Chapter 14
Psychotherapy for Children and Adolescents
John R. Weisz, Mei Yi Ng, Christopher Rutt, Nancy Lau, and Sara Masland
Efforts to help children and adolescents (henceforth “youth”) overcome behavioral and emotional problems are certainly as old as parenthood, but help in the form of psychotherapy may be traced back only about a century (Freedheim, Freudenberger, & Kessler, 1992). The work of Sigmund Freud (1856–1939) was pivotal, including his notion that even young children can be appropriate candidates for therapy. Classic steps in the birth of psychotherapy for young people included Freud's consultation with the father of “Little Hans” and his psychoanalysis of his own daughter, Anna (1895–1982), who became a prominent child analyst in her own right.
The rapid growth of youth psychotherapy was fueled by Freud's intellectual heirs and by models and methods very different from those of psychoanalysis, including an approach called “behaviorism.” Mary Cover Jones (1924a, 1924b), for example, used modeling and “direct conditioning” to help a 2-year-old boy overcome his fear of a white rabbit, thus helping launch a behavioral revolution in therapy. Psychoanalytic and behavioral therapies for young people developed alongside other treatments sparked by the grand theories of psychology and the humanistic tradition. Later Beck and colleagues helped develop cognitive therapy (e.g., Beck, 1970), and Meichenbaum and colleagues (e.g., Meichenbaum & Goodman, 1971) helped launch cognitive-behavioral therapy (CBT) for children. By the late 20th century, youth psychotherapy had mushroomed dramatically. Indeed, Kazdin (2000) identified 551 different named therapies used with children and adolescents. Even this large number greatly underestimates the array of approaches used in practice, with hundreds of thousands of practitioners eclectically blending their different training backgrounds and theoretical orientations to form distinctive approaches unlike those of any other practitioner.
In this chapter we describe the field of youth psychotherapy that has grown up over the past century, emphasizing what research has shown and what remains to be learned. We begin by noting some of the factors that make psychotherapy different with youths than with adults. We describe strategies for studying youth psychotherapy and its effects, including meta-analytic approaches to synthesizing findings across multiple studies. In a section on evidence-based youth psychotherapies, we note how these are defined and identify the treatments identified as evidence-based in a recent series of systematic reviews. This is followed by a section on understanding how, with whom, and under what conditions the evidence-based therapies work—which requires a focus on the study of mediation and moderation. This is followed by a discussion of family factors in youth psychotherapy and efforts to test youth therapies with various population groups that are at special risk. We then view the field from the perspective of a friendly critic, noting limitations of current approaches and suggesting a series of strategies for strengthening youth treatments.
Psychotherapy With Youths Versus Adults: Some Key Differences
Although adult and youth psychotherapy have overlapping ancestry and are similar in many ways, important differences warrant attention. First, most treatment of boys and girls is prompted by parents, teachers, or other adults. It is adults who typically seek professional help, initiate the youth therapy, identify some or all of the referral concerns and treatment goals, pay the bills (or obtain the insurance coverage), and make the final decision as to how long therapy will last. Young people do participate as the “patients,” but the concerns they identify may not agree with those of their parents or other adults, and evidence suggest that they exert less influence than these adults on the focus and direction of therapy (Hawley & Weisz, 2003; Yeh & Weisz, 2001). With the impetus for youth psychotherapy coming mainly from adults, and adults influencing the goals of that therapy more than the youths, perhaps it is not surprising that youngsters often begin therapy with relatively low motivation for treatment. This can mean that a large component of youth therapy is engagement—that is, efforts by the therapist to build rapport, motivation, and a good therapeutic alliance with the young person.
Youth and adult psychotherapy also differ in the information sources available to therapists for planning treatment and tracking how it is going. Therapists working with young people almost invariably deal with information from their young patient as well as adults in the youngster's life—parents and teachers, for example. These different informants typically do not show very high concordance in the youth problems and strengths they report (Achenbach, McConaughy, & Howell, 1987; De Los Reyes, Goodman, Kliewer, & Reid-Quiñones, 2010; Richters, 1992). The accuracy of youth self-reports is limited by constraints on self-awareness and expressive and language ability. The accuracy of adult reports may be limited by lack of opportunity to observe youths in multiple settings, the effects of parents' own life stresses or mental health problems (see e.g., Kazdin & Weisz, 1998), and even by undetected agendas (e.g., high problem levels reported by adults who are desperate for help, or low levels reported by those who fear child protective services). Additionally, adults' reports of youths' behavior and reasons for referral can reflect the values, standards, practices, and social ideals of their cultural reference group (see Weisz, McCarty, Eastman, Chaiyasit, & Suwanlert, 1997). In sum, because youth therapy involves multiple stakeholders, each with different motivations, perceptions, and goals, assessing treatment needs, progress, and outcomes via information from these different stakeholders can magnify complexity in a way that appears less likely with adults.
Finally, boys and girls, much more than adults, are dependent on—and thus captives of—their externally engineered environments. Their family, neighborhood, and school contexts are largely selected and shaped by others, and in fact the “pathology” being treated may sometimes reside less in the youth than in the environment, which the youngster can neither escape nor alter significantly. The powerful impact of such factors as who lives in the home, how these people interact, what financial resources they have, and whether outside agencies (e.g., for child protection) are involved, may limit the impact of interventions that focus on the youth as solo or primary participant, highlighting a need to involve key members of the youth's social context in intervention (see, e.g., Henggeler, Schoenwald, Borduin, Rowland, & Cunningham, 1998), and sometimes making case management as salient as psychotherapy.
Studying the Effects of Youth Psychotherapy
Given the differences noted between youth and adult psychotherapy, it should be no surprise that separate treatments—albeit heavily influenced by adult approaches—have evolved for young people, together with a separate body of treatment outcome research. In contrast to the acceleration of youth psychotherapy practice over the past century, research tests of youth therapies took shape quite slowly, and only after a rough start. In 1952, Eysenck published a classic review of adult psychotherapy studies, raising serious doubts about whether therapy was effective. A few years later, Levitt (1957, 1963) reviewed treatment outcome research that included young people and concluded that rates of improvement in the youth samples were about the same with or without treatment. The studies available for those landmark reviews were irregular in quality. Treatment outcome research has grown more rigorous since those early days, treatments have evolved, and the number of youth outcome studies has increased dramatically, particularly in recent decades (see Silverman & Hinshaw, 2008; Weisz & Kazdin, 2010). The focus of youth treatment research has also sharpened over time, with a shift from studies of unspecified “treatment” for often vaguely specified youth problems to tests of specific, well-documented therapies for specific problems and disorders.
The benefit derived from youth treatment is often assessed in randomized controlled trials (RCTs), and these RCTs are often pooled and synthesized in meta-analyses (see later). Multiple baseline designs, ABAB (sometimes called reversal) designs, and other single-subject approaches are useful, as well. These approaches (well described in Barlow, Nock, & Hersen, 2009; Kazdin, 2011) have been used in a variety of youth treatment situations—such as programs for attention-deficit/hyperactivity disorder (ADHD; see, e.g., Pelham et al., 2010), studies where an entire classroom needs to receive an intervention (see, e.g., Wurtele & Drabman, 1984), and cases (sometimes involving rare conditions) where only one or two youngsters will be treated (e.g., McGrath, Dorsett, Calhoun, & Drabman, 1987; Tarnowski, Rosen, McGrath, & Drabman, 1987). These alternative outcome assessment designs have generated a rich body of outcome data and some useful meta-analyses, for example on treatment approaches for disruptive behavior (Chen & Ma, 2007), autism spectrum disorders (Campbell, 2003), and social skill deficits (Mathur, Kavale, Quinn, Forness, & Rutherford, 1998). However, meta-analyses in the field have most often focused on RCTs.
Meta-Analytic Findings
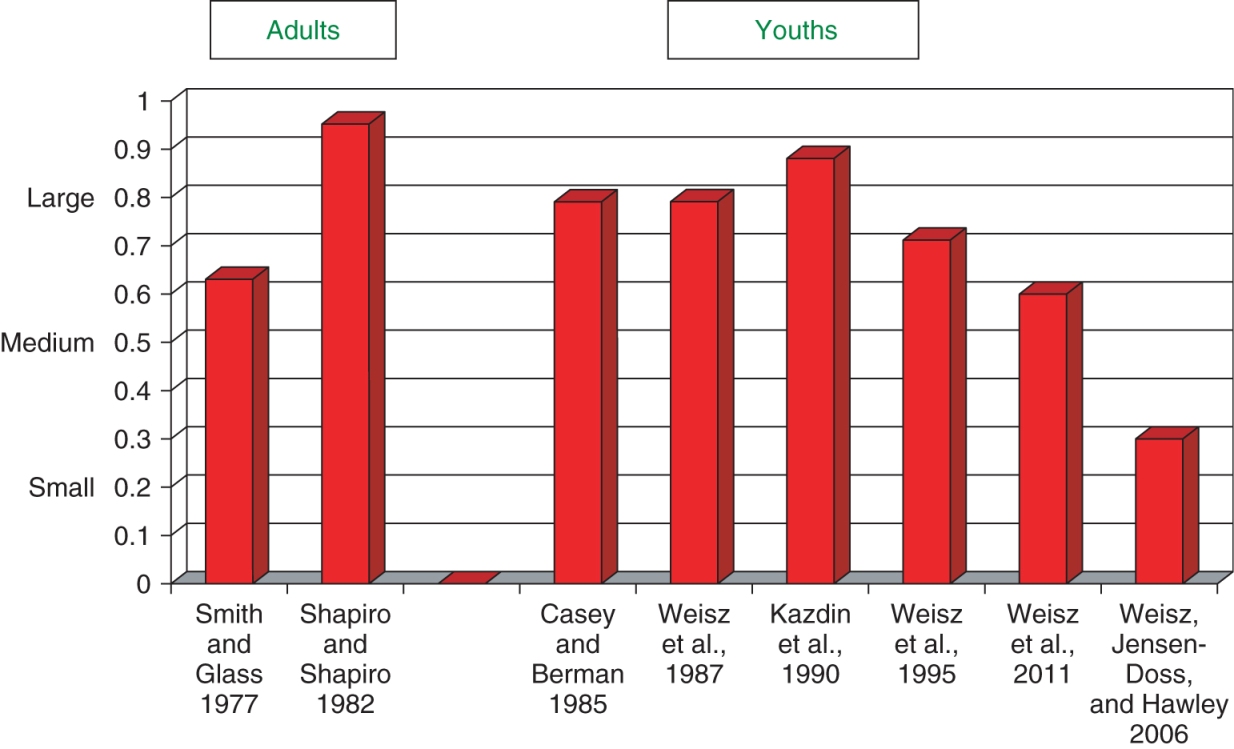
Among meta-analyses of the RCTs, a few have synthesized findings from particularly broad arrays of youth treatments and forms of dysfunction. In four particularly broad-based meta-analyses, encompassing more than 350 outcome studies, the meta-analysts imposed few limits on the types of treated problems or types of intervention that would be included. In the earliest of the four, Casey and Berman (1985) focused on studies with children age 12 and younger. Weisz, Weiss, Alicke, and Klotz (1987) included studies with 4- to 18-year-olds. Kazdin, Bass, Ayers, and Rodgers (1990) synthesized findings of studies with 4- to 18-year-olds. And Weisz, Weiss, Han, Granger, and Morton (1995) included studies spanning ages 2 to 18. Mean effect sizes found in these four meta-analyses are shown in Figure 14.1, with a comparison to two widely cited meta-analyses of predominantly adult psychotherapy (Shapiro & Shapiro, 1982; Smith & Glass, 1977). As the figure shows, the youth treatment effect sizes in Casey and Berman (1985), Weisz et al. (1987), Kazdin et al. (1990), and Weisz et al. (1995) fall roughly within the range of what has been found for adult therapy, and on average within the range of what Cohen (1988) suggests as benchmarks for medium (i.e., .5) to large (.8) effects. The last bar on the right in Figure 14.1 is discussed later in this chapter.
In addition to overall mean effects, two other youth meta-analytic findings sharpen the picture. First, findings (in Weisz et al., 1987; Weisz et al., 1995) indicate that effects measured immediately after treatment are quite similar to effects measured at follow-up assessments, averaging 5 to 6 months after treatment termination. This suggests that youth treatment benefit may have reasonable holding power. Second, findings on treatment specificity have shown that effects are larger for the specific problems targeted in treatment than for related problems that were not specifically addressed (Weisz et al., 1995, p. 460). This suggests that the tested therapies are not merely producing global “feeling better all over” effects, but instead are rather precise in impacting the forms of dysfunction they are designed to treat.
Although these findings suggest certain strengths of youth psychotherapies, meta-analysis can also be used to highlight challenges and critical questions for the field—for example, identifying problems and disorders for which youth treatment effects are modest, suggesting a need to strengthen interventions. Psychotherapies for youth depression, for example, appear to show more modest effects, on average, than treatments for a number of other youth problems and disorders (see Weisz, McCarty, & Valeri, 2006). Meta-analysis has also been used to evaluate the benefits of “evidence-based” psychotherapies, to which we now turn.
Identifying “Evidence-Based Psychotherapies”
As evidence accumulated over time showing beneficial effects of well-documented (typically manual-guided) psychotherapies for youths, adults, couples, and families, efforts were launched to identify the specific therapies sufficiently well-supported to be considered “empirically validated” or “evidence-based.” Various task forces and review teams were formed—notably the APA Division 12 Task Force on Promotion and Dissemination of Psychological Procedures, led by Dianne Chambless (see e.g., Chambless et al., 1998)—to distill the evidence from outcome studies and identify therapies that reached threshold for different levels of empirical support. Building on this work, experts in youth psychotherapy have conducted systematic literature reviews, in some cases including meta-analytic findings, to compile reports on evidence-based psychotherapies (EBPs) for young people (see Lonigan, Elbert, & Johnson, 1998; Silverman & Hinshaw, 2008). In the most recent report, edited by Silverman and Hinshaw (2008), reviewers identified psychotherapies that met criteria for status as well-established (e.g., two good group-design experiments by different research teams in two different settings, showing the treatment to be “superior to pill, psychological placebo, or another treatment”), probably efficacious (e.g., “at least two good experiments showing the treatment is superior…to a wait-list control group”), possibly efficacious (e.g., “At least one ‘good’ study showing the treatment to be efficacious in the absence of conflicting evidence”), or experimental (“not yet tested in trials meeting task force criteria”).
The reviewers in this 2008 report identified dozens of youth psychotherapies as either well-established or probably efficacious, spanning problem areas including early autism, anorexia nervosa, depression, anxiety disorders, ADHD, disruptive behavior problems and disorders, and substance abuse. Taken together, the reviews report a bumper crop of tested treatments, with more abundant lists in some treatment domains (e.g., conduct problems and anxiety) and more limited options in others (e.g., autism and eating disorders). Table 14.1 shows the treatments identified by the reviewers in the Silverman–Hinshaw (2008) special issue at the two highest levels of empirical support for various youth mental health problems and disorders.
Table 14.1 Youth Psychotherapies Identified as “Well-Established” or “Probably Efficacious”1,2. Tables can be downloaded in PDF formats at http://higheredbcs.wiley.com/legacy/college/lambert/1118038207/pdf/c14_t01.pdf.
|
| Table Layout Image |
Early autism
(Rogers & Vismara, 2008) |
Eating disorders in adolescence
(Keel & Haedt, 2008) |
Depression
(David-Ferdon & Kaslow, 2008) |
Phobic and anxiety disorders
(Silverman, Pina, & Viswesvaran, 2008) |
Obsessive-compulsive disorder
(Barrett, Farrell, Pina, Peris, & Piacentini, 2008) |
Youths exposed to traumatic events
(Silverman, Ortiz, et al., 2008) |
Attention-deficit/hyperactivity disorder
(Pelham & Fabiano, 2008) |
Disruptive behavior
(Eyberg, Nelson, & Boggs, 2008) |
Adolescent substance abuse
(Waldron & Turner, 2008) |
Specific Evidence-Based Treatments Identified as “Well-Established” and “Probably Efficacious”
As Table 14.1 shows, interventions for several forms of youth dysfunction were been rated probably efficacious or well-established by the reviewers. For purposes of this chapter, we refer to these interventions in Table 14.1 as evidence-based psychotherapies (EBPs) for youth.
Autism
The only autism treatment rated as a well-established EBP in the review by Rogers and Vismara (2008) was Ivar Lovaas's model of early intensive behavioral intervention (EIBI; Lovaas, 1987; Smith, 2010), which involves individual discreet trials training (30 hours/week or more) to build, then scaffold, an array of specific core skills in such domains as language, self-help, and social interaction. Therapists provide treatment and train parents to conduct the intervention at home. Pivotal Response Training (PRT; Koegel, Koegel, Vernon, & Brookman-Frazee, 2010), rated probably efficacious, uses core skills of the Lovaas model but with an expanded emphasis on intervention in the child's natural environment and finding ways to boost motivation for learning (e.g., by using activities the youngster chooses and by identifying natural reinforcers). The treatment focuses on teaching communication, self-help, and academic, recreational, and social skills; parent training is a key component in reaching these goals.
Eating Disorders
Only one treatment for eating disorders was identified as an EBP by Keel and Haedt (2008). This was family therapy for anorexia nervosa, in particular the Maudsley model (Lock, Le Grange, Agras, & Dare, 2001). This model focuses on (a) “refeeding the client,” a process in which family members work to return the young client to more normal eating behavior; (b) negotiating improved relationships in areas that impact eating behavior [e.g., if the family uses deceit to avoid conflict and the youth hides bingeing through deceit, then therapy focuses on alternatives to deceit]; and (c) termination, which includes ways of sustaining healthy intrafamily relationships, appropriate boundaries, and increased youth autonomy. Keel and Haedt (2008) found no EBPs for bulimia nervosa in adolescents, but they noted that CBT (e.g., addressing distorted cognitions about body shape and size, using behavioral procedures to structure healthy eating habits, and using behavioral exposure to build resistance to triggers that spark cycles of bingeing and overcompensation) is a well-established treatment for bulimia in samples of young adults and older adolescents. A challenge in the eating domain is the array of different forms that eating disorders can take. Symptomatic of the problem is the fact that the most prevalent of all the eating disorder categories is “not otherwise specified.” Thus, even with effective treatments established for anorexia and bulimia, significant work will remain to encompass the full spectrum of dysfunctional eating behavior.
Depression
David-Ferdon and Kaslow (2008) placed two broad approaches to depression treatment—that is, Interpersonal Psychotherapy for Adolescents (IPT-A; Mufson, Weissman, Moreau, & Garfinkel, 1999) and CBT—within the upper two categories of empirical support. IPT-A focuses therapeutic attention on interpersonal issues that are common among adolescents, such as changes in the parent–teen relationship as roles shift; the intervention is designed to help adolescents deal with their difficulties in relation to role transitions and disputes, grief, and interpersonal deficits; an important goal is to help the adolescents develop effective strategies for addressing the difficulties. Although CBT has varied in specific contents across various treatment trials, it typically includes such core components as identifying and scheduling mood-elevating activities, identifying and modifying inappropriately negative cognitions, relaxation training, and learning and practicing problem-solving skills. An approach deemed “behavior therapy” was included among the probably efficacious EBPs for youths (e.g., Kahn, Kehle, Jenson, & Clark, 1990); the contents resembled CBT in most respects.
Anxiety Disorders
For phobic and anxiety disorders in youth (reviewed by Silverman, Pina, & Viswesvaran, 2008), the most extensively tested psychotherapies are the CBTs, which blend graduated exposure to feared stimuli with identification and modification of distorted cognitions that can stimulate and sustain unreasonable fears. Several forms of CBT were rated as EBPs. These included individual youth CBT, group CBT, and group CBT with parents. Silverman, Pina, et al. (2008) also classified Social Effectiveness Therapy for Children (Beidel, Turner, & Morris, 2000) as an EBP. This treatment, designed for social phobia, includes group sessions for the youngsters in treatment, in vivo exposure sessions (including practice interacting with nonanxious peers), and work with parents to help them reward their children's progress toward less anxious behavior in social situations.
In a complementary review, focused only on obsessive-compulsive disorder (OCD), Barrett, Farrell, Pina, Peris, and Piacentini (2008) identified a single EBP: individual exposure-based CBT. The core component is exposure and response prevention (ERP): Youths are repeatedly exposed to stimuli that trigger obsessive fears with the mandate not to engage in the compulsive behavior typically prompted by those fears. Over time, across repeated exposures, obsession-prompted anxiety is thought to dissipate via autonomic habituation. Cognition is considered central, as well, as the youths learn that feared consequences of refraining from the compulsive rituals do not actually materialize.
Finally, focusing on treatment of youths exposed to traumatic events, Silverman, Ortiz, et al. (2008) identified trauma-focused CBT (TF-CBT; Cohen, Mannarino, & Deblinger, 2010) as an EBP. This treatment, designed for youngsters who have experienced sexual abuse and other forms of maltreatment, uses core components of CBT for anxiety, but with important additions tailored to fit the situations in which youngsters have experienced trauma. These include safety planning (to reduce future environmental risk) and the use of a “trauma narrative,” in which young people describe, in writing, their traumatic experiences. The narrative is first created in draft form, then read repeatedly in the presence of the therapist, as a form of exposure therapy. Distorted cognitions are addressed by modifying parts of the narrative—for example, by altering inappropriate self-blaming statements. Caregivers participate in the process, including by joining therapist and youth at later readings of the narrative and offering support for the youth's courage in sharing the story. Silverman, Ortiz, et al. (2008) also identified school-based group CBT (Kataoka et al., 2003; Stein et al., 2003) as an EBP. This treatment, designed for youths who have experienced trauma via exposure to community violence, includes psychoeducation, cognitive and coping skills training, social skills training, and graduated exposures in the form of writing and/or drawing activities.
Attention-Deficit/Hyperactivity Disorder
Pelham and Fabiano (2008) identified three treatments for ADHD as well-established. One was behavioral parent training, in which parents are taught a set of techniques (e.g., clear instructions, differential attention for desired versus undesired behavior, use of praise and reward, time-out) for effective behavior management. A second was behavioral contingency management in classrooms. The third was intensive peer-focused behavioral interventions in recreational settings (e.g., summer day camps). The model program of this type is Pelham's Summer Treatment Program (Pelham et al., 2010), in which youngsters are immersed in sports, academic, and social skill-building activities, all within the context of carefully-structured behavioral contingencies, and complemented by behavioral training and consultation with caregivers. Significantly, Pelham and Fabiano (2008) did not find empirical support for cognitive-behavioral or nonbehavioral treatments for ADHD youths.
Conduct-Related Problems and Disorders (Disruptive Behaviors)
In their review focused on disruptive behavior, Eyberg, Nelson, and Boggs (2008) identified a remarkable 16 EBPs. These included behavioral parent-training programs, some emphasizing parent management training (Forgatch & Patterson, 2010; Kazdin, 2010), some emphasizing real-time coaching during parent–child interaction sessions (e.g., McMahon & Forehand, 2003; Zisser & Eyberg, 2010), and one involving parent training at different levels of intensity delivered within a public health dissemination framework (Sanders & Murphy-Brennan, 2010). A video-guided approach developed by Webster-Stratton and colleagues (e.g., Webster-Stratton & Reid, 2010) includes programs for behavioral training with parents in groups and problem-solving and social skills training with children (ages 3 to 8) in groups; in these programs, shown to be beneficial independently and in combination, participants view and discuss video clips illustrating effective and ineffective strategies and apply what they learn to their own behavior. Other EBPs for conduct problems include cognitive and behavioral training programs to enhance anger management (Lochman, Boxmeyer, Powell, Barry, & Pardini, 2010), problem-solving skill (Kazdin, 2010), and appropriately assertive social behavior (Huey & Rank, 1984), as well as a school-based program, based on rational-emotive theory, designed to reduce disruptive and disobedient behavior by helping youths learn to make accurate cognitive appraisals of self and social situations (Block, 1978).
Finally, two EBPs blend behavioral training for caregivers with methods for engaging others in the youth's social system. These include the extensively studied Multisystemic Therapy (MST; Henggeler & Schaeffer, 2010), developed originally for delinquent youths but extended to treatment of other forms of youth dysfunction (e.g., sexual offending, suicidal behavior), and Multidimensional Treatment Foster Care (MTFC; Smith & Chamberlain, 2010), designed to provide effective foster care for disruptive youths in the child welfare system. Both MST and MTFC are discussed in greater detail later in this chapter.
Adolescent Substance Abuse
EBPs for adolescent substance abuse have focused most heavily on alcohol and marijuana use. For these and other substances, Waldron and Turner (2008) identified three EBPs that use a blend of behavioral methods, family systems perspectives, and outreach to systems outside the family. One of these, functional family therapy (FFT; Alexander & Parsons, 1982; Sexton, 2010), combines reliance on core behavioral techniques and a family systems orientation in an effort to establish new patterns of family interaction, and therapists work with external systems such as schools and probation departments to maximize generalization in the community. In addition, both individual and group CBT approaches (see Waldron & Kaminer, 2004) were identified as EBPs. In general, these combine an emphasis on identifying and modifying distorted cognitions with an emphasis on behavioral coping skills needed to avoid substance use (e.g., coping with cravings, refusal in the face of social pressure, avoiding situations where substance use might be likely).
Understanding How, With Whom, and Under What Conditions Treatments Work
Identifying youth EBPs can be useful in a number of ways. The process can prompt detailed reviews of the evidence base, nudging experts in the field into periodic self-study and encouraging a kind of “taking stock” of what has been learned about how to help youths and families deal with dysfunction in various forms. Identifying efficacious treatments can also serve as a springboard, encouraging an understanding of the treatments that goes deeper than just finding out that they “work.” Logical next questions can include, for example, how (i.e., through what processes) the treatments work, with whom they work, and under what conditions they work—questions to which we turn next (see also Chapter 2, this volume, for an overview of mediators and moderators).
Mediators and Mechanisms of Change
Ultimately, understanding how a treatment works requires identifying mechanisms of change (also known as mechanisms of action), the specific processes through which the treatment produces outcomes. A sound understanding of these mechanisms could help treatment developers strengthen the active ingredients of psychotherapy and reduce or eliminate inactive components, thereby increasing efficacy, efficiency, and cost-effectiveness of the therapy (Kraemer, Wilson, Fairburn, & Agras, 2002). A useful first step in identifying change mechanisms is testing whether a particular variable is a mediator of treatment outcome in a RCT, that is, an intermediate variable evident during treatment that statistically accounts for the treatment-outcome relationship (Kazdin, 2007; Kraemer et al., 2002; Weersing & Weisz, 2002b).
Moderators of Treatment Outcome
In addition, researchers try to understand with whom treatments work and under what conditions they work, by studying moderators of treatment outcome. In the context of an RCT, a moderator is a variable present prior to randomization that interacts with treatment condition; that is, the effects of that treatment on outcome depend on the level of the moderator (Kraemer et al., 2002). Identifying treatment moderators can inform efforts to establish the boundaries of treatment benefit. For example, identifying client characteristics that moderate treatment effects can help investigators learn which groups benefit most, and least, from various treatments (Kraemer et al., 2002), and this information can be used to guide decisions about which treatments to employ with which groups, so as to optimize the effects of psychotherapy.
Mediators and Moderators Identified in Studies of Evidence-Based Psychotherapies
In the following sections, we review examples of findings on mediators and moderators of youth EBPs derived from treatment outcome studies. We focused only on those treatments identified as well-established and probably efficacious psychotherapies, as discussed in the previous section and shown in Table 14.1, and on treatment rather than prevention studies (i.e., the sample has to have elevated symptoms of a disorder to be recruited into the treatment study). Because a larger number of moderators have been identified in individual trials of youth therapies, we focused on the most robust ones, and where possible those that reach significance in meta-analyses. We limited our review of moderators to meta-analyses of randomized trials when available; otherwise, we extended our review of moderators to meta-analyses that include both randomized and nonrandomized trials and to individual RCTs. In the meta-analyses reviewed, we focused on moderators of between-group (treatment versus control) effect sizes rather than moderators of pre- to posttreatment effect sizes because the former type of moderator is conceptually similar to moderators in an individual RCT, whereas the latter type of moderator is more similar to predictors in an individual RCT.
Mediators and Moderators of EBPs for Autism
We did not find any research examining mediation of the effects of EIBI or PRT. The absence of studies examining mediation of EBPs for autism may be due in part to the small number of RCTs in this area and to the fact that the low prevalence rate of the condition makes it difficult to obtain the large study samples needed for properly-powered mediation testing. Two promising candidates—social initiations (i.e., behaviors aimed at seeking help, attention, or social interaction) and peer social avoidance—were identified by Rogers and Vismara (2008) as targets for future research on mediation in autism treatment.
Several moderators of EIBI or similar early behavioral treatments have been identified. Consistent with expectations, several characteristics of the treatment including higher treatment intensity, longer treatment duration, and the presence of a parent training component were associated with significantly larger between-group effect sizes in a meta-analysis that included randomized and nonrandomized trials (Makrygianni & Reed, 2010). Only one characteristic of the sample emerged as a significant moderator in the same meta-analysis; higher baseline adaptive functioning was associated with larger between-group effect sizes. Interestingly, higher baseline intellectual and language abilities did not moderate treatment effects (Makrygianni & Reed, 2010). The association between younger age and larger treatment effects approached significance (Makrygianni & Reed, 2010); the failure to reach significance may have been due to a ceiling effect because a mean sample age of 54 months or younger at baseline was an inclusion criterion in this meta-analysis. Makrygianni and Reed (2010) observed that studies with mean child age of 35 months or younger and treatment intensity of more than 25 weeks seemed to have larger pre-post effect sizes, but they did not subject this observation to a statistical test. We did not find any studies examining moderators of PRT, but research (Sherer & Schreibman, 2005) on behavioral profiles of responders and nonresponders to PRT may point to promising candidate moderators for future study. Clinical practice implications are limited thus far, given the small number of significant findings, but EIBI moderator evidence does suggest that better treatment outcomes for early intervention are associated with higher treatment intensity and longer duration, plus inclusion of parent training.
Mediators and Moderators of EBPs for Eating Disorders
A recent study (Le Grange et al., 2012) tested six candidate mediators of the effects of family therapy, compared to adolescent-focused therapy, on rates of remission among adolescents with anorexia nervosa. None of the candidates—changes in weight, restraint in eating, depressive symptoms, self-esteem, self-efficacy, and parent self-efficacy after 4 weeks of treatment—were significant treatment mediators. The mediators were tested separately in two subgroups based on a median split of the adolescents' baseline severity of eating-related obsessions and compulsions (because this was a significant moderator), which may have limited the power to detect significant mediation, according to Le Grange and colleagues (2012).
We found a few moderators of family therapy effects for adolescent anorexia in individual RCTs, but not in meta-analyses. Eating- and weight-related obsessions and compulsions were significant moderators of treatment outcome in two RCTs. Adolescents with more severe obsessions and compulsions benefited more from a year-long course of family therapy compared to adolescent-focused therapy of the same duration (Le Grange et al., 2012), and compared to a shorter 6-month course of family therapy (Lock, Agras, Bryson, & Kraemer, 2005), even though the treatments worked equally well for the whole sample. Adolescents with more severe eating disorder symptoms also benefited more from year-long family therapy than adolescent-focused therapy (Le Grange et al., 2012). Interestingly, other measures of baseline psychopathology (e.g., body mass index, comorbidity, internalizing symptoms) did not moderate treatment effects (Le Grange et al., 2012; Lock et al., 2005). These findings imply that adolescents with more severe psychopathology specific to eating disorders would respond best to a year-long course of family therapy, but that those with milder eating disorder psychopathology may respond well to family therapy (year-long or 6-month) or adolescent-focused therapy.
There are mixed findings on whether intact family status and parental Expressed Emotion (EE; Hooley & Parker, 2006)—critical, hostile, and emotionally overinvolved attitudes toward the patient by close family members—moderate family therapy outcomes for adolescent anorexia nervosa. Adolescents from nonintact families benefited more from the year-long course than the 6-month course of family therapy in one study (Lock et al., 2005), but benefited equally from family therapy and adolescent-focused therapy when both treatments lasted a year. This suggests that adolescents from nonintact families may simply need longer treatment, regardless of whether the treatment was focused on the family or on the adolescent. In addition, adolescents whose mothers displayed higher levels of critical EE (i.e., made three or more criticisms in a structured interview) responded significantly better to separated family therapy (i.e., adolescent and parents seen separately) than to conjoint family therapy (i.e., adolescent and parents seen together), whereas adolescents whose mothers displayed lower levels of critical EE (i.e., fewer than three criticisms) responded equally well to both kinds of family therapy at posttreatment and at 5-year follow-up (Eisler et al., 2000; Eisler, Simic, Russell, & Dare, 2007). The authors suggested that maternal criticism during treatment sessions may trigger feelings of guilt and blame, thereby attenuating treatment effects. However, EE did not significantly moderate outcome when family therapy was compared to adolescent-focused therapy in another RCT, possibly because separated family therapy targets the reduction of parental criticism whereas adolescent-focused therapy targets increases in the adolescent's autonomy (Le Grange et al., 2012). Implications for clinical practice with high EE families are to conduct separate therapy sessions for adolescents and parents and to make reduction of parental criticism a focus of treatment.
Mediators and Moderators of EBPs for Depression
Several RCTs have found cognitive variables to be significant mediators of CBT for youth depression. Explanatory style mediated outcomes for youths with elevated depressive symptoms, whereby shifts to less pessimistic (Jaycox, Reivich, Gilham, & Seligman, 1994) or more optimistic (Yu & Seligman, 2002) attributional patterns were associated with reduced depressive symptoms. In addition, reductions in negative cognitions mediated reductions in depressive symptoms among depressed adolescents (Ackerson, Scogin, McKendree-Smith, & Lyman, 1998; Kaufman, Rohde, Seeley, Clarke, & Stice, 2005; Stice, Rohde, Seeley, & Gau, 2010). However, findings are not consistent between and even within studies. Ackerson et al. (1998) found that reductions in negative cognitions as assessed by the Dysfunctional Attitudes Scale (DAS; Weissman, 1979) but not by the Automatic Thoughts Questionnaire (ATQ; Hollon & Kendall, 1980) mediated outcome. Conversely, Kaufman et al. (2005) showed the opposite pattern of results—the ATQ but not the DAS mediated outcome. To explain their findings, Kaufman et al. (2005) suggested that their version of CBT may have been able to change cognitions only at the level of negative automatic thoughts as measured by the ATQ, and that more intensive CBT may be required to change more entrenched core beliefs as measured by the DAS. However, Ackerson et al.'s (1998) version of CBT, cognitive bibliotherapy, was unlikely to be more intensive than Kaufman et al.'s (2005) in-person group CBT. Evidently, more research is needed to clarify these mixed findings.
Several other variables have been tested as potential mediators in the context of CBT for adolescent depression. Increased frequency of engaging in pleasant activities was a significant mediator in one RCT (Stice et al., 2010) of group CBT for adolescents recruited for treatment from high schools due to their elevated depressive symptoms, but not in another RCT (Kaufman et al., 2005) of group CBT for adolescents with diagnoses of major depression and comorbid conduct disorder referred for treatment by the juvenile justice system. These findings provide preliminary evidence that mediators may differ according to severity and comorbidity of the sample, as well as referral source, but of course any two studies will differ along so many dimensions that ferreting out the cause of different findings is essentially educated speculation. Other candidate mediators—frequency of engaging in relaxation, social problem solving, and youth–therapist alliance—were also not found to mediate treatment outcome in the sample with major depression and comorbid conduct disorder (Kaufman et al., 2005). Finally, readiness to change mediated treatment outcome in the Treatment for Adolescents with Depression Study (Lewis et al., 2009), with adolescents receiving CBT or combination treatment of CBT and fluoxetine displaying the greatest increase in readiness to change.
To summarize, there is some evidence that shifts in explanatory style may mediate CBT effects for child depression, mixed evidence that change in negative cognitions and engagement in pleasant activities are mediators of CBT effects for adolescent depression, and limited evidence that readiness to change is a mediator of CBT effects for adolescent depression. Future research will be needed to determine which of these findings can be replicated, to clarify inconsistencies, and also to demonstrate temporal precedence of the mediators relative to change in depression levels. In the only study that documented the temporal relations of the mediators and outcome (Stice et al., 2010), fewer than 10% of youths showed a meaningful change (defined as 0.33 SD) in each of the two mediators (ATQ and engagement in pleasant activities) before a meaningful reduction in depressive symptoms. This raises a question as to whether change in cognitions and engagement in pleasant activities operate as true mechanisms of change in depression treatment, a question that warrants attention in future research (see our discussion of future research on mechanisms of change, below; see also discussion of mediation in Chapter 9, this volume). Future research will also be needed to help identify mediators of change in the context of IPT-A for adolescents and of behavior therapy for children; we have not identified any mediation research with these EBPs.
Moderators identified from meta-analyses of RCTs of psychotherapy for youth depression that included EBPs as well as non-EBPs include informant (i.e., who reports on the depression; Weisz, McCarty, et al., 2006) and depression severity at baseline (Watanabe, Hunot, Omori, Churchill, & Furukawa, 2007). Larger treatment effects were associated with youth-report than parent-report measures (see our later section on informant effects), and with higher baseline severity compared to lower baseline severity, possibly because youths with more severe psychopathology have more room for improvement. Youth age was a significant moderator in one of the meta-analyses (Watanabe et al., 2007), with larger effects obtained for adolescents than for children, but not in the other (Weisz, McCarty, et al., 2006). The positive finding, though not evident in both meta-analyses, is consistent with the idea that adolescents' more advanced cognitive level makes them better able than children to grasp concepts discussed in therapy.
Mediators and Moderators of EBPs for Phobic and Anxiety Disorders
Reductions in youths' anxious self-statements and improvements in the ratio of positive self-statements to the sum of positive and anxious self-statements (their “states of mind ratio”) mediated youth-reported symptom reduction in two RCTs (Kendall & Treadwell, 2007; Treadwell & Kendall, 1996) of individual CBT for youth anxiety. Positive self-statements and depressive self-statements, by contrast, were not found to mediate treatment outcome (Kendall & Treadwell, 2007; Treadwell & Kendall, 1996). Another research team (Lau, Chan, Li, & Au, 2010) has replicated the mediating effects of anxious self-statements on outcome in group CBT for youth anxiety; this team also demonstrated that improvement in the youths' ability to cope with fear-inducing situations, as perceived by youths and by parents, mediated treatment-induced symptom reduction.
As with CBT for youth depression, future research will need to demonstrate temporal precedence for the above mediators of individual CBT and group CBT, relative to changes in youth anxiety symptoms, to be considered true mechanisms of change. Future research will also be needed to identify mediators associated with other EBPs for phobic and anxiety disorders (i.e., group CBT for social phobia, group CBT with parents, and social effectiveness training for social phobia).
Studies conducted in North America had larger effects than studies conducted elsewhere, but there appeared to be no other moderators of treatment outcome according to a meta-analysis of randomized and nonrandomized trials of psychosocial treatments for youth anxiety (Silverman, Pina, et al., 2008). Another meta-analysis (James, Soler, & Weatherall, 2005) that included only RCTs of CBT compared to a wait-list or attention control detected no heterogeneity among the 13 studies, suggesting that there were no robust moderators of CBT for youth anxiety. These findings suggest that more work needs to be done on adapting CBT for youth anxiety to cultures and treatment contexts outside North America, but otherwise, research has not yet found marked differences in anxiety treatment response between different groups of youths.
Mediators and Moderators of EBPs for Obsessive-Compulsive Disorder
As best we can determine, no mediators or moderators have been identified for individual exposure-based CBT to date. This gap in the evidence-base has been attributed to small sample sizes and the low power of treatment outcome studies of psychotherapy in this area (Barrett et al., 2008). Comorbid tic disorder was found to be a moderator of the effects of sertraline treatment, but not of CBT. Because youths with comorbid tic disorder did not respond well to medication alone in the Pediatric OCD Treatment Study (POTS), CBT alone or combined with medication has been recommended as a first-line treatment for these youths (March et al., 2007).
Mediators and Moderators of EBPs for Youths Exposed to Traumatic Events
We have not found good evidence for any mediators of TF-CBT or of school-based group CBT. A review by Cohen et al. (2010), creators of TF-CBT, suggests that potential candidates for a mediation role in TF-CBT might include parent emotional distress, parent support, and abuse-related attributions and perceptions of the youth (e.g., youths believing they are responsible for the abuse, perceiving that others do not believe their accounts of abuse, or feeling different from their peers; see Cohen & Mannarino, 2000).
We did not find any meta-analyses of CBT for youths exposed to traumatic events, and RCTs did not report significant moderators. One meta-analysis (Silverman, Ortiz, et al., 2008) that included both EBPs and non-EBPs for youths exposed to trauma suggested that treatment orientation, type of trauma, and parent involvement were moderators of treatments; differences between effect sizes at each level of the moderators were compared but not subjected to significance testing. As expected, CBT interventions performed better than non-CBT interventions, but surprisingly, youth-only interventions performed better than those with parent involvement (Silverman, Ortiz, et al., 2008). In addition, interventions for sexual abuse had relatively large effects on posttraumatic and depression symptom outcomes and relatively small effects on externalizing symptoms, compared to interventions for other types of trauma (Silverman, Ortiz, et al., 2008). The authors speculated that internalizing symptoms may be more severe in sexually abused youths, leading to a treatment focus on reducing internalizing symptoms among these youths, whereas the treatment focus may be on reducing externalizing symptoms among youths with other kinds of trauma such as physical abuse. Future research should confirm if the above findings are statistically significant (i.e., not merely due to chance), and if so, probe the underlying processes that explain these moderation effects.
Mediators and Moderators of EBPs for Attention-Deficit/Hyperactivity Disorder
The Multimodal Treatment Study of Children with ADHD (MTA; MTA Cooperative Group, 1999a), the largest RCT of ADHD treatments to date, compared behavioral treatment (i.e., behavioral parent training, summer treatment program, and teacher consultation emphasizing behavioral classroom management), medication management (methylphenidate, Ritalin), a combination of behavioral treatment plus medication, and regular community care. Youths receiving combination treatment or medication only did better than those receiving behavioral treatment only or community care. The superior effects of the combination treatment on youth social skills relative to community care were mediated by reductions in negative/ineffective discipline by parents (Hinshaw et al., 2000). Although both combination and behavioral treatments improved discipline, improved discipline was associated with improved youth social skills for the combination treatment only. It is possible that reduced behavior problems due to stimulant medication caused parents to use less harsh discipline, resulting in improved self-regulation by their children. It is also possible that improved social skills, driven by medication, caused parents to use less harsh discipline because temporal relationships between mediator and outcome could not be distinguished. Furthermore, a third variable could have driven improvements in both discipline and social skills (Hinshaw et al., 2000). It is noteworthy that other parent variables (i.e., attendance at behavioral treatment sessions, positive involvement, deficient monitoring) were not mediators of behavioral or combination treatment effects (Hinshaw et al., 2000; MTA Cooperative Group, 1999b).
Publication year was a moderator of outcome in a meta-analysis (Fabiano et al., 2009) of behavioral treatments for ADHD, with more recent publications associated with smaller effects, but various participant and family characteristics were not. The publication year finding is puzzling, in that treatments might be expected to become more effective with improved understanding of ADHD and intervention effects over the years. In another meta-analysis (Corcoran & Dattalo, 2006) of behavioral and cognitive-behavioral interventions for ADHD with parent involvement, two-parent households and older youths were associated with larger treatment effects. Finally, the MTA study identified a moderator that has noteworthy implications—youngsters with comorbid anxiety disorder benefited more from behavioral treatment than did those with no anxiety disorder. The anxious youths showed outcomes comparable to those of the medication management group and superior to those of the community care group (MTA Cooperative Group, 1999b). Thus, Hinshaw (2007) has suggested that behavior therapy alone may potentially be a suitable first-line treatment for the subgroup of youths with ADHD who have comorbid anxiety.
Mediators and Moderators of EBPs for Disruptive Behavior Problems
Research on mediators of EBPs for disruptive behavior problems is especially rich compared to other problem areas. This reflects, in part, the fact that treatment in this area has been such a priority for the field, generating so much treatment development and intervention testing.
Most mediators identified across the various EBPs for disruptive behavior are some aspect of parent/caregiver practices and skills. This is consistent with expectations given that the parent or caregiver is seen as the principal change agent in most EBPs for disruptive behavior and is taught parenting skills in a number of domains, such as close monitoring of the youth, and preventing the youth from associating with deviant peers. For example, in MST, improved family and peer functioning were found to mediate reductions in delinquent behavior (Huey, Henggeler, Brondino, & Pickrel, 2000). In addition, caregivers' improved ability to follow through with disciplinary action and decreased concern about youths' negative peer relationships partially accounted for the superiority of MST over usual care in the treatment of juvenile sex offenders (Henggeler et al., 2009). Similarly, in MTFC, improvement in caregivers' family management skills (e.g., adult–youth relationship, supervision, discipline) and reduction in youths' relationships with deviant peers mediated treatment effects on the subsequent antisocial behavior of adolescent boys who were severe offenders (Eddy & Chamberlain, 2000). In addition, decreases in harsh, critical, and ineffective parenting practices accounted for reductions in youth externalizing symptoms in a study (Beauchaine, Webster-Stratton, & Reid, 2005) that pooled data from six RCTs of the Incredible Years (IY) treatment program in which participants received various combinations of child, parent, and/or teacher training. Interestingly, other aspects of parenting and peer relationships (i.e., caregiver monitoring, parent–youth communication, and peer delinquent behaviors and conventional activities) were not mediators in the Henggeler et al. (2009) study of sex offender treatment, suggesting that just which aspects of parenting need to be altered to generate youth behavior change may depend on the specific EBP or the condition being treated.
Youth-focused variables have also been shown to mediate outcomes of EBPs for disruptive behavior problems, but these mediators seem to be specific to the particular EBP or sample. Homework completion—a measure of engagement in school—mediated the effects of MTFC on the number of days offending girls spent in locked settings (Leve & Chamberlain, 2007). In addition, changes in boys' hostile attributions, reduced expectations that aggression would result in favorable outcomes, and increased internal locus of control, among other changes, accounted for improvements in school behavior, delinquency, and substance use among youths receiving anger control training (Lochman & Wells, 2002). This is not surprising given the emphasis in this treatment program on individual changes in the youths themselves.
It is encouraging that multiple studies by different research teams have converged on the conclusion that parenting practices and relationships with deviant peers mediate the effects of EBPs on disruptive behavior among youths. Indeed, this may be the most robust finding on any mediator of any EBP for youths. Evidence on youth-focused mediators are more limited and more in need of replication. As with EBPs for depression and anxiety, RCTs of EBPs for disruptive behavior will need to include multiple assessments of both mediators and outcomes during and after therapy to establish identified mediators as true mechanisms of change (see our later section on this topic).
Several moderators of behavioral parent training were identified in a meta-analysis (Lundahl, Risser, & Lovejoy, 2006) that included randomized and nonrandomized controlled trials. Youths from nonintact and economically disadvantaged families made smaller treatment gains than those not in these subgroups. It is probable that single and economically disadvantaged parents have less time and energy to attend all therapy sessions, to practice the parenting skills learned during therapy at home, and to monitor and regulate their children's peer associations. Lundahl et al. (2006) examined moderators of outcome within the group of studies with economically disadvantaged samples and found that individual parent training was more helpful than group parent training, suggesting that close individual attention may be especially helpful with economically disadvantaged families. Interestingly, treatments that involved only parents were associated with better outcomes in parent behavior and perceptions than were treatments that involved both parents and their children. An explanation proposed by Lundahl et al. (2006) is that parents may be more likely to see themselves as the primary agents of change and take more responsibility for effecting change when they are the sole recipients of treatment. In addition, studies with samples including clinically significant disruptive behavior problems showed larger treatment effects, possibly because there was more room for improvement in those samples.
Mediators and Moderators of EBPs for Adolescent Substance Abuse
Mirroring the mediation research on EBPs for ADHD and disruptive behavior problems, a change in parenting practices was a significant mediator of an EBP for adolescent substance abuse. MDFT improved parental monitoring of adolescents' daily activities and peers relative to peer group intervention, thereby increasing abstinence from substance use during a 12-month period following baseline assessment (Henderson, Rowe, Dakof, Hawes, & Liddle, 2009). Interestingly, improved parental monitoring mediated treatment effects only when the outcome was proportion of youths who were abstinent and not frequency of substance use, leading Henderson and colleagues (2009) to suggest that parental monitoring may prevent substance use, but not reduce substance use among adolescents who continue using substances after treatment. Improved parent-adolescent relationship quality, although associated with greater abstinence, was observed in both MDFT and peer group intervention conditions and thus was not a treatment mediator (Henderson et al., 2009). We do not know of any published mediation studies for other EBPs of adolescent substance abuse, but Waldron and Turner (2008) have suggested several candidates to examine, including family variables in FFT and MST, coping skills in individual and group CBT, and therapeutic alliance for all treatment approaches.
We found several individual RCTs, but no meta-analyses, that identified moderators of EBPs for adolescent substance abuse. MDFT outperformed two alternative treatments (individual CBT and enhanced treatment as usual) for adolescents with more severe baseline substance use and comorbidity, but performed similarly to the alternative treatments for adolescents who had less severe baseline substance use and comorbidity (Henderson, Dakof, Greenbaum, & Liddle, 2010). The authors suggested that common factors of good psychotherapy (e.g., strategies to engage adolescents, sufficient duration and intensity) may be adequately therapeutic for adolescents with less psychopathology, whereas MDFT's specific focus on changing a greater number of documented risk factors, particularly family interactions, may be especially beneficial to adolescents with more psychopathology. Gender appears to moderate the effects of CBT on substance use, but findings are mixed on the direction of moderation, with one RCT favoring boys (Kaminer, Burleson, & Goldberger, 2002) and another favoring girls (Kaminer, Burleson, & Burke, 2008). The first RCT tested group CBT against a group psychoeducation control whereas the second RCT tested an aftercare intervention that included CBT and motivational enhancement therapy delivered either in-person or through the phone against a no aftercare control group after all participants completed group CBT. The discrepancy on the direction of moderation could reflect different processes involved in the initiation versus maintenance of behavior change (Kaminer et al., 2008), the use of different intervention approaches, or the presence of motivational enhancement therapy in the one instance. In other findings, several personality and temperament variables have been shown to moderate the effects of group CBT, including sensation seeking, anxiety sensitivity, hopelessness (Conrod, Stewart, Comeau, & Maclean, 2006) and rhythmicity (Burleson & Kaminer, 2008). These are early days for research on moderation in substance abuse treatment, but as future studies document which of these specific findings can be replicated, treatment may be optimized for substance-using adolescents by first screening them for personality/temperament variables and then matching them to treatments that have been documented to be more beneficial for individuals with their particular personality/temperament type.
Therapeutic Alliance and Other Relationship Variables
Notably absent from our review of mediators of youth EBPs are therapeutic alliance and other therapeutic relationship variables, which have been hypothesized to be key mechanisms of change in youth psychotherapy (Karver, Handelsman, Fields, & Bickman, 2005, 2006; Shirk & Karver, 2003). Unfortunately, we have only identified one youth RCT that has tested alliance as a mediator, and it found therapeutic alliance not to be a significant mediator (Kaufman et al., 2005; see our section on mediators and moderators of EBPs for depression). This dearth of research on alliance as a mediator is disappointing given the substantial number of studies that have examined the association between alliance and outcome in youths, as well as the intuitive belief by many that youngsters who see their therapist as understanding them and collaborating with them will have better outcomes. Evidence for this belief, via appropriate mediation testing, is absent thus far.
A meta-analysis (Karver et al., 2006) documented significant associations between a number of different therapeutic relationship variables (e.g., counselor interpersonal skills, therapist direct influence skills, youth affect toward therapist) and outcome. More recently, another meta-analysis (McLeod, 2011) with an exclusive focus on therapeutic alliance (rather than the broader construct of therapeutic relationship) and outcome in youth psychotherapies found a small but significant association (r = 0.14), with roughly equal associations for the alliance between youth and therapist (youth–therapist alliance) and the alliance between parent and therapist (parent–therapist alliance). This alliance–outcome association from 38 youth psychotherapy studies is half of that found in a meta-analysis of 190 adult psychotherapy studies (r = 0.275, Horvath, Del Re, Flückiger, & Symonds, 2011). Why is the alliance–outcome association so much weaker in youth psychotherapies than in adult psychotherapies? McLeod (2011) suggested that the moderators identified in his meta-analysis may provide clues to explain the smaller association in youth psychotherapies. Two of these moderators—therapeutic orientation and informant—may be especially pertinent to this question. Smaller alliance–outcome associations emerged for family-based or systemic therapies compared to individual-based youth or parent therapies and for youth- or observer-report compared to parent-report measures of alliance. Because family-based and systemic therapies are more common among youth than adult clients, the smaller alliance–outcome association of these therapies may have brought down the mean association across youth psychotherapies. It is also intriguing that the alliance–outcome association differed by informant but not by the specific client–therapist alliance (youth–therapist versus parent–therapist alliance) assessed. McLeod (2011) argued that the parent's perception of therapeutic alliance may be especially important for youth psychotherapy outcome because parents are the ones who seek treatment, consent to treatment, and physically bring the youth to treatment; moreover, youths may not be able to rate alliance as accurately as can adults due to their lower level of cognitive development (see our later section on this topic).
Even though the alliance-outcome association is small in youth psychotherapies, it is nevertheless reliably larger than zero. One potentially useful next step will be to test therapeutic alliance and other therapeutic relationship variables as mediators of treatment outcome in future youth psychotherapy studies.
Summary of Research on Mediators and Moderators of Evidence-Based Psychotherapies
To summarize the mediation evidence presented in the previous sections, mediators of EBPs for youths with depression, anxiety and phobic disorders, disruptive behavior problems, or substance abuse have been identified; a mediator of a medication-EBP combination treatment for ADHD has been identified; and no mediators of EBPs for youths with autism, eating disorders, OCD, or trauma have been identified, to our knowledge. Therapeutic alliance and relationship variables are promising candidates for future testing. Among the identified mediators, empirical support appears to be strongest for parenting skills and practices in the context of EBPs for disruptive behavior problems; evidence is also substantial for cognitive variables in the context of CBT for youth depression. More research will be needed to establish these mediators as true mechanisms of change (see our later section on this topic).
The evidence base on moderators of EBPs for youths is larger than that on mediators. Moderators were identified in relation to EBPs for every youth disorder except OCD (confirming significance tests are also needed for EBPs for trauma). A number of parent and family variables, including parent involvement in youth-focused treatments, youth involvement in parent-focused treatments, maternal EE, single- versus two-parent households, and parent versus youth as informant, emerged as moderators across several different disorders and treatment orientations.
Not surprisingly, a number of the findings on mediation and moderation concern family factors, a topic that warrants detailed attention in its own right. So, we focus now on the role of family factors in youth psychotherapy.
Family Factors in Youth Psychotherapy
As noted earlier, youth psychotherapy typically involves caregivers, and often other family members as well, and in a variety of roles—for example, referring the youth for treatment; identifying reasons for referral; providing information on the youth's current functioning and response to treatment; participating in the therapy; and collaborating in decisions about treatment content, structure, and termination. In some psychotherapy programs—such as Barkley's (1997) Defiant Children and Kazdin's (2010) Parent Management Training for disruptive, disobedient, and aggressive youngsters—caregivers are the primary participants in sessions with the therapist, learning skills to use with their children at home. In the context of such treatment programs, it is no surprise to find that parent–therapist alliance, like youth–therapist alliance, predicts treatment outcomes for young people (e.g., Kazdin, Whitley, & Marciano, 2006), and that youth outcomes are also predicted by the extent to which caregivers learn and use the new parenting skills therapy is designed to convey (Zisser & Eyberg, 2010). The full range of family factors relevant to youth psychotherapy is extensive and beyond the scope of this chapter (but see Chapter 15 in this volume for further elaboration). However, we offer here two examples of family factors that may warrant increased attention in future research.
Expressed Emotion
The home environment is a source of important protections from psychological distress and potential risk factors for poor psychological functioning. Of these risk factors, EE may be particularly relevant to the understanding of how psychological disorders develop and are maintained among both youths and adults. EE has been found to predict treatment outcome and relapse for a broad range of disorders (Hooley, 2007). Earlier in this chapter we noted the role of EE as a moderator of anorexia nervosa treatment effects (Eisler et al., 2000; Eisler et al., 2007). In addition, Asarnow, Goldstein, Tompson, and Guthrie (1993) found that youths with mood disorders were significantly more likely to maintain symptom reductions one year after inpatient treatment when returning home to live with a low rather than high EE mother. A correlation has been shown between critical EE and externalizing problems for children in first grade, and the critical EE of mothers of preschool children has been shown to longitudinally predict ADHD at grade three, even when accounting for both preschool behavior problems and maternal stress (Peris & Baker, 2000).
Although such findings are intriguing, further research is needed to clarify the association between EE and treatment process and outcome for children and adolescents. There has been considerable research on EE in children and adolescents, but questions remain regarding how the construct—originally developed for research on adult psychopathology—should be operationalized for youths. For example, McCarty and Weisz (2002) found that when using the Five Minute Speech Sample (FMSS; Magana et al., 1986) to assess EE, the emotional overinvolvement (EOI) facet has little connection to youth psychopathology, and positive comments made by the parent, which partially comprise EOI, have negative associations with youth psychopathology. These findings stand in direct conflict with predictions based on traditional conceptualization of EE, suggesting a need for a developmentally sensitive conceptualization of, and research on, EE. Consistent with traditional conceptualizations, however, McCarty and Weisz (2002) did find that critical EE was positively associated with symptoms of youth psychopathology.
Given that critical EE may well be the most important facet of EE for youth, based on research to date, it makes sense for future research to examine the role of perceived criticism (PC) in youth psychotherapy outcome and relapse. The study of EE within the adult literature naturally gave rise to the study of PC. Although critical expressed emotion is a measure of how much criticism is expressed by a relevant family member (e.g., a parent or a spouse) toward a specific patient or individual, it does not necessarily measure how much criticism “gets through” to the patient. Perceived criticism may be a better indicator of how much criticism gets through to a patient, and even of how much criticism is perceived regardless of the actual content or the intent of the speaker. Hooley and Teasdale (1989) found that perceived criticism, which is much easier to assess than EE, is a powerful predictor of treatment relapse in its own right, has strong test–retest reliability, and yields ratings independent of illness severity. As further research is done on these constructs, it will be useful to investigate the impact of criticism and perceived criticism in their own right, controlling for the patient behavior that may, in some cases, prompt the criticism (i.e., higher levels of criticism might, in some cases, reflect higher levels of youth psychopathology, which are linked to more of the behavior that parents and others find objectionable, and thus criticize). Level of parental criticism could in principle be studied as a possible moderator of treatment outcome and as a candidate mediator (i.e., improved youth functioning might be mediated in part by reductions in parental criticism). Despite evidence that EE is important for predicting outcome and relapse in both youths and adults and that PC is a powerful predictor of adult outcome, we know of no research examining PC in the context of youth psychotherapy.
The Challenge of Different Perspectives
Going beyond the attitudes and behavior of caregivers, we focus next on the fact that different family members differ from one another in their perception of events and behavior, and how these differences impact youth psychotherapy processes and outcomes. Informant discrepancies in the reports of various family members on youth behavior, functioning, and psychopathology have been among the most consistent findings in youth clinical research (Achenbach et al., 1987; De Los Reyes, Goodman, et al., 2010; De Los Reyes & Kazdin, 2005; Richters, 1992; Weisz & Weiss, 1991). As suggested by Weisz et al. (1997), the study of youth psychopathology “is inevitably the study of two phenomena: the behavior of the child, and the lens through which adults view child behavior” (p. 569). Different adults inevitably view the young person's behavior through different lenses, and these differ from the lenses used by the youth.
The complications associated with informant discrepancies are apparent in a variety of studies using community samples. For example, in a study of female caregiver–youth dyads, discrepant reports of parental monitoring predicted increased levels of youth-reported delinquent behaviors after a period of 2 years (De Los Reyes, Goodman, et al., 2010). In other community samples, disagreement between adolescents and parents has been shown to predict a variety of undesirable future outcomes, including drug abuse, police and judicial contact, expulsion from school, job loss, deliberate self-harm, and suicidal ideation/attempts (Ferdinand, van der Ende, & Verhulst, 2004, 2006).
Although some of these findings are open to multiple interpretations (e.g., youth–caregiver discrepancy might reflect youth–caregiver discord, parental inattention, or even success by the youth in concealing behavior), the associations with adverse outcomes do raise the question of whether caregiver–youth discrepancy has consequences for the process or outcome of psychotherapy. Clinicians who work with young people routinely face the challenge of determining the appropriate problems to address in therapy when youth and caregiver perspectives disagree. Prior studies have illustrated how challenging the task can be. In a sample of clinic-referred youths and their parents, Yeh and Weisz (2001) obtained information separately from the youths and their parents regarding what problems needed to be targeted in treatment. Some 63% of the youth-parent pairs failed to agree on a single specific target problem, and 36% failed to agree on even a single broad category (e.g., aggressive behavior, anxiety/depression). Extending these findings to include the perspectives of therapists, Hawley and Weisz (2003) found that 76% of parent-youth-therapist triads failed to agree on a single target problem and 44% failed to reach consensus on even one general problem category.
One common explanation for a lack of agreement between youths and parents in the treatment context is that discrepancies result in part from differing perspectives (Achenbach et al., 1987; Forehand, Frame, Wierson, Armistead, & Kempton, 1991). According to this view, externalizing problems are readily observable by parents whereas internalizing problems (e.g., worry or sad feelings) are less outwardly observable and thus more likely to be detected by the youth, who experiences the internalizing distress, than the parent. Consistent with this view, Weisz and Weiss (1991) provided evidence that externalizing problems were more commonly the basis of youth clinic referrals by parents than internalizing problems were. But as these authors noted, there are additional reasons why externalizing problems might be referred more often than internalizing problems (e.g., externalizing behavior is more disruptive at home and school and more likely to be distressing to others in the youth's world). An additional factor may be relevant: language fluency.
Disagreement as to what problems a youth has, or which problems warrant treatment, could affect treatment process and outcome. In a study of youth outpatient clinic treatment, Brookman-Frazee, Haine, Gabayan, and Garland (2008) found a positive association between caregiver–youth agreement on treatment goals, on the one hand, and number of sessions attended, on the other. In another study of outpatient treatment, level of caregiver–youth agreement in reports of youth psychopathology and interpersonal problems was positively associated with level of caregiver involvement in the treatment process (Israel, Thomsen, Langeveld, & Stormark, 2007). It will be useful, in future research, to explore the extent to which caregiver–youth agreement/disagreement is a predictor of treatment outcome, and also important to explore methods of reducing discrepancies before dropout occurs.
De Los Reyes, Alfano, and Beidel (2010a) have stressed the potential information value of informant discrepancies in psychotherapy. In a study investigating discordant reports among parent–youth dyads on measures of youth social phobia symptoms, parent-youth discrepancies at pretreatment significantly predicted discrepancies at posttreatment. This relation was found to be moderated by treatment responder status in that significant relations were found only for treatment non-responders. De Los Reyes, Alfano, et al. (2010) argued that this stability in measures of informant discrepancies across time suggests that discordant reports may serve as tools for evaluating youths' response to treatment. Repeated measures of caregiver-youth agreement during the course of therapy, these authors' believe, may shed light on how well youths are responding to treatment. Thus, informant discrepancies, rather than being “measurement error,” may provide information that can enrich our understanding of youth psychotherapy process and outcome (De Los Reyes, 2011; De Los Reyes & Kazdin, 2005).
Testing the Reach of Psychotherapies Across Population Groups
One way to test the strength and “reach” of youth EBPs is to examine the breadth of their impact across a range of population groups and risk conditions. We turn now to research addressing that agenda, with four groups of special interest.
Ethnic Minority Populations
The percentage of youths in the United States who are ethnic minorities was 43% in 2008, and this percentage continues to grow (Pollard & Mather, 2009). The prevalence of psychological disorders among ethnic minority groups in the United States is about the same as that of the general population (21%; U.S. Department of Health and Human Services, 2001), and the most recent statistics available suggest that about 13% of ethnic minority youths receive mental health services each year (Stagman & Cooper, 2010, estimate that 31% of European-American youths receive services). Although a large percentage of youths receiving mental health services belong to ethnic minority groups, some of the reports on treatment process and outcome for these youths have not been encouraging. For example, a U.S. Department of Health and Human Services document (DHHS, 2001) reported that only a small number of ethnic minorities had participated in psychotherapy RCTs, and that none of the studies had assessed the efficacy of the treatment by ethnicity or race. Chambless and colleagues (1996), in their review of treatments meeting EBP criteria, stated “We know of no psychotherapy treatment research that meets basic criteria important for demonstrating treatment efficacy for ethnic minority populations…” (Chambless et al., 1996). Additionally, some research had found ethnic minority youths more likely than European-Americans to drop out of treatment (Kazdin & Whitley, 2003) and significantly less likely to show clinical improvement when treated for depression (Weersing & Weisz, 2002a).
A more hopeful note was sounded by Huey and Polo (2008), in a selective review of youth treatment outcome studies from 1960 through 2006, in which at least 75% of participants in each study were ethnic minorities. Using the levels-of-support criteria we outlined earlier (see Silverman & Hinshaw, 2008), Huey and Polo (2008) found no “well-established” treatments, but they identified multiple treatments that were “probably efficacious” and “possibly efficacious” for minority youths, encompassing a range of conditions including anxiety, ADHD, depression, disruptive conduct, substance use, posttraumatic stress, and suicide risk, with CBT as the best-documented effective treatment for anxiety disorders, depression, and trauma-related disorders. Adding a meta-analysis of 25 studies, Huey and Polo (2008) found a mean pre-post treatment effect size for minority youths averaging .44, just below Cohen's (1988) benchmark for a medium effect (as compared to control participants receiving no treatment, placebo, or treatment-as-usual).
Some in the field believe that assessing the effects of existing EBPs with minority youths is insufficient, and that, instead, EBPs should be structured specifically for, or at least tailored to fit ethnic minority populations. There is considerable interest in treatments that are sensitive to cultural values and norms (Sue, Fujino, Hu, Takeuchi, & Zane, 1991), and it is possible that treatments developed with European-American samples “may not take into account the language, values, customs, child-rearing traditions, expectancies for child and parent behavior, and distinctive stressors and resources associated with different cultural groups” (Weisz, Huey, & Weersing, 1998, p. 70). The intuitive appeal of these ideas notwithstanding, when Huey and Polo (2008) reviewed the small collection of RCTs that compared culturally adapted and tailored treatments to standard EBPs, they found no significant differences in treatment outcomes with minority youths. The one form of cultural adjustment for which some supportive evidence has been found is therapist–patient ethnic match, which has been found to be associated with superior treatment perseverance (e.g., reduced rates of dropout after initial treatment session; Yeh, Eastman, & Cheung, 1994) and superior treatment outcome (e.g., 33% improvement in level of symptom reduction on the Child Behavior Checklist; Halliday-Boykins, Shoenwald, & Letourneu, 2005).
It is clear that research on psychotherapy effects with ethnic minority populations has begun in earnest, but it has only begun. We look forward to reviewing an ever-richer base of information on this topic in the years ahead.
War-Exposed Youths
As we learn more about the best ways to make treatment responsive to ethnic and cultural variation, we are likely to learn more, as a field, about ways to help some of the world's youth who are most in need of support: youths exposed to armed conflict in low-resource and war-torn countries. These youths have experienced stressors such as military assault, sexual trauma, conscription as “child soldiers,” and diverse sequelae of involuntary displacement (e.g., life in refugee camps, failure to understand the local language and culture, separation from family members) that can put them at risk for significant disorder and dysfunction. UNICEF (1996) reported that wars in the past decade had hampered normal child development, subjecting an estimated 20 million youths to homelessness, 6 million to physical injury and disability, and 1 million to parental separation. Research has shown that war-exposed youths are at increased risk for substance abuse, depression, anxiety, conduct problems, posttraumatic stress, and suicidal ideation (Lustig et al., 2004; Shaw, 2003).
Can the current array of therapies make a difference for youths exposed to armed conflict? The modest evidence base to date is somewhat encouraging. Bolton et al. (2007) tested a group interpersonal therapy (IPT) intervention for depression among adolescent Ugandan war refugees. IPT was compared to a creative play treatment program and to a waitlist control group. Compared to the other two interventions, IPT was more successful in significantly reducing depression symptoms (but not anxiety or conduct problems) for girls; boys also benefited from IPT but symptom reductions were nonsignificant. In the IPT condition at posttreatment, 37.1% of adolescents met criteria for recovery and 29.1% for remission, as compared to 12.4% recovery and 6.7% remission in the creative play condition, and 13.5% recovery and 8.9% remission in the control condition. The authors suggest the treatment may have been less effective for boys due to their being less open to discussing emotional problems in a group. Another contributing factor is the group IPT intervention has been shown to be less effective for youths with comorbid anxiety disorders and boys in the sample had more symptoms of posttraumatic stress disorder (PTSD) than girls. RCTs have also been conducted as large-scale school-based interventions. Tol, Komproe, Susanty, Jordans, and de Jong (2008) tested a trauma-focused group intervention for PTSD symptoms among youths in Indonesia exposed to political violence. The treatment included group CBT along with structured play activities and performing arts exercises. Compared to a waitlist control, the CBT group experienced a significantly larger decrease in PTSD symptoms (but not depression or anxiety symptoms). Jordans et al. (2010) tested a classroom-based intervention broadly designed to improve psychosocial functioning and general well-being among adolescents in civil war–affected Nepal experiencing psychosocial stress. The intervention consisted of CBT, structured play activities, performing arts exercises, and narrative exposure techniques. Compared to a wait-list control, the treatment group experienced significantly larger improvements in general functioning, general psychological functioning, and significantly greater reduction in depression symptoms and anxiety symptoms. PTSD symptoms decreased and feelings of hope increased to a significant and comparable degree in both groups. Jordans et al.'s (2010) CBT program was a broad intervention to improve general well-being, whereas the Tol et al. (2008) CBT program was a trauma-focused intervention for youths who had experienced at least one violent event and PTSD symptoms. Given these differences in scope, objectives, and sample, it is difficult to interpret the difference in outcomes between the two studies.
Layne et al. (2008) assessed the effectiveness of components of a manualized treatment protocol known as trauma and grief component therapy (TGCT) for war-exposed Bosnian adolescents experiencing PTSD, depression, or grief symptoms along with impairment in functioning. TGCT has been widely disseminated in war-torn Bosnia as part of a UNICEF mental health program. Students were randomized to one of two treatment conditions, each consisting of components of TGCT: (1) trauma- and grief-centered therapy along with psychoeducation and social skills training (treatment condition), and (2) psychoeducation and social skills training only (active comparison group). Both TGCT treatment groups experienced a significant decrease in PTSD and depression symptoms; only the treatment condition involving trauma- and grief-centered therapy along with psychoeducation and social skills training showed a significant decrease in grief symptoms.
Dybdahl (2001) tested a psychosocial intervention for mother–youth refugee pairs internally displaced within Bosnia. The intervention consisted of parent discussion groups centered around trauma-processing and improving mother–youth interactions. As compared to a control group (receiving medical care only), the treatment group (who received the psychosocial intervention along with medical care) showed significantly more improvement in mothers' PTSD hyperarousal symptoms and youngsters' weight gain and psychosocial functioning (youths' PSTD symptoms were not explicitly assessed).
These studies illustrate that it is feasible to deliver structured psychotherapy interventions derived from the RCT evidence base to war-exposed youths even in very remote and under-resourced regions, and that measurable psychological benefit may result, at least for some groups on some dimensions of psychological functioning. Perhaps these early findings will be a springboard for work with other war-exposed and refugee populations whose need for support, and effective coping skills, is so profound. Longer-term follow-up evaluations appear to be missing, but these are obviously needed.
Youths in the Juvenile Justice System
More than 90,000 youths are detained in residential juvenile justice facilities, or adult jails or prisons, in the United States each year (Snyder & Sickmund, 2006; National Evaluation and Technical Assistance Center, 2010), and many more were involved with police and the court system. About 67% of adjudicated youths are housed in facilities that screen for mental health needs (Snyder & Sickmund, 2006), providing some limited data on psychopathology prevalence for this population. There have also been numerous studies of mental health problems and disorders in juvenile justice facilities, although the results have been inconsistent across studies, and the U.S. Department of Justice considers the information from extant studies to be insufficient to guide policy decisions (Teplin et al., 2006). Teplin and colleagues (Teplin et al., 2006) have assessed the prevalence of psychiatric disorders within the juvenile justice system using random sampling of detainees and empirically supported measures of psychopathology, including the Diagnostic Interview Schedule for Children (DISC) Version 2.3 (Shaffer et al., 1996). These investigators have found that the most common disorders among juvenile justice-involved youth relate to substance use and conduct-related disorders. Additionally, more than 25% of females and 20% of males meet criteria for at least one affective disorder, and comorbidity is substantial (Teplin et al., 2006).
One ostensible objective of the U.S. juvenile justice system is rehabilitation, and treatment for mental health problems is widely viewed as essential. It is disappointing that empirical support for many of the interventions used is mixed or absent, and it is possible that some of the most popular interventions may well be ineffective or harmful. The Blueprints for Violence Prevention project of the Center for the Study and Prevention of Violence, at the University of Colorado (see e.g., Mihalic, Fagan, Irwin, Ballard, & Elliott, 2002), has evaluated more than 900 programs aimed at rehabilitating youths. Supporting evidence for most of these was found to be either disappointing or entirely lacking. Examples include Scared Straight, a program using shock probation (the program actually appears to increase crime rates), youth boot camps, gun buy-back programs, peer counseling, summer job programs for at-risk youth, neighborhood watch programs, and home detention and monitoring programs. Blueprints did identify 11 treatment programs showing substantial evidence of effectiveness. Arguably the strongest evidence supports MST (Glisson et al., 2010; Henggeler & Schaeffer, 2010; Schoenwald, 2010), a coordinated array of interventions targeting multiple systems in youths' lives, including immediate and extended family, neighborhood, peer networks, and school. Across the various trials, MST has been shown to increase parenting skills, improve family relations, expand positive social resources such as number of non-delinquent friends, improve grades and vocational skills, and boost engagement in positive activities and social support networks. MST trials have shown reductions of up to 70% in rates of re-arrest and reductions of up to 64% in out-of-home placements. MST has proven more effective than a variety of “usual care” alternatives to which youths are typically assigned, including probation services, child welfare services, and individual outpatient therapy (Weisz, Kuppens, Eckshtain, Ugueto, Hawley, & Jensen-Doss, 2012). Unfortunately, a number of the practices found to be ineffective, or even harmful, continue to be widely used.
Most research on youths in the juvenile justice system has focused mainly on boys, or has neglected to explore potential gender differences. This is understandable in the light of the much higher rates of adjudication among boys, higher rates of conduct disorder in boys (Teplin et al., 2006), and generally more violent nature of crimes by boys relative to crimes by girls. However, the proportion of violent crimes perpetrated by girls is rising, particularly assault (Snyder & Sickmund, 2006), and more girls than boys commit status offenses (e.g., truancy, running away from home). These nuanced gender differences highlight the need for research that specifically addresses how adjudicated boys and girls differ and how treatments may be tailored to fit the differences. Some evidence suggests that female delinquents have higher rates of psychological dysfunction than male delinquents, and may also have experienced more abuse, neglect, and family history of mental illness (McCabe, Lansing, Garland, & Hough, 2002; Teplin et al., 2006). There does appear to be a need for research on effective strategies for tailoring treatments to the distinctive histories and current profiles of girls in the juvenile justice system.
Youths in the Child-Welfare System
Like youths involved in juvenile justice, youngsters caught up in the child welfare system often have complex needs. The maltreatment that causes youngsters to be removed from their homes and the stressful and confusing process of foster placement—indeed, often a series of placements—can be potent risk factors for mental disorder. The youths may live with total strangers, and in unfamiliar settings, with frequent changes making it difficult to form stable friendships or even school placements. Complicating the picture, the child welfare system is a secondary service sector, meaning it is not specifically designed for treatment of mental health problems, despite the fact that entry into the system is a common precursor to mental health services (see Garland, Hough, Landsverk, & Brown, 2001; Garland, Hough, McCabe, et al., 2001; Garland, Landsverk, Hough, & Ellis-Macleod, 1996), particularly for youths who have experienced physical or sexual abuse (Garland et al., 1996).
As with the juvenile justice population, successful interventions for child welfare youths have tended to employ strategies in multiple domains, and to involve multiple caregivers and community supports. A special adaptation of MST, Multisystemic Therapy-Child for Child Abuse and Neglect (MST-CAN) has proven effective in at least one randomized effectiveness trial (e.g., Swenson, Schaeffer, Henggeler, Faldowski, & Mayhew, 2010). MST-CAN includes the standard components of MST and integrates safety planning, anger management for parents, and additional emphasis on family problem-solving and communication. MST-CAN, when used in a community mental health treatment setting, is significantly more effective than enhanced outpatient treatment (EOT) in reducing youth psychopathology, youth out-of-home placements (e.g., hospitalizations), and youth placement changes. MST-CAN is also significantly more effective than EOT in improving parent functioning, as reflected in reduced psychological distress and fewer instances of violent discipline or other forms of maltreatment.
Another beneficial approach, this one growing out of four decades of research on development and treatment of antisocial behavior (see e.g., Forgatch & Patterson, 2010), is MTFC (Smith & Chamberlain, 2010). MTFC was developed in the mid-1980s to provide a community-based alternative to incarceration and placement of delinquent boys in residential group care settings; it has since been adapted for use with delinquent girls, and with youths referred from mental health and child welfare systems due to serious emotional and mental health problems. Intervention within MTFC involves working with youths, biological parents, and MTFC-trained foster parents using a combination of multilevel interventions that take place in family, community, and school contexts. Each youth is placed in an MTFC home for 6 to 9 months, where a comprehensive individually tailored behavior management program and case management are provided, together with close supervision and frequent reinforcement for learning and using positive adaptive social skills. Caregivers receive weekly family therapy guided by the Oregon Parent Management Training model (see Forgatch & Patterson, 2010); this includes effective parenting techniques, such as limit-setting, close monitoring of the youth's whereabouts, behavior, and peer associations, and reinforcement of the youth for prosocial and adaptive behavior.
Published trials have shown that MTFC is more effective in reducing delinquent behavior in boys (Chamberlain & Reid, 1998) and girls (Chamberlain, Leve, & DeGarmo, 2007) than standard group care. Importantly, the effects for girls included reduced pregnancy rates; at 24 months postbaseline, the rate was 27% for MTFC girls versus 46% for group care girls. Other trials have shown beneficial effects of MTFC in reducing severe mental health problems in youths from a mental hospital (Chamberlain & Reid, 1991) and the child welfare system (Chamberlain, Moreland, & Reid, 1992). More evidence on the nature, strength, and moderators of these effects will be useful in the years ahead, but given its success in the trials to date, MTFC is spreading fast as a resource for child welfare leaders who seek evidence-based approaches.
Young people involved in the child welfare system who have histories of maltreatment are at increased risk for PTSD, and may need specialty services for PTSD. Several relevant treatments are available, but the evidence appears strongest for TF-CBT (Cohen et al., 2010). TF-CBT has been shown to be effective for children as young as 3 (Sheeringa, Weems, Cohen, Amaya-Jackson, & Guthrie, 2011). This treatment integrates traditional CBT techniques with components specifically targeting trauma-related symptoms; one such component involves the creation and repeated reading of a trauma narrative—a form of exposure designed to reduce arousal and distress over time. Other components include parent training, safety planning, graduated exposure to nonthreatening trauma reminders (e.g., to safe playgrounds, if a traumatic event on a playground has prevented the youngster from enjoying playgrounds ever since), and joint parent–youth sessions designed to enhance communication and foster adaptive discussion about the abuse. RCTs have shown TF-CBT to be more effective in reducing PTSD symptoms than waitlist control groups, “supportive therapy,” and “child-centered therapy” (see review in Cohen et al., 2010). This treatment approach was designated “well-established” in the Silverman et al. (2008) review of evidence-based treatments for youths exposed to trauma (see Table 14.1).
As we have seen, there are tested treatments available for youngsters in the child welfare system. A particular challenge for this group may be the broad array of mental health and behavioral challenges that can arise, and the fact that the profile may be quite different from one youth to another within the system. Chavira, Accurso, Garland, & Hough (2010) argue that evidence-based treatments for CW-involved youths should be sensitive to this diversity of profiles, equipped to address aggression and antisocial behavior, scholastic difficulties, socioeconomic disadvantage, and even suicidal behavior, as up to 33% of child welfare-involved youth report suicidal thoughts, threats, or attempts (Hukkanen, Souranger, & Bergroth, 2003).
Evidence-Based Psychotherapies and Everyday Youth Mental Health Care
At the heart of so much of the research on EBPs for youth is the implicit aim of improving care for the many youths who struggle with mental health problems, most of whom will never be participants in a treatment trial. It is worthwhile, from time to time, to take stock of how well we are doing, as a field, in pursuing this aim, and what the associated challenges and opportunities for improvement may be.
Limited Success in Dissemination
There certainly is extensive publicity for EBPs, within prominent journals (e.g., the special issue of Journal of Clinical Child and Adolescent Psychology, noted previously) and through government entities (e.g., the Office of the Surgeon General [1999, 2004], the President's New Freedom Commission on Mental Health [2003], and the National Registry of Effective Programs and Practices, operated through the Substance Abuse and Mental Health Services Administration [SAMHSA]). Despite the publicity, not to mention the replicated scientific support for the numerous EBPs noted in Table 14.1, most of the tested treatments are currently “practiced” largely in treatment studies and have not made their way into most everyday clinical care. Some EBPs that focus on improving behavior management skills for caregivers of delinquent or aggressive youth (e.g., MST, MTFC, and Triple P) have active dissemination programs and have made inroads, but penetration is relatively low even for these programs, and most everyday clinical service programs show very low levels, if any, of EBP components (see Brookman-Frazee, Haine, Baker-Ericzen, Zoffness, & Garland, 2010; Garland et al., 2010; Southam-Gerow et al., 2010; Weisz et al., 2009). There is also some evidence from surveys of training directors that emphasis on EBPs may not actually be growing in training programs, at least within North American doctoral programs and internship sites in clinical psychology (Woody, Weisz, & McLean, 2005). Complementing these data from North America, a U.K. survey published in 2006 by the Association for Child and Adolescent Mental Health (see http://www.acamh.org/) found that CBT was the dominant approach of only 20% of practitioner respondents, despite very substantial government pressure favoring CBT. Although the data available to us from North America and the United Kingdom are patchy, and certainly do not cover all practice or training sites, they do suggest that the EBPs emerging from five decades of research are not making their way into training or practice very quickly. Why not? Why wouldn't professionals who chose careers to help young people be eager to adopt practices that have been tested and shown to work?
Dissemination Challenges
Research in practice settings and with practitioner partners has suggested several challenges to dissemination of EBPs (Weisz, 2004; Weisz, Sandler, Durlak, & Anton, 2005; Weisz, Ugueto, Herren, Afienko, & Rutt, 2011). One is the fact that most of these treatments (see Table 14.1) have been designed for single problems or disorders (or homogeneous clusters—e.g., a few depressive disorders). For practitioners, whose caseloads tend to include a broad array of disorders, and whose cases tend to show marked comorbidity, learning one or two single-disorder EBPs may not be perceived as valuable enough to warrant the time and cost. An additional concern for some practitioners is that EBPs tend to ask a lot of therapists–e.g., learning a detailed manual (often a very lengthy one), preparing in advance for each session to an extent that would be rare in everyday practice, working from an agenda rather than letting the session flow freely, and coming up with creative ways to make the manualized, agenda-guided content engaging and motivating for the youth. None of these challenges is insurmountable, but each may require attention in efforts to disseminate EBPs, and perhaps in the very development of EBPs, a theme to which we turn next.
EBP Development and Testing Conditions Have Differed From the Conditions of Everyday Practice
The shape of EBPs, and particularly the degree to which they are compatible with the conditions of everyday practice, may have a lot to do with the conditions under which they are developed and tested. These conditions have tended to differ markedly from the conditions of actual clinical practice (Weisz, Jensen-Doss, & Hawley, 2005; Weisz & Gray, 2008). This may have limited our ability to extrapolate from the research findings to everyday youth clinical care. It may also have slowed the pace of dissemination to some degree, in part by raising practitioner concern over whether the treatments that look so promising in research are really equipped for prime time in real-world clinical practice. Youths referred to clinical care settings may differ from those recruited for efficacy trials in diverse ways, including severity and family adversity (Hammen, Rudolph, Weisz, Burge, & Rao, 1999; Southam-Gerow, Weisz, & Kendall, 2003). Staff clinicians in clinics tend to differ from research therapists in RCTs in their background and training, daily work, clientele, and professional goals (see Palinkas et al., 2008; Weisz & Addis, 2006). In addition, clinical practice and research settings tend to differ in numerous ways that could affect youth treatment outcomes and prospects for dissemination. In practice settings, for example, a variety of time, productivity, financial, and other work pressures prevail that can make it hard to optimize the treatment environment in ways that are common in RCTs (Weisz & Addis, 2006). Such differences between the youths, therapists, and contexts of typical research and those of typical clinical care suggest that there is a significant gap between research and practice.
That gap might be addressed, of course, by research that examines the performance of treatment programs in real-world clinical care contexts. However, such research has been relatively rare, to date. In our own review of youth RCTs (Weisz, Jensen-Doss, & Hawley, 2005), we found that most studies took place in settings created for research (e.g., university labs and lab clinics, rooms in a school set aside for the study), with treatment provided to youths who were recruited (e.g., through ads), and with treatment provided not by practicing clinicians but rather by graduate students or others dependent on the researcher for their employment and income. Across the RCTs, only 13% of the youth samples were clinically-referred, treatment-seeking youth; only 19% of the studies used any practitioner as therapist (we only required that at least one practitioner be included among the study therapists); and in only 4% of the studies was treatment provided in a clinical service setting separate from the research program. Combining the three dimensions, we found that only 1% of the RCTs included clinically referred youths, at least one practicing clinician, and some treatment in a service setting. In sum, the literature provided little information about how EBPs might fare in fully representative clinical care conditions.
The evidence base is also limited in terms of a related question: Do EBPs produce better outcomes than the treatments youths would otherwise receive in usual clinical care? In some respects, this is the most basic question many in clinical practice might ask. Training and building competence in a typical manual-guided EBP can be quite costly, in both money and time, and may be challenging for clinicians who are managing the demands of a practice career (and it is unclear how many EBPs an individual therapist will need to be trained in). Thus, it is reasonable for practitioners, clinic directors, policy makers, and funders to ask whether shifting from usual treatment practices to EBPs will lead to better youth outcomes than current practices do. Youth treatment research has not emphasized the kinds of studies that could answer that question—that is, RCTs in which youths with significant mental health problems or disorders are randomly assigned to a specific EBP or to usual clinical care. However, a limited pool of such studies can be found, and we turn to those studies next.
Can EBPs Produce Better Outcomes Than Usual Clinical Care?
When our research group (Weisz, Jensen-Doss, & Hawley, 2006) set out to identify these studies and synthesize their findings within a meta-analysis, we were not at all sure what the studies would show. Although proponents of EBPs have suggested that they should be used in preference to usual clinical care, a number of authors have expressed concerns about EBPs and their manuals that raise questions about whether they would even be as effective as usual care. Various writers have raised concerns that EBPs (a) have been developed mainly with relatively simple cases, even subclinical youths, and may not work well with the more challenging cases often seen in usual care; (b) have been structured for single disorders or problems and may not fare well with co-occurring problems and comorbidity, which are common in usual care; (c) are so rigidly manualized that they make it hard for therapists to individualize treatment to fit distinctive client needs, including those of minority clients, or adjust to unexpected events in client's lives; and (d) are lacking in the flexibility needed for building rapport and a strong therapeutic relationship (Addis & Krasnow, 2000; Addis & Waltz, 2002; Bernal & Scharron-Del-Rio, 2001; Garfield, 1996; Gray-Little & Kaplan, 2000; Hall, 2001; Havik & VandenBos, 1996; Strupp & Anderson, 1997; Sue, 2003; Westen, Novotny, & Thompson-Brenner, 2004a, 2004b).The concerns raise questions about whether EBPs have the characteristics needed to outperform, or even match, the performance of usual clinical care when the two are pitted against one another in fair comparisons.
Our search yielded 32 methodologically acceptable RCTs (23 published articles, 9 dissertations) that had directly compared usual care to EBPs (identified through reviews explicitly structured to determine which treatments qualified as evidence-based). The 32 studies spanned 1973 to 2004; mean sample age ranged from 6 to 17 years; about three quarters of the EBPs were specific behavioral or CBT interventions, and most of the remainder were systems-oriented approaches such as multisystemic therapy. On average, the EBPs did outperform usual care. The mean posttreatment effect size was .30, falling between conventional cutoffs for “small” and “medium,” and markedly lower than mean effects found in prior meta-analyses (see Figure 14.1). The superiority of the EBPs was not reduced by high levels of youth severity or by inclusion of minority youths, thus providing no support for at least two of the concerns raised by critics of these treatments. To put the findings into context, a mean effect of .30 translates into a probability of 58% (slightly better than the chance expectancy of 50%) that a randomly selected youth receiving an EBP would be better off after treatment than a randomly selected youth receiving usual care. A more pessimistic picture was presented in a reanalysis of the Weisz et al. (2006) meta-analysis studies by Spielmans, Gatlin, and McFall (2010); controlling for factors that they believed might bias study findings in favor of EBPs, Spielmans et al. (2010) concluded that EBPs did not significantly outperform usual care (see Ougrin & Latif [2011] for a similar conclusion regarding therapy engagement in six RCTs comparing usual care to a specific manualized (or replicable) psychotherapy for treatment of youth self-harm). One conclusion on which all the meta-analysis authors would likely agree is that outcomes have been quite variable across studies, with a number of studies showing the outcomes of usual care to be similar or superior to the EBP outcomes to which they were compared. This variability is shown in Figure 14.2.
Some Implications of the EBP Versus Usual Care Findings for Stakeholders in Youth Mental Health Care
The EBP versus usual care meta-analysis by Weisz et al. (2006), the reanalysis by Spielmans et al. (2010), and the therapy engagement meta-analysis by Ougrin and Latif (2011) are certainly not definitive, given the modest sample of studies included. However, the findings do suggest implications for future research and a question related to treatment adoption by various stakeholders in youth mental health. The question: What kind of evidence on “evidence-based psychotherapies” should be used when policy makers, clinical administrators, practitioners, and consumers of youth mental health care decide whether to shift from usual clinical practices to tested treatments? Because such a decision is a weighty one for most providers, encompassing the cost of care and the question of which forms of help will really help young people most, it seems important to know whether the evidence shows that a shift to the new treatment is likely to lead to better outcomes than simply retaining the intervention status quo. The meta-analytic findings shown in Figure 14.2 indicate that a number of treatments officially designated “evidence-based” may not meet that standard. Figure 14.2 suggests that we cannot safely assume that all EBPs are superior to what clinicians are doing routinely in usual care. Even studies testing EBPs of the same name (e.g., anger management and problem-solving skills) showed very different effects depending on (a) the specific treatment procedures used, and (b) to what form of usual care the EBPs were compared. From a clinical policy perspective, a case could be made that whether a specific form of usual care should be replaced with a particular EBP may need to depend on (a) not just the generic form of the EBP (e.g., anger management training) but the specific protocol, and (b) what form(s) of usual care prevail in the setting in question. Priority for changing current practices might best be given to the specific EBPs that outperform the kinds of usual care that prevail in the service setting where a change is contemplated. We consider other implications of the EBP versus usual care comparisons as we turn to a discussion of strategies for strengthening our tested treatments.
Strategies for Strengthening Youth Psychotherapies
Several strategies for building stronger treatments are suggested by the evidence reviewed thus far, including, but not limited to, the meta-analytic findings shown in Figure 14.2.
Learning From Usual Care
One possibility suggested by Figure 14.2 is that some of the interventions now regarded as usual care may have genuine potential as effective treatments. Those forms of usual care that outperform current EBPs may turn out to be interventions that warrant documenting in written protocols and testing in their own right. Some of these might eventually make their way into future lists of EBPs. For this to be feasible, however, investigators will need to shift from treating usual care as a mere “control condition” to regarding it as a set of interventions worth documenting and studying in their own right. In general, the studies cited in Figure 14.2 provided good documentation of the EBPs but poor documentation of the contents and procedures of the usual care conditions to which the EBPs were compared. In most cases we were unable to determine, with any precision, what “usual care” actually consisted of. This problem needs to be solved if we are to maximize the hypothesis-generating potential of EBP versus usual care research. Methods are now available for documenting the contents of usual care, through a standardized clinician checklist (Weersing, Weisz, & Donenberg, 2002) and through a system for observer coding of intervention sessions (McLeod & Weisz, 2005, 2010). The checklist has been used to describe usual care for a variety of youth problems and conditions (Weersing et al., 2002), and the observational coding system has been used to document characteristics of usual care in treatment of youth disruptive disorders (Brookman-Frazee et al., 2010; Garland et al., 2010) and depressive and anxiety disorders (Southam-Gerow et al., 2010; Weisz et al., 2009). In the next generation of youth treatment studies, these methods and others could be used to characterize those patterns of usual care that show evidence of benefit and might thus become candidates for testing in their own right.
Enriching Our Understanding of What Makes Treatments Work
Whatever the collection of EBPs looks like at any particular time, there is much to be gained by enriching our understanding of what makes these treatments work—that is, what the specific change processes are through which treatment benefit is generated. This knowledge can be used to strengthen the “punch” of treatments while shrinking or eliminating less essential components, thus enhancing both the potency and efficiency of intervention. One approach to this goal is mediation testing, ideally leading to identification of true mechanisms of change, but as our earlier review showed, surprisingly few mediators have been replicated in youth psychotherapy research. There are myriad plausible reasons for the elusiveness of replicated mediators, some of which may be addressed only by changing the way RCTs are designed, with assessment of multiple candidate mediators and outcomes at pretreatment, posttreatment, and at several occasions during treatment (Kazdin, 2007). Because frequent assessments with multiple measures are resource- and time-intensive, it may be wise to identify the most promising candidate mediators from existing RCT datasets with less-than-ideal assessment schedules for testing in future RCTs with enriched assessment schedules. Reviews (Chu & Harrison, 2007; Weersing & Weisz, 2002b) have found that researchers have often collected data on potential mediators but without then conducting formal tests of mediation. We encourage researchers to include such formal tests and to consider four strategies that could markedly enhance our understanding.
Boosting power to detect mediation. Because youth psychotherapy outcome studies rarely have very large sample sizes, it is imperative that researchers choose statistical methods with the highest power to detect hypothesized mediation effects (and with reasonable Type I error rates). Baron and Kenny's (1986) causal-steps method, used in 71% of the mediation tests published in the Journal of Consulting and Clinical Psychology and the Journal of Applied Psychology from 2000 to 2003, actually has very low power, according to Fritz and MacKinnon (2007). These authors recommended that researchers use, instead, one of the following more amply powered methods: (a) bias-corrected bootstrapping (a kind of resampling method), (b) joint significance testing, or (c) PRODCLIN asymmetric confidence-intervals testing (but see Fritz, Taylor, & MacKinnon, 2012 for conditions under which bias-corrected bootstrapping is likely to produce inflated Type I errors). An additional advantage of the recommended mediation tests is that the statistical code to conduct some of these tests with various software programs (e.g., SPSS, SAS, R) has been made freely available by mediation methodologists.1
Testing for mediation in the absence of a treatment main effect. Identifying a significant treatment condition main effect is a necessary step in Baron and Kenny's (1986) causal-steps test of mediation. However, mediation can occur in the absence of a main effect of treatment.2 This is because a main effect (total effect) may be the sum total of several effects, including the direct effect of the treatment on the outcome and indirect effects of the treatment on the outcome through one or more mediators; if the direct and indirect effects are in opposite directions, they may sum to zero, resulting in a nonsignificant main effect (Hayes, 2009; MacKinnon, Fairchild, & Fritz, 2007). Mediation testing in the absence of significant main effects is particularly pertinent to more recent RCTs that have compared a target treatment to usual care or to an alternative treatment (rather than to a waitlist control) and found no significant treatment effects. The target therapy may lead to improved outcomes through increasing one hypothesized mediator, and the alternative treatment may lead to similarly improved outcomes through a second mediator. In such cases it would be unfortunate to miss out on the discovery of two mediators that could illuminate how two different treatments work because there was no main effect of treatment. Therefore, several mediation researchers have recommended testing for mediation even when main effects are nonsignificant (see e.g., Hayes, 2009). Fortunately, the three methods recommended in the previous paragraph allow tests of mediation whether main effects are significant or not.
Testing for moderated mediation or mediated moderation. For youth psychotherapy in general, change processes are likely to be too complex to be captured by a simple model involving one mediator. The strength or direction of the mediation relationship may be different in each treatment condition of an RCT or at each level of a moderator. These more complex models are examples of moderated mediation (Muller, Judd, & Yzerbyt, 2005), also termed conditional indirect effects (Preacher, Rucker, & Hayes 2007). Moderated mediation models make sense in that two different therapy protocols may have different effects on the mediator and also on how the mediator relates to outcome (Kraemer et al., 2002). On the other hand, mediated moderation occurs only when there is overall moderation of treatment effects and when a mediation relationship accounts for the moderation (Muller et al., 2005), that is, the mediator is an intermediate variable between the interaction (of the treatment and moderator) and the outcome (MacKinnon, Fairchild, et al., 2007). In a special case of mediated moderation, the mediated baseline by treatment moderation, the moderator is a baseline variable and the mediator is the change in that same variable during treatment (MacKinnon, Fairchild, et al., 2007). For example, in an RCT of parent training, if families high on harsh parenting at baseline (i.e., the moderator) showed greater improvement in youth externalizing symptom outcomes than families low on harsh parenting at baseline, relative to control, and change in harsh parenting mediated treatment effects, then the mediation would be accounting for the moderation. The mediated baseline by treatment moderation model is common in prevention research (MacKinnon, Fairchild, et al., 2007) and could be useful to youth psychotherapy researchers.
Identifying true mechanisms of change. Eventually it will be important to move beyond mere mediation to identify processes that operate as true mechanisms of change. Kazdin (2007) has proposed that although demonstrating statistical mediation is a first step in this process, for the mediator to qualify as a change mechanism requires (a) strong associations between the treatment and the mediator and between the mediator and change in outcome, (b) specificity of the mediator such that other candidate variables are shown not to mediate treatment outcome, (c) consistency of the mediation effect across studies, (d) experimental manipulation of the mediator in subsequent studies to confirm that the relation between mediator and outcome is causal and in the expected direction, (e) temporal precedence of the mediator in relation to treatment outcome, (f) a dose–response relationship in which enhancement of the mediator is associated with enhanced outcome, and (g) plausibility or coherence of how the mediator brings about therapeutic change and how relevant findings fit into the evidence base. As best we can determine, no true mechanism of change has yet been established according to these criteria, either in youth or adult psychotherapy. Indeed, satisfying all these criteria may well require marked improvements in measurement technology (e.g., to capture the precise timing of change in mediators and outcomes). Nonetheless, identifying change mechanisms is an important long-term aspiration for the field.
Understanding and Supporting Treatment Fidelity: Therapist Adherence and Competence
Regardless of the prior evidence supporting a particular treatment, its impact going forward is likely to depend significantly on how therapists deliver it. This brings us to the need for quality control in youth therapy. The development and testing of quality control standards, embodied within treatment fidelity measures, lags well behind the development and dissemination of evidence-based treatment protocols. Treatment fidelity includes two components: (1) adherence, defined as the degree to which a therapist follows the content and procedures of a manualized treatment protocol, and (2) competence, defined as the skillfulness with which a therapist conducts treatment (Waltz, Addis, Koerner, & Jacobson, 1993). In research trials, it is important that the treatment procedures used be a faithful representation of the treatment protocol that is ostensibly being evaluated, so that findings will indeed reflect on that specific protocol. In clinical practice, accurately representing the intervention provided to patients is a matter of professional ethics. However, in both research and clinical practice, there are surprisingly few quality control standards in place to ensure that treatments are carried out as they were intended to be delivered.
Treatment fidelity, although often discussed in our field, has remained surprisingly understudied to date. Kazdin et al. (1990) reviewed youth psychotherapy outcome studies published between 1970 and 1989 and found that 19.3% of the studies reported assessment of treatment fidelity. Perepletchikova, Treat, and Kazdin (2007) developed a measure, the Implementation of Treatment Integrity Procedures Scale (ITIPS), to determine the degree to which RCTs assess treatment fidelity. The 22-item measure taps treatment integrity assessment (adherence and competence) via direct and indirect methods, psychometric properties of the treatment integrity measures used, a protocol to determine whether treatments delivered were an accurate representation of the intended treatment, the training of treatment integrity raters and evaluation of interrater reliability, and report of treatment integrity protocol implementation. A review of 147 youth and adult psychotherapy research articles published between 2000 and 2004 (Perepletchikova et al., 2007) revealed that only 3.5% of the RCTs included what the authors considered adequate assessment of treatment fidelity.
Measuring adherence. Therapist adherence has been studied more frequently and extensively than therapist competence. However, there is no commonly accepted measurement methodology. Adherence measures differ widely in a variety of important dimensions (Waltz et al., 1993), such as the criterion against which the therapist's performance is measured, complexity of the ratings scheme and level of expertise required to make ratings, sources of information (e.g., audiotapes, videotapes, therapist- or client-report on checklists and questionnaires), and unit of analyses (e.g., complete treatment session, randomly selected segments). Additionally, most adherence measures have been developed by researchers and only used for a single study or cluster of related studies conducted by a single research group, and thus may not be particularly transportable.
Direct methods of assessment, such as ratings of videotaped treatment sessions by an independent team of trained raters, certainly provide greater potential for objectivity than ratings by therapists, supervisors, or clients. However, feasibility of implementation is an important issue in treatment fidelity assessment, and observational coding systems are costly and time-consuming. Thus, Schoenwald, Henggeler, Brondino, and Rowland (2000) recommended the use of simple, brief, user-friendly measures that can be implemented in everyday clinical care settings and can be shown to be associated with treatment outcomes. Few such measures exist, but the MST treatment fidelity literature is headed in this direction.
Henggeler, Borduin, Schoenwald, Huey, and Chapman (2006) developed the 28-item MST Adherence Measure-Revised (TAM-R) rated on a 5-point Likert scale, to assess in-session therapist adherence. The TAM-R is completed separately by youths, caregivers, and therapists to rate level of adherence of treatment sessions. Examples of measure items are “the therapist tried to understand how the family's problems all fit together” (consistent with MST Principle 1, which states that the goal of assessment is to contextualize problems within a broader conceptual framework) and “the therapist recommended that family members do specific things to solve their problems” (consistent with MST Principle 4, which states that treatment should be present-focused and target specific problems for intervention). In a study assessing MST for juvenile offenders, Schoenwald, Chapman, Sheidow, and Carter (2009) found that parent-reported ratings of therapist adherence using the TAM-R predicted reduced rates of long-term criminal offenses. Similarly, Schoenwald and colleagues (2000) found that parent-reported ratings of therapist adherence using the TAM (Henggeler & Borduin, 1992) predicted reduced rates of criminal offenses, drug use, antisocial behavior problems, and improvements in family relationships. Ratings of youths, caregivers, and therapists have not been found to correlate very highly with one another, and we have not seen assessments of whether these informant reports are associated with external observer ratings; assessing these associations, to address the important question of measure validity, will be a valuable direction for future research.
Measuring competence. Youth psychotherapy fidelity research has mainly focused on therapist adherence. Competence assessments share the complexities noted earlier for adherence measurement (e.g., varied measurement modalities, sources of information, units of analyses), with the added challenge of operationalizing the construct of therapist competence. Additionally, raters are required to have a high level of expertise in order to assess quality of treatment delivery, and the subjectivity of such ratings could lead to low interrater reliability. Sburlati, Schniering, Lyneham, and Rapee (2011) proposed a model for conceptualizing therapist competencies in working with youngsters who have anxiety and depressive disorders; the model includes generic therapist competencies (general skills that are valued in therapists regardless of treatment orientation) and specific cognitive-behavioral therapy technique competencies, taking into account social, cognitive, and emotional developmental stages. It seems clear that operationalizing and measuring competence in the delivery of youth treatments remains a significant challenge for the field.
Future directions for the study of treatment fidelity. As we have seen, adherence assessment methods have been developed and implemented in a number of youth therapy studies, and in multiple forms. Competence assessment has lagged behind, and significant work on the measure development front will be needed in the days ahead. For both forms of fidelity assessment, practical feasibility will be a key issue. In a recent review, Schoenwald and colleagues (2011) identified several challenges to implementation of fidelity measures, including financial and professional burdens and the ability to fit data collection and measurement seamlessly into clinic routines and protocol. Although observational coding systems are more objective and rigorous in their methodology, they may not be either practical or feasible in most treatment research or clinical practice (e.g., due to high cost, high level of expertise required, and time requirements). It seems clear that if fidelity assessment is to become a routine part of clinical research, and to be feasible for clinical practice, what will be needed are brief, user-friendly treatment fidelity measures that are low-cost and efficient while retaining psychometric integrity and validity. This may be a tall order, requiring some of our best minds.
Improving Our Use of Technology
Many youths who need effective mental health services cannot access them because of their geographic location or limited family resources. To address these and other barriers to care, some researchers are capitalizing on modern technological advances to increase the accessibility and cost-effectiveness of psychosocial treatments. In some cases, this involves a shift away from traditional forms of face-to-face therapist-patient talk therapy. Preliminary research on the use of computer-based and computer-assisted treatments for internalizing disorders and eating disorders in adults has been promising, but less research has been conducted with young people.
Camp Cope-A-Lot is a computer-assisted, animated treatment for youth anxiety disorders, based on the Coping Cat program (see Table 14.1; see Kendall and Hedtke, 2006). The young patient navigates through session activities and videos on the computer, interacting with animated figures, and with the therapist acting as a coach to guide the youngster through the program. One RCT comparing this computer-assisted treatment to standard individual CBT and a computer-based academic learning control condition showed that greater gains were made in both CBT conditions than the computer control condition (Kendall, Khanna, Edson, Cummings, & Harris, 2011). Although comparable gains were made in the two CBT conditions, youth participants reported greater treatment satisfaction with Camp Cope-a-Lot than with standard CBT.
Cognitive bias modification (CBM) interventions have also been used to treat youth anxiety disorders. The rationale is that youths with anxiety disorders, compared to nonanxious controls, have been found to show a bias toward automatic attention to threat. CBM is designed to target biased automatic cognitive/attentional processes by shaping disengagement from threatening stimuli and an attentional shift toward neutral stimuli. In the very first study of CBM for youth anxiety disorders, Rozenman, Weersing, and Amir (2011) used an attention dot probe task to treat 16 anxious youths. Youths completed the attention dot probe task on a computer. First, a fixation cross appeared on the computer screen for 500 ms. It was then replaced by two faces, one above the other, depicting the same person with either a neutral or disgust facial expression. After the presentation of the faces for 500 ms, a probe (the letter “E” or “F”) appeared where one of the two faces used to be, and participants indicated the probe letter by pressing the “E” or “F” key on the computer keyboard. The probe appeared behind the neutral face for 80% of the trials; this tilt toward the neutral face was designed to create attentional disengagement from the threatening stimuli and increase attention to the neutral stimuli. In an open trial of this treatment approach, Rozenman and colleagues (2011) found that youths experienced a significant reduction in anxiety and depression symptoms at posttreatment, with 12 of the 16 youths no longer meeting DSM-IV criteria for an anxiety disorder diagnosis. These intriguing findings point to the potential value of a full RCT testing the CBM method against an appropriate control or comparison condition.
Merry and colleagues (see Fleming, Dixon, Frampton, & Merry, 2011; Merry et al., 2012) developed a self-help computer program (SPARX) for youth depression. SPARX is a video game in which youths customize an avatar and navigate through a 3-D fantasy world with challenges and puzzles that teach them CBT skills such as problem solving, coping with negative thoughts, and relaxation techniques. SPARX was tested against a wait-list control group in a randomized trial focused on adolescents who had been excluded from mainstream education and who had significant symptoms of depression (Fleming et al., 2011); those treated with SPARX showed significantly greater symptom reduction on core depression measures, but not on all measures of psychological functioning. In a second RCT (Merry et al., 2012), a “noninferiority trial” with adolescents who were seeking help for depression, SPARX showed similar outcomes to an active treatment-as-usual comparison group, suggesting that the efficient, low-cost computerized approach to CBT was no less effective than significantly more costly treatment involving primarily individual face-to-face counseling delivered by trained clinicians.
Technology may also prove helpful in therapist training. Kendall and Khanna (2008) developed a computer-based therapist training program for CBT for youth anxiety disorders. The program, called CBT4CBT, is a DVD that walks the therapist, step-by-step, through the same content as the print version of the therapist treatment manual, with quizzes included to check for understanding. The program also contains other helpful supplements, such as therapist notes/tips for each treatment session, and various audio-visual stimuli (e.g., exposure videos) for the therapist to use in-session. Kendall et al. (2011) conducted one RCT evaluating a CBT4CBT training group as compared to a manual-based training group and a waitlist control group; Trainees in the CBT4CBT and manual-based training groups (versus the wait-list control) showed similarly high levels of treatment knowledge and program satisfaction.
Future directions for technology-assisted and technology-based treatments for youth psychopathology are almost certainly more extensive than any of us can now imagine. As the reach of computer games, smartphone applications, and Internet sites spreads, and the forms of electronic communication diversify, opportunities to reach young people in new ways will continue to expand. There can be little doubt that we are on the verge of a massive mushrooming of RCTs testing new ways to deliver interventions to young people through the emerging technological advances that have so captured youth attention and interest.
Guiding Treatment Through Ongoing Feedback on Youth Treatment Response
One burgeoning field of research that has the potential to complement and improve therapy is the provision of feedback on youth treatment response to clinicians (and supervisors) throughout the course of therapy. Recent work with adult therapy has shown that providing feedback to clinicians can result in improved therapy success rates and reduced deterioration in client functioning (Anker, Duncan, & Sparks, 2009; Lambert et al., 2002). Relatively few studies have focused explicitly on youth treatment, but initial findings have shown an association between the use of routine feedback and improved therapeutic relationships and therapy outcome (Bickman, Breda, deAndrade, & Kelley, 2010; Stein, Kogan, Hutchison, Magee, & Sobero, 2010).
In a recent meta-analysis by Shimokawa, Lambert, and Smart (2010), data from six major studies employing a psychotherapy feedback system for adult therapy (i.e., Outcome Questionnaire-45) were reanalyzed in an effort to determine the effects of progress feedback on clinical outcomes. Feedback interventions were broken into three distinct categories—patient progress feedback to clinicians only, patient progress feedback to clinicians and patients, and patient progress feedback to clinicians plus additional clinical support tools. Results indicated that the use of all three forms of feedback intervention were associated with enhanced treatment outcomes.
In recent work on the youth therapy front, Chorpita, Weisz, and colleagues (Chorpita et al., 2010; Weisz et al., 2011) have developed strategies for generating ongoing, frequent feedback on youth patient progress during treatment via two brief, psychometrically sound measures, displayed within an Internet-based system. One of the measures, the Brief Problem Checklist (Chorpita et al., 2010) is a 12-item method for obtaining weekly youth and caregiver reports on severity of the youth's internalizing and externalizing problems. The other measure, Youth Top Problems (Weisz et al., 2011), is a 3-item idiographic consumer-driven method through which youths and caregivers identify, at pretreatment, the three most important problems for which the youth needs help in treatment, and then rate the severity of these problems weekly thereafter. Weekly ratings on these two measures are displayed within a web-based system that provides quick access to those making treatment plans and adjusting those plans throughout an episode of care. The system provides the kind of frequent updates on the youth's response to treatment that can guide ongoing treatment planning and supervision. The approach used to integrate this information with a manual-guided treatment program is described next.
Restructuring Evidence-Based Psychotherapies to Fit Clinical Practice Needs
Discussion of feedback systems connects in an interesting way to the theme of restructuring EBPs to fit the conditions of clinical practice. As we have seen (and as shown in Table 14.1), more than five decades of research have produced a rich array of EBPs, and a rich body of information on the groups with which and the conditions under which these treatments work. As we have also seen, most of these EBPs have been developed and tested under carefully arranged conditions that are appropriate for experimental tests but not very representative of the clientele, clinicians, or conditions of everyday clinical practice; and when EBPs are pitted against usual clinical care in randomized trials, their relative benefit is modest on average, and variable, such that a number of the EBPs show effects that are similar to or weaker than usual care. We have noted some of the challenges that may limit the effectiveness of many EBPs in everyday practice conditions. Among the challenges, (a) most EBPs are designed for single disorders or homogenous clusters (e.g., two depressive disorders), but most practitioners carry quite diverse caseloads, limiting the value of any single-disorder protocol; (b) the single-disorder focus of most EBPs also conflicts with the fact that most referred youths have comorbid disorders and co-occurring problems; (c) most EBPs are ballistic, designed for sustained focus on one goal or objective throughout treatment, but youths in treatment often show change in patterns of dysfunction and treatment needs during episodes of care. To address these needs, some investigators are moving toward restructured treatments that provide broader and more flexible coverage of problems and disorders while retaining the core components of the EBPs that have been developed and tested so carefully over the decades.
Our own effort in this regard is illustrative; it has developed as part of the work of the Research Network on Youth Mental Health (see Schoenwald, Kelleher, Weisz, & the Research Network on Youth Mental Health, 2008), which set out to address challenges like those noted above. One result was an integrative modular approach to delivering the components of EBPs for depressive, anxiety, and conduct-related problems and disorders (Chorpita & Weisz, 2009; Weisz & Chorpita, 2011. The modules of this treatment protocol, called MATCH (for Modular Approach to Therapy for Children…[Chorpita & Weisz, 2009]), were brief summaries of treatment elements commonly included in CBT for depression, CBT for anxiety, and behavioral parent training for disruptive conduct (see Chorpita & Daleiden, 2009; Chorpita, Daleiden, & Weisz, 2005). These modules are shown in Figure 14.3. By encompassing multiple broad domains of psychopathology, the modular treatment addresses the concern that practitioners typically carry broad caseloads, and that referred youths tend to have multiple co-occurring disorders and problems. The multiproblem focus of MATCH also makes it possible to address the flux in treatment needs and problems that youths in treatment often show during episodes of care. As a youth's treatment needs shift, therapists are able to respond by navigating across the modules shown in Figure 14.3, to shift the focus of treatment as needed.
Navigating across modules appropriately, however, requires an ongoing flow of feedback on the youth's current functioning and response to treatment. This need for ongoing, timely feedback—ideally, weekly—has led us to develop the two brief, psychometrically sound measures described above—Brief Problem Checklist (Chorpita et al., 2010) and Youth Top Problems (Weisz et al., 2011)—and to build a Web-based system for displaying information from these measures, obtained from youths and caregivers each week. Weekly ratings on these two measures are displayed within an Internet-based system for ease of access. The weekly updates help guide decisions as to whether shifts in treatment focus are needed and which modules may be most appropriate for the next steps of treatment.
We have tested the MATCH modular approach in one completed randomized effectiveness trial (Weisz et al., 2012). Community practitioners from 10 different outpatient service settings participated. These were randomly assigned to three conditions: Standard manual treatment (therapists used standard separate manuals for CBT for depression, CBT for anxiety, and behavioral parent training for conduct problems); modular treatment (i.e., the MATCH manual, integrating the elements of the three separate treatments); and usual care. Outcomes were assessed in this study through the weekly BPC and TPA measures as well as through standardized diagnostic assessment at pre- and posttreatment. Our analyses showed that MATCH produced significantly steeper trajectories of improvement than usual care and standard treatment on multiple BPC and TPA measures. Youths treated with MATCH also had significantly fewer diagnoses than usual care youths at post-treatment. In contrast, outcomes of standard manual treatment did not differ significantly from usual care. These findings suggest that a modular redesign of EBPs that integrates core elements of EBPs for multiple forms of dysfunction may be an effective approach to adapting EBPs for everyday clinical care. Two other randomized effectiveness trials of MATCH are now underway.
Designing and Testing Treatments With Their Ultimate Deployment in Mind
Our effort to design EBPs for use in clinical care contexts is but one of a number of examples in the youth intervention literature (see, for example, Henggeler & Schaeffer, 2010; Smith & Chamberlain, 2010). These illustrate a broader approach to thinking about treatment development that has been identified in prior work (e.g., Weisz, 2004) as the deployment-focused model of treatment development and testing. This model reflects the basic idea that it makes sense to build and test interventions with the clientele and clinicians, and in the contexts for which those interventions are ultimately intended. Despite examples to the contrary, most EBPs have not been developed and tested in this manner, and it is possible that this fact may have contributed to some of what we saw in Figures 14.1 and 14.2. The growing body of research in implementation science (Fixsen, Naoom, Blasé, Friedman, & Wallace, 2005) strongly suggests that any practices—including EBPs—risk a loss of potency when moved into contexts and conditions that are new and different from those where they were previously used and tested. Successful implementation usually requires considerably more than simply relocating the intervention; multiple steps of intervention adaptation, intervener selection and coaching, and often even recipient and organizational preparation may be required (Fixsen et al., 2005). The modest mean effect size for EBP versus usual care comparison, shown in Figure 14.1, and the fact that a number of EBPs did not outperform usual care, as shown in Figure 14.2, might be seen as highlighting the challenges of implementation.
This challenge may be particularly serious in those cases where the implementation context differs most from the context in which development and testing took place. The research lab development and series of efficacy trials through which most youth EBPs have been developed and tested have not exposed these therapies to the full array of factors present in the clientele, clinicians, and service clinic context of real-world clinical care. This might not be a major problem for psychotropics or other interventions that operate through the biological system. But for psychosocial interventions, a sequence of development and testing that bypasses those clinical context factors that may impact treatment process and outcome could leave the resulting therapies poorly prepared for real-world treatment conditions. As a result, the treatments that fare well in efficacy trials may not look so strong when placed in everyday care contexts and compared to the usual care that takes place in those conditions.
A relatively common pattern in youth therapy research has been for investigators to use carefully controlled efficacy designs to build and provide the evidence base for their treatment protocols, with the idea that effectiveness tests in representative clinical care settings will come later, when the intervention procedures have been perfected. Although this last step has not actually happened with EBPs, to date, the concept does acknowledge the value of assessing how well treatments fare in real-world treatment contexts. It is possible, though, that even when that last step is taken, the differences between treatment within efficacy research and treatment in actual practice are too numerous and too pronounced to be bridged as simply the final step after a series of efficacy studies. The number of dimensions along which treatment must be adjusted to span the lab-to-clinic gap may make the task of moving efficacy-tested treatments into everyday clinical care so complex that the task really needs to be a part of the treatment development process. Indeed, the very real-world factors that efficacy trial researchers might view as a nuisance or “noise” (e.g., youth comorbidity, parent pathology, family stressors that produce no-shows and dropouts, therapists with heavy caseloads) and thus attempt to avoid (e.g., by recruiting and screening cases, applying exclusion criteria, adding incentives for therapy attendance, hiring their own therapists), may in fact be precisely the kinds of factors that need to be understood and addressed if psychotherapy treatment protocols are to be created that fit well into clinical practice. EBPs that are stymied by these real-world factors may not fare so well in practice, no matter how strong they look in efficacy trials.
A closely related point is that implementing EBPs in practice settings may require interventions in those settings to address obstacles to effective use of the treatments. For example, treatments that call for weekly installments of skill-building with youths or parents may require new family engagement procedures (e.g., Nock & Kazdin, 2005) to generate faithful attendance. Or interventions that do not fit smoothly into the standard procedures of a clinic (e.g., assessment or supervision requirements that differ from the clinic routine) may only be possible if paired with organizational problem solving. Putting EBPs into the real-world settings for which they are ultimately intended could be the best way to identify, construct, and test the setting-focused interventions needed to make the target treatments succeed.
A Deployment-Focused Model of Treatment Development and Testing
Following this reasoning, we have proposed a shift from the traditional sequential efficacy trials model to a deployment-focused model of treatment development and testing (Weisz, 2004; Weisz, Jensen, & McLeod, 2005). This model includes a series of steps designed to (a) place the process of building treatments and testing their effects within the contexts for which they are ultimately intended, and (b) construe this process as ongoing and sequential, not as a single final step. A primary aim of the model is to create a process through which the treatment characteristics needed for success in real-world clinical application can be identified and built into the intervention as a natural part of the scientific process. A testable premise underlying the model is that the potential of an EBP to be beneficial in a practice context is most likely to be realized if the treatment has been adapted to practice conditions as a part of its development and testing. The model is consistent with findings in implementation science (Fixsen et al., 2005) that when interventions that succeed in one setting are moved to a very different setting, it is common for such efforts to struggle, and often fail initially. Some are ultimately successful, after multiple steps of intervention adaptation. The proposed deployment-focused model is a way of making that adaptation process a natural part of treatment development and testing, with the objective of creating treatments that are ready for prime time in clinical practice.
Summary and Conclusions
Youth psychotherapy has evolved over the past century from an art to a science, from a rich collection of principles and procedures built on the grand theories of the early 1900s to an empirically guided enterprise in which claims of effectiveness are tested scientifically. One result of this transition is an array of youth interventions that have met criteria for the status of “evidence-based psychotherapies,” and a growing body of evidence on the processes through which these therapies work, and on the boundaries within which they work. As we learn more about how to implement these interventions in various settings and with various populations, we also need to monitor their goodness of fit to representative clinical care clients and conditions, and their effectiveness relative to the usual care that prevails in everyday treatment. Evidence indicates that our current collection of youth EBPs does improve on usual care, on average, but only modestly so, and not in every comparison. This suggests, in turn, that the agenda for future research might profitably include investigating strategies for strengthening EBPs, expanding their potential to benefit the youths and families who seek treatment in everyday clinical care.
References
Achenbach, T. M., McConaughy, S. H., & Howell, C.T. (1987). Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101, 213–232.
Ackerson, J., Scogin, F., McKendree-Smith, N., & Lyman, R. D. (1998). Cognitive bibliotherapy for mild and moderate adolescent depressive symptomatology. Journal of Consulting and Clinical Psychology, 66, 685–690.
Addis, M. E., & Krasnow, A. D. (2000). A national survey of practicing psychologists' attitudes toward psychotherapy treatment manuals. Journal of Consulting and Clinical Psychology, 68, 331–339.
Addis, M. E., & Waltz, J. (2002). Implicit and untested assumptions about the role of psychotherapy treatment manuals in evidence based mental health practice. Clinical Psychology: Science and Practice, 9, 435–438.
Alexander, J. F., & Parsons, B. V. (1982). Functional family therapy: Principles and procedures. Monterey, CA: Brooks/Cole.
Anker, M. G., Duncan, B. L., & Sparks, J. A. (2009). Using client feedback to improve couple therapy outcomes: A randomized clinical trial in a naturalistic setting. Journal of Consulting and Clinical Psychology, 77, 693–704.
Asarnow, J. R., Goldstein, M. J., Tompson, M., & Guthrie, D. (1993). One-year outcomes of depressive disorders in child psychiatric inpatients: Evaluation of the prognostic power of a brief measure of expressed emotion. Journal of Child Psychology and Psychiatry, 34, 129–137.
Barkley, R. (1997). Defiant children (2nd ed.). New York, NY: Guilford Press.
Barlow, D. H., Nock, M. K., & Hersen, M. (2009). Single case experimental designs: Strategies for studying behavior change (3rd ed.). Boston, MA: Allyn & Bacon.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182.
Barrett, P. M., Farrell, L., Pina, A. A., Peris, T. S., & Piacentini, J. (2008). Evidence-based psychosocial treatments for child and adolescent obsessive-compulsive disorders. Journal of Child and Adolescent Clinical Psychology, 37, 131–155.
Beauchaine, T. P., Webster-Stratton, C., & Reid, M. J. (2005). Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: A latent growth curve analysis. Journal of Consulting and Clinical Psychology, 73, 371–388.
Beck, A. T. (1970). Cognitive therapy: Nature and relation to behavior therapy. Behavior Therapy, 1, 184.
Bernal, G., & Scharron-Del-Rio, M. R. (2001). Are empirically supported treatments valid for ethnic minorities? Toward an alternative approach for treatment research. Cultural Diversity and Ethnic Minority Psychology, 7, 328–342.
Bickman, L., Breda, C., deAndrade, A. R. V., & Kelley, S. D. (2010). CFIT evaluation report: The effects of CFIT on clinician behavior and youth mental health outcomes. Nashville, TN: Center for Evaluation and Program Improvement.
Beidel, D. C., Turner, S. M., & Morris, T. L. (2000). Behavioral treatment of childhood social phobia. Journal of Consulting and Clinical Psychology, 68, 1072–1080.
Block, J. (1978). Effects of a rational-emotive mental health program on poorly achieving, disruptive high school students. Journal of Counseling Psychology, 25, 61–65.
Bolton, P., Bass, J., Betancourt, T., Speelman, L., Onyango, G., Clougherty, K.,…Verdeli, H. (2007). Interventions for depression symptoms among adolescent survivors of war and displacement in Northern Uganda: A randomized controlled trial. Journal of the American Medical Association, 298, 519–527.
Brookman-Frazee, L., Haine, R. A., Baker-Ericzen, M., Zoffness, R., & Garland, A. F. (2010). Factors associated with use of evidence-based practice strategies in usual care youth psychotherapy. Administration & Policy in Mental Health & Mental Health Services Research, 37, 254–269.
Brookman-Frazee, L., Haine, R. A., Gabayan, E. N., & Garland, A. F. (2008). Predicting frequency of treatment visits in community-based youth psychotherapy. Psychological Services, 5, 126–138.
Burleson, J. A., & Kaminer, Y. (2008). Does temperament moderate treatment response in adolescent substance use disorders? Substance Abuse, 29, 89–95.
Campbell, J. M. (2003). Efficacy of behavioral interventions for reducing problem behavior in persons with autism: A quantitative synthesis of single-subject research. Research in Developmental Disabilities, 24, 120–138.
Casey, R. J., & Berman, J. S. (1985). The outcome of psychotherapy with children. Psychological Bulletin, 98, 388–400.
Chamberlain, P., Moreland, S., & Reid, K. (1992). Enhanced services and stipends for foster parents: Effects on retention rates and outcomes for children. Child Welfare, 5, 387–401.
Chamberlain, P., & Reid, J. B. (1991). Using a specialized foster care community treatment model for children and adolescents leaving the state mental hospital. Journal of Community Psychology, 19, 266–276.
Chamberlain, P., & Reid, J. B. (1998). Comparison of two community alternatives to incarceration for chronic juvenile offenders. Journal of Consulting and Clinical Psychology, 66, 624–633.
Chamberlain, P., Leve, L. D., & DeGarmo, D. S. (2007). Multidimensional Treatment Foster Care for girls in the juvenile justice system: A 2-year follow-up of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 75, 187–193.
Chambless, D. L., Baker, M. J., Baucom, D. H., Beutler, L. E., Calhoun, K. S., Crits-Christoph, P.,…Woody, S. R. (1998). Update on empirically validated therapies II. Clinical Psychologist, 51, 3–16.
Chambless, D. L., Sanderson, W. C., Shoham V., Johnson, S. B., Pope, K. S., Crits-Cristoph, P.,…McCurry, S. (1996). An update on empirically validated therapies. Clinical Psychologist, 49, 5–18.
Chavira, D. A., Accurso, E. C., Garland, A. F., & Hough, R. (2010). Suicidal behavior among youth in five public sectors of care. Child and Adolescent Mental Health, 15, 44–51.
Chen, C., & Ma, H. (2007). Effects of treatment on disruptive behaviors: A quantitative synthesis of single-subject researches using the PEM approach. Behavior Analyst Today, 8, 380–397.
Chorpita, B. F., & Daleiden, E. L. (2009). Mapping evidence-based treatments for children and adolescents: Application of the distillation and matching model to 615 treatments from 322 randomized trials. Journal of Consulting and Clinical Psychology, 77, 566–579.
Chorpita, B. F., Daleiden, E. L., & Weisz, J. R. (2005). Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research, 7, 5–20.
Chorpita, B. F., Reise, S., Weisz, J. R., Grubbs, K., Becker, K. D., Krull, J. L., & the Research Network on Youth Mental Health. (2010). Evaluation of the brief problem checklist: Child and caregiver interviews to measure clinical progress. Journal of Consulting and Clinical Psychology, 78, 526–536.
Chorpita, B. F., & Weisz, J. R. (2009). Modular approach to therapy for children with anxiety, depression, trauma, or conduct problems (MATCH-ADC). Satellite Beach, FL: PracticeWise.
Chu, B. C., & Harrison, T. L. (2007). Disorder-specific effects of CBT for anxious and depressed youth: A meta-analysis of candidate mediators of change. Clinical Child and Family Psychology Review, 20, 352–372.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum.
Cohen, J. A., & Mannarino, A. P. (2000). Predictors of treatment outcome in sexually abused children. Child Abuse & Neglect, 24, 983–994.
Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2010). Trauma-focused cognitive-behavioral therapy for traumatized children. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 295–311). New York, NY: Guilford Press.
Conrod, P. J., Stewart, S. H., Comeau, N., & Maclean, A. M. (2006). Efficacy of cognitive-behavioral interventions targeting personality risk factors for youth alcohol misuse. Journal of Child and Adolescent Clinical Psychology, 35, 550–563.
Corcoran, J., & Dattalo, P. (2006). Parent involvement in treatment for ADHD: A meta-analysis of the published studies. Research on Social Work Practice, 16, 561–570.
David-Ferdon, C., & Kaslow, N. J. (2008). Evidence-based psychosocial treatments for child and adolescent depression. Journal of Child and Adolescent Clinical Psychology, 37, 62–104.
De Los Reyes, A. (2011). Special section: More than measurement error: discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child and Adolescent Psychology, 40, 1–9.
De Los Reyes, A., Alfano, C. A., & Beidel, D. C. (2010a). The relations among measurements of informant discrepancies within a multisite trial of treatments for childhood social phobia. Journal of Abnormal Child Psychology, 38, 395–404.
De Los Reyes, A., Goodman, K. L., Kliewer, W., & Reid-Quiñones, K. (2010b). The longitudinal consistency of mother–child reporting discrepancies of parental monitoring and their ability to predict child delinquent behaviors two years later. Journal of Youth and Adolescence, 39, 1417–1430.
De Los Reyes, A., & Kazdin, A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131, 483–509.
Dybdahl, R. (2001). Children and mothers in war: An outcome study of a psychosocial intervention program. Child Development, 71, 1214–1230.
Eddy, J. M., & Chamberlain, P. (2000). Family management and deviant peer association as mediators of the impact of treatment condition on youth antisocial behavior. Journal of Consulting and Clinical Psychology, 68, 857–863.
Eisler, I., Dare, C., Hodes, M., Russell, G., Dodge, E., & Le Grange, D. (2000). Family therapy for adolescent anorexia nervosa: The results of a controlled comparison of two family interventions. Journal of Child Psychology and Psychiatry and Allied Disciplines, 41, 727–736.
Eisler, I., Simic, M., Russell, G. F. M., & Dare, C. (2007). A randomized controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa: A 5-year follow-up. Journal of Child Psychology and Psychiatry, 48, 552–560.
Eyberg, S. M., Nelson, M. M., & Boggs, S. R. (2008). Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Child and Adolescent Clinical Psychology, 37, 215–237.
Eysenck, H. J. (1952). The effects of psychotherapy: An evaluation. Journal of Consulting Psychology, 16, 319–324.
Fabiano, G. A., Pelham, W. E., Coles, E. K., Gnagy, E. M., Chronis-Tuscano, A., & O'Connor, B. C. (2009). A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clinical Psychology Review, 29, 129–140.
Ferdinand, R. F., van der Ende, J., & Verhulst, F. C. (2004). Parent–adolescent disagreement regarding psychopathology in adolescents from the general population as a risk factor for adverse outcome. Journal of Abnormal Psychology, 113, 198–206.
Ferdinand, R. F., van der Ende, J., & Verhulst, F. C. (2006). Prognostic value of parent–adolescent disagreement in a referred sample. European child & adolescent psychiatry, 15, 156–62.
Fixsen, D. D., Naoom, S. F., Blasé, K. A., Friedman, R. M., & Wallace, F. (2005). Implementation research: A synthesis of the literature (FMHI Publication No. 231). Tampa, FLP University of South Florida, Luis de la Parte Florida Mental Health Institute, National Implementation Research Network.
Fleming, T., Dixon, R., Frampton, C., & Merry, S. (2011). Pragmatic randomised controlled trial of computerized CBT (SPARX) for depression among adolescents alienated from mainstream education. Behavioural and Cognitive Psychotherapy. doi:10.1017/S1352465811000695
Forehand, R., Frame, C. L., Wierson, M., Armistead, L., & Kempton, T. (1991). Assessment of incarcerated juvenile delinquents: Agreement across raters and approaches to psychopathology. Journal of Psychopathology and Behavioral Assessment, 13, 17–25.
Forgatch, M. S., & Patterson, G. R. (2010). Parent management training—Oregon model: An intervention for antisocial behavior in children and adolescents. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 159–177). New York, NY: Guilford Press.
Freedheim, D. K., Freudenberger, H. J., & Kessler, J. W. (1992). History of psychotherapy: A century of change. Washington, DC: American Psychological Association.
Fritz, M. S., & MacKinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18, 233–239.
Fritz, M. S., Taylor, A. B., & MacKinnon, D. P. (2012). Explanation of two anomalous results in statistical mediation analysis. Multivariate Behavioral Research, 47, 61–87.
Garfield, S. L. (1996). Some problems associated with “validated” forms of psychotherapy. Clinical Psychology: Science and Practice, 3, 218–229.
Garland, A. F., Brookman-Frazee, L., Hurlburt, M., Accurso, E., Zoffness, R., Haine-Schlagel, R., & Ganger W. (2010). Mental health care for children with disruptive behavior problems: A view inside therapists' offices. Psychiatric Services, 61, 788–795.
Garland, A. F., Hough, R. L., Landsverk, J. A., & Brown, S. A. (2001a). Multi-sector complexity of systems of care for youth with mental health needs. Children's Services: Social Policy, Research, and Practice, 4, 123–140.
Garland, A. F., Hough, R. L., McCabe, K. M., Yeh, M., Wood, P. A., & Aarons, G. A. (2001b). Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 409–418.
Garland, A. F., Landsverk, J. A., Hough, R. L., & Ellis-Macleod, E. (1996). Type of maltreatment as a predictor of mental health service use for children in foster care. Child Abuse and Neglect, 20, 675–688.
Glisson, C., Schoenwald, S. K., Hemmelgarn, A., Green, P., Dukes, D., Armstrong, K. S., & Chapman, J. E. (2010). Randomized trial of MST and ARC in a two-level evidence-based treatment implementation strategy. Journal of Consulting Psychology, 78, 537–550.
Gray-Little, B., & Kaplan, D. (2000). Race and ethnicity in psychotherapy research. In C. R. Snyder & R. E. Ingram (Eds.), Handbook of psychological change: Psychotherapy processes & practices for the 21st century (pp. 591–613). New York, NY: Wiley.
Hall, G. C. N. (2001). Psychotherapy research with ethnic minorities: Empirical, ethical, and conceptual issues. Journal of Consulting and Clinical Psychology, 69, 502–510.
Halliday-Boykins, C. A., Schoenwald, S. K., & Letourneau, E. J. (2005). Caregiver–therapist ethnic similarity predicts youth outcomes from an empirically based treatment. Journal of Consulting and Clinical Psychology, 73, 808–818.
Hammen, C., Rudolph, K., Weisz, J. R., Burge, D., & Rao, U. (1999). The context of depression in clinic-referred youth: Neglected areas in treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 64–71.
Havik, O. E., & VandenBos, G. R. (1996). Limitations of manualized psychotherapy for everyday clinical practice. Clinical Psychology: Science and Practice, 3, 264–267.
Hawley, K. M., & Weisz, J. R. (2003). Child, parent, and therapist (dis)agreement on target problems in outpatient therapy: The therapist's dilemma and its implications. Journal of Consulting and Clinical Psychology, 71, 62–70.
Hayes, A. F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76, 408–420.
Henderson, C. E., Dakof, G. A., Greenbaum, P. E., & Liddle, H. A. (2010). Effectiveness of multidimensional family therapy with higher severity substance-abusing adolescents: Report from two randomized controlled trials. Journal of Consulting and Clinical Psychology, 78, 885–897.
Henderson, C. E., Rowe, C. L., Dakof, G. A., Hawes, S. W., & Liddle, H. A. (2009). Parenting practices as mediators of treatment effects in an early-intervention trial of multidimensional family therapy. American Journal of Drug and Alcohol Abuse, 35, 220–226.
Henggeler, S. W., & Borduin, C. M. (1992). Mutiltisystemic therapy adherence scales. Unpublished instrument. Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina.
Henggeler, S. W., Borduin, C. M., Schoenwald, S. K., Huey, S. J., & Chapman, J. E. (2006). MST therapist adherence measure–Revised (TAM–R). Charleston: Medical University of South Carolina, Family Services Research Center.
Henggeler, S. W., Letourneau, E. J., Chapman, J. E., Borduin, C. M., Schewe, P. A., & McCart, M. R. (2009). Mediators of change for multisystemic therapy with juvenile sexual offenders. Journal of Consulting and Clinical Psychology, 77, 451–462.
Henggeler, S. W., & Schaeffer, C. (2010). Treating serious antisocial behavior using Multisystemic Therapy. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 259–276). New York, NY: Guilford Press.
Henggeler, S. W., Schoenwald, S. K., Borduin, C. M., Rowland, M. D., & Cunningham, P. B. (1998). Multisystemic treatment of antisocial behavior in children and adolescents. New York, NY: Guilford Press.
Holmbeck, G. N. (1997). Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology, 65, 599–610.
Hinshaw, S. P. (2007). Moderators and mediators of treatment outcome for youth outcome for youth with ADHD: Understanding for whom and how interventions work. Journal of Pediatric Psychology, 32, 664–675.
Hinshaw, S. P., Owens, E. B., Wells, K. C., Kraemer, H. C., Abikoff, H. B., Arnold, L. E.,…Wigal, T. (2000). Family processes and treatment outcome in the MTA: Negative/ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child Psychology, 28, 555–568.
Hollon, S., & Kendall, P. (1980). Cognitive self-statements in depression: Development of an automatic thoughts questionnaire. Cognitive Therapy and Research, 4, 383–397.
Hooley, J. M. (2007). Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology, 3, 329–352.
Hooley, J. M., & Parker, H. A. (2006). Measuring expressed emotion: An evaluation of the shortcuts. Journal of Family Psychology, 20, 386–396.
Hooley, J. M., & Teasdale, J. D. (1989). Predictors of relapse in unipolar depressives: Expressed emotion, marital distress, and perceived criticism. Journal of Abnormal Psychology, 98, 229–235.
Horvath, A. O., Del Re, A. C., Flückiger, C., & Symonds, D. (2011). Alliance in individual therapy. Psychotherapy, 48, 9–16.
Huey, S. J. Jr., Henggeler, S. W., Brondino, M. J., & Pickrel, S. G. (2000). Mechanisms of change in multisystemic therapy: Reducing delinquent behavior through therapist adherence and improved family and peer functioning. Journal of Consulting and Clinical Psychology, 68, 451–467.
Huey, S. J. Jr., & Polo, A. J. (2008). Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology, 37, 262–301.
Huey, W. C., & Rank, R. C. (1984). Effects of counselor and peer-led group assertive training on black-adolescent aggression. Journal of Counseling Psychology, 31, 95–98.
Hukkanen, R., Souranger, A., & Bergroth, L. (2003). Suicidal ideation and behavior in children's homes. Nordic Journal of Psychiatry, 57, 131–137.
Israel, P., Thomsen, P. H., Langeveld, J. H., & Stormark, K. M. (2007). Parent–youth discrepancy in the assessment and treatment of youth in usual clinical care setting: Consequences to parent involvement. European Child & Adolescent Psychiatry, 16, 138–148.
Jaycox, L., Reivich, K., Gillham, J. E. & Seligman, M. E. P. (1994). Prevention of depressive symptoms in school children. Behavioral Research and Therapy, 32, 801–816.
James, A. A. C. J., Soler, A., & Weatherall, R. R. W. (2005). Cognitive behavioural therapy for anxiety disorder in children and adolescents. Cochrane Database of Systematic Reviews, (4). doi: 10.1002/14651858.CD004690.pub2.
Jones, M. C. (1924a). A laboratory study of fear: The case of Peter. Pedagogical Seminary, 31, 308–315.
Jones, M. C. (1924b). The elimination of children's fears. Journal of Experimental Psychology, 7, 382–390.
Jordans, M. J. D., Komproe, I. H., Tol, W. A., Kohrt, B. A., Luitel, N. P., Macy, R. D., & De Jong, J. T. V. M. (2010). Evaluation of a classroom-based psychosocial intervention in conflict-afflicted Nepal: A cluster randomized controlled trial. Journal of Child Psychology and Psychiatry, 51, 818–826.
Kahn, J., Kehle, T., Jenson, W., & Clark, E. (1990). Comparison of cognitive-behavioral, relaxation, and self-modeling interventions for depression among middle-school students. School Psychology Review, 19, 196–211.
Kaminer, Y., Burleson, J. A., & Burke, R. (2008). Efficacy of outpatient aftercare for adolescents with alcohol use disorders: A randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 1405–1412.
Kaminer, Y., Burleson, J. A., & Goldberger, R. (2002). Cognitive behavioral coping skills and psychoeducation therapies for adolescent substance abuse. Journal of Nervous and Mental Disease, 190, 737–745.
Karver, M. S., Handelsman, J. B., Fields, S., & Bickman, L. (2005). A theoretical model of common process factors in youth and family therapy. Mental Health Services Research, 7, 35–51.
Karver, M. S., Handelsman, J. B., Fields, S., & Bickman, L. (2006). Meta-analysis of therapeutic relationship variables in youth and family therapy: The evidence for different relationship variables in the child and adolescent treatment outcome literature. Clinical Psychology Review, 26, 50–65.
Kataoka, S. H., Stein, B. D., Jaycox, L. H., Wong, M., Escudero, P., Tu, W.,…Fink, A. (2003). A school-based mental health program for traumatized Latino immigrant children. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 311–318.
Kaufman, N. K., Rohde, P., Seeley, J. R., Clarke, G. N., & Stice, E. (2005). Potential mediators of cognitive-behavioral therapy for adolescents with co-morbid major depression and conduct disorder. Journal of Consulting and Clinical Psychology, 73, 38–46.
Kazdin, A. E. (2000). Psychotherapy for children and adolescents: Directions for research and practice. New York, NY: Oxford University Press.
Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27.
Kazdin, A. E. (2010). Problem-solving skills training and parent management training for oppositional defiant disorder and conduct disorder. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 211–226). New York, NY: Guilford Press.
Kazdin, A. E. (2011). Single-case research designs: Methods for clinical and applied settings. Oxford, United Kingdom: Oxford University Press.
Kazdin, A. E., Bass, D., Ayers, W. A., & Rodgers, A. (1990). Empirical and clinical focus of child and adolescent psychotherapy research. Journal of Consulting & Clinical Psychology, 58, 729–740.
Kazdin, A. E., & Weisz, J. R. (1998). Identifying and developing empirically supported child and adolescent treatments. Journal of Consulting and Clinical Psychology, 66, 19–36.
Kazdin, A. E., & Whitley, M. K. (2003). Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. Journal of Consulting & Clinical Psychology, 71, 504–515.
Kazdin, A. E., Whitley, M., & Marciano, P. L. (2006). Child–therapist and parent–therapist alliance and therapeutic change in the treatment of children referred for oppositional, aggressive, and antisocial behavior. Journal of Child Psychology and Psychiatry, 47, 436–445.
Keel, P. K., & Haedt, A. (2008). Evidence-based psychosocial treatments for eating problems and eating disorders. Journal of Child and Adolescent Clinical Psychology, 37, 39–61.
Kendall, P. C., & Hedtke, K. (2006). Cognitive-behavioral therapy for anxious children: Therapist manual (3rd ed.). Ardmore, PA: Workbook. Available from http://workbookpublishing.com
Kendall, P. C., & Khanna, M. S. (2008). Camp cope-a-lot: The coping cat DVD [DVD]. Ardmore, PA: Workbook. Available from http://workbookpublishing.com
Kendall, P. C., Khanna, M. S., Edson, A., Cummings, C., & Harris, M. S. (2011). Computers and psychosocial treatment for child anxiety: Recent advances and ongoing efforts. Depression and Anxiety, 28, 58–66.
Kendall, P. C., & Treadwell, K. H. (2007). The role of self-statements as a mediator in treatment for youth with anxiety disorders. Journal of Consulting and Clinical Psychology, 75, 380–389.
Koegel, R. L., Koegel, L. K., Vernon, T. W., & Brookman-Frazee, L. I. (2010). Empirically supported pivotal response treatment for children with autism spectrum disorders. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 327–344). New York, NY: Guilford Press.
Kraemer, H. C., Wilson, G. T., Fairburn, C. G., & Agras, W. S. (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883.
Lambert, M. J., Whipple, J. L., Vermeersch, D. A., Smart, D. W., Hawkins, E. J., Nielsen, S. L. & Goates, M. (2002). Enhancing psychotherapy outcomes via providing feedback on client progress: A replication. Clinical Psychology & Psychotherapy, 9, 91–103.
Lau, W.-Y., Chan, C. K.-Y., Li, J. C.-H., & Au, T. K.-F. (2010). Effectiveness of group cognitive-behavioral treatment for childhood anxiety in community clinics. Behaviour Research and Therapy, 48, 1067–1077.
Layne, C. M., Saltzman, W. R., Poppleton, L., Burlingame, G. M., Pasalic, A., Durakovic, E.,…Pynoos, R. S. (2008). Effectiveness of a school-based group psychotherapy program for war-exposed adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 1048–1062.
Le Grange, D., Lock, J., Agras, W. S., Moye, A., Bryson, S. W., Jo, B., & Kraemer, H. C. (2012). Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behaviour Research and Therapy, 50, 85–92.
Leve, L. D., & Chamberlain, P. (2007). A randomized evaluation of multidimensional treatment foster care: Effects on school attendance and homework completion in juvenile justice girls. Research on Social Work Practice, 17, 657–663.
Levitt, E. E. (1957). The results of psychotherapy with children: An evaluation. Journal of Consulting Psychology, 21, 189–196.
Levitt, E. E. (1963). Psychotherapy with children: A further evaluation. Behaviour Research and Therapy, 60, 326–329.
Lewis, C. C., Simons, A. D., Silva, S. G., Rohde, P., Small, D. M., Murakami, J. L.,…March, J. S. (2009). The role of readiness to change in response to treatment of adolescent depression. Journal of Consulting and Clinical Psychology, 77, 422–428.
Lochman, J. E., Boxmeyer, C. L., Powell, N. P., Barry, T. D., & Pardini, D. A. (2010). Anger control training for aggressive youth. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 227–242). New York, NY: Guilford Press.
Lochman, J. E., & Wells, K. C. (2002). Contextual social-cognitive mediators and child outcome: A test of the theoretical model in the coping power program. Development and Psychopathology, 14, 971–993.
Lock, J., Agras, W. S., Bryson, S., & Kraemer, H. (2005). A comparison of short- and long-term family therapy for adolescent anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 632–639.
Lock, J., Le Grange, D., Agras, W. S., & Dare, C. (2001). A treatment manual for anorexia nervosa: A family-based approach. New York, NY: Guilford Press.
Lonigan, C. J., Elbert, J. C., & Johnson, S. B. (1998). Empirically supported psychosocial interventions for children: An overview. Journal of Clinical Child Psychology, 27, 138–145.
Lovaas, O. I. (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology, 55, 3–9.
Lundahl, B., Risser, H. J., & Lovejoy, M. C. (2006). A meta-analysis of parent training: Moderators and follow-up effects. Clinical Psychology Review, 26, 86–104.
Lustig, S. L., Kia-Keating, M., Knight, W. G., Geltman, P., Ellis, H., Kinzie, J.D.,…Saxe, G.N. (2004). Review of child and adolescent refugee mental health. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 24–36.
MacKinnon, D. P., Fairchild, A. J., & Fritz, M. S. (2007). Mediation analysis. Annual Review of Psychology, 58, 593–614.
MacKinnon, D. P., Fritz, M. S., Williams, J., & Lockwood, C. M. (2007). Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods, 39, 348–389.
Magana, A. B., Goldstein, M. J., Karno, M., Miklowitz, D. J., Jenkins, J., & Falloon, R. H. (1986). A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Research, 17, 203–212.
Makrygianni, M. K., & Reed, P. (2010). A meta-analytic review of the effectiveness of behavioural early intervention programs for children with autistic spectrum disorders. Research in Autism Spectrum Disorders, 4, 577–593.
March, J. S., Franklin, M. E., Leonard, H., Garcia, A., Moore, P., Freeman, J., & Foa, E. (2007). Tics moderate treatment outcome with sertraline but not cognitive–behavior therapy in pediatric obsessive-compulsive disorder. Biological Psychiatry, 61, 344–347.
Mathur, S. R., Kavale, K. A., Quinn, M. M., Forness, S. R., & Rutherford, R. B. Jr. (1998). Social skills interventions with students with emotional and behavioral problems: A quantitative synthesis of single-subject research. Behavioral Disorders, 23, 193–201.
McCabe, K. M., Lansing, A. E., Garland, A., & Hough, R. (2002). Gender differences in psychopathology, functional impairment, and familial risk factors among adjudicated delinquents. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 1221–1229.
McCarty, C. A., & Weisz, J. R. (2002). Correlates of expressed emotion in mothers of clinically-referred youth: An examination of the five-minute speech sample. Journal of Child Psychology and Psychiatry, 43, 759–768.
McGrath, M. L., Dorsett, P. G., Calhoun, M. E., & Drabman, R. S. (1987). “Beat-the-buzzer”: A method for decreasing parent–child morning conflicts. Child and Family Behavior Therapy, 9(3–4), 35–48.
McLeod, B. D. (2011). Relation of the alliance with outcomes in youth psychotherapy: A meta-analysis. Clinical Psychology Review, 31, 603–616.
McLeod, B. D., & Weisz, J. R. (2005). The therapy process observational coding system—Alliance scale: Measure characteristics and prediction of outcome in usual clinical practice. Journal of Consulting and Clinical Psychology, 73, 323–333.
McLeod, B. D., & Weisz, J. R. (2010). Therapy process observational coding system for child psychotherapy strategies scale. Journal of Clinical Child and Adolescent Psychology, 39, 436–443.
McMahon, R. J., & Forehand, R. (2003). Helping the noncompliant child: Family based treatment for oppositional behavior (2nd ed.). New York, NY: Guilford Press.
Meichenbaum, D., & Goodman, S. (1971). Training impulsive children to talk to themselves: A means of developing self-control. Journal of Abnormal Psychology, 77, 115–126.
Merry, S. N., Stasiak, K., Shepherd, M., Frampton, C., Fleming, T., & Lucassen, M. F. G. (2012). The effectiveness of SPARX, a computerized self help intervention for adolescents seeking help for depression: randomized controlled non-inferiority trial. British Medical Journal, 344, 1–16. doi: 10.1136/bmj.e2598
Mihalic, S., Fagan, A., Irwin, K., Ballard, D., & Elliott, D. (2002). Blueprints for violence prevention replications: Factors for implementation success. Boulder, CO: Center for the Study and Prevention of Violence.
MTA Cooperative Group. (1999a). A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 56, 1073–1086.
MTA Cooperative Group. (1999b). Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 56, 1088–1096.
Mufson, L. H., Weissman, M. M., Moreau, D., & Garfinkel, R. (1999). Efficacy of interpersonal therapy for depressed adolescents. Archives of General Psychiatry, 56, 573–579.
Muller, D., Judd, C. M., & Yzerbyt, V. Y. (2005). When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology, 89, 852–863.
National Evaluation and Technical Assistance Center. (2010). Fact sheet: Juvenile justice facilities. Washington, DC: NETAC.
Nock, M. K., & Kazdin, A. E. (2005). Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting & Clinical Psychology, 73, 872–879.
Office of the Surgeon General. (1999). Mental health: A report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services.
Office of the Surgeon General. (2004). Report of the surgeon general's conferences on children's mental health: A national action agenda. Rockville, MD: U.S. Department of Health and Human Services.
Ougrin, D., & Latif, S. (2011). Specific psychological treatment versus treatment as usual in adolescents with self-harm: Systematic review and meta-analysis. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 32, 74–80.
Palinkas, L. A., Aarons, G. A., Hoagwood, K. E., Chorpita, B. F., Landsverk, J., Weisz, J. R., & the Research Network on Youth Mental Health. (2008). An ethnographic study of implementation of evidence-based practice in child mental health: First steps. Psychiatric Services, 59, 738–746.
Pelham, W. E., & Fabiano, G. A. (2008). Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology, 37, 184–214.
Pelham, W. E., Gnagy, E. M., Greiner, A. R., Waschbusch, D. A., Fabiano, G. A., & Burrows-MacLean, L. (2010). Summer treatment programs for attention-deficit/hyperactivity disorder. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 277–292). New York, NY: Guilford Press.
Perepletchikova, F., Treat, T. A., & Kazdin, A. E. (2007). Treatment integrity in psychotherapy research: analysis of the studies and examination of the associated factors. Journal of Consulting and Clinical Psychology, 75, 829–841.
Peris, T. S., & Baker, B. L. (2000). Applications of the expressed emotion construct to young children with externalizing behavior: Stability and prediction over time. Journal of Child Psychology and Psychiatry, 41, 457–462.
Pollard, K., & Mather, M. (2009). U.S. Hispanic and Asian population growth levels off. Retrieved from the Population Reference Bureau website, www.prb.org/Articles/2009/hispanicasiall.aspx.
Preacher, K. J., & Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers, 36, 717–731.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891
Preacher, K. J., Rucker, D. D., & Hayes, A. F. (2007). Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behavioral Research, 42, 185–227.
President's New Freedom Commission on Mental Health. (2003). Achieving the promise: Transforming mental health care in America. Final Report. DHHS Pub. No. SMA-03–3832: Rockville, MD.
Richters, J. E. (1992). Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin, 112, 485–499.
Rogers, S. J., & Vismara, L. A. (2008). Evidence-based comprehensive treatments for early autism. Journal of Child and Adolescent Clinical Psychology, 37, 8–38.
Rozenman, M., Weersing, V. R., & Amir, N. (2011). A case series of attention modification in clinically anxious youths. Behaviour Research and Therapy, 49, 324–330.
Sanders, M. R., & Murphy-Brennan, M. (2010). The international dissemination of the triple P— Positive parenting program. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 519–537). New York, NY: Guilford Press.
Sburlati, E. S., Schniering, C. A., Lyneham, H. J., & Rapee, R. M. (2011). A model of therapist competencies for the empirically supported cognitive behavior treatment of child and adolescent anxiety and depressive disorders. Clinical Child and Family Psychology Review, 14, 89–109.
Schoenwald, S. K. (2010). From policy pinball to purposeful partnership: The policy contexts of Multisystemic Therapy transport and dissemination. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 538–553). New York, NY: Guilford Press.
Schoenwald, S. K., Chapman, J. E., Sheidow, A. J., & Carter, R. E. (2009). Long-term youth criminal outcomes in MST transport: The impact of therapist adherence and organizational climate and structure. Journal of Clinical Child & Adolescent Psychology, 38, 91–105.
Schoenwald, S. K., Garland, A. F., Chapman, J. E., Frazier, S. L., Sheidow, A. J., & Southam-Gerow, M. A. (2011). Toward the effective and efficient measurement of implementation fidelity. Administration and Policy in Mental Health and Mental Health Services Research, 38, 32–43.
Schoenwald, S. K., Henggeler, S. W., Brondino, M. J., & Rowland, M. D. (2000). Multisystemic therapy: monitoring treatment fidelity. Family Process, 39, 83–103.
Schoenwald, S. K., Kelleher, K., Weisz, J. R., & the Research Network on Youth Mental Health. (2008). Building bridges to evidence-based practice: The MacArthur foundation child system and treatment enhancement projects (Child STEPs). Administration and Policy in Mental Health and Mental Health Services Research, 35, 66–72.
Sexton, T. L. (2010). Functional family therapy in clinical practice: An evidence-based treatment model for working with troubled adolescents. New York, NY: Routledge.
Shaffer, D., Fisher, P., Dulcan, M., Davies, M., Piacentini, J., Schwab-Stone, M. E.,…Regier, D. A. (1996). The NIMG diagnostic interview schedule for children version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 865–877.
Shapiro, D. A., & Shapiro, D. (1982). Meta-analysis of comparative therapy outcome studies: A replication and refinement. Psychological Bulletin, 92, 581–604.
Shaw, J. A. (2003). Children exposed to war/terrorism. Clinical Child and Family Psychology Review, 6, 237–246.
Sheeringa, M. S., Weems, C. F., Cohen, J. A., Amaya-Jackson, L., & Guthrie, D. (2011). Trauma-focused cognitive behavioral therapy for posttraumatic stress disorder in three-through six year-old children: A randomized trial. Journal of Child Psychology and Psychiatry, 52, 853–860.
Sherer, M. R., & Schreibman, L. (2005). Individual behavioral profiles and predictors of treatment effectiveness for children with autism. Journal of Consulting and Clinical Psychology, 73, 525–538.
Shimokawa, K., Lambert, M. J., & Smart, D. W. (2010). Enhancing treatment outcome of patients at risk of treatment failure: Meta-analytic and mega-analytic review of a psychotherapy quality assurance system. Journal of Consulting and Clinical Psychology, 78, 298–311.
Shirk, S. R., & Karver, M. (2003). Prediction of treatment outcome from relationship variables in child and adolescent therapy: A meta-analytic review. Journal of Consulting and Clinical Psychology, 71, 452–464.
Silverman, W. K., & Hinshaw, S. P. (2008). The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal of Child and Adolescent Clinical Psychology, 37, 1–7.
Silverman, W. K., Ortiz, C. D., Viswesvaran, C., Burns, B. J., Kolko, D. J., Putman, F. W., & Amaya-Jackson, L. (2008a). Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Child and Adolescent Clinical Psychology, 37, 156–183.
Silverman, W. K., Pina, A. A., & Viswesvaran, C. (2008b). Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Child and Adolescent Clinical Psychology, 37, 105–130.
Smith, T. (2010). Early and intensive behavioral intervention in autism. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 312–326). New York, NY: Guilford Press.
Smith, D. K., & Chamberlain, P. (2010). Multidimensional treatment foster care for adolescents: Processes and outcomes. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 243–258). New York, NY: Guilford Press.
Smith, M. L., & Glass, G. V. (1977). Meta-analysis of psychotherapy outcome studies. American Psychologist, 32, 752–760.
Snyder, H. N., & Sickmund, M. (2006). Juvenile offenders and victims: 2006 national report. Pittsburgh, PA: National Center for Juvenile Justice.
Southam-Gerow, M. A., Weisz, J. R., Chu, B. C., McLeod, B. D., Gordis, E. B., & Connor-Smith, J. K. (2010). Does CBT for youth anxiety outperform usual care in community clinics? An initial effectiveness test. Journal of the American Academy of Child & Adolescent Psychiatry, 49, 1043–1052.
Southam-Gerow, M. A., Weisz, J. R., & Kendall, P. C. (2003). Youth with anxiety disorders in research and service clinics: Examining client differences and similarities. Journal of Clinical Child and Adolescent Psychology, 32, 375–385.
Spielmans, G. I., Gatlin, E. T., & McFall, J. P. (2010). The efficacy of evidence-based psychotherapies versus usual care for youths: Controlling confounds in a meta-reanalysis. Psychotherapy Research, 20, 234–246.
Stagman, S., & Cooper, J. L. (2010). Children's mental health: What every policymaker should know. New York, NY: National Center for Children in Poverty, Columbia University Mailman School of Public Health.
Stein, B. D., Jaycox, L. H., Kataoka, S. H., Wong, M., Tu, W., Elliott, M. N., & Fink, A. (2003). A mental health intervention for schoolchildren exposed to violence. Journal of the American Medical Association, 290, 603–611.
Stein, B. D., Kogan, J. N., Hutchison, S. L., Magee, E. A., & Sorbero, M. J. (2010). Use of outcomes information in child mental health treatment: Results from a pilot study. Psychiatric Services, 61, 1211–1216.
Stice, E., Rohde, P., Seeley, J. R., & Gau, J. M. (2010). Testing mediators of intervention effects in randomized controlled trials: An evaluation of three depression prevention programs. Journal of Consulting and Clinical Psychology, 78, 273–280.
Strupp, H. H., & Anderson, T. (1997). On the limitations of therapy manuals. Clinical Psychology: Science and Practice, 4, 76–82.
Sue, S. (2003). In defense of cultural competency in psychotherapy and treatment. American Psychologist, 58, 964–970.
Sue, S., Fujino, D. C., Hu, L.T., Takeuchi, D. T., & Zane, N. W. S. (1991). Community mental health services for ethnic minority groups: A test of the cultural responsiveness hypothesis. Journal of Consulting & Clinical Psychology, 59, 533–540.
Swenson, C. C., Schaeffer, C. M., Henggeler, S. W., Faldowski, R., & Mayhew, A. M. (2010). Multisystemic Therapy for Child Abuse and Neglect: A randomized effectiveness trial. Journal of Family Psychology, 24, 497–507.
Tarnowski, K. J., Rosén, L. A., McGrath, M. L., & Drabman, R. S. (1987). A modified habit reversal procedure in a recalcitrant case of trichotillomania. Journal of Behavior Therapy and Experimental Psychiatry, 18, 157–163.
Teplin, L. A., Abram, K. M., McClelland, G. M., Mericle, A. A., Dulcan, M. K., & Washburn, J. J. (2006). Psychiatric disorders of youth in detention. Washington, DC: U.S. Department of Justice.
Tol, W. A., Komproe, I. H., Susanty, D., Jordans, M. J. D., & de Jong, J. T. V. M. (2008). School-based mental health intervention for children affected by political violence in Indonesia: A cluster randomized trial. Journal of the American Medical Association, 300, 655–662.
Treadwell, K. H., & Kendall, P. C. (1996). Self-talk in youth with anxiety disorders: States of mind, content specificity. Journal of Consulting and Clinical Psychology, 64, 941–950.
UNICEF. (1996). The state of the world's children. New York, NY: Oxford University Press.
U.S. Department of Health and Human Services. (2001). Mental health: Culture, race, and ethnicity–A supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General.
Waldron, H. B., & Kaminer, Y. (2004). On the learning curve: The emerging evidence supporting cognitive-behavioral therapies for adolescent substance abuse. Addiction, 99(Suppl. 2), 93–105.
Waldron, H. B., & Turner, C. W. (2008). Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Child and Adolescent Clinical Psychology, 37, 238–261.
Waltz, J., Addis, M. E., Koerner, K. & Jacobson, N. S. (1993). Testing the integrity of a psychotherapy protocol: Assessment of adherence and competence. Journal of Consulting and Clinical Psychology, 61, 620–630.
Watanabe, N., Hunot, V., Omori, I. M., Churchill, R., & Furukawa, T. A. (2007). Psychotherapy for depression among children and adolescents: A systematic review. Acta Psychiatrica Scandinavica, 116, 84–95.
Webster-Stratton, C. & Reid, M. J. (2010). The incredible years parents, teachers, and children's training series: A multifaceted treatment approach for young children with conduct problems. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 194–210). New York, NY: Guilford Press.
Weersing, V. R., & Weisz, J. R. (2002a). Community clinic treatment of depressed youth: Benchmarking usual care against CBT clinical trials. Journal of Consulting and Clinical Psychology, 70, 299–310.
Weersing, V. R., & Weisz, J. R. (2002b). Mechanisms of action in youth psychotherapy. Journal of Child Psychology and Psychiatry, 43, 3–29.
Weersing, V. R., Weisz, J. R., & Donenberg, G. R. (2002). Development of the therapy procedures checklist: A therapist-report measure of technique use in child and adolescent treatment. Journal of Clinical Child and Adolescent Psychology, 31, 168–180.
Weissman, A. (1979). The dysfunctional attitude scale: A validation study (Doctoral dissertation, University of Pennsylvania, 1979). Dissertation Abstracts International, 40, 1389–1390b.
Weisz, J. R. (2004). Psychotherapy for children and adolescents: Evidence-based treatments and case examples. Cambridge, United Kingdom: Cambridge University Press.
Weisz, J. R., & Addis, M. E. (2006). The research–practice tango and other choreographic challenges: Using and testing evidence-based psychotherapies in clinical care settings. In C. D. Goodheart, A. E. Kazdin, & R. J. Sternberg (Eds.), Evidence-based psychotherapy: Where practice and research meet (pp. 179–206). Washington, DC: American Psychological Association.
Weisz, J. R., & Chorpita, B. F. (2011). Mod squad for youth psychotherapy: Restructuring evidence-based treatment for clinical practice. In P.C. Kendall (Ed.), Child and adolescent therapy: Cognitive-behavioral procedures (4th ed., pp. 379–397). New York, NY: Guilford Press.
Weisz, J. R., Chorpita, B. F., Frye, A., Ng, M. Y., Lau, N., Bearman, S. K.,…the Research Network on Youth Mental Health (2011a). Youth top problems: Using idiographic, consumer-guided assessment to identify treatment needs and track change during psychotherapy. Journal of Consulting and Clinical Psychology, 79, 369–380.
Weisz, J. R., Chorpita, B. F., Palinkas, L. A., Schoenwald, S. K., Miranda, J., Bearman, S. K.,…the Research Network on Youth Mental Health. (2012a). Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry, 69, 274–282.
Weisz, J. R., & Gray, J. S. (2008). Evidence-based psychotherapies for children and adolescents: Data from the present and a model for the future. Child and Adolescent Mental Health, 13, 54–65.
Weisz, J. R., Huey, S. J., & Weersing, V. R. (1998). Psychotherapy outcome research with children and adolescents: The state of the art. Advances in Clinical Child Psychology, 20, 49–91.
Weisz, J. R., Jensen-Doss, A. J., & Hawley, K. M. (2005). Youth psychotherapy outcome research: A review and critique of the evidence base. Annual Review of Psychology, 56, 337–363.
Weisz, J. R., Jensen-Doss, A., & Hawley, K. M. (2006). Evidence-based youth psychotherapies versus usual clinical care: A meta-analysis of direct comparisons. American Psychologist, 61, 671–689.
Weisz, J. R., Jensen, A. L., & McLeod, B. D. (2005b). Milestones and methods in the development and dissemination of child and adolescent psychotherapies: Review, commentary, and a new deployment-focused model. In E. D. Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (2nd ed., pp. 9–39). Washington, DC: American Psychological Association.
Weisz, J. R., & Kazdin, A. E. (Eds.). (2010). Evidence-based psychotherapies for children and adolescents (2nd ed.). New York, NY: Guilford Press.
Weisz, J. R., Kuppens, S., Eckshtain, D., Ugueto, A. M., Hawley, K. M., & Jensen-Doss, A. (2012b). Do evidence-based youth psychotherapies outperform usual care? A multilevel meta-analysis. Submitted for publication.
Weisz, J. R., McCarty, C. A., Eastman, K. L., Suwanlert, S., & Chaiyasit, W. (1997). Developmental psychopathology and culture: Ten lessons from Thailand. In S. S. Luthar, J. Burack, D. Cicchetti, & J. R. Weisz (Eds.), Developmental psychopathology: Perspectives on adjustment, risk, and disorder (pp. 568–592). Cambridge, United Kingdom: Cambridge University Press.
Weisz, J. R., McCarty, C. A., & Valeri, S. M. (2006b). Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin, 132, 132–149.
Weisz, J. R., Sandler, I. N., Durlak, J. A., & Anton, B. S. (2005c). Promoting and protecting youth mental health through evidence-based prevention and treatment. American Psychologist, 60, 628–648.
Weisz, J. R., Southam-Gerow, M. A., Gordis, E. B., Connor-Smith, J. K., Chu, B. C., Langer, D. A.,…Weiss, B. (2009). Cognitive-behavioral therapy versus usual clinical care for youth depression: An initial test of transportability to community clinics and clinicians. Journal of Consulting and Clinical Psychology, 77, 383–396.
Weisz, J. R., Ugueto, A. M., Herren, J., Afienko, S. R., & Rutt, C. (2011b). Kernels vs. ears, and other questions for a science of treatment dissemination. Clinical Psychology: Science and Practice, 18, 41–46.
Weisz, J. R., & Weiss, B. (1991). Studying the “referability” of child clinical problems. Journal of Consulting and Clinical Psychology, 59, 266–273.
Weisz, J. R., Weiss, B., Alicke, M. D., & Klotz, M. L. (1987). Effectiveness of psychotherapy with children and adolescents: A meta-analysis for clinicians. Journal of Consulting & Clinical Psychology, 55, 542–549.
Weisz, J. R., Weiss, B., Han, S. S., Granger, D. A., & Morton, T. (1995). Effects of psychotherapy with children and adolescents revisited: A meta-analysis of treatment outcome studies. Psychological Bulletin, 117, 450–468.
Westen, D., Novotny, C. M., & Thompson-Brenner, H. (2004a). The empirical status of empirically supported therapies: Assumptions, findings, and reporting in controlled trials. Psychological Bulletin, 130, 631–663.
Westen, D., Novotny, C. M., & Thompson-Brenner, H. (2004b). The next generation of psychotherapy research: Reply to Ablon and Marci (2004), Goldfried and Eubanks-Carter (2004), and Haaga (2004). Psychological Bulletin, 130, 677–683
Woody, S. R., Weisz, J. R., & McLean, C. (2005). Empirically supported treatments: 10 years later. Clinical Psychologist, 58, 5–11.
Wurtele, S. K., & Drabman, R. S. (1984). “Beat the buzzer” for classroom dawdling: A one-year trial. Behavior Therapy, 15, 403–409.
Yeh, M., Eastman, K., & Cheung, M. K. (1994). Children and adolescents in community health centers: Does the ethnicity or the language of the therapist matter? Journal of Community Psychology, 22, 153–163.
Yeh, M., & Weisz, J. R. (2001). Why are we here at the clinic? Parent–child (dis)agreement on referral problems. Journal of Consulting and Clinical Psychology, 71, 62–70.
Yu, D. L., & Seligman, M. E. P. (2002). Preventing depressive symptoms in Chinese children. Prevention and Treatment, 5(1). Article 9, posted May 8, 2002.
Zisser, A., & Eyberg, S. M. (2010). Parent–child interaction therapy and the treatment of disruptive behavior disorders. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed., pp. 179–193). New York, NY: Guilford Press.