TEN
Stimulator Battery Maintenance and Checkups
In Chapter 8, we discussed what happens at the initial programming visit. After arriving to the clinic in the morning, the DBS programmer checks all of the contacts at the tip of the DBS lead to find the “sweet spot,” the place where stimulation has the best effect on your symptoms with the least amount of side effects. If you have Parkinson’s disease, this visit is done “off medications,” that is, it is done without taking your Parkinson’s medications the night before. If you have essential tremor or dystonia, you may take your medications in the morning. All subsequent programming visits for people living with Parkinson’s are usually able to be done in the “on” medication state, although some centers may still occasionally have you come in “off” medications to troubleshoot problems.
In general, you may have several visits over the first 6 months after the initial programming (see Chapter 8) if you have essential tremor or Parkinson’s disease. For people with dystonia, it may take weeks for you to notice an improvement with a stimulator change. As a result, dystonia programming visits are spread out more, maybe once every 4 weeks or so. No matter if you have Parkinson’s, tremor, or dystonia, once your stimulation parameters have stabilized, the follow-up DBS checkup visits are spread further apart. The DBS checkup visit schedule may end up being once every 3–6 months for people with Parkinson’s and once every 6–12 months for people living with essential tremor and dystonia. More frequent checkups may be needed as the battery nears its end of life.
WHAT HAPPENS AT A DBS CHECKUP?
The main purpose of a DBS checkup is to check the stimulator battery. Unfortunately, the existing stimulators on the market do not have a warning beep or warning light to let you know the stimulator battery is failing. However, the DBS neurologist or programmer can quickly check the stimulator and see whether the battery is failing. This is often called “interrogating the stimulator.”
When the programmer uses the programming device to interrogate the stimulator, he or she can get a reading on your battery. Depending on the model of your stimulator, the readings are slightly different. With the Soletra model made by Medtronic, Inc., the battery level stays at 3.72 V for most of the life of the battery. When the battery level starts to fall below 3.70 V, then the programmer knows that the battery is approaching end-of-life. At 3.60 V, the level starts to drop rapidly, and by 3.40 V, the battery needs to be replaced immediately. Different centers have different thresholds at which they do battery replacements. If you can be monitored frequently, and if surgical battery replacement can be scheduled within a day or two, then you can wait until the battery drops to 3.40 V. At some centers, it may take a longer time to schedule surgery, so these centers may opt to change the stimulator battery earlier.
With the Kinetra model made by Medtronic, Inc., the stimulator should be monitored more closely when the battery level reaches 2.44 V and should be replaced quickly when it gets to 2.36 V. The Kinetra has an additional feature in that it will tell the programmer that less than 20% of the battery has been used, or it will say that 45%–70% of the battery has been used.
The Activa PC/RC model by Medtronic, Inc., will let the DBS programmer know that the battery still has life by showing “OK” on the physician’s programming screen. When the stimulator is running low, “ERI” will appear on the physician’s programmer. Once an “ERI” warning appears, there is approximately 3 months before the stimulator battery runs out. It will show “EOL” when the battery life is gone.
A second purpose of the DBS checkup is to make sure that the stimulator is still delivering stimulation to your brain appropriately. The programmer will check your settings to make sure that they are still the same as the end of the previous visit. The programmer can also check if your stimulator has been on the entire time since your last visit or if it has only been on 67% of the time (seen with people with essential tremor because they turn their stimulators off at night). In addition, impedance and amount of current are checked. These are measures of how well the electrical stimulation is being delivered to the brain. The impedance is the resistance of an electric circuit to current and is measured in ohms. If the impedance is high, it could suggest that there is a broken lead or connection problem. If the impedance is really low, it could suggest a short circuit. People can sometimes feel a short circuit if they have consistent electrical shocks along the extension wire or over the stimulator battery.
Finally, the DBS checkup is your chance to tell the DBS programmer or neurologist how you have been doing. If the stimulation settings are not controlling your symptoms quite as well, it may be time to increase them. If you are having side effects, then it may be time to lower the voltage or try a bipolar stimulation configuration to cut down on side effects.
HOW LONG DOES THE STIMULATOR BATTERY LAST?
The battery in the stimulator can last anywhere from 3 to 5 years. This is a wide range, and it is because some people need higher stimulation settings than others. If your symptoms can be controlled with low stimulation settings, the stimulator is likely to last more toward 5 years. If you need higher stimulation settings to control your symptoms, then the stimulator will run out of juice more quickly.
The stimulators of individuals with essential tremor tend to last the longest. This is because, typically, tremor can be controlled at lower stimulation settings. In addition, people living with essential tremor are instructed to turn their stimulators off at night. Why? The main problem in essential tremor is shaking of the hands, which interferes with the ability to use them. As a result, people may be unable to write, eat, or drink from a cup with one hand, etc. When people with essential tremor are sleeping, they do not need to use their hands, so the stimulator can be turned off. They can then turn it back on in the morning when they wake up. This cuts down on the amount of time the stimulator is working, and batteries tend to last more than 5 years.
On the other hand, people with Parkinson’s disease will still have symptoms overnight. The slowness and stiffness that occur with Parkinson’s may interfere with the ability to get comfortable when trying to fall asleep. These symptoms may also make it difficult to get up in the middle of the night to go to the bathroom. People living with Parkinson’s who have rest tremors will often say that the tremor prevents them from falling asleep. As a result, people with Parkinson’s are instructed to leave their stimulators on all the time. This allows them to feel more relaxed, and many report better sleep because of the stimulator. Because their stimulators are on all night, the battery generally lasts between 3 and 5 years.
Individuals with dystonia usually need high stimulation settings to help their symptoms. Voltages and pulse widths are typically set higher for dystonia than for essential tremor and Parkinson’s disease. As a result, their stimulators tend to last at most 3 years, although there will be exceptions to this rule.
DBS HANDHELD DEVICE
Soletra Handheld Device (Access Review Therapy Controller)
Each stimulator available on the market has its own handheld device. The Soletra stimulator’s handheld device is called the Access Review Therapy Controller. This device has four buttons on the front, two gray and two blue. The blue buttons to the right are the on and off buttons. The on button is above, and the off button is below. To turn your stimulator on, you would place the Access Review device over your stimulator and press the on button until you hear a beep. Then look at the back. There are three lights to the left that should be green. If the top one is lit and green, then the stimulator is on. To turn the stimulator off, place the Access Review device over your stimulator and press the off button until you hear a beep. Then look at the back. If there is an amber light that lights up on the right side of the controller, then your stimulator is off.
You can check if the stimulator is on by using the bottom gray button on the left. To do so, place the Access Review device over your stimulator and press the bottom gray button until you hear a beep. Then look at the back. If the topmost green light is lit on the back, then it is on. If the amber light on the right is lit on the back, then it is off.
Kinetra Handheld Device (Access Therapy Controller)
The Kinetra’s handheld device is called the Access Therapy Controller. On this device, the on/off buttons are the two blue buttons in the middle, with the top one being on and the bottom one being off. To turn your stimulator on, you would place the Access Therapy Controller over your stimulator and press the on button until you hear a beep. Then look at the back. There are three lights to the left that should be green. If the top one is lit and green, then the stimulator is on. To turn the stimulator off, place the Access Therapy Controller device over your stimulator and press the off button until you hear a beep. Then look at the back. If the amber light on the right is lit, then it is off.

Access review controller (for Soletra)
The Access Therapy Controller has four gray buttons with arrows on them. The two buttons on the left are for controlling the right side of the body, whereas the two buttons on the right are for controlling the left side of the body. These buttons can be set by the DBS programmer to allow you to increase your voltage up or down. If the DBS programmer does not enable this function, you can use any of the gray buttons to check if your stimulator is on.

Access devices, back side
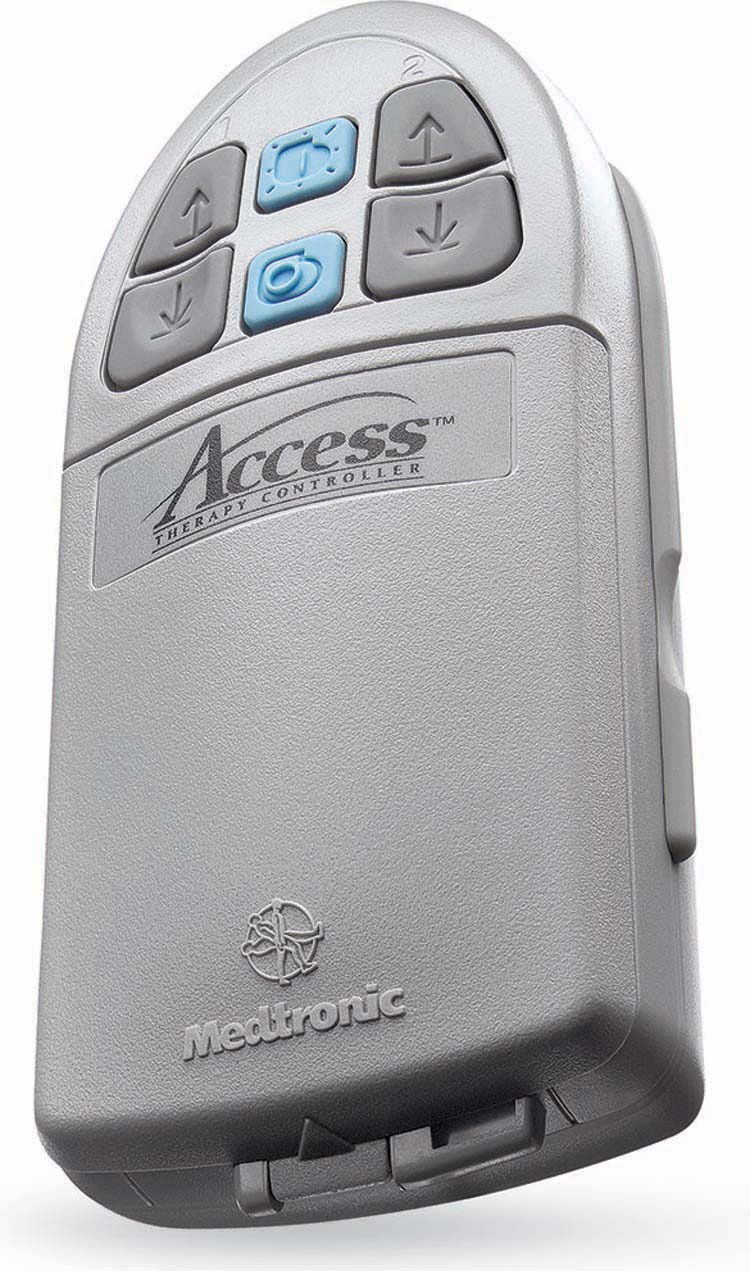
Access therapy controller (for Kinetra)

Patient programmer (Activa PC/RC)
Activa PC/RC Handheld Device (Patient Programmer)
The handheld device that comes with the Activa PC or RC stimulators is called the Patient Programmer and looks different from the other handhelds. It has a simple and advanced mode. The simple mode allows you to check the status of your stimulator battery and turn it on or off. The advanced mode can be set by your neurologist and will allow you to change your stimulator settings or toggle between preset settings.
To turn your stimulator off with this device, hold the Patient Programmer over the stimulator while pressing the gray “On/Off” key located at the top left corner of the device. The display screen on the handheld device will say “On” or “Off” depending on whether the stimulator is on or off. You can also use the orange “check” button at the top right of the device to check if your stimulator is on or off. To do this, simply hold the Patient Programmer over the stimulator while pressing the orange “check” button and then looking at the display screen.
Changing your stimulator settings or switching between preset settings is a little more complex. If you and your neurologist decide that having these options would be helpful for you, your neurologist should explain how to switch your stimulator settings using the device.
REPLACING THE STIMULATOR
Replacing the stimulator is a relatively simple operation that is done on an outpatient basis. It is usually performed under general anesthesia so that you are completely comfortable. In the operating room, you will be placed on the operating table, and the skin over the stimulator will be thoroughly cleaned and sterilized. An incision is made at the stimulator site, which is usually in the chest. The original incision site is reopened. After the incision is made, the old stimulator is removed. Once the old stimulator is removed, the new stimulator can be placed in the same skin pocket in the same location under the skin. Care is taken when placing the new stimulator to be sure not to damage the extension lead where it attaches to the stimulator. The incision is usually closed with sutures, but surgical adhesive or staples can also be used.
Because this is a simple outpatient procedure, you can plan on being discharged from the recovery room after you are feeling well. Prior to discharge, the new stimulator will be set back to your old stimulator’s settings. Once you are awake, and without nausea or other adverse effects, you will be discharged to home. You will experience some pain and swelling at the incision and stimulator site. Prescriptions for mild pain medication are given upon your discharge. You will also need to have someone drive you home. Upon discharge, you will be given instructions about resuming activity, diet, and medication.
Once you are home, make sure to become familiar with the instructions given to you. You should not drive until your physician gives approval. You should be active, but avoid exaggerated movements such as swinging a golf club or vacuuming.
The risks related to replacing the stimulator are low. The most significant risk is infection. Infection can occur despite administering antibiotics in the operating room. Signs of infection are redness at the stimulator, drainage, increased swelling, and fever. Infections are treated aggressively so that they do not result in having to remove the entire DBS. If you suspect an infection, it is important that you call your surgeon immediately.
Another risk to consider is possible damage to the extension wire where it is connected to the stimulator. As discussed in previous chapters, the extension wire is a tube that encases four tiny wire within. Extreme care must be taken to avoid damaging these tiny wires when disconnecting from the old stimulator and connecting to the new stimulator. If the extension gets damaged, it will need to be replaced surgically.