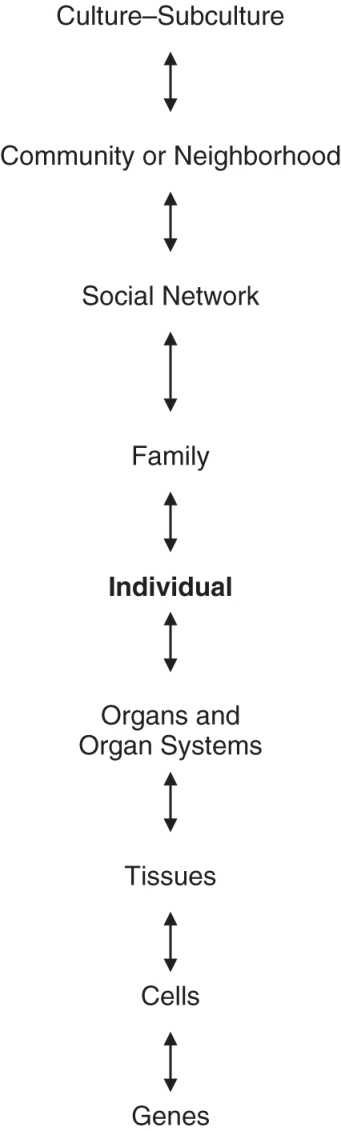
Figure 17.1 Systems hierarchy in the biopsychosocial model (based on Engel, 1977).
Since their formal beginnings in the 1970s, the related fields of behavioral medicine and health psychology have grown substantially and evolved. In many ways, their emergence was a necessary response to changing patterns of health. By the latter half of the 20th century, advances in public health and medicine (e.g., improved sanitation, hygiene, and nutrition; development of vaccines and antibiotics) had produced a dramatic reduction in morbidity and mortality from infectious disease in the United States and other industrialized nations, where previously they had been the leading causes of death. In these nations, infectious diseases were replaced by cardiovascular disease (e.g., coronary heart disease, stroke), cancer, chronic pulmonary disease, and diabetes as leading causes of death in adulthood.
These noncommunicable, chronic diseases differ from the previously predominant infectious diseases in several ways that involve major roles for behavioral science in biomedical research and health care (Fisher et al., 2011). Specific modifiable behaviors (e.g., smoking, high dietary intake of calories and fat, physical inactivity) strongly increase the risk for the initial development of these chronic conditions and influence their course, making behavioral processes key targets in prevention and treatment. Hence, the development of a scientific understanding of the determinants and modification of these behavioral risk factors has become a pressing priority. Also, these chronic diseases can have a profound impact on psychological and behavioral functioning or quality of life, broadly defined (e.g., emotional adjustment, social and vocational functioning, disability). As a result, management of these health outcomes and related effects of chronic disease (e.g., physical symptoms and distress) is an important component of efforts to reduce the burden of these conditions. Management of these consequences of chronic disease goes beyond biomedical treatments of the underlying physical condition, to include psychosocial approaches specifically targeting these emotional and behavioral outcomes, as adjuncts to traditional medical care. Finally, for several of these conditions, physiological effects of stress, negative emotion, and other psychosocial factors seem to play a direct role—independent of health behavior risk factors—in their development and course, creating a potential role for related psychological interventions in treatment of the underlying disease process.
The rapid expansion and evolution of health psychology and behavioral medicine is evident in the chapters on the topic appearing in prior versions of this handbook, and in the somewhat distinct focus of this, the fourth such chapter. Pomerleau and Rodin (1986) provided an overview of these still-emerging fields, focusing on areas of basic research (e.g., psychobiology of stress and disease) and applied research (e.g., adherence with medical regimens, coping with stressful medical procedures) that became important elements of the foundation of these fields. They also reviewed a smaller number of topics in emerging research on interventions (e.g., smoking cessation). Blanchard (1994) focused more specifically on intervention research, in which mostly individual and small group behavioral and cognitive-behavioral approaches targeted specific conditions (e.g., hypertension, chronic pain, insomnia) or risk factors for important diseases (e.g., obesity, smoking). This review provided clear evidence—from a rapidly growing number of increasingly methodologically rigorous intervention studies—that such treatments could produce clinically meaningful changes in risk factors, reduce the severity of several chronic medical conditions, and lessen their impact on functioning, making them useful additions to traditional approaches to medical care and prevention in many instances.
Creer, Holroyd, Glasgow, and Smith (2004) provided an updated review of many of these same intervention topics that included much additional evidence of clinically meaningful effects, but noted that the field had expanded so rapidly that a comprehensive review was no longer feasible. They also broadened their focus beyond the chronic diseases and conditions in industrialized nations to include more global or world health issues, such as the burden of infectious diseases (i.e., HIV, tuberculosis) in less developed nations. This global focus made clear that much of the potential impact of behavioral medicine and health psychology lies in their role in public health, policy, and various population-level interventions, as well as the more traditional individual and small group-level approaches.
In this chapter, after a brief overview of the conceptual foundations of these closely related fields we, too, provide a necessarily condensed and selective update of the empirical status of intervention research and applications in behavioral medicine and health psychology, focusing almost exclusively on adults. As a guide to a more thorough coverage of the field for interested readers, we cite qualitative and quantitative reviews of many specific topics. Consistent with the overall focus of the handbook, we primarily review intervention issues, covering other topics to the extent that they are needed to appreciate the current state and future directions of these fields. Although we heartily endorse the view of Creer and colleagues (2004) that health psychology and behavioral medicine have much to offer efforts to address the burdens of infectious illness in developing and less industrialized nations of the world, we focus primarily on intervention issues in the United States and other industrialized countries. However, it is important to note that 60% of deaths worldwide are due to noncommunicable chronic diseases, and 80% of those deaths occur in the developing world (Alwan et al., 2010). Hence, the issues we address are highly relevant in both industrialized and developing nations. Further, as we discuss in closing, in the coming years the health agendas in industrialized and developing nations are expected to converge further, and we discuss the implications of these trends for health psychology and behavioral medicine.
Given the primary focus of this handbook on services delivered to individuals and small groups, we emphasize similar approaches to the modification of health relevant behavior and the treatment or management of chronic disease, as opposed to more broadly focused large-group, population-level, policy, or public health intervention approaches. Hence, in a departure from prior editions of the handbook, our chapter title specifically refers to behavioral medicine and clinical health psychology, to designate our greater focus on the delivery of psychological services in medical settings and psychological consultation or collaboration with traditional health care providers. The rapidly evolving nature of medical care in the United States and other industrialized nations poses both major opportunities and daunting challenges for these central aspects of behavioral medicine and clinical health psychology.
However, just as the psychotherapy and behavior change research community has increasingly recognized the need to expand the portfolio of mental health services beyond traditional interventions for emotional distress and disorders delivered to individuals and small groups to include more population-based, preventive, and public health strategies (Kazdin & Blase, 2011), we also discuss the larger-group and population-based approaches that are a central focus in more broadly defined behavioral medicine and health psychology. These aspects of behavioral medicine and health psychology face an equally far-reaching set of opportunities and challenges. Indeed, these two trends in the field—refinement of individual and small group approaches and their integration into evolving models of medical care, and the development and dissemination of more large-group and population-focused strategies primarily addressing health behavior change—represent an evolving distinction within these fields. These two segments of behavioral medicine and health psychology involve different training requirements (e.g., traditional psychological approaches, transposed to health care settings and medical populations versus organizational, community, policy, and public health approaches to behavior change) and sets of likely collaborators (e.g., primary medical care providers and medical specialists versus health educators, practitioners in community and public health, policy makers).
The terms health psychology and behavioral medicine are sometimes distinguished quite carefully (Pomerleau & Rodin, 1986), and at other times are used interchangeably (Creer et al., 2004). Initially, the two fields were distinguished in part by a more explicit inclusion of biomedical science and clinical medicine within the description of behavioral medicine. Also, early in its emergence, behavioral medicine was more closely based in operant and classical learning theory approaches to psychological aspects of the development and management of disease (Pomerleau & Brady, 1979; Surwit, Williams, & Shapiro, 1982). That is, behavioral medicine was explicitly associated with behaviorism in early definitions, in part to distinguish it from the psychoanalytic perspective that had previously characterized one of its main historical predecessors—psychosomatic medicine. In contrast, health psychology reflected a broader array of conceptual perspectives on psychological processes, based in social, clinical, developmental, experimental, physiological, and personality psychology (Stone, Cohen, & Adler, 1979). Soon, behavioral medicine also came to include a greater variety of conceptual approaches and traditions regarding the behavioral, psychological, and social-environmental aspects of disease (Gentry, 1984), as did psychosomatic medicine (cf. Novak et al., 2007).
Currently, both behavioral medicine and health psychology involve the development and integration of behavioral, psychosocial, and biomedical research in an effort to understand health and illness, and the application of the resulting knowledge in efforts to prevent and treat physical illness. The distinction between health psychology and behavioral medicine now lies mostly in matters of professional identify and training, rather than their overall mission or conceptual orientation. Health psychology is conducted largely—but not exclusively—by psychologists, whereas behavioral medicine involves a greater variety of professionals, including psychologists, physicians, epidemiologists, sociologists, nurses, and others. In this way, behavioral medicine is the broader, more inclusive field, of which health psychology is a subfield. Clinical health psychology, in turn, is the subfield within health psychology that involves research and applied services regarding the prevention, management, and treatment of physical illness. Whereas health psychology broadly defined includes large-group and population-based approaches to prevention and health behavior change, clinical health psychology focuses more specifically on applications with individuals and small groups, often for those with well-established unhealthy behavior or existing physical illness or other medical conditions.
Both health psychology and behavioral medicine comprise three general, interrelated topics. Stress and disease—or psychosomatics—is perhaps the oldest, and concerns the direct psychobiological effects of stress, negative emotion, and related processes on the pathophysiology of disease. Within this topic, researchers examine the associations of psychosocial risk factors (e.g., social isolation, job stress, chronic anger, depression) with the development and course of disease (Everson-Rose & Clark, 2010). Other studies examine the physiological mechanisms (e.g., alterations in neuroendocrine, cardiovascular, or immune system responses) that link psychosocial inputs and disease outcomes (Lovallo, 2010). Animal studies of this topic manipulate levels of environmental stress in ways that are not possible with human participants to examine effects on disease processes and underlying physiological mechanisms (Nation, Schneiderman, & McCabe, 2010). Results of such efforts guide the development and evaluation of interventions that target stress, negative emotion, and related factors in order to alter the development and course of disease (Schneiderman, Antoni, Penedo, & Ironson, 2010).
The second major topic—health behavior and prevention—examines the association of daily habits (e.g., smoking, diet, physical activity) with the development and course of disease (Kaplan, 2010), as well as the determinants of these behaviors (Schwarzer, 2011). This information then guides the development, evaluation, and implementation of interventions intended to promote healthier lifestyles. The third topic—psychosocial aspects of medical illness and medical care—examines the impact of physical illness and related medical care on a variety of aspects of functioning, including emotional adjustment, physical distress, social and vocational roles, and general levels of functional activity versus disability (Stanton, Revenson, & Tennen, 2007). This general topic also includes behavioral aspects of medical treatment (e.g., adherence with medical regimens), and the process of health care utilization (e.g., patient-provider communication, seeking health services; Baldwin, Kellerman, & Christensen, 2010). Research in this third area guides the development, evaluation, and implementation of adjunctive psychological and behavioral treatments for medical conditions (Schneiderman et al., 2010).
These topics are clearly overlapping. For example, exercise may be prescribed for recovering heart patients not only because of its direct physiological effects in reducing the risk of recurrent coronary events, but also because exercise is sometimes useful both in managing the depressive symptoms that often accompany coronary disease and in helping the patients to return to work and prior levels of functional activity (Stein, 2012). Across all three topics, treatment research of various types tests the efficacy and effectiveness of the resulting interventions as potential additions to standard medical and surgical approaches to prevention and disease management (Oldenburg, Absetz, & Chan, 2010).
Since their inception, health psychology and behavioral medicine have been strongly tied to the biopsychosocial model (Suls, Luger, & Martin, 2010). Traditional medicine is based on the biomedical model of disease, in which biological processes are seen as providing a sufficient basis for understanding, treating, and preventing disease. The success of this model is readily apparent in dramatic improvements in health and advances in medical treatment over the last century. Yet, many authors over many decades have deemed the biomedical approach to be incomplete, given its neglect of the role of psychological, social, and cultural factors in disease etiology and medical treatment (Suls et al., 2010). As a response to these perceived limitations, Engel (1977) proposed the biopsychosocial model (see Figure 17.1). Rather than reducing disease to basic biological causes and focusing only on biologically based treatments, the biopsychosocial model describes health and illness as the result of reciprocal influences among hierarchically arranged levels of analysis (von Bertalanffy, 1968). These levels range from the lower or more basic levels of the traditional biomedical model (i.e., biochemical processes, genes, cells, tissues, and organ systems) to the level of the behaving individual and on to higher levels of interpersonal, social, and broader environmental and cultural levels. In traditional scientific approaches, each level of analysis is understood through its own models and methods. However, in the biopsychosocial framework, each system or level influences and is influenced by the adjacent levels. In this view, any specific disease process (e.g., atherosclerosis in the coronary arteries) cannot be fully understood through a given level of analysis (e.g., molecular biology of inflammation; tissue pathology). It also must be considered at the multiple levels above and below in the hierarchy.
Figure 17.1 Systems hierarchy in the biopsychosocial model (based on Engel, 1977).
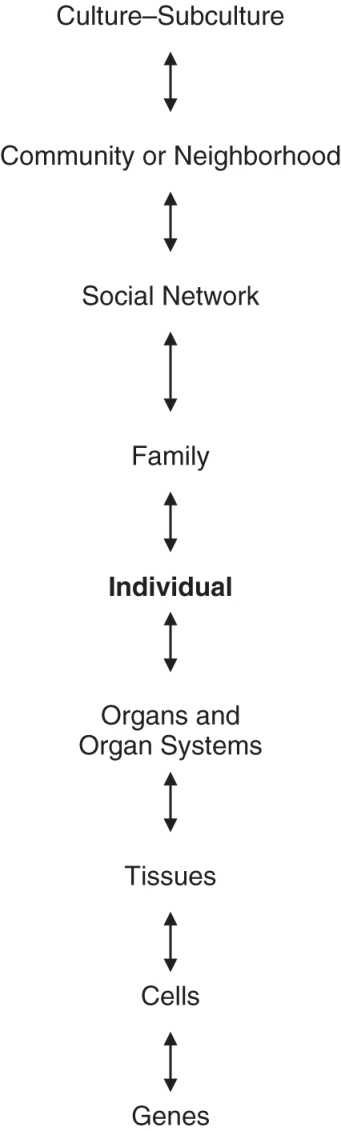
The implications for research, medical care, and the prevention of disease are clear. To understand the contributing factors for any given disease or medical condition, multilevel, integrative research is needed. Similarly, for an optimal approach to prevention, treatment, and management, opportunities at multiple levels must be explored. In discussing the applied implications of his model for clinical care, Engel (1980) suggested that “while the bench scientist can with relative impunity single out and isolate for sequential study components of an organized whole, the physician does so at the risk of neglect of, if not injury to, the object of study” (p. 536). Hence, the biopsychosocial model directs health care providers toward a multilevel, integrative approach to the evaluation and treatment of individual patients.
This framework also clearly suggests that regardless of whether they are biological or behavioral in focus, individual-based approaches to a given medical problem are incomplete; they should be augmented by broader social, organizational, community, and cultural level strategies for prevention and management. Leading causes of death (e.g., cardiovascular disease, cancer) will be best understood, prevented, and managed if each of these levels of analysis are considered and addressed. Although it is typically not feasible to address all levels of analysis in providing care to individual patients, a comprehensive medical, public health, and policy approach to the challenges posed by any given disease must consider the full range of levels of analysis. Consideration of these multiple levels also makes clear that a comprehensive, biopsychosocial model includes not only treatment of existing disease, but the prevention and reduction of disease risk well before its clinical onset.
As described previously, the behavioral perspective was the main psychological conceptual view during the formative years of behavioral medicine (Pomerleau & Brady, 1979; Surwit et al., 1982), and remains an important, but less dominant perspective today. Many interventions currently in use in the field are based on operant and classical learning models, both in prevention efforts and in the management of chronic illness and other medical problems. Paralleling trends in clinical psychology, behavioral medicine soon incorporated the cognitive-behavioral perspective (Wilson, 1980), most notably social learning theory (Bandura, 1977) and related perspectives emerging in the 1970s (Beck, 1976; Mahoney, 1977; Meichenbaum, 1977).
A major influence in all areas of health psychology and behavioral medicine has been the stress and coping model developed by Lazarus and his colleagues (Cohen & Lazarus, 1979; Lazarus, 1966; Lazarus & Folkman, 1984). Articulation of the role in stress of primary appraisal (i.e., judgments about potential for threat, harm, or loss) and secondary appraisal (i.e., judgments about opportunities for preventing or moderating the potential negative outcome) and emotion-focused coping (i.e., efforts to reduce the negative affect in response to stress) and problem-focused coping (i.e., efforts to reduce the demands of the stressor) produced a clear set of testable hypotheses and potential targets for interventions for stress-related problems. Given that stress plays a central role in all three of the major issues or topics in behavioral medicine and health psychology described previously (i.e., health behavior and prevention, stress and disease, psychosocial aspects of medical illness and medical care), this general perspective is a cornerstone in the foundation of these fields. The cognitive-behavioral perspective provided an important extension of the stress and coping paradigm, in describing an array of interventions easily adapted to focus on modification of the key concepts of appraisal and coping.
Personality characteristics are increasingly recognized as important influences on stress and disease, health behavior, and the impact of medical illness and aspects of medical care on emotional adjustment and functional activity (Smith, 2006a). For example, personality characteristics influence exposure to various sources of stress (e.g., interpersonal conflict), the magnitude of emotional and physiological stress responses, emotional and physiological recovery after stress exposure, and stress-related restorative processes (e.g., sleep quality; Williams, Smith, Gunn, & Uchino, 2011). Current theory and research in behavioral medicine and health psychology utilizes traditional trait approaches to personality, as well as social-cognitive and interpersonal perspectives to address these issues. Social psychological perspectives on individual behavior are also prominent, especially those perspectives that emphasize individuals' attitudes and beliefs about health relevant behavior (Kiviniemi & Rothman, 2010) and internal representations or “cognitive models” of the nature of specific medical conditions and related treatments (Leventhal, Breland, Mora, & Leventhal, 2010).
In each of the three main research topics in behavioral medicine and health psychology, social relationships are a central consideration. The availability and quality of personal relationships (i.e., social support and integration versus isolation) is an important predictor of the development and course of serious disease (Holt-Lunstad, Smith, & Layton, 2010; Lett et al., 2005), and a variety of psychobiological mechanisms have been identified as potentially underlying such associations (Uchino, 2006). The quality of marriage and similar close relationships is a similarly important influence on the development and course of disease (e.g., De Vogli, Chandola, & Marmot, 2007; Rohrbaugh, Shoham, & Coyne, 2006; Smith, Uchino, Berg, & Florsheim, 2012), and on adaptation to chronic medical conditions (Hagedoorn, Sanderman, Bolks, Tuinstra, & Coyne, 2008; Leonard, Cano, & Johansen, 2006). Couple-based interventions have been found to be useful in addressing a variety of behavioral risk reduction efforts and the management of several chronic diseases (Martire, Schulz, Helgeson, Small, & Saghafi, 2010; Shields, Finley, Chawla, & Meadows, 2012).
Broader features or levels of social context are an important component of the biopsychosocial model. For example, effective health behavior change programs have been developed for delivery in schools (Katz, 2009), worksites (Goetzel & Ozminkowski, 2008), and churches (Campbell et al., 2007). Characteristics of neighborhoods and the built environment (e.g., socioeconomic level, cohesion, safety, “walk-ability” and conduciveness to physical activity) have robust influences on health (Diez-Roux & Mair, 2010). Socioeconomic status (SES) has a strong, inverse relationship with the development and course of virtually all major causes of morbidity and mortality (Matthews & Gallo, 2010). Low SES is also associated with smaller declines in major causes of morbidity and mortality in recent years, due primarily to slower decreases in behavioral risks, less access to effective procedures for early detection, and less access to improved treatments (Byers, 2010). Public policy and environmental-level interventions (e.g., prohibition on smoking in public places) can clearly have effects on health behavior and the development and course of chronic disease (Brownson, Haire-Joshu, & Luke, 2006; Fisher et al., 2010). Hence, multiple levels of social—environmental context are the focus of current research and interventions in behavioral medicine and health psychology.
In recent years, behavioral medicine and health psychology have responded to the growing influence of the evidence based medicine movement (Spring et al., 2005), which calls for the development and use of a sound research base as a guide to medical care (Sackett, Rosenberg, Gray, Haynes, & Richardson, 1996). In this perspective, a hierarchy of evidence informs clinical practice, with randomized clinical trials (RCTs) and systematic reviews of multiple RCTs as the top two tiers of evidence. This has involved adopting accepted, rigorous standards for conducting and reporting both RCTs (Altman et al., 2001) and systematic reviews of literatures where multiple trials have been conducted (Higgins & Green, 2011). Many previous RCTs in behavioral medicine and health psychology had been designed, analyzed, and/or reported in ways that fell short of these commendable, more recent standards (Davidson et al., 2003; Davidson, Trudeau, Ockene, Orleans, & Kalpan, 2004; Spring, Pagato, Knatterud, Kozak, & Hedeker, 2007), as had many systematic reviews and meta-analyses (Coyne, Thombs, & Hagendoorn, 2010). As a result, the impact of much of the prior intervention research in the field has been reduced somewhat by this recent history of new and rising methodological standards. At the same time, issues surrounding appropriate endpoints or health outcomes for intervention research have been also been evolving in important ways.
In some cases, behavioral endpoints (e.g., smoking cessation, physical activity levels) have always been straightforward in intervention research, as have some intermediate biologic endpoints (e.g., weight loss, blood pressure reductions), although the methods used to measure the endpoints and draw conclusions about the clinical implications of observed treatment effects have been a matter of considerable discussion (Smith, 2011). However, because traditional medical research typically emphasizes objective indicators of disease-specific morbidity and mortality (i.e., evidence of myocardial infarction in ECG changes and cardiac enzyme elevations; survivorship in advanced cancer) in evaluating medical and surgical interventions, demonstrations of effects of behavioral interventions on these “hard” medical outcomes has been an important source of evidence in the field. Indeed, the field as a whole has periodically been criticized by traditional medical researchers for the lack of consistent effects of psychological intervention on these endpoints (Relman & Angell, 2002).
Although objectively assessed morbidity and mortality continue to be outcomes of paramount importance in intervention research, medical research and policy as a whole has expanded to emphasize a broader view of health outcomes. Specifically, emerging definitions of health include behavioral and subjective endpoints. Levels of functional activity versus disability, physical symptoms (e.g., pain, fatigue), emotional adjustment, and social functioning in personal relationships and vocational or academic roles have long been important outcomes in behavioral medicine and health psychology intervention research. But interest in these behavioral outcomes and subjective reports has been increasing in recent years in the biomedical and health care research community.
For example, in 2004 the National Institutes of Health established the Patient Reported Outcomes Measurement Information System (PROMIS; www.nihpromis.org), and expanded the program in 2010. The goal of this initiative is the development and dissemination of patient-reported measures of physical, mental, and social well-being. Traditional measurement issues (i.e., reliability, validity) are a major focus of current and planned PROMIS research, but the mission is broader. One goal is to develop measures that provide standardized, comparable information across a variety of domains and medical conditions. Flexibility in measurement use and applicability to a wide range of demographic groups is also a major focus. In this way the impact of a variety of medical conditions can be compared, as can variations in their impact across segments of the population. Importantly, standardized and broadly applicable measures will facilitate more precise, integrated, and comparative evaluations of a wide variety of interventions.
The increased emphasis on patient reported outcomes is also evident in the recently established Patient-Centered Outcomes Research Institute (P-CORI: www.pcori.org). This independent, nonprofit institute was established by the United States Congress in 2010, through the Patient Protection and Affordable Care Act. Its mission is to develop and disseminate information to inform health care decisions, specifically information based on empirical evidence about the effectiveness, benefits, and harms of treatment options patients and providers are considering, and the ways in which those outcomes differ for specific types of patients. In addition to information about survival or longevity and other objective biomedical outcomes for morbidity in various conditions (e.g., blood pressure, plasma lipid levels, blood glucose levels), the P-CORI mission specifically includes patient functioning (i.e., activity versus disability), symptoms, and health-related quality of life (H-QOL). Hence, classes of outcomes that have historically been seen as “soft” and providing weak evidence regarding the effects of interventions in behavioral medicine and health psychology are increasingly seen as important—for evaluations of clinical efficacy and effectiveness, for patients and providers choosing among treatment options, and as a guide to policy decisions regarding health care spending.
Outcomes that capture morbidity, mortality, and H-QOL have an important role not only in evaluating the effects of specific interventions, but also in comparing the relative benefits of various interventions. An increasingly common outcome index is the quality adjusted life year (QALY), which essentially weights each year of life by the H-QOL during that year (Kaplan & Groessl, 2002). QALYs can be used to compare not only a variety of intervention outcomes, but also can evaluate their cost-effectiveness by quantifying the cost associated with each QALY produced by that intervention (Kaplan & Groessl, 2002). It is possible that this growing emphasis on broader assessments of health outcomes will make the value of interventions in behavioral medicine and health psychology more apparent. They have the potential to influence not only mortality, but also directly improve components of H-QOL and do so at relatively low cost.
In addition to efforts to implement new standards for design, analysis, and reporting of RCTs, the choice of appropriate comparison or control conditions has received increased attention in behavioral medicine and clinical health psychology intervention research (Freedland, Mohr, Davidson, & Schwartz, 2011). The magnitude and meaning of the observed intervention effect depend, in large part, on the nature of the comparison or control conditions, and different comparison conditions are appropriate for specific questions. For example, comparisons to usual medical or surgical care are often used in initial evaluations of the efficacy of an adjunctive behavioral or psychological intervention, but can be faulted for failure to control for expectancies and other nonspecific factors. Variations in comparison conditions across multiple RCTs evaluating a given intervention can complicate systematic reviews and meta-analyses, the highest form of evidence in the EBM perspective.
Relative to prior reviews of the efficacy of interventions in behavioral medicine and health psychology (e.g., Blanchard, 1994), it is clear that methodological standards for the RCTs have been raised. However, facilitating an expansion of the research base demonstrating efficacy is not the only challenge for current intervention research. Enhancing the external validity of intervention trials and producing stronger evidence of effectiveness of interventions in representative health care settings is an increasingly important concern (Glasgow, 2008; Glasgow & Emmons, 2007).
In terms of impact on population health, intervention efficacy and effectiveness are critical concerns, but so is the number of individuals reached by a given intervention (Abrams et al., 1996). Even a highly efficacious intervention will have limited impact on population health if high costs or restricted access means it reaches a limited number of people who might otherwise benefit. Conversely, an intervention with relatively modest efficacy (i.e., a small treatment effect size) can have a substantial impact on population health if it reaches a very large portion of that population. This concept has been expanded in the RE-AIM (Reach, Efficacy, Adoption, Implementation, Maintenance) framework of Glasgow and colleagues, which has been applied to both prevention-oriented health behavior change interventions (Glasgow, Vogt, & Boles, 1999) and chronic illness management (Glasgow, McKay, Piette, & Reynolds, 2001). In this expanded perspective (see Table 17.1), the health impact of a given intervention is the product of its reach and efficacy (i.e., Impact = Reach × Efficacy), but other critical determinants of health impact are the extent to which the intervention is adopted in health services, the consistency and fidelity with which it is implemented in those settings, and the maintenance of that implementation. The RE-AIM model defines the important issue of intervention effectiveness as Efficacy × Implementation.
Table 17.1 The RE-AIM Framework (Glasgow, Vogt, & Boles, 1999). Tables can be downloaded in PDF formats at http://higheredbcs.wiley.com/legacy/college/lambert/1118038207/pdf/c17_t01.pdf.
| Reach | Proportion of the target population participating in the intervention |
| Efficacy | Success rate if intervention is implemented as intended in guidelines |
| Adoption | Proportion of settings, practices, and health care plans adopting the intervention |
| Implementation | Extent to which intervention is implemented as intended in real-world settings |
| Maintenance | Extent to which intervention program is sustained over time |
From this perspective, some issues in maximizing the potential health impact of behavioral medicine and health psychology interventions are largely new topics for research. Specifically the process of dissemination of research findings from RCTs of intervention efficacy, effectiveness studies, and systematic reviews, and the processes of intervention adoption and implementation are increasingly the focus of research in their own right (Kerner, Rimer, & Emmons, 2005; McHugh & Barlow, 2011). This emerging focus on translational science in the field recognizes that, “the behaviors in need of change are not just those of our patients, but also those of our main professional partners” including health care providers and policy makers (Spring, 2011, p. 1).
Smoking, levels of physical activity and fitness, dietary intake of calories and fat, and related levels of adiposity (i.e., overweight) are strongly related—individually and in combination—to cardiovascular disease (CVD) morbidity and mortality, cancer morbidity and mortality, diabetes, and all-cause mortality (Lee, Sui, Artero, et al., 2011; Lee, Sui, & Blair, 2009; Lee, Sui, Hooker, Herbert, & Blair, 2011). A substantial proportion of the decreases in morbidity and mortality associated with CVD and cancer in recent decades are attributable to population decreases in unhealthy behaviors (Byers, 2010; Ford & Capewell, 2011). Despite this progress, some estimates suggest that approximately 80% of CVD and diabetes, and 40% of cancers are still due to poor diet, physical inactivity, and tobacco use (Fisher et al., 2011; Spring, 2011). Further, has been suggested that type 2 diabetes could be largely eliminated through population-based changes in excess adiposity, moderate diet, and physical activity (Schulz & Hu, 2005). Yet in the United States spending on related prevention efforts is 5% or less of total health care expenditures (McGinnis, Williams-Russo, & Knickman, 2002; Satcher, 2006). Relative to the costs of treating these chronic health conditions, efforts to prevent them through the modification of related behaviors are highly cost-effective (Gordon, Graves, Hawkes, & Eaken, 2007).
Prominent models conceptualize health behavior change as a multiphase process, in which different points in the change process pose distinct challenges and require distinct intervention elements. This view is most formally represented in the Stages of Change Model, also known as the Trans-Theoretical Model (SOC/TTM; J. O. Prochaska, DiClemente, & Norcross, 1992). In this view, individuals pass sequentially through precontemplation, contemplation, preparation, action, and maintenance stages, perhaps multiple times in the event of relapse and renewed change attempts. In theory, different types of interventions are effective at different stages, creating a stage-by-intervention-type matching prediction regarding optimal change; interventions tailored or matched to the individual's specific location along the multistage process will be more effective than unmatched interventions. This tailoring or matching prediction has been supported in some research (Johnson et al., 2008; Krebs, Prochaska, & Rossi, 2010), as have other elements of the model (Hall & Rossi, 2008). However, the stages are often difficult to distinguish empirically (Herzog, 2008; Weinstein, Rothman, & Sutton, 1998), and matched or tailored interventions are often no more effective—or only slightly more effective—than nonmatched interventions (Armitage, 2009; Noar, Benac, & Harris, 2007).
The earliest point in the process of health behavior change is the primary focus of another influential model and related technique—motivational interviewing (Miller & Rose, 2009). This approach to patient interviews regarding potential health behavior change involves empathy, acceptance, and collaboration rather than the directive and problem-focused style that characterizes most medical encounters. The motivational interviewing (MI) approach also attempts to evoke and reinforce the patient's spontaneous and self-initiated “change talk.” Motivational interviewing is often implemented in brief contacts with patients in primary medical care, and has been found to have positive effects on efforts to modify smoking, diet, exercise, and the control of chronic disease (e.g., diabetes) (Lundahl & Burke, 2009; Martin & McNeil, 2009). However, RCTs on motivational interviewing have been criticized as methodologically limited, and producing small effect sizes (Knight, McGowan, Dickens, & Bundy, 2006). Many health behavior change attempts result in initial success but subsequent failure (Brandon, Vidrine, & Litvin, 2007), leading to the common practice of incorporating relapse prevention training as a component of interventions (Hendershot, Witkiewitz, George, & Marlatt, 2011). The approach is understandably widely used, but it has been difficult to demonstrate its independent efficacy (Agboola, McNeill, Coleman, & Bee, 2010).
Finally, in an effort to maximize health impact while minimizing costs, stepped care approaches have been developed in which low cost, largely self-guided health behavior change interventions are attempted initially, reserving professionally—delivered small group and individual treatments for cases where the less involved and costly “steps” fail to produce desired results (Abrams et al., 1996). The initial, low intensity and low cost steps have greater reach (Glasgow et al., 1999), and therefore have the potential to have important population impact. The higher efficacy but more intensive and costly approaches can be reserved for individuals who experience difficulty achieving or maintaining desired changes. Large group, organizational, and public policy interventions have the greatest potential reach. Given the remarkable prevalence of nearly all of the major behavioral risk factors, these approaches are a major focus of more broadly defined behavioral medicine and health psychology.
After decades of steady reductions in the prevalence of smoking in the United States and some other industrialized nations, this progress has slowed in recent years. Currently, approximately 20% of adults in the United States smoke, and this behavior remains the leading cause of preventable death. The most common reason for attempting to quit smoking is a concern about health (McCaul et al., 2006), and for smokers there is no other behavior change that will provide as great a potential health benefit. Yet, most cessation attempts result in failure. Hence, smoking cessation is a major challenge in current behavioral medicine and clinical health psychology.
For individual and small-group based approaches to smoking cessation, the major treatments currently in use are multicomponent interventions, often combining pharmacologic and behavioral interventions. Major meta-analyses indicate that CBT for smoking cessation (e.g., problem solving, skills training, stress management) is modestly effective, producing a 40% to 60% increase in the odds of maintained cessation (Fiore et al., 2008; Lancaster & Stead, 2005). However, it is important to note that given that as many as 90% or more of unaided quit attempts result in failure within 6 to 12 months, even in the most successful interventions the majority of smokers relapse within the typical follow-up periods. Given the design of the individual trials, it is difficult to identify the most effective elements of CBT. In most of the individual RCTs the experimental control of nonspecific factors is minimal. To address these limitations, RCTs are needed to test specific components and packages, while controlling nonspecific factors and evaluating hypotheses regarding the mechanisms contributing to change (Bricker, 2010).
Meta-analytic reviews and major RCTs have demonstrated the efficacy of nicotine replacement therapy in both longer-acting (e.g., nicotine patches) and shorter-acting (e.g., nicotine gum) forms, and the efficacy of buproprion (i.e., Zyban, Wellbutron) and varenicline (i.e., Chantix) (Baker et al., 2011; Fiore et al., 2008; Fiore & Baker, 2011; Stead, Perera, Bullen, Mant, & Lancaster, 2008). These pharmacological treatments provide improved outcomes over CBT alone, and hence the combination of CBT or similar counseling approaches with pharmacological treatment is currently considered the standard of care (Fiore et al., 2008), although even the strongest effects of medication demonstrated in these reviews indicate that most treated smokers do not maintain cessation. It is possible that pharmacologic treatment may be even more effective if initiated well before the smoker's “quit date” (Baker et al., 2011).
Many smokers have considered smoking cessation but have not made a serious attempt to quit, or have failed in previous attempts. As a result, at any given time a large number of smokers are characterized by a low level of motivation for cessation. Motivational interviewing would seem to be a useful approach in this scenario, but to date there is little evidence that it produces a significant, independent effect on cessation (Bricker, 2010; Hettema, Steele, & Miller, 2005). Given that many smokers relapse after an initially successful quit attempt, relapse prevention is a common element of CBT approaches to smoking cessation. However, the evidence from RCTs specifically evaluating the effects of relapse prevention training indicates that it has little or no additional benefit (Lancaster, Hajek, Stead, West, & Jarvis, 2006). Research on the SOC/TTM approach in which specific interventions are matched to the smoker's stage along the continuum of change described previously has produced evidence of small improvements in cessation and abstinence (Noar et al., 2007), but some RCTs based on the model have not found evidence of the predicted benefits of matching (e.g., Aveyard, Massey, Parsons, Manasecki, & Griffin, 2009). This pattern of findings has led to the conclusion that the model is largely unsupported in this important health behavior domain (e.g., Bricker, 2010; West, 2005).
Despite the limited evidence in support of the SOC/TTM predictions regarding the effects of matching specific interventions to phases of the change process on smoking cessation and abstinence, it is clear that different sets of multifaceted challenges are prominent at different points in the smoking cessation process—motivating smokers to seriously consider quitting, preparing for cessation, the actual process of cessation, and maintaining abstinence and managing brief lapses and more prolonged relapses. Further, it is apparent that within each of these phases, the multiple challenges likely require multiple intervention approaches (Baker et al., 2011). Thus, process approaches warrant additional research, though perhaps should be expanded beyond the traditional stages of change framework. However, even in the absence of clear and specific evidence from RCTs, the current status of the evidence on the psychobiology of nicotine dependence and addiction and related behavioral research on addictive behavior suggests that it is appropriate to select and combine approaches to address these specific sets of challenges (Baker et al., 2011). Hence, this emerging expansion of the standard of care recognizes the value of combined pharmacologic and CBT treatments that should also reflect the differing challenges at various points in the process of smoking cessation.
Several environmental and policy-level approaches to smoking have been found effective in reducing smoking and lowering related health care costs, including raising taxes on tobacco, reducing smoke exposure (i.e., “secondhand” smoke) by prohibiting smoking in public places, bans on tobacco advertising and sponsorships, regulation of packaging and warning labels, promoting public awareness, increasing access to smoking cessation through expanded insurance coverage and public funding, and decreasing tobacco sales to minors through increased penalties for illegal sales (Cummings, Fong, & Borland, 2009). Policy-based changes in health care systems have also been found to be effective, including improved tracking of smoking status in health records, and increasing health care professionals' frequency and consistency of asking about smoking status and providing encouragement to quit (Curry, Keller, Orleans, & Fiore, 2008). Specific guidelines have been developed for health care providers for addressing smoking among their patients (Fiore & Baker, 2011). These guidelines involve regular inquires about the patient's smoking status and readiness to pursue smoking cessation, motivational interventions for those low in readiness, and specific pharmacological and behavioral interventions for those smoking patients who are ready to proceed.
Obesity defined as a body mass index (BMI) greater than 30 kg/m2 has been associated with a host of negative health outcomes including coronary heart disease (Bogers et al., 2007), type 2 diabetes (Guh et al., 2009), some forms of cancer (Renehan, Tyson, Egger, Heller, & Zwahlen, 2008), and mortality related to these and other conditions (Whitlock et al., 2009). Importantly, recent prevalence estimates indicate that more than 30% of adults are obese (Flegal, Carroll, Ogden, & Curtin, 2010). Prevalence rates have more than doubled since the late 1970s, and even though this dramatic increase has slowed in recent years for children, adolescents, and adults (Flegal, Carroll, Kit, & Ogden, 2012; Ogden, Carroll, Kit, & Flegal, 2012), medical experts now consider obesity to be “epidemic” (Stein & Colditz, 2004). Not surprisingly then, behavioral approaches to weight loss continue to be a major focus of clinical health psychology and behavioral medicine.
A recent review of behavioral treatments for obesity concluded that, on average, intervention studies report a 10% decrease in body weight—enough for improvements in health—but that maintaining weight loss continues to be challenging (Butryn, Webb, & Wadden, 2011). Using in-person, Internet, or telephone contact between patients and providers to prolong engagement in interventions, encouraging high amounts of physical activity, or combining lifestyle behavior change with pharmacotherapy have shown promise in preventing weight regain (Butryn et al., 2011). For example, a recent randomized controlled trial demonstrated the efficacy of combined naltrexone/bupropion therapy as an adjunct to intensive behavior modification for obesity, with the drug intervention producing a 9% reduction in body weight compared to 5% among controls (Wadden et al., 2011). In another recent RCT, two behavioral interventions, one delivered with in-person support and the other delivered remotely, without face-to-face contact between participants and weight-loss coaches, resulted in clinically significant weight loss averaging more than 10 pounds over a period of 24 months, compared to only approximately 2 pounds in a comparison group (Appel et al., 2011). Other RCTs of web-based intervention have found that greater weight loss is observed among those with higher levels of website utilization (Bennett et al., 2010). Another recent RCT examined the efficacy and cost-effectiveness of a cognitive-behavioral weight management program in the form of written materials and basic web access, complemented by an interactive website and brief telephone/email coaching. Participants (1,755 overweight) were randomized to one of three conditions with increasing intervention intensity. Participants experienced significant weight loss, increased physical activity, and decreased blood pressure across conditions. Cost-effectiveness ratios were $900 to $1,100/quality-adjusted life year for the two lower intensity interventions and $1,900/quality-adjusted life year for the higher intensity intervention (web intervention plus coaching). The cost recovery analyses indicated that the costs of treatment were matched by savings in health care expenditures after 3 years for the two lower intensity interventions and after 6 years for the other intervention (Hersey et al., 2012). A recent meta-analysis indicated that the addition of motivational interviewing to weight loss intervention resulted in a small (3 pounds) additional weight loss in obese and overweight individuals (Armstrong et al., 2011). Collectively, these studies highlight the importance of adequate and continued support, which can be in varying modalities and that this increased support is cost-effective in the long run.
Promoting increases in physical activity is central to prevention of obesity, weight loss among obese individuals, and in maintenance of weight loss. In a recent review, Goldberg and King (2007) report that to prevent age-related weight gain generally, levels of vigorous physical activity above the usually recommended 30 minutes daily (e.g., to 45 to 60 minutes daily) may be necessary. For weight loss, physical activity interventions alone usually produce only modest results (e.g., 3 to 6 pounds), suggesting that for obese individuals significant weight loss also requires dietary change. Goldberg and King (2007) also note that current research suggests that high levels of physical activity (e.g., 40 to 90 minutes daily) may be necessary for weight loss maintenance.
Meta-analysis of psychobehavioral interventions in preventing weight gains or reducing weight among U.S. multiethnic and minority adults has indicated that multicomponent (versus single component) lifestyle interventions were efficacious and suggested that incorporation of individual sessions, family involvement, and problem-solving strategies are useful (Seo & Sa, 2008). Beyond traditional individually delivered weight loss intervention, recent research has also focused on environmental approaches to healthy eating (Story, Kapingst, Robinson-O'Brien, & Glanz, 2008) and worksite weight-loss intervention (Anderson et al., 2009). Given the dramatic recent increases in childhood obesity and the robust association of childhood and adolescent obesity with obesity in adulthood, it is clear that intervention efforts targeting weight loss in children are essential. Approaches with at least preliminary evidence of success in producing meaningful and sustained weight loss include school-based interventions (Katz, 2009), family-based approaches (Epstein, Paluch, Roemmich, & Beecher, 2007), and environmental and policy approaches (Brennan, Castro, Brownson, Claus, & Orleans, 2011).
Physical activity level and sedentary behavior are risk factors for the development of many chronic illnesses and negative health conditions including obesity, hypertension, type 2 diabetes, and coronary heart disease. Interestingly, recent research suggests that sedentary behavior may be a distinct risk factor, independent of commonly used measures of physical activity, for a variety of adverse health outcomes in adults (Thorpe, Owen, Neuhaus, & Dunstan, 2011). The “dose” of physical activity that is needed continues to be debated; however, recent research has emphasized that even light activity improves health in sedentary individuals and that recommending small, gradual increases in activity helps to mitigate the incidence of adverse events and improve adherence to physical activity regimens (Powell, Paluch, & Blair, 2011). Given the role of physical activity and sedentary behavior in development of chronic illness, interventions focused on increasing activity levels and exercise behavior continue to be central to clinical health psychology and behavioral medicine. For example, current evidence supports the effectiveness of increasing physical activity in the prevention and treatment of obesity (Goldberg & King, 2007) and in the management of type 2 diabetes (Umpierre et al., 2011). Exercise has sustained beneficial effects on depression (Conn, 2010; Hoffman et al., 2011), and a recent meta-analysis of randomized controlled trials concluded that exercise is effective in reducing depressive symptoms in individuals with chronic illness, particularly those with mild-to-moderate depression (Herring, Puetz, O'Connor, & Dishman, 2012). Exercise has also been found to improve various aspects of cognitive functioning, including attention, processing speed, executive functioning, and memory (Smith, Blumenthal et al., 2010).
Given the evidence that declining physical activity and increases in sedentary behavior in the population over recent decades derive largely from environmental factors (Brownson, Boehmer, & Luke, 2005) interventions have increasingly moved beyond individually delivered approaches. Examples include worksite interventions (Abraham & Graham-Rower, 2009) and ecological approaches (e.g., increasing the “walk-ability” of communities and access to recreation sites) to increase physical activity (Sallis et al., 2006). Further, given the dramatic increase in childhood obesity and the success of adult-focused diabetes prevention efforts focused on increasing physical activity (Diabetes Prevention Program Research Group, 2002), school-based exercise programs have been the focus of recent RCTs demonstrating improvement in body composition, fitness, and insulin sensitivity in children (Carrel et al., 2005). However, maintenance of such benefits over prolonged school vacations can be problematic (Carrel et al., 2007).
HIV continues to be a major public health burden, with incidence rates in the United States ranging from 47,800 to 56,000 over the years 2006 to 2009 (Prejean et al., 2011), making preventive intervention a continued focus of clinical health psychology and behavioral medicine. HIV prevention efforts have involved a combination of behavioral (e.g., condom use, reduction in presex alcohol and drug use, reduction in needle-sharing among drug users), biomedical (e.g., antiretroviral medications to reduce transmission), and structural (i.e., social, economic, political) intervention strategies; many of these interventions have been found effective in reducing HIV risk behaviors by 25% to 50% (see Rotheram-Borus, Swendeman, & Chovnick, 2009). Although a variety of interventions have proven useful and cost-effective, inadequate funding, imperfect targeting strategies, and a problematic policy environment have been barriers to the widespread implementation of these life-saving interventions (Holtgrave & Curran, 2006).
Given these issues, HIV prevention efforts have increasingly focused on targeted interventions for high-risk groups. Groups at particular risk include young men who have sex with men, the only group that continues to show an increase in HIV infection, and African American men and women who have an estimated HIV incidence rate 7 times that of whites (Prejean et al., 2011). In a recent review of prevention efforts in young men who have sex with men, Mustanski, Newcomb, Du Bois, Garcia, and Grov (2011) suggest that Internet-based interventions, integration of biomedical and behavioral approaches, and interventions that take advantage of community and network factors are particularly promising. African American women also represent a high-risk target group. A recent meta-analysis indicated that interventions that used gender- or culture-specific materials, used female deliverers, addressed empowerment issues, provided skills training in condom use and negotiation of safer sex, and used role-playing to teach negotiation skills were particularly efficacious in HIV prevention in this risk group (Crepaz et al., 2009). Individuals who already have a sexually transmitted disease are at higher risk for additional STDs as well as HIV infection; a recent meta-analysis confirmed that targeting prevention efforts toward patients at STD clinics is effective and should be a high public health priority (Scott-Sheldon, Fielder, & Carey, 2010).
Many individuals are characterized by more than one unhealthy behavior; smokers often are relatively sedentary, as are many individuals who consume a diet too high in calories, refined sugars, and saturated fat. The scope of this problem is even greater, if emotional difficulties such as depression are included in the definition of multiple risks. This creates the need for effective approaches to multiple risk behavior change interventions (J. J. Prochaska, Nigg, Spring, Velicer, & Prochaska, 2010; J. J. Prochaska & Prochaska, 2009). As seen in the preceding discussion of interventions for obesity and weight loss, the targeting of multiple behaviors (e.g., diet and exercise) is standard in many instances. Yet, RCTs of multiple health behavior change approaches are a relatively new development in the field. In many cases, the issue poses minimal difficulties. For example, treatment of other behavioral risks (e.g., diet, sun exposure) does not appear to interfere with the effectiveness of smoking cessation (J. J. Prochaska, Velicer, Prochaska, Delucchi, & Hall, 2006). Other combinations of risks poses more complicated challenges. For example, many smokers express the concern that smoking cessation will lead to weight gain, and weight gain can lead to failure to achieve and maintain abstinence. Combined treatments for smoking cessation and weight management can increase abstinence and reduce weight gain initially, but these benefits are often not maintained (Spring et al., 2009), indicating the need for additional treatment methods.
In weight loss efforts, comorbid depression is a common concern (Fabricatore & Wadden, 2006). Obesity and depression have a robust concurrent association, perhaps reflecting a bidirectional pattern of influence over time (Atlantis & Baker, 2008; Markowitz, Friedman, & Arent, 2008). The prospective association in which depression predicts weight gain over time is somewhat stronger than the role of initial adiposity in later depression (Atlantis & Baker, 2008; Gariepy, Wang, Lesage, & Schmitz, 2010; Patten, Williams, Lavorato, Khaled, & Bulloch, 2011). Attrition from clinical weight loss trials has been found to be related to depression at baseline and poor early weight loss (Fabricatore et al., 2009). In an RCT aimed at addressing co-occurring depression, women with comorbid obesity and depression were randomized to behavioral weight loss or behavioral weight loss combined with cognitive-behavioral depression management. Women in both groups demonstrated significant weight loss and reduction in levels of depression (Linde et al., 2011). The failure to find added benefit of specific depression treatment may reflect common elements across these two interventions. Both included behavioral activation, problem-solving training, social support, and cognitive restructuring. Hence, the weight loss only condition may have included useful treatment elements for addressing depression. High levels of stress have a modest but significant prospective association with increasing adiposity (Wardle, Chida, Gibson, Whitaker, & Steptoe, 2011). Hence, the effects of stress reduction as an adjunctive treatment in weight loss programs among patients experiencing high levels of stress or related emotion regulation difficulties is a potentially important topic for future intervention research. Given the prevalence of both depression and obesity in the general population, the efficacy and effectiveness of approaches to weight loss among depressed persons is an important topic for further research.
The co-occurrence of smoking and depression is also common and poses similar challenges (Aubin, Rollema, Svensson, & Winterer, 2012; Hall & Prochaska, 2009). Traditional cessation programs can be successfully adapted for use with depressed smokers (Hall et al., 2006), and smoking cessation does not appear to increase depression or other emotional symptoms (Bolan, West, & Gunnell, 2011), even among initially depressed smokers (J. J. Prochaska, Hall, Tsoh, et al., 2008). However, rates of successful cessation and maintained abstinence are often lower in depressed smokers (Hall & Prochaska, 2009). Preliminary evidence suggests that the addition of CBT for depression may be a useful addition to cessation treatments for individuals prone to depression (Kapson & Haaga, 2010). Further, physical activity may facilitate abstinence after smoking cessation (J. J. Prochaska, Hall, Humfleet, et al., 2008), especially in light of the fact that exercise can have beneficial effects on depression (Blumenthal, 2011).
Chronic medical illness poses a multifaceted adaptive challenge for patients and their families. The physical symptoms and distress (i.e., pain) stemming from these illnesses can be burdensome, and they often are the cause of serious reductions in functional activity across a variety of roles and domains (Stanton, Revenson, & Tennen, 2007). Depression and other emotional difficulties are much more common among persons with chronic medical illness, given these stressors (Smith, 2010a). Patients must also adhere to often complex medical regimens, and the extent to which they do so has important effects on health outcomes (Cramer, Benedict, Muszbek, Keskinaslan, & Khan, 2008; Gehi, Ali, Na, & Whooley, 2007). Yet, even in conditions like cardiovascular disease where the value of medications is quite substantial, as little as 50% of prescribed medications are taken (Baroletti & Dell'Orfano, 2010). In the same health care settings in which psychologists provide services to individuals with chronic medical illness, they are increasingly called to manage other presenting complaints and problems where traditional medical approaches are not optimal (e.g., sleep disturbance, somatoform disorders). In what follows here, we review intervention research findings on both the most common medical illnesses, and complaints that often are presented in medical settings.
Approaches to adjunctive psychosocial care vary somewhat across specific illness and presenting problems, but several are broadly applicable. Cognitive-behavioral interventions for stress, pain, sleep, somatic complaints, and emotional adjustment are widely used, as are supportive-expressive therapies. Rehabilitation often includes operant and exposure-based treatments for progressively increasing functional activities and reducing avoidance of feared activities. Couple and family approaches are less commonly used, but have considerable potential given that the patient's degree of adaption to chronic illness affects and is affected by family members. Exercise interventions have broad applicability. They can improve functional activity, but in some conditions are useful in treating the underlying disease and in improving emotional adjustment (Herring et al., 2012).
Cardiovascular disease is the leading cause of death in the United States, as it is in many industrialized nations. One of these conditions, essential hypertension is a contributing cause of the other two primary cardiovascular diseases—coronary heart disease and stroke—but also increases risk of other serious illness (e.g., renal disease).
Behavior changes involving diet, exercise, and weight loss are standard aspects of the medical management of essential hypertension, both as an initial intervention for mild levels and as an adjunct to pharmacologic treatment. This is particularly true in the case of overweight individuals, as adiposity is a common contributing factor in essential hypertension. Clinical trials have demonstrated the efficacy and effectiveness of the Dietary Approaches to Stop Hypertension (DASH) and DASH-low sodium diets in preventing and treating hypertension (Appel et al., 2006). Compared to a typical U.S. diet, the DASH diet is low in saturated fat, red meat, and refined sugars, and high in intake of fruits, vegetables, and low fat dairy products, with a substantial portion of the diet including whole grain, fish, poultry, and nuts. Adherence to DASH diet has been found to reduce blood pressure by a clinically meaningful 5 to 10 mmHg among high-risk individuals, and risk of CHD and stroke by as much as 20% (Fung et al., 2008).
These important reductions in blood pressure can be augmented when the DASH diet is accompanied by exercise and weight loss interventions. For example, combining the DASH diet with an exercise program and a reduction in caloric intake intended to produce weight loss improves both standard clinic-based measurements of blood pressure and levels of the more prognostic indicator of ambulatory blood pressure for overweight hypertensives (Blumenthal, Babyak, Hinderliter, et al., 2010). This combined intervention was also more effective in altering other markers of vascular, cardiac, and metabolic risk including pulse wave velocity (i.e., arterial stiffness), left ventricular mass, insulin insensitivity or glucose regulation, and plasma cholesterol and triglycerides (Blumenthal, Babyak, Sherwood, et al., 2010; Blumenthal, Babyak, Hinderliter, et al., 2010). Hence, the combined dietary, exercise, and weight loss intervention has broad health benefits, especially among overweight persons. The exercise and weight loss also reduce depressive symptoms among hypertensives, especially among those with higher initial levels of depression (Smith, Blumenthal, Babyak, et al., 2007). Attenuated nocturnal decreases (i.e., “dipping”) in blood pressure are an independent risk factor for cardiovascular disease, more common among African Americans than whites. In this regard, it is important to note preliminary evidence that the DASH diet can improve nocturnal blood pressure dipping among African Americans (Prather, Blumenthal, Hinderliter, & Sherwood, 2011).
Chronic stress is associated with increased risk of high blood pressure and the development of diagnosed hypertension (Sparrenberger et al., 2009), providing the rationale for various stress management and relaxation therapies as adjuncts to traditional approaches to the management of hypertension. A meta-analysis of 25 trials including a total of more than 1,000 patients found small but significant reductions (SBP −5.5 mmHg; DBP −3.5 mmHg) in blood pressure (Dickinson et al., 2008). Although even small blood pressure reductions can be clinically meaningful, methodological weaknesses of some the individual trials (e.g., small sample sizes, failure to control nonspecific factors) raise concerns about the reproducibility of this result. As a result, exercise, dietary, and weight loss interventions have stronger support as treatments for hypertension, compared to stress management.
The standard medical management of coronary heart disease (CHD) has included behavioral interventions for many years. Adherence to diet, exercise, and smoking cessation recommendations for CHD patients is associated with a 40% to 50% reduction in recurrent cardiac events (e.g., additional myocardial infarction, death) within the first 6 months after hospitalization for acute coronary syndrome (Chow et al., 2010). Among smokers who develop acute coronary disease, between 30% and 50% quit without formal smoking cessation intervention. However, interventions for smoking cessation produce added benefits among these patients, increasing the chances of successful cessation by 60% (Barth, Critchley, & Bengel, 2008) with associated reductions in risk of future cardiac events following successful cessation. However, quit rates are far from satisfactory, suggesting the need for more effective interventions and more consistent implementation of effective approaches. Meta-analyses have consistently demonstrated that exercise-based cardiac rehabilitation reduces recurrent cardiac events and all-cause mortality by approximately 20% (Taylor et al., 2004), although improvements in access, implementation, and adherence are needed.
The effects of psychological stress and negative emotion on the development and course of coronary heart disease (CHD) are well-established, with extensive evidence accumulating from animal models, human epidemiological research, and clinical studies of CHD patient populations (Williams, 2008). Specific forms of stress linked to CHD include work stress (Eller et al., 2009) and stress in personal close relationships (De Vogli et al., 2007; Matthews & Gump, 2002; Orth-Gomer et al., 2000; Rohrbaugh et al., 2006; Smith et al., 2012). Further, psychological stress and negative emotion are associated with increased CHD risk across the full time course of the disease, from the development and progression of asymptomatic atherosclerosis, to the emergence of cardiac events, and the course of established CHD (Bhattacharyya & Steptoe, 2007; Williams, 2008). Given the important historical role played by the Type A behavior pattern in this research area, a major aspect of this evidence concerns the association of anger and hostility—key unhealthy elements of the broader Type A pattern—with the development and course of CHD (Chida & Steptoe, 2009). However, in recent years extensive evidence has accumulated indicating that depression and anxiety are also risk factors for the development of CHD among initially healthy persons, and for increased risk among patients with disease (Nicholson, Kuper, & Hemingway, 2006; Rutledge, Reiss, Linke, Greenberg, & Mills, 2006; Smith, 2010a; Suls & Bunde, 2005). These associations with CHD provide the foundation for a variety of studies of the effectiveness of stress management and interventions for negative affective symptoms and conditions.
The potential value of such approaches was initially demonstrated in the Recurrent Coronary Prevention Project (RCPP), in which group therapy intended to reduce Type A behavior among CHD patients not only successfully modified this behavioral endpoint, but also resulted in a significant and nearly 50% reduction in subsequent coronary events (15% in comparison condition versus 8% in treatment condition; Friedman et al., 1986). A recent meta-analysis of RCTs of stress management and similar psychosocial interventions for patients with CHD found evidence of a significant reduction of more than 40% in recurrent coronary events for 2 years after treatment and a 27% reduction in all-cause mortality over the same follow-up period (Linden, Phillips, & Leclerc, 2007). These benefits were limited to men, however, with no effect on prognosis among women. Further, interventions were significantly more effective when initiated 2 months or more after the initial coronary event rather than closer in time to hospitalization, and the interventions were significantly more effective if they also reduced indications of emotional distress (Linden et al., 2007).
Subsequent studies have confirmed the general effectiveness of these interventions. In a randomized controlled trial of cognitive-behavioral stress management in a sample of more than 350 CHD patients, the intervention produced a significant reduction in risk of recurrent cardiovascular events. Specifically, 47% of patients receiving usual care experienced a recurrent cardiovascular event over an average of 8 years of follow-up, compared to 36% of the patients receiving CBT (Gulliksson et al., 2011). Importantly, a recent RCT of cognitive-behavioral stress management for women with CHD (Orth-Gomer et al., 2009) found that over a 7-year follow-up women in the treatment group had a 3-times smaller risk of death than those in the control (i.e., 7% mortality versus 20%). Thus, the CBT approach was successfully adapted for women with CHD in this case. Given the considerable attention to the study of anger and CHD (Chida & Steptoe, 2009) and the availability of empirically supported anger treatments (Smith & Traupman, 2012), it is surprising that few studies have directly examined the benefits of such interventions among CHD patients. One small RCT did find that CBT for anger and hostility produced a significant reduction in recurrent coronary events and a related savings in health care costs (Davidson, Gidron, Mostofsky, & Trudeau, 2007). Stress management interventions have also been found to alter biomarkers of CHD severity (e.g., reductions in stress-induced cardiac ischemia, increases in flow-mediated arterial dilation), illustrating plausible mechanisms underlying the effect of psychosocial interventions on coronary outcomes (Blumenthal, Sherwood et al., 2005). However, it is important to note that other systematic reviews of the topic (Whalley et al., 2011) have not reached the same positive conclusions as those of Linden et al. (2007).
In another historically important behavioral approach to the treatment of coronary disease, Ornish and colleagues (1990, 1998) have examined the effects among CHD patients of a comprehensive lifestyle change program involving a low-fat, whole foods diet (i.e., whole grains, fruits, vegetables), moderate exercise, stress management, and attendance at regular support group meetings. Early RCTs of the program demonstrated significant effects on the coronary risk factors, extent of coronary artery disease, other indicators of underlying disease severity, and coronary events (e.g., Gould et al., 1995; Ornish et al., 1990, 1998). Subsequent research has demonstrated additional beneficial effects on coronary outcomes, various aspects of quality of life, and related health care costs (for reviews, see Vizza, 2012; Weidner & Kendel, 2010).
The extensive evidence of an association between depression and the course of CHD has prompted efforts to examine the benefits of related treatments. The most notable effort was the multicenter Enhancing Recovery in Coronary Heart Disease (ENRICHD) (Berkman et al., 2003). ENRICHD enrolled more than 2,000 CHD patients selected primarily for elevated levels of depression, but also for social isolation, a related and significant psychosocial risk for poor cardiac outcomes. In comparison to the control condition, the CBT-based intervention produced small but significant improvements in depression and social isolation, but no effects on the primary combined outcomes of death and recurrent coronary events (Berkman et al., 2003). Secondary subgroup analyses indicated that there were beneficial effects on the primary outcome for white men (Schneiderman et al., 2004) and those patients who had received at least some of the CBT intervention in group as opposed to only individual sessions (Saab et al., 2009).
CBT for depression has been found to be effective for CHD patients experiencing depression following coronary artery bypass graft surgery (CABG) (Freedland et al., 2009). Also among depressed post-CABG patients, telephone-based collaborative care that includes psychoeducation and supportive counseling for depression was found to be effective in reducing negative mood symptoms, improving HQOL, and levels of physical functioning (Rollman et al., 2009). Davidson et al. (2010) randomized depressed acute coronary syndrome patients to usual care or an enhanced depression care condition in which patients self-selected into either pharmacotherapy or problem-solving therapy, followed by stepped care for continuing depression. The treatment group showed significantly better depression outcomes and a significant reduction in adverse cardiac events, although the latter outcome should be considered preliminary given the small number of events. To date, studies evaluating the effects of pharmacotherapy for depression in CHD patients have found mixed evidence of effects on depression, and no evidence of improved cardiac outcomes (for a review, see Kop & Plumoff, 2012).
As noted above, exercise is effective for CHD improving prognosis for patients, and it has also been found to improve depression. Hence, exercise seems promising as a potential treatment for depressed CHD patients (Blumenthal, 2011; Smith 2006b). However, it is important to note that the supporting evidence is indirect and preliminary, and such exercise interventions for depression in CHD patients would need to address the fact that depression predicts failure to complete exercise-based cardiac rehabilitation (Casey, Hughes, Waechter, Josephson, & Rosneck, 2008).
Given the high prevalence of depression in various CHD patient groups and its association with adverse events and mortality in this population, the American Heart Association has endorsed screening and increased availability of depression management for CHD patients (Lichtman et al., 2008). However, to date there are no empirical demonstrations that such procedures result in improved care or cardiac outcomes (Thombs et al., 2008). Nonetheless, depression is a direct contributor to poor HQOL, and can interfere with other behavioral interventions with well-established benefits for CHD patients, such as exercise (Casey et al., 2008) and smoking cessation (Thorndike et al., 2008). Hence, depression treatment should be a regular focus in the clinical management of CHD, but one whose effect is not as strong as would be hoped.
The mixed results of interventions for depression in CHD raise the important question as to whether the interventions have the optimal focus. Specifically, in health populations and in CHD populations, depressive symptoms and disorders overlap considerably with other negative affective symptoms and disorders related to adverse cardiac outcomes (Smith 2010a; Suls & Bunde, 2005). In addition to further attention to the unique versus independent associations of these interrelated psychosocial risk factors with the course of CHD, intervention research should explore the value of treatments that address common rather than unique features of various negative affective problems (e.g., Wilamowska et al., 2010). Negative affective characteristics also are closely related to difficulties in close relationships (e.g., high conflict, low support) known to influence the development and course of CHD (e.g., Matthews & Gump, 2002; Rohrbaugh et al., 2006). As a result, intervention research for CHD patients might also usefully explore the potential benefits of empirically supported treatments for relationship difficulties generally (Lebow, Chambers, Christensen, & Johnson, 2012) and in the specific context of health problems (Shields et al., 2012).
The rehabilitation and management of stroke patients has traditionally been the purview of rehabilitation psychologists and neuropsychologists, rather than clinical health psychologists, and as a result is somewhat beyond our present scope. However, in addition to cognitive rehabilitation and physical therapy, it should be noted that many of the behavioral interventions described for hypertension and CHD are core elements of the medical management of these patients (review Caplan, 2010). Further, depression is common among stroke patients, and is more frequent among patients with more severe strokes, greater physical disability, and greater cognitive impairments (Hackett & Anderson, 2005). Psychological therapies (i.e., counseling, psychotherapy) are at least somewhat effective for preventing depression after strokes, but pharmacological therapies are not (Hackett, Anderson, House, & Halteh, 2008). However, among stroke patients who have already developed significant levels of depression, the opposite seems to be true; pharmacological therapies are at least somewhat useful, but psychological therapies are not (Hackett, Anderson, House, & Xia, 2008).
Psychosocial interventions in cancer have targeted the emotional distress that often accompanies the disease, quality of life generally, and side effects of cancer treatment, such as fatigue. The effect of psychosocial treatments on survival among cancer patients has a controversial history in the field.
CBT and related therapies (e.g., problem-solving training) for depression and general emotional distress in cancer patients reduces distress, improves social support, and improves health behavior (e.g., diet, smoking) (Andersen et al., 2004; Antoni et al., 2009; Nezu, Nezu, Felgoise, McClure, & Houts, 2003). CBT is also effective specifically among depressed cancer patients (Hopko et al., 2008). Psychotherapy has been found to be effective for reducing depressive symptoms among incurable cancer patients (Akechi, Okuyama, Onishi, Morita, & Furukawa, 2008). Coping and communication interventions are also effective in reducing depression relative to usual care control conditions, as is supportive counseling (Manne et al., 2007). Mindfulness-based stress reduction has been found to reduce levels of depression and anxiety, and to increase energy, physical functioning, and role functioning (Lengacher et al., 2009). Some meta-analyses of mindfulness-based approaches have demonstrated positive effects on indicators of psychological adjustment (Ledesma & Kumano, 2009), but others have reached more cautious conclusions (Edwards, Hulbert-Williams, & Neal, 2008).
Across multiple interventions and specific cancer populations, psychosocial interventions are effective in reducing emotional distress, but the effect size is up to 3 times larger among patients preselected for elevated signs of distress, as compared to unselected patients (Linden & Girgis, 2011). Despite these generally consistent results, some reviews have concluded that the overall evidence of benefits from adjunctive psychosocial treatments in cancer is limited by methodological features of many individual RCTs (Coyne, Lepore, & Palmer, 2006). Further, to date there is no strong evidence that screening for depression or distress in cancer patient populations by itself results in improved overall outcomes for emotional adjustment (Meijer et al., 2011; Palmer, Van Scheppinger, & Coyne, 2011). Some evidence suggests that screening for unmet psychosocial needs rather than depression specifically may be a more efficient approach to the identification of cancer patients who would benefit from the treatments described above (van Scheppingen et al., 2011). Thus, the best means for identification of patients most likely to benefit from specific psychosocial treatments is an important topic for research.
Medical treatments for cancer, although often highly effective, frequently have major side effects that are themselves a detriment to H-QOL. Fatigue is the most common example. Meta-analyses of RCTs have demonstrated that exercise and other psychosocial treatments are effective in reducing fatigue in cancer patients (Cramp & Daniel, 2008; Kangas, Bovbjerg, & Montgomery, 2008). Of the nonexercise treatments, both supportive-expressive therapy and CBT show promise. Notably, fatigue and its seeming opposite physical or emotional symptoms (e.g., vigor) actually function as separate outcomes; when both fatigue and vigor or positive affect are measured independently, treatment effects on one are not necessarily accompanied by parallel changes on the other. In this regard, it is important to note that a combined CBT and hypnosis intervention reduced the fatigue accompanying radiation therapy in breast cancer patients (Montgomery et al., 2009), and reduced negative affect while increasing positive affect (Schnur et al., 2009).
In basic research on animal models of cancer progression and in human clinical studies of recurrence and survival, there is considerable evidence that stress, negative emotion, and other psychosocial risk factors can contribute to the course of some forms of the disease (Antoni et al., 2006; Chida, Hamer, Wardle, & Steptoe, 2008). Further, in animal research and human clinical studies, plausible psychobiologic mechanisms underlying these effects have been identified (Antoni et al., 2006). These observations have raised the question as to whether psychosocial treatments known to effect emotional adjustment, side effects, and H-QOL generally might also have beneficial effects on the course of the illness. An early study reported that supportive-expressive group therapy for women with advanced, metastatic breast cancer not only had beneficial effects on psychosocial functioning but also resulted in increased survival (Spiegel, Bloom, Kraemer, & Gottheil, 1989). Similar results were reported by other investigators for other forms of cancer (Fawzy et al., 1993). However, meta-analyses and related critiques have called these findings into serious question (Coyne, Stefanek, & Palmer, 2007; Edwards et al., 2008). Even though subsequent RCTs evaluating CBT have reported positive effects on cancer survival (Andersen et al., 2008) and on multiple biologic pathways that could alter the course of cancer progression (Antoni et al., 2009; Antoni et al., 2012), the evidence of effects on the course of cancer is not sufficient to support using these interventions as treatments of the disease, per se (Stefanek, Palmer, Thombs, & Coyne, 2009). Rather, their other, better-documented effects on important aspects of H-QOL provide a more appropriate rationale.
Diabetes is a group of diseases marked by high levels of blood glucose resulting from defects in insulin production, insulin action, or both. Type 1 diabetes, previously called insulin-dependent diabetes mellitus or juvenile-onset diabetes, develops when the body's immune system destroys insulin-producing pancreatic beta cells. To survive, people with type 1 diabetes must have insulin delivered by injection or a pump. This form of diabetes usually strikes children and young adults, although disease onset can occur at any age. Type 2 diabetes, previously called non–insulin-dependent diabetes mellitus or adult-onset diabetes, accounts for the vast majority of all diagnosed cases of diabetes. It is characterized by insulin resistance, and as the need for insulin rises the pancreas gradually loses its ability to produce it. Type 2 diabetes is associated with older age, obesity, family history of diabetes, history of gestational diabetes, impaired glucose metabolism, physical inactivity, and race/ethnicity. African Americans, Hispanic/Latino Americans, American Indians, and some Asian Americans and Native Hawaiians or other Pacific Islanders are at particularly high risk for type 2 diabetes and its complications. With an adult prevalence of 20.7 million that has increased in recent years (Cowie et al., 2010) and the continued emphasis on behavior change in disease management, a focus on type 2 diabetes continues to be a key part of clinical health psychology and behavioral medicine intervention science.
In addition to medical intervention (e.g., insulin), diabetes management typically involves multicomponent lifestyle changes including regular blood glucose monitoring, weight loss/dietary changes, and exercise. Stress management has also proven to be beneficial (Surwit et al., 2002). Given the active role of patients in monitoring blood glucose and adjusting self-administered insulin, adherences to this demanding medical regimen and overall self-management is an important challenge. Further, because modest weight loss and exercise changes have been demonstrated to significantly reduce the incidence of diabetes (Diabetes Prevention Program Research Group, 2002), behavioral medicine intervention to prevent the onset of type 2 diabetes has become a priority (see Schulz & Hu, 2005).
Given the prevalence of type 2 diabetes, intervention efforts have increasingly focused on integrated care strategies that reach large numbers of primary care patients. For example, in a recent RCT targeting type 2 diabetes and depression, integrated care managers collaborated with physicians to offer education and guideline-based treatment recommendations and to monitor adherence and clinical status. Compared to usual care, this intervention increased the percentage of patients meeting treatment goals for diabetic control (i.e., HbA1C < 7%; 61% in intervention group versus 36% in usual care) and depression (59% scoring in nondepressed range in intervention group versus 31% in usual care) (Bogner, Morales, de Vries, & Capolla, 2012).
The issue of depression in diabetes care is increasingly important. Meta-analyses have demonstrated that depression predicts the development of Type 2 diabetes (Knol et al., 2006), and depression and related psychosocial risk factors predict poor glucose control and prognosis in diabetes (Chida & Hamer, 2008). Some evidence suggests a bidirectional association between depression and diabetes (Golden et al., 2008), although in some studies self-report scales assessing emotional distress specifically related to diabetes rather than scales measuring depression are stronger predictors of impaired glucose regulation (Fisher et al., 2010). Depression is also associated with poor adherence to medical treatment regimens in diabetes (Gonzalez et al., 2008). A variety of psychosocial interventions have been found to be effective in treating depression in diabetes, although effects on metabolic control (i.e., glucose regulation) are not demonstrated consistently (Van der Feltz-Cornelis, Nuygen, et al., 2010). Despite a lack of clear effects on glucose regulation, collaborative care for depression in diabetes is cost-effective in reducing both depression and overall health care costs (Simon et al., 2007)
Although group-based patient education interventions reach more patients and have some demonstrated efficacy (Deakin, McShane, Cade, & Williams, 2005), individual approaches have been found to be more effective than group-delivered education (Sperl-Hillen et al., 2011). Utilizing available technology, patient-centered, computer-assisted self-management intervention appears effective in improving diabetes self-management outcomes and increases in perceived autonomy and competence are mechanisms of change in this approach (Williams, Lynch, & Glasgow, 2007). Beyond individually focused intervention, adding a brief, family-based intervention targeting negative and/or inaccurate illness perceptions to usual care results in improvements in HbA1C levels in patients with poorly controlled type 2 diabetes (Keogh et al., 2011). Review of trials of various dietary approaches and diet plus exercise interventions for treatment of type 2 diabetes indicated that adoption of regular exercise is a good way to promote better glycemic control (Nield et al., 2007).
The metabolic syndrome (MetS) is a collection of biomedical risk factors (i.e., elevated blood glucose/insulin resistance; elevated cholesterol and triglycerides, high blood pressure; abdominal adiposity) that although falling short of the criteria for diabetes, is a strong risk factor for the development of type 2 diabetes, as well as atherosclerotic cardiovascular disease (Eckel, Grundy, & Zimmet, 2005). Modification of diet and physical activity are mainstays of the treatment of MetS, and are effective, especially if they produce weight loss. However, maintenance is difficult (Magkos Yannakoulia, Chan, & Mantzoros, 2009). Psychosocial factors (e.g., depression, chronic stress) increase risk for MetS (Goldbacher & Matthews, 2007), but little research has examined the effects of related interventions on this “prediabetic” condition.
Introduced in 1996, highly active antiretroviral therapy (HAART) produced a marked decrease in AIDS related morbidity and mortality. As a result HIV has become much more of a chronic disease similar to others reviewed here. The related impact on psychosocial functioning has become a major focus of current care in HIV, much more so than in the pre-HAART era when acute illness issues were more central. However, the medication regimen that made this change possible is complex and demanding, with notable side effects. Even with a simplified dosing, lifelong adherence is often highly challenging, especially in light of the fact that a very high level of adherence is required to produce maximum effectiveness. Psychosocial factors such as life stress and depression can disrupt adherence to HAART (Bottonari, Safran, McQuaid, Hsiao, & Roberts, 2010; Gonzalez, Batchelder, Psaros, & Safren, 2011). One RCT of a multi-component intervention addressing barriers to adherence, supporting the patients' autonomy in meeting these challenges, and promoting social support and network involvement demonstrated important improvements in adherence (Koenig et al., 2008). In another recent RCT, CBT focused on reducing depression and improving adherence with the medical regimen had beneficial effects in both cases, both after treatment and during a prolonged follow-up period (Safren et al., 2009).
Given the serious nature of the disease and the demands of related treatment, psychosocial issues are an important focus of patient care. The ways in which individuals cope with HIV-related stressors is important. Direct action and positive reappraisal are associated with better outcomes, across emotional adjustment, health behavior, and physical symptoms and medical outcomes (Moskowitz, Hult, Bussolari, & Acree, 2009). In contrast, behavioral disengagement and coping through use of drugs and alcohol are associated with worse outcomes across domains. Hence, CBT and related interventions may be more effective to the extent that they enhance the former and reduce the latter forms of coping.
In meta-analyses of prospective studies, psychosocial factors have been found to predict the course of HIV (Chida & Vedhara, 2009), and psychobiologic mechanisms potentially contributing to these effects of chronic stress and negative emotion on the course of HIV have been described (Cole, 2008). These findings raise the question as to whether psychosocial interventions can alter the underlying immunologic condition. In some studies of persons with HIV, CBT, relaxation therapies, and other interventions (e.g., tai-chi) have been found to improve immune functioning relative to control conditions (e.g., McCain et al., 2008). However, meta-analyses have concluded that stress management has beneficial effects on emotional adjustment and H-QOL, but not immune functioning, although the latter finding is inconclusive given methodological limitations of the available studies (Scott-Sheldon, Kalichman, Carey, & Fielder, 2008). Further, the literature on stress management in HIV has been criticized as too focused on mindfulness-based approaches to the exclusion of other promising treatments, characterized by short follow-ups that raise concerns about the maintenance of treatment effects, and also a lack of specific attention to HIV-related stressors (Brown & Vanable, 2008).
The prevalence of chronic pain is estimated to be between 15% and 20% of adults in the United States and similar industrialized nations (Turk, Wilson & Cahana, 2011). Musculoskeletal pain (e.g., chronic low back pain), headache, rheumatoid and osteoarthritis, fibromyalgia, and chronic fatigue syndrome are the most common types of chronic pain problems. A growing variety of interventions have been developed to treat chronic pain (Jensen, 2011; Turk et al., 2011), and several have been evaluated in multiple RTCs. Chronic pain treatments have the obvious goal of reducing pain, but also improving levels of functional activity (versus disability), improving H-QOL, and reducing the depression that often accompanies chronic pain. Behavioral approaches emphasize the operant strategies for the reduction of reinforcement for pain behavior, the shaping of functional (i.e., “nonpain”) behavior, and graded exposure to activities that are sources of fear of further injury or pain. Cognitive-behavioral approaches address maladaptive thoughts and coping strategies (e.g., catastrophizing), whereas relaxation and stress management approaches reduce emotional and physiological arousal that can exacerbate pain. These approaches are often combined in multicomponent interventions, including comprehensive pain rehabilitation programs that combine psychosocial treatments with rehabilitation-oriented physical therapy.
In a meta-analysis of 22 studies of chronic low back pain, psychosocial treatments were found to have positive effects on pain levels, pain-related interference in daily activities, H-QOL, and depression. CBT and self-regulation approaches were found to be particularly effective, and comprehensive, multidisciplinary programs had the additional benefit of improved rates of return to work (Hoffman, Papas, Chatkoff, & Kerns, 2007). However, it is important to note that others have suggested that the conclusions of this meta-analysis should be qualified by the limitations of several of the studies included and the review processes (Coyne et al., 2010). More recently developed acceptance-based treatments (i.e., acceptance and commitment therapy, mindfulness-based stress reduction) for chronic pain have been evaluated in multiple RCTs, and a meta-analysis indicated significant, albeit small to medium effects relative to control conditions for both pain and depression (Veehof, Oskam, Scheurs, & Bohlmeijer, 2011). The benefits of these various psychosocial treatments for chronic pain demonstrated in efficacy-focused RCTs are also evident in effectiveness studies in practice settings (e.g., Morley, Williams, & Hussain, 2008). Chronic pain is often associated with poor sleep, and a preliminary RCT of CBT for insomnia among patients with chronic neck or back pain demonstrated significant improvements in sleep and the degree to which pain interfered with the patients' daily activities (Jungquist et al., 2010).
Both tension headaches and migraine headaches have been the subject of multiple RCTs, most often evaluating the effects of various forms of biofeedback, CBT, stress management, relaxation therapies, and multicomponent approaches. Quantitative and qualitative reviews indicate the effectiveness of most of these treatment modalities (Holroyd, Martin, & Nash, 2006; Nestoric & Martin, 2007; Nestoric, Rief, & Martin, 2008; Sun-Edelstein & Mauskop, 2011). These therapies are often found to be superior to comparison conditions that provide controls for nonspecific factors (D'souza, Lumley, Kraft, & Dooley, 2008). The evidence has been sufficiently compelling as to warrant the inclusion of these psychological therapies in established clinical guidelines for headache care.
A meta-analysis of psychosocial interventions for rheumatoid arthritis and osteoarthritis found significant effects on pain, emotional adjustment (i.e., reduced anxiety and depression), functional activity, and biological outcomes (i.e., joint swelling on physical exam) (Dixon, Keefe, Scipio, Perri, & Abernethy, 2007). CBT was by far the most common treatment among the available studies. A RCT found that mindfulness-based stress reduction had modest, delayed effects in improving emotional adjustment in rheumatoid arthritis but no effects on disease activity (Pradhan et al., 2007). However, another recent RCT comparing CBT, mindfulness meditation, and a patient education control for rheumatoid arthritis suggested mindfulness interventions may be useful in some contexts. Specifically, CBT was more effective than mediation and education in reducing pain and biologic evidence of systemic inflammation (i.e., IL-6 levels) (Zautra et al., 2008). However, among patients with a history of recurrent depression, mindfulness meditation was superior to CBT in reducing emotional adjustment and joint tenderness. A recent meta-analysis for psychosocial treatments for fibromyalgia indicated an overall beneficial effect on short-term reductions in pain, and somewhat larger effect on longer term reductions in pain, improved sleep, lower depression, increases in functional activity, and reduced catastrophizing (Glombiewski et al., 2010).
Although symptoms of fatigue are the primary focus in treatments of chronic fatigue syndrome, chronic pain complaints are a common and distressing clinical feature. Cognitive-behavioral stress management has been found to reduce stress, mood disturbance, and physical symptoms in chronic fatigue patients (Lopez et al., 2011), and a recent meta-analysis found that both CBT and graded physical exercise were effective, although CBT was somewhat better when chronic fatigue was accompanied by symptoms of anxiety and depression, as is common (Castell, Kazantzis, & Moss-Morris 2011).
Patients seeking treatment for chest pain are often found to be free of clinical indications of CHD. Despite the lack of evidence of serious heart disease, noncardiac chest pain remains a distressing problem. Both cognitive-behavioral coping skills training and sertraline have been found effective in reducing pain in a placebo-controlled RCT (Keefe et al., 2011). The combination of CBT and pharmacotherapy may be particularly useful, as it reduced pain, anxiety, and catastrophizing.
Other treatment-delivery modalities have been found to be useful in managing chronic pain. For example, telephone-based CBT for chronic widespread pain produced significant and sustained improvement in overall functioning (McBeth et al., 2012). A telephone-based self-management intervention also produced reductions in pain among osteoarthritis patients (Allen et al., 2010). Internet-based interventions have also been evaluated. For example, an Internet-based intervention for headache demonstrated significant reductions in headache activity (i.e., frequency, duration) and related limitations in functional activity (Devineni & Blanchard, 2005). A recent meta-analysis found overall small but significant reductions in pain for Internet-based treatments of chronic pain (Macea, Gajos, Calil, & Fregni, 2010).
Solid organ transplantation has become increasingly common in medical intervention for a variety of conditions including liver and kidney disease and cystic fibrosis (i.e., lung transplantation). Behavioral medicine issues relevant for the psychologist involved in organ transplantation programs include pretransplant assessment, adherence following transplant, prevention of alcohol and drug use, and adjustment/quality of life. Psychosocial evaluation to determine eligibility for organ transplantation typical includes psychiatric history; history and current use of alcohol, nicotine, and other substances; past and current adherence to medical regimens; cognitive capacity, especially related to understanding of post-transplant medical and self-care requirements; and social support system, especially relevant to post-transplant care (see Dew & DiMartini, 2011). The critical issues regarding eligibility vary somewhat with the specific organ. Behavioral medicine interventions that have been shown to be beneficial in patients following organ transplantation include educational-behavioral interventions to improve medication adherence (DeGeest et al., 2006), group and individual psychotherapy for reduction of depressive symptoms (Baines, Joseph, & Jindal, 2004), and mindfulness-based stress reduction (Gross et al., 2010).
Although clinical health psychologists and behavioral medicine practitioners may encounter patients with a variety of gastrointestinal disturbances, irritable bowel syndrome (IBS) is among the most prevalent. IBS is characterized by abdominal pain and abnormal bowel habits (i.e., diarrhea or constipation), as well as general physical weakness in the absence of abnormal morphological, histological, or inflammatory markers. The main diagnostic Rome III criteria, established by international professional organizations, are based on exclusion criteria and the occurrence and rate of symptoms. Because the pathophysiology and causes of IBS are poorly understood, treatment approaches are mainly focused on symptom management to maintain everyday functioning and improving quality of life for persons with IBS; thus, biopsychosocial interventions are central to disease management. The mainstay of medical intervention is pharmacological treatment with antispasmodics and antidiarrheals for diarrhea, prokinetics and high-fiber diets for constipation, and supportive therapy with low-dose antidepressants to normalize gastrointestinal motility (Grundmann & Yoon, 2010). Behavioral medicine interventions include lifestyle and dietary changes and psychotherapy. Additional alternative medicine therapies include herbal therapies and acupuncture.
In recent RCTs focused on behavioral intervention for IBS, a manualized CBT-based self-management program was effective in reducing subjective IBS symptom severity at the end of treatment (2 months), and 3 and 6 months posttreatment (Moss-Morris, McAlpine, Didsbury, & Spence, 2009). The addition of relaxation training to enhanced medical care (treatment as usual plus two counseling sessions) has resulted in significant improvement in subjective functional impairment (Lahmann et al., 2010). A small RCT demonstrated that a brief (5-week) CBT-based Internet intervention with limited therapist email resulted in significant symptom reduction and improved quality of life in IBS patients compared to a wait-list control group (Hunt, Moshier, & Milonova, 2009). Both Internet-delivered (Ljótsson et al., 2010) and in-person mindfulness group intervention (Gaylord et al., 2011) have been found to reduce IBS symptoms and improved quality of life in randomized controlled trials.
Historically, neurological disease has not been a major focus in behavioral medicine and clinical health psychology. However, recent research on multiple sclerosis (MS) indicates the considerable potential for important contributions to patient care. For example, fatigue is a common and often debilitating symptom in MS. In a RCT comparing the efficacy of CBT for fatigue, relaxation therapy, and a usual care control, van Kessel et al. (2008) found that both CBT and relaxation were beneficial, but CBT was more so. Both treatments produced sustained benefits. Depression is also common in MS, and CBT delivered via the telephone has been found to reduce depression (Mohr et al., 2005) and improve H-QOL in depressed MS patients (Cosio, Jin, Siddique, & Mohr, 2011).
Poor sleep is associated with increased health care use, work absenteeism, and reduced work productivity (Daley et al., 2009), along with a growing list of adverse health outcomes, including impaired immune functioning (Lange, Perras, Fehm, & Born, 2003), susceptibility to infectious illness (Cohen, Doyle, Alper, Janicki-Deverts, & Turner, 2009), metabolic syndrome (Hall et al., 2008; Jennings, Muldoon, Hall, Buysee, & Manuck, 2007), inflammation (Irwin et al., 2008; Mills et al., 2007), coronary artery disease (King et al., 2008), all-cause mortality (Dew et al., 2003; Gallicchio & Kalesan, 2009), as well as obesity and diabetes (see Pack & Pien, 2011). Thus, whereas insomnia is considered a mental health disorder, poor sleep generally is central to health and is, therefore, a target for intervention among clinical health psychologists and behavioral medicine practitioners. Indeed, behavioral sleep medicine is now a specific subspecialty with its own certification process from the American Board of Sleep Medicine.
To date, intervention research has largely focused on the treatment of insomnia. For many years, the treatment of choice has been cognitive behavioral therapy for insomnia (CBT-I) a multicomponent treatment that includes stimulus control, sleep restriction, sleep hygiene, paradoxical intention, relaxation therapy, and cognitive restructuring (Morin & Espie, 2003). More recently, variations and extensions of this treatment have been tested (see Bootzin & Epstein, 2011). For example, it has been shown that adding intensive sleep retraining (ISR) to stimulus control intervention results in superior treatment outcomes (Harris, Lack, Kemp, Wright, & Bootzin, 2012). ISR is a brief (25 hours in a sleep lab) behavioral conditioning intervention in which patients are awakened after a few consecutive minutes of each sleep stage, measured by electroencephalograph (EEG), thereby inducing acute sleep deprivation and repeatedly exposing patients to sleep onset.
It is important to note, however, that much of the insomnia intervention research has not focused on chronic illness. Further, research linking poor sleep to adverse health outcomes is not specific to insomnia. Thus, an important recent direction for health psychology and behavioral medicine is the improvement of sleep both as a preventive effort, as well as in the management of chronic illnesses with associated sleep difficulties. For example, CBT-I has been successfully applied to patients with comorbid osteoarthritis and insomnia resulting in improved sleep and decreased pain (Vitiello, Rybarczyk, Von Korff, & Stepanski, 2009). Exercise training has been shown to be effective in improving objective indicators of obstructive sleep apnea, as well as improvements in sleep (Kline et al., 2011). An RCT is underway to investigate the effectiveness of mindfulness-based stress management and CBT in improving sleep among cancer patients (Garland, Carlson, Antle, Samuels, & Campbell, 2011). Increasing evidence for the role of sleep and circadian rhythm disturbance in the development of mood disorders (Harvey, 2011) suggest that sleep intervention may also prove useful in treating co-occurring chronic illness and mood disorder, especially depression.
The somatoform disorders are relevant to clinical health psychology and behavioral medicine because patients with these disorders often first present in medical settings and this can have profound effects on health care service provision; relationships between physicians and patients are often strained in such cases, and the quality, cost, and outcome of medical care can suffer (see Williams, Smith, & Jordan, 2010). In the current diagnostic system, the somatoform disorders include hypochondriasis, somatization disorder, somatoform pain disorder, body dysmorphic disorder, and conversion disorder, though there will likely be changes in the future revision of the DSM. The shared focus of these diagnoses is a dysfunction in the perception of the body. Beyond the DSM, hypochondriasis and somatization disorder are included in the category of medically unexplained symptoms (Brown, 2007). Medically unexplained symptoms refer to conditions patients present to medical care that are subsequently judged as not having an identifiable physical basis. Hence, somatoform disorders are relatively extreme and persistent versions of such symptoms. Recent research has also focused on illness behavior (e.g., avoidance of physical activity) in the maintenance and chronicity of the somatoform disorders (Witthoft & Hiller, 2010).
Although there is some variation across the somatoform disorders, the most common and well-supported intervention is cognitive behavioral therapy (CBT). A CBT approach for hypochondriasis, for example, targets both inaccurate and catastrophic cognitions about the meaning of physical sensations and the amplification of symptoms. Cognitive restructuring involves the monitoring of illness-related thoughts and reappraisal of somatic experiences, and is often combined with relaxation training and desensitization (Stuart, Noyes, Starcevic, & Barski, 2008). Randomized clinical trials generally demonstrate that CBT produces reductions in symptoms of hypochondriasis and health anxiety, other types of emotional distress (e.g., anxiety, depressive symptoms), functional disability levels, and even health care utilization (e.g., Barsky & Ahern, 2004; Greeven et al., 2007). The general CBT approach produces similar benefits for patients with somatization disorder (Allen, Woolfolk, Escobar, Gara, & Hamer, 2006). Indeed, a recent review of randomized controlled trials found that the CBT model has broad applicability and effectiveness for somatoform disorders (Kroenke, 2007). Recent systematic reviews also indicate that collaborative care and mental health consultation produce improvements in patient functioning and well-being, and reductions in health care utilization and related costs (Van der Feltz-Cornelis, Van Os, Van Marwijk, & Leentjens, 2010). Effective consultations typically involve documentation of the somatoform disorder, recommendations for a conservative approach to future medical diagnostic and treatment procedures, and the use of regularly scheduled health care visits, rather than “on demand” use of medical services.
Stress management has been a long-standing, key component of clinical health psychology and behavioral medicine intervention across many health foci. However, one particular type of stress has emerged as so significant as to provoke a substantial intervention literature: caregiver stress. Individuals who care for others through chronic, debilitating illness, such as Alzheimer's disease, experience such significant stress that intervention science has begun to target this population specifically. For example, coping skills training can reduce caregiver burden (Elliott, Burgio, & DeCoster, 2010).
A prominent evidence-based intervention for caregivers of dementia patients is the Resources for Enhancing Alzheimer's Caregiver Health (REACH) II program (Belle et al., 2006). In this randomized controlled trial, caregivers received education on dementia and caregiving, skills training focused on increasing pleasant events or relaxation techniques, physical environment safety instruction, guidance and encouragement in caregiver physical self-care, skills for accessing social support, and written “behavioral prescriptions” for managing various activities of daily living (ADL) and independent ADL in patients, and common behavior problems. Results from the clinical trial showed significantly greater improvements in quality of life and depression in the intervention group. These results were true for African American, Caucasian, and Hispanic samples. The REACH II program has recently been modified for use in other contexts, with demonstrated positive effects on caregiver subjective burden, social support, caregiver frustration, depression, caregiver health, care recipient behavior problems, and mood (Burgio et al., 2009; Nichols, Martindale-Adams, Burns, Graney, & Zuber, 2011).
Another recently reported longitudinal, randomized controlled trial examined the effects of the Tailored Caregiver Assessment and Referral (TCARE®) protocol, a care management process designed to help family caregivers with care planning and assess caregiver outcomes. Caregivers in the intervention group utilized a greater number of support services, had lower stress burden, and reduced depressive symptoms than caregivers in the control group (Kwak, Montgomery, Kosloski, & Lang, 2011). A pilot randomized trial evaluated the effectiveness of a mindfulness meditation intervention in relation to two comparison groups: an education class based on Powerful Tools for Caregivers serving as an active control group and a respite-only group serving as a pragmatic control in caregivers of close relatives with dementia. Both mindfulness and education interventions decreased the self-rated caregiver stress compared to the respite-only control (Oken et al., 2010). A randomized controlled trial is underway to evaluate the effectiveness of mindfulness-based stress reduction for caregivers (Whitebird et al., 2011).
Recent research on the determinants and consequences of caregiving stress may lead to further refinements in these interventions. For example, in some cases caregiving is associated with reduced distress and improved well-being (Brown et al., 2009), raising questions regarding potential moderators of the effects of caregiving or “active ingredients” in its unhealthy effects. Some evidence suggests that witnessing suffering of loved ones, rather than caregiving, per se is unhealthy (Monin & Schulz, 2009). If supported in future research, such findings could lead to more precisely targeted interventions.
The intervention research findings reviewed here demonstrate that behavioral medicine and clinical health psychology continue to make considerable progress in the reduction of behavioral risk factors for disease, in the management of chronic medical conditions that are the leading sources of morbidity and health care expenditures, and in the management of other distressing and costly problems patients often present in medical care settings. Several issues will shape the agenda for future intervention research and the implementation of those research findings in the delivery of health services.
In earlier reviews of intervention research in behavioral medicine and clinical health psychology (e.g., Blanchard, 1994; Smith, Kendall, & Keefe, 2002) the vast majority of studies were RCTs of the efficacy of well-defined interventions for specific behavioral risk factors or medical conditions. This type of intervention research will continue to be important, in part because much of the earlier intervention research in the field did not meet the more recently articulated standards for the design, analysis and reporting of RCTs. The field has quickly evolved to meet these standards much more routinely, but the “second generation” of larger, higher quality RCTs of intervention efficacy will continue to be an essential part of the research portfolio in the field going forward.
With increasing emphasis on evidence-based practice in medical care and related aspects of health policy, this second generation of RCTs in clinical health psychology must take full advantage of various approaches to documenting the clinical significance of intervention effects. In addition to commonly reported information about effect sizes, consistent reporting of the percentage of patients with clinically meaningful improvements is important (e.g., Thieme, Turk, & Flor, 2007). For some outcomes and medical problems, this may require additional research to establish the optimal criteria for such improvements. Increasing use of common metrics across specific medical problems (e.g., quality-adjusted life years) will facilitate clinically meaningful and policy-relevant comparisons. In addition, the effects of various interventions of health care utilization and related health care costs will be increasingly important. When the endpoints of trials include outcomes that are relatively low in frequency (e.g., prevention of recurrent cardiac events among patients with CHD), multisite trials that have been rare in behavioral medicine and clinical health psychology but more common in other medical treatment research will be needed. Even though the ENRICHD trial (Berkman et al., 2003) produced null results on the primary endpoint, the experience gained by the researchers involved in the trial will be an invaluable asset in future efforts of this type.
However, other kinds of intervention studies that are familiar to psychotherapy and behavior change researchers are also needed. Person by treatment interactional or moderational designs are needed to address the important challenge of matching specific types of clinical problems and patients with specific types of treatments. Dismantling designs will be useful for identifying the critical elements within the widely used multicomponent interventions. In several cases, treatments have been evaluated with inadequate control of non-specific factors, resulting in the need for critical considerations of appropriate comparison conditions in future research (Freedland, Mohr, Davidson, & Schwartz, 2011).
A small but growing literature in behavioral medicine and clinical health psychology addresses mechanisms of change in interventions, and results to date suggest that this comparatively understudied issue is also important. For example, reductions in catastrophizing mediate therapeutic improvement not only in CBT for chronic pain, but also other forms of pain treatment that do not directly address this cognitive process (Burns, Day, & Thorn, 2012; Smeets, Vtaeyen, Kester, & Knottnerus, 2006). The quality of the therapeutic alliance predicts therapeutic outcomes in adjunctive psychological treatments for MS patients (Beckner, Vella, Howard, & Mohr, 2007; Howard, Turner, Okin, & Mohr, 2006). Also, group cohesion and rapport in group-based psychosocial treatments for cancer patients similarly predict therapeutic outcomes (Andersen, Shelby, & Golden-Kreutz, 2007; Schnur & Montgomery, 2010). Additional research on mechanisms of change and intervention processes could help refine the development and delivery of interventions, and identify key competences to be emphasized in training. To date, much of the behavioral and cognitive-behavioral intervention research in behavioral medicine and clinical health psychology has implicitly emphasized the high-fidelity delivery of manualized therapies; a broader intervention research agenda could be a very valuable addition.
As noted previously, for interventions found to be efficacious in closely controlled RCTs, research on their effectiveness when delivered in representative health care settings will be important (Glasgow, 2008; Glasgow & Emmons, 2007). Finally, research on the dissemination and uptake of evidence-based practices in health care will be an increasingly important focus in the field (Kerner et al., 2005; McHugh & Barlow, 2011). In such efforts, traditional intervention researchers may find value in collaborative efforts with health services researchers. For effectiveness and dissemination research, the RE-AIM framework as applied to health behavior change (Glasgow et al., 1999) and chronic illness management (Glasgow et al., 2001) articulates several specific research topics to address these issues.
In some emerging models, clinical health psychology and behavioral medicine services are delivered as an integral component of medical care. Rather than providing separate services in distinct settings, clinical health psychologists work in direct collaboration with other health care professionals. In these new roles, psychologists often provide both typical services for mental health problems (e.g., anxiety, depression) that patients present in those medical settings, as well as services more directly related to the medical issues (e.g., behavioral risk reduction, adjunctive treatments for chronic disease). Hence, these recent care models cross traditional boundaries between clinical and counseling psychology on the one hand, and health psychology and behavioral medicine on the other.
Much of this change and the related opportunities involve the expanding role of psychological services in primary medical care. Four formal medical specializations provide primary care (i.e., general internal medicine, family practice, pediatrics, and obstetrics-gynecology). In addition, primary medical care is provided by nurse practitioners and physician assistants who practice in collaboration with primary care physicians. Primary medical care in the United States currently faces a variety of challenges, especially problems with access and staffing, but also managing the growing burden of chronic medical illness (Bodenheimer & Phan, 2010). The concept of the patient-centered medical home is considered a valuable new model for more effective and efficient primary medical care (Landon, Gill, Antonelli, & Rich, 2010), in which team-based, coordinated care under the direction of a primary care physician is the foundation for providing both acute and chronic care, addressing the needs of the “whole person” from childhood through end-of-life issues (Strange et al., 2010).
Over the past decade, psychologists have articulated the potential value of primary medical care as a setting for the provision of psychological services, proposing the development of the new field or specialty of primary care psychology (Frank, McDaniel, Bray, & Heldring, 2004; Haas, 2004). This emerging role for psychologists fits quite well with descriptions of the patient-centered medical home (McDaniel & Fogerty, 2009). The behavioral risk reduction interventions reviewed here could routinely be delivered in this context, as could adjunctive treatments for the management of chronic illness and interventions for common psychological problems presenting in primary care (i.e., mood and anxiety disorders, insomnia, somatoform disorders). The common comorbidity of depression and chronic medical illness is a prototypical example of the need for such integrative services (Smith, 2010b). In addition to direct psychological treatment of such conditions, there is substantial evidence of improved outcomes for depression and somatoform disorders when mental health consultations are readily available (Van der Feltz-Cornelis, Van Os, et al., 2010). Hence, after emerging as distinct new fields several decades ago, clinical health psychology and behavioral medicine may be poised to become a more common element of multifaceted, comprehensive health care, in which traditional distinctions between mental health services and behavioral medicine/clinical health psychology services are blurred as they are both increasingly delivered in the context of primary medical settings.
To the extent that the patient-centered medical home does come to include the full life span, other roles are available for psychologists. For example, stress, anxiety, and low social support during pregnancy increase the risk of preterm births and low birth weight, which in turn often have negative long-term consequences for the child's emotional, social, and educational functioning (Dunkel Schetter, 2011; Lobel et al., 2008). Group-based provision of comprehensive psychosocial care for high-risk expectant mothers has been found to reduce preterm birth and low birth weight, and to improve a variety of aspects of psychosocial functioning among such women (Ickovics et al., 2007, 2011).
In terms of end-of-life care, an emerging psychosocial topic among terminal patients involves end-of-life planning discussions, which are sometimes seen as a potential stressor for patients and their families, and passively or intentionally avoided by health care providers as a result. However, such discussions are generally well tolerated by patients and their caregivers, and are associated with less aggressive medical care as patients approach death and earlier referral to hospice care (Wright et al., 2008). Less aggressive medical care, in turn, has been found to be associated with higher patient quality of life in the days and weeks preceding death, and with less emotional distress among their caregivers (Wright et al., 2008). Hence, consultation-liaison interventions surrounding these issues could be a useful element of expanded roles of clinical health psychologists in the patient-centered medical home. Similarly, bereavement is normal, but it does pose a health risk (Stroebe, Schut, & Stroebe, 2007). Although psychological interventions have no demonstrable beneficial effects in cases of normal bereavement (Stroebe, Schut, & Stroebe, 2005), a meta-analysis demonstrated that bereavement therapy was useful for people with more severe and prolonged reactions (Currier, Neimeyer, & Berman, 2008). Hence, primary care psychology as a component of the patient-centered medical home has the potential to make useful additions to care across the life span. The possibilities for integration of psychology in primary medical care are increasingly recognized as important challenges and opportunities for a broad range of psychological researchers and service providers (Bray, 2010; Goodheart, 2011). As psychologists transition into these roles, issues of the general and unique training needs for this interdisciplinary environment will require further attention (France et al., 2008), as will the empirical evaluation of the effects of various training models for psychologists on health services outcomes.
In health behavior change and chronic illness management, research has at least initially demonstrated the value of a range of options for delivery of behavioral interventions, from traditional one-on-one and small group approaches, to interactive computer and telephone delivery, to alterations in health system practices (Glasgow et al., 2001). Telephone and Internet-delivery models can be useful in meeting the needs of rural populations with limited access to behavioral health professionals, as well as the needs of patients whose chronic medical conditions pose mobility and transportation challenges. Examples of the efficacy of telephone interventions include challenging and specialized populations such as MS patients (Mohr, Hart, & Vella, 2007) and transplant candidates (Blumenthal et al., 2006). Computer-based interventions have been developed and evaluated in an even greater variety of applications (for reviews, see Bennett & Glasgow, 2009; Strecher, 2007), including CBT for gastrointestinal conditions (Hunt et al., 2009), management of diabetes (Glasgow et al., 2005), and bereavement support (van der Houwen, Schut, van den Bout, Stroebe, & Stroebe, 2010). Telephone interventions have the potential to address many problems with health care access, but still require real-time availability of health care providers. In contrast, computer-based approaches also can address access problems, but also have tremendous potential as large-scale interventions that can have important effects on population levels of behavior change and chronic illness management due to the their dramatically greater reach. In this way, computer-based interventions can be a “first step of choice” in stepped care approaches to many specific problems.
In the United States and other industrialized nations, increasing ethnic and racial diversity poses a variety of challenges. In terms of the leading sources of morbidity and mortality, several ethnic and racial minority groups are at increased risk of CVD, for example. They often have increased levels of modifiable risk factors, yet are underserved in terms of various prevention resources (Stuart-Shor, Berra, Kamau, & Kumanyika, 2012). Racial and ethnic minority status is an essential aspect of external validity considerations in effectiveness research. There is also a great need for culturally and linguistically tailored community-based interventions. Initial efforts in culturally enhanced or tailored health behavior change interventions indicate major potential benefits (Barrera, Castro, Strycker, & Tolbert, 2012).
In many industrialized nations, the average age of the population is increasing. Chronic illness is more prevalent among older adults, as are the related burdens. Hence, health behavior change and chronic disease management will increasingly need to incorporate the concepts, methods, and knowledge base from adult development and aging research (Aldwin, Park, & Spiro, 2007). However, some chronic diseases of middle and later adulthood, such as CHD, often have their beginnings in pathophysiological changes evident in childhood and adolescence (Charakida, Deanfield, & Halcox, 2009). Further, the health behaviors (e.g., excessive dietary intake of calories and saturated fat, physical inactivity, smoking) that are major sources of these same chronic diseases among middle-aged and older adults are first apparent—and most easily modified—in childhood and adolescence (Wilson, St. George, & Zarrett, 2010). Similarly, exposure to psychosocial stressors during childhood and adolescence (e.g., low childhood SES, severe family stressors) can influence risk for chronic diseases of aging (Cohen, Janicki-Deverts, Chen, & Matthews, 2010; Miller, Chen, & Parker, 2011). Thus, it is possible that health behavior and psychosocial risk reduction efforts for the prevention of adult chronic disease could usefully incorporate a broader set of child and adolescent prevention approaches (Smith, Orleans, & Jenkins, 2004).
In the United States, the Department of Health and Human Services has sponsored the development and revision of the Healthy People initiatives for the past three decades, the most recent version being Healthy People 2020. The overarching goals of the initiative and the foundation health measures that are tracked to evaluate progress include not only longer lives and a reduction in preventable causes of death, but also higher quality lives free of limitations in functional activity and threats to well-being, broadly but specifically defined (see www.healthypeople.gov/2020/topicsobjectives2020). These goals and progress benchmarks make clear that the perspectives and approaches of behavioral medicine and health psychology converge closely with national priorities for the foreseeable future.
The primary current health challenges for more and less developed countries differ, with nonindustrialized nations facing greater relative overall burdens and death rates from perinatal conditions (i.e., prematurity, birth trauma, infections) and various infectious diseases (e.g., lower respiratory infections, tuberculosis, HIV/AIDS), compared to the proportionally greater burdens and death rates associated with cardiovascular disease (i.e., ischemic heart disease and cerebrovascular disease) and cancer in industrialized nations (Oldenburg, de Courten, & Frean, 20102010). However, projections suggest a trend toward convergence over the next 25 to 30 years, in which the burden of perinatal and infections disease other than HIV/AIDS falls worldwide while deaths and overall burdens from cardiovascular disease, tobacco-related conditions, obesity related conditions, and HIV/AIDS rise (Mathers & Loncar, 2006). These trends suggest that across the globe the current prevention perspective in health psychology and behavioral medicine focusing on smoking, diet, physical activity, and sexually transmitted infections will only increase in importance, as will the need for psychosocial adjunctive treatments for cardiovascular and other chronic conditions. Hence, within the industrialized nations—and increasingly beyond them—the need for research and intervention services in health psychology and behavioral medicine is likely to grow.
In the years since the last edition of this handbook, intervention research in behavioral medicine and clinical health psychology has expanded considerably—increasing not only in amount, but also in quality and the range of applications. Yet, during the same period, the standards for intervention research have been raised substantially, to the point where the status of the evidence base is promising but quite modest in some areas (Oldenburg, Absetz, et al., 2010). This underscores the need for continued efforts in methodologically rigorous RCTs and systematic reviews, but with an even greater emphasis on the degree of clinically meaningful change, broadly comparable outcome metrics, and effects on health care utilization and costs. However, there is also a need for an expanded view of intervention research that includes a greater investment in research on effectiveness, applications to diverse populations and health disparities, intervention process and mechanisms of change, dissemination, and implementation. Behavioral medicine and health psychology have always been multidisciplinary endeavors; this expanded intervention research agenda seems to require additional partnerships in health services research, health care policy, and other areas.
At a time when health care costs in the United States and elsewhere are rising to levels that pose unsustainable economic burdens, health psychology, and behavioral medicine face both daunting challenges and major opportunities in the prevention and management of disease, by contributing to more effective and efficient medical care. These challenges and opportunities lie in two distinct areas. The first challenges involve a growing divergence in its focus on two very different forms of intervention and intervention research. Research and applications in behavioral medicine and health psychology must retain and enhance its active focus on traditional clinical models of individual and small-group based approaches, because these interventions have the potential to provide improved care and much needed reductions in health care spending (Belar & Deardooff, 2009). However, intervention research must also continue to address the challenges posed by the need for much broader population-based approaches that dramatically extend the reach of evidence based interventions for health behavior change and the management of chronic illness, with even greater possibilities for efficiencies in care. This growing divergence of intervention missions has the potential to alter traditional conceptualizations of the structure of the field, as it becomes more closely related to public health on the one hand, and more closely linked to an expanded multidisciplinary approach to clinical health care, on the other.
In the second challenge, research and applications regarding the more traditional individual and small group approaches in behavioral medicine and clinical health psychology must address the rapidly changing economic, policy, and practice environment in health care. If behavioral medicine and clinical health psychology can firmly establish a substantial role in evolving systems of primary medical care while maintaining their more long-standing role in some specialized medical applications (e.g., pain treatment, oncology), their place among the intervention sciences and health care professions will continue to grow and evolve.
Abraham, C., & Graham-Rower, E. (2009). Are worksite interventions effective in increasing physical activity? A systematic review and meta-analysis. Health Psychology Review, 3, 108–144.
Abrams, D. B., Orleans, C. T., Niaura, R., Goldstein, M., Prochaska, J., & Velicer, W. (1996). Integrating individual and public health perspectives for treatment of tobacco dependence under managed care. A combined stepped care and matching model. Annals of Behavioral Medicine, 18, 290–304.
Agboola, S., McNeill, A., Coleman, T., & Bee, J. L. (2010). A systematic review of the effectiveness of smoking relapse prevention interventions for abstinent smokers. Addiction, 105, 1362–1380.
Akechi, T., Okuyama, T., Onishi, J., Morita, T., & Furukawa, T. A. (2008). Psychotherapy for depression among incurable cancer patients. Cochrane Database of Systematic Reviews (2), CD005537.
Aldwin, C. M., Park, C. L., & Spiro, A. (Eds). (2007). Handbook of health psychology and aging. New York, NY: Guilford Press.
Allen, K. D., Oddone, E. Z., Coffman, C. J., Datta, S. K., Juntilla, K. A., Lindquist, J. H.,…Bosworth, H. B. (2010). Telephone-based self-management of osteoarthritis: A randomized trial. Annals of Internal Medicine, 153, 570–579.
Allen, L. A., Woolfolk, R. L., Escobar, J. I., Gara, M. A., & Hamer, R. M. (2006). Cognitive-behavioral therapy for somatization disorder: A randomized controlled trial. Archives of Internal Medicine, 166, 1512–1518.
Altman, D. G., Schulz, K. F., Moher, D., Egger, D., Davidoff, F., & Elbourne, D. (2001). The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Annals of Internal Medicine, 134, 663–694.
Alwan, A., MacLean, D. R., Riley, L. M., d'Espaignet, E. T., Mathers, C. D., Stevens, G. A., & Bettcher, D. (2010). Monitoring and surveillance of chronic non-communicable diseases: Progress and capacity in high-burden countries. Lancet, 376, 1861–1868.
Andersen, B. L., Farrar, W. B., Golden-Kreutz, D. M., Glaser, R., Emery, C. F., Crespin, T. R.,…Carson, W. E. (2004). Psychological, behavioral, and immune changes after a psychological intervention: A clinical trial. Journal of Clinical Oncology, 22, 3570–3580.
Andersen, B. L., Shelby, R. A., & Golden-Kreutz, D. M. (2007). RCT of a psychological intervention for patients with cancer: I. Mechanisms of change. Journal of Consulting and Clinical Psychology, 75, 927–938. doi: 10.1037/0022–006X.75.6.927
Andersen, B. L., Yang, H., Farrar, W., Golden-Kreutz, D., Emery, C., Thornton, L.,…Carson, W. (2008). Psychologic intervention improves survival for breast cancer patients: A randomized clinical trial. Cancer, 113, 3450 3458.
Anderson, L., Quinn, T., Glanz, K., Ramirez, G., Kahwati, L., Johnson, D. B.,…Katz, D. L. (2009). The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity. American Journal of Preventive Medicine, 37, 340–357.
Antoni, M. H., Lechner, S., Diaz, A., Vargas, S., Holley, H., Phillips, K.,…Blomberg, B. (2009). Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain, Behavior, and Immunity, 23, 580–591.
Antoni, M., Lutgendorf, S. K., Blomberg, B., Carver, C. S., Lechner, S., Diaz, A.…Cole, S. W. (2012). Cognitive-behavioral stress management reverses anxiety-related leukocyte transcriptional dynamics. Biological Psychiatry, 71, 366–372.
Antoni, M. H., Lutgendorf, S., Cole, S., Dhabhar, F., Sephton, S., McDonald, P.,…Sood, A. (2006). The influence of biobehavioral factors on tumor biology: Pathways and mechanisms. Nature Reviews Cancer, 6, 240–248.
Appel, L. J., Brands, M. W., Daniels, S. R., Karanja, N., Elmer, P. J., & Sacks, F. (2006). Dietary approaches to prevent and treat hypertension. Hypertension, 47, 296–308.
Appel, L. J., Clark, J. M., Yeh, H. C., Wang, N. Y., Coughlin, J. W., Daumit, G.,…Brancati, F. L. (2011). Comparative effectiveness of weight-loss interventions in clinical practice. New England Journal of Medicine, 365, 1959–1968.
Armitage, C. J. (2009). Is there utility in the transtheoretical model? British Journal of Health Psychology, 14, 195–210.
Armstrong, M. J., Mottershead, T. A., Ronksley, P. E., Sigal, R. J., Campbell, T. S., & Hemmelgarn, B. R. (2011). Motivational interviewing to improve weight loss in overweight and/or obese patients: A systematic review and meta-analysis of randomized controlled trials. Obesity Reviews, 12, 709–723.
Atlantis, E., & Baker, M. (2008). Obesity effects on depression: Systematic review of epidemiological studies. International Journal of Obesity, 32, 881–891.
Aubin, H., Rollema, H., Svensson, T., & Winterer, G. (2012). Smoking, quitting, and psychiatric disease. A review. Neuroscience and Biobehavioral Reviews, 36, 271–284.
Aveyard, P., Massey, L., Parsons, A., Manasek, S., & Griffin, C. (2009). The effect of transtheoretical model based interventions on smoking cessation. Social Science and Medicine, 68, 397–403.
Baines, L. S., Joseph, J. T., & Jindal, R. M. (2004). Prospective randomized study of individual and group psychotherapy versus controls in recipients of renal transplants. Kidney International, 65, 1937–1942.
Baker, T. B., Mermelstein, R., Collins, L. M., Piper, M. E., Jorenby, D. E., Smith, S. S.,…Fiore, M. C. (2011). New methods for tobacco dependence treatment research. Annals of Behavioral Medicine, 41, 192–207.
Baldwin, A. S., Kellerman, Q. D., & Christensen, A. J. (2010). Coping with chronic illness. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds.), Handbook of health psychology and behavioral medicine (pp. 494–507). New York, NY: Guilford Press.
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavior change. Psychological Review, 84, 191–215.
Baroletti, S., & Dell'Orfano, H. (2010). Medication adherence in cardiovascular disease. Circulation, 121, 1455–1455.
Barrera Jr., M., Castro, F. G., Stryker, L. A., & Tolbert, D. J. (2012). Cultural adaptations of Behavioral health interventions: A progress report. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0027085
Barsky, A. J., & Ahern, D. K. (2004). Cognitive behavior therapy for hypochondriasis: A randomized controlled trial. Journal of the American Medical Association, 291, 1464–1470.
Barth, J., Critchley, J., & Bengel, J. (2008). Psychosocial interventions for smoking cessation in patients with coronary heart disease. Cochrane Database of Systematic Reviews (1), CD006886.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders. New York, NY: International Universities Press.
Beckner, V., Vella, L., Howard, I., & Mohr, D. C. (2007). Alliance in two telephone-administered treatments: Relationship with depression and health outcomes. Journal of Consulting and Clinical Psychology, 75, 508–512.
Belar, C. D., & Deardorff, W. W. (2009). Clinical health psychology in medical settings: A practitioner's guidebook (2nd ed). Washington, DC: American Psychological Association.
Belle, S. H., Burgio, L., Burns, R., Coon, D., Czaja, S. J., & Gallagher-Thompson, D. (2006). Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: A randomized, controlled trial. Annals of Internal Medicine, 145, 727–738
Bennett, G. G., & Glasgow, R. E. (2009). The delivery of public health interventions via the Internet: Actualizing their potential. Annual Review of Public Health, 30, 273–292.
Bennett, G. G., Herring, S. J., Puleo, E., Stein, E. K., Emmons, K. M., & Gillman, M. W. (2010). Web-based weight loss in primary care: A randomized controlled trial. Obesity, 18, 308–313.
Berkman, L. F., Blumenthal, J., Burg, M., Carney, R. M., Catellier, D., Cowan, M. J., …Schneiderman, N. (2003). Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. Journal of the American Medical Association, 289, 3106–3116.
Bhattacharyya, M. R., & Steptoe, A. (2007). Emotional triggers of acute coronary syndromes: Strength of evidence, biological processes, and clinical implications. Progress in Cardiovascular Disease, 49, 353–365.
Blanchard, E. B. (1994). Behavioral medicine and health psychology. In A. E. Bergin & S. L. Garfield (Eds.), Handbook of psychotherapy and behavior change (4th ed., pp. 701–733). New York, NY: Wiley.
Blumenthal, J. A. (2011). New frontiers in cardiovascular behavioral medicine: Comparative effectiveness of exercise and medication in treating depression. Cleveland Clinic Journal of Medicine, 78, s35–s43.
Blumenthal, J. A., Babyak, M. A., Hinderliter, A., Watkins, L., Craighead, L., Caccia, C., …Sherwood, A. (2010). Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: The ENCORE study. Archives of Internal Medicine, 170, 126–135.
Blumenthal, J. A., Babyak, M., Keefe, F. J., Davis, R. D., Lacaille, R. A., Carney, R.,…Palmer, S. M. (2006). Telephone-based coping skills training for patients awaiting lung transplantation. Journal of Consulting and Clinical Psychology, 74, 535–544.
Blumenthal, J. A., Babyak, M. A., Sherwood, A., Craighead, L., Lin, P. H., Johnson, J.,…Hinderliter, A. (2010). Effects of the dietary approach to stop hypertension diet alone and in combination with exercise and caloric restriction on insulin sensitivity and lipids. Hypertension, 55, 1199–1205.
Blumenthal, J. A., Sherwood, A., Babyak, M., Watkins, L., Waugh, R., Georgiades, A.,…Hinderliter, A. (2005). Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart diseases: A randomized controlled trial. JAMA, 293, 1626–1634.
Bodenheimer, T., & Pham, H. H. (2010). Primary care: current problems and proposed solutions. Health Affairs, 29, 799–805.
Bogers R. P., Bemelmans, W. J., Hoogenveen, R. T., Boshuizen, H. C., Woodward, M., Knekt, P., …Shipley, M. J., for the BMI-CHD Collaboration Investigators. (2007). Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: A meta-analysis of 21 cohort studies including more than 300,000 persons. Archives of Internal Medicine, 167, 1720–1728.
Bogner, H. R., Morales, K. H., de Vries, H. F., & Cappola, A. R. (2012). Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: A randomized controlled trial. Annals of Family Medicine, 10, 15–22.
Bolan, B., West, R., & Gunnell, D. (2011). Does smoking cessation cause depression and anxiety? Findings from the ATTEMPT cohort. Nicotine and Tobacco Research, 13, 209–214.
Bootzin, R. R., & Epstein, D. R. (2011). Understanding and treating insomnia. Annual Review of Clinical Psychology, 7, 435–458.
Bottonari, K. A., Safren, S. A., McQuaid, J. R., Hsiao, C. B., & Roberts, J. E. (2010). A longitudinal investigation of the impact of life stress on HIV treatment adherence. Journal of Behavioral Medicine, 33, 486–495.
Brandon, T. H., Vidrine, J. I., & Litvin, E. B. (2007). Relapse and relapse prevention. Annual Review of Clinical Psychology, 3, 257–284.
Bray, J. H. (2010). The future of psychology practice and science. American Psychologist, 65, 355–369.
Brennan, L., Castro, S., Brownson, R. C., Claus, J., & Orleans, C. T. (2011). Accelerating evidence reviews and broadening evidence standards to identify effective, promising, and emerging policy and environmental strategies for prevention of childhood obesity. Annual Review of Public Health, 32, 199–223.
Bricker, J. B. (2010). Theory-based behavioral interventions for smoking cessation: Efficacy, processes, and future directions. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds.), Handbook of health psychology and behavioral medicine (pp. 544–566). New York, NY: Guilford Press.
Brown, J. L., & Vanable, P. A. (2008). Cognitive–behavioral stress management interventions for persons living with HIV: A review and critique of the literature. Annals of Behavioral Medicine, 35, 26–40.
Brown, R. J. (2007). Introduction to the special issue on medically unexplained symptoms: Background and future directions. Clinical Psychology Review, 27, 769–780.
Brown, S. L., Smith, D. M., Schulz, R., Kabeto, M. U., Ubel, P. A., Poulin, M.,…Langa, K. M. (2009). Caregiving behavior is associated with decreased mortality risk. Psychological Science, 20, 488–494.
Brownson, R. C., Boehmer, T. K., & Luke, D. A. (2005). Declining rates of physical activity in the United States: What are the contributors? Annual Review of Public Health, 26, 421–443.
Brownson, R. C., Haire-Joshu, D., & Luke, D. A. (2006). Shaping the context of health: A review of environmental and policy approaches in the prevention of chronic disease. Annual Review of Public Health, 27, 341–370.
Burgio, L. D., Collins, I. B., Schmid, B., Wharton, T., McCallum, D., & Decoster, J. (2009). Translating the REACH caregiver intervention for use by area agency on aging personnel: The REACH OUT program. Gerontologist, 49, 103–116.
Burns, J. W., Day, M. A., & Thorn, B. E. (2012). Is reduction of pain catastrophizing a therapeutic mechanism specific to cognitive-behavioral therapy for chronic pain? Translational Behavioral Medicine. doi: 10.1007/s13142–011–0086–3
Butryn, M. L., Webb, V., & Wadden, T. A. (2011). Behavioral treatment of obesity. Psychiatric Clinics of North America, 34, 841–859.
Byers, T. (2010). Two decades of declining cancer mortality: Progress with disparity. Annual Review of Public Health, 31, 121–132.
Campbell, M. K., Hudson, M. A., Resnicow, K., Blakeney, N., Paxton, A., & Baskin, M. (2007). Church-based health promotion interventions: Evidence and lessons learned. Annual Review of Public Health, 28, 213–234.
Caplan, B. (2010). Rehabilitation psychology and neuropsychology with stroke survivors. In R. G. Frank, M. Rosenthal., & B. Caplan (Eds.), Handbook of rehabilitation psychology (2nd ed., pp. 63–94). Washington, DC: American Psychological Association.
Carrel, A. L., Clark, R. R., Peterson, S. E., Nemeth, B. A., Sullivan, J., & Allen, D. B. (2005). Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: A randomized, controlled study. Archives of Pediatric and Adolescent Medicine, 159, 963–968.
Carrel, A. L., Clark, R. R., Peterson, S. E., Eichhoff, J., & Allen, D. B. (2007). School-based fitness changes are lost during summer vacation. Archives of Pediatric and Adolescent Medicine, 161, 561–564.
Casey, E., Hughes, J. W., Waechter, D., Josephson, R., & Rosneck, J. (2008). Depression predicts failure to complete phase-II cardiac rehabilitation. Journal of Behavioral Medicine, 31, 421–431.
Castell, B. D., Kazantzis, N., & Moss-Morris, R. E. (2011). Cognitive-behavioral therapy and graded exercise for chronic fatigue syndrome: A meta-analysis. Clinical Psychology: Science and Practice, 18, 311–324.
Charakida, M., Deanfield, J. E., & Halcox, P. J. (2009). Childhood origins of arterial disease. Current Opinion in Pediatrics, 19, 538–545.
Chida, Y., & Hamer, M. (2008). An association of adverse psychosocial factors with diabetes mellitus: A meta-analytic review of longitudinal cohort studies. Diabetologia, 51, 2168–2178.
Chida, Y., Hamer, M., Wardle, J., & Steptoe, A. (2008). Do stress-related psychosocial factors contribute to cancer incidence and survival? Nature Clinical Practice: Oncology, 5, 466–475.
Chida, Y., & Steptoe, A. (2009). The association of anger and hostility with future coronary heart disease: A meta-analytic review of prospective evidence. Journal of the American College of Cardiology, 53, 774–778.
Chida, Y., & Vedhara, K. (2009). Adverse psychosocial factors predict poorer prognosis in HIV disease: A meta-analytic review of prospective investigations. Brain, Behavior, and Immunity, 23, 434–445.
Chow, C. K., Jolly, S., Rao-Melacini, P., Fox, K. A., Anand, S. S., & Yusuf, S. (2010). Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation, 121, 750–758.
Cohen, F., & Lazarus, R. S. (1979). Coping with the stress of illness. In G. C. Stone, F. Cohen, & N. E. Adler (Eds.), Health psychology (pp. 217–254). San Francisco, CA: Jossey-Bass.
Cohen, S. Doyle, W. J., Alper, C. M., Janicki-Deverts, D., & Turner, R. B. (2009). Sleep habits and susceptibility to the common cold. Archives of Internal Medicine, 169, 62–67.
Cohen, S., Janicki-Deverts, Chen, E., & Matthews, K. A. (2010). Childhood socioeconomic status and adult health. Annals of the New York Academy of Science, 1186, 37–55.
Cole, S. W., (2008). Psychosocial influences on HIV-1 disease progression: Neural, endocrine, and virologic mechanisms. Psychosomatic Medicine, Special Issue: Psychosocial Influences in HIV/AIDS, 70, 562–568.
Conn, V. S. (2010). Depressive symptom outcomes of physical activity interventions: Meta-analytic findings. Annals of Behavioral Medicine, 39, 128–138.
Cosio, D., Jin, L., Siddique, J., & Mohr, D. C. (2011). The effect of telephone-dministered cognitive-behavioral therapy on quality of life among patients with multiple sclerosis. Annals of Behavioral Medicine, 41, 227–234.
Cowie, C. C., Rust, K. F., Byrd-Holt, D. D., Gregg, E. W., Ford, E. S., Geiss, L. S.,…Fradkin, J. E. (2010). Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988–2006. Diabetes Care, 33, 562–568.
Coyne, J. C., Lepore, S. J., & Palmer, S. C. (2006). Efficay of psychosocial interventions in cancer care: Evidence is weaker that it first looks. Annals of Behavioral Medicine, 32, 104–110.
Coyne, J. C., Stefanek, M., & Palmer, S. C. (2007). Psychotherapy and survival in cancer: The conflict between hope and evidence. Psychological Bulletin, 133, 367–394.
Coyne, J. C., Thombs, B. D., & Hagedorrn, M. (2010). Ain't necessarily so: Review and critique of behavioral medicine interventions in health psychology. Health Psychology, 29, 107–116.
Cramer, J., Benedict, A., Muszbek, N., Keskinaslan, A., & Khan, Z. (2008). The significance of compliance and persistence in the treatment of diabetes, hypertension, and dyslipidaemia: A review. International Journal of Clinical Practice, 63, 76–87.
Cramp, F., & Daniel, J. (2008). Exercise for the management of cancer-related fatigue in adults. Cochrane Database of Systematic Reviews (2), CD006145.
Creer, T. L., Holroyd, K. A., Glasgow, R. E., & Smith, T. W. (2004). Health psychology. In M. J. Lambert (Ed.), Bergin and Garfield's handbook of psychotherapy and behavior change (5th ed., pp. 697–742). Hoboken, NJ: Wiley.
Crepaz, N., Marshall, K. J., Aupont, L. W., Jacobs, E. D., Mizuno, Y., Kay, L. S.,…O'Leary, A. (2009). The efficacy of HIV/STI behavioral interventions for African American females in the United States: A meta-analysis. American Journal of Public Health, 99, 2069–2078.
Cummings, K. M., Fong, G. T., & Borland, R. (2009). Environmental influences on tobacco use: Evidence from societal and community influences on tobacco use and dependence. Annual Review of Clinical Psychology, 5, 433–458.
Currier, J. M., Neimeyer, R. A., & Berman, J. S. (2008). The effectiveness of psychotherapeutic interventions for bereaved persons: A comprehensive quantitative review. Psychological Bulletin, 134, 648–661.
Curry, S. J., Keller, P. A., Orleans, C. T., & Fiore, M. C. (2008). The role of health care systems in increased tobacco cessation. Annual Review of Public Health, 29, 411–418.
Daley, M., Morin, C. M., LeBlanc, M., Gregoire, J. P., Savard, J., & Ballargeon, L. (2009). Insomnia and its relationship to health-care utilization, work, absenteeism, productivity and accidents. Sleep Medicine, 10, 427–438.
Davidson, K. W., Gidron, Y., Mostofsky, E., & Trudeau, K. J. (2007). Hospitalization cost offset of a hostility intervention for coronary heart disease patients. Journal of Consulting and Clinical Psychology, 75, 657–662.
Davidson, K. W., Goldstein, M., Kaplan, R. M., Kaufman, P. G., Knatterud, G. L., Orleans, C. T., …Whitlock, E. P. (2003). Evidence-based behavioral medicine: What is it and how do we achieve it? Annals of Behavioral Medicine, 26, 161–171.
Davidson, K. W., Rieckman, N., Clemow, L., Schwartz, J. E., Shimbo, D., Medina, V.,…Burg, M. M. (2010). Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms: Coronary psychosocial evaluation studies randomized controlled trial. Archives of Internal Medicine, 170, 600–608.
Davidson, K. W., Trudeau, K. J., Ockene, J. K., Orleans, C. T., & Kaplan, R. M. (2004). A Primer on current evidence-based review systems and their implications for behavioral medicine. Annals of Behavioral Medicine, 28, 226–238.
Deakin, T., McShane, C. E., Cade, J. E., & Williams, R. D. (2005). Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews, CD003417.
DeGeest, S., Schafer-Keller, P., Denhaerynck, K., Thannberger, N., Köfer, S., Bock, A.,…Steiger, J. (2006). Supporting medication adherence in renal transplantation (SMART): A pilot RCT to improve adherence to immunosuppressive regimens. Clinical Transplantation, 20, 359–368.
Devineni, T., & Blanchard, E. B. (2005). A randomized controlled trial of an internet-based treatment for chronic headache. Behaviour Research & Therapy, 43, 277–293.
De Vogli, R., Chandola, T., & Marmot, M. G. (2007). Negative aspects of close relationships and heart disease. Archives of Internal Medicine, 167, 1951–1957.
Dew, M. A., & DiMartini, A. F. (2011). Transplantation. In H. S. Friedman (Ed.), The Oxford handbook of health psychology (pp. 522–559). New York, NY: Oxford University Press.
Dew, M. A., Hoch, C. C., Buysse, D. J., Monk, T. H., Begley, A. E., Houck, P. R.,…Reynolds III, C. F. (2003). Healthy older adults' sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosomatic Medicine, 65, 63–73.
Diabetes Prevention Program Research Group. (2002). Reduction of the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine, 346, 393–403.
Diez Roux, A. V., & Mair, C. (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186, 125–145.
Dickinson, H., Campbell, F., Beyer, F., Nicholson, D., Cook, J., Ford, G., & Mason, J. (2008). Relaxation therapies for the management of primary hypertension in adults: A Cochrane review. Journal of Human Hypertension, 22, 809–820.
Dixon, K. E., Keefe, F. J., Scipio, C. D., Perri, L. M., & Abernethy, A. P. (2007). Psychological interventions for arthritis pain management in adults: A meta-analysis. Health Psychology, 26, 241–250.
D'souza, P. J., Lumley, M. A., Kraft, C. A., & Dooley, J. A. (2008). Relaxation training and written emotional disclosure for tension or migraine headaches: A randomized, controlled trial. Annals of Behavioral Medicine, 36, 21–32.
Dunkel Schetter, C. (2011). Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology, 62, 531–558.
Eckel, R. H., Grundy, S. M., & Zimmet, P. Z. (2005). The metabolic syndrome. Lancet, 365, 1145–1128.
Edwards, A. G. K., Hulbert-Williams, N., & Neal, R. D. (2008). Psychological interventions for women with metastatic breast cancer. Cochrane Database of Systematic Reviews (3), CD004253.
Eller, N. H., Netterstrom, B., Gyntelberg, F., Kristensen, T., Nielsen, F., Steptoe, A., & Theorell, T. (2009). Work-related psychosocial factors and the development of ischemic heart disease: A systematic review. Cardiology Reviews, 17, 83–97.
Elliott, A. F., Burgio, L. D., & DeCoster, J. (2010). Enhancing caregiver health: Findings from the resources for enhancing Alzheimer's caregiver health II intervention. Journal of the American Geriatrics Society, 58, 30–37.
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196, 129–136.
Engel, G. L. (1980). The clinical application of the biopsychosocial model. American Journal of Psychiatry, 137, 535–544.
Epstein, L. H., Paluch, R. A., Roemmich, J. N., & Beecher, M. D. (2007). Family-based treatment, then and now: Twenty-five years of pediatric obesity treatment. Health Psychology, 26, 381–391.
Everson-Rose, S. A., & Clark, C. J. (2010). Assessment of psychosocial factors in population studies. In A. Steptoe (Ed.), Handbook of behavioral medicine: Methods and applications (pp. 291–306). New York, NY: Springer.
Fabricatore, A. N., & Wadden, T. A. (2006). Obesity. Annual Review of Clinical Psychology, 2, 357–377.
Fabricatore, A. N., Wadden, T. A., Moore, R. H., Butryn, M. L., Heymsfield, S. B., & Nguyen, A. M. (2009). Predictors of attrition and weight loss success: Results from a randomized controlled trial. Behaviour Research and Therapy, 47, 685–691.
Fawzy, F. I., Fawzy, N. W., Hyun, C. S., Elashoff, R., Guthrie, D., Fahey, J. L., & Morton, D. L. (1993). Malignant melanoma: Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Archives of General Psychiatry, 50, 681–689.
Fiore, M. C., & Baker, T. B. (2011). Treating smokers in health care settings. New England Journal of Medicine, 365, 1222–1231.
Fiore, M. C., Jaen, C. R., Baker, T. B., Bailey, W., Benowitz, N., Curry, S.,…Wewers, M. (2008). Treating tobacco use and dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services.
Fisher, E. B., Fitzgibbons, M. L., Glasgow, R. E., Haire-Joshu, D., Hayman, L. L., Kaplan, R. M., …Okene, J. K. (2011). Behavior matters. American Journal of Preventive Medicine, 40(5), e15–e30.
Fisher, L., Mullan, J. T., Arean, P., Glasgow, R. E., Hessler, D., & Masharani, U. (2010). Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care, 33, 23–28.
Flegal, K. M., Carroll, M. D., Kit, B. D., & Ogden, C. L. (2012). Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA, 307, 491–497.
Flegal, K. M., Carroll, M. D., Ogden, C. L., & Curtin, L. R. (2010). Prevalence and trends in obesity among US adults, 1999–2008. JAMA, 303, 235–241.
Ford, E. S., & Capewell, S. (2011). Proportion of the decline in cardiovascular disease mortality due to prevention versus treatment: Public health versus clinical care. Annual Review of Public Health, 32, 5–22.
France, C. R., Masters, K. S., Belar, C. D., Kerns, R. D., Klonoff, E. A., Larkin, K. T.,…Thorn, B. E. (2008). Application of the competency model to clinical health psychology. Professional Psychology: Research and Practice, 39, 573–580.
Frank, R. G., McDaniel, S. H., Bray, J. H., & Heldring, M. (Eds.). (2004). Primary care psychology. Washington, DC: American Psychological Association.
Freedland, K. E., Mohr, D. C., Davidson, K. W., & Schwartz, J. E. (2011). Usual and unusual care: Existing practice control groups in randomized controlled trials of behavioral interventions. Psychosomatic Medicine, 73, 323–325.
Freedland, K. E., Skala, J. A., Carney, R. M., Rubin, E. H., Lustman, P. J., Davila-Roman, V. G., …Hogue, C. W. (2009). Treatment of depression after coronary artery bypass surgery: A randomized controlled trial. Archives of General Psychiatry, 66, 387–396.
Friedman, M., Thoreson, C. E., Gill, J. J., Ulmer, D., Powell, L. H., Price, V.,…Dixon, T. (1986). Alteration of type A behavior and its effects on cardiac recurrences in post myocardial infarction patients: Summary of results of the recurrent coronary prevention project. American Heart Journal, 112, 653–665.
Fung, T. T., Chiuve, S. E., McCullough, M. L., Rexrode, K. M., Logroscino, G., & Hu, F. B. (2008). Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Archives of Internal Medicine, 168, 713–720.
Gallicchio, L., & Kalesan, B. (2009). Sleep duration and mortality: A systematic review. Journalof Sleep Research, 18, 148–158.
Gariepy, G., Wang, J., Lesage, A. D., & Schmitz, N. (2010). The longitudinal association from obesity to depression: Results from the 12-year national population health survey. Obesity, 18, 1033–1038.
Garland, S. N., Carlson, L. E., Antle, M. C., Samuels, C., & Campbell, T. (2011). I-CAN SLEEP: Rationale and design of a non-inferiority RCT of mindfulness-based stress reduction and cognitive behavioral therapy for the treatment of insomnia in CANcer survivors. Contemporary Clinical Trials, 32, 747–754
Gaylord, S. A., Palsson, O. S., Garland, E. L., Faurot, K. R., Coble, R. S., Mann, J. D.,…Whitehead, W. E. (2011). Mindfulness training reduces the severity of irritable bowel syndrome in women: Results of a randomized controlled trial. American Journal of Gastroenterology, 106, 1678–1688.
Gehi, A. K., Ali, S., Na, B., & Whooley, M. A. (2007). Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: The heart and soul study. Archives of Internal Medicine, 167, 1798–1803.
Gentry, W. D. (1984). Behavioral medicine: A new research paradigm. In W. D. Gentry (Ed.), Handbook of behavioral medicine (pp. 1–12). New York, NY: Guilford Press.
Glasgow, R. E. (2008). What types of evidence are most needed to advance behavioral medicine? Annals of Behavioral Medicine, 35, 19–25.
Glasgow, R. E., & Emmons, K. M. (2007). How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health, 28, 413–433.
Glasgow, R. E., McKay, H. G., Piette, J. D., & Reynolds, K. D. (2001). The RE-AIM framework for evaluating interventions: What can it tell us about approaches to chronic illness management? Patient Education and Counseling, 44, 119–127.
Glasgow, R. E., Nutting, P. A., King, D. K., Nelson, C. C., Cutter, G., Gaglio, B.,…Whitesides, H. (2005). Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care, 28, 33–39.
Glasgow, R. E., Vogt, T. M., & Boles, S. M. (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89, 1322–1327.
Glombiewski, J. A., Sawyer, A. T., Gutermann, J., Koenig, K., Rief, W., & Hofmann, S. G. (2010). Psychological treatments for fibromyalgia: A meta-analysis. Pain, 151, 280–295.
Goetzel, R. Z., & Ozminkowski, R. J. (2008). The health costs and benefits of work site health promotion programs. Annual Review of Public Health, 29, 303–323.
Goldbacher, E. M., & Matthews, K. A. (2007). Are psychological characteristics related to risk of the metabolic syndrome? A review of the literature. Annals of Behavioral Medicine, 34, 240–252.
Goldberg, J. H., & King, A. C. (2007). Physical activity and weight management across the lifespan. Annual Review of Public Health, 27, 145–170.
Golden, S. H., Lazo, M., Carnethon, M., Bertoni, A. G., Schreiner, P. J., Diez Roux, A. V.,…Lyketsos, C. (2008). Examining a bidirectional association between depressive symptoms and diabetes. Journal of the American Medical Association, 299, 2751–2759.
Gonzalez, J. S., Batchelder, A. W., Psaros, C., & Safren, S. A. (2011). Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. Journal of Acquired Immune Deficiency Syndrome, 58, 181–187.
Gonzalez, J. S., Peyrot, M., McCarl, L. A., Collins, E. M., Serpa, L., Mimiaga, M. J., & Safren, S. A. (2008). Depression and diabetes treatment nonadherence: A meta-analysis. Diabetes Care, 31, 2398–2403.
Goodheart, C. D. (2011). Psychology practice: Design for tomorrow. American Psychologist, 66, 339–347.
Gordon, L., Graves, N., Hawkes, A., & Eaken, E. (2007). A review of the cost-effectiveness of face-to-face behavioral interventions for smoking, physical activity, diet and alcohol. Chronic Illness, 3, 101–129.
Gould, K. L., Ornish, D., Scherwitz, L., Brown, S., Edens, R. P, Hess, M. J.,…Brand, R. (1995). Changes in myocardial perfusion abnormalities by positron emission tomography after long-term intense risk factor modification. JAMA, 274, 894–901.
Greeven, A., van Balom, A., Visser, S., Merkelbach, J., van Rood, Y., van Dyck, R.,…Spinhoven, P. (2007). Cognitive behavior therapy and paroxitine in the treatment of hypochondriasis: A randomized controlled trial. American Journal of Psychiatry, 164, 91–99.
Gross, C. R., Kreitzer, M. J., Thomas W., Reilly-Spong, M., Cramer-Bornemann, M., Nyman, J. A.,…Ibrahim, H. N. (2010). Mindfulness-based stress reduction for solid organ transplantation: A randomized controlled trial. Alternative Therapies in Health & Medicine, 16, 30–38.
Grundmann, O., & Yoon, S. L. (2010). Irritable bowel syndrome: epidemiology, diagnosis and treatment: An update for health-care practitioners. Journal of Gastroenterology and Hepatology, 25, 691–699.
Guh, D. P., Zhang, W., Bansback, N., Amarsi, Z., Birmingham, C. L., & Anis, A. H. (2009). The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health, 9, 88.
Gulliksson, M., Burrell, G., Vessby, B., Lundin, L., Toss, H., & Svardsudd, K. (2011). Randomized controlled trial of cognitive behavior therapy vs. Standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary prevention in Uppsala primary care project (SUPRIM). Archives of Internal Medicine, 171, 134–140.
Haas, L. J. (Ed.). (2004). Handbook of primary care psychology. New York, NY: Oxford University Press.
Hackett, M. L., & Anderson, C. S., (2005). Predictors of depression after stroke: A systematic review of observational studies. Stroke, 36, 2296–2310.
Hackett, M. L., Anderson, C. S., House, A., & Halteh, C. (2008). Interventions for preventing depression after stroke. Cochrane Database of Systematic Reviews (3), CD003689.
Hackett, M. L., Anderson, C. S., House, A., & Xia, J. (2008). Interventions for treating depression after stroke. Cochrane Database of Systematic Reviews (4), CD0003437.
Hagedoorn, M., Sanderman, R., Bolks, H. N., Tuinstra, J., & Coyne, J. C. (2008). Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychological Bulletin, 134, 1–30.
Hall, K. L., & Rossi, J. S. (2008). Meta-analytic examination of the strong and weak principles across 48 health behaviors. Preventive Medicine, 46, 266–274.
Hall, M. H., Muldoon, M. F., Jennings, R., Buysee, D. J., Flory, J. D., & Manuck, S. B. (2008). Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep, 31(5), 635–643.
Hall, S. M., & Prochaska, J. J. (2009). Treatment of smokers with co-occurring disorders: Emphasis on integration in mental health and addiction treatment settings. Annual Review of Clinical Psychology, 5, 409–431.
Hall, S. M., Tsoh, J. Y., Prochaska, J. J., Eisendrath, S., Rossi, J. S., Redding, C. A.…Gorecki, J. A. (2006). Treatment for cigarette smoking among depressed mental health outpatients: A randomized clinical trial. American Journal of Public Health, 96, 1808–1814.
Harris, J., Lack, L., Kemp, K., Wright, H., & Bootzin, R. (2012). A randomized controlled trial of intensive sleep retraining (ISR): A brief conditioning treatment for chronic insomnia. Sleep, 35, 49–60.
Harvey, A. G. (2011). Sleep and circadian functioning: Critical mechanisms in the mood disorders? Annual Review of Clinical Psychology, 7, 297–319.
Hendershot, C. S., Witkiewitz, K., George, W. H., & Marlatt, G. A. (2011, July 19). Relapse prevention for addictive behaviors. Prevention & Policy, 6, Art ID 17.
Herring, M. P., Puetz, T. W., O'Connor, P. J., & Dishman, R. K. (2012), Effect of exercise training among patients with a chronic illness: A systematic review and meta-analysis of randomized controlled trials. Archives of Internal Medicine, 172, 101–111.
Hersey, J. C., Khavjou, O., Strange, L. B., Atkinson, R. L., Blair, S. N., Campbell, S.,…Britt, M. (2012). The efficacy and cost-effectiveness of a community weight management intervention: A randomized controlled trial of the health weight management demonstration. Preventive Medicine, 54, 42–49.
Herzog, T. A. (2008). Analyzing the transtheoretical model using the framework of Weinstein, Rothman, and Sutton (1998): The example of smoking cessation. Health Psychology, 27, 548–556.
Hettema, J., Steele, J., Miller, W. R. (2005). Motivational interviewing. Annual Review of Clinical Psychology, 1, 91–111.
Higgins, J. P. T., & Green, S. (Eds.). (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March, 2011] The Cochrane collaboration. Available from www.cochrane-handbook.org
Hoffman, B. M., Babyak, M. A., Craighead, W. E., Sherwood, A., Doraiswamy, P. M., Coons, M. J., & Blumenthal, J. A. (2011). Exercise and pharmacotherapy in patients with major depression: One year follow-up of the SMILE study. Psychosomatic Medicine, 73, 127–133.
Hoffman, B. M., Papas, R. K., Chatkoff, D. K., & Kerns, R. D. (2007). Meta-analysis of psychological interventions for chronic low back pain. Health Psychology, 26, 1–9.
Holroyd, K. A., Martin, P. R., & Nash, J. M. (2006). Psychological treatments for tension type headache. In J. Olesen, P. Tfelt-Hansen, & K. Welsh (Eds.), The headaches (pp. 711–719). Philadelphia, PA: Lippincott, Williams, & Wilkins.
Holtgrave, D. R., & Curran, J. W. (2006). What works, and what remains to be done, in HIV prevention in the United States. Annual Review of Public Health, 27, 261–275.
Holt-Lunstad, J., Smith, T. D., & Layton, J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine: e1000316.
Hopko, D. R., Bell, J. L., Armento, M., Robertson, S., Mullane, C., Wolf, N., & Lejuez, C. W. (2008). Cognitive-behavioral therapy for depressed cancer patients in a medical care setting. Behavior Therapy, 39, 126–136.
Howard, I., Turner, R., Okin, R., & Mohr, D. C. (2006). Therapeutic alliance mediates the relationship between interpersonal problems and depression outcome in a cohort of multiple sclerosis patients. Journal of Clinical Psychology, 62, 1197–1204.
Hunt, M. G., Moshier, S., & Milonova, M., (2009). Brief cognitive-behavioral internet therapy for irritable bowel syndrome. Behaviour Research and Therapy, 47, 797–802.
Ickovics, J. R., Kershaw, T. S., Westdahl, C., Magriples, U., Massey, Z., Reynolds, H., & Rising, S. S. (2007). Group prenatal care and perinatal outcomes: A randomized controlled trial. Obstetrics and Gynecology, 110, 330–339.
Ickovics, J. R, Reed, E., Magriples, U., Westdahl, C., Schindler Rising, S., & Kershaw, T. S. (2011). Effects of group prenatal care on psychosocial risk in pregnancy: Results from a randomized controlled trial. Psychology and Health, 26, 235–250.
Irwin, M. R., Wang, M., Ribeiro, D., Cho, H. J., Olmstead, R., Breen, E. C.,…Cole, S. (2008). Sleep loss activates cellular inflammatory signaling. Biological Psychiatry, 64, 538–540.
Jennings, J. R., Muldoon, M. F., Hall, M., Buysee, D. J., & Manuck, S. B. (2007). Self-reported sleep quality is associated with the metabolic syndrome. Sleep, 30, 219–223.
Jensen, M. P. (2011). Psychosocial approaches to pain management: An organizational framework. Pain, 152, 717–725.
Johnson, S. S., Paiva, A. L., Cummins, C. O., Johnson, J. L., Dymet, S. J., Wright, J. A.,…Sherman, K. (2008). Transtheoretical model-based multiple behavior intervention for weight management: Effectiveness on a population basis. Preventive Medicine, 46, 238–246.
Jungquist, C. R., O'Brien, C., Matteson-Rusby, S., Smith, M. T., Pigeon, W. R., Xia, Y.,…Perlis, M. L. (2010). The efficacy of cognitive-behavioral therapy for insomnia in patients with chronic pain. Sleep Medicine, 11, 302–309.
Kangas, M., Bovbjerg, D. H., & Montgomery, G. H. (2008). Cancer-related fatigue: A systematic and meta-analytic review of non-pharmacological therapies for cancer patients. Psychological Bulletin, 134, 700–741.
Kaplan, R. M. (2010). Behavioral epidemiology. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds.), Handbook of health psychology and behavioral medicine (pp. 203–216). New York, NY: Guilford Press.
Kaplan, R. M., & Groessl, E. J. (2002). Applications of cost-effectiveness methodologies in behavioral medicine. Journal of Consulting and Clinical Psychology, 70, 482–493.
Kapson, H. S., & Haaga, D. (2010). Depression vulnerability moderates the effects of cognitive behavior therapy in a randomized controlled trial for smoking cessation. Behavior Therapy, 41(4), 447–460.
Katz, D. L., (2009). School-based interventions for health promotion and weight control: Not just waiting for the world to change. Annual Review of Public Health, 30, 253–272.
Kazdin, A. E., & Blase, S. L. (2011). Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science, 6, 21–37.
Keefe, F. J., Shelby, R. A., Somers, T. J., Varia, I., Blazing, M., Waters, S. J.,…Bradley, L. (2011). Effects of coping skills training and sertraline in patients with non-cardiac chest pain: A randomized trial. Pain, 152, 730–741.
Keogh, K. M., Smith, S. M., White, P., McGilloway, S., Kelly, A., Gibney, J., & O'Dowd T. (2011). Psychological family intervention for poorly controlled type 2 diabetes. American Journal of Managed Care, 17, 105–113.
Kerner, J., Rimer, B., & Emmons, K. (2005). Introduction to the special section on dissemination: Dissemination research and research dissemination: How can we close the gap? Health Psychology, 24, 443–446.
King, C. R., Knutson, K. L., Rathouz, P. J., Sidney, S., Liu, K., & Lauderdale, D. S. (2008). Short sleep duration and incident coronary artery calcification. Journal of the American Medical Association, 300(24), 2859–2866.
Kiviniemi, M. T., & Rothman, A. J. (2010). Specifying the determinants of people's health beliefs and health behavior: How a social psychological perspective can inform initiatives to promote health. In J. M. Suls, K. W. Davidson, & R. M. Kaplan, Handbook of health psychology and behavioral medicine (pp. 64–83). New York, NY: Guilford Press.
Kline, C. E., Crowley, E. P., Ewing, G. B., Burch, J. B., Blair, S. N., Durstine, J. L.,…Youngstedt, S. D. (2011). The effect of exercise training on obstructive sleep apnea and sleep quality: A randomized controlled trial. Sleep, 34, 1631–1640.
Knight, K. M., McGowan, L., Dickens, C., & Bundy, C. (2006). A systematic review of motivational interviewing in physical health care settings. British Journal of Health Psychology, 11, 319–332.
Knol, M. J., Twisk, J. W. R., Beekman, A. T. F., Heine, R. J., Snoek, F. J., & Fouwer, F. (2006). Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia, 49, 837–845.
Koenig, L. J., Pals, S. L., Bush, T., Pratt Palmore, M., Stratford, D. & Ellerbrock, T. V. (2008). Randomized controlled trial of an intervention to prevent adherence failure among HIV-infected patients initiating antiretroviral therapy. Health Psychology, 27, 159–169.
Kop, W. J., & Plumhoff, J. E. (2012). Depression and coronary heart disease: Diagnosis, predictive value, biobehavioral mechanisms, and intervention. In R. Allen & J. Fisher (Eds.), Heart and mind: The practice of cardiac psychology (pp. 143–168). Washington, DC: American Psychological Association.
Krebs, P., Prochaska, J. O., & Rossi, J. S. (2010). A meta-analysis of computer-tailored interventions for health behavior change. Preventive Medicine, 51, 214–221.
Kroenke, K. (2007). Efficacy of treatment for somatoform disorders: A review of randomized controlled trials. Psychosomatic Medicine, 69, 881–888.
Kwak, J., Montgomery, R. J. V., Kosloski, K., & Lang, J. (2011). The impact of TCARE® on service recommendation, use, and caregiver well-being. Gerontologist, 51, 704–713.
Lahmann, C., Röhricht, F., Sauer, N., Noll-Hussong, M., Ronel, J., Henrich, G.,…Loew, T. (2010). Functional relaxation as complementary therapy in irritable bowel syndrome: A randomized, controlled clinical trial. Journal of Alternative and Complementary Medicine, 16, 47–52.
Lancaster, T., Hajek, P., Stead, L. F., West, R., & Jarvis, M. J. (2006). Prevention of relapse after quitting smoking: A systematic review of trials. Archives of Internal Medicine, 166, 828–835.
Lancaster, T., & Stead, L. F. (2005). Individual behavioral counseling for smoking cessation. Cochrane Database of Systematic Reviews (3), CDO 02852.
Landon, B. E., Gill, J. M., Antonelli, R. C., & Rich, E. C. (2010). Prospects for rebuilding primary care using the patient-centered medical home. Health Affairs, 29, 827–834.
Lange, T., Perras, B., Fehm, H. L., & Born, J. (2003). Sleep enhances the human antibody response to hepatitis A vaccination. Psychosomatic Medicine, 65, 831–835.
Lazarus, R. (1966). Psychological stress and the coping process. New York, NY: McGraw-Hill.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer.
Lebow, J. L., Chambers, A. L., Christensen, A., & Johnson, S. M. (2012). Research on the treatment of couple distress. Journal of Marital and Family Therapy, 38, 145–168.
Ledesma, D., & Kumano, H. (2009). Mindfulness-based stress reduction and cancer: A meta-analysis. Psycho-Oncology, 18, 571–579.
Lee, C. D., Sui, X., Artero, E. G., Church, T. S., McAuley, P. A., Stanford, F. C.,…Blais, S. N. C. (2011). Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men. The aerobics center longitudinal study. Circulation, 124, 2483–2450.
Lee, C. D., Sui, X., & Blair, S. N. (2009). Combined effects of cardiorespiratory fitness, not smoking, and normal waist girth on morbidity and mortality in men. Archives of Internal Medicine, 169, 2096–2101.
Lee, C. D., Sui, X., Hooker, S. P., Herbert, J. R., & Blair, S. N. (2011). Combined impact of lifestyle factors on cancer mortality in men. Annals of Epidemiology, 21, 749–754.
Lengacher, C. A., Johnson-Mallard, V., Post-White, J., Moscoso, M. S., Jacobsen, P. B., Klein, T. W.,…Kip, K. E. (2009). Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology, 18, 1261–1272.
Leonard, M. T., Cano, A., & Johansen, A. B. (2006). Chronic pain in a couples context: A review and interpretation of theoretical models and empirical evidence. Journal of Pain, 7, 377–390.
Lett, H. S., Blumenthal, J. A., Babyak, M., Strauman, T., Robbins, C., & Sherwood, A. (2005). Social support and coronary heart disease: Epidemiologic evidence and implications for treatment. Psychosomatic Medicine, 67, 869–878.
Leventhal, H., Breland, J. Y., Mora, P. A., & Leventhal, E. A. (2010). Lay representations of illness and treatment: A framework for action. In A. Steptoe (Ed.), Handbook of behavioral medicine: Methods and applications (pp. 137–154). New York, NY: Springer.
Lichtman, J. H., Bigger, J. T., Blumenthal, J. A., Frasure-Smith, N., Kaufman, P. G., Lesperance, F., Mark, D. B.,…American Psychiatric Association. (2008). Depression and coronary heart disease: Recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: Endorsed by the American Psychiatric Association. Circulation, 118, 1768–1775.
Linde, J. A., Simon, G. E., Ludman, E. J., Ichikawa, L. E., Operskalski, B. H., Arterburn, D.,…Jeffery, R. W. (2011). A randomized controlled trial of behavioral weight loss treatment versus combined weight loss/depression treatment among women with comorbid obesity and depression. Annals of Behavioral Medicine, 41, 119–130.
Linden, W., & Girgis, A. (2011, September 1). Psychosocial treatment outcomes for cancer patients: What do meta-analyses tell us about distress reduction? Psycho-Oncology. doi: 10.1002/pon.2035
Linden, W., Phillips, M. J., & Leclerc, J. (2007). Psychological treatment of cardiac patients: A meta-analysis. European Heart Journal, 28, 24, 2964–2966.
Ljótsson, B., Falk, L., Vesterlund, A. W., Hedman, E., Lindfors, P., Rück, C.,…Andersson, G. (2010). Internet-delivered exposure and mindfulness based therapy for irritable bowel syndrome—A randomized controlled trial. Behaviour Research & Therapy, 48, 531–539.
Lobel, M., Cannella, D. L., Graham, J. E., DeVincent, C., Schneider, J. & Meyer, B. A. (2008). Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychology, 27, 604–615.
Lopez, C., Antoni, M., Penedo, F., Weiss, D., Cruess, S., Segotas, M. C.,…Fletcher, M. A. (2011). A pilot study of cognitive behavioral stress management effects on stress, quality of life, and symptoms in persons with chronic fatigue syndrome. Journal of Psychosomatic Research, 70, 328–334.
Lovallo, W. R. (2010). Emotions and stress. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds.), Handbook of health psychology and behavioral medicine (pp. 31–48). New York, NY: Guilford Press.
Lundahl, B., & Burke, B. L. (2009). The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. Journal of Clinical Psychology, 65, 1232–1245.
Macea, D. D., Gajos, K., Calil, Y. A. D., & Fregni, F. (2010). The efficacy of web-based cognitive behavioral interventions for chronic pain: A systematic review and meta-analysis. Journal of Pain, 11, 917–929.
Magkos,F., Yannakoulia,M., Chan,J. L., & Mantzoros, C. S. (2009). Management of the metabolic syndrome and type 2 diabetes through lifestyle modification. Annual Review of Nutrition, 29, 223–256.
Mahoney, M. J. (1977). Reflections on the cognitive-learning trend in psychotherapy. American Psychologist, 32, 5–13.
Manne, S. L., Rubin, S., Edelson, M., Rosenblum, N., Bergman, C., Hernandez, E.,…Winkel, G. (2007). Coping and communication-enhancing intervention versus supportive counseling for women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology, 75, 615–628.
Markowitz, S., Friedman, M. A., & Arent, S. M. (2008). Understanding the relation between obesity and depression: Causal mechanisms and implications for treatment. Clinical Psychology: Science and Practice, 15, 1–20.
Martin, R. K., McNeil, D. W. (2009). Review of motivational interviewing in promoting health behaviors. Clinical Psychology Review, 29, 283–293.
Martire, L. M., Schulz, R., Helgeson, V. H., Small, B. J., & Saghafi, E. M. (2010). Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine, 40, 325–342.
Mathers, C. D., & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine, 3, e442. doi:10.1371/journal.pmed.0030442
Matthews, K. A., & Gallo, L. C. (2010). Psychological perspectives on pathways linking socioeconomic status and physical health. Annual Review of Psychology, 62.
Matthews, K. A., & Gump, B. B. (2002). Chronic work stress and marital dissolution increase risk of posttrial mortality in men from the multiple risk factor intervention trial. Achieves of Internal Medicine, 162, 309–315.
McBeth, J., Prescott, G., Scotland, G., Lovell, K., Keeley, P., Hannaford, P.,…MacFarland, G. J. (2012). Cognitive behavior therapy, exercise, or both for treating chronic widespread pain. Archives of Internal Medicine, 172, 48–57.
McCain, N. L., Gray, D. P., Elswick, R. K. Jr., Robins, J. W., Tuck, I., Walter, J. M.,…Ketchum, J. M. (2008). A randomized clinical trial of alternative stress management interventions in persons with HIV infection. Journal of Consulting and Clinical Psychology, 76, 431–441.
McCaul, K., Hockemeyer, J. R., Johnson, R. J., Zetocha, K., Quinlan, K., & Glasgow, R. E. (2006). Motivation to quit using cigarettes: A review. Addictive Behaviors, 31, 42–56.
McDaniel, S. H., & Fogerty, C. T., (2009). What primary care psychology has to offer the patient-centered medical home. Professional Psychology: Research and Practice, 40, 483–492.
McGinnis, J. M., Williams-Russo, P., & Knickman, J. R. (2002). The case for more active policy attention to health promotion. Health Affairs (Millwood), 21, 78–93.
McHugh, R. K., & Barlow, D. H. (2011). The dissemination and implementation of evidence-based psychological treatments: A review of current efforts. American Psychologist, 65, 73–84.
Meichenbaum, D. H. (1977). Cognitive behavior modification. New York, NY: Plenum Press.
Meijer, A., Rosenman, M., Milette, K., Coyne, J. C., Stefanek, M., Ziegelstein, R.,…Thombs, R. (2011). Depression screening and patient outcomes in cancer: A systematic review. PLoS One, 6(11), pe27181.
Miller, G. E., Chen, E., & Parker, K. J. (2011). Psychological stress in childhood and susceptability to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137, 959–997.
Miller, W. R., & Rose, G. S. (2009). Toward a theory of motivational interviewing. American Psychologist, 64, 527–537.
Mills, P. J., von Känel, R., Norman, D., Natarajan, L., Ziegler, M. G., & Dimsdale, J. E. (2007). Inflammation and sleep in healthy individuals. Sleep, 30, 729–735.
Mohr, D. C., Hart, S., Julian, L., Catledge, C., Honos-Webb, L., Vella, L. & Tasch, E. (2005). Telephone-administered psychotherapy for depression. Archives of General Psychiatry, 62, 1007–1014.
Mohr, D. C., Hart, S., & Vella, L. (2007). Reduction in disability in a randomized controlled trial of telephone-administered cognitive-behavioral therapy. Health Psychology, 26, 554–563.
Monin, J. K., & Schulz, R. (2009). Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging, 24, 681–695.
Montgomery, G. H., Kargas, M., David, D., Hallquist, Green, S., Bovjberg, D. H., & Schnur, J. B. (2009). Fatigue during breast cancer radiotherapy: An initial randomized study of cognitive-behavioral therapy plus hypnosis. Health Psychology, 28, 317–322.
Morin, C. M., & Espie, C. A. (2003). Insomnia. A clinical guide to assessment and treatment. New York, NY: Plenum Press.
Morley, S., Williams, A., & Hussain, S. (2008). Estimating the clinical effectiveness of cognitive behavioural therapy in the clinic: Evaluation of a CBT informed pain management programme. Pain, 137, 670–680.
Moskowitz, J. T., Hult, J. R., Bussolari, C., & Acree, M. (2009). What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin, 135, 121–141.
Moss-Morris, R., McAlpine, L., Didsbury, L., & Spence, M. J. (2009). A randomized controlled trial of a cognitive behavioural therapy-based self-management intervention for irritable bowel syndrome in primary care. Psychological Medicine, 40, 85–94.
Mustanski, B. S, Newcomb, M. E., Du Bois, S. N., Garcia, S. C., & Grov, C. (2011). HIV in young men who have sex with men: A review of epidemiology, risk and protective factors, and interventions. Journal of Sex Research, 48, 218–253.
Nation, D. A., Schneiderman, N., & McCabe, P. M. (2010). Animal models in health psychology research. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds.), Handbook of health psychology and behavioral medicine (pp. 163–181). New York, NY: Guilford Press.
Nestoric, Y., & Martin, A. (2007). Efficacy of biofeedback for migraine: A meta-analysis. Pain, 128, 111–127.
Nestoric, Y., Rief, W., & Martin, A. (2008). Meta-analysis of biofeedback for tension-type headache: Efficacy, specificity, and treatment moderation. Journal of Consulting and Clinical Psychology, 76, 379–396.
Nezu, A. M., Nezu, C. M., Felgoise, S. H., McClure, K. S., & Houts, P. S. (2003). Project Genesis: Assessing the efficacy of problem-solving therapy for distressed adult cancer patients. Journal of Consulting and Clinical Psychology, 71, 1036–1048.
Nichols, L. O., Martindale-Adams, J., Burns, R., Graney, M., & Zuber, J. (2011). Translation of a dementia caregiver support program in a health care system—REACH VA. Archives of Internal Medicine, 171, 353–359.
Nicholson, A., Kuper, H., & Hemingway, H. (2006). Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146,538 participants in 54 observational studies. European Heart Journal, 27, 2763–2774.
Nield, L., Moore, H. J., Hooper, L., Cruickshank, J. K., Vyas, A., Whittaker, V., & Summerbell, C. D. (2007). Dietary advice for treatment of type 2 diabetes mellitus in adults. Cochrane Database of Systematic Reviews, CD004097.
Noar, S. M., Benac, C. N., & Harris, M. S., (2007). Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin, 133, 673–693.
Novak, D., Cameron, O., Epel, E., Ader, R., Waldstein, S. R., Levenstein, S.,…Wainer, A. R. (2007). Psychosomatic medicine: The scientific foundation of the biopsychosocial model. Academic Psychiatry, 31, 388–401.
Ogden, C. L., Carroll, M. D., Kit, B. D., & Flegal, K. M. (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA, 307, 483–490.
Oken, B. S., Fonareva, I., Haas, M., Wahbeh, H., Lane, J. B., Zajdel, D., & Amen, A. (2010). Pilot controlled trial of mindfulness meditation and education for dementia caregivers. Journal of Alternative & Complementary Medicine, 16, 1031–1038.
Oldenburg, B., Absetz, P., & Chan, C. K. Y. (2010). Behavioral interventions for prevention and management of chronic disease. In A. Steptoe (Ed.), Handbook of behavioral medicine: Methods and applications (pp. 969–988). New York, NY: Springer.
Oldenburg, B., de Courten, M., & Frean, E. (2010). The contribution of health psychology to the advancement of global health. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds.), Handbook of health psychology and behavioral medicine (pp. 397–408). New York, NY: Guilford Press.
Ornish, D., Brown, S. E., Scherwitz, L. W., Billings, J. H., Armstrong, W. T., Ports, T. A.,…Brand, R. (1990). Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet, 336, 129–133.
Ornish, D., Scherwitz, L. W., Billings, J. H., Gould, K. L., Merritt, T. A., Sparler, S.,…Brand, R. (1998). Intensive lifestyle changes for reversal of coronary heart disease. JAMA, 280, 2001–2007.
Orth-Gomér, K., Schneiderman, N., Wang, H. X., Walldin, C., Blom, M., & Jernberg, T. (2009). Stress reduction prolongs life in women with coronary disease: the Stockholm women's intervention trial for coronary heart disease (SWITCHD). Circulation. Cardiovascular Quality and Outcomes, 2, 25–32.
Orth-Gomér, K., Wamala, S. P., Horsten, M., Schenck-Gustafsson, K., Schneiderman, N., & Mittleman, M. A. (2000). Marital stress worsens prognosis in women with coronary heart disease: The Stockholm female coronary risk study. JAMA, 284, 3008–3014.
Pack, A. I., & Pien, G. W. (2011). Update on sleep and its disorders. Annual Review of Medicine, 62, 447–460.
Palmer, S. C., van Scheppinger, C., & Coyne, J. C. (2011). Clinical trial did not demonstrate benefits of screening patients with cancer for distress. Journal of Clinical Oncology, 29, e277–e288.
Patten, S. B., Williams, J., Lavorato, D., Khaled, S., & Bulloch, A. (2011). Weight gain in relation to major depression and medication use. Journal of Affective Disorders, 134, 288–293.
Pomerleau, O. F., & Brady, J. P. (1979). Introduction: The scope and promise of behavioral medicine. In O. F. Pomerleau & J. P. Brady (Eds.), Behavioral medicine: Theory and practice. Baltimore, MD: Williams & Wilkins.
Pomerleau, O. F., & Rodin, J. (1986). Behavioral medicine and health psychology. In A. E. Bergin & S. L. Garfield (Eds.), Handbook of psychotherapy and behavior change (3rd ed., pp. 483–522). New York, NY: Wiley.
Powell, K. E., Paluch, A. E., & Blair, S. N. (2011). Physical activity for health: What kind? How much? How intense? On top of what? Annual Review of Public Health, 32, 349–365.
Pradhan, E. K., Baumgarten, M., Langenberg, P, Handwerger, B., Gilpin, A. K., Magyari, T., …Berman, B. (2007). Effect of mindfulness-based stress reduction in rheumatoid arthritis patients. Arthritis & Rheumatism, 57, 1134–1142.
Prather, A. A., Blumenthal, J. A., Hinderliter, A., & Sherwood, A. (2011). Ethnic differences in the effects of the DASH diet on nocturnal blood pressure dipping in individuals with high blood pressure. American Journal of Hypertension, 24, 1338–1344.
Prejean, J., Song, R., Hernandez, A., Ziebell, R., Green T, Walker, F.,…Hall, H. I., for the HIV Incidence Surveillance Groups. (2011). Estimated HIV incidence in the United States, 2006–2009. PLoS ONE, 6, e17502.
Prochaska, J. J., Hall, S. M., Humfleet, G., Munoz, R. F., Reus, V., Gorecki, J., & Hu, D. (2008). Physical activity as a strategy for maintaining tobacco abstinence: A randomized trial. Preventive Medicine, 47, 215–220.
Prochaska, J. J., Hall, S. M., Tsoh, J. Y., Eisendrath, S., Rossi, J. S., Redding, C. A.,…Gorecki, J. A. (2008). Treating tobacco dependence in clinically depressed smokers: Effect of smoking cessation on mental health functioning. American Journal of Public Health, 98, 446–448.
Prochaska, J. J., Nigg, C. R., Spring, B., Velicer, W., & Prochaska, J. O. (2010). The benefits and challenges of multiple health behavior change in research and practice. Preventive Medicine, 50, 26–29.
Prochaska, J. J., & Prochaska, J. M. (2009). Multiple risk behavior change: What most individuals need. In S. A. Shumaker, J. K. Ockene, & K. A. Riekert (Eds.), The handbook of health behavior change (3rd ed., pp. 287–305). New York, NY: Springer.
Prochaska, J. J., Velicer, W. F., Prochaska, J. O., Delucchi, K., & Hall, S. M. (2006). Comparing intervention outcomes in smokers treated for single versus multiple behavioral risks. Health Psychology, 25, 380–388.
Prochaska, J. O., DiClemente, C. C., & Norcross, J. C. (1992). In search of how people change: Applications to addictive behaviors. American Psychologist, 47, 1102–1114.
Relman, A. S., & Angell, M. (2002). Resolved: Psychosocial interventions can improve clinical outcomes in organic disease (Con). Psychosomatic Medicine, 64, 558–563.
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F., & Zwahlen, M. (2008). Body-mass index and incidence of cancer: A systematic review and meta-analysis of prospective observational studies. Lancet, 371, 569–578.
Rohrbaugh, M. J., Shoham, V., & Coyne, J. C. (2006). Effect of marital quality on eight-year survival of patients with heart failure. American Journal of Cardiology, 98, 1069–1072.
Rollman, B. L., Belnap, B. H., LeMenager, M. S., Mazumdar, S., Houck, P. R., Counihan, P.,…Reynolds, C. F. 3rd. (2009). Telephone-delivered collaborative care for treating post-CABG depression: a randomized controlled trial Journal of the American Medical Association, 302, 2095–2103.
Rotheram-Borus, M., Swendeman, D., & Chovnick, G. (2009). The past, present, and future of HIV prevention: Integrating behavioral, biomedical, and structural intervention strategies for the next generation of HIV prevention. Annual Review of Clinical Psychology, 5, 143–167.
Rutledge, T., Reis, V. A., Linke, S. E., Greenberg, B. H., & Mills, P. J. (2006). Depression in heart failure: A meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. Journal of the American College of Cardiology, 48, 1527–1537.
Saab, P. G., Bang, H., Williams, R. B., Powell, L. H., Schneiderman, N., Thoresen, C.,…Keefe, F. (2009). The impact of cognitive behavioral group training on event-free survival in patients with myocardial infarction: The ENRICHD experience. ENRICHD investigators. Journal of Psychosomatic Research, 67, 45–56.
Sackett, D., Rosenberg, W., Muir Gray, J., Haynes, R., & Richardson, W. (1996). Evidence based medicine: What it is and what it isn't. British Medical Journal, 312, 71–72.
Safren, S. A., O'Cleirigh, C., Tan, J. Y., Raminani, S. R., Reilly, L. C., Otto, M. W., & Mayer, K. H. (2009). A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychology, 28, 1–10.
Satcher, D. (2006). The prevention challenge and opportunity. Health Affairs (Millwood), 25, 1009–1011.
Sallis, J. F., Cervero, R. B., Ascher, W., Henderson, K. A., Kraft, M. K., & Kerr, J. (2006). An ecological approach to creating active living communities. Annual Review of Public Health, 27, 297–322.
Schneiderman, N., Antoni, M. H., Penedo, F. J., & Ironson, G. H. (2010). Psychosocial-behavioral interventions and chronic disease. In A. Steptoe (Ed.), Handbook of behavioral medicine: Methods and applications (pp. 989–1008). New York, NY: Springer.
Schneiderman, N., Saab, P. G., Catellier, D. J., Powell, L. H., DeBusk, R. F., Williams, R. B., …Kaufman, P. (2004). Psychosocial treatment within sex by ethnicity subgroups in the enhancing recovery in coronary heart disease clinical trial. Psychosomatic Medicine, 66, 475–483.
Schnur, J. B., David, D., Kangas, M., Green, S., Bovbjerg, D., & Montgomery, G. H. (2009). A randomized trial of a cognitive-behavioral therapy and hypnosis intervention on positive and negative affect during breast cancer radiotherapy. Journal of Clinical Oncology, 65, 443–455.
Schnur, J. B., & Montgomery, G. H. (2010). A systematic review of therapeutic alliance, group cohesion, empathy, and goal consensus/collaboration in psychotherapeutic interventions in cancer: Uncommon factors? Clinical Psychology Review, 30, 238–247.
Schulz, M. B., & Hu, F. B. (2005). Primary prevention of diabetes: What can be done and how much can be prevented? Annual Review of Public Health, 26, 445–467.
Schwarzer, R. (2011). Health behavior change. In H. S. Friedman (Ed.), The Oxford handbook of health psychology (pp. 591–611). New York, NY: Oxford University Press.
Scott-Sheldon, L. A., Fielder, R. L., & Carey, M. P. (2010). Sexual risk reduction interventions for patients attending sexually transmitted disease clinics in the United States: A meta-analytic review, 1986 to early 2009. Annals of Behavioral Medicine, 40, 191–204.
Scott-Sheldon, L. A. J., Kalichman, S. C., Carey, M. P., & Fielder, R. L. (2008). Stress management interventions for HIV+ adults: A meta-analysis of randomized controlled trials, 1989 to 2006. Health Psychology, 27, 129–139.
Seo, D. C., & Sa, J. (2008). A meta-analysis of psycho-behavioral obesity interventions among US multiethnic and minority adults. Preventive Medicine, 47, 573–582.
Shields, C. G., Finley, M. A., Chawla, N., & Meadors, P. (2012). Couple and family interventions for health problems. Journal of Marital and Family Therapy, 38, 265–280.
Simon, G. E., Katon, W. J., Lin, E. H., Rutter, C., Manning, W. G., Von Korff, M.,…Young, B. A. (2007). Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Archives of General Psychiatry, 64, 65–72.
Smeets, R., Vtaeyen, J., Kester, A., & Knottnerus, J. (2006). Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. Journal of Pain, 7, 261–271.
Smith, P. J., Blumenthal, J. A., Babyak, M. A., Georgiades, A., Hinderliter, A., & Sherwood, A. (2007). Effects of exercise and weight loss on depressive symptoms among men and women with hypertension. Journal of Psychosomatic Research, 63, 463–469.
Smith, P. J., Blumenthal, J. A., Hoffman, B. M., Cooper, H., Strauman, T., Welsh-Bohmer, K., …Sherwood, A. (2010). Aerobic exercise and neurocognitive performance: A meta-analytic review of randomized controlled trials. Psychosomatic Medicine, 72, 239–252.
Smith, T. W. (2006a). Personality as risk and resilience in physical health. Current Directions in Psychological Science, 15, 227–231.
Smith, T. W. (2006b). Blood, sweat, and tears: Exercise in the management of mental and physical health problems. Clinical Psychology: Science and Practice, 13, 198–202.
Smith, T. W. (2010a). Conceptualization, measurement, and analysis of negative affective risk factors. In A. Steptoe (Ed.), Handbook of behavioral medicine research: Methods and applications (pp. 155–168). New York, NY: Springer.
Smith, T. W. (2010b). Depression and chronic medical illness: Implications for relapse prevention. In C. S. Richards & M. G. Perri (Eds.), Relapse prevention for depression (pp. 199–225). Washington, DC: American Psychological Association.
Smith, T. W. (2011). Measurement in health psychology research. In H. S. Friedman (Ed.), Oxford handbook of health psychology (pp. 42–72). New York: Oxford University Press.
Smith, T. W., Kendall, P. C., & Keefe, F. J. (2002). Behavioral medicine and clinical health psychology: A view from the decade of behavior. Journal of Consulting and Clinical Psychology, 70, 459–462.
Smith, T. W., Orleans, C. T., & Jenkins, C. D. (2004). Prevention and health promotion: Decades of progress, new challenges, and an emerging agenda. Health Psychology, 23, 126–131.
Smith, T. W., & Traupman, E. K. (2012). Anger, hostility, and aggressiveness in coronary heart disease: Clinical applications of an interpersonal perspective. In R. Allan & J. Fisher (Eds.), Heart and mind II: Evolution of cardiac psychology (pp. 197–217). Washington, DC: American Psychological Association.
Smith, T. W., Uchino, B. N., Berg, C. A., & Florsheim, P. (2012). Marital discord and coronary artery disease: A comparison of behaviorally-defined discrete groups. Journal of Consulting and Clinical Psychology, 80, 87–92.
Sparrenberger, F., Cichelero, F. T., Ascoli, A. M., Fonseca, F. P., Weiss. G., Berwanger, O.,…Fuchs, F. D. (2009). Does psychosocial stress cause hypertension? A systematic review of observational studies. Journal of Human Hypertension, 23, 12–19.
Sperl-Hillen, J., Beaton, S., Fernandes, O., Von Worley, A., Vazquez-Benitez, G., Parker, E.,…Spain C. V. (2011). Comparative effectiveness of patient education methods for type 2 diabetes: A randomized controlled trial. Archives of Internal Medicine, 171, 2001–2010.
Spiegel, D., Bloom, J. R., Kraemer, H. C., & Gottheil, E. (1989). Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet, 334, 888–891.
Spring, B. (2011). Translational behavioral medicine: a pathway to better health. Translational Behavioral Medicine, 1, 1–3.
Spring, B., Howe, D., Berendsen, M., McFadden, H. G., Hitchcock, K., Radenmaker, A. W., & Hitsman, B. (2009). Behavioral intervention to promote smoking cessation and prevent weight gain: a systematic review and meta-analysis. Addiction, 104, 1472–1486.
Spring, B., Pagato, S., Knatterud, G., Kozak, A., & Hedeker, A. (2007). Examination of the analytic quality of behavioral health randomized clinical trials. Journal of Clinical Psychology, 63, 53–71.
Spring, B., Pagoto, S., Kaufman, P. G., Whitlock, E. P., Glasgow, R. E., Smith, T. W.,…& Davidson, K. W. (2005). Invitation to a dialogue between researchers and clinicians about evidence-based behavioral medicine. Annals of Behavioral Medicine, 30, 125–127.
Stanton, A. L., Revenson, T. A., & Tennen, H. (2007) Health psychology: Psychological adjustment to chronic disease. Annual Review of Psychology, 58, 565–92.
Stead, L. F., Perera, R., Bullen, C., Mant, D., & Lancaster, T. (2008). Nicotine replacement therapy for smoking cessation. Cochrane Database for Systematic Reviews (1), CD 000146.
Stein, C. J., & Colditz, G. A. (2004). The epidemic of obesity. Journal of Clinical Endocrinology and Metabolism, 89, 2522–2535.
Stein, R. A. (2012). Exercise for the prevention and treatment of depression in patients with coronary heart disease. In R. Allen & J. Fisher (Eds.), Heart and mind: The practice of cardiac psychology (pp. 459–474). Washington DC: American Psychological Association.
Stefanek, M., Palmer, S. C., Thombs, B., & Coyne, J. C. (2009). Finding what is not there: Unwarranted claims of an effect of psychosocial intervention on recurrence and survival. Cancer, 115, 5612–5616.
Strange, K. C., Nutting, P. A., Miller, W. L., Jaen, C. R., Crabtree, B. F., Flocke, S. A., & Gill, J. M. (2010). Defining and measuring the patient-centered medical home. Journal of General Internal Medicine, 25, 601–612.
Strecher, V. (2007). Internet methods for delivering behavioral and health-related interventions (eHealth). Annual Review of Clinical Psychology, 3, 53–76.
Stroebe, M., Schut, H., & Stroebe, W. (2007). Health outcomes of the bereaved. Lancet, 370, 1960–1973.
Stroebe, W., Schut, H., & Stroebe, M. S. (2005). Grief work, disclosure and counseling: Do they help the bereaved? Clinical Psychology Review, 25, 395–414.
Stone, G. C., Cohen, F., & Adler, N. E. (1979). Health psychology. San Francisco, CA: Jossey-Bass.
Story, M., Kaphingst, K. M., Robinson-O'Brien, R., & Glanz, K. (2008). Creating healthy food and eating environments: Policy and environmental approaches. Annual Review of Public Health, 29, 253–272.
Stuart, S., Noyes, R. Jr., Starcevic, V., & Barski, A. (2008). An integrative approach to somatoform disorders combining interpersonal and cognitive-behavioral therapy and techniques. Journal of Contemporary Psychotherapy, 38, 45–53.
Stuart-Shor, J., Berra, K. A., Kamau, M. W., & Kumanyika, S. K. (2012). Behavioral strategies for cardiovascular risk reduction in diverse and underserved racial/ethnic groups. Circulation, 125, 171–184.
Suls, J., & Bunde, J. (2005). Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin, 131, 260–300.
Suls, J. M., Luger, T., & Martin, R. (2010). The biopsychosocial model and the use of theory in health psychology. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds.), Handbook of health psychology and behavioral medicine (pp. 15–30). New York, NY: Guilford Press.
Sun-Edelstein, C., & Mauskop, A. (2011). Alternative headache treatments: Neutraceuticals, behavioral and physical treatments. Headache, 51, 469–483.
Surwit, R. S., van Tilburg, M. A. L., Zucker, N., McCaskill, C. C., Parekh, P., Feinglos, M. N.,…Lane, J. D. (2002). Stress management improves long-term glycemic control in type 2 diabetes mellitus, Diabetes Care, 25, 30–34.
Surwit, R. S., Williams, R. B., & Shapiro, D. (1982). Behavioral approaches to cardiovascular disease. New York, NY: Academic Press.
Taylor, R. S., Brown, A., Ebrahim, S., Jolliffe, J., Noorani, H., Rees, K.,…Oldridge, N. (2004). Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. American Journal of Medicine, 11, 682–692.
Thieme, K., Turk, D. C., & Flor, H. (2007). Responder criteria for operant and cognitive-behavioral treatment of fibromyalgia syndrome. Arthritis and Rheumatism, 57, 830–836.
Thombs, B. D., de Jonge, P., Coyne, J. C., Whooley, M. A., Frasure-Smith, N., Mitchell, A., …Ziegelstein, R. C. (2008). Depression screening and patient outcomes in cardiovascular care: a systematic review. Journal of the American Medical Association, 300, 2161–2171.
Thorndike, A. N., Regan, S., McKool, K., Pasternak, R. C., Swartz, S., Torres-Finnerty, N., & Rigotti, N. A. (2008). Depressive symptoms and smoking cessation after hospitalization for cardiovascular disease. Archives of Internal Medicine,168, 186–191.
Thorpe, A. A., Owen, N., Neuhaus, M., & Dunstan, D. W. (2011). Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. American Journal of Preventive Medicine, 41, 207–215.
Turk, D. C., Wilson, H. D., & Cahana, A. (2011). Treatment of chronic non-cancer pain. Lancet, 377, 2226–2235.
Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29, 377–387.
Umpierre, D., Ribeiro, P. A., Kramer, C. K., Leitão, C. B., Zucatti, A. T., Azevedo, M. J.,…Schaan, B. D. (2011). Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: A systematic review and meta-analysis. JAMA, 305, 1790–1799.
Van der Feltz-Cornelis, C. M., Nuygen, J., Stoop, C., Chan, J., Jacobson, A., Katon, W.,…Sartorius, N. (2010). Effectiveness of interventions for major depressive disorder and significant depressive symptoms in patients with diabetes mellitus: A systematic review and meta-analysis. General Hospital Psychiatry, 32, 380–395.
Van der Feltz-Cornelis, C. M., Van Os, T. W., Van Marwijk, H. W., & Leentjens, A. F. (2010). Effect of psychiatric consultation models in primary care: A systematic review and meta-analysis. Journal of Psychosomatic Research, 68, 521–533.
van der Houwen, K., Schut, H., van den Bout, J., Stroebe, M., & Stroebe, W. (2010). The efficacy of a brief internet-based self-help intervention for the bereaved. Behaviour Research and Therapy, 48, 359–367.
van Kessel, K., Moss-Morris, R., Willoughby, E., Chalder, T., Johnson, M. H., & Robinson, E. (2008). A randomized controlled trial of cognitive behavior therapy for multiple sclerosis fatigue. Psychosomatic Medicine, 70, 205–213.
van Scheppingen, C., Schroevers, M., Smink, A., van der Linden, Y. M., Mul, V., Langendik, J. A.,…Sanderman, C. (2011). Does screening for distress efficiently uncover unmet needs in cancer patients? Psycho-Oncology, 20, 655–663.
Veehof, M. M., Oskam, M., Schreurs, K. M. G., & Bohlmeijer, E. T. (2011). Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain, 152, 533–542.
Vitiello, M. V., Rybarczyk, B., Von Korff, M., & Stepanski, E. J. (2009). Cognitive behavioral therapy for insomnia improves sleep and decreases pain in older adults with co-morbid insomnia and osteoarthritis. Journal of Clinical Sleep Medicine, 5, 355–362.
Vizza, J. (2012). Comprehensive lifestyle intervention and group support. In R. Allan & J. Fisher (Eds.), Heart and mind: The practice of cardiac psychology (2nd ed., pp. 401–416). Washington, DC: American Psychological Association.
Von Bertalanffy, L. (1968). General systems theory. New York, NY: Braziller.
Wadden, T. A., Foreyt, J. P., Foster, G. D., Hill, J. O., Klein, S., O'Neil, P. M.,…Dunayevich, E. (2011). Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR-BMOD trial. Obesity, 19, 110–120.
Wardle, J., Chida, Y., Gibson, E. L., Whitaker, K. L., & Steptoe, A. (2011). Stress and adiposity: A meta-analysis of longitudinal studies. Obesity, 19, 771–778.
Weidner, G., & Kendel, F. (2010). Prevention of coronary heart disease. In J. M. Suls, K. W. Davidson, & R. M. Kaplan, Handbook of health psychology and behavioral medicine (pp. 354–369). New York, NY: Guilford Press.
Weinstein, N. D., Rothman, A. J., & Sutton, S. R. (1998). Stage theories of health behavior: Conceptual and methodological issues. Health Psychology, 17, 290–299.
West, R. (2005). Time for a change: Putting the transtheoretical (stages of change) model to rest. Addiction, 100, 1036–1039.
Whalley, B., Rees, K., Davies, P., Bennett, P., Ebrim, S., Liu, Z.,…Taylor, R. S. (2011, August 10). Psychological interventions for coronary heart disease. Cochrane Database of Systematic Reviews, CD002902.
Whitebird, R. R., Kreitzer, M. J., Lewis, B. A., Hanson, L. R., Crain, A. L., Enstad, C. J., & Mehta, A. (2011). Recruiting and retaining family caregivers to a randomized controlled trial on mindfulness-based stress reduction. Contemporary Clinical Trials, 32, 654–661.
Whitlock, G., Lewington, S., Sherliker P., Clarke, R., Emberson, J., Halsey J.,…Prospective Studies Collaboration (2009). Body-mass index and cause-specific mortality in 900,000 adults: Collaborative analyses of 57 prospective studies. Lancet, 373, 1083–1096.
Wilamowska, Z. A., Thompson-Hollands, J., Fairholme, C. P., Ellard, K. K., Farchione, T. J., & Barlow, D. H. (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27, 882–890.
Williams, G. C., Lynch, M., & Glasgow, R. E. (2007). Computer-assisted intervention improves patient-centered diabetes care by increasing autonomy support. Health Psychology, 26, 728–734.
Williams, P. G., Smith, T. W., Gunn, H., & Uchino, B. N. (2011). Personality and stress: Individual differences in exposure, reactivity, recovery, and restoration. In R. J. Contrada & A. Baum (Eds.), Handbook of stress science: Biology, psychology, and health (pp. 231–246). New York, NY: Springer.
Williams, P. G., Smith, T. W., & Jordan, K. D. (2010). Health anxiety and hypochondriasis: Interpersonal extensions of the cognitive-behavioral perspective. In J. G. Beck (Ed.), Interpersonal perspectives in the anxiety disorders (pp. 261–284). Washington, DC: American Psychological Association.
Williams, R. B. (2008). Psychosocial and biobehavioral factors and their interplay in coronary heart disease. Annual Review of Clinical Psychology, 4, 349–365.
Wilson, D. K., St. George, S. M., & Zarrett, N. (2010). Developmental influences in Understanding child and adolescent health behaviors. In J. M. Suls, K. W. Davidson, & R. M. Kaplan (Eds). Handbook of behavioral medicine (pp. 133–146). New York, NY: Guilford Press.
Wilson, G. T. (1980). Cognitive factors in lifestyle changes: A social learning perspective. In P. O. Davidson & S. M. Davidson (Eds.), Behavioral medicine: Changing health lifestyles (pp. 3–37). New York, NY: Bruner/Mazel.
Witthoft, M., & Hiller, W. (2010). Psychological approaches to origins and treatment of somatoform disorders, Annual Review of Clinical Psychology, 6, 257–283.
Wright, A. A., Zhang, B., Ray, A., Mack, J., Trice, E., Balboni, T.,…Prigerson, H. G. (2008). Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA, 300, 1665–1673.
Zautra, A. J., Davis, M. C., Rich, J. W., Nicassio, P., Tennen, H., Finan, P.,…Irwin, M. (2008). Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. Journal of Consulting and Clinical Psychology, 76, 408–421.