4.1 Disease and Disorder, Illness and Issue
- (a)
Present the core concept in this context, as it is fundamental to keep in mind the theoretical background to the scientific method used in medicine, as well as the parameters used to define terms such as disease and disorder, illness and issue.
- (b)
Understand how such contributions from medical philosophy apply to the mind–body problem, especially in regard to neuroscience.
The existential component of the appreciation of psychiatric disorders and manifestations of the psyche in general are also representatives of the “integrated and fragmented nature of consciousness” (Tononi 2015) as analyzed by Giulio Tononi and Gerald Edelman, but also (via a multifaceted analysis which covers areas far beyond psychiatry and neuroscience) Ervin Laszlo, Aurelio Peccei, Rick Strassman and Harald Walach. In this regard, philosophy helps us better frame what benefits, in terms of diagnostic classification and targeted clinical interventions, can originate from an accurate analysis of the combinations ‘Disease and Disorder, Illness and Issue’. To provide a specific example in this context, we can think of a very complex diagnosis with uncertain etiology such as panalgesia, more commonly known outside of Europe as fibromyalgia, first isolated-classified by the Italian physician Federigo Sicuteri. This condition is characterized by an increase in muscular tension and generalized chronic pain caused by what has been identified as a multifactorial rheumatic idiopathic syndrome often associated with multiple symptomatologies involving disturbances of sensitivity, mood, sleeping pattern, anxiety and depression (Stahl 2008). We will further discuss the definition of fibromyalgia, and we would like to begin with a historical reference. Florence Nightingale is widely known as the founding mother of modern nursing. She was also a researcher, a statistician, and advocate for human rights and a social reformer. Although it is still very difficult to assess the extent of her role as well as her clinical and social achievements in the Crimean war, many historical accounts depicts a clear picture of her progressively complicated health condition (Young 1995). In particular, many have argued that her increasing depressive state might be linkable to conditions such as brucellosis and spondylitis (Bostridge 2008). In the context of the relation between neuroscientific perspectives and medicine, we will focus on the most complicated condition—in the sense of etiology and pathophysiology, as well as in diagnosis and prognosis—of fibromyalgia as potential underlying medical condition Florence Nightingale might have been suffering from (Keddy 2008; Fowler 2013). According to McCance and Huether (2014, p. 1579), fibromyalgia is a “chronic musculoskeletal syndrome characterized by widespread joint and muscle pain, fatigue, and tender points” with a wide symptomatology in multiple body systems, which includes muscle and joint stiffness and “generalized, localized or diffuse pain, tingling and numbness” (Simms and Goldenberg 1988), sleeping pattern disturbances linked to compromised circadian activity in the endocrine system, as well as disturbances in cognition, memory and mood, affecting depression (between 25% and 60% in patient affected by FM), anxiety, and posttraumatic stress disorder (PTSD), which are also discussed as possible precondition or causal effectors for fibromyalgia itself (Schweinhardt et al. 2008). Florence Nightingale was 34 years old when she was deployed to Scutari during the Crimean war and spent over 6 months taking care of the sick and wounded in horrible hygienic conditions, with lack of ventilation and defective sewers, before the British Government sent out the Sanitary Commission to help her. Although Nightingale was able to visibly improve the situation and reduce the death rate of soldiers by 2%, dealing with overcrowding, constant stressors, fatigue and other medical conditions appeared to take a toll on her psychological well-being and immune system (Small 1998). She spent 21 months taking care of approximately 18,000 patients, providing direct clinical care and constantly reassessing, readjusting and improving the quality of care by changing bandages (previously simple rags clotted with blood), food intake, medical supplies and other clinical tools, as well as bathing the wounded, changing linens and helping the wounded with physiotherapeutic strategies (Huntley et al. 2014). Her work as a nurse and as a manager was very intense, psychologically and emotionally, as well as physically. Based on many accounts, including her own writings (McDonald et al. 2015), we can argue that Florence Nightingale might have been developing a history of medical traits very similar to the symptomatology often found in fibromyalgia, more specifically sharp pain in the neck area, shoulders, lower back and hips, with possible myofascial pain syndrome, or MPS. Nightingale also reported vision problems, which became dramatically challenging 30 years after her experience in Crimea, although the early onset was reported during the war, according to the accounts (Genschorek 1990). These issues were followed by a rapid memory loss in 1896 and multiple physical problems, leading her to spend most of her time bedridden (Genschorek 1990). These aspects, together with the more physical symptoms of generalized pain are especially important in our analysis of Nightingale’s medical conditions during her work in the Crimean war, as a “history of widespread pain lasting more than three months affecting all four quadrants of the body” is a major criteria, together with “generalized pain and 18 designated possible tender points,” for the diagnosis of fibromyalgia, according to the American College of Rheumatology (AMR 2015).
The case of Florence Nightingale serves as a perfect scenario, although technically not a true clinical case given its history and the lack of specific diagnostic documents, for a thorough investigation of the connections between pain perception, mental states and physical well-being. In the context of a critical investigation of psychophysical components of health, we could imagine a possible treatment plan for the condition, by focusing for instance on immediate pain reduction and general relaxation, both presenting strong effectors in terms of neurological underpinnings. As pain reduction and relaxation are directly linked to the patient’s perception of pain, self-assessment and pain threshold, these two therapeutic goals are deeply intertwined with the ‘bigger picture’ of more advanced, future planning, thus including (a) a general psychological assessment focus on improving psychoneuroimmunology and (b) lifestyle changes and coping skills, physical exercise in particular. As expected, in order to address general relaxation, deep breathing, meditation and mindfulness exercises are recommended. For pain reduction, the physician might recommend supplements, pain relievers and anti-seizure drugs. In these categories we could certainly list vitamin D, CNS-active medications and opioids, as well as anti-inflammatories (Müller et al. 2007). Medication prescription will follow an appropriate clinical evaluation by a specialized physician or rheumatologist. In order to better plan a specialized doctor’s appointment, it is important that the patient has educated himself–herself on his/her medical history and symptomatology, as well as family medical history. Furthermore, a detailed list of all the medication currently prescribed or taken in the past—including herbal and/or dietary supplements—will give a better clinical picture, especially because of their direct effects on neurobiological areas as well as due to possible placebo effects. To work on long-term goals it is also important that the patient thinks about potential questions for the physician, in order to gain knowledge and be proactive in the development of effective strategies and a positive attitude toward the healing process. Although the International Classification of Diseases (ICD-10) lists fibromyalgia as a “Disease of the musculoskeletal system and connective tissue” and a “functional somatic syndrome” (Häuser et al. 2009), the multilayered etiology of fibromyalgia is fertile ground for a more omnicomprehensive and balanced approach which includes a psychoneuroimmunological evaluation to support the patient physically, as well as psychologically/emotionally (Mujkanović 2016). As fibromyalgia is observed to reduce pain threshold and tolerance for extended exercise and physical activity, a well-balanced daily schedule will need to be assessed to provide enough stability, routine and motivation to the patient, thereby helping the physician monitor the improvement or difficulties encountered by the patient in his/her recovery, or at least management of the disorder. To plan a long-term treatment, we need to rely on the statistical data found on widespread muscle tension and pain, headaches and migraines, which is present in 50% of cases affected by fibromyalgia; chronic fatigue syndrome, with 70% of the cases; widespread muscle tension and pain, headaches and migraines (50%); irritable bowel syndrome and temporomandibular joint disorder (between 50% and 80%). Finally, to address our specific case (Florence Nightingale) we need to keep in mind that polymorphism and other possible genetic factors and internal/external clinical environmental factors such as viral illnesses, HIV and other infections, Lyme and rheumatic diseases, as well as medications’ side-effects might be connected to fibromyalgia, and that a misdiagnosis of the disorder might occur in 75% of the cases (Clauw et al. 2011).
To assess fibromyalgia, comprehensive clinical and diagnostic tools should include a complete blood test with complete blood count and erythrocyte sedimentation rate (Mujkanović 2016). Recommended are also thyroid function tests. In any case, given the complexity of the disorder, it is important to evaluate the specific scenario of each individual patient. In this regard, Müller et al. (2007) identify four typologies of fibromyalgia, with related best clinical strategies for management and treatment:
- 1.
Extreme sensitivity to pain but without associated psychiatric conditions (5-HT3 receptor blockers)
- 2.
Fibromyalgia and comorbid, pain-related depression (antidepressants)
- 3.
Depression with concomitant fibromyalgia syndrome (antidepressants)
- 4.
Fibromyalgia due to somatization (psychotherapy)

The amygdalae, as primary area of emotional, mnemonic and decision-making processing in the limbic system
Among the major weaknesses and problems that this systematic review revealed (as with many other systematic reviews in general), we can identify issues with length and/or time frame in which the single or multiple study has been conducted, as well as the relatively low total number of subjects examined. Certainly, as our analysis covers multiple disciplines we cannot infer that the same patterns can and should be recognized as valid across the studies examined. However, with a fair degree of accuracy we can point out to major positive trends in terms of respectable sources and publishers using sound scientific method involving both qualitative and quantitative research, and a strong indication suggesting the empirical validity of mind–body therapeutic modalities. More specifically, in this regard we briefly examined single studies, meta-reviews and databases published in the New England Journal of Medicine, CINAHL, EMBASE, MEDLINE, AMED, HealthSTAR, PsychINFO, PapersFirst, ProceedingsFirst and the Cochrane Central Registry of Controlled Trials. Our analysis clearly suggests that the state of science in regard to the management of fibromyalgia is indicative of higher clinical success in integrative therapies focusing on mind–body connection and psychophysiological stimulus-response mechanisms, in particular meditation and mindfulness-based techniques, massage therapy, gentle movement and T’ai Chi Chuan, relaxation and breathing exercises, guided imagery and hypnosis. The clinical data presented within the quantitative research studies examined indicated low cortisol production, improved and more balanced heart rate, appropriate oxygenation levels (Busse et al. 2013), and general positive response on a neurological level, especially in the areas of procedural processes in the prefrontal cortex and the responses in the parietal lobe (Bernardy et al. 2011). In the qualitative research studies, the responses given via direct questionnaires to the subject were also indicative on a general increase in psychophysiological well-being, albeit partially justified—which doesn’t undermine the validity of the examination—by a more appropriate and functional self-perception, in terms of pain management. This is a core concept in the management of fibromyalgia, as the subjects affected by this very complex disorder tend to have a very low threshold for pain in general, in combination with a high tolerance for generalized pain. Examining the effects of natural methods on the promotion and maintenance of health and well-being in our patients is a fundamental responsibility for the practicing medical professional. Healthcare providers often find themselves dealing with a vast array of problems spanning from purely physical issues, to psychological, social and spiritual components. The relation between history, theory, practice and research in medicine and neuroscience from the perspective of integrative approaches can be an important channel for improved therapeutic modalities and the general amelioration of our clinical interactions with our patients. The data collected clearly indicate that a multidisciplinary approach, combining traditional and western medicine with integrative modalities is beneficial in the treatment of the main symptoms of fibromyalgia, as well as in the management of the pain associated with this disorder. More specifically, those practices which focused on the intersection and interaction of mind–body therapy, such as meditation and mindfulness-based techniques, massage therapy, gentle movement and T’ai Chi Chuan, relaxation and breathing exercises, guided imagery and hypnosis have provided the best therapeutic strategy. Furthermore, the results of this meta-analysis provide strong evidence for possible changes in patient care and research. In particular, relational-focused guidelines to ameliorate the general pain management and improve patient-provider relationship have been at the center of funding opportunities promoted by the US National Institute of Health and the National Center for Complementary and Integrative Health. From the clinical perspective, direct care will benefit from new ways to measure patient-reported outcomes, such as pain, fatigue, physical functioning, emotional distress and social role participation as well as their vital role in the maintenance of appropriate interactions to determine physiological differences and similarities from the perspective of generalized chronic pain. Given the aforementioned result data, we recommend more evidence-based, possibly double-blind studies with an extensive cohort/case-control group. In this regard, a very good resource is the meta-analysis and multiple study examinations presented in the National Center for Complementary and Integrative Health at the US National Institutes of Health (NIH). Furthermore, given the very nature of both the symptomatologies (especially due to the connection between mental health and psychosomatic manifestations) and treatment modalities hereby discussed, we would like to stress another fundamental aspect of ‘Medicine on, of and off the Brain’. A parallel we would like to draw in this context is between the concept of (a) mental disorder and (a) sin. Alvin Plantinga (2015, p. 50) pointed out in numerous occasions that, following the Christian perspective, especially the ‘A/C model’ there might be multiple levels of interpretations of a disorder, far beyond the biological, developmental, behavioral, social or environmental areas usually covered by the Multiaxial Assessment used in psychiatry, according to the DSM model. Plantinga mentions the possibility that original sin (in the orthodox conception of the term) might be responsible for a deficit which we would call affective disorder, not cognitive disorder, due to the damage operated on the Sensus Divinitatis. This concept brings us to Isaac Newton and his definition of time and space as sensorium Dei, as an integral part of the philosophical basis to the scientific debate on time during the Industrial Revolution, and defined eternally and immutably, always the same and the same-to-itself, in its own image. This has a much deeper and more practical applicability in iatrological terms, as it clearly represents a theoretical understanding of the course of a disease. To be more specific, as Newton defined the true motion of a body to be its motion through absolute space, time and space are not true, genuine substances. Therefore, time is completely distinct from the world-space, and it passes uniformly regardless of the succession of (historical) events in the world (Rynasiewicz 2012), giving a different interpretation to the hereby presented notion of an absolute space and absolute time. These ‘absolute concepts of absolute’ are deeply connected to subjective worldviews. When working with complex—general medical and psychiatric—symptomatologies, professionals need to understand the patient’s values, and relate them to the patient’s current presentation and diagnosis, especially in relation to philosophical concepts such as the preservation of the self (Bunge 2013). Patient’s privacy, confidentiality, autonomy, beneficence and nonmaleficence need to be analyzed under the lenses of principlism and universalism, in relation to the wide range of ethical framework such as Kantian and deontological ethics all the way to virtue ethics, care ethics, bioethics and casuistry (McGonigle and Mastrian 2015). These aspects have a practical and immediate application in the patient-provider interaction. In their care, providers need to discuss with the patient the procedures or practices which will be used to minimize their susceptibility to undue influences and unnecessary risk (physical, psychological, etc.). Moreover, healthcare team members need to monitor the specificity of each patient to account for Inclusion/Exclusion Criteria of care (thus incorporating medical, psychological, and pharmacological interventions), also from the perspective of healthcare coverage: eligibility and ineligibility criteria should be specific and analyzed with reference to the Centers for Medicare and Medicaid Services (CMS), the Internal Review Boards (IRBs) and the broader US healthcare delivery system, in particular the Department of Health and Human Services (DHHS). In order to guarantee the best possible care, each of these interventions involves a constant monitoring of patient condition/presentation with reference to the patient medical history (with further consideration especially under the lens of the Diagnostic and Statistical Manual, as in the case of the Multiaxial Diagnostic Impression in Psychiatry). Thus, medical professionals need to be able to access patient information and share such data with other clinicians within the treatment team and also be able to understand and maintain confidentiality measures according to the Health Insurance Portability and Accountability Act (HIPAA) standards. Medical professionals need to be able to discuss risks and benefits of care with the patient and illustrate the possible alternatives in terms of therapeutic intervention or non-intervention. This includes physical, psychological, social, legal or other risks. Moreover, nurses in particular are responsible for sharing with the patient the planned procedures—previously discussed with the treatment team—for protecting against or minimizing potential risks and assess their likely effectiveness, as well as the probability that given risks may occur, including their severity and potential reversibility. In addition, routine procedures such as additional diagnostic/follow-up tests should be identified. Finally the clinical decisions from physician to other team members in terms of therapeutic intervention versus non-intervention should also be part of the conversation, as the full disclosure of such important pieces of information should be shared by all the members of the treatment team for that particular patient, and include the patient in every decision-making aspect. Certainly, the biggest challenge is delivering enough information to enable the patient to understand the choice, given the specific presentation (in diagnostic terms) of the subject (especially when dealing with mental health disorders) and making sure that the best treatment option is given the appropriate clinical emphasis. In this sense, medical professionals need to understand that “HIPAA seeks to balance protecting the privacy of patients’ health information and assuring that this information is available to those who need it to provide health care, payment for care, and for other important purposes” (Mujkanović 2016).
- (a)
Help their patient understand the specific aspects of the care they receive, including risks and benefits, typology (and/or dosage and administration) of treatment, therapy, medication, visits, diagnostic tests and laboratory results.
- (b)
Guide the patients in their personal efforts to obtain more information about their condition, symptomatology and related treatment from the perspective of the information they can find on the world wide web. They can play an important role in presenting and comparing different websites and other internet resources based on quality, credibility and hierarchy of evidence.
- (c)
Understand the patient’s perspective, both from the medical as well as from the personal perspective, by learning how to accurately, precisely and appropriately interpret the patient’s clinical-therapeutic preferences. Integrating classes and continuing education opportunities and certifications in Narrative Medicine could in this sense increase the therapeutic effectiveness of the provider.
A similar analysis can be applied to telemedicine. To be sure, this technology only works if the human (and humane) presence in the direct delivery of care is present. In other words, the clinician is first and foremost responsible for the appropriate and effective application of such system to the benefit of the patient and of the broader communication with the healthcare team. As an integral part of this team, nurses have added abilities to help the system by focusing on the specific clinical aspects of care—including, but not limited to treatment plan, monitoring and evaluating medical outcomes, assessing possible and present risks, and evaluating clinical workflow—as well as the broader range of safety and security perspectives, such as sharing and delivery mechanisms, signatures and encryption informatics, and biometrics (Mathews and McCormick 2007). Moreover, there are several aspects of telemedicine which improve the general delivery of care to the patient: Telehomecare helps monitor and deliver clinical care, by reaching patients in their homes; telemedicine fosters clinical collaboration and professional autonomy within shared responsibility; teletrauma can reach patient even in the most distant and rural areas, thereby bridging the gap in geographic and possibly ethnocultural disparities; e-intensive care units further promote the remote monitoring of critical ill patients’ care; telemental health combines the above-listed aspects to improve clinical care in specific vulnerable populations in vulnerable areas such as the aforementioned rural areas, as well as other areas in which access to healthcare might be difficult (war zones, prisons, etc.). Telemental health has been particularly developed in the healthcare system of the US state of Vermont, where a shared effort between the governmental institutions, the University of Vermont and the local hospitals have provided new and innovative developments to support and improve the care to mental health patients throughout the state (Rabinowitz 2015). Given all these premises, we could get the impression that telemedicine in its various and diverse subdefinitions and applications can be a definitive positive shift in the system, directly benefiting the patient. However, in our judgment we might actually be misled by the system itself. If Telemedicine is expected to improve healthcare outcomes, reduce health and geocultural disparities within the population and/or minorities, improve and help develop data infrastructure, collection, quality assessment and delivery, as well as balance patients’ interests in protection of their privacy, health, and safety (Mathews and McCormick 2007), we would expect a lesser benefit in the absence of Telemedicine. More in detail, there is a disconnect in causal terms between the demands of healthcare and the needs of both business-oriented technological developments and insurance policies. For instance, we can address the supposed increase in cost due to the providers’ accountability demanded by patients (often, quite unfortunately—and only in the United States—referred to as ‘consumers’ or ‘clients’) or due to medication-related policies. A much easier path rather than an expected increase in cost due to the very development of computer-based technology (at the core of modern telemedicine) is universal, free healthcare. The very claim that increasing healthcare costs result in a decrease in an uninsured population is both a logical fallacy and an oxymoron, in that there won’t be any need for private insurances if everything would be covered by the state/country (National Audit Office, London 2003). Aside from the vast literature on these aspects, the strong evidence-based proof is given by the way other countries, especially Europe (some argue with a possible exception of Germany and the United Kingdom), successfully keep healthcare costs down, while at the same time provide the same level (most often a higher level) of both direct clinical care, research and education (World Health Organization, The world health report 2010). In this sense, even the need of standardization of healthcare informatics, technologies and programs/systems, albeit very positive in terms of allowing broader access, could be utilized by the same capitalist-oriented policy making strategies in order to foster profit, not necessarily to serve the patient or the provider (unless by ‘provider’ we include certain pharmacological or medical corporations).
Furthermore, many aspects related to the possible negative effects of social media on our healthcare system in terms of patient’s safety should also be analyzed under this socio-economical perspective. By no means should we change our policies to move the focus away from the patients—in this sense, patient’s safety and privacy should be always protected. However, there are at least two examples of areas of patient safety in which changes to the system itself could be beneficial. To be sure, due to the very complexity of Healthcare Informatics, the more we strive for accessibility of data and safeguarding the privacy of such data, the more we will find ourselves struggling to balance these two opposites, trying to come up with more and more technological devices to prevent the possible theft of such data. Telemental health is, for instance, a great tool to provide clinical help and support to patient. It is of no use when we are still struggling with social stigma toward definitions-diagnosis of a specific mental health disorder. In other words, instead of spending yet even more time, resources and funds to keep potential theft of private data in relation to these aspects, we should make sure that society understands (and clinicians can be instrumental in this sense) what it means, for instance, to be suffering from depression. Our point of view is that we should not overemphasize the importance that ‘nobody will find out about that person’s depression’, because (in our example) depression itself won’t be something to be ashamed of. In this sense, a much bigger shift in paradigm and culture than a technological development is needed. A second example could be the theft of person/identity-sensitive data such as social security number (Forsyth 2011). Once more, in countries where a Universal and free healthcare system provides services to everybody, regardless of gender, religion, color, socioeconomic status (even citizenship) and so on, the very social security number is shared—since everybody gets the same services, it is simply pointless to steal it.
Increased and improved user-centered design in healthcare (from both the perspective of the patient as well as the provider)
Addressing workplace safety
Anticipating unexpected outcomes
Avoiding reliance on provider’s memory
Improving access to healthcare
Directly involving patients in the care provided and administered to them, thereby contributing to future amelioration of clinical framework
Risks from individuals and collective actors, including stealing data from digital storage areas
Risks from corporations, including shared profiles and systems of data collection and analysis
Possible risks from the government. Regarding the latter, the author points out to the breach in confidentiality, privacy and safety within email exchanges in public universities. These aspects have a direct link to the security policies in University Hospitals, and healthcare facilities in general, as the sharing technologies allowing direct access to Electronic Medical Records could potentially cause harm to patients.
4.2 To Treat, to Heal, to Cure
4.2.1 Clinical and Medical Neuroscience
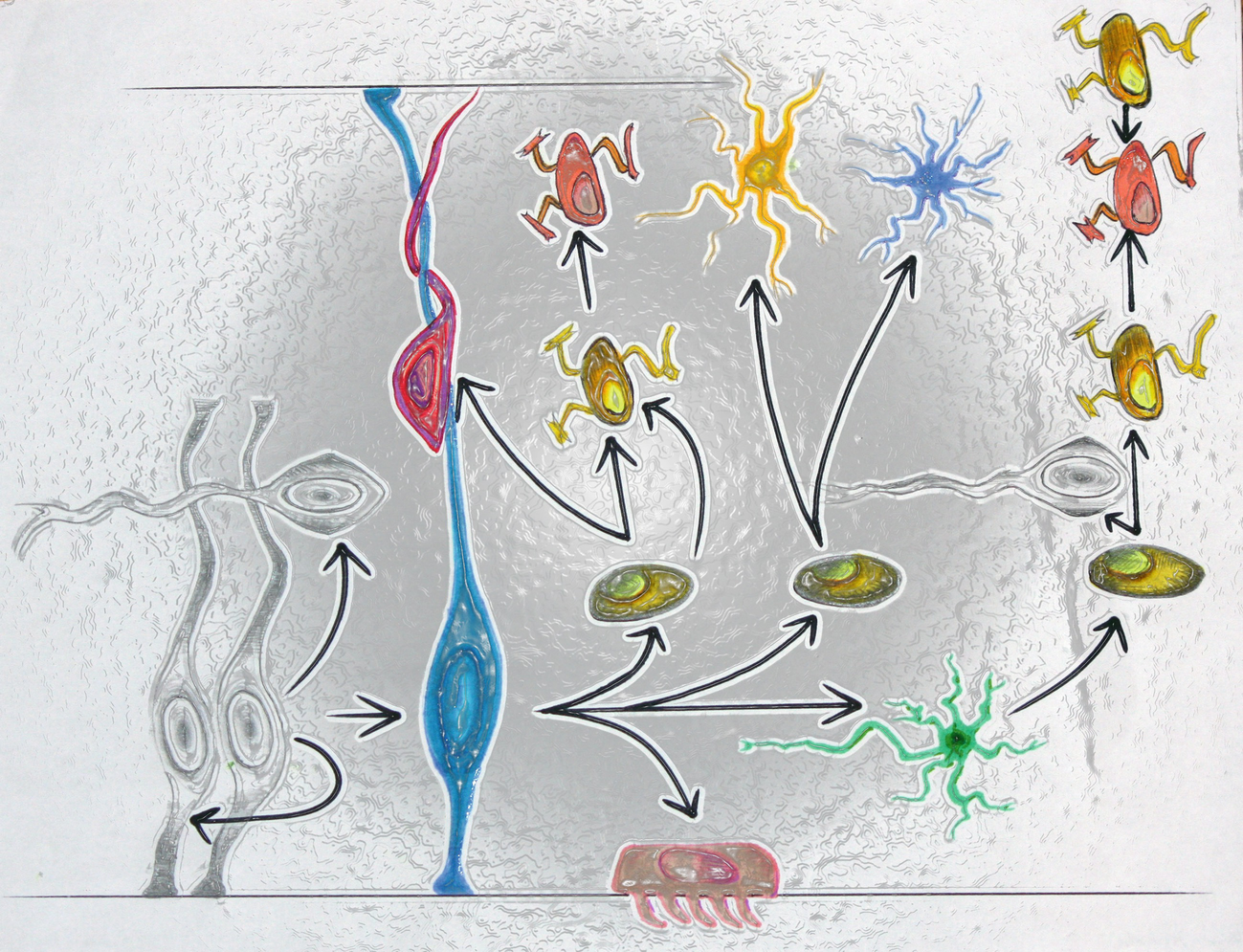
The process of neurogenesis as a reinterpretation of the model. In the bottom left ventricular zone, we observe the neural stem cell (neuroepithelial cell) and the neuron (silver), followed by the radial glial cell and the neuron (in blue and bright red, respectively), followed by type 3 cells (dark yellow), ependymal cell (gray/pink), subventricular-zone astrocyte (type 2 cell, in green) and oligodendrocyte precursor cell (in bright orange/yellow), all in the subventricular zone. In the white matter we observe oligodendrocytes (light orange) and ALDg1L+ GFAP+ (yellow)
From the clinical perspective, this field promotes a deeper understanding of disorders and diseases such as addiction, Alzheimer’s disease, amyotrophic lateral sclerosis, anxiety disorders, attention deficits and ADHD, autism spectrum disorder (ASD), many other psychiatric disorders including bipolar disorder, BPD, MDD, OCD, SAD and schizophrenia, but also brain tumors, cataplexy, dyslexia, Down syndrome, epilepsy, Huntington’s Disease, multiple sclerosis, narcolepsy, neurological AIDS, neurological trauma, Parkinson’s disease, stroke and Tourette syndrome. Technologies and techniques used in this setting make great use of MEG/EEG, MRT, TMS and tDCS/tACS with advanced analysis techniques. Among the many scopes of investigation in clinical and medical neuroscience, we find developing new clinical interventions for neurological and psychiatric disorders. Such interventions focus on the amelioration of medical, especially psychiatric, diagnosis, as well as developing patient-centered approaches, and multidisciplinary treatment teams. Furthermore, these changes link perspectives developed within translational science to new treatment theories and applications for (especially neuropathic) pain, speech/person recognition (including associative visual agnosia and category-specific visual object agnosia such as prosopagnosia), as well as identifying developmental risk factors in relation to biomarkers and genetic transmission, and improving treatment of addiction and lifestyle/behavioral problems. These include sleep patterns and multiaxial effectors on health and wellbeing, preventing and treating disorders of immunity or inflammation (in relation to psychoneuroimmunology), cerebrovascular disease, and metabolic and mitochondrial disorders, promoting further study of anesthesia, and (better) understanding of mechanisms and processes of neurogenesis and neurodegeneration.
4.2.2 Neurocritical Care or Neurointensive Care
In a study on critical neuroscience, the term ‘critical’ conveys a multilayered interpretation. In the context of neurocritical care or neurointensive care, the focus is on medical interventions targeting life-threatening diseases of the nervous system from the emergency department and intensive care unit through the operating room and post-surgical period. As with previous subfields of both medicine and neuroscience, a multidisciplinary approach is used to treat diseases such as trauma-related medical problems, (major acute) strokes, seizures and epilepsy; specific, local or non-localized intracranial edema or encephalitis; intracerebral and subarachnoid hemorrhages; meningitis; brain tumors, as well as to prevent or treat myasthenic crisis, spine/secondary neurological injuries and non-neurological/systemic issues, immune system-related problems such as Guillain-Barre syndrome and possible medical complications with the collaboration of treatment teams in anesthesiology, emergency medicine, neurology and neurosurgery. Given the nature of this discipline, efforts in this area cover technical and technological advancements, scientific discoveries, social policy and public health, as well as patient–provider relations, especially in the case of direct clinical care (in particular medicine and nursing, especially neuro-intensive nursing/care nursery as we have previously seen) and long-term and palliative care.
Many of the philosophical, social and legal debates around the individual’s functionality and ability to think and perform certain tasks following a medical or mental problem focus on both etiology of the condition and the individual’s personal action, that is, responsibility in terms of actions to take to prevent or treat the problem. The etiology of epilepsy is still unknown, although there have been many speculations based on scientific data and peer-reviewed research which appear to indicate a probable neurological cause, oftentimes following other medical problems located in the cerebral areas such as brain injury, tumors, infections, and stroke, as well as possible genetic factors, including birth defects. Aside from the more historical-spiritual/spiritist speculations (in any case absolutely confuted by modern science, in part due to the very scope and areas of investigation of evidence-based medicine) on possible demonic possession of once-called ‘Sacred Disease’, the issue of personal responsibility (leaving aside the free will problem for a moment) seems to have a clear answer: the person affected by epileptic seizure is not at fault (and we will further explore the complexity of personal responsibility, especially in the context of free will and lateralization) for either eliciting the problem or failing to prevent it; thus we can benefit from more research studies in those critical areas of medicine that deal with neural activity. In particular, neurocritical care or neurointensive care utilizes many theoretical and technological approaches to investigate these aspects. Studying the normal/regular/baseline function and the abnormal/mal-function of the nervous system, researchers develop cognitive, computational and developmental models of (expected) biochemical response or behavior in order to ameliorate the level of fidelity of artificial neural models and neurotechnological devices to mimic the natural neural networks. Focusing on complex aspects such as channel kinetics, synaptic transmission from the perspective of specific frameworks such as that of dynamic system theory, tri-dimensional network templates are created to combine theoretical investigations coded in mathematical equations to the actual (observed) behavior elicited. This approach can also be expanded via the modulatory application of brain-computer interfaces and virtual reality technologies to treat mental health disorders such as OCD as well as neurological disorders such as Parkinson’s disease. Although technological advancements in this area represent an interesting development of applied medical science, standard neural interfaces are used by engineers as a solid base upon which are determined the structure and function of the artificial neural renderings. More specifically, research studies focus on the regeneration of damaged or lost neural tissue via the engineered versions of the mechanical properties of the nervous system itself. Creating artificial electronic circuits mimicking the tissue is a very important part of neural-interfaced structures that replicate the electro-chemical activity in the body and account for the possible challenges and rejection of artificial materials by the body. In this context, further research developments cover microelectrodes and optical neural interfaces with fiber optics, as well as complete microsystems to collect and modulate multiple signals and deliver them to the neural tissue. Researchers can therefore study the properties of these chemical, electrical, magnetic and optical signals, including production, transmission and (artificial vs. natural) delivery modalities, that is, aperture, amplitude, length, shape and population of spikes/action potentials. Focusing on both neuromodulation and neuroregeneration, the cutting-edge scientific research contributed to regulating the electrochemical activity to correct and re-balance the neural functions of specific brain areas without negatively affecting neighboring regions and/or causing undesirable side effects such as alteration in visuo-spatial perception, psychomotor agitation and tremor, localized or generalized pain, and many others.
Furthermore, enhancing the naturally occurring neurogenesis using the above-discussed techniques helps address problems of partial/limited function or relative/absolute malfunction by using artificial-engineered tissues (as in spinal cord tissue) or neural prostheses allowing for stimulation, regeneration, reactivation of damaged areas and recording neural activity to foster adjusted signal neurotransmission or stimulation—for instance, Functional electrical stimulation or FES to restore motor processes—through artificial sensors interfaced with natural neural tissue or through the interaction between extracellular matrix protein and neural stem cells. Of course, narrowing down to pre-op and post-op elements of neurointensive care and management, we find ourselves in the realm of neuroengineering, which we already discussed in Chap. 1.
4.2.3 Neurosurgery and Neurology
As the medical aspects of the direct application of neuroscience for the clinical treatment of patients are discussed throughout this volume from a theoretical framework, we would like to provide a very brief definition of the specialties neurosurgery and neurology. As a sub-branch of medicine, neurology involves the clinical study of the nervous system, more specifically investigating medical conditions, disorders and diseases involving the central and peripheral nervous system.
The main difference between neurology and neurosurgery is in fact the focus on diagnosis, prevention, prognosis and treatment of such disorders of the latter. In this context, the surgical methods and follow-up rehabilitation techniques are an integral part of neurosurgery, albeit based on the scientific investigations developed in neurology. A related specialty to neuroscience, neurology is therefore also a closer discipline to both neuropsychiatry and neuropsychology, with specific sets of clinical interests on Agnosia, Agraphesthesia, Agraphia, Alexia, Amnesia, Anosognosia, Aphasia (especially thanks to the studies by Broca and Wernicke), Apraxia, Aprosodia, ADHD and ASD, but also disorders such as Alzheimer’s, Dementia, Dyslexia, Epilepsy, Psychosis, Stroke and TBI. Aside from the contributions of Alois Alzheimer, Karl Lashley, Arnold Pick and Norman Geschwind, other researchers such as Antonio Damasio contributed to further develop the discipline into behavioral neurology. Of course, among the most important research areas in these fields we need to mention neuroendoscopy and spinal surgery as more specialized subspecialties for neurological treatment, the surgical removal of tumors in the brain, the localization of new structures such as lymphatic vessels, the accuracy of techniques with frameless stereotaxy, and the beneficial effects of a more precise understanding of the neuroplastic activity to promote healing and growth processes.
4.2.4 Paleoneurology
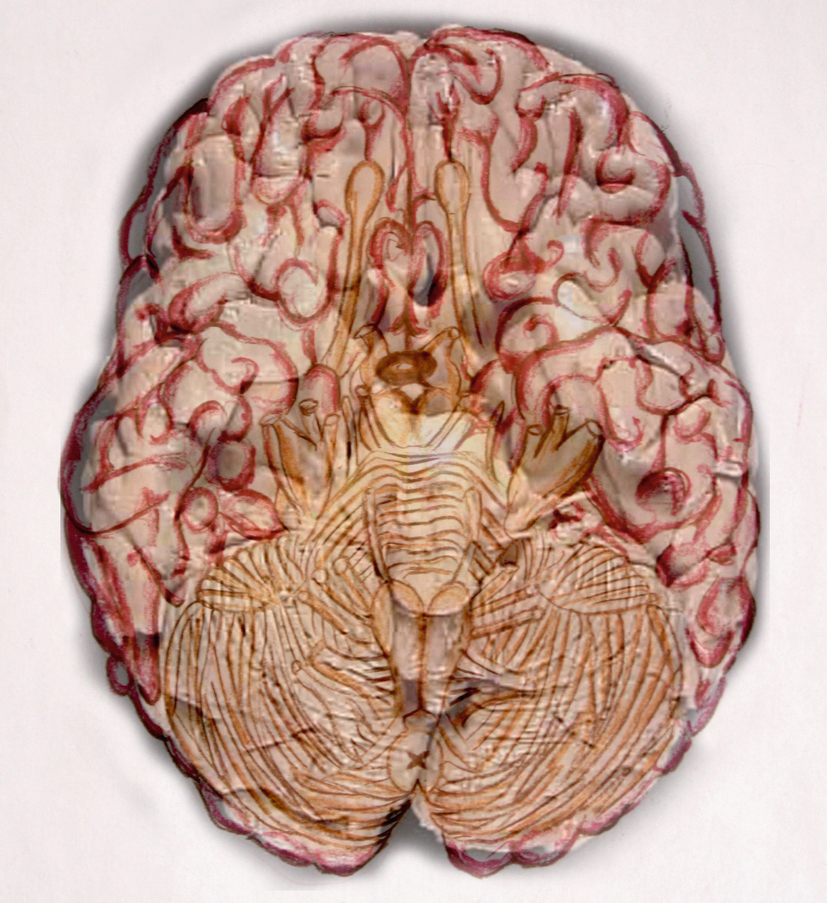
A ventral, semitransparent and superimposed view of the brain showing inferior olives, flocculi, middle cerebellar peduncles, optic tract, nerve, and chiasm, olfactory bulb and corpus callosum, infundibulum, mammillary body, cerebellum, pyramid, and posterior perforated substance
This research also comes with challenges such as the ones discussed previously and regarding the translation of data obtained via dioptograph-based measurements in actual-applicable information—from 3-D rendering to 2-D view—for different, extinct or living, species, as well as due to the conflicting points of view on the interpretation of these data. Differences in interpretation generally swing between more or less distance, in terms of anatomical-structural identification between human and non-human animals. For instance, some researchers believe that certain anatomical features are a sign of cerebral organization moving toward a more human pattern (in the case of Ralph Holloway and the endocast of Australopithecus afarensis), while others (in this example, Dean Falk) suggest that these patterns, more specifically the position of the depression, are indicators of the lunate sulcus, similarly to what is found in an ape-like sulcal pattern. Of course, some scientists believe that similarities between skulls from different species could provide proof of relations, which could be justifying similarities in cognitive-emotional functions as well. From this perspective, geometry, asymmetry and/or unevenness (petalia) between right and left hemispheres could indicate hemispherical specialization, which in turn could account for specific qualitative/quantitative differences in terms of emotion and behavior, as well as processing ‘speed’ in terms of computational-cognitive performance.
4.2.5 Neurophysiology
The combination of comparative studies found in paleoneurology and the analytical research in disciplines such as neuroanatomy and neurology contributes to the strength of neurophysiology as a scientific field interested in the functional properties of the nervous system, more specifically of glia, neurons and neural networks. Of course, neurology contributes to a further understanding of disorders from a medical-scientific perspective, while neurophysiology—aside from being, at least academically, not a sub-branch of (clinical) medicine—studies ‘the whole spectrum’ of neural function, including its physiology. Of course, further differentiation and specialization in areas such as clinical neurophysiology—which is part of medicine in countries like the United States, and a separate field in many European countries—truly bridge the two, artificially separated, perspectives. From the perspective of research tools, neurophysiology uses technologies similarly to the ones utilized by psychophysiology and psychological physiology. Therefore, molecular biology-based technologies are used in combination with multiple imaging techniques such as calcium imaging, electrophysiological recordings (including patch and voltage clamp) but also field potential and single-unit recording technologies, and optogenetics resources.
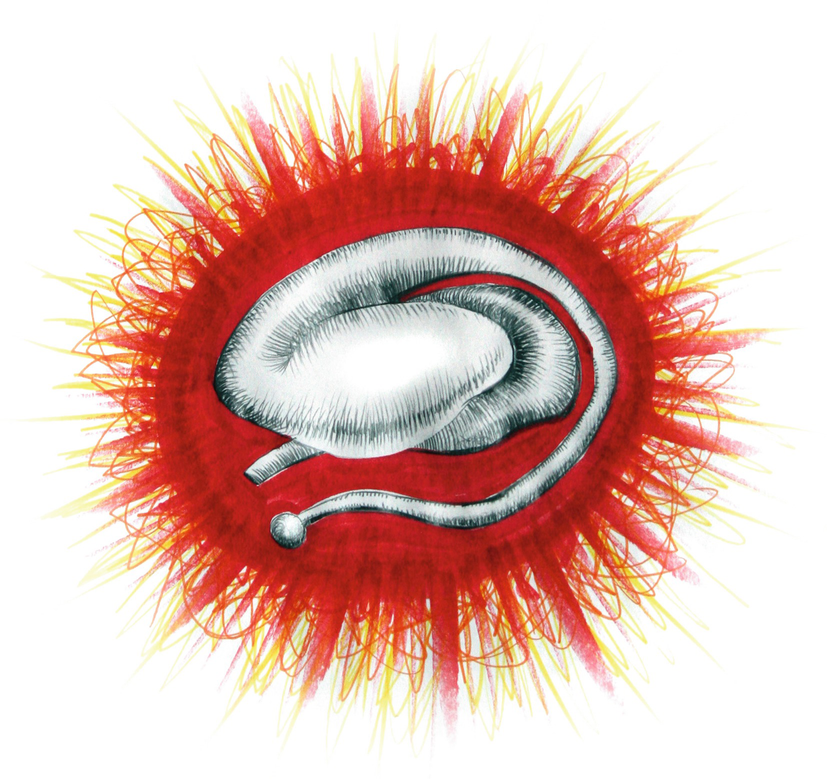
Rendering of the basal ganglia with pallidum, striatum, substantia nigra and subthalamic nucleus
4.2.6 Psychoneuroimmunology, Psychobiology and Psychopharmacology
In a volume addressing critical aspects of the mind-brain-problem, it is fundamentally important to discuss the connection between disciplines involved with the study of the mind-psyche, the study of biology and the study of immunology. As psychobiology is a term often used as a synonym for behavioral neuroscience, we will refer the reader to our analysis of such discipline, as found in Chap. 2, Between Psyche and Mind. In any case, as psychobiology “describes the interaction between biological systems and behavior” (British Psychological Society 2015), the focus on the system-based (especially the nervous system) processes determines the mechanic basis of emotions-thoughts, and actions. A further elaboration of this point of view and methodological framework is represented by psychoneuroimmunology (a term officially used in academia for the first time by the psychologist Robert Ader and the immunologist Nicholas Cohen, while studying conditioning and immunosuppression), which further develops the analysis on the connection between these elements. Psychoneuroimmunology moves the attention onto the etiological and diagnostic aspects of possible medical-mental syndromes and disorders (especially including allergies, hypersensitivities, intolerances, immune deficiency, and autoimmune diseases), and preventive measures to foster effective health strategies and well-being. Moreover, psychoneuroimmunology promotes a more comprehensive view of the effects which complex symptomatologies and processes such as the HPA axis and the stress response on psychophysical well-being. This is evidenced by the studies of Hans Selye on ‘General Adaptation Syndrome’ and George Solomon on ‘psychoimmunology’. Thus, this discipline connects multiple systems, including the nervous, immune and endocrine systems as evidenced by the alternative names it is known by, that is, psychoendoneuroimmunology or psychoneuroendocrinoimmunology. For these reasons, the history of psychoneuroimmunology dates back to both ‘holistic’ approaches of traditional-ancient medical practices as well as, in the modern sense of evidence-based medical science, the studies by Claude Bernard and Louis Pasteur. In this sense, definitions such as the previously encountered ‘pneuma’, ‘vis vitalis’, ‘milieu interieur’ (internal state) and ‘homeostasis’, all define the focus and scope of analysis and intervention of psychoneuroimmunology, and define the viewpoint according to which health disorders truly describe disturbances, dislocation, disruption, perturbation of a (natural) order, which creates, monitors and promotes the regular/regulated functions of the body. In the case of the homoeostatic process of course, the final stasis in never achieved, as it would imply (mean) instant death, being the intention-tension, an ever functioning ‘motion/movement towards balance’ without ever fully achieving it. These balancing features are at the center of the connection between mind and body, and it is important to understand that, although some scholars would completely disagree with the existence of a dualistic separation of the two, and some would argue for a monistic perspective according to which only matter (in our case, the body, especially the CNS) exists, from the perspective of clinical interventions saying that mind and body influence one another is at least very useful and effective to promote health.
Psychoneuroimmunology, psychobiology and psychopharmacology are also among the primary strategies to understand empathy. In fact dopamine and serotonin, associated with the emotion center of the brain, which is in turn connected to the brain’s reward center, are the primary neurotransmitters that modulate our biologically-based connection to the external world, in terms of praise and reward, but also in relation to stressors and triggers, and human interaction starting with the earliest stages of development. This obviously includes mother-infant connection and the fact that human babies thrive when there is empathy, having the most postnatal neuronal growth of any species (Marci et al. 2007), fundamental in the psychoneural development of attachment, which in itself is fundamental for our survival. From the perspective of neuroscience, several studies clearly indicate that the stress response is also mediated by these connections, as mothers directly impact their babies’ cortisol levels by their reaction to internal and external stressors and related hormonal levels. More specifically, these reactions cause different responses in the modulatory ability of their children (Lyons-Ruth et al. 2013). In summary, psychoneuroimmunology, psychobiology and psychopharmacology research studies indicate that our physical health depends on our biology and its related activity on multiple levels, especially in the endocrine, immune and nervous systems. Thus, health depends on the factors that directly influence biology and is influenced by biology, as in our sense of connection-connectivity-connectedness with others. In the context of practical applications of neuroscientific research on mind–body medicine, Candace Pert was able to show that neuropeptides and neurotransmitters directly impact the immune system, and that this system and the endocrine systems are modulated by the entire central nervous system (therefore, not only the brain) and are connected deeper to the processes involved in emotions, cognition, self-awareness, etc. Another important research on neuro-immune interaction came from David Felten, while new perspectives on the Enteric (Intrinsic) Nervous System, the so-called Second Brain and the function of gastroenteric neurotransmitters from the studies conducted by McConalogue, Furness, Gershon, Lißina-Krause, Lychkova, Baldissera, Luczak and Porro. More specifically, connecting multiple systems, and working, for instance, on perspectives of immune alterations producing changes in behavior, and (vice versa) behaviorally induced changes to the immune system, directly help disciplines such as psychopharmacology to study the best medication strategies for the treatment of mental health disorders, fostering an understanding of “Protein binding (how available the medication is to the body), Half-life (how long the medication stays in the body), Polymorphic genes (genes which vary widely from person to person), and Drug-to-drug interactions (how medications affect one another)” (The American Society of Clinical Psychopharmacology 2015).
Of course, scientific efforts in psychopharmacology did not come without controversies, especially regarding the possibility of artificially induced behavioral aspects in subjects, and thereby changing their (self) awareness, perspectives, and, according to some, even conscience-consciousness. In this regard, we refer to the Vichian expression coscienza non è conoscenza.1 This is true not only for the earliest stages of psychopharmacological research on psychotropic agents (especially barbiturates and opiates), but far into contemporary analysis and clinical use of antipsychotics and antidepressants (including selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, noradrenergic and specific serotonergic antidepressant, reversible monoamine oxidase A inhibitors, tetracyclic antidepressants tricyclic antidepressants), benzodiazepines and others.
List of the most important neurotransmitters and neuroreceptors subdivided by type/class

List of the most commonly prescribed modern psychotropic medications with generic and US brand names
Antidepressants | Antipsychotics | Stimulants |
|---|---|---|
Selective serotonin reuptake inhibitors, SSRI: Celexa (citalopram) Luvox (fluvoxamine) Paxil (paroxetine) Prozac (fluoxetine) Zoloft (sertraline) Tricyclics: Anafranil (clomipramine) Asendin (amoxapine) Elavil (amitriptyline) Norpramin (desipramine) Pamelor (nortriptyline) Sinequan (doxepin) Surmontil (trimipramine) Tofranil (imipramine) Vivactil (protriptyline) MAOIs: Nardil (phenelezine) Parnate (tranylcypromine) Others: Effexor (venlafaxine) Desyrel (trazodone) Ludiomil (maprotiline) Parnate (tranylcypromine) Wellbutrin (bupropion) Zyban | Typical antipsychotics: Haldol (haloperidol) Haldol Decanoate (long acting injectable) Loxitane (loxapine) Mellaril (thioridazine) Moban (molindone) Navane (thiothixene) Prolixin (fluphenazine) Serentil (mesorizadine) Stelazine (trifluoperazine) Thorazine (chlorpromazine) Trilafon (perphenazine) Atypical antipsychotics: Aibilfy (aripiprazole) Clozaril (clozapine) Risperdal (risperidone) Seroquel (quetiapine) Zyprexa (olanzapine) | Adderall (amphetamine, mixed salts) Concerta (methylphenidate, long acting) Cylert (pemoline) Dexedrine (dextroamphetamine), Dextrostat Dexedrine Spansules (dextoamphetamine, long acting) Metadate (methylphenidate, long acting), Ritalin SR Ritalin (methylphenidate), Methylin |
Mood stabilizers (Antimanic agents) | Antianxiety drugs | Anti-obsessive agents |
Depakene (valproic acid, sodium divalproex) Depakote Lamictal (lamotrigine) Lithium, (lithium carbonate) Lithobid Tegretol (carbamazepine) Topamax (topiramate) | Ativan (lorazepam) BuSpar (buspirone) Klonopin (clonazepam) Lexapro (escitalopram) Librium (chlordiazepoxide) Serax (oxazepam) Tranxene (clorazepate) Valium (diazepam) Xanax (alprazolam) | Anafranil (clomipramine) Luvox (fluvoxamine) Paxil (paroxetine) Prozac (fluoxetine) Zoloft (sertraline) |
Anti-panic agents | ||
Klonopin (clonazepam) Paxil (paroxetine) Xanax (alprazolam) Zoloft (sertraline) |
Certainly, culture plays a fundamental role in determining the indications for medications in every geographical area in the world, and that is true for both modern, laboratory-based pharmacology, as well as for natural remedies, folk medicine and ethnobotany-ethnopharmacology (although, to be fair, the very definition of ‘ethno-’ is in itself an ethnocentric separation similar to ‘complementary and alternative medicine’). This also means that, once again, psychiatric disorders are very rarely individual disorders, and much more inter-individual, social, situated, cultural, societal disorders, and therefore require a further analysis of brain, culture and society, as we will see in the next chapter.