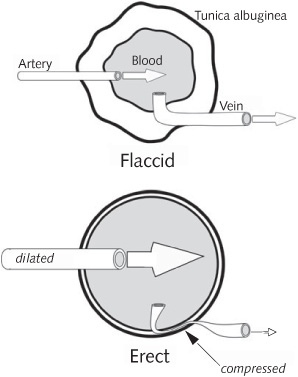
SEXUAL STIMULATION OF THE penis or psychogenic (cognitively induced) arousal activates specialized nerves that travel from the pelvic region of the spinal cord to the penis. These nerves release nitric oxide (NO) and other nerve products (neurotransmitters) that relax the smooth muscles and blood vessels of the penis (smooth describes muscles that, unlike skeletal muscles, are not under our voluntary control). Relaxation of these muscles allows increased blood flow into the penis. Spongy tissues (the corpora cavernosa) in the penis become filled (engorged) with blood and expand rapidly. There is a capsule (the tunica albuginea) that surrounds the internal penile tissues, which is made of connective tissue and is flexible but not stretchable. When the corpora cavernosa become engorged with blood, they “inflate” against the capsule, making the penis rigid. The compression inside the penis almost totally closes down the veins that drain blood from the penis, so blood is trapped in the penile tissues, maintaining the erection.
Because erection is so dependent on an adequate blood flow, the condition known as erectile dysfunction can provide an early warning sign, or red flag, for impending vascular (blood vessel) disease. Erectile dysfunction in men who have no other symptoms of vascular disease may be a marker of a “silent” vascular disorder, especially coronary artery disease, and this has become an important new means of identifying men at risk for such disease.
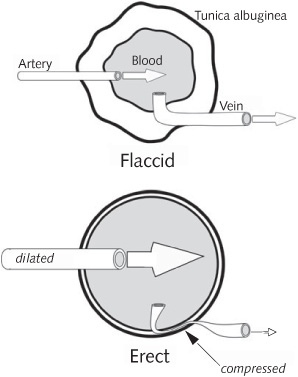
Penile erection. Erection occurs as a result of a two-stage process. The top diagram shows (in cross section) the penis before erection. In the first stage of erection, the arteries that supply the penis dilate, allowing more blood to enter and fill the open spaces (“sinuses”) of the penis The amount of inflation is limited by a flexible but non-expandable membrane (like a mylar balloon), the tunica albuginea, which envelops the penile tissues. In the second stage of erection, the veins that drain blood from the penis get squeezed almost shut against the tunica albuginea. The resulting pressurized accumulation of blood in the penis produces the erection.
EJACULATION REQUIRES PRECISE COORDINATION among several different organs, from the testicles to the penis. Two intriguing aspects of ejaculation are: First, how exactly are the spurts of semen produced? Second, is the pleasurable sensation of orgasm a consequence of the sensory activity produced by the mechanics of ejaculation, or is it mainly a brain phenomenon that is pleasantly enhanced by the sensory activity generated by the expulsive flow of semen at ejaculation? This is a case in which understanding the structure of a system is key to understanding its function.
From a purely mechanical standpoint, contraction of the muscles of the male genital system is, by itself, not strong enough or sudden enough to account for the emission of semen in spurts. Instead, the spurts are produced by precise timing between muscle contractions of the ejaculatory duct system and the sphincter muscles (valves that act much like purse strings) situated in the path of the semen flow. In sequence, this is what happens: (1) the ducts fill with semen (the process of “emission”); (2) pressure builds up behind a closed sphincter valve (the semen-filled duct and the sphincter together are aptly called the “pressure chamber”); (3) a sudden release of the sphincter valve emits a spurt of semen (“ejaculation”); (4) the ejaculatory ducts fill up again behind the re-closed sphincter; and (5) a repeat of the process results in another spurt of semen. This sequence of events repeats several times in rapid succession in a matter of a few seconds.
The initial, emission, stage in the ejaculation process is produced by contractions of the muscles in several places: in the capsules of the testicles, seminal vesicles, and prostate, and in the ducts of the epididymis and vas deferens. The vas deferens contracts as a unit, from one end (at the caudal, or tail-end, epididymis) to the other (at the ejaculatory duct of the prostate); the seminal vesicles contract by peristalsis (traveling waves of muscle contraction and relaxation that propel the semen through this tubular organ).
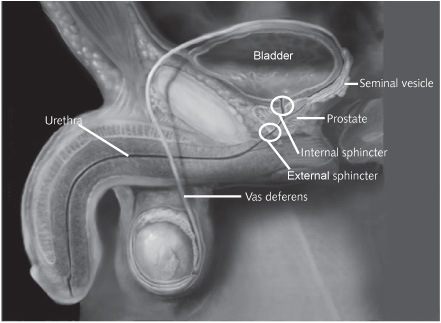
The path taken by sperm during ejaculation. Sperm travel from the testicles through the vas deferens (one on each side) to exit the body through the urethra. The seminal vesicles and prostate contribute the seminal fluid that carries and nourishes the sperm. The external and internal sphincters consist of rings of muscle that surround and squeeze shut the urethra. Contractions of the vas deferens tubes and the seminal vesicles during sexual stimulation, building up to ejaculation, increase the pressure against the closed sphincters. At orgasm, the external sphincter relaxes rhythmically, enabling the pressurized semen to be released in spurts. (Image courtesy Alexander Tsiaras, TheVisualMD.com)
Contraction of the internal sphincter prevents the backflow of semen into the bladder. If this sphincter fails to close sufficiently during ejaculation, semen can make a U turn and enter the urinary bladder, a process known as “retrograde ejaculation.”
At orgasm, under the control of the pudendal nerves, the pelvic muscles start contracting rhythmically and involuntarily. A sphincter opens and closes in closely coordinated timing with the contraction of specific muscles. The intermittent opening and closing aids in propulsion of the semen through the urethra. Studies have shown the importance of the coordination of the opening and closing of this sphincter. If the sphincter becomes paralyzed or is incapacitated by experimental anesthesia, a dripping seminal emission, rather than ejaculation, occurs.
GILES BRINDLEY NOTED IN 1983 that ejaculation and orgasm don’t necessarily require erection. In Brindley’s studies, men were equipped with a mechanical clamp that squeezed shut the pudendal arteries—the arteries that supply blood to the penis. The men were still able to ejaculate and experience orgasm, even though the penis remained entirely flaccid (non-erect). In other words, the nerves that convey sensations from the penis during stimulation do so whether the penis is erect or flaccid. Many men who have had surgery for prostate cancer are able to experience orgasm without erection (men with successful nerve-sparing prostate surgery will most likely continue to have erections).
SOME MEN EXPERIENCE GREATLY increased sensitivity (hypersensitivity), and even pain, of the penis after orgasm. The physiological basis for this hypersensitivity is not known. During penetrative sex, the friction of the skin of the penis against the walls of the vagina (or other surface) could make the skin sensitive. There is some evidence that release of the hormone prolactin into the bloodstream at orgasm may increase the sensitivity of the penis, as well as the nipples.
There is no consensus among researchers as to whether circumcision at infancy affects the sensitivity of the penis. Abnormally low penile sensitivity, as a result of trauma to the genital region, injury to the penile sensory (pudendal) nerves, or diabetes, can result in erectile dysfunction.
YES, MOST MEN HAVE experienced orgasm without obvious penile stimulation, while asleep (commonly known as wet dreams, or more technically as nocturnal emissions). In rare cases, men have reported experiencing orgasm without mechanical (e.g., tactile) stimulation while fully awake. According to an extensive study by Kinsey and his colleagues in 1948, three or four men in five thousand claimed to have experienced ejaculatory orgasm without mechanical stimulation while awake. Some men who practice a specialized form of forced rapid deep breathing combined with Tantric meditation (“fire breath”) claim that they experience orgasms in the absence of physical genital stimulation.
YES, MEN CAN EXPERIENCE orgasm with no ejaculatory fluid expelled, and they can ejaculate without feeling the pleasure of orgasm.
There are certain conditions that prevent ejaculation despite an erection and orgasm. These include surgery affecting the genital system, such as prostatectomy (removal of the prostate gland, typically as a treatment for cancer); certain psychiatric conditions, such as obsessive compulsive disorder (for example, when a man is overly concerned about hygiene and thinks ejaculation will be messy); psychological/psychosexual issues, such as fear of impregnating a partner, fear of losing control, or cultural inhibitions; and side effects of certain medications such as SSRIs (selective serotonin reuptake inhibitors), which are prescribed as antidepressants (for example, citalopram or fluoxetine). Although SSRIs and other medications can interfere with sexual desire and function, individuals should not discontinue these medications without consulting their physician, because serious complications could result. Interference with ejaculation may also result from a progressive neurological disease such as MS (multiple sclerosis), from neurological damage resulting from stroke or spinal cord injury, or from hormonal deficiencies.
By contrast, there are some conditions in which a man can ejaculate in the absence of erection or orgasm. These include severe cases of premature ejaculation (early ejaculation), in which the man ejaculates before developing an erection or before physical stimulation of the penis; psycho-logical factors, such as overexcitement, fear of intimacy, or relationship issues; psychiatric disorders such as severe schizophrenia; complications after surgery involving the genital system; and other conditions such as hormone imbalance, progressive neurological disorders, chronic diabetes, abuse of drugs or alcohol, and brain or spinal cord injury.
Some men voluntarily separate their orgasm from ejaculation. They do so by noting the point after which they can’t hold back (the point of “ejaculatory inevitability”) and training themselves to control their ejaculation just before reaching this point. By delaying ejaculation in this way, they claim to experience an enjoyable, prolonged sexual session with their partner, with a deeper and more intense sexual intimacy. An example of this practice is the teaching of Tantric sex, through which a man learns to be orgasmic while delaying ejaculation until he feels ready.
NOBODY KNOWS FOR SURE. However, sleepiness in men after orgasm is very common. The physical exertion of sexual intercourse can feel as if it’s considerable, but a 175-pound man participating in vigorous sex for thirty minutes expends only 63 calories. If he had spent the same amount of time jogging, he would have used 288 calories (and most joggers claim to feel energized, not sleepy, after their run). So, it’s probably something other than physical exertion that accounts for the sleepy feeling after orgasm. We do know that women seem to feel less tired than men after orgasm. Men share their tendency to want to doze with at least one other mammal. Carefully constructed laboratory studies showed that male rats fall deeply asleep shortly after mating (but, so do female rabbits!).
In one study, of five men and five women, researchers compared three conditions: masturbation to orgasm with a latency of about fifteen minutes; masturbation for fifteen minutes, while intentionally refraining from orgasm; and reading a newspaper for fifteen minutes. They found no significant difference among the three conditions in the time delay between the event and when the person fell asleep, or in the duration of sleep, or in the type of sleep pattern. However, this study was just a start, not an ideal way to study this topic. Many disruptive factors could account for the lack of difference among the three conditions in the study, including the laboratory setting, the fact that an investigator entered the room after every fifteen-minute period to remove the anal probe used to measure orgasmic muscular contractions, the presence of EEG (electroencephalogram) electrodes to measure sleep, the possible sleep-inducing effect of reading a newspaper, the combining of the data for the men and the women, and the absence of the personal physical and emotional interactions inherent in sexual encounters. So, with our present state of knowledge about any connection between orgasm and sleep, anecdotal reports, jokes, and cartoons appear to characterize reality better than does the existing scientific research!
Still, even though science has yet to offer a satisfactory explanation for the widely reported tendency of men (and some women) to become sleepy after orgasm, at least knowing that this sleepiness is so common offers some comfort to those who may “take it personally.” As humans, many of us have the capacity to generate a modicum of conversation and hugging and caressing in the aftermath of orgasm, at least for a while. To our male readers, especially, we suggest giving it a try. An interlude of post-orgasm tender bonding—even if only briefly, before sleep over-whelms—doesn’t hurt.
SECRETION OF THIS PRE-EJACULATORY fluid, which in some cases starts during sexual foreplay, can be surprisingly abundant—half to one milliliter (1 mL is about one-fifth of a teaspoonful). The presence of this fluid is evidence of a high level of sexual arousal. For many years it was associated with voluptuous thinking, and medieval writers called it “the distillate of love.”
Long before the nineteenth century, when William Cowper described the glands involved in this secretion, the secreted fluid was recognized as being different from semen. There is now good evidence that the secretion comes from a small set of structures named Cowper’s glands, in honor of their discoverer (and also called the bulbo-urethral glands). Cowper’s glands, together with the prostate and seminal vesicles, comprise the “sex accessory” glands in men. Cowper’s glands are the male counterpart of women’s Bartholin’s glands (or greater vestibular glands), which produce some of the vaginal fluid.
The secretion from Cowper’s glands is composed of a clear fluid with a high concentration of glycoproteins (proteins with some sugars attached). The fluid neutralizes the acidity of the urine residue in the man’s urethra and the normal acidity of the vaginal environment. It may also provide lubrication for the penis during intercourse. For some time it was thought that this secretion could contain some stray sperm that escape from the epididymis before ejaculation, and that this could explain unexpected pregnancies during coitus interruptus (a contraceptive technique in which the man withdraws his penis from the vagina before ejaculating). However, recent studies have shown that the pre-ejaculatory fluid that leaks from the tip of the penis during sexual stimulation does not contain any sperm.
SEMEN (ALSO CALLED SEMINAL fluid, seminal plasma, or ejaculatory fluid) consists of a combination of secretions from the testicles, epididymis, vas deferens, seminal vesicles, prostate, and Cowper’s glands.
When the free-swimming sperm cells (also called spermatozoa) leave the testicles (where they are produced), they enter, on each side, a long, convoluted tube—the epididymis—situated above the testicles. The sperm are mixed with a fluid secreted by the epididymis and testicles, and this mixture moves slowly toward the vas deferens, a slightly wider tube than the epididymis. (The paired vas deferens tubes, left and right, are the tubes that are “tied” in the vasectomy procedure.) After passing through the vas deferens on each side, the sperm and fluids enter the urethra, the tube that also transports urine from the bladder. During this journey, the sperm acquire their capacity to fertilize the ovum (a process termed “capacitation”). This involves a series of physical and chemical changes in the “head” of the sperm (the acrosome, as distinct from the sperm’s moving tail). The semen is therefore a mixture of various fluids; it conveys the sperm.
The fluids that comprise semen serve a variety of functions. They provide for more powerful ejaculation and contain a source of energy for the vigorously swimming sperm, in the form of fructose (a sugar) and inositol (another type of nutrient). The semen also contains pros-taglandins (secreted by the prostate gland), which stimulate contraction of the muscles of the female reproductive tract, assisting the sperm in their voyage toward the egg (ovum).
The normal color of ejaculatory fluid is a semitransparent yellowish color. If any major changes occur in the color or texture of ejaculatory fluid (for example, becoming orange, thick and white, or with drops of blood), it’s advisable for a man to consult his physician. A physician should always be alerted if ejaculation is combined with a feeling of urgency to urinate, a burning sensation when urinating, or pain, because these may be signs of a urinary tract infection or an STI (sexually transmitted infection), which, if untreated, could lead to kidney damage or other serious complications.
EJACULATED HUMAN SEMEN TYPICALLY appears opaque—a grayish-white mass mixed with a clear liquid. The mass consists of protein that is coagulated (jelled) by an enzyme secreted by the seminal vesicles. The clear liquid is secreted mainly by the prostate gland and Cowper’s glands.
Within about ten to twenty minutes of ejaculation, the opaque mass begins to change into a clear liquid. This change is due to the action of another enzyme, known as seminin, that is secreted into the semen by the prostate gland. This enzyme gives a characteristic aroma to the semen. As an aside, “seminin” is another name for “prostate-specific antigen,” or PSA. The level of PSA in the bloodstream is commonly used to screen for prostate cancer. The normal function of PSA—or seminin—is to liberate the sperm from the coagulated semen so that the sperm cells are free to move toward the egg.
Evidence suggests that the coagulated mass in semen restricts the free movement of the ejaculated sperm, which probably has the effect of “herding” them, keeping them near the cervix, which is the gateway to the uterus. Thus the semen helps keep the sperm from flowing out of the vagina. Then, seminin starts to convert the coagulated mass into a clear liquid (a process called liquefaction), allowing the sperm to swim out of the mass and enter the uterus on their way to the egg.
This coagulation function of semen is developed to an extreme in some rodents. In these animals, coagulation forms a “copulatory plug” almost instantaneously after ejaculation into the vagina. The copula-tory plug has the texture of dried rubber cement. It forms a hard piston that fills the inner end of the vagina just in front of the cervix, trapping the sperm, under pressure, between the tip of the plug and the cervix. The pressure forces the semen and sperm through the cervix and into the uterus.
THE PROCESS OF EJACULATION in men has been investigated by numerous techniques, including genital physiological recordings, genital imaging, and brain imaging. Several genital organs contribute to semen. A typical orgasm produces about five milliliters (5 mL; about one teaspoonful) of semen, which has the following components: sperm cells and secretions from the seminal vesicles (3 mL), prostate (1.5 to 2 mL), Cowper’s glands (0.5 mL), and glands of Littre, also known as preputial glands (0.1 to 0.2 mL). The amount, aroma, taste, texture, density, and color of semen vary from person to person and from time to time in each individual. Temperature, physical activity, diet, and recent ejaculations can also affect the properties and amount of the fluid. In the case of two closely successive ejaculations, the second volume is typically less than the first.
MEN’S SEXUAL BEHAVIOR AND sexual function, including orgasm, are influenced by the action of hormones. A man’s natural steroid hormones, in particular, affect sexual processes. These hormones are secreted into the bloodstream by the gonads (testicles) and by the adrenal glands (specifically, the part of the gland known as the adrenal cortex). The term steroid refers to their chemical structure, and this family of chemicals includes the sex steroids (androgens, estrogens, and progestins) and the corticoids (which are secreted by the adrenal cortex). By far the most important male hormone is testosterone, an androgen, which is secreted almost exclusively by the testicles. Castrating males (surgically removing the testicles) greatly affects their sexual functioning.
Castration has been carried out in men and animals since prehistoric times. It’s a relatively easy operation, because of the accessibility of the testicles, and was practiced by several cultures for its biological and psychological effects. In the middle of the nineteenth century, it was observed that castration of roosters not only induced physical changes but also inhibited their sexual behavior. Early scientists found that the effects of castration could be reversed when a testicular graft was placed into the castrated rooster. This type of experiment has been repeated in many mammalian species, including humans, with the same results. Indeed, the rooster experiment is credited with creating the entire field of endocrinology (the study of hormones and their effects). Despite these known effects of drastically reducing testosterone levels by castration, normal levels of testosterone do not guarantee normal sexual behavior and orgasm.
It isn’t always possible to establish a clear correlation between levels of testosterone circulating in the bloodstream and sexual activity (desire, arousability, and orgasm), but we do know that a clear and abrupt decrease in sexual interest may occur in healthy men when treated with drugs that inhibit their testosterone secretion.
We also know that medical treatment with testosterone affects orgasms. In men, aging is often associated with a lowered secretion of testosterone, and sexual disorders including anorgasmia (inability to have an orgasm) can occur. According to a recent study, 30 percent of men over the age of sixty have clear signs of what is known as hypogonadism (low levels of androgen secretion). Currently, testosterone is the usual treatment for these men, and most studies indicate a clear improvement in sexual life following administration of the hormone. Injections of a long-acting chemical derivative of testosterone (testosterone undecanoate) have often been used successfully to improve men’s sexual activity and ability to experience orgasm. In more recent studies, testosterone has been administered transdermally (through the skin), by a skin patch that delivers constant, low amounts of the hormone into the bloodstream. Although there is no doubt that testosterone improves sexual life in hypogonadal men, it’s not clear how it works, whether through its action on brain structures related to sexual desire and orgasm or, indirectly, by increasing physical energy and/or by maintaining the genital structures.
There has been some controversy about the side effects of testosterone treatments for men with hypogonadism. Some researchers worry, for example, that the treatments might activate dormant prostate cancer in older men or might cause immunodeficiency. In the United States, a controversy between the Endocrine Society and a National Institutes of Health panel occurred only a few years ago on this topic. In recent well-controlled studies using the dosages actually used for treatment of hypogonadism, no serious side effects occurred. Indeed, positive effects on cardiovascular health were reported when proper doses of testosterone were administered. However, most physicians are not likely to prescribe testosterone for men who have undergone treatment for prostate cancer.
There is no consensus on whether testosterone can act as an aphrodisiac. Some studies have reported that testosterone administered to men with normal levels of testosterone can increase sexual enjoyment and activity. However, other studies suggest there is no benefit to increasing the androgen level beyond that of normal secretions by the testicles.
At the other extreme, treatment with certain steroids has been used to inhibit undesired male sexual behavior, such as pedophilia (sex with children), with variable success. For example, a synthetic progestin (medroxy-progesterone) has been reported to inhibit undesired sexual behavior. It acts by inhibiting the secretion of the pituitary hormones that maintain the production of testosterone by the testicles. Another way to decrease unwanted sexual activity is by the use of drugs known as anti-androgens (such as cyproterone acetate), which don’t affect testosterone secretion but instead prevent the action of the hormone in the brain, by preventing its interaction with specific receptors in brain neurons and other cells.
In yet another use of steroids, for more than thirty years, men of all ages have been using anabolic steroids (androgens that stimulate protein synthesis, particularly in muscle) for bodybuilding. One of these steroids is 5-alpha-dihydrotestosterone (DHT), which is a normal metabolic product of testosterone. In most experimental animals, anabolic steroids such as DHT are much less potent in stimulating sexual behavior than is testosterone, and apparently the same is true in men. Some recent studies, however, indicate that when administered together with estrogen, DHT can be used to treat male anorgasmia and several other types of sexual disorder.