
CHAPTER 1
HOW (NOT) TO PRESENT A PATIENT HISTORY
Only connect. …
—E.M. FORSTER (1879–1970), Howards End
A doctor who cannot take a good history and a patient who cannot give one are in danger of giving and receiving bad treatment.
—ANONYMOUS, quoted by Paul Dudley White, M.D., in Clues in the Diagnosis and Treatment of Heart Disease (1956)
For students, either you have already discovered, or will soon learn, that delivering a medical presentation on rounds is a challenging and sometimes terrifying experience. You have to satisfy two conflicting sets of goals simultaneously: accuracy and comprehensiveness vs. succinctness and efficiency.
It is surprising how ineffectively and inefficiently many physicians, especially those in training, communicate clinical information. Clinical savvy, technical skills, and communication skills are not necessarily positively correlated. A reliable sign of this problem is the restless legs syndrome or flamingo sign (shifting of weight from one leg to the other) observable in colleagues visibly chomping at the bit to move on during seemingly endless presentations.

For attendings, presentations by students and house officers can also be anxiety-provoking. As the ultimately responsible physicians, they need to integrate the information they hear, separate signal from noise, and figure out what may have been left out and what may be inaccurate. These pressures are magnified by the time urgencies imposed by high-volume case loads, work hour restrictions, and unavoidable multitasking demands. In addition, rounds are a major component of teaching; employing case material in clinically effective and creative ways is one of the great challenges of clinical didactics.
Following is the flow of information recommended in initial case presentations:
Clinical rounds can serve at least six major purposes:
The purpose of this first chapter is to review common pitfalls and how to avoid them in your presentation of information on rounds. In addition, we discuss briefly the presentation of data from the other perspective: that of the hospital-based attending.
Communication problems are especially prevalent in presentations and write-ups by medical students and incipient house officers. However, even more experienced clinicians are not immune to information-conveying “disorders.” Eight of the most common pitfalls you will encounter are summarized below. You and your attending are invited to revise and rework this list.
A number of elements are required for a complete medical history (Exhibit 1.1). If any of this information is not available or not applicable, you should indicate this fact. Some books list things in different order (e.g., are vaccinations medications or part of health care maintenance?—obviously, they are both). Should sexual risk assessment be part of the past medical history or listed separately? Where should a sleep health history be included? A major challenge is learning which elements of the history are of importance in a given context. For example, the details of which coronary arteries were bypassed at the time of prior cardiac surgery are critical data to present when a patient is admitted for recurrent exertional angina, but not when he is admitted for cellulitis. In the latter case, the oral presentation would still need to note his important history of coronary disease, the status following his uncomplicated bypass surgery four years ago, and the most recent follow-up with his cardiologist.
EXHIBIT 1.1 Ingredients of an Adult’s Admission History (Narrative)
1. Chief complaint
2. History of present illness
3. Review of systems
4. Past medical history: childhood; surgical evaluations and procedures/operations; adult medical (including hospitalizations); reproductive (for females: menses; pregnancy/obstetric; psychiatric)
5. Medication profile
(a) Current and prior medications (including herbal/nutritional supplements)
(b) Allergies (immunologic reactions)
(c) Nonallergic adverse drug reactions/intolerances (e.g., nausea with erythromycin)
(d) Recreational or illicit drug use: past and present 6. Personal: habits and health care maintenance
(a) Dietary and exercise history: include food allergies, restrictions, and special needs
(b) Tobacco use: past and present (cigarettes, cigars, chewing tobacco, etc.)
(c) Alcohol: past and present
(d) Screening procedures (e.g., colonoscopy, etc.)
(e) Vaccinations
(f) Injury prevention (e.g., seat belt use)
(g) Screening for abuse, neglect, or domestic violence
(h) Sexual risk assessment (including preferences, birth control, sexually transmitted diseases)
(i) Sleep-related problems (insomnia, loud snoring, daytime somnolence, etc.) 7. Occupational/environmental hazards or exposures (e.g., asbestos, sunburns)
8. Geriatric (as indicated): routine activities of daily living (ADLs): dressing, eating, continence, transfer, toileting, bathing, locomotion, etc.: Instrumental ADLs: shopping, housework, finances, meds, laundry, cooking, etc.
9. Social history: including major relationships and social supports; living arrangements; work status; relevant spiritual and cultural beliefs
10. Family history (including cause and age of death; psychiatric problems)
11. Concerns: financial and insurance-related; impact of illness on job and home life; sexual function; relationships; etc.
12. Advance directive and health care proxy status |
Next, we discuss four selected aspects of major trouble spots in write-ups and case presentations: the CC, HPI, ROS, and PMH.
The chief complaint (CC) sets the tone for the rest of the presentation, analogous to a brief overture to an opera or musical. A major problem with the statement of the CC is a lack of guideposts or pointers. In addition to stating a patient’s actual complaint in his or her words—essential information—it is helpful to include a few orienting phrases, or indicators, to give context to the patient’s admission. These phrases do not bias the analysis but, rather, help the listener process extremely complex information.
As with all elements of the presentation, what you actually decide to present on rounds will differ from what is written in your admission note (which should be as complete as possible, as the reader can choose which areas to focus on, but not be burdened with unnecessary detail). Below are two renditions of the CC on three patients that would be found in an admission note or presented orally. The use of a few guidepost qualifiers (shown in italics) is intended to provide useful context to the admission, without creating listener bias.
The second versions of the CC are preferable in the three cases since they accomplish three goals: the goals are (1) to be concise, (2) to convey specific information, and (3) to conserve a patient’s own words. Using the patient’s own words in the CC [patients rarely, if ever, complain of an “FUO” (a fever of unknown origin) or of “atypical chest pain”] is important. For example, a patient who reports “discomfort” or an “ache” or pressure in his chest, representing angina pectoris, may actually deny that he has “chest pain.” For physicians, all of these terms may be red flags for symptomatic myocardial ischemia or infarction, but your patient may emphatically resist using the word “pain” even when asked specifically.
Two common flaws in presenting a history of the present illness (HPI) are (1) failure to follow a time line—instead, skipping around in a disjointed fashion, and (2) failure to segment the history into subcomplaints when there is a complicated set of problems. As is the case for the CC, you should make a practice of adding guideposts and context to your recounting of the history. Two patients may both present with abdominal pain; the two statements that follow refer to the same chief complaint but have very different contexts essential to the informed listener:
The first is about a long chronic history, the second about an apparently acute event.
Not uncommonly, patients will have multiple complaints or their histories will require several concisely summarized subthemes for clarity of presentation. In the example below, the patient has the two concomitant complaints of hyperglycemia and angina pectoris in the context of known diabetes mellitus and coronary disease:
The key indicator of success for history-telling is how well your listeners grasp the essential information in a concise but sufficiently detailed presentation to serve as the basis of management. If you are constantly being interrupted by your attending and team members, you are probably confusing them or leaving out key information. (Or they are just being rude.) The use of notes (e.g., electronic or manual on a 3 × 5 card) is acceptable, even desirable—but with all records always take care to ensure that HIPAA (Health Insurance and Portability Act) regulations (which serve to protect patient privacy) are being followed (http://www.hhs.gov/ocr/privacy/).
Finally, it is important not to try to convey a specific diagnosis in the history, although one might inadvertently create this type of formulation bias. To quote a catch phrase from the classic TV series, Dragnet: “Just the facts, ma’am.”
The review of systems (ROS) is sometimes mistakenly referred to as the “review of symptoms,” which is imprecise since many ingredients of the ROS have nothing to do with symptoms (which are subjective findings). The ROS is equivalent to a comprehensive verbal body scan. A sample inventory of the conventional ROS is given in Exhibit 1.2.
EXHIBIT 1.2 Major Ingredients of ROS
General/constitutional
Skin
Breast
Head/eyes/ears/nose/mouth/throat
Cardiovascular
Respiratory
Gastrointestinal
Genitourinary
Musculoskeletal
Neurologic
Psychiatric
Allergic/immunologic/lymphatic
Rheumatologic
Endocrine |
Perhaps the major pitfall in obtaining the ROS is failure to be comprehensive. This shortcoming may be due to lack of time, emergency situations, when information gathering is necessarily truncated by multiple admissions and other stresses on the medical system itself, and by limitations in the patient’s own recollection and knowledge. At least three strategies can be used to avoid these pitfalls:
At the same time, the verbal presentation of a comprehensive ROS too often becomes a time sink. Students and house officers often give an exhaustive and exhausting recitation of positives and negatives. Although essential to the written history, this type of extra information causes the oral presentation to bog down.
The most condensed form of presentation is simply a statement that the “Review of systems is positive for … ” followed by the relevant information. Be mindful of situations in which the ROS is “grossly positive.” Furthermore, if truly relevant to the CC, the pertinent positives or negatives might be given in the HPI. From the example above, additional information would help frame the context of the abdominal pain: Mrs. Jones denies any melena, hematochezia, weight loss, or loss of appetite.
In the example of a 50-year-old patient who presents with documented fevers up to 101.7°F and night sweats for a month, the differential diagnosis centers importantly on infection (e.g., HIV, bacterial endocarditis, tuberculosis), and cancer (especially lymphoma). A concise ROS could be:
However, again, it may be preferable to include these key positives and negatives in the HPI.
Similarly, the family history can be an aspect of the presentation that gets bogged down with excessive detail or weakened by inadequate history taking. For example, in a patient admitted with cholecystitis, relaying that the patient’s parents had asthma is not important. In a 65-year-old man admitted with chest pain, knowing that his father had an MI when he was 50 years old is extremely helpful. Furthermore, sometimes valuable clues may be “buried” and emerge only after some detective work.
FIGURE 1.1 Normal and long QT intervals.
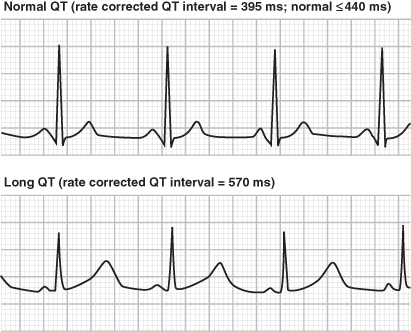
In this example, detailed history taking helped uncover the diagnosis of a subtle but life-threatening cardiac electrophysiologic syndrome. The family history prompted genetic testing for one of the more common inherited causes of sudden cardiac arrest. (Obviously, genetic screening is inappropriate for every patient who presents with palpitations and light-headedness. The long-term management of patients such as this, as well as for patients who have the genetic mutation but who are asymptomatic, is a subject of much debate.)
A past medical history (PMH) must be presented in full as part of the admission note. Based on the attending’s preferences and specialty, it may be thematically subgrouped into past medical, past surgical, past psychiatric, past obstetric, and so on. At times, as with the examples above of coronary artery disease and diabetes mellitus, details of the past history are presented in the HPI because of their immediate relevance to these two major disease processes. What if the patient is being admitted for a problem (e.g., a tibial fracture after being hit by a bicycle) that is not apparently related to coronary disease or diabetes? In such cases, the details of these two problems could be presented separately in the PMH section. However, because of the multisystem nature of conditions such as diabetes mellitus, which may affect therapy, if not diagnosis, on rounds one might present the past medical history succinctly by saying “the patient’s past medical history is notable for asymptomatic coronary artery disease, status post angioplasty of the left anterior descending artery two years ago, and for stable type 2 diabetes mellitus, which is diet-controlled.” In the write-up, appropriate details can be provided.
Finally, uncovering the past medical history may be challenging, especially if the patient is a “poor historian” because of age, complicated management, stress, effects of a chronic or acute process on memory, and if reliable medical records are incomplete or unavailable. In some cases, a patient’s medications may be helpful (see below). As an example, if the patient is known to be on metformin and glipizide, the diagnosis of diabetes mellitus is virtually assured. On the other hand, finding that the patient is on digoxin does not necessarily mean that he or she has heart failure or an atrial arrhythmia—often, patients are still on medications prescribed years ago for a remote or even misdiagnosed problem, or when “archaic” prescriptions are never discontinued. A certain amount of imaginative detective work may be required with calls to physicians named on prescriptions, the pharmacies, and of course, family members with instructions to “bring in all the pill bottles” as discussed further below.
The importance of a complete medication history cannot be overemphasized. The medication profile should include both current and, where possible to document, prior medications and adverse medication reactions. This category includes two distinct features that are very different but often confused, especially by patients: (1) allergies and (2) side effects and intolerances. Furthermore, a variety of sources suggest that at least 10–20% of Americans use herbal or other supplemental medications, and most often do not report this use to their medical practitioners.
A common and important error is to give an incomplete rendering of a patient’s drug history or current medication profile. For example, a typical statement might be:
What is missing from this summary?
Is Mr. Kramer actually taking the medications as prescribed? A consistent finding in medical surveys is the low level of adherence with prescribed medications. Just because a patient relates “being on” certain medications is no guarantee that the medications are actually being taken as prescribed, or taken at all. Adherence rates as low as 43–78% have been reported for patients taking medications prescribed for chronic conditions. Such nonadherence can have major consequences during a hospital admission, as the patient is usually guaranteed to receive those medications as prescribed rather than the dosages actually taken at home. For example, in cases such as “treatment-resistant” hypertension, precipitous falls in blood pressure may occur upon exposure to the assumed doses of antihypertensives.
Many reasons for nonadherence are identifiable (Exhibit 1.3), including inability of the patient to afford the medication; unreported intolerance or side effects (not actual allergies) of the medication (e.g., headache, nausea, diarrhea), confusion about the indication for the medication, lack of belief in the therapy, contradictory inputs from multiple caregivers, psychiatric syndromes, and multidose regimens.
EXHIBIT 1.3 Major Predictors of Poor Adherence to Medication
Source: Adapted from Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497.
Presence of psychological problems, particularly depression
Presence of cognitive impairment
Treatment of asymptomatic disease
Inadequate follow-up or discharge planning
Side effects of medication
Patient’s lack of belief in benefit of treatment
Patient’s lack of insight into the illness
Poor provider–patient relationship
Presence of barriers to care or medication
Missed appointments
Complexity of treatment
Cost of medication, copayment, or both |
Even among professional caregivers, compliance rates are rather low. One study of physicians and nurses by Rhonda Corda, M.P.H., and her colleagues at New York Medical College (2000) revealed that only about 80% of respondents reported taking medications properly 80% or more of the time. As the authors noted, expecting patients to exceed their physicians in compliance with medications is unlikely.
An important and probably underreported source of medication errors is the tendency to automatically transcribe in admission orders the same medications that a patient reported to be taking at home or on transfer in the identical doses. A related common pitfall is to use the discharge medications from a prior hospitalization list as a surrogate for a current medication profile because that list reflects medications the patient was reliably receiving and taking while hospitalized. This “reflex” can have a number of serious and even fatal consequences. The admission itself may be due to a medication allergy or intolerance. Reordering the same panel of medications may therefore inadvertently perpetuate the disease process that caused the admission. As such, medication reconciliation is absolutely critical to patient care. This term (see Exhibit 1.4) refers to the interactive multistage process of identifying and cross-checking the most accurate, updated list of all medications your patient is taking, including name, dosage, frequency, and route, and then using this list to provide correct medications for the patient anywhere within the health care system.
EXHIBIT 1.4 The Four Steps of Medication Reconciliation
Step 1: Obtain and document the most complete and accurate list possible for all current medications.
Step 2: Compare the “home medications” listed with any new orders, to reconcile discrepancies.
Step 3: Update the list as orders change during the clinic/office visit or hospital stay and make necessary and appropriate medication changes based on the patient’s clinical condition.
Step 4: Communicate the updated list to the next provider of service and to the patient when the patient is transferred to another setting, service, practitioner, or level of care within or outside the organization. |
Lack of medication reconciliation can have serious and even life-threatening effects and accounts for an estimated 50% of all medication errors and up to 20% of adverse drug events in the hospital setting. In the example above, failure to document the actual dose of insulin led to a series of life-threatening complications.
In the case of Mr. Kramer, mentioned earlier, a preferable statement would be:
Other consequences of reflex prescribing include giving medications that may interfere with imminent surgical procedures (e.g., warfarin) and continuing medications that interact with one or more drugs that are being added to the current regimen without consideration of dose modification. Digitalis toxicity, including potentially serious brady- or tachyarrhythmias, may ensue.
In this case, the seemingly nonspecific complaints of an elderly man turn out to be symptoms of a life-threatening iatrogenic problem: digitalis toxicity. Digoxin interacts with numerous commonly prescribed drugs, especially those taken by patients with heart failure, for which digoxin is often prescribed (thiazide and “loop” diuretics, calcium-channel blockers, and antiarrhythmics). Amiodarone increases the steady-state concentration of digitalis and may cause a twofold increase in the serum digoxin level. As such, maintenance doses of digoxin should be reduced by 50% in those also taking amiodarone.
This case also raises another important issue: the potential overuse of drugs without documented indications. Digoxin has a narrow therapeutic margin and is mainly indicated in chronic symptomatic systolic heart failure and as an adjunct to maintaining a controlled ventricular response in atrial fibrillation (see Chapter 8). Further, the use of digoxin to prevent atrial fibrillation has not been documented. In retrospect, its use in this case, where the patient was discharged in sinus rhythm without heart failure, lacked compelling justification.
As mentioned above, an important but often overlooked aspect of the medication history is documentation of nonformulary medications and supplements. This topic has received increased attention in the medical and popular press recently, with the important finding that substantial numbers of patients in the United States and other countries take a variety of complementary and alternative medications and utilize a wide range of interventions outside the sphere of traditional medical practice. This phenomenon is, of course, independent of the “recreational” use of illegal substances, which is also widespread and an essential part of the medical history.
Comment: This vignette is important because it illustrates how elucidating a “hidden history”—in this case, taking St. John’s wort—averted potentially life-threatening complications. This herbal supplement can have major interactions with HIV treatment (lowering serum concentrations) along with many other commonly prescribed medications [e.g., warfarin (reduced effect), paroxetine (grogginess and lethargy), oral contraceptives (reduced efficacy), and cyclosporine (reduced levels)]. Another example is provided by garlic (Allium sativum) supplements, which may reduce the level of certain protease inhibitors, such as saquinivar, and enhance the effects of antiplatelet agents and of warfarin. Certain herbal medications may also affect anesthetic management.
Exhibit 1.5 is a more comprehensive list of substances considered as medications that goes well beyond prescribed and nonprescribed pharmacy-type agents (e.g., vaccines, radioactive preparations, blood derivatives, respiratory therapy-related agents, and a variety of others).
EXHIBIT 1.5 What Is a Medication?
Prescription medications
Sample medications
Vitamins
Nutraceuticals (e.g., dietary supplements and herbal products)
Over-the-counter (nonprescription) drugs (e.g., common allergy and cold formulations)
Vaccines
Diagnostic and contrast agents
Radioactive medications (e.g., radioactive iodine for hyperthyroidism)
Respiratory therapy-related medications
Parenteral nutrition
Blood derivatives
Intravenous solutions (plain or with additives)
Any other product designated as a drug by the U.S. Food and Drug Administration |
Note: This official list, based on the Joint Commission, does not include biologically active chemicals that you might have added as other candidate “drugs,” including recreational/illicit substances, caffeinated drinks, and nicotine-containing tobacco products. Is exercise a medication? What about certain types of light exposure? What else is missing from this list?
Take care not to confuse true medication allergies (i.e., immunologically mediated effects such as rash, laryngospasm, bronchospasm, angioedema, pruritis, and urticaria) with medication intolerance or other nonimmunological side effects (e.g., nausea, weakness, diarrhea, headache, dizziness). Furthermore, not infrequently, patients mistake an allergy for a drug’s pronounced desired effect (e.g., bradycardia with beta-blockers, nausea with disulfuram). In the latter example, the fact that an adverse effect is not a true allergy does not mean that it cannot be life-threatening. Consider hypotension and bradycardia due to blood pressure medications, which may induce syncope, with disastrous consequences. Another class of examples includes the proarrhythmic effects of drugs used to treat arrhythmias (e.g., flecainide, propafenone). Such drugs may actually cause or promote life-threatening electrical instability associated with cardiac arrest and sudden death (N Engl J Med. 1989;321:406–412).
Always review allergies and intolerances, as several medications that are routinely (and automatically) prescribed on standardized order sets on hospital admission (e.g., acetaminophen, diphenhydramine, promethazine, prochlorperazine, morphine sulfate) may cause allergies or side effects. More often than not, some of the allergies reported are wholly incorrect, and preclude the use of that agent in favor of one that may be more expensive or less effective.
For example, in patients following acute myocardial infarction, aspirin decreases risk for recurrent infarction and for death. However, a reported allergy to aspirin may preclude providers from administering this medication when in truth the “allergy” is simply an instance of gastrointestinal upset. True allergies to aspirin do occur but are relatively rare.
[I]t’s easy to write prescriptions, but difficult to come to an understanding with people.
—FRANZ KAFKA (1883–1924), Country Doctor
The discussion above on presenting cases, directed primarily at students and house officers, is aimed at improving their communication skills vis-à-vis each other and their attendings. However, attendings have an added challenge beyond deciphering often overly long and less than optimally organized presentations. They not only need to assimilate and integrate the data and vet its reliability but also need to interrupt the presentation at selected points for clarification and teaching purposes. Individual preferences will guide whether one favors letting a presentation run its course or whether interruptions are helpful. The authors favor the latter, especially during walking or sitting-down teaching rounds. One particularly useful strategy for attendings (and residents) is to freeze the presentation at key stages and ask what members of the team are thinking. This procedure will not only help prevent junior colleagues from having mental “walkabouts,” but is also essential for developing skills in actively processing information and developing differential diagnosis skills.
For example, you are listening to a presentation that begins:
A dramatic device for teaching, and one that may help elucidate the cause of this patient’s dyspnea, is to stop the presentation abruptly and ask: What is the differential diagnosis of dyspnea in a 37-year-old woman given no other information? The ensuing discussion, which can be brief, would encompass (1) pulmonary (thromboembolic syndromes, obstructive disease, restrictive disease due, for example, to infection, metastatic cancer or pleural effusion with lung compression, pneumothorax, etc.), (2) cardiac (heart failure or an anginal equivalent), (3) metabolic (anemia, or acidosis with Kussmaul respiration), and (4) psychogenic (anxiety) etiologies.
As the case develops, you can interrupt again to ask how the new information helps focus on one or more of the initial broad range of possibilities or what was not mentioned that may be relevant (e.g., recent travel with prolonged sitting on a plane, or intake of oral contraceptives, both of which would increase the pretest probability of thromboembolic disease). No prescription exists or should exist for how many times per diem a presentation should be freeze-framed or what the questions should be. Indeed, scores of possibilities exist as the attending becomes a role model of active listening and clinical hypothesis generation and testing.
Overall, it is helpful to point out, up front, what you expect from student presentations, and be aware that it is likely to differ from others’ preferences. Students will always adopt their own styles and preferences as they become more senior, and their preferred method of hearing and giving presentations may be biased toward what they learn early on—in both positive and negative ways.
The term teachable moment has entered politics as well as medicine and other disciplines. The authors declare their bias/opinion here that the term, like most buzzwords, has lost whatever meaning it may originally have had. In medicine, all “moments” are potentially teachable, constrained only by time and priorities. Selecting the obvious ones weights them unduly and may draw attention away from the equally important but less apparent “clinical pearls.”