SEVEN
What Should I Expect during the Surgery?
Deep brain stimulation (DBS) surgery generally takes place in two stages. In the first stage, the DBS leads are placed into the target locations in the brain. In the second stage, the implanted leads are connected to the stimulator or the implantable pulse generator (IPG). Depending on available resources and the preferences of the neurosurgeon, each DBS team performs the surgery differently.
For example, at some centers, both stages are performed on the same day, making the DBS procedure into a single, long operation. At the other extreme, some centers will implant one lead at a time and one stimulator per side at a time, for a total of four separate operations. Each approach has its advantages and disadvantages. The advantage of having everything done in one operation is that you have fewer operations, which reduces risk of infection and side effects from anesthesia. On the other hand, having everything done in a single operation means that it takes much longer to complete on that day. It makes for a much more complex procedure.
In this chapter, we describe a staged DBS surgery where stage I (lead implantation) occurs first, followed by stage II (placement of the extension wire and stimulator). Stages I and II are separated by some period of time, ranging from a week to several weeks. This approach is between the two extremes listed above and is done at many centers. Thus, for people living with Parkinson’s disease or dystonia, two DBS leads would be placed during stage I, one on each side of the brain, followed by stage II later. For essential tremor, a unilateral lead would be placed on the side of the brain opposite the dominant hand in stage I, and then followed by stage II some time later. The advantage to performing surgery in a staged manner like this is that the procedure tends to be tolerated better.
STAGE I: IMPLANTATION OF DBS LEADS
Frame Placement
On the day of surgery, you will start in the preoperative area. You will be asked to remove your clothing, jewelry, and other personal items and change into a hospital gown. An intravenous (IV) line will be placed in your vein so that medications can be administered during surgery. Many centers try to avoid placing a urinary catheter during this part of the surgery. Because you are typically awake during stage I, you will be able to use a bedpan or urinal if needed. However, because you have not been able to eat or drink for several hours, there is usually little concern for your bladder.
The first step in the implantation of the DBS leads is the placement of a lightweight metal frame that looks like a hollow cube. You will be seated comfortably and facing forward. The frame is then fixed to the skull and held in position by four screws, two in the front and two in the back. Numbing medication is injected into the skin at four points where the frame will be fixed to the skull. When the frame is applied, you may feel pressure from the screws, but not pain, due to the numbing medication. If you complain of some pain, then more numbing medication is given. The sense of pressure that people feel can be initially significant but goes away entirely within 5–10 minutes. With the frame placed, you are then taken to the MRI scanner. The MRI uses magnetic fields to take clear and detailed pictures of the brain.

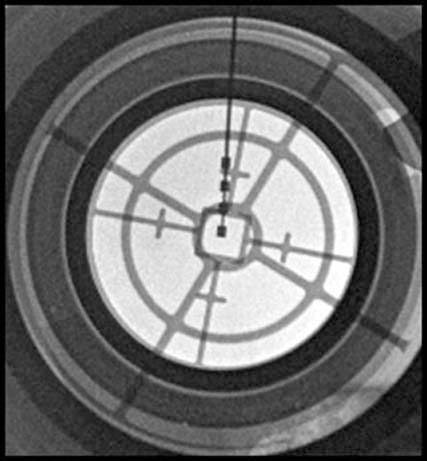
Stereotactic frame
Keep in mind that some centers may do “frameless” surgery. Although not technically frameless, this technique uses a much smaller frame. Rather than looking like a hollow cube that goes around your entire head, the “frameless” approach uses either a small frame that looks like a tripod and is screwed to the top of the skull or another small frame that attaches to the hole drilled in the skull. The approach that your neurosurgeon takes is generally based on his or her training and experience. Neither approach is clearly better than the other. What is important is that your neurosurgeon is experienced with one of the approaches.
Pre-operative MRI
Before entering the MRI, two additional components are attached to the frame: a localizer and an orientation adapter. The localizer includes a fluid-filled chamber that contains a solution that can be seen on the MRI scan. The orientation adapter holds the individual and the frame in good position during the MRI scan. This preoperative MRI scan takes about 10 minutes to perform.
Choosing the Target
The MRI allows the neurosurgeon to see all of the structures in the brain. The neurosurgeon uses this picture to mark the structure where the DBS lead will be placed and determines the path that the electrode shall take from the skull surface to the deep brain target. You are given an intravenous dye prior to the MRI scan, which allows the neurosurgeon to avoid important blood vessels when planning the path of the electrode and thus reduce complications.
The MRI-visible solution in the localizer component allows a unique set of coordinates to be assigned to each location in the brain. By examining the MRI scan, the neurosurgeon can estimate the location of any of the targeted structures such as the subthalmic nucleus (STN), thalamus, or globus pallidus interna (GPi) and associate it with a set of X, Y, and Z coordinates. This allows the surgeon to accurately determine where to place the tip of the lead.
In addition to determining the coordinates of each target, the neurosurgeon also determines the location of the small hole where the DBS electrode can most safely enter the skull. The straight-line trajectory from the skull to the DBS target determines where entry holes may be made safely. The neurosurgeon must take great care to ensure that the trajectory does not cross any blood vessels or other important brain structures. With the targets calculated and the entry locations determined, the operation may now proceed.
Going to the Operating Room
After the MRI is completed, you will be taken from the MRI scanner to the operating room. Once you are in the operating room, you may find it noisy and quite busy with staff preparing for the procedure. Your comfort is important to the neurosurgeon and staff. If you feel discomfort, you should let your surgeon know so that steps can be taken to alleviate any pain or discomfort. Also, if you find the room too cold, ask for additional blankets. Ask if headphones and a CD player or iPod are available for listening to your favorite music or relaxation message.
You will be positioned comfortably on the operating table, and the operating room staff will make sure that the table is well-padded so that you will not be sore. Additional padding may be used to be sure that your back and neck are comfortable. The frame that is fixed to your skull will be secured to the operating table so that it cannot move during the procedure. The head of the bed is raised slightly, so that you will be able to look forward. You will not be able to move your head because it is secured to the table (but you would not want to anyway, since moving your head would alter the path of the electrode and you would risk having the DBS lead placed incorrectly). However, you will be able to freely move your arms and legs.
A narrow strip of hair, just above the forehead (and behind the hairline), is then shaved. It should be noted that the amount of hair shaved differs from center to center. Some neurosurgeons will shave the entire skull, whereas others will shave only a small area. If you care about how much hair is shaved off, you should ask about this before the surgery. The skin is cleansed thoroughly with antibacterial solution to prevent infection. Once the solution dries, sterile drapes are placed to cover the surgical area and to form a bacteria-proof shield. Numbing medicine is then injected into the area where the incision is to be made. Once the incision is made, the targeting apparatus of the frame is used to mark the location on the skull where the small holes are to be made.
Each hole for each DBS electrode is fashioned with a very special drill. The drill is designed to cut through the bone without cutting through any softer tissues than the bone. Because of this feature, the hole can be made in the skull without injuring the brain or its coverings. Because sound conducts well in the bone and earplugs only block sound conducted in the air, the sound of the drill is quite loud for the person undergoing surgery. Some people are also bothered by the vibration or chatter of their teeth from the drill. Because of these two factors, many people say that the drilling is the worst part of the entire procedure. If the vibration is bothersome, ask for a small cloth to hold in your mouth briefly until the drilling is complete. Fortunately, the drilling itself lasts only for a few seconds. The size of the drill hole is about the width of a dime.
Once the drilling is completed, the neurosurgeon attaches the targeting mechanism, which is shaped like a semicircular arc, to the frame. The targeting arc is set to guide the electrode to the intended target coordinates along the planned trajectory. An X-ray may be taken to double-check that the electrode trajectory is accurate.

Arc assembly
Electrophysiological (Microelectrode) Recording
Electrophysiological or microelectrode recording is a technology that allows the neurosurgeon, often working with a neurologist or neurophysiologist, to measure the activity of brain cells. By looking at the activity of cells, the neurosurgeon can often determine where the cells are located. Imagine yourself taking a road trip from Detroit down to Miami. If you keep the radio on, you might hear the sounds of Motown when you start the trip. As you drive past Nashville, you probably will start to hear country music on the radio. When you get into Miami, you might hear more Cuban music. The cells of the thalamus, STN, and GPi regions all have very distinct firing patterns, just like Detroit, Nashville, and Miami have different music playing on their radio stations. By measuring the activities of cells, the neurosurgeon can determine the optimal location for the tip of the DBS lead along the trajectory and confirm that the lead is being placed in the correct area.
The electrodes used to examine the firing patterns of brain cells are very fine. In fact, the tips of these electrodes are twenty-five times narrower than the tip of the DBS electrode itself. The use of electrophysiological or microelectrode recording, therefore, allows the optimal DBS electrode target to be found without having to test multiple areas by passing the large DBS electrode into the brain. There is no sensation as the leads are passed through the brain, so there is no discomfort from placement of the electrode.
Placement and Testing of Leads
Once the optimized target location is determined, the DBS lead is placed into the brain. The placement of the lead is confirmed by X-ray. After that, the DBS lead will be turned on and you will be examined. The purpose of this is to make sure that the DBS system can improve symptoms. It also allows the DBS team to test for side effects. When the DBS system is turned on in the operating room, you may feel tingling sensations or mild electrical shocks in the face, arm, or leg opposite the side of the DBS lead. Depending on the location of the lead and the contact being tested, you may see a burst of light, experience double vision, or even feel hot and sweaty. Sometimes you may even feel that the muscles in your face, arm, or leg are spasming. Typically, these side effects will occur only at higher settings. If side effects occur at low settings, the DBS lead may be slightly off and may need to be replaced. If you have ET, the DBS team will see if the stimulation can help stop your tremor. If you have Parkinson’s disease, the DBS team will look at whether stimulation will help tremor (if you have it), relieve stiffness, or improve slowness. You may be asked to write, drink, repeat words or phrases, or move the arms or legs, depending on what your symptoms are. For dystonia, unfortunately, improvement in the posture and pain is usually not seen in the operating room. However, the DBS team can confirm if it is in the correct place based on the side effects you get when the stimulation is turned on.

Getting an X-ray in the operating room
Lead verification

Patient testing
At some centers, the neurosurgeon and neurophysiologist do the testing. At others, the DBS neurologist is called into the operating room to perform the testing. Some centers may also have a speech-language pathologist present during testing to make sure that there are no speech problems with the stimulator turned on. After testing, the members of the DBS team will come together in the room to discuss whether the lead is appropriately placed or whether adjustments need to be made.
At this point, if you have essential tremor, the bulk of the surgery is over, and you only need to wait for the surgeon to secure the lead to the skull and close the incision before you are taken to the postoperative care unit. However, if you have Parkinson’s or dystonia, the electrophysiological recording and DBS lead placement and testing are repeated on the other side of the head. Once both leads are placed, each is secured into its location with a plastic locking cap that fits into the hole drilled in the skull. This cap remains under the skin. As a result, your scalp will feel irregular or “lumpy.” This is normal. Your hair will cover the irregularity so that it is not noticeable (unless you have a bald head). The DBS electrodes are placed under the skin, just above the ear. The scalp incision is then closed with surgical staples or sutures. There may be mild pain from the incision at this time, which is easily managed with pain medication. People also often have a headache and feel tired after surgery. Some people will notice swelling at the forehead and under or around their eyes, and there may also be bruising of the soft tissue on the face. This is normal and will subside over the next few days.
DBS Lead Placement Using Intraoperative MRI
A new technique for placement of DBS leads is using intraoperative MRI. This is only being performed at a few select centers thus far. Instead of being placed in a traditional stereotactic frame (the “hollow cube” mentioned earlier), an “aiming device” is applied to the top of the skull that allows the neurosurgeon to get X, Y, and Z coordinates for each part of the brain. Individuals are placed under general anesthesia, and the procedure is done in the radiology suite, not the operating room. The target structure is seen using MRI after the holes are drilled, and the placement of the lead is confirmed with the MRI before closing the incision. All of the instruments and hardware developed for this technique are MRI compatible. No electrophysiological recording or clinical testing is done with this method. The advantages are that the surgery can be done more quickly and can be done under general anesthesia. However, this method is not yet being used at all centers, and the success of the surgery depends on the quality of the pictures obtained by the MRI.
Recovery and Post-operative Imaging
Once the leads are secured in position and the incision is closed, you will be taken to the recovery room. Before that, however, you may be taken to get a postoperative computed tomography (CT) scan to verify the location of the leads and to confirm that there is no abnormal bleeding due to the lead placement. The CT scan does not take as long as an MRI and is not as clear, but is a much better way of detecting blood in the brain. Sometimes this CT may be done after a short wait in the recovery room and before being taken up to your hospital bed.

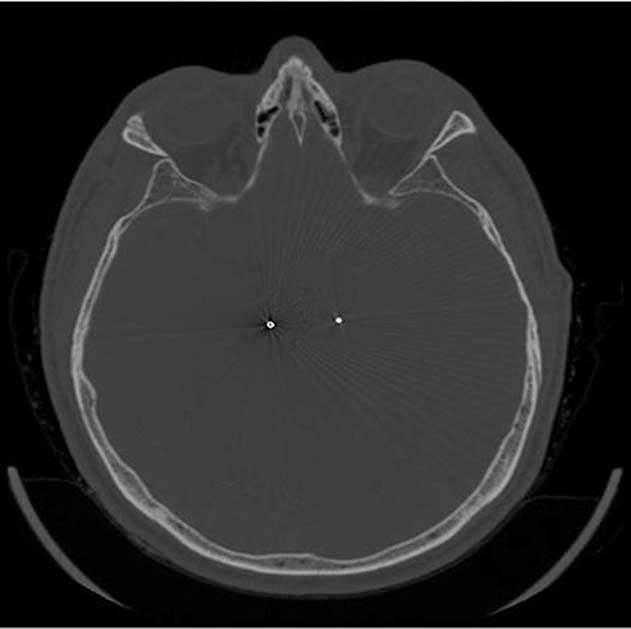
Postoperative CT scan
After surgery, you may be placed in the intensive care unit or in a regular unit. It is typical for most people to be discharged from the hospital on the day after lead placement. When you are discharged to home, you will be given instructions about care of your incisions, pain management, and activity limitations. Those living with Parkinson’s disease will likely resume their regular medications, but it is possible that less medication will be needed. Make sure you have someone who will stay with you for a few days until it is certain you have no untoward effects from surgery.
During your hospital stay, you may be surprised that the staff often knows little about the management of movement disorders, especially Parkinson’s disease. That is because people with movement disorders are rarely hospitalized for their disease. If you have Parkinson’s, you may find that nurses are not as responsive to your need to take your medication promptly, and your medication schedule may be altered. Because the hospital formulary may not have your particular medications available, you may be prescribed different medication than you take at home. To reduce some of the problems related to changes in your medication regimen, we recommend that you bring an accurate list of your medications with the dose and frequency. Your friends and family who are going to support you will need to be your advocate at this time. They (or you) should provide the nurse on each shift a brief educational summary about your condition, especially how alterations in your medications impact your ability to move and function. You should also monitor the administration of your medications, and question any medications you do not normally take. Being proactive about these issues will help make your hospital stay a more comfortable one.
STAGE II: PLACEMENT OF THE STIMULATOR
Stage II is an outpatient procedure in which the stimulator or implantable pulse generator is placed under the skin in the chest and is connected by wires under the skin to the earlier implanted DBS lead. The second stage of DBS surgery may be scheduled anywhere from the next day to several weeks after the first stage, depending on the DBS center. One of the advantages to waiting longer in between stages is that it allows adequate time for the wounds to heal and to ensure that there are no signs of infection from the lead-placement surgery. However, performing stage II closer to stage I may be more efficient in terms of recovery time. Regardless of the interval between lead placement and placement of the stimulator or IPG, it is recommended that there be at least 4 weeks between placement of the lead and initial programming of the stimulator.
Unlike stage I where the individual is awake, stage II is performed under general anesthesia. In other words, you will be completely knocked out. After the anesthesia kicks in, you will be moved to the operating room and placed on the operating table. After cleaning the skin and washing the head with antiseptic solution, a small incision is made over the location where the electrodes are buried under the scalp. The electrodes are then brought to the surface, where they can be accessed.
The neurosurgeon then creates a pocket under the skin, just below the collarbone. This pocket is large enough to hold the stimulator or IPG snugly. Once the pocket is made, the neurosurgeon creates a tunnel under the skin from the pocket, up the side of the neck, and behind the ear to the location where the electrode was buried, using a special tunneling device. Through this tunnel, an extension wire is passed and connected to the DBS electrode on one end and the stimulator on the other. The stimulator is then tested to make sure that it is working properly and is connected correctly to each DBS electrode. The incisions are then closed with sutures. All parts of the DBS system are internal, and nothing is outside of the skin.
For stage II, most people are able to go home as soon as they wake up from surgery. Prescriptions for oral pain medications will be given to help make you comfortable. Rarely, the pain is so intolerable that a person will need to be admitted for further observation. Again, make sure that you have someone with you for this surgery who will be able to drive you home. We also recommend that someone stay with you for a few days after surgery to make sure there are no complications.