5-3. Cold Injuries
Cold injuries are most likely to occur when conditions are moderately cold, but accompanied by wet or windy conditions. Cold injuries can usually be prevented. Well-disciplined and well-trained service members can be protected even in the most adverse circumstances. They and their leaders must know the hazards of exposure to the cold. They must know the importance of personal hygiene, exercise, care of the feet and hands, and the use of protective clothing.
- a. Contributing Factors.
-
- (1) Temperature, humidity, precipitation, and wind greatly increase likelihood of cold injuries, and the service members with wet clothing are at great risk of cold injuries. Riverine operations (river, swamp, and stream crossings) increase likelihood of cold injuries. Low temperatures and low relative humidity (dry cold) promote frostbite. Higher temperatures, together with moisture, promote immersion syndrome. Windchill accelerates the loss of body heat and may aggravate cold injuries.
- (2) Relatively stationary activities such as being in an observation post or on guard duty increase the service member’s vulnerability to cold injury. Also, a service member is more likely to receive a cold injury if he is —
-
- • In contact with the ground (such as marching, performing guard duty, or engaging in other outside activities).
- • Immobile for long periods (such as while riding in an unheated or open vehicle).
- • Standing in water, such as in a foxhole.
- • Out in the cold for days without being warmed.
- • Deprived of an adequate diet and rest.
- • Not able to take care of his personal hygiene.
- (3) Physical fatigue contributes to apathy, which leads to inactivity, personal neglect, carelessness, and reduced heat production. In turn, these increase the risk of cold injury. Service members with prior cold injuries have a higher-than-normal risk of subsequent cold injury; not necessarily involving the body part previously injured.
- (4) Depressed or unresponsive service members are also vulnerable because they are less active. These service members tend to be careless about precautionary measures, especially warming activities, when cold injury is a threat.
- (5) Excessive use of alcohol or drugs leading to faulty judgment or unconsciousness in a cold environment increases the risk of becoming a cold injury casualty.
- b. Signs and Symptoms. Once a service member becomes familiar with the factors that contribute to cold injury, he must learn to recognize cold injury signs and symptoms.
-
- (1) Many service members suffer cold injury without realizing what is happening to them. They may be cold and generally uncomfortable. These service members often do not notice the injured part because it is already numb from the cold.
- (2) Superficial cold injury usually can be detected by numbness or tingling sensations. These signs and symptoms often can be relieved simply by loosening boots or other clothing and by exercising to improve circulation. In more advanced cases involving deep cold injury, the service member often is not aware that there is a problem until the affected part feels like a stump or block of wood.
- (3) Outward signs of cold injury include discoloration of the skin at the site of injury. In light-skinned persons, the skin first reddens and then becomes pale or waxy white. In dark-skinned persons, grayness in the skin is usually evident. An injured foot or hand feels cold to the touch. Swelling may be an indication of deep injury. Also note that blisters may occur after rewarming the affected parts. Service members should work in pairs (buddy teams) to check each other for signs of discoloration and other symptoms.
- c. First Aid Measures. First aid for cold injuries depends on whether they are superficial or deep. Rewarming the affected part using body heat can adequately treat cases of superficial cold injury. (For example, this can be done by covering cheeks with hands, putting fingertips in armpits, or placing the casualty’s feet under the clothing of a buddy [next to his belly].) The injured part should NOT be massaged, exposed to a fire or stove, rubbed with snow, slapped, chafed, or soaked in cold water. Walking on injured feet should be avoided. Deep cold injury (frostbite) is very serious and requires prompt first aid to avoid or to minimize the loss of parts or all of the fingers, toes, hands, or feet. The sequence for treating cold injuries depends on whether the condition is life-threatening. The first priority in managing cold injuries is to remove the casualty from the cold environment (such as building an improvised shelter). Other injuries the casualty may have are provided first aid simultaneously while waiting for transportation or evacuation. If the casualty is to be transported in a nonmedical vehicle, first aid measures should be continued en route to the MTF.
- d. Conditions Caused by Cold. Conditions caused by cold include chilblain, immersion syndrome (immersion foot and trench foot), frostbite, snow blindness, dehydration, and hypothermia.
-
- (1) Chilblain.
-
- • Signs and symptoms. Chilblain is caused by repeated prolonged exposure of bare skin at temperatures from 60° Fahrenheit (F) to 32°F, or 20°F for acclimated, dry, unwashed skin. The area may be acutely swollen, red, tender, and hot with itchy skin. There may be no loss of skin tissue in untreated cases but continued exposure may lead to infected, ulcerated, or bleeding lesions.
- • First aid measures. Within minutes, the area usually responds to locally applied body heat. Rewarm the affected part by applying firm steady pressure with your hands, or placing the affected part under your arms or against the stomach of a buddy. DO NOT rub or massage affected areas.
NOTE
Medical personnel should evaluate the injury, because signs and symptoms of tissue damage may be slow to appear.
-
- (2) Immersion syndrome (immersion foot and trench foot). Immersion foot and trench foot are injuries that result from fairly long exposure of the feet to wet conditions at temperatures from approximately 32°F to 50°F. Inactive feet in damp or wet socks and boots, or tightly laced boots which impair circulation, are even more susceptible to injury. This injury can be very serious; it can lead to loss of toes or parts of the feet. If exposure of the feet has been prolonged and severe, the feet may swell so much that pressure closes the blood vessels and cuts off circulation. Should an immersion injury occur, dry the feet thoroughly and transport the casualty to an MTF by the fastest means possible.
-
- • Signs and symptoms. At first, the parts of the affected foot are cold and painless, the pulse is weak, and numbness may be present. Second, the parts may feel hot, and burning and shooting pains may begin. In later stages, the skin is pale with a bluish cast and the pulse decreases. Other signs and symptoms that may follow are blistering, swelling, redness, heat, hemorrhaging (bleeding), and gangrene.
- • First aid measures. First aid measures are required for all stages of immersion syndrome injury. Rewarm the injured part gradually by exposing it to warm air. Protect it from trauma and secondary infections. Dry, loose clothing or several layers of warm coverings are preferable to extreme heat. Under no circumstances should the injured part be exposed to an open fire. Elevate the injured part to relieve the swelling. Transport the casualty to an MTF as soon as possible. When the part is rewarmed, the casualty often feels a burning sensation and pain. Symptoms may persist for days or weeks even after rewarming.
NOTE
When providing first aid for immersion foot and trench foot — DO NOT massage the injured part. DO NOT moisten the skin. DO NOT apply heat or ice.
-
- (3) Frostbite. Frostbite is the injury of tissue caused from exposure to cold, usually below 32°F depending on the windchill factor, duration of exposure, and adequacy of protection. Individuals with a history of cold injury are likely to suffer an additional cold injury. The body parts most easily frostbitten are the cheeks, nose, ears, chin, forehead, wrists, hands, and feet. Frostbite may involve only the skin (superficial), or it may extend to a depth below the skin (deep). Deep frostbite is very serious and requires prompt first aid to avoid or to minimize the loss of parts or all of the fingers, toes, hands, or feet.
-
- • Signs and symptoms.
-
- • Loss of sensation (numb feeling) in any part of the body.
- • Sudden blanching (whitening) of the skin of the affected part, followed by a momentary tingling sensation.
- • Redness of skin in light-skinned service members; grayish coloring in dark-skinned service members.
- • Blisters.
- • Swelling or tender areas.
- • Loss of previous sensation of pain in affected area.
- • Pale, yellowish, waxy-looking skin.
- • Frozen tissue that feels solid (or wooden) to the touch.
CAUTION
Deep frostbite is a very serious injury and requires immediate first aid and subsequent medical treatment to avoid or minimize loss of body parts.
-
-
- • First aid measures.
-
- • Face, ears, and nose. Cover the casualty’s affected area with his and/or your bare hands until sensation and color return.
- • Hands. Open the casualty’s field jacket and shirt. (In a chemical environment, do not loosen or remove the clothing and protective overgarments.) Place the affected hands under the casualty’s armpits. Close the field jacket and shirt to prevent additional exposure.
- • Feet. Remove the casualty’s boots and socks if he does not need to walk any further to receive additional treatment. (Thawing the casualty’s feet and forcing him to walk on them will cause additional pain and injury.) Place the affected feet under clothing and against the body of another service member.
WARNING
DO NOT attempt to thaw the casualty’s feet or other frozen areas if he will be required to walk or travel to an MTF for additional medical treatment. The possibility of additional injury from walking is less when the feet are frozen than when they are thawed. (However, if possible avoid walking.) Thawing in the field increases the possibilities of infection, gangrene, or other injury.
NOTE
Thawing may occur spontaneously during transportation to the MTF; this cannot be avoided since the body in general must be kept warm.
In all of the above areas, ensure that the casualty is kept warm and that he is covered (to avoid further injury). Seek medical treatment as soon as possible. Reassure the casualty, protect the affected area from further injury by covering it lightly with a blanket or any dry clothing, and seek shelter out of the wind. Remove or loosen constricting clothing (except in a contaminated environment) and increase insulation. Ensure the casualty exercises as much as possible, avoiding trauma to the injured part, and is prepared for pain when thawing occurs. Protect the frostbitten part from additional injury. DO NOT —
-
-
- • Rub the injured part with snow or apply cold water soaks.
-
- • Warm the part by massage or exposure to open fire because the frozen part may be burned due to the lack of feeling.
- • Use ointments or other salves.
- • Manipulate the part in any way to increase circulation.
- • Use alcohol or tobacco because this reduces the body’s resistance to cold.
NOTE
Remember, when freezing extends to a depth below the skin, it is a much more serious injury. Extra care is required to reduce or avoid the chances of losing all or part of the toes or feet. This also applies to the fingers and hands.
-
- (4) Snow blindness. Snow blindness is the effect that glare from an ice field or snowfield has on the eyes. It is more likely to occur in hazy, cloudy weather than when the sun is shining. Glare from the sun will cause an individual to instinctively protect his eyes. However, in cloudy weather, he may be overconfident and expose his eyes longer than when the threat is more obvious. He may also neglect precautions such as the use of protective eyewear. Waiting until discomfort (pain) is felt before using protective eyewear is dangerous because a deep burn of the eyes may already have occurred.
-
- • Signs and symptoms. Symptoms of snow blindness are a sensation of grit in the eyes with pain in and over the eyes, made worse by moving the eyeball. Other signs and symptoms are watering, redness, headache, and increased pain on exposure to light.
- • First aid measures. First aid measures consist of blindfolding or covering the eyes with a dark cloth which stops painful eye movement. Complete rest is desirable. If further exposure to light is not preventable, the eyes should be protected with dark bandages or the darkest glasses available. Once unprotected exposure to sunlight stops, the condition usually heals in a few days without permanent damage. The casualty should be evacuated to the nearest MTF.
- (5) Dehydration. Dehydration occurs when the body loses too much fluid. A certain amount of body fluid is lost through normal body processes. A normal daily intake of liquids replaces these losses. When individuals are engaged in any strenuous exercises or activities, fluid is lost through sweating and this loss creates an imbalance of fluids in the body, and if not matched by rehydration it can contribute to dehydration. The danger of dehydration is as prevalent in cold regions as it is in hot regions. In hot weather, the individual is aware of his body losing fluids through sweat. In cold weather, however, it is extremely difficult to realize that this condition exists since sweating is not as apparent as in a hot environment. The danger of dehydration in cold weather operations is a serious problem. In cold climates, sweat evaporates so rapidly or is absorbed so thoroughly by layers of heavy clothing that it is rarely visible on the skin. Dehydration also occurs during cold weather operations because drinking is inconvenient. Dehydration will weaken or incapacitate a casualty for a few hours, or sometimes, several days. Because rest is an important part of the recovery process, casualties must take care that limited movement during their recuperative period does not enhance the risk of becoming a cold injury casualty.
-
- • Signs and symptoms. The symptoms of cold weather dehydration are similar to those encountered in heat exhaustion. The mouth, tongue, and throat become parched and dry, and swallowing becomes difficult. The casualty may have nausea (with or without vomiting) along with extreme dizziness and fainting. The casualty may also feel generally tired and weak and may experience muscle cramps. Focusing the eyes may also become difficult.
- • First aid measures. The casualty should be kept warm and his clothes should be loosened (if not in a chemical environment) to allow proper circulation. Shelter from wind and cold must be provided. Fluid replacement should begin immediately and the service member transported to an MTF as soon as possible.
- (6) Hypothermia (general cooling). When exposed to prolonged cold weather a service member may become both mentally and physically numb, thus neglecting essential tasks or requiring more time and effort to achieve them. Under some conditions (particularly cold water immersion), even a service member in excellent physical condition may die in a matter of minutes. The destructive influence of cold on the body is called hypothermia. This means bodies lose heat faster than they can produce it. Hypothermia can occur from exposure to temperatures either above or below freezing, especially from immersion in cold water, wet-cold conditions, or from the effect of wind. Physical exhaustion and insufficient food intake may also increase the risk of hypothermia. General cooling of the entire body to a temperature below 95°F is caused by continued exposure to low or rapidly dropping temperatures, cold moisture, snow, or ice. Fatigue, poor physical condition, dehydration, faulty blood circulation, alcohol or other drug use, trauma, and immersion can cause hypothermia. Remember, cold may affect the body systems slowly and almost without notice. Service members exposed to low temperatures for extended periods may suffer ill effects even if they are well protected by clothing.
-
- • Signs and symptoms. As the body cools, there are several stages of progressive discomfort and impairment. A sign that is noticed immediately is shivering. Shivering is an attempt by the body to generate heat. The pulse is faint or very difficult to detect. People with temperatures around 90°F may be drowsy and mentally slow. Their ability to move may be hampered, stiff, and uncoordinated, but they may be able to function minimally. Their speech may be slurred. As the body temperature drops further, shock becomes evident as the person’s eyes assume a glassy state, breathing becomes slow and shallow, and the pulse becomes weaker or absent. The person becomes very stiff and uncoordinated. Unconsciousness may follow quickly. As the body temperature drops even lower, the extremities freeze, and a deep (or core) body temperature (below 85°F) increases the risk of irregular heart action. This irregular heart action or heart standstill can result in sudden death.
- • First aid measures. Except in cases of the most severe hypothermia (marked by coma or unconsciousness and a weak pulse), first aid measures for hypothermia are directed towards protecting the casualty from further loss of body heat. For the casualty who is conscious, first aid measures are directed at rewarming the body evenly and without delay. Provide heat by using a hot water bottle or field expedient or another service member’s body heat.
CAUTION
DO NOT expose the casualty to an open fire, as he may become burned.
NOTE
When using a hot water bottle or field expedient (canteen filled with warm water), the bottle or canteen must be wrapped in cloth prior to placing it next to the casualty. This will reduce the chance of burning the casualty’s skin.
Always call or send for help as soon as possible and protect the casualty immediately with dry clothing or a sleeping bag. Then, move him to a warm place. Evaluate other injuries and provide first aid as required. First aid measures can be performed while the casualty is waiting transportation or while he is en route. In the case of an accidental breakthrough into ice water, or other hypothermic accident, strip the casualty of wet clothing immediately and bundle him into a sleeping bag. Rescue breathing should be started at once if the casualty’s breathing has stopped or is irregular or shallow. Warm liquids (NOT HOT) may be given gradually if the casualty is conscious. DO NOT force liquids on an unconscious or semiconscious casualty because he may choke. The casualty should be transported on a litter because the exertion of walking may aggravate circulation problems. Medical personnel should immediately treat any hypothermia casualty. Hypothermia is life threatening until normal body temperature has been restored. The first aid measures for a casualty with severe hypothermia are based upon the following principles: attempt to avoid further heat loss, handle the casualty gently, and transport the casualty as soon as possible to the nearest MTF. If at all possible, the casualty should be evacuated by medical personnel.
WARNING
Rewarming a severely hypothermic casualty is extremely dangerous in the field due to the possibility of such complications as rewarming, shock and disturbances in the rhythm of the heartbeat. These conditions require treatment by medical personnel.
NOTE
Resuscitation of casualties with hypothermic complications is difficult if not impossible to do outside of an MTF setting.
CAUTION
The casualty is unable to generate his own body heat. Therefore, merely placing him in a blanket or sleeping bag is not sufficient.
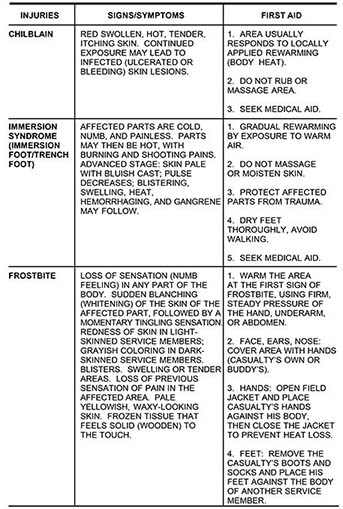
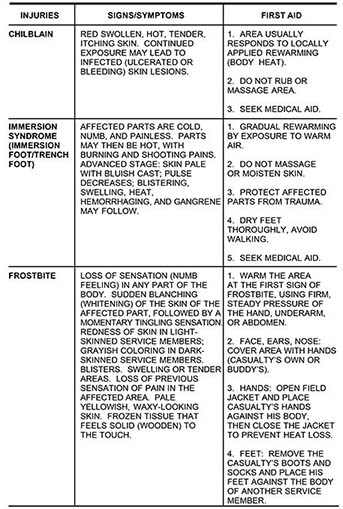
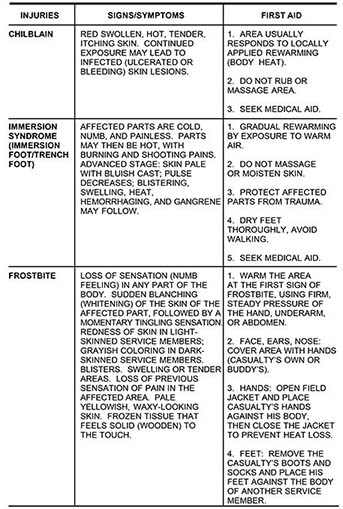
- e. Table. See Table 5-2 for further information.
Table 5-2. Injuries Caused by Cold and Wet Conditions