CHAPTER 4
Looking into the ADD Brain and the Discovery of the ADD Types
My path to looking into the brain started in an unlikely place: at a military hospital in the middle of nowhere. I did my psychiatric training at the Walter Reed Army Medical Center, now renamed Walter Reed National Medical Center in Washington, D.C. I had been an infantry medic in the early 1970s during the Vietnam War and the GI Bill helped to support me through college and medical school. Walter Reed was the premier military hospital in the world, responsible for the medical care of soldiers, family members, and international political figures. After three years at Walter Reed, I went to Honolulu, Hawaii, to do a child and adolescent psychiatry fellowship at Tripler Army Medical Center. Military training was very practical. Learning about combat psychiatry and taking care of soldiers and their families in times of crises did not leave one with the inclination to become married to any particular psychiatric dogma or tradition. We learned to use what worked, what was helpful, what made a difference—right then and there.
After my formal specialty training in psychiatry, I was stationed at Fort Irwin, forty miles north of Barstow, in California’s Mojave Desert. Halfway between Los Angeles and Las Vegas, Fort Irwin was also known as the National Training Center—the place where American soldiers were taught to fight the Russians (and later the Iraqis) in the desert. At the time, I was the only psychiatrist for four thousand soldiers and an equal number of family members. It was considered an isolated assignment. There were problems with domestic violence, drug abuse (especially amphetamine abuse), depression, and ailments resulting from the stress of living in the middle of nowhere. I dealt with many people who suffered from headaches, anxiety attacks, insomnia, and excessive muscle tension.
Shortly after arriving at Fort Irwin, I went through the cabinets in the community mental health clinic to see what instruments and psychological tests my predecessors had left behind. To my delight, there was an old Autogen biofeedback apparatus that measured hand temperature. There was one lecture on biofeedback during my psychiatric training. The concept of biofeedback is fascinating: If you get feedback on the physiological processes in your body, such as hand temperature or heart rate, you can learn to change them through mental exercise and discipline. The problem with biofeedback, as I knew it at that time, was that the training was boring. The needles and dials on the machines were not interesting to patients. Nonetheless, the old machine was dusted off and we used it with patients who had migraine headaches. I taught them how to warm their hands, using only their imagination. It was fascinating to see how patients could actually warm their hand temperature, sometimes as much as 15 to 20 degrees. Temperature training taught patients how to participate in their own healing process.
In late 1987, six months after coming to Fort Irwin, I wrote a request to Colonel Knowles, our hospital commander, to buy the mental health clinic thirty thousand dollars’ worth of the latest computerized biofeedback equipment, including ten days of training for me in San Francisco. He laughed at me: He said that the Army didn’t have the money (this was at a time when they were spending six hundred dollars on hammers and toilet seats) and that when my assignment at Fort Irwin was over, the equipment would just end up in a closet somewhere, much like the equipment I had found. I dropped the idea but continued using the old temperature trainer. In May 1988, Colonel Knowles called me into his office. He asked if I had kept a copy of the biofeedback proposal. When I said yes, he authorized its funding. In the Army at the time if a unit did not spend its entire annual budget in one year, they lost the unspent portion the next year. We had money left over, and the colonel wanted to make sure he spent it all. I was very excited: Great new equipment, and ten days in San Francisco!
The biofeedback training course in San Francisco changed my life. It was the most stimulating and intense learning experience I had as a physician. The ten-hour days went by in a flash. The new computerized biofeedback equipment was patient-friendly, interesting, and easy to learn. I learned how to help people relax their muscles, warm their hands (much faster than with the old equipment), calm sweat-gland activity, lower blood pressure, slow their own heart rates, and breathe in ways that promoted relaxation.
The lectures on brain wave biofeedback were the most amazing. I was taught that people can learn how to change their own brain wave patterns. What an exciting concept, being able to change your own mental state! I also learned about Dr. Joel Lubar’s research at the University of Tennessee on brain wave underactivity in children with ADD. In published research using quantitative electroencephalograms (qEEGs), Dr. Lubar demonstrated that ADD children had excessive slow brain wave activity in the front part of their brain, which worsened when they tried to concentrate. This diminished activity, when compared to a group of people without ADD, made perfect sense to me. Psychostimulants, such as Dexedrine and Ritalin, were the treatment of choice for calming hyperactive children and helping them concentrate. I was taught that these medications exerted a “paradoxical effect”: a stimulant calming down a hyperactive child. Understanding Dr. Lubar’s research meant that psychostimulants probably corrected the underactivity in the ADD brain—not a paradoxical effect, but rather a direct effect: stimulating the brain’s frontal lobe so that the brain could calm and focus the person.
Dr. Lubar’s work gave me a critical insight: the importance of looking at the brain in different thought states. He studied people with ADD at rest and while they were doing concentration tasks. After all, people with ADD have problems when they try to concentrate, not when they are at rest.
Dr. Lubar also demonstrated that many children can develop more normal brain wave patterns (and therefore improved focus and behavior) through brain wave biofeedback, also called neurofeedback. In brain wave biofeedback, electrodes are placed on the scalp and connected to computerized biofeedback equipment. The computer screen shows the patient his or her own moment-by-moment brain wave patterns. By knowing these patterns, many patients can learn to change them to more normal, more focused patterns. When I first heard this I was interested, but very skeptical: How can you change your brain? I started talking to other clinicians around the country doing this work who were getting exciting results. Why not change your brain? After all, if you can warm hand temperature by 20 degrees, why can’t you increase the amount of focused brain wave activity?
When I returned to Fort Irwin, I tried everything I had learned. I did biofeedback on almost all of the patients who came to see me. I loved it. My patients loved it. I also spent time each day doing it myself. I became a master at breathing with my diaphragm. I could slow my heart rate. And I could even warm my own hands over 15 degrees whenever I felt stressed. I also started to evaluate ADD children with EEG measures. Many of them, although certainly not all, demonstrated the same patterns that Dr. Lubar had written about. Many of them benefited from biofeedback training. I had to learn more.
In 1989 my commitment to the U.S. Army ended and I started a private practice in Fairfield, California. I bought my own biofeedback equipment and continued using it in clinical practice. Also, I became the medical director of the dual diagnosis unit (where patients had both substance abuse and psychiatric problems) at a local psychiatric hospital. I instituted the use of biofeedback throughout the hospital. My interest in biofeedback and evaluating brain function in ADD patients grew each year. In late 1990 and early 1991 it exploded.
In October 1990, Alan Zametkin, M.D., of the National Institutes of Health published an article in the New England Journal of Medicine on brain PET (positron emission tomography) studies in ADD adults. PET studies are sophisticated nuclear medicine studies that evaluate glucose metabolism, blood flow, and activity in the brain. His research showed that when ADD adults concentrate, there is decreased activity in the prefrontal cortex. There was quite a buzz in the medical community. This meant that ADD was real: It is a medical problem you can actually see. For many people this was a paradigm shift. I wasn’t quite as excited as many of my colleagues. Dr. Lubar had virtually said the same thing many years earlier, using EEG scalp measurements. But I was excited about the developing new technology to help study our patients. Shortly after Dr. Zametkin’s article appeared, I attended a lecture at the hospital by Jack Paldi, M.D., a nuclear medicine physician, who taught us about brain SPECT imaging.
SPECT (single photon emission computed tomography), like PET, is a nuclear medicine study that evaluates brain blood flow and activity patterns. Dr. Paldi said that SPECT was easier to perform, less expensive, and involved less radiation than PET studies. He showed SPECT images of patients with depression, dementia, schizophrenia, and head trauma. He showed brain images before and after treatment. Unlike the PET researchers who felt that their technology was still very experimental, Dr. Paldi said that, in his opinion, SPECT was ready to be used clinically and it could provide useful diagnostic information for psychiatric patients. I was intrigued. When he offered physicians no-cost SPECT scans to try them out, I took him up on his offer. The same day of Dr. Paldi’s lecture, I met Sally.
Sally, a forty-year-old woman, had been hospitalized for depression, anxiety, and suicidal ideas. In my clinical interview with her I discovered that she had many ADD symptoms, such as short attention span, distractibility, disorganization, and restlessness. She had an ADD son (a frequent tip-off in diagnosing ADD in adults). She had never finished college, despite having an IQ of 140, and she was employed below her ability.
When I mentioned the possibility of adult ADD to her, she didn’t want to think it applied to her and was not open to treatment for it. She had minimized her symptoms. Since I had just heard Dr. Paldi’s lecture and read Dr. Zametkin’s paper, I asked her if it would be okay to study her brain with SPECT. She was intrigued by the idea. I called the University of Wisconsin, known for research in brain SPECT studies, and asked them how to perform the scans on an ADD adult. They gave us their protocol: a rest study, with the patient doing nothing, and then two days later a concentration study done while the patient performs a series of random math problems.
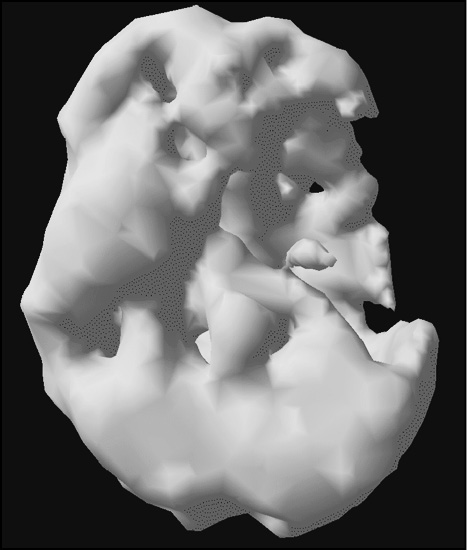
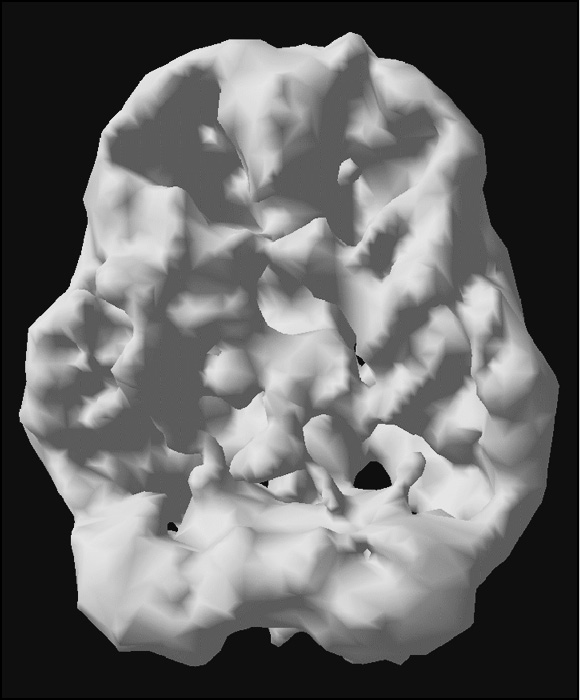
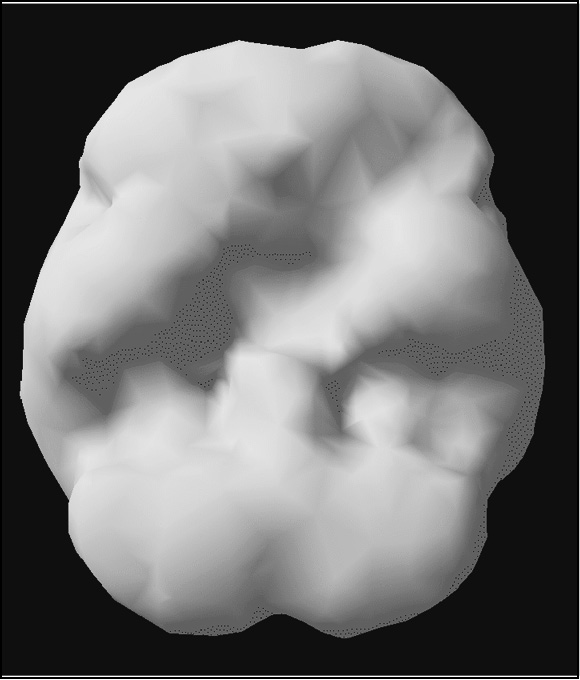
Sally’s concentration study was abnormal. At rest, she had good overall brain activity, especially in the prefrontal cortex. When she performed the math problems, she had marked decreased activity across her whole brain, especially in the prefrontal cortex! This correlated with Dr. Lubar’s EEG finding and Dr. Zametkin’s paper.
When I showed her the scans she started to cry and said, “You mean it is not my fault?”
“Right,” I said, taking the glasses I wear to drive out of my coat pocket, “having ADD is just like people who need glasses. People who wear glasses aren’t dumb, crazy, or stupid. Their eyes are shaped funny and we wear glasses to focus. For people who have ADD, they are not dumb, crazy, or stupid. Their prefrontal cortex shuts down, when it should turn on. And they need treatment to keep their prefrontal cortex working properly, so they can focus.”
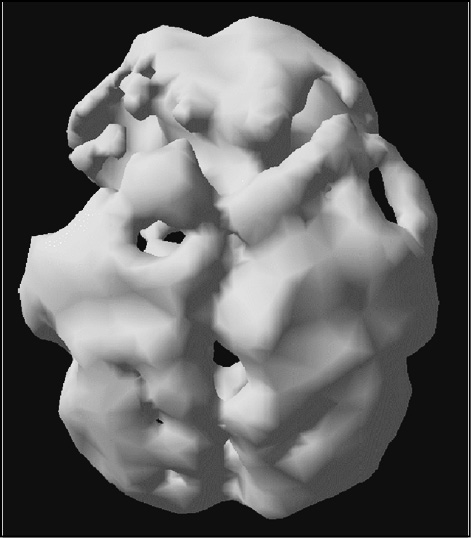
Sally’s SPECT Studies (Underside Surface Views)
Good activity at rest
Marked drop-off with concentration
The analogy made sense to Sally, and she had a wonderful response to a low dose of a stimulant medication. Her mood was better, she was less anxious, and she could concentrate for longer periods of time. She eventually went back to school and finished her degree. No longer did she think of herself as an underachiever, but rather as someone who needs treatment for a medical problem. Seeing the pictures were very powerful for Sally. Watching her facial expression when she saw her own scans led me to believe that SPECT may have a powerful application in decreasing the stigma many patients feel when they are diagnosed with a “psychiatric” problem. It makes them realize that these conditions are not just manifestations of a weak will or poor conduct. The scan and her response to medication changed the perception she had about herself. I have seen the reaction Sally had to her scans many, many times over the last twenty-two years.
With Sally’s positive response to treatment fresh in my mind, I ordered more SPECT studies, especially on my most difficult patients. I found SPECT immediately useful in a number of different ways. I was able to “see” areas of good brain function and areas of compromised function. I could see areas of the brain that worked too hard and areas of the brain that did not work hard enough. I read everything I could on brain imaging, especially SPECT. A number of my colleagues at the hospital where I worked also ordered SPECT studies on their patients. To my surprise, by early 1991 there was already a very large body of medical literature on SPECT imaging for psychiatric indications.
At this point in the story it is important to understand a bit about SPECT technology. SPECT is a nuclear medicine study that evaluates blood flow and activity in the brain. A radioisotope (which, as we will see, is akin to a beacon of energy or light that emits gamma rays) is attached to a medicine that is readily taken up by the cells in the brain. A small amount of this compound is injected into a vein in the patient’s arm, from which it runs throughout the bloodstream and a portion is taken up by cells in the brain. The patient then lies on the SPECT table for about fifteen minutes while a camera rotates slowly around his head. The camera has special crystals that detect where the medicine (signaled by the gamma rays or pieces of light) has gone. The SPECT camera is open and no one feels claustrophobic, which is common with MRI-based procedures. A supercomputer then reconstructs 3-D images of brain activity levels.
The images that result give us blood flow/activity brain maps. With these maps, physicians have been able to identify certain patterns of brain activity that give us specific information on how your brain works.
Nuclear medicine studies measure the physiological functioning of the body and can be used to diagnose a multitude of medical conditions: heart disease, certain forms of infection, the spread of cancer, and bone and thyroid disease. Brain SPECT studies help in the diagnosis of head trauma, dementia, atypical or unresponsive mood disorders, strokes, seizures, the impact of drug abuse on brain function. At the Amen Clinics we have also used SPECT to subtype complex forms of ADD, anxiety, depression, addictions, obesity, aggression, and patients who have failed common treatments.
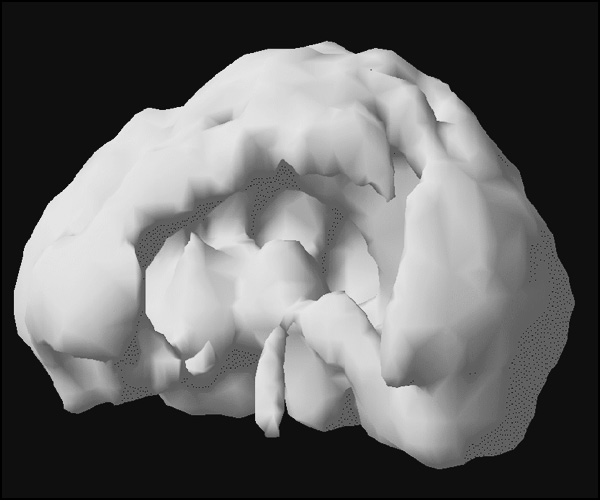
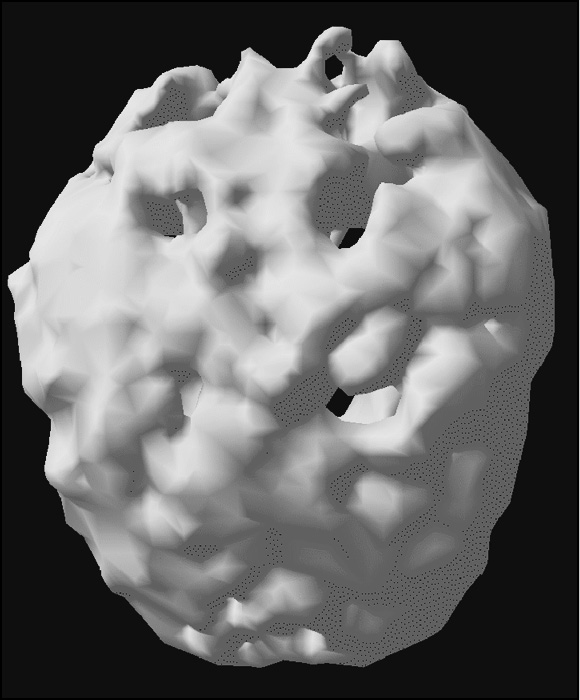
SPECT can be displayed in a variety of different ways. Traditionally the brain is examined in three different planes: horizontal (cut from top to bottom), coronal (cut from front to back), and sagittal (cut from side to side). What do physicians see when they look at a SPECT study? We examine it for symmetry and activity levels and compare it to what we know a healthy brain looks like. You will see two types of 3-D images in the book. One kind is a 3-D surface image, looking at the blood flow of the brain’s outside surface. These images are helpful for picking up areas of healthy activity and low activity. They give insight into the effects of strokes, brain trauma, drug abuse, etc. A normal 3-D surface scan shows good, full, symmetrical activity across the brain’s cortical surface.
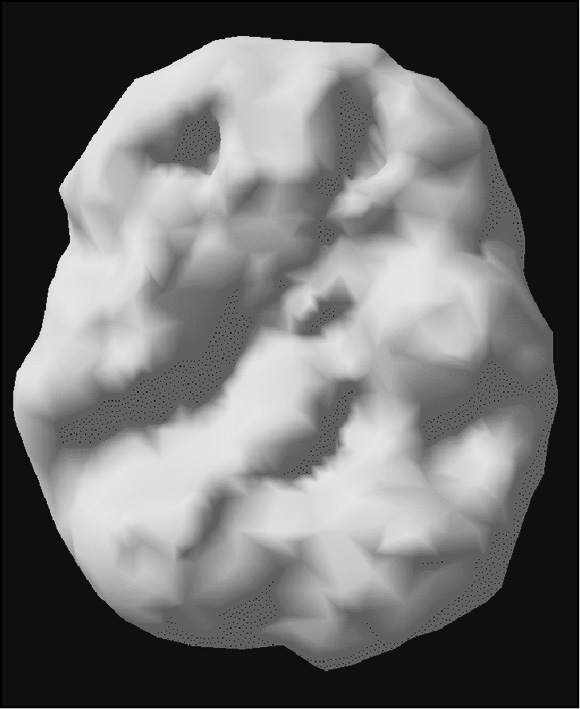
The other kind is a 3-D active brain image, which compares average brain activity to the most active 15 percent. These images are helpful for picking up areas of overactivity, as seen in active seizures, obsessive-compulsive disorder, bipolar disorder, anxiety problems, certain forms of depression, etc. A normal 3-D active scan shows increased activity (seen by the light color) in the back of the brain (the cerebellum and visual or occipital cortex) and average activity most everywhere else (shown by the background grid). Physicians are usually alerted that something is wrong in one of three ways:
(a) they see too much activity in a certain area;
(b) they see too little activity in a certain area; or
(c) they see asymmetrical areas of activity.
In addition, other SPECT studies were published on dementia, stroke, head trauma, depression, schizophrenia, and drug abuse. In 1992, I went to the American Psychiatric Association’s (APA) Annual Meeting in Washington, D.C. To my excitement I met other psychiatrists using SPECT, particularly Thomas Jaeger from Creighton University in Omaha, Nebraska, who had extensive experience with it. Dr. Jaeger and colleagues were presenting an all-day course on how to utilize brain SPECT imaging in child psychiatry. I was very excited.
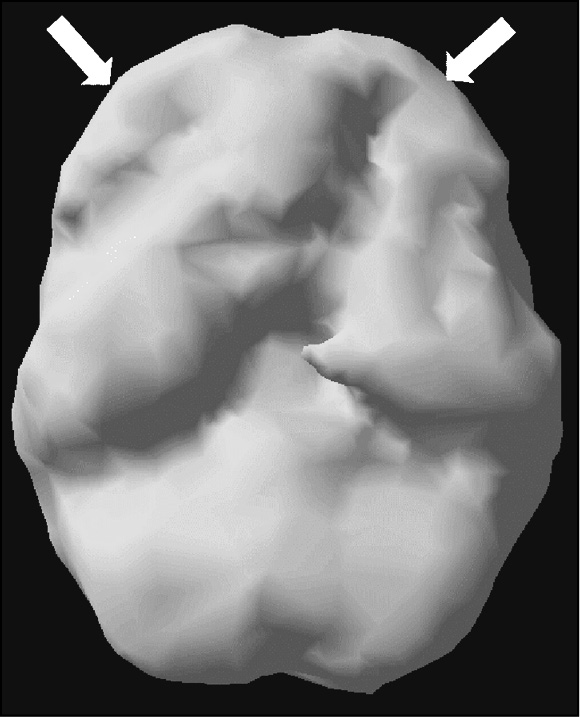
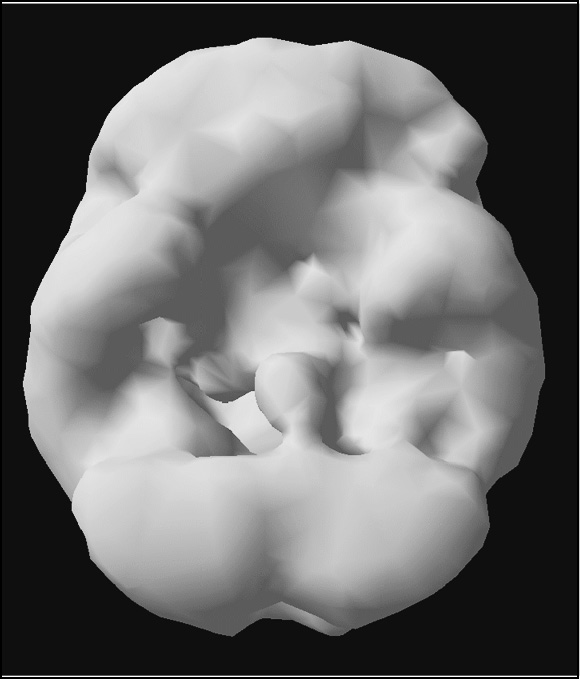
Healthy SURFACE SPECT Scan
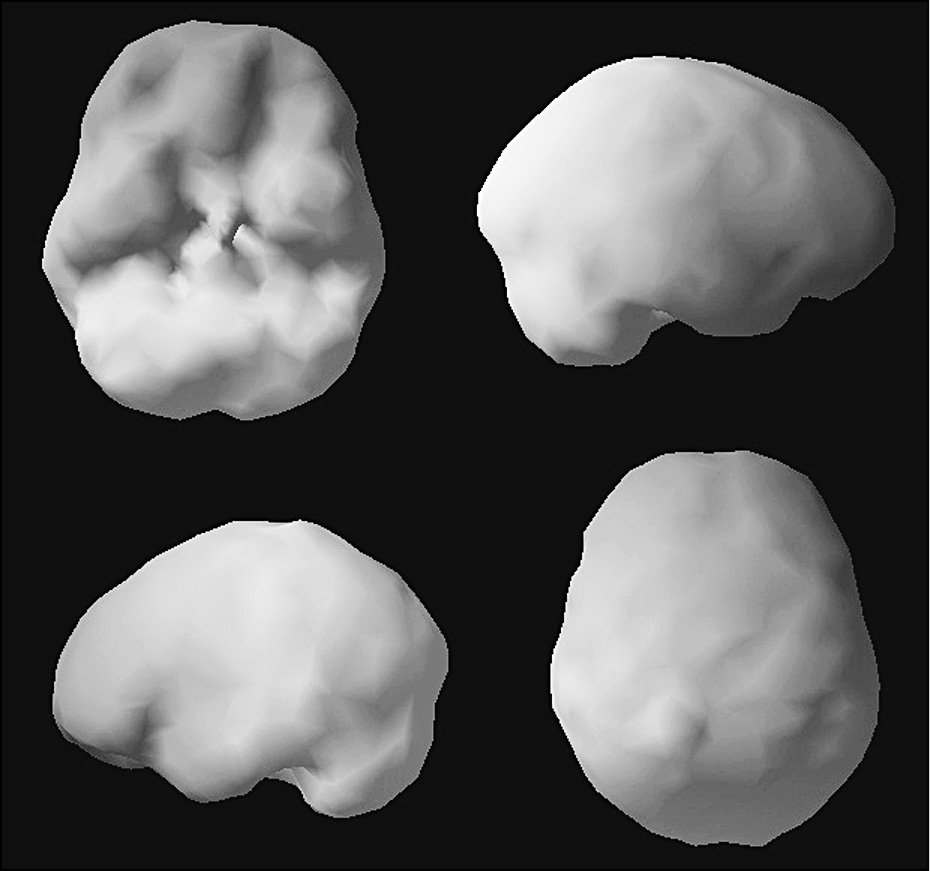
Note full, even, symmetrical activity. Top left image is looking underneath the brain, bottom right image is looking down from the top, the other two are looking at the brain from the sides.
The day of the course, however, was my first sense that a storm was brewing in the brain-imaging world. I went to hear a lecture by Dr. Zametkin, who had led the PET research on ADD in adults. After the lecture I went up to him and told him that, partially based on his work, I was using brain imaging in my clinical practice and that I found it very helpful. He gave me an angry look and said that the imaging work was just for research: It wasn’t ready for clinical use, and we shouldn’t use it until people like him gave us the okay. I protested, giving him example after example of how it was helpful, but it was clear he did not want to hear it. I told him about the all-day course by Dr. Jaeger and his group. He said that he should go “crash their party and set them straight.” I was livid. There was such a chasm between clinical practice and research-based physicians.
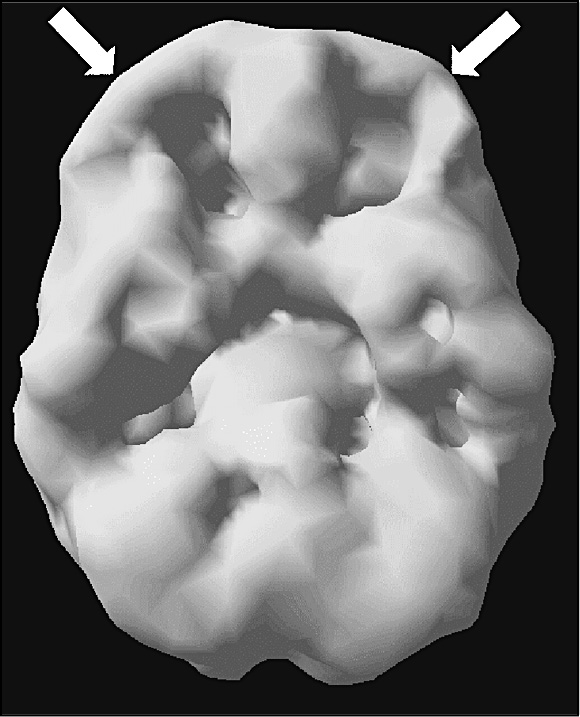
Healthy ACTIVE SPECT Study
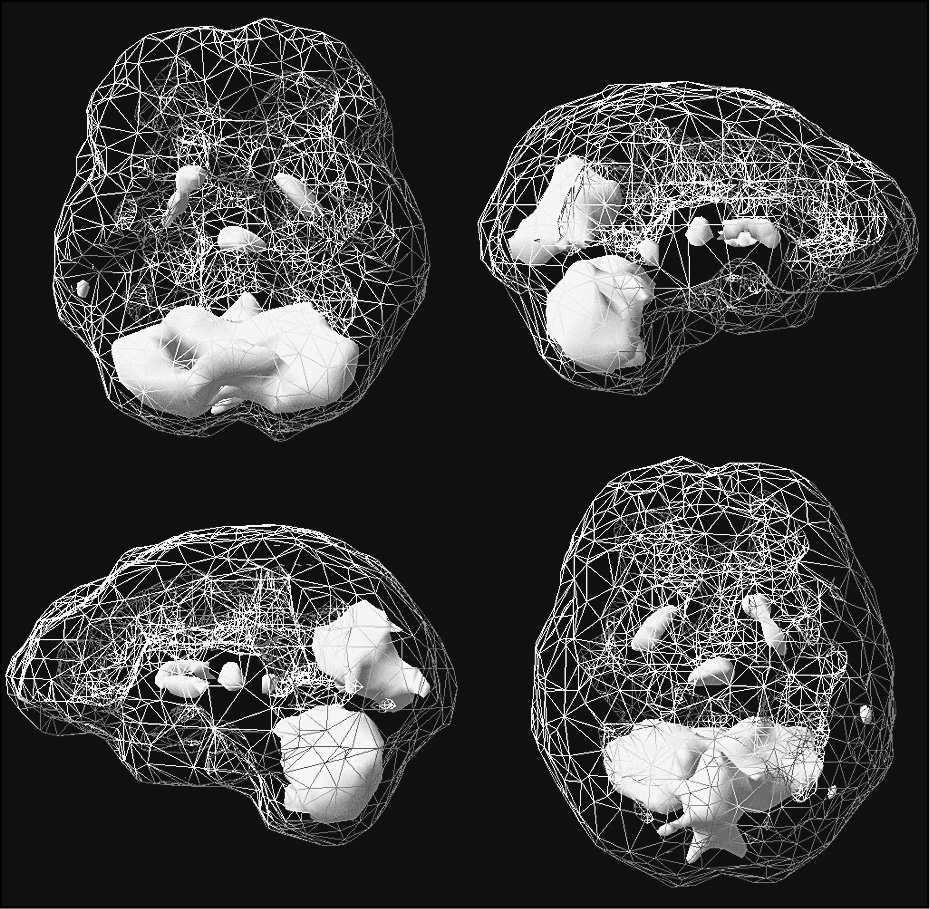
Grey = average activity, white is top 15 percent or most active areas. Typically in a healthy brain cerebellum the back bottom part of the brain is most active.
Dr. Jaeger’s course was wonderful. He showed all of the different ways SPECT could be applied in a clinical setting: with ADD, depression, bipolar disorder, head trauma, drug abuse, etc. In the APA program abstract Dr. Jaeger wrote, “Regardless of the initial diagnosis, patients who underwent brain SPECT prior to, or during, psychiatric hospitalization had markedly shorter stays than controls. As demonstrated by this clinical database (two thousand patients), brain SPECT may lead to more effective, shorter, safer, and less expensive diagnostic and treatment modes in children and adolescents with suspected neuropsychiatric illness.” His experience completely dovetailed with mine.
I wondered, “How can we not look at the brain?” Cardiologists look at the heart, orthopedic doctors have X-rays to examine bones, gastroenterologists look at the gut, pulmonologists look at the lungs, every other medical specialist looks at the particular organ they treat. And, we deal with the most complicated organ in the body. How can we treat it without having any information on how it functions? Psychiatrists are the only medical specialists who never look at the organ we treat!
By 1993, I had ordered several hundred SPECT studies on my patients, and I continued to find them helpful and fascinating. I started to lecture about the findings. I was asked to give grand rounds at local hospitals and then at the University of Colorado School of Medicine. I wrote a research article based on our findings with ADD children.
We performed brain SPECT studies on fifty-four medication-free ADD children and adolescents. We compared this group to eighteen medication-free children and adolescents who did not have ADD. The studies were performed at rest and while the patients were doing a concentration task. Sixty-five percent of the ADD children and adolescents diagnosed with ADD had significant decreased activity in the prefrontal cortex when they tried to concentrate, compared to only 5 percent of those who did not have ADD. Of the nineteen ADD patients (34 percent) who did not suppress their prefrontal lobe activity with concentration, twelve (63 percent) had decreased prefrontal cortex activity at rest.
In 1993, Dr. Jaeger asked me to help teach the brain-imaging course at the 1993 American Psychiatric Meeting in San Francisco. The enthusiasm was growing, as were the naysayers. Within two years of starting our brain imaging work my colleagues and I created a firestorm of criticism among our colleagues. “Psychiatrists don’t do this” was something we heard a lot. Being naturally anxious, I hated the criticism. It caused sleepless nights and a general underlying uneasiness. For over a year I stopped talking about the work at our clinic. I was trying to figure out how to handle the conflict.
Then late one night in April 1995, I received a phone call from my sister-in-law Sherrie who was in tears. She told me that Andrew, my nine-year-old nephew and godson, had attacked a little girl on the baseball field that day for no particular reason. The attack was unprovoked and out of the blue. Sherrie told me that for the last year Andrew’s behavior had been getting increasingly worse. His personality had changed from a sweet, happy child to someone who was angry and depressed, who had serious suicidal and homicidal thoughts. In his room that day she found two drawings, one of him hanging from a tree, another one where he was shooting other children. I told Sherrie to bring Andrew to see me the next day. His parents drove to my clinic, which was eight hours away.
As I sat with Andrew and his parents I knew something was wrong. I had never seen him look so angry or so sad. He had no explanations for his behavior: “I am just mad all the time.” He said no one was hurting or teasing him. He had no idea why he felt the way he did. There was no family history of serious psychiatric illnesses or head injuries. And he had a wonderful family. Unlike most clinical situations, I knew this family. Andrew’s parents were loving, caring, and concerned. What was the matter?
The vast majority of my colleagues would have placed Andrew on some sort of medication and had him see a counselor for psychotherapy. Having performed more than one thousand SPECT studies by that time, I first wanted a picture of Andrew’s brain. But with the hostility from my colleagues fresh in my mind about the imaging work I asked myself again, Maybe this was really due to a family problem that I just didn’t know about. Maybe this is a psychological problem. As an aside, if you have extensive psychiatric training you can find dirt in anybody’s family. I thought, Maybe Andrew was acting out because his older brother was a “perfect” child who did well in school and was very athletic. Maybe Andrew had these thoughts and behaviors to ward off feelings of insecurity related to being the second son in a Lebanese family (I had personal knowledge of this scenario). Maybe Andrew wants to feel powerful and these behaviors are associated with issues of control. Then logic took over my brain. Nine-year-old children do not attack other children for no reason. They do not normally think about suicide or homicide. I needed to scan his brain. If it was normal then I could look further into the underlying emotional problems that might be present.
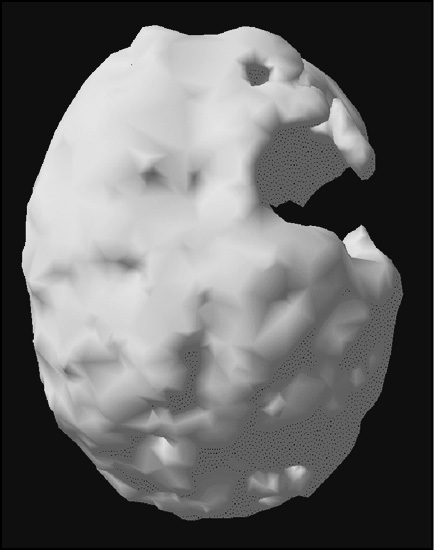
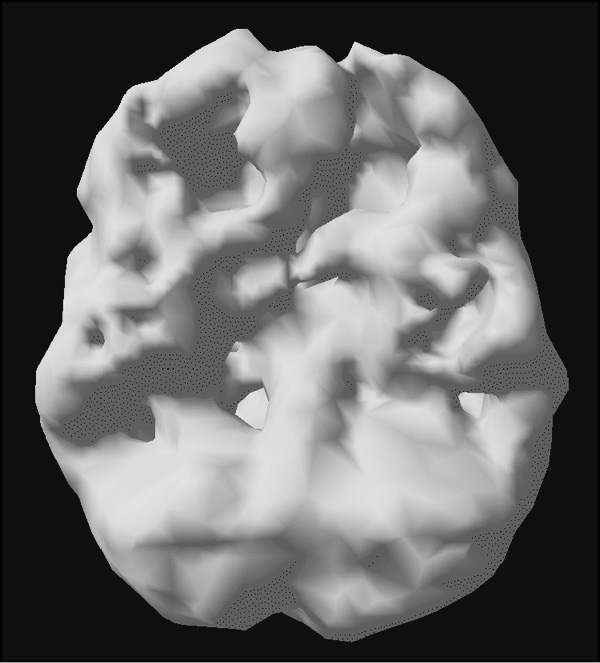
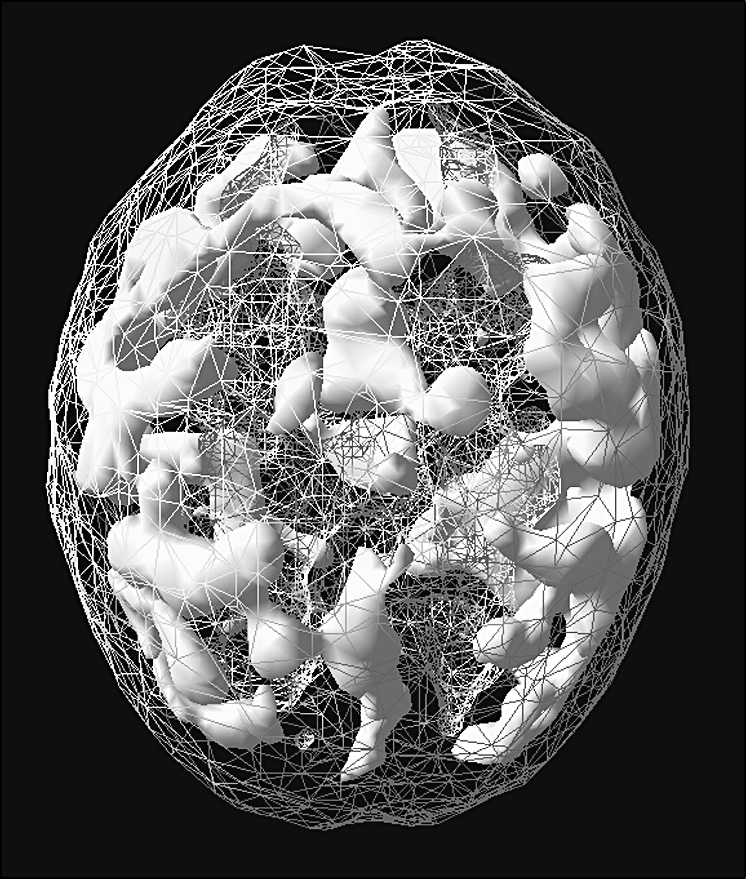
I went with Andrew to the imaging center and held Andrew’s hand during the study while he held his teddy bear. As his brain scan appeared on the computer screen I thought a mistake was done in performing the procedure. Andrew had NO left temporal lobe. Upon quick examination of the complete study, I realized the quality of the scan was fine. He was indeed missing the function of his left temporal lobe. Did he have a cyst, a tumor, a prior stroke? A part of me felt scared for him as I was looking at the monitor. Another part of me felt relieved that we had some explanation for his aggressive behavior. My research and the research of others had implicated the left temporal lobe in aggression. The next day Andrew had an MRI (an anatomical brain study) which showed a cyst (a fluid-filled sac) about the size of a golf ball occupying the space where his left temporal lobe should have been. I knew the cyst had to be removed. Getting someone to take this serious, however, proved frustrating.
That day I called Andrew’s pediatrician in Orange, California, and told him both of the clinical situation and brain findings. I told him to find the best person possible to drain the cyst and relieve the pressure on his brain. He contacted three pediatric neurologists. All of them said that Andrew’s negative behavior was probably not in any way related to the cyst in his brain and they would not recommend operating on him until he had “real symptoms.” When the pediatrician told me this information I became furious. Real symptoms!! I had a child with homicidal and suicidal thoughts who loses control over his behavior and attacks people!
I contacted a pediatric neurologist in San Francisco, who told me the same thing. I then called a friend of mine at Harvard Medical School, also a pediatric neurologist, who told me yet again the same thing. She even used the words “real symptoms.” I said to her, “Real symptoms? I have a child with homicidal and suicidal thoughts who attacks people, what do you mean by real symptoms?” “Oh, Dr. Amen,” the neurologist replied with a condescending tone, “When I say real symptoms I mean problems like seizures or speech problems.” Could the medical profession really not connect the brain to behavior? I was angry and appalled! But I wasn’t going to wait until this child killed himself or someone else.
I called the pediatric neurosurgeon, Jorge Lazareff, M.D., at UCLA and told him about Andrew. Dr. Lazareff was famous to me before he was to the world. He is the neurosurgeon who later separated the Guatemalan twins who were connected at the head. He told me that he had operated on three other children with left temporal lobe cysts who were all aggressive. He wondered if it was related. Thankfully, after evaluating Andrew he agreed to drain the cyst.
After his surgery I got two calls. The first one was from Andrew’s mother. Sherrie told me that when Andrew woke up from surgery he smiled at her. “Danny,” she said. “It was the first time he had smiled at me in a year.” The next call was from Dr. Lazareff, who said, “Oh my God, Dr. Amen, Andrew’s cyst had been so aggressive and put so much pressure on his brain that it had actually thinned the bone over his left temporal lobe. If he had been hit in the head with something like a basketball it would have killed him instantly. Or the pressure from the cyst could have likely killed him within six months.” Andrew was fortunate. He had someone who loved him paying attention to his brain when his behavior was off. He is now twenty-eight, employed, and a wonderful young man. That personal experience gave me the motivation and courage to deal with my critics and do the work I have loved for so long.
Sometimes when I lecture and tell Andrew’s story, tears still come to my eyes, even though I have told it hundreds of times. I think of all the children, teenagers, and adults who do terrible things, who we just label as bad, evil, or less than human, even though we have never looked at their brains. We just condemn them. It is so much easier to judge people if you never look at how their brains struggle.
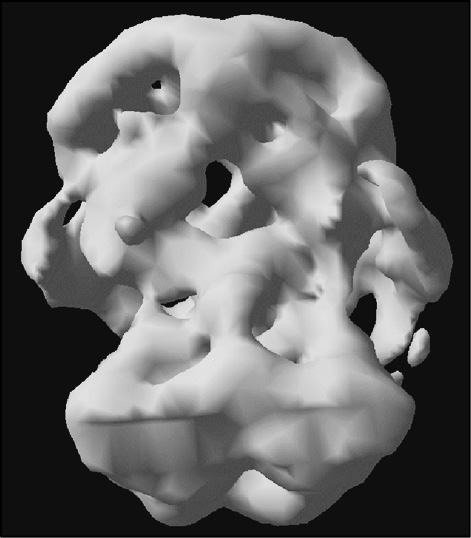
Andrew’s Missing Left Temporal Lobe (3-D Underside Surface View)
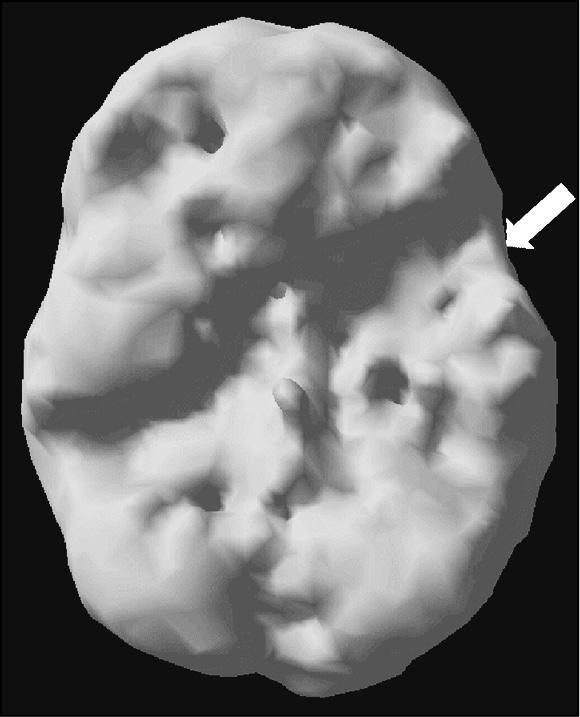
Before
After surgery
A year after his surgery, Andrew and I were in Hawaii on vacation with our families. When we were on a boat, getting ready to snorkel, Andrew looked at me and said, “Uncle Danny, why did I have the cyst and have to go through all those problems?” Feeling a bit overwhelmed, I tenderly looked at Andrew and said, “We’ll never really know why, but I think a part of the reason was for me. When I was able to help you, it gave me the courage to tell others about the importance of our brain imaging work without caring about all the people who criticized me. I have to tell everyone I know about it.” He didn’t fully understand what I was saying to him, but he accepted my response and we had a great time snorkeling.
Now, twenty-two years since I ordered my first SPECT scan there are centers across North America doing this work. The criticism from some academics remain; some people are very slow to change their ways. But we have published studies and collaborated with colleagues, including researchers at UC Irvine, UCLA, University of British Columbia, NYU, University of Pennsylvania, Thomas Jefferson, and Harvard. There is an openness of spirit that represents a major shift in thinking than even five years ago.
SPECT GUIDED BRAIN BASIC TENETS
Here are some of the guiding principles that underlie our work:
- The brain is involved in everything you do, how you think, how you feel, how you act, and how well you get along with other people.
- When your brain works right, you work right.
- When your brain doesn’t work right, it is very hard for you to be your best.
- There are many things that hurt our brains, such as injuries, drugs, excessive caffeine, smoking, infections, environmental toxins, poor nutrition, and too little or too much exercise, excessive stress, insomnia, sleep apnea, any physical illnesses, chemotherapy.
- There are things that help the brain, such as proper nutrition, exercise, stress management techniques, new learning, omega-3 fatty acids, meditation, etc.
- Psychiatric illnesses, such as ADD, anxiety, depression, and addictions are not single or simple disorders. They all have multiple types.
Lawrence Left-Sided Stroke
(3-D Underside and Left Side Surface Views)
Underside
Left side
Steven Head Trauma (3-D Top Down and Left Side Surface Views)
Top down
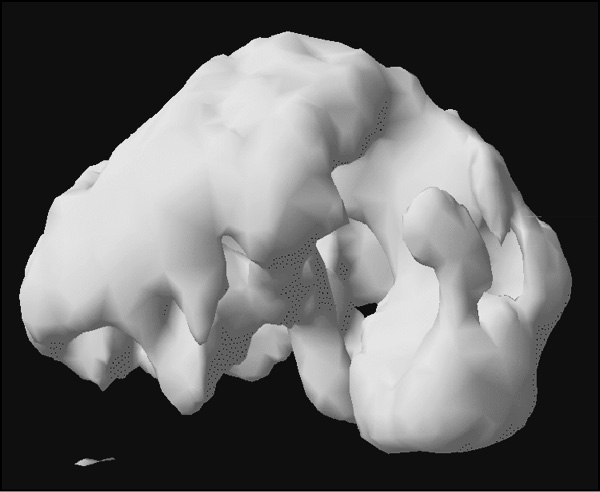
Left side
Laura Alcohol Abuse
(3-D Underside and Top Down Surface Views)
Underside
Top down
When I first started imaging I thought that different disorders, such as ADD, would have specific signature patterns, but soon found out that each particular illness, like ADD, actually had many different patterns. This made perfect clinical sense, because someone could meet all of the clinical criteria for ADD, but be made dramatically worse with the standard ADD treatment, stimulant medication. The SPECT scans helped us uncover the specific types.
Here are some examples from our collections of brain SPECT scans. In order to appreciate the functional changes in ADD brains, it’s helpful to look at more dramatic examples of brain dysfunction.
Lawrence had a stroke, and since then, his speech has been affected, he has problems with depression, and he has trouble with short-term memory.
Steven fell off a roof onto his head and fractured his skull. He was unconscious for several days. Since the accident, he has had problems with his temper, seizures, and impulse control.
Kathy has Alzheimer’s disease. Over the last few years her memory has gotten progressively worse. She gets lost easily and she says inappropriate things to her loved ones.
Laura had been abusing alcohol heavily for ten years. She now complained of memory problems and trouble learning new information.
Due to my personal situation at home, throughout the brain-imaging work I have always had a strong interest in ADD. Initially, as in Sally’s case, I thought that ADD was primarily a problem of decreased activity in the prefrontal cortex. My 1993 study showed that 65 percent of ADD patients had decreased prefrontal cortex activity with concentration, but we soon saw other patterns emerge, especially in our more complex patients. As our brain-imaging became better known, the volume and complexity of our cases increased, as did our knowledge and database of scans. We found that there were a number of different brain systems involved. Here is a brief summary of the brain-imaging findings and symptoms for the different types of ADD that I saw. I will devote a chapter to each type with several examples for each.
TYPE 1: CLASSIC ADD
SPECT findings: a generally healthy brain at rest, but during concentration there tends to be decreased blood flow in the underside of the prefrontal cortex, cerebellum, and left and right basal ganglia (structures deep within the brain that help produce the neurotransmitter dopamine). Primary symptoms: inattentive, distractible, disorganized, hyperactive, restless, and impulsive.
This is the easiest pattern to spot. Almost all of the brain-imaging studies performed outside of Amen Clinics have been done on this type of ADD. Typically, prefrontal and cerebellar deactivation can be seen on the scans. This pattern tends to be seen more frequently in boys.
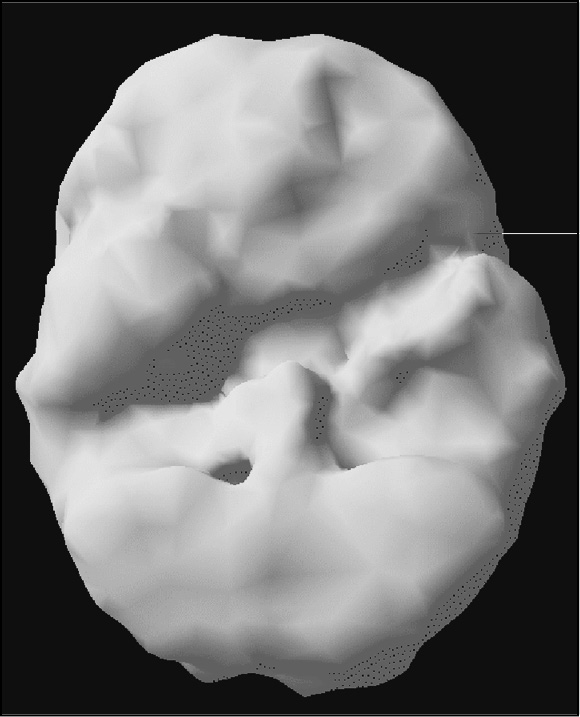
Type 1: Classic ADD (3-D Underside Surface View at Rest and with Concentration)
At rest
TYPE 2: INATTENTIVE ADD
SPECT findings: a generally healthy brain at rest, but during concentration there tends to be decreased blood flow in the underside of the prefrontal cortex, cerebellum, and basal ganglia.
Primary symptoms: inattentive, disorganization, distractible, but not hyperactive.
This pattern is common in males and females.
Type 2: Inattentive ADD (3-D Underside Surface View at Rest and with Concentration)
At rest
With concentration
TYPE 3: OVERFOCUSED ADD
SPECT findings: At rest and during concentration there is increased activity in the anterior cingulate gyrus. During concentration there is also decreased activity in the underside of the prefrontal cortex, cerebellum, and basal ganglia. Primary symptoms: inattentive, trouble shifting attention, frequently get stuck in loops of negative thoughts or behaviors, obsessive, excessive worrying, inflexible, frequent oppositional and argumentative behavior. May or may not be hyperactive. This pattern tends to be seen more commonly in children and grandchildren of alcoholics. For personal reasons, families with alcohol-abuse histories were my research interest during training. This is a pattern I discovered within my first year of doing SPECT imaging.
TYPE 4: TEMPORAL LOBE ADD
SPECT findings: At rest and during concentration there is decreased (and infrequently increased) activity in the temporal lobes. During concentration there is also decreased activity in the underside of the prefrontal cortex, cerebellum, and basal ganglia. Primary symptoms: inattentive, easily distracted, disorganized, irritable, short fuse, dark thoughts, mood instability, memory issues, and may struggle with learning disabilities. May or may not be hyperactive.
A great number of my initial cases involved temporal lobe dysfunction. Early in my imaging education, I discovered how important the temporal lobes are in psychiatric illness, mood instability, violence, and learning disabilities.
Type 4: Temporal Lobe ADD
(3-D Underside Surface Concentration View)

Underside view
TYPE 5: LIMBIC ADD
SPECT findings: At rest there is increased deep limbic activity (thalamus and hypothalamus). During concentration there remains increased deep limbic activity and now there is also decreased activity in the prefrontal cortex, cerebellum, and basal ganglia. Primary symptoms: inattentive, easily distracted, disorganized, chronic low-grade sadness or negativity, “glass half empty syndrome,” low energy, tends to be more socially isolated, and frequent feelings of hopelessness and worthlessness. May or may not be hyperactive.
Some people say that Limbic ADD is really a combination of ADD and depression. That may be so, but we see this combination very frequently in our ADD patients and it leads us to specific treatments that seem best for this type.
Type 5: Limbic ADD (3-D Underside Active Concentration View)

Underside view
TYPE 6: RING OF FIRE ADD
SPECT findings: At rest and during concentration (often worse during concentration) there is patchy increased uptake across the cerebral cortex with focal areas of increased activity, especially in the left and right parietal lobes, left and right temporal lobes, and left and right prefrontal cortex. In addition there is often increased activity in the cingulate gyrus. Primary symptoms: inattentive, easily distracted, irritable, overly sensitive, cyclic moodiness, and oppositional. May or may not be hyperactive.
Many of our younger “difficult cases” had this pattern in the brain. Initially, I thought it was related to perhaps an early bipolar pattern. While that may be true, it is more complex and it can also be related to infections, allergies, or inflammation. It is important to note here that young children naturally have very busy brains and this pattern has to be adjusted for age.
Type 6: Ring of Fire ADD (3-D Top Down Active Concentration View)
Top-down view
TYPE 7: ANXIOUS ADD
SPECT findings: At rest and during concentration there is increased activity in the basal ganglia, an area associated with anxiety. With concentration, there is decreased activity in the underside of the prefrontal cortex and cerebellum. Primary symptoms: inattentiveness, distractibility, disorganization, anxiety, tension, a tendency to predict the worst, freeze in test-taking situations, and a tendency toward social anxiety.
One of the main reasons we have been so successful in both our clinical and brain-imaging work is that they were done in a clinical setting. Being a neuroscientist who studied the brain as well as being a psychiatrist responsible for patient care put me in a unique position to understand what I was seeing in the scans of my patients. They kept me searching, asking questions, and looking for answers.
Type 7: Anxious ADD (3-D Underside Active Concentration View)

Underside view