard 3—letter abbreviation: left occiput anterior (LOA) (most common), left occiput posterior (LOP), right occiput anterior (ROA), right occiput posterior (ROP), left occiput transverse (LOT), right occiput transverse (ROT).
Category: Planning/Health Promotion and Maintenance
- A—CORRECT: point of maximum intensity for fetal heart tones with fetus in LOA position
- B—PMI location for fetus in LOP position
- C—PMI location for fetus in ROA position
- D—PMI location for fetus in ROP position
- The Answer is 4
When completing data collection of an immobilized client, the LPN/LVN knows that edema is commonly observed in which of the following locations?
Reworded Question: Where does dependent edema occur in an immobile client? What position is the immobilized client usually in?
Strategy: Identify where dependent edema is likely to settle due to gravity in a client supine.
Needed Info: Immobile clients: most often horizontal in bed, gravity would cause fluid pooling at the most dependent place, namely, the sacrum. Mobile clients: fluids pool in dependent areas such as their feet and ankles.
Category: Data Collection/Physiological Integrity/Basic Care and Comfort
- Abdomen—not a likely place for dependent edema
- Feet and ankles—a primary place for edema in a client who is sitting up or out of bed walking
- Fingers and wrists—not a likely place to initially find dependent edema
- Sacrum—CORRECT: gravity causes dependent edema to develop at the sacrum in immobile clients
- The Answer is 1
A client is preparing to take her 1-day-old infant home from the hospital. The LPN/LVN discusses the test for phenylketonuria (PKU) with the client. The LPN/LVN’s reinforcement of teaching should be based on an understanding that the test is most reliable in which of the following circumstances?
Reworded Question: When is the PKU test most reliable?
Strategy: Focus on the key words in the question. Think about what you know about the PKU test.
Needed Info: PKU: genetic disorder caused by a deficiency in liver enzyme phenylalanine hydroxylase. Body can’t metabolize essential amino acid phenylalanine, allows phenyl acids to accumulate in the blood. If not recognized, resultant high levels of phenyl ketone in the brain cause intellectual disability. Guthrie test: screening for PKU. Treatment: dietary restriction of foods containing phenylalanine. Blood levels of phenylalanine monitored to evaluate the effectiveness of the dietary restrictions.
Category: Implementation/Health Promotion and Maintenance
- After a source of protein has been ingested—CORRECT: recommended to be performed before newborns leave hospital; if initial blood sample is obtained within first 24 hours, recommended to be repeated at 3 weeks
- After the meconium has been excreted—no relationship; dark-green, tarry stool passed within first 48 hours of birth
- After the danger of hyperbilirubinemia has passed—no relationship; excessive accumulation of bilirubin in blood; S/S: jaundice (yellow discoloration of skin); common finding in newborn; not cause for concern
- After the effects of delivery have subsided—no relationship
- The Answer is 3
The LPN/LVN is caring for an Rh-negative client who has delivered an Rh-positive child. The client states, “The doctor told me about RhoGAM, but I’m still a little confused.” Which of the following responses by the LPN/LVN is most appropriate?
Reworded Question: What is RhoGAM and why is it used?
Strategy: Remember what you know about RhoGAM.
Needed Info: RhoGAM: given to unsensitized Rh-negative (RH–) mother after delivery or abortion of an Rh-positive (Rh+) infant or fetus to prevent development of sensitization. Rh– mother produces antibodies in response to the Rh+ RBCs of fetus. If occurs during pregnancy, fetus is affected. If occurs during delivery, later pregnancies may be affected. An indirect Coombs’ test is performed on the mother during pregnancy, and a direct Coombs’ test is done on cord blood after delivery. If both are negative and the neonate is Rh+, the mother is given RhoGAM to prevent sensitization. RhoGAM is usually given to unsensitized mothers within 72 hrs of delivery, but may be effective when given 3–4 weeks after delivery. To be effective, RhoGAM must be given after the first delivery and repeated after each subsequent delivery. RhoGAM is ineffective against Rh+ antibodies that are already present in the maternal circulation. The administration of RhoGAM at 26–28 weeks’ gestation is also recommended.
Category: Implementation/Health Promotion and Maintenance
- “RhoGAM is given to your child to prevent the development of antibodies.”—not given to neonate
- “RhoGAM is given to your child to supply the necessary antibodies.”—not given to neonate
- “RhoGAM is given to you to prevent the formation of antibodies.”—CORRECT: prevents maternal circulation from developing antibodies
- “RhoGAM is given to you to encourage the production of antibodies.”—not accurate; given to discourage antibody production
- The Answer is 2
A woman is hospitalized with a diagnosis of bipolar disorder. While she is in the client activities room on the psychiatric unit, she flirts with male clients and disrupts unit activities. Which of the following approaches would be most appropriate for the LPN/LVN to take at this time?
Reworded Question: How should you deal with a client with bipolar disorder who is disruptive?
Strategy: Determine the outcome of each answer. Is it desirable?
Needed Info: Nursing responsibilities: accompany client to room when hyperactivity escalates, set limits, remain nonjudgmental.
Category: Planning/Psychosocial Integrity
- Set limits on the behavior and remind the client of the rules—too confrontational
- Distract the client and escort the client back to the room—CORRECT: clients are easily distracted; nonthreatening action
- Instruct the other clients to ignore this client’s behavior—does not ensure safety
- Inform client of negative behavior and return client to room—too confrontational; may agitate
- The Answer is 1
A client is brought to the emergency department bleeding profusely from a stab wound in the left chest area. Vital signs include: blood pressure 80/50 mm Hg, pulse 110 beats/minute, and respiratory rate 28 breaths/minute. The LPN/LVN should expect which of the following potential problems?
Reworded Question: What type of shock is described?
Strategy: Form a mental image of the person described.
Needed Info: Symptoms of hypovolemic shock: tachycardia, reduced output, irritability. Treatment: oxygen therapy, IV fluids to restore volume, adrenaline, hydralazine. Nursing responsibilities: check airway, vital signs, insert IV catheter, check arterial blood gas results, central venous pressure measurements, insert indwelling urinary catheter, hourly intake and output, position flat with legs elevated, keep warm.
Category: Planning/Physiological Integrity/Physiological Adaptation
- Hypovolemic shock—CORRECT: loss of circulating volume
- Cardiogenic shock—decrease in cardiac output; causes include heart failure, MI, cardiac dysfunction
- Neurogenic shock—increase in vascular bed; caused by spinal anesthesia, spinal cord injury
- Septic shock—decreased cardiac output, hypotension; may be caused by gram-negative or gram-positive bacteria
- The Answer is 3
A client is admitted to the hospital for surgical repair of a detached retina in the right eye. In implementing the plan of care for this client postoperatively, the LPN/LVN should encourage the client to do which of the following?
Reworded Question: What should you do after surgery for a detached retina?
Strategy: Picture the client as described.
Needed Info: Detached retina: separation of retina from pigmented epithelium. S/S: curtain falling across field of vision, black spots, flashes of light, sudden onset. Treatment: surgical repair (photocoagulation, electrodiathermy, cryosurgery, scleral buckling). Complications: infection, redetachment, increased intraocular pressure. Nursing responsibilities postoperatively: check eye patch for drainage, position with detached area dependent; no rapid eye movement (reading, sewing); no coughing, vomiting, sneezing.
Category: Planning/Physiological Integrity/Reduction of Risk Potential
- Perform self-care activities—activity restrictions depend on location and size of tear
- Maintain patches over both eyes—only affected eye covered
- Limit movement of both eyes—CORRECT: bed rest with eye patch or shield
- Refrain from excessive talking—no restriction
- The Answer is 2
The LPN/LVN is caring for a client who receives a balanced complete formula through an enteral feeding tube The LPN/LVN knows that the most common complication of an enteral tube feeding is which of the following?
Reworded Question: What is a common complication of a tube feeding?
Strategy: Think about each answer choice. Focus on the words “Most common,” which means there may be more than one answer. And in this situation there is: #4 is a complication but is not common.
Needed Info: Enteral tube feedings are used for clients who are unable to tolerate feeding by the oral route but who have a functioning GI tract. May be given by intermittent or continuous infusion. Elevate head of bed 30–45 degrees. Give at room temperature. Check for placement before feeding. Don’t hang solution for more than 6 hrs. Flush tubing with 30 mL water every 4 hrs. Change feeding set every 24 hrs. Balanced complete formula contains intact protein.
Category: Evaluation/Physiological Integrity/Basic Care and Comfort
- Edema—not frequently seen; if present primary health care provider may change formula to a low-sodium
- Diarrhea—CORRECT: formula intolerance or rate intolerance; give slowly; other symptoms of intolerance: nausea, vomiting, aspiration, glycosuria, diaphoresis
- Hypokalemia—normal potassium 3.5–5 mEq/L (3.5–5 mmol/L); not commonly seen; common causes: diuretics, diarrhea, GI drainage
- Vomiting—can happen with rapid increase in rate; adminster slowly
- The Answer is 4
An infant is brought to the hospital for treatment of pyloric stenosis. The following nursing diagnosis is on the infant’s care plan: “fluid volume deficit related to vomiting.” The LPN/LVN would expect to see which of the following findings to support this diagnosis?
Reworded Question: What would indicate volume deficit?
Strategy: How does each answer relate to fluid volume deficit?
Needed Info: Pyloric stenosis: obstruction of the sphincter between stomach and duodenum. Onset: within 2 months of birth. S/S: vomiting that becomes projectile. Treatment: surgery. Nursing responsibilities: small frequent feedings with glucose water or electrolyte solutions 4–6 hrs postoperatively. Small frequent feedings with formula 24 hrs postoperatively.
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- The infant eagerly accepts feedings—may vomit after eating
- The infant vomited once since admission—don’t assume will continue to vomit
- The infant’s skin is warm and moist—normal; would be cool and dry with fluid volume deficit
- The infant’s anterior fontanel is depressed—CORRECT: indicates dehydration
- The Answer is 1
The LPN/LVN is caring for a preschool-age client diagnosed with a fractured pelvis caused by a motor vehicle accident. The LPN/LVN prepares the child for the application of a hip spica cast. It is most important for the LPN/LVN to take which of the following actions?
Reworded Question: How do you prepare a preschool-age client for the procedure?
Strategy: “Most important” indicates that discrimination is required to answer the question.
Needed Info: Hip spica cast immobilizes the hip and knee. Preschool children (age 36 months to 6 years) fear injury, mutilation, and punishment; allow child to play with models of equipment; encourage expression of feelings.
Category: Planning/Health Promotion and Maintenance
- Obtain a doll for the client with a hip spica cast in place—CORRECT: preschoolers need to see and play with dolls and equipment; explain procedure in simple terms and explain how it will affect the client
- Tell the client that the cast will feel cold when applied—may feel a warm or burning sensation under cast while it dries due to chemical reaction between the plaster and the water
- Reassure the client that the cast application is painless—will be placed on special cast table that holds the client’s body; turning to apply the cast may be painful
- Introduce the client to another client who has a hip spica cast—more important to allow client to play with doll with a hip spica cast; viewing the cast may be frightening
- The Answer is 2
A client comes to the clinic because for suspected pregnancy. Tests confirm pregnancy. The client’s last menstrual period began on September 8 and lasted for 6 days. The LPN/LVN calculates that her expected date of confinement (EDC) is which of the following?
Reworded Question: How do you calculate the EDC?
Strategy: Perform the calculation required and check for math errors!
Needed Info: EDC or estimated date of delivery (EDD): calculated according to Nägele’s rule (first day of the last normal menstrual period minus 3 months plus 7 days and 1 year). Assumes that every woman has a 28-day cycle and pregnancy occurred on 14th day. Most women deliver within a period extending from 7 days before to 7 days after the EDC.
Category: Implementation/Health Promotion and Maintenance
- May 15—too early
- June 15—CORRECT September 8 minus 3 months = June 8 plus 7 days plus one year = June 15 of next year
- June 21—EDC is calculated from first, not last day, of last normal menstrual period
- July 8—not accurate
- The Answer is 3
An infant is brought to the pediatrician’s office for a well-baby visit. During the examination, congenital subluxation of the left hip is suspected. The LPN/LVN would expect to see which of the following symptoms?
Reworded Question: What will you see with congenital hip dislocation?
Strategy: Form a mental image of the deformity.
Needed Info: Subluxation: most common type of congenital hip dislocation. Head of femur remains in contact with acetabulum but is partially displaced. Diagnosed in infant less than 4 weeks old S/S: unlevel gluteal folds, limited abduction of hip, shortened femur affected side, Ortolani’s sign (click). Treatment: abduction splint, hip spica cast, Bryant’s traction, open reduction.
Category: Data Collection/Health Promotion and Maintenance
- Lengthening of the limb on the affected side—inaccurate
- Deformities of the foot and ankle—inaccurate
- Asymmetry of the gluteal and thigh folds—CORRECT: restricted movement on affected side
- Plantarflexion of the foot—seen with clubfoot
- The Answer is 4
After completing data collection, the LPN/LVN observes that a client is exhibiting early symptoms of a dystonic reaction related to the use of an antipsychotic medication. Which of the following actions by the LPN/LVN would be most appropriate?
Reworded Question: What is the first thing you do for a client with a dystonic reaction?
Strategy: Set priorities. Remember Maslow’s hierarchy of needs.
Needed Info: Dystonic reaction: muscle tightness in throat, neck, tongue, mouth, eyes, neck, and back; difficulty talking and swallowing. Treatment: IM or IV diphenhydramine or benztropine.
Category: Implementation/Psychosocial Integrity
- Reality-test with the client and assure the client that physical symptoms are not real—real symptoms, not delusions
- Teach the client about common side effects of antipsychotic medications—physical needs highest priority
- Explain to the client that there is no treatment that will relieve these symptoms—diphenhydramine used IM or IV
- Notify the primary health care provider to obtain a prescription for IM diphenhydramine—CORRECT: emergency situation, can occlude airway
- The Answer is 1
The LPN/LVN is preparing to perform mouth care for an unconscious client. Which of the following actions should the LPN/LVN take first?
Reworded Question: Before initiating any care or procedure, what should the LPN/LVN do first to provide for client safety?
Strategy: Think ABCs when identifying first nursing action.
Needed Info: An unconscious client cannot protect himself from injury. Consider the ABCs. Sims’ position: lying on left side with right knee and thigh drawn up to the chest. Gag reflex: prevents aspiration of secretions and food, fluid, and objects.
Category: Data Collection/Physiological Integrity/Basic Care and Comfort
- Assess for the presence of a gag reflex—CORRECT: the LPN/LVN is responsible for determining if the client can clear own airway or is at risk for occlusion or aspiration
- Place the client into Sims’ position—an accurate position for mouth care for this client, but not the initial step
- Separate teeth with a padded tongue blade—nothing should be used to separate the teeth; would likely lead to tooth damage
- Suction secretions from the oral cavity—an accurate procedural step that should occur after the client’s gag reflex is determined
- The Answer is 1
As a client nears death, the client’s husband says, “I wish I could do something for her.” Which of the following responses by the LPN/LVN is most appropriate?
Reworded Question: What is the most therapeutic communication for the husband?
Strategy: Think about the husband’s need to help his wife.
Needed Info: End-of-life research: last of the senses of a dying person is believed to be hearing, reports of survivors support the reassurance they felt from the words of the caregivers present. Therapeutic communication: supports inclusion of significant others, supports “hope” or “usefulness” on the part of significant others.
Category: Evaluation/Psychosocial Integrity
- “It may be comforting if you talk to her calmly and clearly.”—CORRECT: the client may actually hear her family member's communications; the family member is offered something to do that may be helpful to both the client and the family member
- “She does not know that you are here, but you can sit here.”—the client may be aware that her family member is there, and it is nontherapeutic to exclude the family member from offering comfort
- “Unfortunately, there is little that you can do at this point.”—it is nontherapeutic to exclude the family member from offering comfort
- “Why don’t you take a break? It is just a matter of time now.”—it is nontherapeutic to exclude the family member from offering comfort
- The Answer is 4
The LPN/LVN is providing care to clients in a long-term care facility. Four meal choices are available to the clients. The LPN/LVN should ensure that a client on a low-cholesterol diet receives which of the following meals?
Reworded Question: What should a client on a low-cholesterol diet eat?
Strategy: Remember which foods are part of a low-cholesterol diet.
Needed Info: Low-cholesterol diet should reduce total fat to 20–25% of total calories and reduce the ingestion of saturated fat. Carbohydrates (especially complex carbohydrates) should be 55–60% of calories. High-cholesterol foods: eggs, dairy products, meat, fish, shellfish, poultry.
Category: Implementation/Physiological Integrity/Basic Care and Comfort
- Egg custard and boiled liver—high amounts of cholesterol
- Fried chicken and potatoes—avoid fried foods
- Hamburger and french fries—avoid fried foods
- Grilled flounder and green beans—CORRECT: fish instead of meat; increase vegetables
- The Answer is 465
The LPN/LVN is removing a client’s breakfast tray and notes that the client consumed 4 oz of pudding, 4 oz of gelatin, 6 1/2 oz of tea, and 5 oz of apple juice. How many milliliters should the LPN/LVN record for the client’s breakfast intake?
Reworded Question: Calculate the client’s oral fluid intake in mL.
Strategy: Remember what is considered oral fluid intake.
Needed Info: Oral fluid intake: any liquid or food in more solid form that melts at room temperature.
Category: Data Collection/Physiological Integrity/Basic Care and Comfort
The calculation is 4 oz gelatin + 6½ oz of tea + 5 oz of apple juice = 15½ oz × 30 mL = 465 mL. Pudding does not melt at room temperature, so is not considered to be a liquid and therefore it is not included in the calculation.
The correct answer is 465.
- The Answer is 2
The LPN/LVN is caring for a client diagnosed with cholecystitis. The client says to the LPN/LVN, “I don’t understand why my right shoulder hurts when the gallbladder is not by my shoulder!” Which of the following responses by the LPN/LVN is best?
Reworded Question: Why does the client’s shoulder hurt?
Strategy: “Best” indicates discrimination is required to answer the question.
Needed Info: Cholecystitis is inflammation of the gallbladder; indications include intolerance to fatty foods, indigestion, severe pain in right upper quadrant of abdomen radiating to back and right shoulder; leukocytosis, and diaphoresis.
Category: Implementation/Physiological Integrity/Physiological Adaptation
- “Sometimes small pieces of the gallstones break off and travel to other parts of the body.”—gallstones do not become emboli
- “There is an invisible connection between the gallbladder and the right shoulder.”—CORRECT: describes referred pain; when visceral branch of a pain receptor fiber is stimulated, vasodilation and pain may occur in a distant body area; right shoulder or scapula is the referred pain site for gallbladder
- “The gallbladder is on the right side of the body and so is that shoulder.”—anatomically correct but is not the best explanation
- “Your shoulder became tense because you were guarding against the gallbladder pain.”—possible; not the best explanation
- The Answer is 4
A woman comes to the clinic at 32 weeks’ gestation. A diagnosis of pregnancy-induced hypertension (PIH) is made. The LPN/LVN is reinforcing teaching performed by the RN. Which of the following statements by the client indicates that further teaching is required?
Reworded Question: What is not accurate about the care of a woman with PIH?
Strategy: This is a negative question. Look for incorrect information.
Needed Info: PIH, preeclampsia, toxemia: development of hypertension (increase 30 mmHg systolic or 15 mmHg diastolic) with proteinuria and/or edema (dependent or facial) after 20 weeks’ gestation. Risk factors: parity (first-time mothers), age (younger than 20 or older than 35), geographic location (southern or western United States), multifetal gestation, hydatidiform mole, hypertension, and diabetes. Prevention: early prenatal care, identify high-risk clients, recognize S/S early; bed rest lying on L side, daily weights. Treatment: urine checks for proteinuria; diet (increased protein and decreased Na+). Can develop into eclampsia (convulsions or coma).
Category: Evaluation/Health Promotion and Maintenance
- “Lying in bed on my left side is likely to increase my urinary output.”—true; bed rest promotes good perfusion of blood to uterus; decreases blood pressure and promotes diuresis
- “If the bed rest works, I may lose a pound or two in the next few days.”—true; causes diuresis; results in reduction of retained fluids; instruct to monitor weight daily and notify primary health care provider if notices abrupt increase even after resting in bed for 12 hours
- “I should be sure to maintain a diet that has a good amount of protein.”—true; replaces protein lost in urine; increases plasma colloid osmotic pressure; avoid salty foods; avoid alcohol; drink 8 glasses of water daily; eat foods high in roughage
- “I will have to keep my room darkened and not watch much television.”—CORRECT: incorrect info, not necessary; diversional activities helpful
- The Answer is 4
The LPN/LVN is collecting data about a client’s fluid balance. Which of the following findings most accurately indicates to the LPN/LVN that the client has retained fluid during the previous 24 hours?
Reworded Question: How can the LPN/LVN most accurately determine fluid retention?
Strategy: Look at the most conclusive means of determining fluid retention.
Needed Info: Means of evaluating fluid retention: recording fluid intake and output; determining areas of edema especially the sacrum, feet, and ankles; listening for wet lung sounds; and measuring short-term weight gain. Weight gain: most objective and accurate. Weight gain of 2.2 lb (1 kg) is equivalent to 1 L of fluid.
Category: Data Collection/Physiological Integrity/Basic Care and Comfort
- Edema is found in both ankles—unable to consistently quantify this form of data
- Fluid intake is equal to fluid output—this is normal but does not account for insensible fluid loss through the skin and lungs
- Intake of fluid exceeds output by 200 mL—provides information, but does not eliminate the possibility of error recording all intake and output
- Weight gain of 4 lb (1.8 kg) is noted—CORRECT: identifies fluid retention in a factual, accurate method and is unlikely to represent a gain of actual body substance (muscle or fat) in a 24-hour time frame
- The Answer is 4
The LPN/LVN is caring for a group of residents in a dependent-living facility. The LPN/LVN determines which of the following clients is most at risk to develop pneumonia?
Reworded Question: Who is most likely to develop pneumonia?
Strategy: Think about each answer.
Needed Info: Pneumonia is an inflammatory process that results in edema of lung tissues and extravasion of fluid into alveoli, causing hypoxia; symptoms include fever, leukocytosis, productive cough, dyspnea, and pleuritic pain.
Category: Evaluation/Health Promotion and Maintenance
- A client female with left-sided hemiparesis after a stroke—stroke is a risk factor
- A client who has a history of hypertension and type 2 diabetes—diabetes is a risk factor
- A client with a history of depression who walks one mile daily—no risk factors
- A client who smokes and has a history of lung cancer—CORRECT: smoking, underlying lung disease, malnutrition, and bedridden status are risk factors for development of pneumonia
- The Answer is 2
The LPN/LVN is caring for a client diagnosed with bipolar disorder. Which of the following behaviors by the client indicates that a manic episode is subsiding?
Reworded Question: What indicates normalizing behavior?
Strategy: Think about the behaviors that indicate mania.
Needed Info: Manic clients may tease, talk, and joke excessively, usually cannot sit to eat and may need to carry fluids and food around in order to eat, often try to take a leadership position in an environment, and try to engage others.
Category: Data Collection/Psychosocial Integrity
- The client tells several jokes during a group meeting—reflects an elated mood and no real participation in the meeting; manic clients may tease, talk, and joke excessively
- The client sits and talks with other clients at mealtimes—CORRECT: manic clients have difficulty socializing because of flight of ideas and intrusiveness; usually cannot sit to eat and will carry fluids and food around
- The client begins to write a book about personal story—manic clients often write voluminously; may help to express feelings, but does not reflect improvement, especially if thoughts are grandiose
- The client initiates a unit effort to start a radio station—manic clients often try to take a leadership position in an environment and try to recruit others
- The Answer is 2
A parent brings a child to the pediatrician for treatment of chronic otitis media. The parent asks the LPN/LVN how to prevent the child from getting ear infections. The LPN/LVN’s response should be based on an understanding that the recurrence of otitis media can be decreased by which of the following?
Reworded Question: What will prevent the development of otitis media? What causes otitis media?
Strategy: Think about the causes of otitis media.
Needed Info: Otitis media: frequently follows respiratory infection; reduce occurrence by holding child upright for feedings, encourage gentle nose-blowing, teach modified Valsava maneuver (pinch nose, close lips and force air up through eustachian tubes), blow up balloons or chew gum, eliminate tobacco smoke or known allergens.
Category: Planning/Health Promotion and Maintenance
- Covering the child’s ears while bathing—does not prevent otitis media
- Treating upper respiratory infections quickly—CORRECT: respiratory fluids are a medium for bacteria; antihistamines used
- Administering nose drops at bedtime—not preventative
- Isolating the child from other children—too extreme a measure
- The Answer is 2
A client is calling the suicide prevention hotline to report a personal suicide plan. Which of the following questions should the LPN/LVN ask first?
Reworded Question: What is most important to know about a client who has threatened suicide?
Strategy: “First” indicates priority.
Needed Info: Signs of suicide: symptoms of depression, client gives away possessions, gets finances in order, has a means, makes direct or indirect statements, leaves notes, increase in energy. Predisposing factors: male over age 50, teenagers between 15–19, poor social attachments, clients with previous attempts, clients with auditory hallucinations, overwhelming precipitating events (terminal disease, death or loss of loved one, failure at school, job).
Category: Data Collection/Psychosocial Integrity
- “What happened to cause you to want to end your life?”—does not determine immediate need for safety
- “Tell me the details of the plan you developed to kill yourself?”—CORRECT: lets you prioritize interventions to assure safety
- “When did you start to feel as though you wanted to die?”—does not determine immediate need for safety
- “Do you want me to prevent you from killing yourself?”—yes/no question, closed
- The Answer is 2
Prior to the client undergoing a scheduled intravenous pyelogram (IVP), it would be most important for the LPN/LVN to ask which of the following questions?
Reworded Question: What do you need to know before an IVP?
Strategy: Think about each answer and how it relates to IVP.
Needed Info: IVP: radiopaque dye injected into the body and is filtered through the kidneys and excreted by the urinary tract. Visualizes kidneys, ureters, and bladder. Preparation: NPO midnight, cathartics evening before test. Injection of dye causes flushing of face, nausea, salty taste in mouth.
Category: Data Collection/Physiological Integrity/Reduction of Risk Potential
- “Do you have any difficulty voiding?”—not most important
- “Do you have any allergies to shellfish or iodine?”—CORRECT: anaphylactic reaction; itching, hives, wheezing; treatment: antihistamines, oxygen, cardiopulmonary resuscitation, epinephrine, vasopressor
- “Do you have a history of constipation?”—not essential information
- “Do you have a history of frequent headaches?”—not most important
- The Answer is 3
The LPN/LVN is assigned to a newly admitted elderly client in the hospital setting that reports having no living relatives and only friends of similar age. One of the LPN/LVN’s most immediate considerations for this client will be to help the RN implement which of the following?
Reworded Question: Given the information provided, what is a priority for this client?
Strategy: Look for the answer that addresses this client’s individualized needs/situation.
Needed Info: Client lengths of stay are very short. Likely that this elderly client does not have anyone to assist with care or activities of daily living (ADL) if needed upon discharge. Discharge planning: begins upon admission for all hospitalized clients. Concept map: a conceptual plan that integrates nursing care. Critical pathway: multidisciplinary plan for clinical interventions during hospitalization. Utilization group: classifies clients by disease or injury.
Category: Implementation/Safe and Effective Care Environment/Coordinated Care
- A concept map—a plan of care is necessary for every client
- A critical pathway—addresses only the acute-care stay
- A discharge plan—CORRECT: will provide for the appropriate support this client needs to return to the community or transfer to another level of care
- A utilization group—not an important consideration for this client
- The Answer is 3
A woman delivers a 6 lb 10 oz baby girl. The mother observes the LPN/LVN in the delivery room place drops in her daughter’s eyes. The mother asks the LPN/LVN why this was done. Which of the following responses by the LPN/LVN is best?
Reworded Question: Why are eyedrops placed in a newborn’s eyes?
Strategy: “Best” indicates that discrimination may be required to answer the question.
Needed Info: Prophylactic care of newborns includes administration of vitamin K to prevent hemorrhage; erythromycin and tetracycline are used for prophylactic eye care.
Category: Implementation/Health Promotion and Maintenance
- “The drops constrict your baby’s pupils to prevent injury.”—erythromycin or tetracycline do not cause myosis
- “The drops will remove mucus from your baby’s eyes.”—does not remove mucus from baby’s eyes
- “The drops will prevent infections that might cause blindness.”—CORRECT: precaution against opthalmia neonatorum (inflammation of the eyes due to gonorrheal or chlamydia infection)
- “The drops will prevent neonatal conjunctivitis.”—conjunctivitis is inflammation of the conjunctiva
- The Answer is 3
The LPN/LVN is caring for a client admitted for a possible herniated intervertebral disk. The primary health care provider prescribed ibuprofen, propoxyphene hydrochloride, and cyclobenzaprine hydrochloride to be given as needed for pain. Several hours after admission, the client reports . Which of the following actions should the LPN/LVN take first?
Reworded Question: What should you do first?
Strategy: Set priorities. Collect data before implementing.
Needed Info: Herniated disk: knifelike pain aggravated by sneezing, coughing, straining.
Category: Planning/Physiological Integrity/Pharmacological Therapies
- Give the client ibuprofen to promptly manage the pain—implementation; not first step
- Ask the primary health care provider which drug to give first—collect data before implementing
- Gather more information from the client about the pain—CORRECT: collect data; first step in nursing process
- Allow the client some time to rest to see if the pain subsides—implementation; not first step
- The Answer is 4
The LPN/LVN is completing a client’s preoperative checklist prior to surgery. The nurse obtains the client’s vital signs: temperature 97.4° F (36° C), radial pulse rate 84 beats/minute, respiratory rate 16 breaths/minute, and blood pressure 132/74 mm Hg. Which action should the LPN/LVN take first?
Reworded Question: What should you do for a client with normal vital signs?
Strategy: Identify normal vital signs.
Needed Info: Normal vital sign values include blood pressure 139/79 mm Hg, heart rate 60 to 100 beats/minute, and respiratory rate 16 to 20 breaths/minute.
Category: Data Collection/Physiological Integrity/Reduction of Risk Potential
- Notify the primary health care provider of client’s vital signs—most primary health care providers do not want to be notified about normal values
- Obtain orthostatic blood pressures lying and standing—there is no information to support this action
- Lower the side rails and place the bed in its lowest position—bed side rails should be raised, not lowered
- Record the data on the client’s preoperative checklist—CORRECT: the vital signs are normal and should be recorded in the client’s medical record
- The Answer is 3
The LPN/LVN is expecting to see which of the following physiological changes in a client experiencing an episode of acute pain?
Reworded Question: What happens to the vital signs when a client is in pain?
Strategy: Think about the cause of each vital sign change. Is it consistent with pain?
Needed Info: Pain causes increased blood pressure and heart rate, which leads to increased blood flow to the brain and muscles; rapid irregular respirations lead to increased oxygen supply to brain and muscles; increased perspiration removes excessive body heat; increased pupillary diameter leads to increased eye accommodation to light.
Category: Data Collection/Physiological Integrity/Physiological Adaptation
- Decreased blood pressure—blood pressure increases to enhance alertness to threats
- Decreased heart rate—heart rate increases
- Decreased skin temperature—CORRECT: skin cools due to diaphoresis
- Decreased respirations—respirations increase
- The Answer is 4
A client is transferred to a long-term care facility after a stroke. The client has right-sided paralysis and dysphagia. The LPN/LVN observes an unlicensed assistive personnel (UAP) preparing the client to eat lunch. Which of the following situations would require an intervention by the LPN/LVN?
Reworded Question: What option is wrong?
Strategy: This is a negative question. Determine if you are looking for a correct situation or a problematic situation.
Needed Info: Dysphagia: difficulty swallowing. Provide support if necessary for the head, have the client sit upright, feed the client slowly in small amounts, place food on unaffected side of mouth. Maintain upright position for 30–45 minutes after eating. Good oral care after eating.
Category: Evaluation/Physiological Integrity/Reduction of Risk Potential
- The client remains in bed in the high Fowler’s position—correct positioning, or may sit in chair
- The client’s head and neck are positioned slightly forward—correct positioning; helps client chew and swallow
- The UAP places food in back of the mouth of unaffected side—helps client handle food
- The UAP adds tap water to pudding to help the client swallow—CORRECT: requires intervention, usually able to better handle soft or semi-soft foods; difficulty with liquids
- The Answer is 2, 3, and 4
The LPN/LVN’s is collecting data and a client’s blood pressure is 146/92 mm Hg with labored respirations at a rate of of 24 breaths/minute. Bloody drainage appears on the client’s IV dressing. The client reports pain in the left hip, depression, and hunger. The LPN/LVN identifies which of these as subjective data? Select all that apply.
Reworded Question: What data have been reported by the client?
Strategy: Look for client-reported data.
Needed Info: Subjective data: client’s perceptions. Objective data: information perceptible to the senses (sight, hearing, touch, smell, taste) or measurable data.
Category: Data Collection/Safe and Effective Care Environment/Coordinated Care
- Blood pressure—measurable objective data
- Depression—CORRECT: subjective client-reported data
- Hip pain—CORRECT: subjective client-reported data
- Hunger—CORRECT: subjective client-reported data
- IV drainage—measurable objective data
- Respirations—measurable objective data