CHAPTER 11
Type 6: Ring of Fire ADD
Ring of Fire,” what kind of name is that for an ADD type? Once you understand the underlying physiology seen on SPECT scans, the name makes perfect sense. Rather than have the typical underactive prefrontal cortex activity that is seen in Type 1 and Type 2, these patients have an overall hyperactive or disinhibited brain. There is too much brain activity across the whole cerebral cortex, especially in the cingulate gyrus, parietal lobes, temporal lobes, and prefrontal cortex. It looks like a ring of hyperactivity around the brain. At the Amen Clinic we look at the 3-D active scans in blue (average activity) and red (the most active). The ring of red on the scan of a typical Ring of Fire ADD patient reminds me of the active volcano Kilawea in Hawaii. The behavior in these patients can also be volcanic in nature. Here’s an example.
Jarred
Jarred was diagnosed with ADD at the age of eight. He was hyperactive, restless, impulsive, hyperverbal, moody, and oppositional. His parents brought him to the pediatrician on the recommendation of the teacher. In succession, he was tried on three stimulant medications (Ritalin, Dexedrine, and Cylert), but they all made him worse: he was more moody, irritable, and talkative. His parents stopped the medication and refused to bring him back for help. Every bad thing that happens to untreated ADD children happened to Jarred. He dropped out of school in ninth grade. He started using drugs and alcohol at age fourteen. His parents threw him out of the house at age sixteen because of his temper and drug use. He had trouble with the law. He often became violent when he drank alcohol, even though he said that alcohol made him feel better. From the ages of eighteen to twenty, he was arrested ten times for violent behavior, all when he was intoxicated. It wasn’t until Jarred was arrested for armed robbery that he came to my clinic.
On the night of the last crime Jarred started drinking about 10:00 P.M. He drank a fifth of peach schnapps within a half-hour followed by forty ounces of malt liquor beer the next half-hour. He then raced a friend down the freeway and crashed his car. He fled the scene on foot. A short while later he flagged down a cab driver. At exactly 12:10 A.M. he pointed a loaded gun at the cab driver’s head and demanded all his money. He got twenty-five dollars. The next morning, after sobering up, he turned himself in to the police.
His defense attorney called me to discuss the case. He wondered if the ADD diagnosis would help his defense. I said I didn’t think it would help, but wondered why, if he really had ADD, the stimulants made him worse and why he continued to drink despite all of the terrible problems it caused him. Since he seemed to only be aggressive when he drank alcohol, I decided to scan him both sober and drunk.
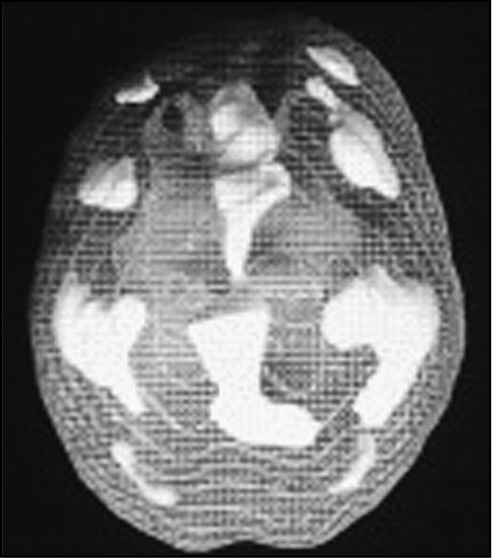
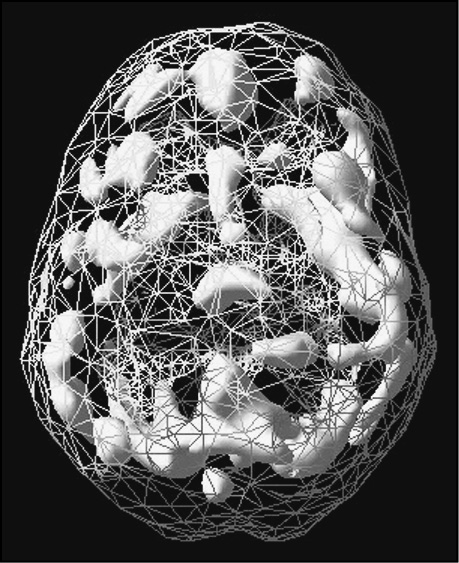
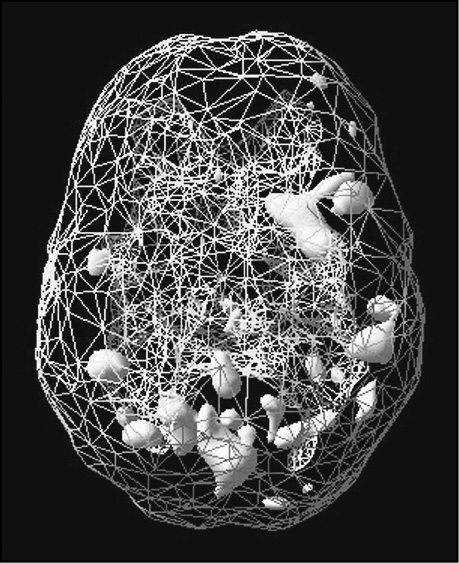
The first SPECT study was performed drug and alcohol free. The second study was performed after he consumed a fifth of peach schnapps, followed by forty ounces of malt liquor beer (the same brand he drank on the night of the crime consumed in the same time frame). The “non-alcohol” study revealed marked overactivity in the cingulate gyrus, the right and left lateral prefrontal cortices, the right and left parietal lobes, and the left and right temporal lobes (the Ring of Fire pattern). These findings are often associated with anxiety, cyclic mood tendencies, and irritability.
For the alcohol study, his blood alcohol level was 0.2g/dl(percent)—double what is legally drunk in most states. This study showed an overall dampening effect on the hyperactive areas of the brain (prefrontal, parietal, and temporal lobes), with only the cingulate gyrus showing excessive activity (although significantly less activity than on the non-alcohol study). In addition, the right and left prefrontal cortex was now significantly underactive, as were the left and right temporal lobes.
Jarred’s SPECT Series Off and On Alcohol
(Top 4 images are 3-D active views—notice the Ring of Fire is calmed by alcohol; bottom 2 images are 3-D surface views—notice alcohol crashes brain activity, especially in the prefrontal cortex and temporal lobes.
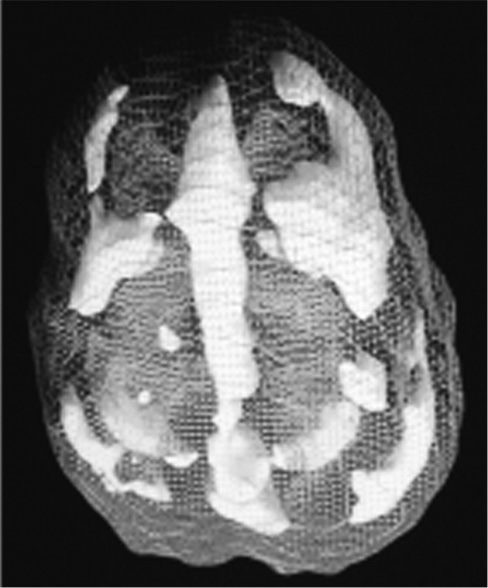
No alcohol
Top down view

Intoxicated
Top down view
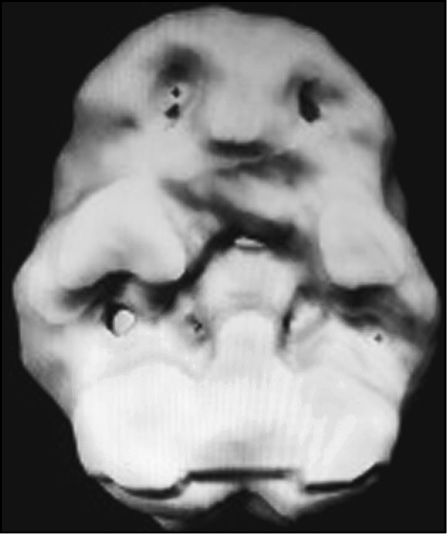
No alcohol
Undersurface view
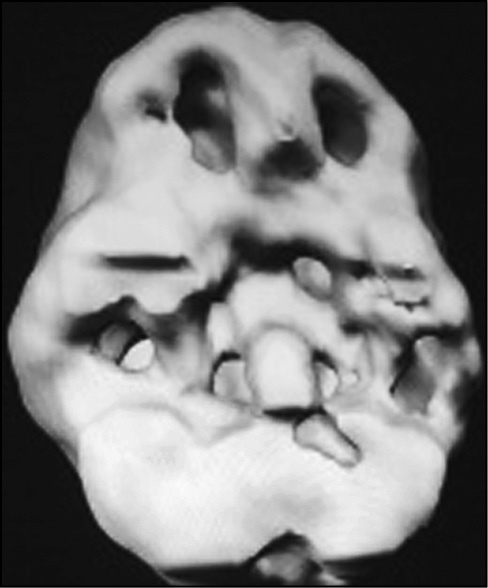
Intoxicated
Undersurface view
Given the marked hyperactivity in his brain in a sober state, along with his report that he felt more relaxed when he drank, it was not unreasonable to assume he may have been using alcohol as a way to settle down his brain and feel more comfortable (self-medication). Unfortunately, by self-medicating, he was inducing a “violent” pattern in his brain. Increased cingulate activity, abnormal left temporal lobe activity, and decreased prefrontal cortex activity is the triad of symptoms that have been found in violent patients. He drank himself into a violent state as a way to medicate underlying abnormalities in his brain.
Jarred had Ring of Fire ADD. Hallmark symptoms of this type include irritability, hyperactivity, excessive talking, overfocus issues, extreme oppositional behavior, and cyclic periods of calm behavior alternating with intense aggressive behavior. The Ring of Fire brain pattern shows excessive activity across the whole cortical surface, as opposed to Classic ADD which shows decreased activity with concentration. Ring of Fire ADD may represent a variant of bipolar disorder mixed with ADD.
Child Psychiatrist Thomas Jaeger from Creighton University in Omaha, Nebraska, has also done pioneering work with brain SPECT imaging. Early in his work he noticed that children and teenagers with bipolar disorder (a phrase for what used to be known as manic-depressive illness) had patchy increased uptake across the cortical surface of the brain. Here is an image of a bipolar patient during a manic episode. Manic episodes are characterized by a cluster of the following symptoms: inflated self-esteem, hyperactive behavior, fleeting attention span, extreme impulsivity (such as in sexual matters or spending foolishly), increased energy, decreased need for sleep, and oftentimes psychotic irrational thinking. The Ring of Fire ADD pattern is very similar to this brain pattern.
We have also seen that psychostimulant medication, such as Ritalin, frequently makes these patients worse. They become more worried, more irritable and more negative. Also, St. John’s Wort and medications which increase serotonin, by themselves, often make this type much worse. It is often helped with an elimination diet, supplements that help balance the brain, such as a combination of GABA, HTP, and L-tyrosine, and in more severe cases an anticonvulsant or atypical antipsychotic medication, such as Risperdal.
Bipolar Brain
3-D top down active view; note patchy uptake throughout the cortex
In looking at the SPECT scans for this pattern, we see a number of abnormalities that seem to explain the clinical picture. Hyperfrontality, a term for the combined findings of increased cingulate activity and increased left and right lateral prefrontal cortex activity, is associated with severe overfocused symptoms, such as worrying, obsessiveness, oppositional behavior, and cognitive inflexibility. Increased parietal lobe activity is often associated with distractibility and hypersensitivity to the environment (extreme sensitivity to sound, touch, taste, smells, and sights). The parietal lobes contain the brain’s sensory cortex, which when overactive seems to cause a person to be hypersensitive to incoming information. Increased lateral temporal lobe activity often causes problems with mood instability and irritability. This Ring of Fire pattern seems to be the most intense ADD type. It is ADD if the core ADD symptoms are present over a prolonged period of time. It is bipolar disorder if the symptoms occur only in a cyclic fashion. Frequently, we see both patterns. The ADD core symptoms are present over time, the mood problems occur in a cyclic fashion. Some doctors would argue that there are really two separate problems, both ADD and bipolar disorder. We see the Ring of Fire pattern so commonly in our ADD patients that we feel the need to classify it as a separate ADD type. Here are several Ring of Fire ADD examples.
Casey
Casey was described by his teacher as a sweet, endearing boy who tries very hard and always does his best. She also said that even though he does worry too much and gets upset if he makes a mistake, he works with enthusiasm and is a super student. But this is only when he is on his medication; without it he is a horror to be around. When he isn’t on his medication he is cruel, combative, angry, and obnoxious. At school, without his medication he often has temper outbursts and will hit other children for little reason. He also has difficulty following rules set by his teacher and will often argue with her or just refuse to obey instructions. At home, without his medication his behavior isn’t much better than at school. He is afraid of new situations and usually reacts to change by covering his ears to block out the new experience. At The Amen Clinics he couldn’t even flush the toilet because of his inability to function in new situations. He also has difficulty following instructions that his mother gives and will often reply to an order by saying things like: “I hate you,” “I wish you were dead,” or “I want to kill you.” Another common reaction to his mother’s orders would be to try to hit her.
Casey’s Concentration SPECT Study (Top Down Active View)

Before treatment was started, a SPECT scan was ordered as part of his evaluation. It showed an overactive brain with increased activity in both prefrontal cortices, both parietal lobes, and in the anterior cingulate gyrus. Given the severity of his symptoms I started Risperdal (a novel antipsychotic medication that we have found to be helpful for this pattern) and then Ritalin. Ritalin by itself had made Casey worse, but in combination with a full treatment program, the changes in his behavior have been vast. The effects of treatment were best summed up by his fourth grade teacher when she said, “This year I have only seen two incidents of misbehavior and both times were days he had missed his medication.”
Ronny
Ronny was nine years old when his mother brought him to The Amen Clinic. His mother first sensed that something was wrong when, at ten months old, he would begin screaming for no apparent reason, while he was playing alone on the floor. Throughout kindergarten he often hid in the cupboards. Even when he wasn’t in the cupboards, he usually refused to participate in class. The few times he did participate, he was a distraction. Toward the end of the year he finally stopped hiding in the cupboards, but he continued to be distracting in class. In the second grade, he and another boy met in the bathroom on several occasions and would touch each other’s genitals. Since then, he sexually experimented with several other boys and became obsessed with sex. He also became increasingly oppositional and argumentative to his parents’ requests. He would scream and throw temper tantrums nine times out of ten when he was asked to do chores around the house and he refused to sit down to do his homework. Right before his initial evaluation his behaviors became even more concerning. He threatened to kill himself when his mother tried to take a knife away from him.
Ronny’s SPECT study showed the Ring of Fire pattern, increased activity in both prefrontal cortices and parietal lobes as well as the anterior cingulate gyrus, and the underside of his prefrontal cortex was noted to be underactive. Before Ronny came to the clinic he had been on Ritalin which had made him more irritable and aggressive. Seeing his scan, the doctor in my clinic put him on Depakote (an anticonvulsant medication often helpful with the Ring of Fire pattern). After some improvement in his behavior was noticed, a second SPECT study was ordered. His second study, which was performed on Depakote, was calmer overall. His prefrontal cortex was still underactive. Adderall was then added to his regimen. It significantly helped him focus. On his current medication his mood is much better, he has a more even temper, and is less distractible. His oppositional behavior is better (not perfect, but better) and through parent training, exercise, and dietary interventions he continues to improve.
Guy
Nineteen-year-old Guy came to the clinic because he was having problems controlling his temper. He had always had a bad temper and was constantly getting into fights, but he had never tried or even gave any serious thought to hurting anyone with anything more than his fists. This all changed ten months before he first came to Amen Clinics. He got in a fight with someone in a gang. In that fight he took several blows to the head from a pair of nunchakus and went to the hospital with a concussion. While he was in the ER of the hospital he got into another fight, this time with a police officer, and was again hit in the head several times—this time with a mag flashlight. Since the incidents of that night ten months before he came to the clinic, Guy has even less control over his temper, especially around figures of authority. He had always been oppositional and had a problem with authority, but now he had no control over his temper around figures of authority. While he was discussing these changes in his temper he told his doctor, “I just don’t understand my own brain anymore.” He was also experiencing an increase in dark thoughts. Now when he is angry, instead of wanting to hurt someone with his fists, his thoughts have turned homicidal. These new thoughts and urges disturbed Guy who said, “I definitely don’t want to hurt anybody or take someone’s life, but my thoughts say something different.” In addition to his increasingly dark, violent thoughts, he also started to think about suicide. He even knew how he would do it—with a shotgun “to make sure it was over.” He said that he wouldn’t ever try to kill himself, but the thought hadn’t even crossed his mind until his head trauma ten months earlier. His relationships with the people in his life also changed. He would cut people out of his life on a whim without any sorrow or remorse. He stated that his attitude had become “my way or the highway.”
Guy has a new son, which is why he sought professional help. He wanted to have more effective and stronger relationships, he wanted to have control over his temper, he wanted to be able to stay on task, to be able to concentrate so he can keep a steady job. A SPECT study was performed as part of his evaluation. It showed increased activity in the cingulate gyrus, left and right prefrontal cortices, left and right lateral parietal lobes, and in the limbic system. There was also decreased activity in the right and left temporal lobes. His doctor put him on a combination of medication (an anticonvulsant, Neurontin, and a stimulating antidepressant, Effexor). In addition, his diet was changed, exercise was increased, and he is seen in weekly psychotherapy to help him deal with the authority issues and to be effective with his son. He has improved greatly. He is less depressed, has control over his temper, and his attention span has improved. Overall he is much happier now and his wife is expecting another child soon.
Michael
Fifteen-year-old Michael came to the clinic with symptoms of ADD, mood swings, impulsivity, and oppositional behavior. He was struggling in school and at home. He was made worse with stimulant medication and antidepressants that raise serotonin. His scan showed a Ring of Fire pattern. On a combination of GABA, 5HTP, and L-tyrosine he did much better and after three months his scan was calmer and more normal as well.
Michael Before Treatment
Michael After Treatment
PARIETAL LOBES
One brain system not discussed yet is the parietal lobes, toward the back top of the brain. Also called the sensory cortex, it is the part of the brain where touch is processed. We frequently see it overactive in ADD, especially the Ring of Fire ADD. It seems when this part of the brain is too active people become hypersensitive to their environment. They tend to see too much, feel too much, and sense too much. Distractibility is especially heightened in these patients.
DIFFERENTIATING TYPE 6 RING OF FIRE ADD FROM BIPOLAR DISORDER
Differentiating this type of ADD from bipolar disorder is generally difficult in children and easy in adults. Until recently, child psychiatrists didn’t think that children had bipolar disorder. They thought that it was a disorder of older adolescence and adulthood. New information has shown that this disorder does occur in children and that it is sometimes very hard to distinguish between it and severe ADD. Bipolar children tend to cycle in their mood and behavior problems. They have times when they are awful, irritable, and aggressive, and they have times when things are relatively normal. Ring of Fire ADD kids tend to have problems on a consistent basis. In order to be diagnosed with bipolar disorder as an adult, the person needs to have a manic episode (pressured speech, trouble sitting still, irritability, decreased need for sleep, grandiose ideas, periods of hypersexuality or hyperreligiosity, extreme impulsivity, and sometimes even psychotic experiences, such as hallucinations or delusions). People with Ring of Fire ADD do not have manic episodes. Their behavior tends to be consistent over long periods of time. People can have both Ring of Fire ADD and bipolar disorder, and some studies suggest that as many as half of the people with bipolar disorder also meet the criteria for ADD.
