1937 Spasticity Control and Elimination
SPASTICITY—THE BEAST UNMASKED
_______________
What Is It?
Spasticity is a disorder that is rarely fully explained to stroke survivors. Clinicians tend to describe spasticity in terms of its effect on muscles or body parts. For instance, they may say, “The stroke causes your hand to be tight,” or they may say, “Your muscles are tightening because of the damage caused to your brain by the stroke.” These explanations of spasticity are incomplete. You need the whole story. Without an understanding of the cause of spasticity, there is little chance of reducing spasticity. Spasticity reduction, like most of stroke recovery, comes from the inside out. Only stroke survivors can reduce their spasticity. Like so many other aspects of stroke recovery, stroke survivors “drive their own nervous system” toward recovery. Spasticity is a nervous system issue. Spasticity is caused by the brain’s lack of control over muscles. Muscles are affected, but are not the cause.
How Is It Done?
How can spasticity be reduced or eliminated in a way that does not involve drugs or surgery? The only way to silence spasticity is to restore control of the spastic muscles to the brain. Using the neuroplastic process is the only way to restore control of the muscles. An understanding of spasticity will help you use the neuroplastic process to reduce spasticity.
194Here is an explanation of spasticity that is scientifically correct and, hopefully, easy to understand:
How the brain controls muscles before stroke:
• Your brain tells your muscles when to contract (tighten, to help you move) and when to relax.
How the brain works after stroke:
• Stroke kills part of the brain responsible for control of affected muscles.
• The damaged part of the brain no longer “hears” those muscles.
• The brain no longer tells affected muscles when to contract or when to relax.
If your brain is not fully able to control your muscles, what makes them tight? Are the muscles acting alone? Or is something telling them to tighten?
How the spinal cord causes spasticity:
• Muscles constantly send signals to the spinal cord. Normally, the spinal cord sends those signals up to the brain.
• Because of the stroke, the brain no longer gets the messages sent from the muscles, so the brain no longer “hears” the muscles. Because of this lack of communication, muscles are under no brain control. Muscles hate being out of control because it means they may overstretch and tear (muscles tear easily).
• Since the brain cannot keep muscles from tearing, the spinal cord takes over the job.
• The spinal cord can only send out one message to muscles: “Muscles, contract!” The spinal cord is a poor brain, but it was not designed to be a brain. It was designed to be a “messenger boy” from brain to muscles and from muscles to brain. Spasticity is a bad thing, but without the spinal cord giving the “Muscles, contract!” command, those muscles would be flaccid (completely and utterly relaxed). Flaccid muscles can lead to tearing of the muscles, subluxation of the shoulder, shoulder-hand syndrome, and so on.
• Impulses from the spinal cord protect muscles by keeping them immobile.
— Good news: The spinal cord protects that would otherwise be flaccid and at risk.
— Bad news: The protection provided by the spinal cord leads to spasticity.
— More good news: Spasticity can help you move, help keep muscles and bones strong. And, at least some messages are getting through to “bad side” muscles.
— More bad news: Too much spasticity can cause a complete lack of movement. Very spastic muscles can turn into something other than muscle (connective tissue) and cause contracture.
The impulse that the spinal cord sends out to protect muscles is similar to a stretch reflex. An example of this is when a doctor tests reflexes with a reflex hammer. When the doctor hits you right below the kneecap, your knee extends. The knee extends whether you want it to or not. The movement of the leg kicking forward is called a stretch reflex. Stretch reflexes stop muscle tearing by instantly shortening muscles. Imagine if the doctor hit the knee over and over and never stopped. Spasticity can be viewed in a similar way. That is, spasticity is a repetition of reflexes.
What spasticity does:
• The spinal cord tells the muscles to contract (shorten).
• This command is spasticity.
• In a matter of a few days, spasticity permanently shortens some muscles.
• Shortened muscles perceive any lengthening as a threat of tearing.
• The muscle sends out an increased amount of “Help! I’m tearing!” messages to the brain and spinal cord. But the brain never “hears” the message because the brain was injured by the stroke.
• The spinal cord continues to send signals to the muscle to tighten.
196Here is a representation of the process of spasticity in the stroke survivor:
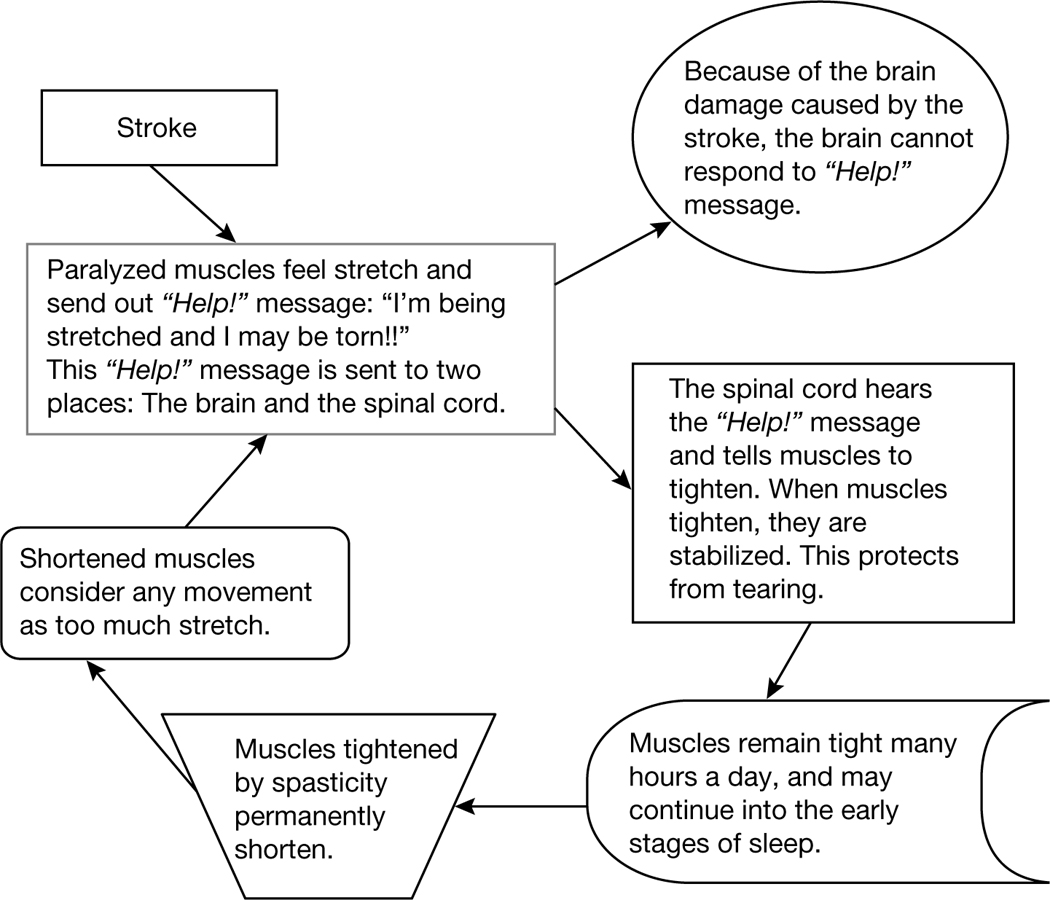
And around and around it goes: The muscle keeps saying “Help!” and the spinal cord says “Contract!” This process makes the muscle tighten even more, causing more “Help!” signals from the muscle. In some survivors, spasticity can continue during everything but the deepest stages of sleep. In most survivors, however, spasticity wanes before the survivor falls asleep.
What Precautions Should Be Taken?
None.
NEUROPLASTIC BEATS SPASTIC
_______________
The brain uses muscles to control movement. Muscles will contract and relax in a precise way to allow you to move fluidly. After stroke, the connection between brain and muscles on the “bad” side is broken. The “bad” side 197muscles may be under little (if any) control, and muscles hate being out of control. Since the muscles are no longer under control, they turn to the spinal cord for control. It is this relationship between muscles and spinal cord that is the core of spasticity. After a stroke, the brain can no longer protect the muscle from being overstretched and torn, so the spinal cord takes over and tells the muscles to stay tight, which protects them from being torn. Spasticity is a protection mechanism. The problem, of course, is that tight muscles make it difficult to move. No drugs, therapies, or modalities will permanently eliminate spasticity. They are all temporary; once they are withdrawn, spasticity returned. There is hope, however. Hiding in plain sight, the answer to the riddle of spasticity may be simple: Repetitively move the spastic muscles.
The Neuroplastic Model of Spasticity Reduction
Purging muscles of spasticity involves our old friend, neuroplasticity. The stroke kills the part of the brain that controls spastic muscles. But what if that was reversed? What if you could dedicate more brain to spastic muscles? That is the neuroplastic model of spasticity reduction. The idea is to use techniques that will give spastic muscles a larger part of the brain. When control of muscles is retaken by the brain, spasticity wanes. Muscle tightness will become less intense, which will, in turn, provide more control of movement. More control of movement will allow for a wider range of movement. A wider range of movement will allow the body to drive more changes in the brain. The more control the brain has over muscles, the more movement is available. The more movement available, the more brain changes can be driven, and so on.
The primary tool used to re-establish brain control over spastic muscles is repetitive practice. For instance, constraint-induced therapy, which uses a lot of repetitive practice, will often decrease spasticity. But your efforts to regain brain control over spastic muscles are not required to follow any standardized “treatment” or “protocol.” Getting the brain to take responsibility for muscles requires using those muscles over and over (repetitively). These repetitive efforts should also be challenging—“nipping at the edges” of your current ability.
Put simply:
• Repetitive and challenging practice of spastic muscles reduces spasticity because . . .
— Repetitive practice restores brain control over muscles
— Restoring brain control over spastic muscles reduces spasticity
198How Is It Done?
The downward spiral after stroke:
Stroke → The part of the brain that controls muscles is damaged → The brain cannot control, or protect, muscles → The spinal cord protects muscles by making them tight → Muscles permanently shorten → Tight, shortened muscles make movement difficult.
The upward spiral after stroke:
Repetitive practice rewires the brain → The brain regains responsibility for muscle control → The spinal cord gives control of muscles to the brain → Spasticity declines or is eliminated → Movement is made more normal.
The only way to permanently reduce or eliminate spasticity is by rewiring the brain to regain control over muscles. The same recovery options that promote brain rewiring will reduce spasticity as well. Increased movement and reduced spasticity are two sides of the same coin.
• As spasticity decreases, the ability to move improves.
• Improved movement chips away at spasticity.
Let’s be clear about this: The neuroplastic model of spasticity reduction involves activating spastic muscle repeatedly. This is controversial among some healthcare workers. Many in healthcare were taught to not use spastic muscles. The reasoning was this: If you use spastic muscles you’ll increase the strength of those muscles. If you strengthen spastic muscles, spasticity gets worse by strengthening the spastic pull. There are two problems with this thinking:
• Spastic muscles are weak. So even if you strengthened them, it would not necessarily be a bad thing.
• The brain will regain control over spastic muscle, thereby decreasing spasticity, but only if those muscles voluntarily move. Spastic muscles, when used in a repetitive way, increase their brain representation. That’s the neuroplastic model of spasticity reduction.
Spasticity is not just bad because it affects muscles—spasticity also affects the brain. Animal research studies have shown that if a limb is immobilized (usually by strapping the limb to the body), the number of brain cells dedicated 199to that limb shrinks. This is exactly what happens to stroke survivors with spasticity. Their muscles are immobilized by spasticity. If the spastic muscles resume movement, the portion of the brain representing those muscles will get larger. As more brain power goes into those muscles, spasticity will subside.
Treatments that physiatrists and neurologists use can help you to rewire your brain to regain control over spastic muscles. These doctors have specialized training in treatments that reduce spasticity. Some drugs and other treatments provide temporary relief from spasticity. The temporary relief can allow for easier movement. The temporary relief may also help create an opportunity for the hard work of rewiring your brain.
Drugs used to reduce spasticity fall into two groups:
• Those given locally (injected directly into the spastic muscles) or administered into the fluid surrounding the spinal cord. These drugs affect only specific muscles.
• Those taken orally. These drugs will affect all the muscles in your body.
These drugs can reduce spasticity, which can:
• Improve movement
• Increase the potential of recovery
• Curb potential bone and joint problems
• Reduce pain
• Increase strength
• Reduce the risk of contracture
• Set the stage for neuroplastic change
Ask your doctor about these options. Remember, though, these medications will not address the underlying cause of spasticity (lack of control by the brain over muscles). No drug will replace the hard work needed to rewire your brain. The drugs and other treatments that temporarily reduce spasticity provide a window of opportunity for you to do the hard work of rewiring the brain.
The hard work comes in the form of:
• Constraint-induced therapy
• The use of repetitive, task-specific massed practice
• Some electrical stimulation (e-stim) treatments
• Some forms of bilateral training
• Mental practice
This list will grow with emerging research, so continue to explore the research and ask lots of questions.
What Precautions Should Be Taken?
Consultation with your doctors, therapists, and other health professionals will help direct your therapy so that spasticity reduction is achieved with a minimum of waste and a maximum of treatment effect.
You and your doctor may decide to use spasticity medications for reasons other than offering a window of opportunity for neuroplastic change. There may be other very good reasons for oral and other forms of spasticity medications. Reasons for continued use of systemic spasticity medications may include better mobility, less pain, better movement, and so on.
SPASTICITY, TONE, AND CONTRACTURE: EVEN CLINICIANS GET IT WRONG
_______________
Spasticity after stroke is often confused with tone and contracture, but they are different.
Confusion About the Terms Spasticity and Tone
Spasticity, and all the other muscles issues mentioned earlier, are often confused and conflated—even by clinicians. It is important to know the difference because they are
• Caused by different things
• Diagnosed differently
• Treated differently
201How Is It Done?
If the muscle has
Tone: The muscle is normal. Muscle is easily moved. Evident, and measurable with electromyography (EMG), tone exists even in relaxed, “normal” muscle. The brain is doing its job controlling muscles well.
Spasticity: Muscles are stiff but moveable. The stiffness increases when the muscle is moved fast. Spasticity is said to be “velocity dependent”; the faster you extend (lengthen) the muscle, the more resistance you get. The part of the brain responsible for the spasticity is not doing its job.
Contracture: Muscles are not moveable. The muscle has become shortened. Although it is often confused for spasticity, it is not spasticity. It may be caused by spasticity, but it is not spasticity. Spasticity is a brain problem. Contracture is a muscle shortening problem.
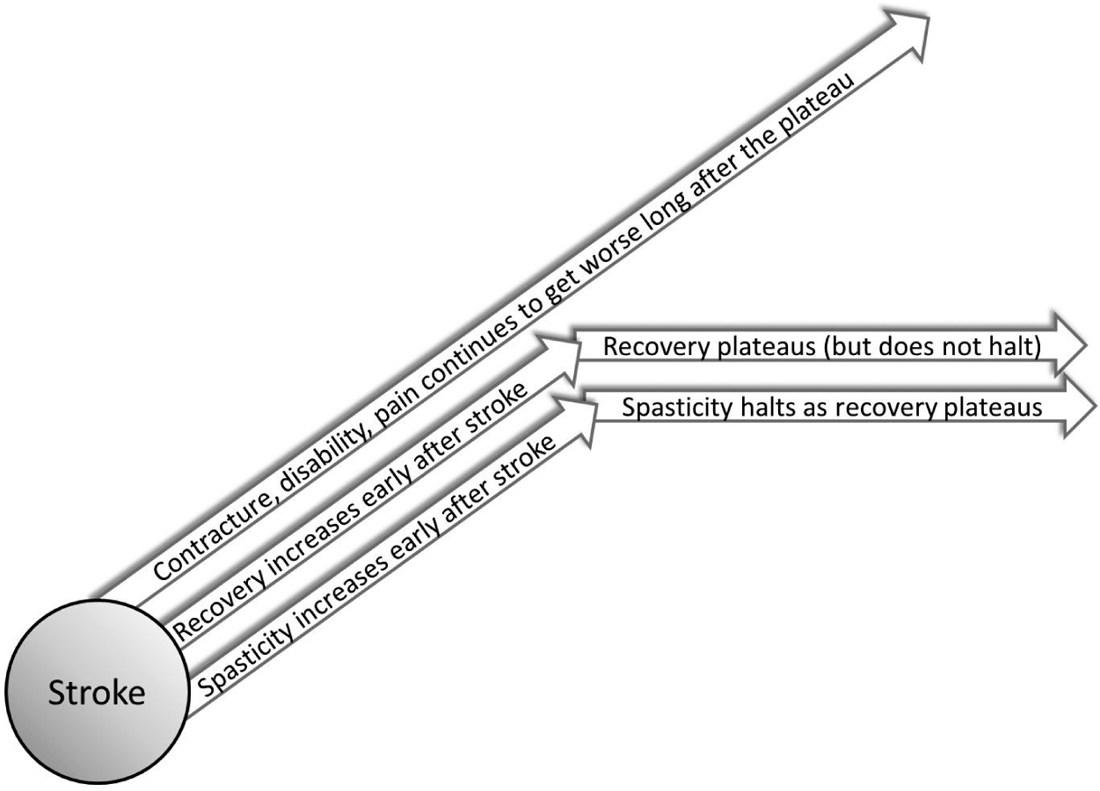
Although most clinicians think that spasticity after stroke is progressive (gets worse), this is only true in some survivors, and only before the plateau. Once the stroke has occurred, spasticity may (or may not) get worse. If it does get worse, the amount of spasticity will not get any worse once 202the survivor has plateaued. So, once the survivor plateaus, the spasticity plateaus. The reason clinicians think that spasticity gets worse over time is because they confuse spasticity with other problems brought on by the spasticity. Those things include pain, deformities, a loss of range of motion in the joint, and contracture. Spasticity does not get worse, but all those other things do get worse.
So, again, tone, spasticity, and contracture
• Are caused by different things.
— Tone: An intact brain
— Spasticity: The part of the brain that should be controlling the spastic muscles is not (because of the stroke)
— Contracture: Caused by spasticity, but now a muscle problem: The muscle is too short
• Are diagnosed differently
— Tone: feels normal when the muscle is extended
— Spasticity: The faster the muscle is moved, the more resistance there is to the movement
— Contracture: No matter the speed, there is the same amount of resistance
• Are treated differently
— Tone: No need to treat!
— Spasticity: See suggestions throughout this chapter
— Contracture: Serial casting and tendon lengthening (a surgery where the tendon is cut so the joint can be taken through its full range of motion)
What Precautions Should Be Taken?
A clinician well trained in diagnosing the difference between tone, spasticity, and contracture should be consulted to make this determination. In large rehabilitation hospitals there are often “spasticity clinics.” These clinics are staffed with clinicians that know how to diagnose and treat spasticity and contracture.
203SPASTICITY—JEKYLL AND HYDE?
_______________
What Is It?
In some ways, spasticity can be of temporary benefit as you move away from the “flaccid phase” of recovery.
Immediately after their stroke, some survivors are flaccid (limp) on the affected side. Nothing on the affected side can be moved under the survivor’s own power. This is a scary time for survivors and their families. It is a cruel joke that stroke survivors are at their worst right after their stroke, when they are least able to understand and react to what has happened.
Research indicates that survivors who are flaccid for a year after their stroke can expect limited recovery. But some stroke survivors, who think they are flaccid, actually are not. Part of the problem is the words that are used to describe problems with movement. The word “paralyzed” is often used by folks who actually mean “hemiparetic.” Hemiparetic means weakness on one side of the body, not paralysis. There are only two kinds of true paralysis after stroke:
• Flaccid paralysis (muscles do not contract—flex, fire, or move)
• Spastic paralysis (muscles are so tight with spasticity the survivor cannot move them)
These forms of paralysis are rare. Most stroke survivors fall into a broad category of “hemiparetic.”
Some folks think this is a distinction without a difference, but they are wrong. Small amounts of movement can be used as a jumping-off point for much larger and more coordinated movement. So there is a huge difference between “no movement” and “small amounts of movement.” Someone who is flaccid after a year has a poor prognosis for return of movement. Someone who has small amounts of movement has retained the brain-muscle connection, and growing that connection means there is potential for greater movement.
The Brunnström stages reveal that, as people recover from stroke, they go from a period of being flaccid and emerge into a period in which 204they are spastic. Having spasticity emerge is seen as a period of hope because muscles are finally able to contract. With the emergence of spasticity, often small amounts of synergistic movement occur.
Brunnström’s stages state that after the flaccid period comes the emergence of spasticity. Can spasticity be viewed in some sort of positive light? The fact is that there are bad and good aspects to spasticity.
How Is It Done?
Spasticity is bad because it:
• Shortens muscles and other soft tissue, which can lead to permanent shortening (contracture)
• Positions joints abnormally, which makes limbs less functional
• Interferes with normal activities
• May cause pain
• May cause insomnia
• May cause deformities
• May cause poor weight gain (permanently contracted muscles burn a lot of calories)
• May cause pressure sores
Spasticity is good because:
• It is useful protection in cases of “unilateral spatial neglect” (when the stroke survivor is less aware or completely unaware of the affected side). For instance, in the arm and hand, spasticity will pull the limb across the body. This may be more desirable than the flaccid state, in which the limb is flopping around and fingers and arm are at risk for injury
• Is a step in the right direction from flaccid
• It may build bone strength (using Wolf’s law), reducing the risk of osteoporosis
• It can be used to substitute for strength, allowing standing, walking, and gripping
• It sometimes makes transfers (e.g., going from sitting to standing) easier
• It may improve circulation, preventing blood clots and swelling
• It maintains muscle bulk
What Precautions Should Be Taken?
The emergence of spasticity can be seen as a positive sign in the overall arc of recovery. But once spasticity has been established, the next stage of recovery requires the reduction and eventual elimination of spasticity. As is true with much of stroke recovery: When one job is done, another begins.
GIVE SPASTICITY THE ONE–TWO PUNCH
_______________
Healthcare workers and stroke survivors sometimes make the mistake of thinking that spasticity in the arm is an arm problem or that spasticity in the leg is a leg problem. One thing is clear: Spasticity is a brain problem. Spasticity is a symptom of the brain damage caused by stroke. Spasticity is a protection mechanism that keeps muscles from being torn. The brain is no longer doing its job, so the spinal cord takes over the job of protecting muscles, joints, and other soft tissue (i.e., nerves, blood vessels, and the muscles themselves). The spinal cord sends out one message, over and over: “Muscles, protect yourself! Tighten!”
Many researchers believe that if enough of the right kind of neuroplasticity (brain rewiring) can occur, spasticity will be reduced; but there is a problem. For the neuroplastic process to start, you need the ability to initiate movements. If spasticity is too strong, movement becomes impossible. If neuroplasticity needs some movement, but the stroke survivor’s limbs and fingers don’t move because of spasticity, how do you jump start the process? For some stroke survivors, there may be a way.
There are three medications that can be used to target the specific muscles that are spastic: Botox, phenol, and alcohol. Together they are called “nerve blocks.” Nerve blocks are usually administered by physiatrists or neurologists.
Botox
Botox has gotten most of its press because folks use it to get rid of wrinkles. The way it eliminates wrinkles is important in understanding how it works on spastic muscles. Lines in your face are created and accentuated by the 206muscles that move your face around during frowning, squinting, and raising the forehead. A doctor can inject Botox, which temporarily paralyzes these muscles and relaxes the muscle’s pull on your face, allowing for fewer wrinkles. Botox works on spastic muscles in the same way: It relaxes spastic muscles.
If you hear the word “botulism” and immediately think of the food poisoning that makes people ill from eating food that has gone bad, you are right. Botox is made from the same bacteria that causes botulism. That bacteria, called Clostridium botulinum, gives off a substance that can paralyze muscles. This substance is harvested from the bacteria to make Botox. Botox does not contain the actual bacteria that causes botulism and does not give patients botulism. Botox decreases the release of acetylcholine, which is a chemical that allows a nerve signal to reach the muscles. In this way, it blocks nerve impulses, like those that cause spasticity.
Phenol and Alcohol
These medications are injected directly into spastic muscles. Like Botox, they temporarily weaken spastic muscles, thereby reducing spasticity. Prior to the introduction of Botox these medications were used quite often. It should be pointed out that both phenol and alcohol as spasticity-blocking agents are significantly less expensive than Botox.
The combination of nerve blocks and exercise techniques used to initiate movement can be effective in improving movement and permanently reducing spasticity. Botox is injected into tight muscles, and those muscles then relax enough to unmask available movement. The idea is to allow for recovery options that promote brain rewiring using movement that was impossible to achieve prior to the administration of the nerve block. Each treatment with nerve blocks usually relaxes the treated muscles for a few months. This treatment provides a window of opportunity to increase active (self-propelled) movement. However, some nerve blocks can be administered more than once, so multiple opportunities to increase movement exist.
There is a new treatment for spasticity reduction. It’s called hyaluronidase and, like Botox and both phenol and alcohol blocks, it is injected directly into the spastic muscle. It shows promise, and has one unique advantage over other nerve blocks: Hyaluronidase does not cause weakness in the injected muscles. That’s important because the other nerve blocks cause weakness. Normally a 207survivor may be accustomed to having those muscles spastic and sometimes uses the spasticity to be more functional. For instance, a survivor may use muscles that are spastic around the knee to stabilize the knee during walking. When nerve blocks are injected, the survivor no longer has the spasticity to “lean on” and this can lead to less function and even falls. Hyaluronidase does not cause weakness and the muscle can be used. Here is a way to look at it: Nerve blocks make the spastic muscle weaker. Hyaluronidase “lubricates” the muscle so it is less stiff and more under the control of the survivor. This is an emerging therapy, and is not yet ready for widespread use.
How Is It Done?
There is a combination of treatments that, when used properly together, can jump start the process of spasticity reduction and encourage movement. This combination of treatments has three parts:
1. A nerve block is injected directly into spastic muscles.
2. (This step may or may not be necessary.) Electrical stimulation (e-stim) is used to help develop your ability to begin to move, even a little bit. The type of e-stim comes in one or more of three forms:
• Cyclic e-stim
• Electromyography (EMG)-based biofeedback e-stim
• E-stim functional orthotics
3. Options that promote brain rewiring are used.
Example A: Robert cannot lift his affected foot because there is a lot of spasticity in the muscles that force the foot down (the calf muscles). He goes to his doctor. His doctor refers Robert to a physiatrist.
• The physiatrist uses a nerve block to relax the calf muscles.
• Once the spastic muscles are relaxed, Robert works hard to lift the foot. He also does a lot of stretching of the calf muscles. His relaxed muscles allow him to stretch more than he has been able to since his stroke, but Robert continues to have trouble lifting his foot, even a little, on his own.
• Robert’s physical therapist suggests cyclic (on, off, repeating) electrical stimulation on the muscles that lift the foot. Progress is slow, and since nerve blocks only last a few months, Robert suggests to his therapist that he try something he has read about: electromyography (EMG)-based electrical stimulation.
• The combination of the nerve block and the electrical stimulation works. Robert can lift his foot a little bit.
• Robert uses the newly gained bit of movement repetitively to build muscle and rewire his brain neuroplastically.
Example B: Kathy’s hand is always flexed at the wrist and fingers. Spasticity is forcing her hand into a permanent fist, forcing the fingernails into the flesh of the palm. This causes cuts in Kathy’s palm and makes her hand difficult to clean. Kathy goes to a neurologist.
• A nerve block is used to relax the muscles that are causing the wrist and fingers to bunch up. These muscles are located in the palm side of the forearm.
• Exercises are prescribed by an occupational therapist to stretch the muscles that were tight (the same muscles that got the nerve block) and strengthen the muscles that open the fingers and lift the wrist.
• Despite a lot of effort with the occupational therapist and at home, Kathy can only open her fingers a small amount.
• Kathy’s therapist suggests she use an e-stim orthotic on her arm. The orthotic had been tried before with Kathy, but the e-stim was not strong enough to open her hand. But now the nerve block relaxed the hand enough for the e-stim orthotic to work.
• The combination of e-stim and practicing grasp and release allows Kathy to begin to open her hand on her own. Kathy notices that her “new” ability to pick up objects has helped not only her hand, but her elbow and shoulder as well.
Some doctors inject nerve blocks, but do not use any sort of intervention to build on the opportunity provided by the nerve block --- which is a mistake. Nerve blocks do not permanently eliminate spasticity. Instead, they create opportunities for spasticity to be permanently reduced. After treatment with a nerve block there should be some intervention to take advantage of the window of opportunity the drug presents.
A quick note about Botox. Some research has shown that electrical stimulation of the muscles that were injected with Botox can do two things . . .
1. Make the effect of Botox stronger, thereby requiring less medication. Botox is expensive. E-stim of muscles that are injected may require less Botox to be injected.
2. Lessen the time that injected Botox takes to “absorb” into the muscle. Without e-stim, Botox uptake is seven to ten days. With e-stim, Botox uptake is approximately two days.
So, direct e-stim to the target muscles will decrease the amount of Botox needed and increase the window of opportunity that the drug provides. This is something that requires a medical doctor to approve.
Here is a partial list of therapies that may be effective in conjunction with nerve blocks:
• Virtual reality
• Repetitive practice
• Modified and classic constraint-induced therapy (mCIT, CIT)
• Cyclic electrical stimulation
• Electromyography-based electrical stimulation with biofeedback (e.g., Mentamove, Neuromove™)
• Stretching programs aimed at the muscles treated
• Traditional occupational and physical therapy (which may include any or all of the therapies in this list)
There are two other treatment options for people with spasticity. One affects spasticity directly, and one affects the symptoms of spasticity:
• Affecting spasticity directly: Dorsal root rhizotomy (DR) or a selective dorsal rhizotomy is appropriate for people with profound spasticity. Spasticity can cause extreme pain, skin breakdown (bedsores), hygiene issues, contractures, and so on. A patient can experience all these, and have cognitive impairment. For this sort of patient, DR is a humane and reasonable option. DR involves the selective surgical severing of parts of the nerves that enter the spinal cord. These are the nerves that send messages from the muscle to the spinal cord. When these are cut spasticity is reduced or eliminated. DR has an upside and a downside. The upside is that it reduces or eliminates spasticity permanently. The downside is that it’s not reversible, and it eliminates or reduces sensation from the corresponding nerves. So if a DR is done to the nerves that represent the upper extremity, the patient would have diminished or absence of sensation from that extremity. This may be a reasonable trade-off for some patients with severe spasticity, especially those patients who are cognitively impaired.
• Affecting the symptoms of spasticity: Serial casting (SC) is a process where a cast is used to hold the joint in a particular position. The cast is applied, removed, and then reapplied (typically) every one or two weeks. Each cast more aggressively stretches the target muscles toward a more functional position. SC holds the muscle in a stretched position for long periods of time. SC is the only way that is clinically proven to increase the length of spastic muscles. SC is sometimes used together with nerve blocks.
What Precautions Should Be Taken?
Doctors, usually physiatrists or neurologists, will decide if you are an appropriate candidate for Botox treatment. After Botox is administered, adjunctive therapy can help foster the muscle relaxation that this treatment provides. Recovery options that involve electrical stimulation have contraindications and precautions. Discuss these with your medical doctor.