CHAPTER 4
The Brain: Target Organ of Addiction
In this chapter, I explain how and why the brain can become addicted to feeling pleasure, even when that pleasure can be detrimental to the life of the addicted person.
Because of the rapid progress in brain research during the 1980s, and in anticipation of accelerating progress to come, the U.S. Senate and House of Representatives in the summer of 1989 passed a Joint Resolution declaring the period of 1990 to 2000 as the Decade of the Brain. Shortly thereafter, President George Bush signed a proclamation ratifying this designation.
One of the most promising aspects of the new brain research is the study of addiction. To understand how drugs work in the brain is to understand how the brain works. Drugs of abuse, as well as brain-altering medicines, produce their effects by traveling through the bloodstream to the brain, where they enter the brain cells. Each drug or medicine modifies the function of specific brain cells in unique ways. Nonmedical drug use distorts healthy brain functions, impairing the workings of the marvelous and fragile brain. A clear and sober brain thinks best. A brain high on alcohol and other drugs is a brain that is dysfunctional. Many of the ill effects of drug abuse on the brain persist, in some cases for a lifetime.
In the last three decades, the United States has invested billions of dollars in the fight against illegal drugs. Most of the money has gone to law enforcement and treatment, but hundreds of millions of dollars have been spent on research aimed at understanding how drugs work, from the physiology of the brain to the sociology of addiction. The study of abused drugs enhances the understanding of how useful medicines, such as antianxiety and antidepressant medicines, work. Painkillers, such as morphine, are a great blessing when used in medical treatment, but when used illicitly, they are a plague, showing that the way a drug is used is as important as its biology.
The human brain is a three-pound gelatinous gray mass covered with deep wrinkles and connected to the rest of the body through the spinal cord and stringlike nerves that extend in an intricate web to every part of the body. Brain cells operate in a chemical bath maintained by the blood passing through and around them. Because the brain is exquisitely vulnerable to changes in this bath, the blood is separated from the brain by the blood-brain barrier, a filtering system that limits the movement of chemicals from the blood vessels into the brain.
The brain’s principal fuels are oxygen, taken from the air by the lungs, and glucose, the sugar used by all of life as the most basic currency of energy, which comes from the food we eat. If the brain’s supply of either oxygen or glucose is interrupted, even for a few seconds, consciousness is lost and in a few minutes the brain dies. Unlike other parts of the body, the brain does not regrow after injury. No other organ in the body is as sensitive to such brief interruptions in the supply of fuel. In addition to oxygen and glucose, some other chemicals pass from the blood to the brain through the blood-brain barrier, including abused drugs.
The brain produces neurotransmitters that affect adjacent nerve cells, and neurohormones that enter the blood supply and affect distant parts of the brain and other parts of the body. The brain is closely linked with the endocrine system, which produces hormones that control most bodily functions, and with the immune system, which protects the body against infection. The three integrated systems—the nervous, endocrine, and immune systems—are the principal guardians of the body’s well-being and its ability to adapt to changing internal and external environments.
The Neuron—The Basic Cell of the Brain
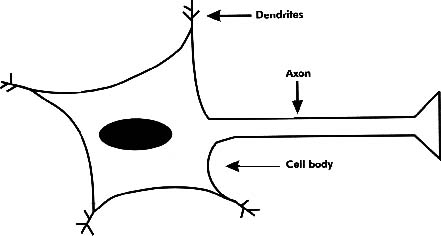
The brain, the organ of the mind, is composed of billions of cells. Neuroscientists believe that in a single human brain there are between 100 billion and 1 trillion neurons, the fundamental cells in the brain, which were discovered just 100 years ago. The neuron is the fundamental building block of the network of nervous tissue in the brain and the nerves. It has three major parts: the cell body, the axon, and the dendrites (see Figure 4–1). The cell body contains genetic information in its nucleus as well as the metabolic engine for the neuron. The axon is the extension of the neuron that reaches out to make contact with other neurons to send messages. The dendrites are extensions of the neuron that receive messages from other nerve cells.
Figure 4–1
The neuron.
Chemical Messengers
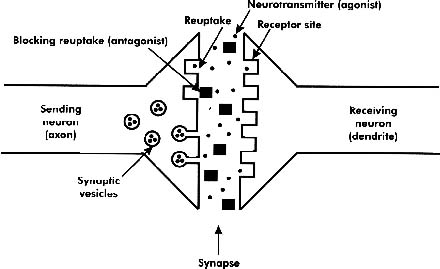
Neurons send messages to each other across a minute space between the sending axon and the receiving dendrite. This tiny space is the synapse. When a message leaves a neuron, the swelling at the end of the axon releases chemicals into the synapse. These chemicals are stored in the axon in packets, called synaptic vesicles. For a signal to pass from one neuron to another in the brain, the sending axon must release chemicals into the synapse and the receiving dendrite must receive these specific neurotransmitters. The nerve impulse, received from another neuron, is sent along the dendrite through the cell body to the axon on to the next neuron in a continuous integrated electrochemical flow of messages. The neurons conserve energy by recycling the neurotransmitters released by their axons into the synapses. The neurotransmitters, having sent their messages, are taken back (reuptake) into the axon to be recycled again and again (see Figure 4–2).
Figure 4–2
Synaptic transmission.
Locks and Keys
A message can be sent only if the axon’s neurotransmitter fits into the highly specific receptor site on the dendrite as a key fits into a lock. The neurotransmitters are keys. The locks, called receptor sites, are on the dendrites of the message-receiving nerve cells. The identification of this lock-and-key relationship, unique for each separate neurotransmitter in the brain, has been the central discovery of neuroscience over the last two decades. The study of drug abuse has played an important role in this rapidly evolving science. Most drugs produce their effects by influencing specific lock-and-key complexes in the brain’s synapses.
Each neurotransmitter in the brain is associated with specific brain areas or brain functions. Some neurotransmitters are relatively widespread in the brain, and others are more localized. Most synapses contain more than one neurotransmitter (key) and more than one type of receptor site (lock). The message is transmitted from the receiving dendrite through the nerve cell body to the sending axon as an electrochemical impulse that depends on the integrity of the entire nerve cell. Drugs that interfere with the cell membrane, as PCP, alcohol, and inhalants do, influence nerve cell transmission by a mechanism separate from drugs that affect the synapse.
Nerve cells have many, often subtle, influences on each other in complex networks, with some cells modifying the transmission from one neuron to another. Neurons primarily serve either excitatory or inhibitory roles in the brain. Drugs of abuse fit both categories. Some, called stimulants, such as amphetamines and cocaine, are primarily excitatory, whereas others, called depresssants, such as alcohol and the opiates, are primarily inhibitory. Reward, or pleasure, can be found by drug abusers from both stimulation and inhibition of particular groups of neurons in the brain.
The nervous system works as a balance of inhibitory and stimulant forces. Stimulating one side of the balance has a similar effect to inhibiting the other side. When it comes to drug abuse, the brain acts as if it seeks change, since many changes in feeling are experienced as desirable by drug abusers. Nonabusers of drugs do not like these changes of feeling. For example, the feeling of being drunk is attractive to alcohol abusers, but most people find it intensely unpleasant. Cigarette smoke makes nonsmokers sick, but smokers pay billions of dollars a year for the feelings nicotine produces.
Local and Long-Distance Messengers
Neurotransmitters work in the synapse in which they are produced. The brain also manufactures chemicals that carry messages to remote parts of the brain or to other parts of the body. Neurotransmitters are local messengers, moving across a single synapse to produce their effects. Hormones are long-distance messengers that are carried by the blood to act at distant sites in the body on organs other than the brain. The midbrain controls the functioning of the pituitary gland, the master gland located in the center of the head at the base of the brain. Hormones are sent out from the pituitary gland to manage vital body functions such as metabolism, sex, and reactions to stress through their effects on the thyroid, sex, and adrenal glands. This complex in the center of the brain is where pleasure and pain are handled, where hormones are managed by the pituitary gland, and where the brain controls all behavior. This is the final common pathway for all drugs of abuse.
Neurotransmitters are called agonists because they activate transmission across the synapse. The effects of specific neurotransmitters are blocked by equally specific antagonists, chemicals that block the receptor sites on the dendrites (see Figure 4–2). When the receptor site is occupied by an antagonist, the agonist (the external chemical stimulus or natural neurotransmitter activating that receptor site) cannot cause the nerve cell to transmit a message. Antagonists block the lock in the receiving dendrite, preventing the sending nerve cell’s messenger, the neurotransmitter, from producing an effect. Scientists now use hundreds of agonists and antagonists, introduced into the blood or directly into specific parts of the brain, to study the brain in both health and disease.
Tolerance and Dependence
When a particular neurotransmitter system is excessively stimulated over a long period, the brain partially reestablishes an equilibrium by reducing the sensitivity of the particular neuroreceptors or by decreasing the number of these specific neuroreceptors. This is called down-regulation. There are limits to this process of adaptation, which is one mechanism of tolerance. This means that the more the brain is exposed to a chemical affecting a neurotransmitter over time, the less the brain responds to a particular dose of that chemical. Cigarette smokers do not commonly smoke more than forty cigarettes (two packs) a day, and alcoholics seldom drink more than about ten ounces of pure alcohol (eighteen beers or a fifth of distilled liquor) a day, no matter how long they use these substances. The fact that people who are addicted to alcohol and other drugs do not use even more of these substances over time demonstrates the limits of drug tolerance.
Most nonusers are impressed by how much drug use tolerance permits. They cannot imagine liking the feelings produced by smoking forty cigarettes a day or drinking twenty-six ounces of vodka a day. Tolerance is one of the most obvious effects of abused drugs. Addicted people use a lot more of a drug than do nondependent people, if nondependent people use it at all.
The other commonly observed effect of abused drugs is physical dependence. After everyday use of a drug for prolonged periods of time, when the drug use is abruptly stopped (sometimes called stopping “cold turkey” because “goose bumps” is a common symptom of withdrawal), there are withdrawal symptoms reflecting physical dependence. Both tolerance and physical dependence are caused by the brain becoming adapted to the regular presence of a chemical. Even though these two phenomena are apparent for many abused drugs, they are not the critical elements of the experience of addiction as is commonly thought. Both tolerance and physical dependence occur in response to most chemicals that affect the brain, whether they produce addiction or not. They reflect the brain’s adaptation to a new chemical environment, one that includes the continuous presence, often at a high concentration, of a particular chemical. This traditional pharmacological definition of physical dependence is quite different from the use of the word dependence in the context of addiction. The narrower and older definition of dependence means that when the substance is removed, the user experiences withdrawal symptoms. The broader and newer definition of addiction reflects the fact that addicts depend on the use of self-destructive, pleasure-causing drugs to conduct their lives. Tolerance and withdrawal symptoms are not necessary for addiction to occur, although they sometimes occur in people who are addicted to alcohol and other drugs.
In this book, the distinction between physical dependence and addiction is made by using the term physical dependence for the narrower and older definition and addiction for the broader and newer definition. Physical dependence is the simple cellular adaptation of the body, especially the neurons in the brain, to the continued presence of a chemical that influences the function of the brain. In contrast, addiction is a complex, lifelong disease of the entire self.
This simplified explanation of how neurons work in the brain focuses on the synapse, the tiny but continuously active space between two neurons, one sending signals and the other receiving them. The activity in the synapse is affected by both abused drugs and psychoactive medicines. These chemicals enter the bloodstream, pass the blood-brain barrier, and become part of the chemical bath reaching all the synapses in the brain. Drugs influence a synapse in many ways. Psychoactive externally supplied chemicals facilitate or inhibit transmission between particular groups of axons and dendrites. Some chemicals act by blocking the reuptake or recycling of chemical messengers (neurotransmitters) from the synapse back to the sending axon. This is called reuptake inhibition. It facilitates transmission by prolonging the period the neurotransmitter stays in the synapse. Other drugs directly mimic neurotransmitters. They are agonists sending messages by themselves, fitting the lock on the dendrite in the synapse. Some drugs act as antagonists, blocking the effects of natural neurotransmitters or drug agonists. Many abused drugs produce their effects by more than one mechanism.
The Structure of the Brain
There are billions of neurons in the brain, which are interconnected in vast, continuously interactive networks. Although most neurons have only one axon, usually a relatively long extension of the cell, a single neuron may have as many as 10,000 dendrites. The dendrites of a single neuron can receive signals from the axons of thousands of different neurons. In the brain of a single person there are over 1 quadrillion synapses, more than the total number of humans who have lived since the brain evolved to its present form about 100,000 years ago. There are more different ways neurons can be linked through their synapses in a single human brain than there are atoms in the entire universe. Even in sleep the brain remains intensely active. Think for a moment about the complexity of this natural biological system, the human brain. It is not difficult to see why even today, with highly developed scientific techniques, the brain, especially the human brain, is the most challenging frontier of modern biology.
Glia—The Other Brain Cells
Neurons are not the only cells in the brain. The glia are even more numerous in the brain than the neurons. One kind of glia cell, the oligodendrocytes, are wrapped around the axon, providing a protective, insulating fatty sheath called myelin. When this protective sheath is lost, as in demyelinating diseases such as multiple sclerosis, nerve transmission is disrupted.
The astrocytes are the other major type of glia. These cells are essential to maintaining the blood-brain barrier that protects the neurons from disruption by many chemicals circulating in the blood. The glia also form the architecture or the structure of the brain. They are essential to the functioning of the neurons. Because the membranes that compose the blood-brain barrier are fatty substances, chemicals that dissolve easily in fat most easily pass through these membranes from the blood to the brain. Most substances eaten and taken into the blood are water soluble, and not fat soluble, so these chemicals do not reach the brain.
The kidney excretes water-soluble wastes from the blood. One key function of the liver is to modify fat-soluble chemicals to make them water soluble so that the kidney can excrete them more easily. This process of chemical breakdown is called metabolism, and the breakdown products are called metabolites. The delta-9-tetra-hydrocannabinol (THC) in marijuana smoke is a good example of a fat-soluble abused drug. Alcohol is an unusual chemical because it is highly soluble in both water and fat.
Gray Matter, White Matter, and Dark Spots
Many neuron cell bodies, often dark gray, are located on the brain surface, making up the gray matter. The axons of these neurons, covered by white myelin, extend in pathways to connect with other groups of neurons throughout the central nervous system. These interlacing pathways are the white matter underlying the covering gray matter of the brain. The white pathways connect with other groups of gray cell bodies in various parts of the brain. Each of these separate collections of neuron cell bodies, dark spots in the white matter of the brain, fulfills a specific role.
The cerebellum at the back of the brain manages the body’s movement and equilibrium, whereas the gray matter above the temples manages most voluntary muscle movement and speech. The central part of the brain has several areas with many cell bodies, or nuclei, managing the response to stress and pain and the experience of pleasure. These central gray areas are closely connected to the endocrine and immune systems.
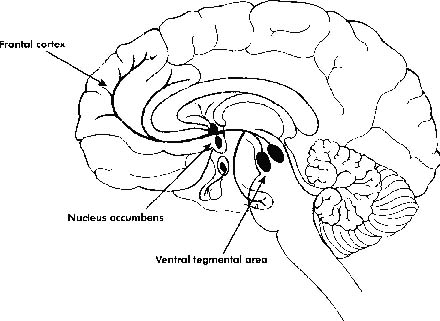
Specific nuclei in the brain and their principal pathways are often served primarily by specific neurotransmitters. For example, the neurotransmitter dopamine is particularly important in the production of pleasure, including feeling high from nonmedical drug use. Central gray areas at the base of the brain that manage the experience of pleasure are the nucleus accumbens and the ventral tegmental area. They are connected by pathways responding to the neurotransmitter dopamine. The pleasure centers are closely connected to the pathways and the nuclei that manage pain, memory, and emotions as well as appetite, sex, fear, and anger. They are part of the brain’s control center for behavior, so they are connected to the centers that manage movement and to the frontal cortex, the part of the brain that manages conscious thoughts (see Figure 4–3).
The brain areas that control pleasure, a major focus of this book, are the locations of the brain mechanisms of addiction. Addiction, and other behaviors associated with appetites (such as feeding and sexual behavior), are primarily associated with the limbic system, the neuron network in the brain that manages feelings and emotions.
Figure 4–3
A cross section of the human brain showing the projection from the ventral tegmental area (in the midbrain) to the nucleus accumbens and the frontal cortex. Addictive drugs produce their rewarding actions by increasing dopamine in the nucleus accumbens and ventral tegmental area.
Neurochemistry
The first neurotransmitter was identified only forty years ago. Today, scientists have identified over sixty neurotransmitters and speculate that there are 300 or more naturally occurring chemicals that are used by the neurons to send messages from one neuron to another. The first specific receptor identified was the opioid receptor discovered in 1972. Shortly thereafter the benzodiazepine receptor, the target of medicines such as Valium (diazepam) and Xanax (alprazolam), was identified. Brain cells are affected by everything that happens to the body: actions, thoughts, experiences, and the fabulous range of chemicals in the blood as well as the chemicals produced by the brain itself.
Three Neurotransmitters
This review focuses on three of the relatively well-understood neurotransmitters, each of which has an important role in drug abuse: norepinephrine (NE), dopamine (DA), and the endorphins.
The catecholamines are a family of related chemicals based on the amino acid tyrosine, one of the fundamental building blocks of proteins. NE and DA, members of the catecholamine family, are major brain neurotransmitters. DA plays a role in the control of appetite and pleasure, including eating and sex. DA is the chemical that brings gusto to the brain. DA blockers are useful medicines in the treatment of schizophrenia, a major mental illness thought to be the result of excessive DA in certain brain areas. Parkinson’s disease is associated with depletion of DA in the midbrain nucleus that controls fine movements and muscle tone. General DA depletion throughout the brain contributes to severe depression. Notice the range of brain activities associated with this single neurotransmitter, DA, from parkinsonism to schizophrenia and from depression to drug abuse.
Norepinephrine and Fear
NE is the neurotransmitter that governs the sympathetic nervous system, which is composed of the nerves that are not subject to voluntary control. These nerves manage the “flight-or-fight” response associated with the feelings of fear and anger. Fear stimulates the sympathetic nervous system as seen in increased heart rate, elevated blood pressure, and shutting down of the blood supply to the intestines so that blood flows to the muscles preparing for emergency action.
The NE neurotransmitter system that controls the sympathetic nervous system is found in all parts of the brain but in only 1% of the brain’s synapses. More than half of the NE system is concentrated in two small areas associated with the alarm function of the brain, including the locus coeruleus, the central gray matter associated with panic attacks in agoraphobia. Some antidepressant medicines influence the NE system, with some of these medicines blocking the reuptake of NE in the synapse. These medicines also block the panic attacks associated with agoraphobia. Because depression is associated with NE deficiency, some chemicals that raise the level of NE in the synapse are effective antidepressants.
The Punch of Dopamine
Chemicals that influence the DA neurotransmitter system not surprisingly have many brain effects. Each chemical that affects the DA system does so in unique ways. For example, although cocaine and Thorazine (chlorpromazine), a medicine used to treat schizophrenia, both affect the brain’s DA system, they do so in entirely different ways. Cocaine, which raises DA levels in the synapse, usually makes the symptoms of schizophrenia worse. Thorazine, which reduces DA, is not a substitute for cocaine in the lives of drug abusers, and they, like most other people, find the drug unpleasant. On the other hand, schizophrenic people, thought to suffer from DA excess, are seldom happy people. This observation highlights the important point that the DA system is not simple or uniform; it is made up of a wide range of subsystems of neurotransmitters and neuroreceptors. For this same reason, although most antianxiety medicines affect a single receptor complex, these medicines are not interchangeable, any more than painkillers or antidepressants are interchangeable, even though many of them affect the same basic receptor complexes in the brain.
Endorphins—Nature’s Heroin
The third highlighted neurotransmitter is different from the closely related NE and DA, both of which are small chemicals called amines. In the 1970s, as scientists sought to understand how heroin, the model abused drug, affected the brain, they discovered the specific brain receptor for morphine, the core of the heroin molecule. Having found the opiate receptor lock in the brain, they searched for the natural neurotransmitter key that fits this lock in the synapses of the pleasure centers in the brain and elsewhere in the body. This neurotransmitter turned out to be not a simple chemical, like NE and DA, but a series of relatively long chains of protein building blocks, or peptides. This family of natural neurotransmitters is now known collectively as endogenous opioid peptides, or endorphins.
The three broad classes of endorphins are the brain’s own morphinelike substances, the natural neurotransmitters that fit the receptor lock that morphine fits. The endorphin brain system moderates pain, promotes pleasure, and manages reactions to stress. Today more than a dozen natural endorphins are known, and at least five different types of opioid receptors have been identified in the mammalian brain. Scientists have recently discovered additional neuropeptides that are also neurotransmitters, some of which do not involve the opioid receptors. Endorphins act not only as neurotransmitters but also as neurohormones (affecting nerve functioning at more distant brain sites to which they are carried by the blood) and as neuromodulators (natural chemicals modifying the workings of other neurotransmitters).
Endorphin receptors are found not only in the brain but in other parts of the body as well. This helps to explain why, although drugs of abuse are used by addicts for their effects on the pleasure centers of the brain, these drugs also affect many other parts of the body. Opioid receptors are prominent in the intestine, so that opiates not only cause addiction but also cause the gut to become quiet. For this reason, opioid drugs are used in the treatment of diarrhea as well as in the treatment of severe pain.
Drugs and the Brain
The effects of chemicals on the brain are determined by how much of the chemical reaches the brain. This is called the dose response. At very low levels of any drug there is no brain response. As the level of the chemical rises, the brain’s responses not only increase but change, so that low levels of a drug produce one response and high levels produce different responses. The brain, continuously active and functioning as a single integrated unit, is influenced by all of the chemicals taken into the body that pass the blood-brain barrier. The rapidly changing concentrations of drug chemicals in the synapse are governed by the chemicals’ concentration in the blood and by the body’s ability to metabolize and eliminate them.
Roadways to the Brain
Drug users take drugs by one of several routes of administration. These routes include entry through the gastrointestinal tract for drugs taken by mouth and through the lungs for smoked drugs. Drugs can be injected with a hypodermic needle under the skin or directly into the bloodstream. A few drugs, such as cocaine, can be absorbed through the nasal membranes directly into the blood, a route of administration that is similar to injection under the skin but that does not require a needle and syringe. When drugs enter the body by smoking, they reach the brain within eight seconds without first passing through the liver. This route of administration produces effects that are similar to injection of drugs into the vein (intravenous use), which produces initial brain effects in about sixteen seconds.
The most intensely rewarding drug experience comes when the brain is hit by a high and rapidly rising level of drug chemicals. When chemicals are used for medical reasons—not to get high—they are usually taken orally to avoid the rapid rise and fall of blood levels that drug abusers avidly seek. A few medical psychoactive chemicals are taken by injection rather than by mouth, because these particular medicines are not absorbed efficiently from the gastrointestinal tract or are quickly metabolized by the liver. With few exceptions, psychoactive medicines, unlike abused drugs, are taken by mouth. When brain-affecting medicines are injected in medical treatments, they are injected into muscles or under the skin. When drug abusers inject drugs they inject into the vein.
Most psychoactive nonmedical drug use is by intravenous injection or smoking to get the most rapid rise to the highest level of the drug in the brain. This rapid rise is highly reinforcing because it is particularly effective in stimulating the brain’s pleasure centers. This is why smoking and intravenous injection are the routes of administration chosen by addicted people and why these routes of administration are so much more addicting than is oral use of the same drug.
Alcohol: An Unusual Drug
Alcohol at first appears to be an exception to the general rule that addicted people take drugs by smoking or injection. A closer look at drinking suggests this exception is more apparent than real. Nonalcoholic drinkers consume low doses of alcohol, often with food, which slows the absorption of the alcohol out of the intestines and into the bloodstream. This pattern of drinking produces a relatively slow rise to low brain levels of alcohol. Nonalcoholic drinkers purposefully consume alcohol in ways that avoid the “buzz” of rapid rises to high levels of alcohol in their blood. Alcoholics, in contrast, consume large amounts of alcohol on an empty stomach, drinking fast to achieve the rapidly rising, high brain levels typically sought by addicted people. The faster the rise of drugs in the blood, and the consequent rise of drugs in the brain, the more reinforcing is the drug use. Alcohol is unique because it is quickly and completely absorbed from the gastrointestinal tract, rapidly passing the blood-brain barrier. Even when taken by mouth, alcohol is relatively fast-acting, especially when taken on an empty stomach, compared with other orally consumed brain-affecting chemicals.
Searching for the Root of Addiction
Addiction to alcohol and other drugs involves the use of a drug nonmedically in such a way as to produce a high, leading to loss of control and denial. Alcoholics and drug addicts use “alcoholically” or “addictively,” meaning that they use alcohol and other drugs in the ways that lovers behave: recklessly, irrationally, and impulsively. Often when people think about the roots of addiction they think of social or economic factors such as race or income, but the root of addiction lies far deeper than demographic characteristics. The root of addiction is in the human brain.
In the 1950s, Robert Heath, a brilliant researcher at Tulane University, sought to understand the brain mechanisms underlying the commonly observed lethargy of many people with chronic schizophrenia. He implanted electrodes into the brains of disturbed patients. To his surprise, he found that patients reported feelings of pleasure following stimulation of certain clusters of neurons at the base of the brain. This finding was particularly remarkable because the brain itself has no sensory nerve endings and cannot feel in the way other parts of the body do. Nonschizophrenic people reported the same experiences when stimulated in these specific brain areas, which led Heath to shift his study to brain-stimulated pleasure rather than schizophrenia.
Shortly thereafter, other researchers found that centers in the brain, located close to these pleasure centers, produced sensations of intense pain. When the pain centers, also deep in the midbrain, were stimulated by electrodes, experimental animals became disturbed. They would do almost anything to avoid stimulation of these particular areas of their brains. Both the pleasure and pain centers are collections of gray matter, clumps of neuron cell bodies, at the base of the brain in the center of the head.
Two researchers in Canada, James Olds and Peter Milner, found that rats with electrodes in their brains would work hard to get electrical stimulation of their pleasure centers. They worked just as hard to avoid electrical stimulation of their closely related pain centers. The rats hooked up to the electrical stimulation pressed the bars to get pleasurable shocks to the point of exhaustion, in preference to water, food, or even sex. When these experiments were extended to human subjects, they reported that electrical stimulation of the pleasure centers not only produced good feelings but changed their moods, producing a sense of well-being and euphoria. This experimental, direct stimulation of pleasure centers in their brains also reduced the sensitivity to pain and minimized the effects of abused drugs.
Brain Research
The line of research just described confirmed the observation made over half a century earlier by Sigmund Freud that “our entire psychical activity is bent upon producing pleasure and avoiding pain.” Freud extended this observation by noting that human beings, who could think about probable consequences of their behaviors over a long period of time, did not simply act to seek immediate pleasure and avoid immediate pain but pursued long-term goals of maximizing pleasure and minimizing pain. He described this longer view as delayed gratification and attributed it to the mental mechanisms that manage human behavior, which he called the ego.
Addicts appear to be prominent exceptions to this rule. Addicted people act, with respect to their alcohol and other drug use, as if they were enslaved to immediate pleasure, despite the prospect of even catastrophic long-term negative consequences of their drug use. This finding led some Freudian psychoanalysts to describe addiction to alcohol and other drugs as an ego defect, a defect in self-care. Because addicts often lose their moral sense, psychoanalysts also described a deficit in addicts’ consciences, labeled superego defects.
Scientists today use chemical probes of the brain, rather than electrical wires as were used by Heath and Olds, to stimulate or inhibit specific brain areas. There are pleasure and pain centers in the brains of all animals, including human beings. These centers are governed by the neurotransmitters that powerfully influence behavior. All the abused drugs, working in remarkably different ways, affect the midbrain pleasure centers.
This final common pathway explains why addicts use seemingly diverse drugs. By a wide variety of separate mechanisms, all abused drugs stimulate the pleasure centers of the brain and inhibit the brain’s pain centers. It is this pleasure, and the reciprocal suppression of pain and distress, for which addicts strive. They are not too picky about the precise pharmacology of how they get this effect although, like all consumers, they are governed by habit, fashion, and price. When addicts change from one drug to another, such ordinary influences on consumer behaviors are usually the cause for the change, not pharmacology.
In the last decade, the work on the brain’s reward mechanisms has become one of the most productive areas of neurophysiological study. There are three areas of the brain with DA-containing neurons. The first brain area includes both the ventral tegmental area and the nucleus accumbens, the principal pleasure centers. The second area is the substantia nigra, the largest cluster of DA-containing neurons in the brain. The substantia nigra manages movements. Depletion of the cells in the substantia nigra produces parkinsonism, a disease associated with muscular rigidity. The third DA-containing area of the brain, the arcuate nucleus, is a major pathway to the pituitary gland and the management of the body’s hormonal balances and immune system.
The study of drugs of abuse has zeroed in on the first of these areas, the ventral tegmental area and the nucleus accumbens. These cells beat in unison, releasing DA in rhythmic pulses. Scientists have discovered that all drugs of abuse cause the neurons in this area of the brain to release relatively large amounts of DA into their synapses. Each drug of abuse does this by a different mechanism. Nicotine causes the same release of DA from the same cells of the ventral tegmental area and the nucleus accumbens as is caused by drugs as diverse as heroin, alcohol, and cocaine, although it does so by an entirely unique mechanism. More important, nicotine stimulates these cells without producing intoxication or impairment, as the drugs of abuse do.
Animal studies of brain mechanisms also have shown that if the axons connecting the ventral tegmental area with the nucleus accumbens are cut, an animal stops working to get drugs. If the animal is physically dependent on alcohol or another drug, the animal will show withdrawal symptoms, even with those particular nerve fibers cut. These experiments made clear that the animal’s drug-using behavior is shaped primarily by reward, by the release of DA in the ventral tegmental area and the nucleus accumbens, not by withdrawal symptoms, because the animals stopped using drugs when the drugs did not produce reward even though stopping the use of the drugs still caused withdrawal symptoms.
Neurophysiologists wondered if these cells were stimulated by nondrug pleasures. Three dogs with probes in their nucleus accumbens were given meat bones, one of the most intense pleasure experiences for a dog. As expected, the dogs were excited and happy, but surprisingly researchers found no release of DA in the dogs’ nucleus accumbens. Worried that they had failed to tap the correct spots in the dogs’ brains, the researchers prepared three more dogs and repeated the experiment, using all six dogs.
The scientists were even more surprised to find that after giving juicy meat bones to all six dogs, the first three dogs now showed release of DA from the nucleus accumbens, but that none of the three dogs added to the experiment did. Repeated experiments showed that there was a learning in the brain following pleasure stimulation. Only after repeating the experience of intense pleasure did these particular brain cells release DA.
The brain pleasure centers had to learn to fire in response to particular stimuli. Even more remarkable, the scientists discovered that much of the DA release occurred before the dog actually began to chew on the meaty bone. As soon as the dog knew it was getting the bone, or even anticipated getting the bone based on prior rewarding experiences, the nucleus accumbens cells released pulses of DA. These experiments showed that reward centers required training by repeated experience. They were highly influenced by anticipation. These centers in the brain were appetite centers, producing strong feelings of pleasure based on past rewarding, stimulating experiences.
This line of research is profoundly important to understanding the working of the addicted brain. The specific part of the brain that responded to all addictive behaviors was turned on by a wide variety of drugs and by many nondrug rewards. The ventral tegmental area and the nucleus accumbens required repeated experience to trigger the pulsing release of DA. The anticipation of rewarding experiences, based on prior brain stimulation, was itself powerfully rewarding. Finally, these experiments showed that reward shaped addictive behavior, not withdrawal as had long been thought based on the experience of heroin addiction.
This research explains why drug abusers easily switch from one drug to another and why withdrawal is an inconstant feature of addiction rather than a crucial aspect of addiction. The different drugs use different mechanisms to produce the same basic brain reward. Behavior is shaped by the reward of drug use, not by the pain of withdrawal symptoms. These experiments also show why addictive behavior tends to be repetitive behavior and why anticipation of pleasure (the set, or the expectation of the drug user) is such an important part of the drug experience.
This important research into the brain’s pleasure centers has not yet explained the differential risk of addiction of different people and the differential risk for particular individuals to addiction with different substances or behaviors. Some people are more likely to have food addictions; others are more likely to have alcohol or drug addictions. It is not as if a person had a single addictive risk, although some people do appear to be especially vulnerable to many addictive substances or behaviors.
Addiction reflects the DA-based pleasure/reward mechanisms of the brain as people (and other animals) repeat experiences that they find to be intensely pleasurable. There are many doors into the reward control room in the brain. Food and sex are natural doors, whereas alcohol and other drugs are chemical doors. For each person, I imagine that some particular doors to the control room are larger than are other doors. This is the reason that some people use alcohol and like it and others use alcohol and do not. The first group has big alcohol doors to their pleasure centers, and the second group has small alcohol doors. The size of each hypothetical door, and the ease with which it is opened, is partly determined by genetic factors. Groups with large doors and groups with small doors both can be addicted to alcohol use and other addicting behaviors if they repeat the experience of reward often enough.
There are some ways to stimulate this part of the brain that are relatively safe and other ways that are inherently unsafe. The environment of the person experiencing pleasure and the values of that person have a major influence on the relative risk of addiction. The substance and the route of administration play major roles in determining relative risk for drugs of abuse. Addiction to alcohol and other drugs is rooted in biology, but addiction is a uniquely human experience that involves far more than brain chemistry.
In specific synapses of the brain, scientists at last discovered the behavior control room and began to explore how it works and what goes wrong in addiction. The new neurophysiology resonated with the new clinical understanding of the experience of addiction, offering important insights for both the prevention and the treatment of addiction. This book is titled The Selfish Brain because the biology of addiction is the central reality shaping the experience of addiction. The brain says yes to pleasure/reward. That experience of pleasure is rooted in the DA-containing neurons in the brain’s ventral tegmental area and in the nucleus accumbens.
How important are the feelings produced by the brain’s DA-containing pleasure centers when it comes to everyday behavior? Sex and feeding are the models for all pleasure-driven behaviors. What happens to sexual behavior when a person feels no reward from sex? It stops. I have seen this many times in my practice of psychiatry. When a person does not feel sexual pleasure, even with an intense effort of willpower, that person’s sexual behavior stops. The same phenomenon takes place with eating. People who are profoundly depressed lose their capacity to experience pleasure. They often stop sexual behavior and eating. People who have exhausted their brain’s pleasure system by abusing drugs also reduce both sex and eating. They commonly lose the normal ability to experience pleasure from anything at all, which is one reason that chronic addicts are so miserable.
Many behaviors are driven by this same process of seeking good feelings and avoiding bad feelings. Feelings of reward not only add depth and color to life but are absolutely necessary to life itself. It is no accident that the mechanisms of reward are universal and powerful in all animal species. That is why these mechanisms are hardwired into our brains and why they are so powerful.
Reinforcement and Punishment
Not only have chemists and anatomists been active in new brain research, but psychologists have been involved as well. Addiction is more than a chemical reaction in the brain. Psychologists describe three types of behavior-affecting stimuli: positive reinforcement, negative reinforcement, and punishment. A good feeling is positive reinforcement. When a hungry laboratory rat is given a food pellet after a specific behavior, this is positive reinforcement. Relief of a painful experience is a negative reinforcement. When a painful shock is stopped by a rat pressing a bar, the rat has received a negative reinforcement. Both positive and negative reinforcement are rewarding; they lead the animal (or the human) to repeat the experience. Both positive and negative reinforcement need to be distinguished from aversive control or punishment. For example, when a rat receives a painful stimulus, such as an electrical shock after a particular behavior, this is punishment. It discourages the behavior with which it is associated.
All three behavior-shaping experiences are common for both animals and humans. They each have direct application to the experience of addiction. The pairing of pleasure and pain is mirrored in the brain’s structure. Pleasure and pain centers in the brain are closely related and generally reciprocally linked in the brain. When heroin addicts take their drug, they not only feel pleasure or euphoria but also feel a waning of whatever negative sensations they were experiencing when they took the drug. Tension and depression, as well as pain and self-doubt, are dissolved in the high of the heroin use. Many abused drugs also have important roles in medicine as painkillers. Medicines used to treat several painful mental illnesses, such as panic attacks, can also, at high doses, produce feelings of euphoria. This is no accident; it is the result of fundamental brain biology.
This linking of positive and negative reinforcement is also deeply connected to the common confusion, among physicians and the public, of the use of potentially abused medicines with drug abuse, as was seen earlier in the role of withdrawal in maintaining addiction. Withdrawal symptoms are distressing. Addicted animals, including humans, find relief from acute symptoms of withdrawal to be reinforcing or rewarding. Scientifically, but confusingly, this is called negative reinforcement, because it involves removal of a painful feeling.
One reason cigarette smokers find pleasure in their hourly lighting up of a cigarette is that the jolt of nicotine, which hits their brains within eight seconds after the first puff, begins to relieve the withdrawal discomfort caused by the wearing off of the nicotine effect of the last cigarette as the nicotine levels in the smoker’s brain fall below the level needed to sustain the effect they seek. That is also why the first cigarette in the morning is uniquely satisfying. Addicted smokers have gone for an unusually long time without a cigarette when they wake up in the morning, so nicotine withdrawal symptoms are relatively severe, and their relief after the start of the first cigarette of the day is particularly reinforcing. This is an example of negative reinforcement. It is seen universally in addiction to alcohol and other drugs.
Paths to the Pleasure Centers
Abused drugs directly affect the synapses in the pleasure centers. Many other activities and substances have an impact on the firing of the pleasure-producing neurons. These centers and the brain mechanisms involving pleasure and pain play a vital role in the everyday life of all animals. Food and sex are obvious stimuli for these centers in humans, but so are more mundane activities, from exercising and watching television to reading a good book or buying new clothes.
Understanding the biological basis of addiction requires putting the uncommon and often mysterious experiences of addiction to alcohol and other drugs into a more easily understandable perspective. Begin by thinking about nonchemical pleasures. Assuming that nonchemical pleasures are inherently safe is clearly wrong. Far too much human misery is caused by nondrug pleasurable experiences, such as eating and sex, to permit such a simple assumption.
Addiction involves principally two features: loss of control (unmanageability) and dishonesty (denial). Addicts have such strong and highly valued experiences with particular pleasurable activities that they put those sensations, those experiences, above everyday responsibilities and risk serious harm to themselves and others by pursuing their addictive pleasures. Addicts also lie about their behavior; they cover up and deceive others. Without these two features—loss of control and dishonesty—addiction cannot exist.
Making Excuses for Irrational Behavior
As a young resident in psychiatry, I attended a lecture on hypnotism that has stayed with me. I was fascinated when a professor hypnotized a patient in front of our class. He told the patient that ten minutes after the patient came out of the hypnotic trance, he would go to the window and open it. The doctor gave the patient no reason to do this. It was a cold day, and the room in which the interview was taking place was cold.
The patient came out of the hypnotic trance and, after ten minutes of general discussion with the professor, went to the window and opened it. The professor asked the patient why he had opened the window. The patient said, “I was hot and thought we would be more comfortable with the window open.” The professor said, “But this is my office. Are you accustomed to opening other people’s windows without asking them?” The patient politely replied, “No I’m not. I am sorry. I didn’t even think about asking your permission.” Then the professor asked, “But it is cold in here now and it is even colder outside. Are you sure you want that window open?” The patient held his ground: “Yes, I am more comfortable with the window open right now, thank you.”
As the professor explained that experiment to our group, he told us that the patient did not have any idea why he had opened the window. He was simply making up the most plausible excuses he could on the spot. Years later I thought of that experience as I saw hundreds of people addicted to alcohol and other drugs who sought to explain why they continued to use alcohol and other drugs despite the terrible things that often happened to them as a result of this use. Like the hypnotized patient, they did not know why they acted as they did. They simply made up excuses for what was irrational and self-destructive behavior.
The brain research on addiction has helped me to understand this mystery. People who are addicted act as if they were hypnotized, as if their pleasure centers, like the professor in the experiment, told them to do things in a voice that was not accessible to their conscious minds. So the addicts made up excuses that seemed to be as lame as that poor patient’s excuses for opening the window on a cold day.
This is the process of denial. It is as if the disease of addiction whispered softly in the ear of the addict: “Do it again, right now. Go ahead. It’s okay.” Without consciously hearing the voice that gave the instructions, the addict acted as the voice directed. Even more mysteriously, denial can act to prevent the addict from seeing the addictive behavior at all. It is as if the hypnotic voice of the addictive disease said, “This is not happening at all. You are not doing it.” It would be as if the patient in the experiment said, when challenged by the professor, “What window? I don’t see a window. And if I did see a window, I can assure you that not only did I not open it, but I would positively refuse to open it. What do you take me for, a fool? Anyone can see that it is cold in here as well as cold outside today. Why did you even ask me such a ridiculous question?”
When you confront addicts about their addictive behavior, they deny it. Are they consciously lying, or are they deceived by their own disease? After many years of studying this fascinating process, I have concluded that the answer is “both.” It is about as rewarding to ask addicts why they behave as they do as it was for that professor to ask that patient thirty years ago why he opened the window. To confirm once more the nature of the disease, I can ask the addicts I see in my practice why they continue to use alcohol and other drugs, but I no longer have hope of finding a useful answer to the question because I have learned that addicts have no idea why they are doing what they are doing when it comes to the use of alcohol and other drugs. Their reason, if they admit use at all, is usually, “I do it because I like to do it.” When asked why they lie about their use of addictive drugs, addicts give similarly direct answers that usually come down to, “Because if I told the truth, someone would try to stop me from using my drug.”
Factors Influencing Addiction
Addicts act like people in love. They have lost control of their lives and become crazy in the pursuit of their particular addictive pleasures. The two most common traditional models for chemically produced addictions, heroin and alcohol, follow this pattern. Some people with eating disorders and some people with sexual addictions act in this same way. They live their lives with reckless disregard for social rules and for their own long-term self-interest, focusing only on immediate pleasure, despite the inescapable long-term pain that comes later.
Because loss of control over pleasure-driven behaviors is always a destructive pattern, and because it has been widely experienced in all societies at all times, every human culture has developed rules to govern all of the common pleasurable behaviors. These rules are seen in social conventions, in religions, in laws, and most especially in the family-based management of behaviors. Addicts not only have lost control of their lives, they not only deny their addiction-caused behaviors and the problems these behaviors cause, but they pursue their addictive behaviors in clear conflict with social norms, laws, and religious values. It is remarkable to see the ability of addiction to overcome even the most moral and sensible person. I have seen many physicians, teachers, ministers, and others of high intelligence and great moral strength turned into dishonest and irresponsible people by their addictions. Both they and those who know them well are amazed by this, because they underestimate the power of addiction to control human behavior, regardless of intelligence or character.
To produce an addictive behavior, the stimulus must be powerful. Relatively mild reinforcement will not produce this syndrome. Genetics plays an important role in vulnerability to addictions. Addictive behavior, often specific addictive behavior, to some extent runs in families. Age plays a powerful role. Most addictive behaviors are first evident in the teenage years and the early twenties. The risk of addiction is influenced by many other factors, from the availability of the particular pleasure-producing stimulus to the social tolerance for the addictive behavior. Pleasurable stimuli that are widely available and more tolerated are more likely to be problems than addictive stimuli that are less available and less tolerated in a society.
Protections Against Addiction
When we think of the role of brain biology in addiction, we need to keep in mind that the addicted brain exists in a social and historical context. The experience of addiction is part of a broad social reality. We can see addictive behavior in laboratory animals and observe that some stimuli are so seductive that almost all exposed animals lose control of their behaviors when they can self-administer a substance. Olds’s rats were able to stimulate their pleasure centers, and monkeys used by other brain researchers were given access to cocaine intravenously. These animals all demonstrated addictive behavior in a simple, easily understood form based solely on brain biology. But in human populations, the experience of addiction to alcohol and other drugs is always more complex and far more interesting.
Sometimes people are protected from certain addictions by lack of exposure. Most North Americans today have never used or known anyone who has used heroin or cocaine, just as most people have never stuffed and vomited food (bulimia) or restricted the intake of food to a life-threatening degree (anorexia nervosa), syndromes that are serious, newly common eating disorders. Neither have most people gambled in a way that jeopardized their financial well-being. Sometimes people are protected from a particular addiction because they do not even consider such actions, and sometimes they are protected because they are not exposed to the behaviors or some aspect necessary for the behaviors (for example, hypodermic syringes containing heroin). Many people are protected by values and other cultural factors: “People like me don’t do things like that.” Most of us have been told not to engage in most addictive behaviors.
Often, our parents, teachers, and religious leaders tell us not to take risks with addiction. Some of us listen to that advice and others do not. Those who are not exposed or who have an inner values-based protection are relatively safe from addiction. Many of those who are exposed to particularly addictive behaviors, as most North Americans are these days to alcohol and tobacco, have a second level of defense. Some who try these behaviors are repelled or simply not interested in them. Some people do not like the taste of alcohol, or they find the experience of being drunk to be unpleasant. Many people are repelled by their first cigarette.
That initial repulsion, as well as the biologically based lack of reward from the initial experience with the addictive behavior, protects many people from addictions. People who are not protected by physical or psychological unavailability or by their lack of satisfaction with the addictive experience routinely progress to the first state of active addiction. This is where the mystery and the danger of this disease deepen.
Learning to Find Pleasure
Many of the most intensely pleasurable behaviors are not fun the first time, even for people who become addicts. One must learn to get high or to have fun in addictive ways, the ways that the pleasure centers of the researchers’ dogs learned to respond to meat bones. Typically, addicts learn by engaging in the addictive behavior with others who are doing it, usually those in their immediate friendship group. This sort of initiation is called “turning on” a friend. It involves teaching the person how to get high. This turning on is rarely, if ever, done out of meanness. It is done out of the enthusiasm the more experienced addicts feel for the pleasure that they have discovered and that they highly value. New drug users, who have yet to feel the full burden of their addictions, are the most likely to spread their addictive behavior because their enthusiasms are the most intense and their restraint is not limited by painful consequences of addiction.
Twenty-year heroin addicts over the age of forty are not eager to turn on a seventeen-year-old neophyte. Neither are they attractive role models. Even with a good friend as a coach, people vary greatly, with some getting hooked quickly and others not getting hooked at all. Biology plays a major role in determining the level of reinforcement of a particular behavior. Some people have genetically large doors to their pleasure centers with particular potentially addictive stimuli. Others have small doors that are not easily opened to the same stimuli.
When I talk with addicts, I ask what their thoughts were the first time they used their favorite drug or first engaged in a particular addictive behavior. When the turning on occurred in early teenage years, and when the answer is, “It was like finding the most important thing in my life—something I had looked for but never found before,” then I know the addiction is especially strong. When the answer is, “I did it for years and never had a problem, but then one day something happened and I lost control,” I know the addiction is serious, but the chances of recovery are better, and the effort needed to get well is likely to be less.
Why Me?
Why do some people get addicted and others do not? Why do some people fall in love and others do not? Why does this person love that other one, whereas another person finds that one to be entirely uninteresting? There are no simple answers to these basic questions, but being in a receptive frame of mind, being in an encouraging environment, and being exposed to powerful brain-stimulating experiences go along with individual biological factors to shape the relative risk for particular addictive behaviors. Environmental and personal factors are both important in the addiction equation.
Another major factor in determining relative addiction risk is the behavior or the substance itself. Some substances and some behaviors are inherently more likely to produce intense pleasure than others. Prudent people, prudent families, and prudent communities limit these exposures, especially for youth under the age of about twenty-five. They also erect clear boundaries so that those who have lost control can identify their affliction as early as possible. Trying heroin is a more risky behavior than is trying alcohol.
Smoking cocaine is more risky than snorting it. Frequent use of a drug is more risky than occasional use. For people with high addiction potentials, however, a single use of a particular drug can be addictive, and for people with low addiction potentials, even repeated intensive use of some drugs can fail to throw the addiction switch to “on.”
The Myth of Self-Medication
The drug abuser’s behavior has sometimes been explained as an attempt to self-medicate. Self-medication means the use of intoxicating drugs (such as alcohol, cocaine, and heroin) to treat unpleasant feelings (such as severe anxiety, depression, or pain) that result from an illness. Although distress from an illness may be a reason some addicts first came in contact with a particular nonmedical drug, I am skeptical of the self-medication hypothesis as an explanation for persistent addictive behavior. Drug abusers do not abuse any medicine that does not produce reward or reinforcement. For example, people do not abuse arthritis medicines or antibiotics, two effective and commonly used classes of medicines that reduce distress. People with panic disorder do not abuse antidepressants even though they block panic attacks. Drug abusers do, however, abuse stimulants and narcotics. The reasons certain drugs are abused, but most medicines are not, has nothing to do with self-medication and everything to do with feelings produced in the brain’s pleasure centers.
For people who have infections and arthritis, both of which can be terribly painful, the medicines used to treat their diseases are powerful. Once people with these diseases understand the importance of specific treatments, they are highly motivated to use the medicines. This is not self-medication, and these medicines have no appeal to drug abusers. Such medical patients, if they are denied access to their pain-relieving medicines, will exhibit “drug-seeking behavior” in the sense that they will take steps to ensure that they get the medicines they need. When drug addicts and alcoholics talk of self-medication, they refer only to their use of abused drugs such as alcohol and cocaine, never to routine, nonabused medicines such as antibiotics or antiarthritic medicines.
Because of my own professional involvement with both addiction and the anxiety disorders, I am drawn to the more complex aspects of the self-medication controversy in addiction, using anxiety as an example. Most clinically anxious people fear loss of control, so they do not drink alcohol or, if they do drink, they use alcohol exceedingly moderately. On the other hand, some people who suffer from anxiety disorders do use alcohol and find that it reduces their painful panic and anxiety, at least for an hour or so following alcohol use. A small percentage of all anxious patients get trapped in their use of alcohol, escalating their alcohol use over time in an alcoholic pattern.
Some anxious people become dependent on alcohol, using it in repeated doses throughout the day (maintenance drinking), and some anxious people use alcohol in a bingelike pattern (binge drinking). Most anxious patients who continue to demonstrate either of these patterns of alcoholic drinking when their drinking persists once the anxiety disorder has been treated have a family history of alcoholism. This makes it apparent that these people found not just brief symptomatic relief from their anxiety in the alcohol, but reward, or a high, with which they literally fell in love. It was the reward that produced the addiction, not the antianxiety effects of the alcohol.
Addicted anxious patients show the typical alcoholic pattern, which is easily distinguished from the common drinking behavior of the typical nonaddicted sufferer from an anxiety disorder. For these alcoholic people, their anxiety disorder does not explain their addiction to alcohol or other drugs, but occasionally it does explain how they became involved with alcohol in the first place.
The relationship of addiction to anxiety disorders is more complex than this initial picture suggests. Alcohol reduces anxiety only in the short run. Over hours, and even more over days and weeks, alcohol makes panic and anxiety worse. In fact, many alcoholics and addicts to other drugs, as part of their addiction, become clinically anxious, even sometimes suffering from panic attacks and other specific anxiety disorders. For most such addicted and anxious people, simply stopping drinking (which usually requires a program of lifelong recovery in Alcoholics Anonymous) will terminate the symptoms of their anxiety disorder. In other words, for these alcoholic people, their anxiety disorder is secondary to their addiction in that their anxiety problem followed their addiction. Once the primary addiction to alcohol is under control, the secondary anxiety disorder diminishes or even disappears.
Anxiety disorders can also be used by addicts as an excuse for their addictions. Even worse, this connection of alcoholism and anxiety can be an excuse for physicians who prescribe addicting drugs to people who are addicted to alcohol and other drugs in the mistaken belief that such treatment will improve both their anxiety and their addiction. When anxiety coexists with addiction, I suggest considering the addiction to be the primary disease when it comes to treatment.
Addicts regularly speak of using drugs to “feel normal.” This is the result of their having so disturbed the normal function of the pleasure centers in their brains that they feel lousy without their alcohol or other drugs. Nevertheless, the drugs that addicts seek for purposes of self-medication are the drugs that stimulate the brain’s pleasure centers. Usually this drug-using behavior is simply addictive behavior hiding behind the rationalization of self-medication.
Whether the bad feeling being “treated” by the addicted person is anxiety, depression, anger, pain, or some other intensely unpleasant state, or whether the bad feelings are the result of prior drug use (as is commonly the case with hangover from drinking alcohol or withdrawal from heroin use), the reason the addicted person is using alcohol and other drugs over a prolonged period of time can be traced to the person’s love affair with getting high, not to the discomfort of a preexisting disease. People who are not vulnerable biologically to addiction, and who experience anxiety, depression, pain, and other uncomfortable feelings, do not become addicted to alcohol and other abused drugs, even if they are exposed to them and find some temporary relief from their discomfort as a result of their use of these substances.
Although called pleasure, the drug high bears little relationship to the joys of stamp collecting, climbing a mountain, or talking with a friend. The drug user’s high is far more intense and gripping—it is much closer to the experience of sexual orgasm or eating a large meal than it is to visiting an art museum. The drug high is a primitive profound brain stimulation, a sledgehammer blow to the brain’s normally subtle pleasure system. Self-medication simply does not explain the experience of persistent use of addicting drugs despite the problems that this use typically causes addicted people.
Brain biology offers a useful way to think about the self-medication hypothesis of addictive drug use. Anxiety and panic are governed by the locus coeruleus in the brain stem. When the ventral tegmental area and the nucleus accumbens in the midbrain, the principal pleasure centers, are stimulated, they send signals to quiet the locus coeruleus. When an addicted person experiences physical withdrawal, the locus coeruleus sends out distressing alarm signals for days, making sleep difficult or impossible and producing profoundly uncomfortable anxiety and even panic attacks.
Drugs that stimulate the ventral tegmental area and the nucleus accumbens, as all addicting drugs do, calm the locus coeruleus. Once addiction has taken hold in the brain, when addicting drug use stops, the locus coeruleus is sent into action, helping to produce the painful withdrawal syndrome. With repeated alcohol and other drug use over time, the pleasure centers of the brain require more and more stimulation to produce pleasure, raising the risks of withdrawal when drug levels fall in the brain. What started as a self-controlled search for pleasure, and relief of discomfort from an anxiety or other mental or physical disorder, increasingly becomes a desperate out-of-control search for a feeling of normality, a way of escaping the brain’s distressing alarm mechanism managed by the locus coeruleus.
For most people who do not have a preexisting vulnerability to addiction, the process of using addictive drugs to suppress uncomfortable feelings is short-lived as they learn that the stimulation of the brain’s pleasure centers by the nonmedical use of drugs from alcohol to heroin is a fool’s game. At best, they get short-term gains at the price of long-term disasters. For most nonalcoholic drinkers, one hangover or one episode of uncomfortable intoxication is enough to convince them that large doses of alcohol and other drugs are, in the end, no fun at all. In contrast, people who are biologically vulnerable to addiction are seduced in the process of repeated nonmedical drug use into persistent addictive behaviors despite the problems their alcohol and other drug use causes. For addiction-prone people, it is often difficult to sort out the positive rewards of addictive drug use (the pleasure from the stimulation of the pleasure centers of their brains) from the negative rewards (the relief of discomfort from the quieting of the locus coeruleus, whether it is stimulated by withdrawal or an underlying mental disorder).
The All-Too-Human Disorder of Addiction
Addiction is a human disorder that can afflict anyone. No one is immune to addiction. Any pleasurable action can be addictive, meaning it can lead to loss of control and dishonesty. There are some simple, and old-fashioned, guidelines that protect people from addictions. The antidote to addiction is honesty with respect to alcohol and other drug use. That approach is fairly easy for most nonaddicted people to understand and even to practice. It is difficult for addicts to practice because the addiction has taken hold of their brains and has induced distortions in their thinking, including dishonesty. They rationalize their addictive behaviors to protect the forbidden fun of their addictive alcohol and other drug use. When a person gets well from any addiction, the inner experience is similar to a person being released from slavery, the experience of a prisoner being freed from captivity. The slavery of addiction is especially painful, humiliating, and cruel because it appears to be self-imposed. Addiction is all the more mysterious because this awesome misery is a “pleasure disease” that makes addicts and those who love them miserable and because addicted people remain vulnerable to relapse throughout their lives.
Case Histories
Here are two stories about the use of prescription medicines that have abuse potentials, and about the boundaries of addictive behaviors.
Jeb
Jeb is a conscientious, forty-seven-year-old, single scientist working for the federal government. He came to me for help with obsessive-compulsive disorder (OCD) because of his continuing morbid fear that when driving his car he had accidentally run over a pedestrian. He was a cautious driver with an unblemished driving record. Nevertheless, his unrealistic fear led to his driving around the block over and over again to check for “bodies.” On many occasions when he came home from work, even after repeated checks to see if he had run over anyone, he could only get a bit of relief from these intrusive, unwanted, repugnant thoughts, which he knew were unreasonable, by watching the local news to see if there was a report of a hit-and-run victim being found on his commuting route. He did well in therapy with a combination of antianxiety and antiobsessional medicines.
As therapy progressed, he told me about his alcoholism. I was surprised by his labeling of himself as an alcoholic because his character was about as far from that of a typical addict as it is possible to be. He was not a risk taker. He was conscientious to a fault. He was introverted and barely social. He explained that he had started to drink in college, “when everyone was doing it,” and that in his thirties his drinking had increased in a pattern he called “self-medication.” He would often drink one or two beers when he got home from work late in the evening. He often experienced social insecurity on the infrequent occasions when he went out in the evenings with friends, saying he often drank “way too much,” often five or six beers, for example. After each of these episodes, he felt sick the next morning with a hangover and swore to stop drinking in the future. He did not have a close relative who was addicted to alcohol or other drugs.
About eight years ago a friend of Jeb’s went into a local addiction treatment program and came out talking about what a big improvement this had produced in his life. Jeb thought more about his own drinking. He admitted himself to the addiction treatment program, which he found generally helpful, and stayed seven weeks. He went to a lot of AA meetings and defined himself as a chronic alcoholic who self-medicated with alcohol for his anxiety symptoms. He stopped going to AA shortly after leaving the treatment program. He had never relapsed to alcohol use since then, although he guiltily told me he had sipped an aperitif with the family of his girlfriend one evening several years ago. He did not crave alcohol; he had no interest in ever drinking again and made no effort whatsoever to control or contain his desire to drink because he had no such desire.
I asked Jeb about how he used his antianxiety medicine. He said he often took a dose at 7 a.m. when he got up and then used one or two additional doses as the day progressed. His use of medicines was very moderate, in low doses, and it showed no tendency to escalate over many years of treatment. His use of medicines improved his life and did not lead to his relapsing to alcohol use. The medicine did not lose its effectiveness. He had never in his life used any other drug nonmedically (such as marijuana or cocaine). I asked Jeb if he ever self-medicated with alcohol the way he used his antianxiety medicine, starting in the morning and using it at low doses throughout the day. He said, “No. I never even thought of that. I didn’t want to be impaired at work or when I drove.” I asked if he ever self-medicated on the weekends, morning, noon, and night, when he was often quite anxious with his OCD. He said, “No. That’s not how I ever drank or even thought of drinking.” I asked him about the comparative effectiveness of alcohol and his antianxiety medicine in terms of his anxiety. He said the alcohol blotted out his feelings entirely, whereas the antianxiety medicine just made him worry less, but did not reduce his ability to drive, work, or think clearly.
Jeb’s pattern of drinking was not normal. He clearly had a tendency to drink too much on the rare occasions when he drank at parties, but he never had an adverse result of his drinking (such as blackouts, accidents, arrests, loss of work, strained relationships), and he never drank in settings other than those commonly used for social drinking. If he was self-medicating with alcohol, it was a pattern that was easily distinguished from the pattern in which he used antianxiety medicine, as were the effects of alcohol use easily distinguished from those of his antianxiety medicine use. Jeb’s use of the antianxiety medicine also was not the way active drug abusers treat these medicines. Addicts tend to use antianxiety medicines at high and unstable doses, and to mix them right in with their heavy use of other drugs nonmedicaliy, most often alcohol, marijuana, and cocaine.
Was Jeb an alcoholic? I am not sure, but I would not label him an alcoholic despite the abnormality of his drinking. The fact that he did not go to AA meetings once he was out of treatment and did not seem to need meetings to stay abstinent reinforces this view. On the other hand, it was clearly helpful to Jeb to think of himself as an alcoholic. His public identification as an alcoholic was helpful to the many people he worked with and knew socially, since it encouraged them to look at their own drinking skeptically and to view treatment for addiction positively. It is also possible that I am wrong and that Jeb is an alcoholic whose repeated self-identification as an alcoholic is vital to his maintaining his sobriety. In the spirit of “if it ain’t broke, don’t fix it,” I listened respectfully to Jeb’s happy story of recovery and congratulated him on his success in overcoming this problem.
Timmy
Timmy was a thirty-seven-year-old chronic heroin addict whose mother paid for him to see me. When he missed an appointment one day, I called him at home. He said, “Oh, gosh Doc, I misplaced your appointment card and I thought I was to see you later in the week.” He had pawned some family heirlooms, ancient dueling pistols he had taken out of his mother’s home. He needed to get them back before they were sold by the pawnshop. He wondered if his mother would pay for this debt, especially since he had already gotten money from her to buy the same items back from the same pawnshop six months before. He knew he was a liar, but he also knew his mother was codependent. He was sure that, when he told his mother how deeply he cared about these old dueling pistols and how mean the pawnbroker was, she would do what she had done thousands of times before. She would scold him, get him to say he was sorry and would never do it again, and then give him the money he asked for.
That did not surprise me, but what did surprise me in this conversation was Timmy’s description of his own codependence. His girlfriend, Julie, was also a heroin addict, but she also liked to abuse antianxiety medicines such as Xanax and Valium. She wanted Timmy to give her $10 and drive her to a downtown public mental health clinic so that she could buy some pills that were sold on the street outside the clinic by patients who got them from their doctors inside the clinic. Julie would take large doses of the pills orally and then pass out in a drunken stupor for several hours. Timmy lamented his own weakness in repeatedly doing this for Julie, even though he knew it was a waste of their scarce money (neither worked) and it did her no good. Julie sometimes got her own pills to abuse, going to doctors and saying that she was anxious and had panic attacks and that these medicines helped her a lot. But when she got prescriptions herself, the medicines were relatively expensive to get at the pharmacies, and the doctors wanted to be paid in advance for visits to them. Julie found it was cheaper on the street to buy the pills, which were provided to welfare patients on Medicaid than to get the drugs from private physicians, but both approaches worked well for her.
Julie’s pattern of abuse of antianxiety medicines contrasts clearly with the pattern of medical use of these same substances by Jeb. Julie’s experience also raises red flags for all doctors when it comes to the use of controlled substances in medical practice. For the social contract for drug use to work, physicians must know their patients and be able to distinguish addicted patients from physically dependent pseudoaddicts. Both the medical and nonmedical use of controlled substances reflect the workings of these chemicals in the human brain.