CHAPTER 13
Soft Brain, Hard Skull
Head-Trauma-Induced ADD
One of the most common causes of ADD-like symptoms outside of genetics is head trauma, especially to the prefrontal cortex. Our brain-imaging work has taught us that head injuries are more important than most physicians have previously believed. SPECT is clearly able to show areas of damage that are not seen in anatomy studies like CAT scans or MRI. SPECT will show early damage, when brain tissue is struggling, while CT or MRI only show up as trouble when the brain tissue has atrophied or died.
With SPECT we can see contra-coup injuries (opposite parts of the brain damaged by the same injury) and old injuries (even damage from birth or forceps deliveries). Why are head injuries so important? Some basic brain facts are in order here.
- Your brain is involved with everything you do. How you think. How you feel. How you act. And how well you get along with other people.
- Your brain is very complex. Did you know you have one hundred billion nerve cells, or neurons? Every one of your neurons is connected to hundreds and even thousands of other neurons. You have more connections in your brain than there are stars in the universe. Your brain is more intricate, delicate, and complicated than any computer that we can imagine.
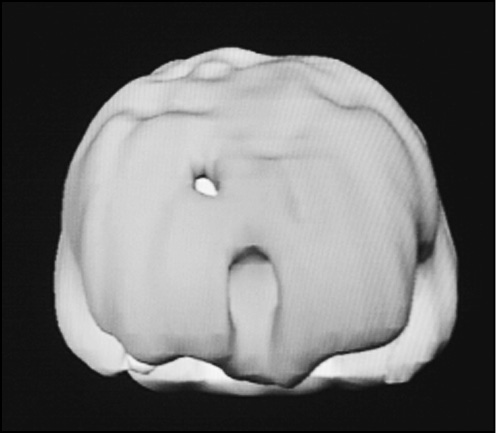
- Your brain is very soft. It is similar in consistency to soft butter. When I was a little boy working in my father’s grocery store I used to see cow brains in little white cups. The cow brains, like human brains, were so soft that they took on the shape of the cup.
- Your skull is really hard. Inside your skull there are many rough areas and sharp bony ridges.
- Your brain is in a closed space. When you experience a blow to the head, there is no place for the brain to go. It ends up slamming against the walls, ridges, and sharp bony edges in the brain, ripping small blood vessels, causing micro-hemorrhaging (bleeding), and over time small areas of scar tissue.
- Consciousness is controlled by deep structures in the brain. The deep structures in the brain may not be injured in a head trauma, but there may be a significant injury to the cortex or surface of the brain, with no loss of consciousness.
Our experience with ADD tells us that when the prefrontal cortex is injured, people have more ADD-like symptoms. The injuries could be from any cause—a damaging forceps delivery; a fall down a couple of stairs or off a bicycle; head-banging as a child; a blow during a fight, a rape, or a robbery; or a motor vehicle accident. Because of higher levels of activity and impulsivity, people with ADD have more head injuries, which may make it hard to determine the real cause of the problematic symptoms.
Frequently patients and their parents forget about head injuries, even though they may have been very significant. When patients come to our clinic, we ask them five times whether or not they have had a head injury. If a patient or his parents repeatedly says no but we see evidence of trauma on the scans, I’ll ask again. If they still say no I’ll ask, “Are you sure? Have you ever fallen out of a tree, fallen off a fence, or dove into a shallow pool?” You cannot believe the number of people who suddenly remember a significant head injury. I had one man last year who said no four times and then when questioned the fifth time remembered a time at the age of seven when he fell out of a second-story window and had been unconscious for ten minutes. I had another patient who said no five times but later said that ten years earlier (about the time her symptoms started) she was in a car accident and her head had broken the windshield. Due to its location, the prefrontal cortex and temporal lobes are especially susceptible to head injuries. Many people do not fully understand how head injuries—sometimes even “minor” ones, in which no loss of consciousness occurs—can alter a person’s character and ability to learn. We see head injuries so often on the SPECT studies we order in our ADD patients that we are tempted to add an eighth type of ADD: Head Injury ADD. Post–head injury symptoms often consist of attention problems, memory difficulties, and decreased energy and motivation. In head-injury-induced ADD, the symptoms follow a significant head injury and frequently look like one of the types of ADD. If the injury just affected the prefrontal cortex, it could look like Type 1 or Type 2. If the injury affected the prefrontal cortex and temporal lobes (common because of the location of the temporal lobes), it could look like Type 4. If the injury damaged the anterior cingulate gyrus, it could look like Type 3. The treatment depends on the clinical picture. We have seen anticonvulsants help to stabilize temporal lobe symptoms, and stimulants or stimulating supplements help prefrontal cortex symptoms.
The brain damage from a head injury has a number of causes. After a head injury, blood vessels may tear or break near the area of injury, causing bleeding, inflammation, and scarring. The blood vessel disruption decreases healthy nutritional supply to an area, and prevents the blood supply from removing the toxic chemicals released from damaged cells. In addition, rotational and shearing effects can also occur from the force of an injury. After an injury, the body’s defense system goes into action and recent studies have indicated that the immune system may release substances that are actually toxic to brain cells.
Here are several clinical examples of head-injury-induced ADD.
Brian
When Brian was seven years old he rode his bike full speed into the corner of a brick column. He was wearing a helmet, but it had cracked under the force of the injury. He was unconscious for about a half an hour. His parents did all of the right things, including taking him to the emergency room and having a CT scan done. The emergency room physician just said to watch him. No one said to watch for problems in behavior or learning. After the injury the mother noted changes, subtle at first and then more drastic. By the age of 12, Brian was moody, emotional, irritable, and struggling in school. When he finally came for evaluation at age 16, he was almost failing in school and had just started to experiment with drugs.
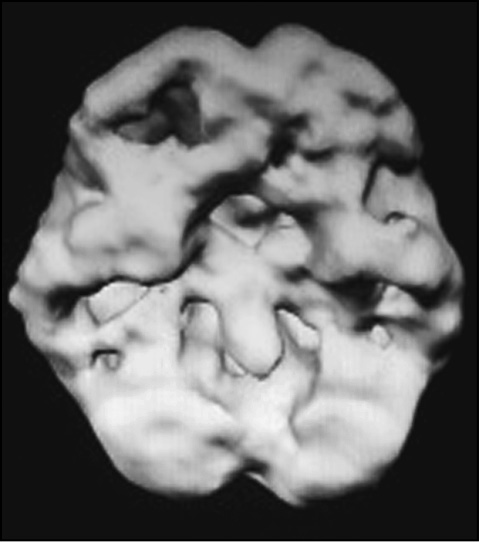
Brian’s SPECT Study Left Side Surface View
(Before and After Treatment)
Brian’s SPECT study showed clear decreased activity in the left lateral prefrontal cortex, underneath the scar from the bicycle accident. His treatment plan included a small dose of Adderall and brain wave biofeedback over his left prefrontal cortex, and natural supplements to help support brain function. Ten milligrams of Adderall enhanced activity in his prefrontal cortex, and the biofeedback was so effective that within eight months he was able to perform in school and at home at a high level without the medication.
Danielle
Danielle, age nine, was a sweet, loving child who was doing well in third grade and got along well with other children. Over Christmas break, while going with her older brother to a family party, she was in a car accident. Danielle had been using a seat belt, but nevertheless, the left side of her head slammed against the rear side window. She was only briefly unconscious. Over about eight weeks Danielle’s behavior began to change. She became negative, irritable, and oppositional. She blurted out in class and she had trouble paying attention to her work at school. Homework was hard, where before it had been very easy for her. Over the next year she lost most of her friends because she started trouble with them and often would say things that hurt their feelings.
A year after the accident, Danielle’s mother knew that there was something seriously wrong. She brought Danielle to a counselor, who thought the problem was psychological; the counselor thought that Danielle had post-traumatic stress disorder because of the accident, but the counseling didn’t help. Her pediatrician thought Danielle was just being oppositional and recommended a tough-love approach. Reluctantly the pediatrician diagnosed her with ADD and tried Ritalin, but it didn’t help very much. In fact, it only seemed to make her more moody and aggressive. By the age of fourteen, when she came to our clinic for evaluation, Danielle was failing in school and had many behavioral problems at home. I suspected that her problems were the result of physical damage to her brain from the accident, and her SPECT study bore that out. It revealed marked decreased activity in the prefrontal cortex and temporal lobes. I placed her on a small dose of Neurontin to stabilize her temporal lobes and Adderall to help her focus, along with supplements to help boost blood flow to the brain. The treatment evened out her mood and helped her focus. She was more successful in school, which helped her overall demeanor.
Wes
Wes was fifty-four years old when he sought help. He was depressed, suicidal, lethargic, and had a very short attention span. His volatile temper, a problem for his whole life, had cost him two marriages and alienated his children. Now, he had just broken up with his girlfriend of two years. In the history I discovered that he had done well in school until the eleventh grade. In between tenth and eleventh grades he was in a car accident with a teenage friend. The friend had been drinking and had lost control of the car. Wes wasn’t wearing a seat belt and his head cracked the windshield. He did not remember if he lost consciousness. Before the accident, he had been a good student with dreams of going to Stanford, but the next semester he did very poorly and gave up the idea of going to a top-rung university. He said, “I couldn’t pay attention anymore. My mind was always wandering off task.” Wes had job security because he worked in his father’s business, but he and his father fought constantly. His father wanted him to be on time and stay the whole day. Wes frequently took off and didn’t finish the tasks assigned to him.
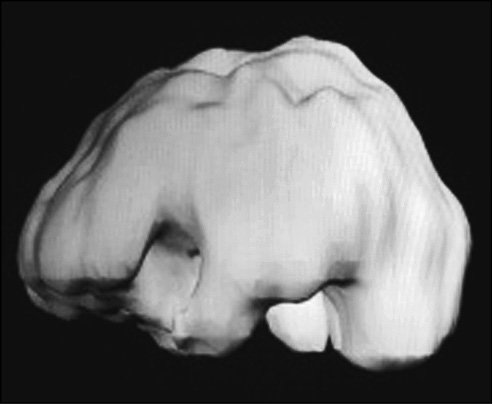
Wes’s SPECT Scan Top Down Surface Views

I ordered a SPECT series to evaluate the underlying metabolic brain issues. His SPECT series was very abnormal. He had decreased activity over the vertex (top) of the brain and decreased prefrontal cortex and temporal lobe activity, especially on the left side of the brain. With concentration, there was further overall decreased activity. Seeing the scan helped Wes understand why he had the struggles he did. On a combination of anticonvulsant and stimulant medication and biofeedback over the left prefrontal and temporal lobe regions, his mood, temper, and attention span stabilized. His girlfriend came back to him when she realized he was dealing with a medical problem, as opposed to just being a difficult person.
Alecia
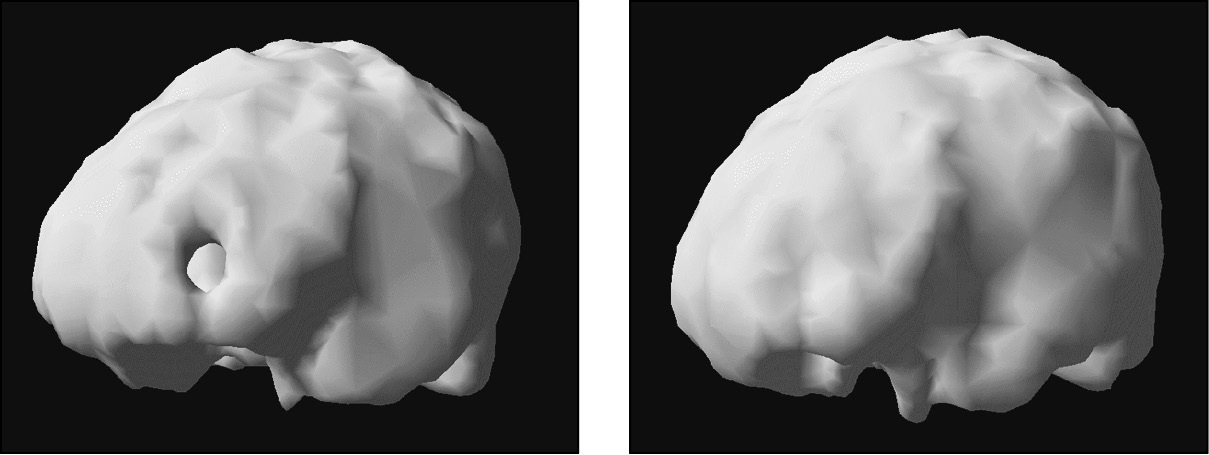
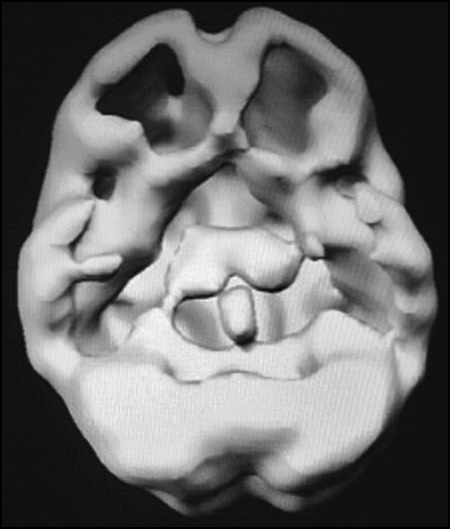
At the age of twenty-two, Alecia tripped and fell facedown on a slick, rain-soaked ramp at college. She slid fifteen feet before her head struck a concrete wall. She was dazed for most of the day, nauseated for a week, and had a headache for a month. A year later she was referred to me by a therapist who had been seeing her for temper problems. She also had trouble thinking clearly and had to drop out of school. She had energy problems, problems with goal setting, trouble organizing herself, and she spent money foolishly. Her parents were very distressed with the change in Alecia. On SPECT there was marked decreased activity in her prefrontal cortex (especially in the prefrontal pole) and temporal lobes. With Alecia we used a combination of hyperbaric oxygen therapy (HBOT) and natural supplements to help support her recovery.
Alecia’s SPECT Study (Concentration, Top Down, Front On, and Underside Surface Views)

Top down
Front
HYPERBARIC OXYGEN THERAPY (HBOT)
I became interested in Hyperbaric Oxygen Therapy (HBOT) after colleagues who were using it with their patients showed me the before and after SPECT studies. They told me HBOT often helped to boost blood flow to the brain thus speeding up recovery in traumatic brain injuries. HBOT works, as its name implies, by increasing oxygen under pressure. The increased pressure of oxygen signals the DNA in our cells to perform healing tasks that the body normally can’t do. Ground zero for this healing activity is the mitochondria, which are the little organelles inside of our cells that convert oxygen and sugar into the gasoline the cells run on (ATP). It doesn’t take much to knock mitochondria off-line, and then that cell can’t perform the job it was assigned. The mitochondria can be damaged by oxygen deprivation, external toxic exposure, an infection, or trauma. HBOT works by reviving the little mitochondria.
In 2011, my colleague Paul Harch, I, and others published a study in the Journal of Neurotrauma on the use of HBOT in sixteen soldiers who had experienced head injuries in Iraq or Afghanistan. Each soldier was thoroughly tested, including having a SPECT study and then given forty sessions of HBOT. After HBOT, the soldiers demonstrated significant improvement in: symptoms, neurological exams, many measures of cognitive and emotional functioning, and even a fifteen-point rise in their IQ. Specifically, we saw improvements in memory, impulse control, mood, anxiety, and quality of life. The SPECT scans also showed improvement in blood flow across many areas of the brain.
Sal
Sal was referred to my clinic by his marital therapist. Sal and his wife had a relationship filled with conflict, tension, and turmoil. Sal’s wife complained that he was inattentive, selfish, and incapable of expressing feelings. Sal was a marginally successful attorney who had trouble keeping clients. Like his wife, they found him aloof and seemingly uninterested.
Sal’s problems began in high school. He played wide receiver on the varsity football team and his senior year he was being scouted by large universities. That year, he suffered four concussions during games—two on the same night! Sal went to college, but only played football for a year. He found that he had to spend inordinate amounts of time studying just to keep up; he had no time for football. After college, it took him three years to get into law school. He was persistent, but academically did not feel as sharp as he had in the early years of high school.
I suspected that the football head injuries were important in explaining his current symptoms. His SPECT study showed very specific damage to his left prefrontal cortex and left temporal lobe in a pattern consistent with head injury. The outside of the left prefrontal cortex (called the dorsal lateral prefrontal cortex) is the expressive language area of the brain. In Sal’s case it had suffered damage and taken with it his ability for empathy and expressive language. I diagnosed him with Alexythymia (a disorder where people do not have access to their own feelings). He cared about his wife, but no amount of therapy helped him to express his feelings. He didn’t understand feelings and said that when people talked about feelings it was like a foreign language to him.
I put him on a combination of an anticonvulsant medication, a group of brain enhancement supplements, and we did biofeedback over his left prefrontal cortex. Over several months his wife noticed that he became more expressive and more empathic.
Head injuries, depending on the areas affected, can present as different ADD types. ADD symptoms subsequent to head injuries often respond to the same treatments as do the specific ADD types. My SPECT work has taught me how devastating head injuries can be and how important it is to protect your head and the heads of children. After seeing these scans, I would not let my children or grandchildren hit soccer balls with their heads, play tackle football, or snowboard without a helmet. I encourage them to play tennis, golf, Ping-Pong, and track.
AMEN CLINICS STUDY ON ACTIVE AND RETIRED NFL PLAYERS
From 2009 to 2012, Amen Clinics performed the world’s largest brain imaging and rehabilitation study on active and retired professional football players. Because of our work with SPECT we had a high suspicion that many players suffered with the effects of chronic traumatic brain injury, and it seemed at the time that the NFL was dragging its feet on understanding and getting the players help.
The results of our study were very clear: A very high percentage of our 135 players had evidence of traumatic brain injury patterns on their scans and they showed the evidence of it in their lives with a high incidence of depression, dementia, obesity, and ADD-like symptoms. In fact, 81 percent of our players complained of attention problems and showed concentration problems on the psychological testing we performed.
The good news came from the second part of the study: After we saw the high level of damage in players, we wondered if their brains could be rehabilitated. I have already shared with you many stories where that, in fact, had occurred. We were hopeful and decided to use lifestyle interventions and sophisticated supplements as our treatments of choice. We taught players how to care for their brains: avoid anything that hurt it and engage in regular brain-healthy habits. In addition, we put them all on NeuroVite +, our high-quality multiple vitamin, high-dose fish oil (5.6 grams of Omega 3 Power), and a brain boosting supplement I designed called Brain and Memory Power Boost that contains seven nutrients to support brain function: gingko and vinpocetine for blood flow; Huperzine A and acetyl-L-carnitine to enhance the neurotransmitter acetylcholine; N-acetylcysteine and alpha lipoic acid, potent antioxidants; and phosphatidylserine to help nerve cell membranes and lower stress hormones. This combination was of significant benefit to 80 percent of our players, including improvements in memory, mood, attention, motivation, and sleep. In addition, we saw that the lifestyle changes and these supplements improved blood flow to their brains.
We were so encouraged by the results that we tested this combination of supplements on two separate groups of reasonably healthy people in double-blind placebo controlled studies (the highest level of scientific evidence) and saw even greater benefits in mood, executive function, memory, reasoning, information processing speed and accuracy. We even saw reduced hostility.
If you have been bad to your brain, have hope. There is high potential for recovery on a brain-smart program.