![]()
![]()
![]()
![]()
![]()
![]()
![]()
A common concern of many women when deciding on surgical treatment for breast cancer is their appearance after surgery. This is especially true of women considering a mastectomy. While you’re gathering information about your treatment options, you may also want to gather information on breast reconstruction.
Some women choose not to have any reconstructive surgery after mastectomy. That’s OK. Such a decision is perfectly acceptable. In addition, some women decide not to wear an external prosthesis, an artificial breast that’s worn in your bra. Many women who take this route are content with this choice.
For women who do choose reconstructive surgery, there are several options available to consider. Breast reconstruction is a surgical procedure designed to restore a more naturally shaped breast mound after mastectomy. Reconstructive surgery, which is generally performed by a plastic surgeon may require a longer recovery than does mastectomy alone. At the same time, some women find reconstructive surgery easier to tolerate than a mastectomy alone because they feel it improves their body image.
Reconstruction may be performed at the same time as a mastectomy (immediate reconstruction), or it can be done later (delayed reconstruction). In general, immediate reconstruction brings the most favorable cosmetic results. In addition, some women feel much better when they wake up from a mastectomy with a reconstructed breast. With immediate reconstruction, a plastic surgeon typically works in tandem with the surgical oncologist who performs the mastectomy.
An important consideration in deciding whether to have immediate or delayed reconstruction is whether you may need radiation therapy to treat your breast cancer. If you may need radiation, you should discuss your reconstruction options with your surgeon before your surgery.
Among women with large tumors and those whose cancer has spread to the underarm (axillary) lymph nodes, radiation therapy is often recommended after mastectomy. Because it can take a day or two after a mastectomy before doctors have a definitive answer as to whether the cancer has spread to the lymph nodes, you may not know before your surgery whether you’ll need radiation. For this reason, immediate reconstruction often isn’t an option.
As for chemotherapy, you can receive it after immediate breast reconstruction, but you’ll need to wait about two to three weeks after your surgery before you can begin treatments. Your surgeon and oncologist will decide when the time is right to begin chemotherapy after surgery.
With delayed breast reconstruction, surgeons generally recommend that you wait several months after completing radiation therapy and chemotherapy before having reconstructive surgery to allow time for healing from your treatment.
![]()
QUESTION & ANSWER
Q: Does breast reconstruction make it more difficult to detect a cancer recurrence?
A: With very rare exceptions, the answer to this question is a strong No. This is because the most likely site for recurrence is in the tissue located just underneath the skin (subcutaneous tissue). During reconstruction, the artificial breast mound is placed deep below the subcutaneous tissue, which pushes the subcutaneous tissue upward and closer to the surface. Therefore, recurrent tumors can still be felt during a self-examination or clinical breast examination.
If you decide to have breast reconstruction, you have three options to consider:
Keep in mind that reconstruction may require multiple surgical procedures. Usually, at least two surgeries are required to achieve a correctly positioned and symmetrical breast mound. Some women also undergo areola and nipple reconstruction. In addition, before surgery, steps must be taken to stretch the remaining chest skin so that it can accommodate an implant, a process called tissue expansion.
If you want both of your breasts — your reconstructed breast and your healthy breast — to have a similar size and shape, you might consider surgery on both of your breasts. When breast reconstruction is performed on just one breast, there may be a difference in size and shape compared to your natural, healthy breast. In addition, over time, your reconstructed breast and your natural breast may change in slightly different ways, and they may end up looking even more different from one another.
Tissue expansion before an implant
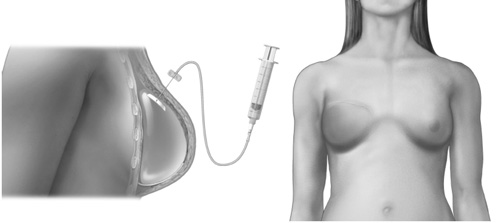
During tissue expansion, a temporary implant (tissue expander) is placed under the chest muscle and gradually filled with saline to stretch the chest muscle and skin to allow for a larger permanent breast implant later.
Tissue expanders
Most women aren’t able to simply have an implant placed in their chest wall at the time of a mastectomy. First, they need to undergo a process called tissue expansion to stretch the remaining chest skin to accommodate the implant. The process begins with the insertion of a temporary implant called a tissue expander. The implant can be surgically placed at the time of your mastectomy, or later if you choose to have delayed breast reconstruction. The tissue expander is placed under your chest muscle and skin.
During a series of regular office visits over the next few months, your surgeon or a member of his or her staff will inject sterile saline into your tissue expander to slowly stretch your chest muscle and skin. The filling is done gradually to give the skin covering the implant a chance to stretch between visits.
A few months after the tissue expansion is complete, you’ll need a second surgery in which the tissue expander is removed and replaced with a permanent breast implant. The permanent implant may be filled with either saline or silicone gel. Your surgeon will discuss these options with you.
Pedicle TRAM flap surgery
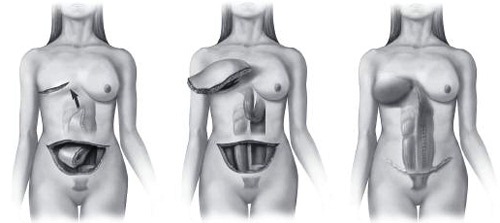
With pedicle TRAM flap surgery, a section of skin, muscle, fat and blood vessels is taken from a woman’s abdomen, tunneled underneath the skin, and used to create a new breast mound.
Free TRAM flap surgery
During a free TRAM flap procedure, a surgeon disconnects a section of abdominal tissue — including skin, fat and sometimes muscle — and reattaches the tissue to the chest area, using microsurgical techniques.
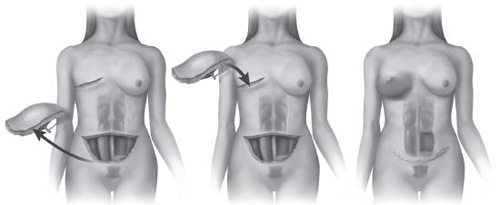
Latissimus flap surgery

Latissimus flap surgery is performed in much the same way as is TRAM flap surgery, but the section of tissue used to create a new breast mound comes from the back instead of the abdomen.
Implants
An implant is a breast-shaped device that’s placed under the pectoral muscles of the chest wall. This technique may be performed in slender, smaller breasted women who don’t have a lot of excess tissue in their abdomens or other parts of their bodies that could be used for autologous breast reconstruction.
The two kinds of implants are saline and silicone. In the 1990s, there were some major concerns regarding silicone implants. At issue was whether the implants caused other health problems. Today, as a result of additional research, these concerns have largely been laid to rest. An advantage of silicone implants, and why they’re often used in breast reconstruction, is that they feel more like breast tissue than do saline implants.
An implant may be put in place at the time of the mastectomy or during a later surgery. Implants may cause pain, swelling, bruising, tenderness or infection. There’s also a possibility of rupture, deflation and shifting. Another possible complication of implants is capsular contracture, a condition in which tight scar tissue forms around the implant. This causes the breast mound to become excessively firm so that it no longer has the feel of breast tissue. Sometimes, a capsular contracture can cause discomfort. Whether to surgically correct a contracture is an individual decision, often based on the severity of the symptoms.
If you’ve had radiation therapy or complications such as a blood clot or infection, you may be at a higher risk of capsular contraction. Your plastic surgeon may recommend that you consider another reconstructive option.
A nipple also can be reconstructed using skin from the new breast mound. This is generally done after the reconstructed breast has time to heal and settle. Later, a tattoo may be applied to color the nipple and create an areola.
The entire process takes about four to six months, sometimes longer depending on other treatments you may need.
Tissue flaps
A more complex reconstructive procedure involves using a woman’s own tissue. In this type of reconstruction, a section of skin, fat and muscle, along with blood vessels, is taken from one part of the body and moved to the chest to form a breast mound.
Women who choose tissue flaps generally like the idea of using their own tissue to reconstruct their breast. For women who undergo radiation, it also may be the only reconstructive option available. After radiation, it’s often difficult to stretch the skin enough to place an implant.
Most often, the tissue is taken from the lower abdomen. This is called a TRAM flap. TRAM stands for transverse rectus abdominis myocutaneous. The rectus abdominis muscle is the “six pack” muscle in the abdomen.
There are two main types of TRAM flap procedures that may be used to reconstruct a breast: the pedicle flap and the free flap. With the pedicle TRAM flap, a surgeon takes the rectus abdominis muscle completely, along with the overlying fat and skin from your abdomen, to construct your new breast. The flap is tunneled under the skin to the chest area, where it’s brought through the mastectomy incision.
With the free flap procedure, a surgeon takes only part of the rectus abdominis, along with skin and fat from your abdomen and reattaches the tissue to blood vessels in the chest wall using microsurgical techniques. This is called a muscle-sparing TRAM flap because most of the rectus abdominis muscle is left untouched.
Some women undergo what’s called a DIEP flap. In this procedure a surgeon takes only the skin and fat from the abdomen to make a new breast. The DIEP flap is appropriate only in some women and is dependent on the size of the abdominal blood vessels.
For women who don’t have enough tissue available on their abdomens for this procedure, the tissue may be taken from the back. This is called a latissimus flap, from the Latin word for the muscle that’s involved in the procedure. The flap is moved to the chest site in the same manner as is done with the pedicle TRAM flap.
In most women, the latissimus flap is too thin to create a natural sized breast. A tissue expander or a breast implant is placed under the flap to create the breast mound. If a tissue expander is used, a second surgery will be necessary to replace the expander with a permanent implant.
In some instances, neither the abdomen nor the back has sufficient extra tissue from which to take a flap. In this case, the tissue may be taken from the buttocks or the inner thigh.
The main advantage of flap reconstruction is that the reconstructed breast mound is made from your own tissue. The mound remains quite soft and, unlike with an implant, contracture doesn’t occur. In addition, if the tissue is taken from the abdomen, you get a tummy tuck. However, because the flap is human tissue, it requires an adequate blood supply. If blood supply to the flap is poor, the tissue may not survive. This may lead to significant complications and an unsatisfactory result.
Once the reconstructed breast mound has healed, a nipple may be formed using skin from the new breast mound, and a tattoo may be applied to color the nipple and create an areola.
In some instances, tissue flap surgery isn’t an option. If you smoke, your doctor may recommend against it because smoking can impair the circulation to the transferred tissue. An abdominal flap may not be an option if you’ve had previous abdominal surgery.
Nipple reconstruction
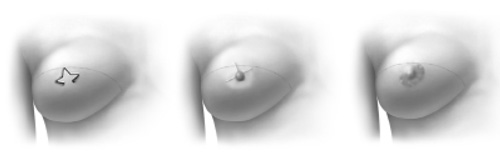
After a reconstructed breast has healed, a plastic surgeon can reconstruct a new nipple and areola.
≈≈≈≈≈≈≈
People have many misconceptions about breast reconstruction. It’s important to approach the procedure with realistic expectations and to ask questions.
What breast reconstruction can do:
What breast reconstruction may do:
What breast reconstruction doesn’t do:
≈≈≈≈≈≈≈
Prosthetics
Some women choose a prosthesis over reconstructive surgery. A prosthesis is a device that’s shaped like a breast and worn in your bra. It’s usually made from nylon, rubber, silicone or Dacron fiberfill, and you slip it into a specially designed bra. Immediately after your surgery, you may select from prostheses in a range of shapes and sizes that can be used temporarily. For long-term use, you may want to consider getting a more customized, permanent prosthesis.
Check with your insurance company to see if your insurance will pay for a prosthesis. Sometimes, having a prescription for a prosthesis from a doctor can help with insurance coverage.
≈≈≈≈≈≈≈
As you think about reconstruction, here are some suggestions to help you in the decision-making process:
≈≈≈≈≈≈≈
In making your decision on whether to have breast reconstruction, or what type of reconstruction to have, consider these issues:
If you have questions regarding reconstruction, be sure to consult your doctor or a plastic surgeon. He or she can usually help clarify the issues for you.