CHAPTER 33
Lurasidone
Philip D. Harvey, Ph.D.
Lurasidone (Latuda), one of the most recent additions to the atypical antipsychotic class, received U.S. Food and Drug Administration (FDA) approval for the treatment of schizophrenia in October 2010 and for the treatment of bipolar depression in June 2013. As with all currently registered antipsychotic medications, lurasidone is a dopamine D2 receptor antagonist. In addition, this compound is a full antagonist at the serotonin 2A (5-HT2A) receptor, similar to other atypical antipsychotic medications. Lurasidone has other receptor affinities that may contribute to additional beneficial or adverse effects. Because lurasidone is relatively new, its database is limited compared with that of other medications, although the recently approved indication for bipolar depression has led to several additional publications. A current interesting line of investigation is lurasidone’s potential utility in the treatment of a new entity defined in DSM-5 (American Psychiatric Association 2013), bipolar depression with mixed features.
In this chapter, I review the pharmacological properties and efficacy basis of lurasidone, the side effects and adverse events from the pivotal studies, and other features of the compound that may prove to be important in later studies as well as in the clinical applications of this agent. I also consider the question of what, if anything, seems unique about lurasidone compared with other available antipsychotic medications.
Pharmacological Properties
Receptor-Binding Profile
Lurasidone belongs to the chemical class of benzisothiazole derivatives (Figure 33–1). The compound is a full antagonist at dopamine D2 and serotonin 5-HT2A receptors, a profile it shares with other atypical antipsychotics. Lurasidone also has high affinity for 5-HT7 receptors, with in vitro affinity for 5-HT7 being relatively higher than that shown by the drug for D2 and 5-HT2A receptors. Lurasidone is a partial agonist at 5-HT1A receptors (Ishibashi et al. 2010), and it has moderate affinity for noradrenergic receptors. Lurasidone’s minimal affinity for α1-adrenergic receptors would be expected to convey a reduced risk for orthostatic hypotension in comparison with compounds that have higher affinity for this receptor. Lurasidone appears to have weak affinity for 5-HT2C receptors and no affinity for histamine H1 receptors, a profile that should carry relatively low risk for weight gain. Lurasidone lacks affinity for muscarinic acetylcholine M1 receptors, which suggests reduced risk for cholinergic cognitive deficits and other side effects.
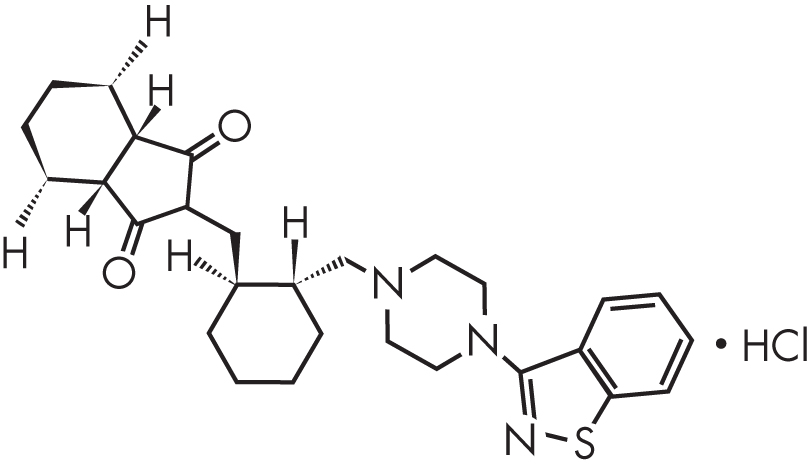
FIGURE 33–1. Chemical structure of lurasidone.
Pharmacokinetics and Dosing
Lurasidone is rapidly absorbed and reaches peak concentrations within 3 hours for the lowest effective antipsychotic dose, 40 mg. Steady state is reached within 7 days (Sunovion Pharmaceuticals 2013). The molecule is metabolized in the liver via the cytochrome P450 (CYP) 3A4 enzyme system, leading to the conclusion that lurasidone should not be used in the presence of strong inducers (e.g., rifampin) or inhibitors (e.g., ketoconazole) of CYP3A4. Lurasidone does show a food effect. A study examining food effects on lurasidone concentrations found that taking the drug with meals containing 350 calories or more, with either low or high fat content, led to a doubling of the bioavailability of lurasidone compared with dosing during fasting (Chiu et al. 2010).
The recommended starting dosage of lurasidone is 40 mg/day taken concurrently with at least 350 calories of food. Dosages up to 160 mg/day are currently approved for schizophrenia and up to 120 mg/day for bipolar depression. As previously noted, lurasidone should not be used by patients taking medications that are strong metabolic inducers or inhibitors of CYP3A4. There are no suggested dosage adjustments based on age, gender, ethnicity, or smoking, but individuals with renal or hepatic impairment should not be prescribed dosages greater than 40 mg/day. Lurasidone is currently available in 20-, 40-, 80-, and 120-mg tablets (Sunovion Pharmaceuticals 2013).
Lurasidone lacks a requirement for initial dosage titration and appears to require minimal adjustment and tinkering. Having a starting dose with substantial efficacy is a strong point for many patients. Food effects are an issue, given that optimal exposure requires the medication to be taken with at least 350 calories of food (with no minimum fat content specified); however, the lack of a need for titration and the uncomplicated requirements for suitable meals will make it easier to apply this treatment to patients who may be challenged in their ability to adhere to complex regimens.
Efficacy and Tolerability
Pivotal Registration Trials in Schizophrenia
In the standard drug development program, lurasidone at daily dosages of 40 mg, 80 mg, and 120 mg was compared with placebo in four separate studies (Meltzer et al. 2011; Nakamura et al. 2009; Nasrallah et al. 2013; Ogasa et al. 2013), with several different dosing and comparator strategies. A fifth study (Loebel et al. 2013) added a 160-mg/day dosage. Citrome (2011a, 2011b) reviewed data based on conference presentations for the schizophrenia development program. Patients ranged in age from 18 to 74 years and were symptomatic with an acute exacerbation of psychosis. In the early clinical studies, the dosage that most consistently separated from placebo was 80 mg/day, although 40 mg/day and 120 mg/day did as well in some trials. Lurasidone at 120 mg/day did not confer additional clinical benefit on the primary outcomes—improved scores on either the Positive and Negative Syndrome Scale (PANSS) or the Brief Psychiatric Rating Scale (BPRS)—across the different studies. However, clinical data submitted to the FDA led to an increase in the approved dosage to a maximum of 160 mg/day.
Comparative Efficacy Studies
Schizophrenia
Four blinded and randomized studies compared lurasidone with other agents in the treatment of schizophrenia.
In the first study (Potkin et al. 2011), lurasidone was compared with ziprasidone in a 3-week randomized trial in 301 patients with schizophrenia. Both treatments improved symptoms as measured by the PANSS, and there was no significant difference in endpoint PANSS scores.
In the second study (Meltzer et al. 2011), lurasidone was compared with olanzapine in clinically unstable patients with schizophrenia who had been admitted to inpatient care. Both olanzapine and lurasidone were superior to placebo for clinical response. In addition, the weight gain with olanzapine was significantly greater than that with either lurasidone or placebo, whereas rates of akathisia were significantly higher in the lurasidone group compared with the other two groups.
In the third study (Loebel et al. 2013), two dosages of lurasidone (80 and 160 mg/day) were compared with quetiapine extended release (XR) 600 mg/day and placebo in inpatients experiencing an acute exacerbation of schizophrenia. Both lurasidone (at both dosages) and quetiapine separated from placebo, and weight gain and sedation/sleepiness were more frequent with quetiapine than with either dosage of lurasidone.
In the fourth study (Citrome et al. 2012), clinically stable patients with schizophrenia were randomly assigned to receive either risperidone or lurasidone and were followed for 12 months to assess potential differences in long-term safety. Findings included greater weight gain with risperidone, minimal differences between lurasidone and risperidone in efficacy, and no differences between the two agents in relapse rates. All-cause discontinuation rates were higher for lurasidone, possibly due to slight elevations in nausea in the lurasidone group.
Bipolar Depression
Two randomized placebo-controlled trials of lurasidone were conducted in patients with bipolar depression. In the first study (Loebel et al. 2014a; monotherapy), lurasidone at two different dosage ranges (20–60 mg/day and 80–120 mg/day) was compared with placebo. Both dosage ranges separated from placebo, with similar effect sizes. In the second study (Loebel et al. 2014b; adjunctive therapy), lurasidone at 20–120 mg/day was added to stable treatment with either valproate or lithium. Statistically significant separation from placebo was found. Lurasidone treatment was administered at a mean modal dose of 75 mg/day, which translates to an available dose of 80 mg/day. The results of these two studies led to lurasidone’s approval by the FDA for both augmentation of lithium or valproate therapy and monotherapy of bipolar depression in June 2013.
In an additional post hoc analysis of the results of the monotherapy study, McIntyre et al. (2015) reported that lurasidone was effective in the treatment of bipolar depression with mixed features, an entity newly defined in DSM-5. The presence of mixed features was defined as having a Young Mania Rating Scale (YMRS; Young et al. 1978) score of 4 or greater. Fifty-six percent of the patients in the study were found to have mixed features (272 out of 485 patients). Of the patients with mixed features, 182 received treatment with active lurasidone and 90 received placebo treatment. Efficacy for the treatment of depression in patients with and without mixed features was essentially equivalent: 15.7-point decreases in Montgomery-Åsberg Depression Rating Scale (MADRS; Montgomery and Åsberg 1979) scores were seen for patients without mixed features, and 15.2-point decreases were found for those with mixed features. Eighty-two percent of the patients without mixed features completed the trial when treated with active lurasidone, and 73% of the patients with mixed features completed the study with active treatment. These data indicate that the presence of mixed features in bipolar depression should not be viewed as a contraindication to treatment with lurasidone.
In a very recent study (Suppes et al. 2016), lurasidone was tested for efficacy in major depression with mixed features. This newly defined condition is characterized by the coexistence within a major depressive episode of a limited set of manic symptoms (American Psychiatric Association 2013). Patients selected for the presence of DSM-IV-TR (American Psychiatric Association 2000)–defined major depressive disorder and two or three manic symptoms were randomly assigned to lurasidone (n=109) or placebo (n=100) for a 6-week trial. Lurasidone was superior to placebo, leading to a 20.5-point change on the MADRS for active treatment compared with a 13-point change for placebo (P<0.001; effect size d=.80). Completion rates were similar for active treatment and placebo (94% and 85%, respectively), and the remission rate was 49% for active treatment. Switch into mania did not occur with lurasidone treatment, and patients who received lurasidone manifested a 7-point decrease in their YMRS scores. These data suggest efficacy for lurasidone in the treatment of depression with mixed features as well as bipolar depression.
Summary of Efficacy and Tolerability Data
The risk–benefit evaluation for lurasidone suggests a lower potential for metabolic consequences and QTc prolongation combined with a slightly higher risk of extrapyramidal side effects (EPS) and akathisia compared with some of the other atypical antipsychotic medications. Prolactin elevation appears to be minimal within the approved dosage range. Given our limited clinical experience with lurasidone, it may be premature to target an optimal patient for this medication; however, the reduced metabolic consequences of lurasidone would seem to be a very strong point. Patients who are extraordinarily vulnerable to EPS may require close monitoring.
Lurasidone’s efficacy in schizophrenia relative to other agents has been examined in four active comparison studies (Citrome et al. 2012; Loebel et al. 2013; Meltzer et al. 2011; Potkin et al. 2011), none of which found lurasidone to be inferior. It is not yet possible to assess lurasidone’s relative efficacy in bipolar depression, given the absence of comparative trials to date.
Side Effects and Safety
Class Warnings
The typical class warnings are present on the lurasidone label (Sunovion Pharmaceuticals 2013), including the black box warning about increased stroke risk in elderly individuals and a variety of other class warnings regarding neuroleptic malignant syndrome, tardive dyskinesia, diabetes, hyperlipidemia, weight gain, glucose abnormalities, hyperprolactinemia, agranulocytosis, suicide, and seizures. Lurasidone has no warning for QTc alteration; a dedicated cardiac safety study (referenced in the package insert) found no evidence of QTc prolongation with lurasidone treatment.
Adverse-Event Reports
Safety information is available from the manufacturer’s safety database (see also www.sunovionprofile.com/sp/latuda-bp.html). Dose-related adverse effects that separated from placebo included somnolence, akathisia, and EPS (as measured by total scores on clinical rating scales for EPS). Of note, weight and metabolic parameters were only minimally affected in patients with schizophrenia or bipolar depression in clinical trials. Although short-term changes in cholesterol, triglycerides, and glucose are likely to be attributable to transition from medications with more substantial adverse profiles in these domains, the weight-gain data for lurasidone are very noticeable and consistent.
Promising Features
Favorable Metabolic Profile
Lurasidone appears to have the promise of weight neutrality. Weight gain in the pooled 6-week studies across doses was 0.75 kg; in the pooled 12-month database from extension studies, patients lost an average of 0.4 kg (Meyer et al. 2015). These statistics compare favorably with those for other antipsychotics in wide clinical use (see review by Citrome 2011b). It is important to note that specific populations outside the current label may have a greater weight-gain risk compared with the typical patient with chronic schizophrenia in these trials. Data are not yet available for lurasidone’s profile in the long-term treatment of bipolar depression. Nevertheless, the suggestion of no weight gain after a year’s treatment, even for patients who may have gained weight with previous treatments, is quite promising.
Potential Cognitive Benefits
Basic Science Rationale
Compounds that interact with the 5-HT7 receptor as their primary binding profile have historically been shown to produce beneficial cognitive effects in animal models (Ballaz et al. 2007). Furthermore, it is postulated that agents with partial agonist properties at the 5-HT1A receptor may have potential benefit in regard to reduction of flat affect and related negative symptoms in schizophrenia (Newman-Tancredi 2010).
MK-801 is a glutamate receptor antagonist that is used to induce cognitive impairments in healthy individuals that are quite similar to those seen in schizophrenia. Like other N-methyl-D-aspartate (NMDA) antagonists, MK-801 is capable of inducing deficits in memory and problem solving. Given that NMDA antagonists such as ketamine and phencyclidine can induce a reliable analog of schizophrenia in healthy people (and exacerbate psychosis in patients with schizophrenia), such manipulations have more intrinsic validity than cholinergic manipulations such as scopolamine challenge. In rats, lurasidone has shown the potential to reverse MK-801–induced learning and memory deficits in the passive avoidance test (Ishiyama et al. 2007) and the Morris water maze (Enomoto et al. 2008).
Research using analogs of cognitive impairment derived from animal models has notoriously failed to yield paradigms with adequate translational relevance to the specific cognitive domains affected in schizophrenia, particularly in terms of reliably predicting beneficial cognitive effects associated with pharmacological treatment (Harvey 2009). A possible reason for this failure may be that the adverse influences on human cognition of dopamine D2 receptor antagonism associated with antipsychotic treatment may override the influences of a “secondary” receptor profile, preventing its beneficial effects from being realized (Harvey and McClure 2006). For example, ziprasidone, a partial agonist at the 5-HT1A receptor, has never demonstrated greater cognitive benefit versus antipsychotics that do not interact with that receptor (e.g., olanzapine; Harvey et al. 2004). Thus, clear evidence of cognitive enhancement in patients with schizophrenia treated with the medication of interest, compared with other treatments in similar populations, is the “bottom line” requirement for demonstration of meaningful cognitive benefit.
Studies in Schizophrenia
Three published studies in patients with schizophrenia have addressed the issue of lurasidone’s cognitive benefit compared with that of other antipsychotics (Harvey et al. 2011, 2013, 2015).
The first study, which was conducted during the early development phases of lurasidone, was a 3-week double-blind, randomized head-to-head comparison of lurasidone versus ziprasidone in generally clinically stable outpatients with schizophrenia (Harvey et al. 2011). At the time this study was conducted, no U.S. patients had ever been exposed to lurasidone. Patients were selected for being naive to treatment with ziprasidone as well. The study examined changes in performance on a neuropsychological assessment consisting of most of the tests in the widely used Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Consensus Cognitive Battery (MCCB; Nuechterlein et al. 2008) and an interview-based assessment of cognitive functioning, the Schizophrenia Cognition Rating Scale (SCoRS; Keefe et al. 2006). The study found that lurasidone was associated with improvements on neuropsychological tests that were generally consistent with practice effects (Harvey et al. 2011). There was one exception, processing speed, which manifested relatively greater improvement with lurasidone than with ziprasidone. However, improvements seen with lurasidone on the SCoRS were double the size of improvements seen on the neuropsychological assessments and nearly significantly larger than the improvements associated with ziprasidone. These results cannot be attributed to practice effects, given that the SCoRS is an interview, not a performance-based measure. Furthermore, the fact that the differential effects of lurasidone and ziprasidone were nearly significant (P<0.06) argues against a generalized bias effect, because the lurasidone effects were clearly larger.
The second study (Harvey et al. 2013) compared two dosages of lurasidone (80 and 160 mg/day) with 600 mg/day of quetiapine XR and placebo. This double-blind, placebo-controlled trial was conducted in patients experiencing an acute exacerbation of psychosis. Lurasidone 160 mg/day was compared with placebo, quetiapine XR, or lurasidone 80 mg/day over a 6-week period, followed by a 6-month double-blind extension. Follow-ups were conducted at 3 and 6 months, and placebo patients were switched to lurasidone at flexible dosages; quetiapine XR patients remained on the same treatment. The CogState Computerized Cognitive Battery (Pietrzak et al. 2009) and the University of California San Diego (UCSD) Performance-based Skills Assessment—Brief version (UPSA-B; Mausbach et al. 2007; Patterson et al. 2001) were administered at baseline and at each assessment point. When patients who provided invalid baseline CogState data were censored from the analysis, lurasidone at 160 mg/day separated from placebo on composite cognitive improvement at the 6-week endpoint, whereas lurasidone at 80 mg/day and quetiapine XR did not.
Harvey et al. (2015) presented an analysis of the dose–response relationships of lurasidone compared with quetiapine during the full 6-month duration of the trial. The full sample, regardless of the validity of baseline performance, was examined at two follow-up assessments (at 3 and 6 months). Both dosages of lurasidone were found to be superior to quetiapine XR at both assessments (Harvey et al. 2015). Scores on the UPSA-B improved with all active treatments at each of the assessment time points, with no between-group differences in improvements.
Although these results clearly require replication, they suggest that lurasidone may have beneficial cognitive effects. In all three studies, performance- and interview-based assessments of functionally relevant cognitive processes showed treatment-related improvements. In the Harvey et al. (2013) study, the performance-based cognitive assessments also showed improvements that were superior to those seen with placebo or the active comparator. This superiority to the comparator was confirmed across all dosages of lurasidone in the Harvey et al. (2015) study. The sleepiness-inducing effects of quetiapine XR may have contributed to the difference between this compound and lurasidone (Loebel et al. 2014c); however, that circumstance would not have explained the separation of lurasidone from placebo.
Conclusion
Lurasidone is a new antipsychotic with some benefits compared with other available medications, including low weight-gain propensity and reduced risk for metabolic side effects. Little of the published data have been supported by sources other than the sponsor of the medication. We will watch this medication carefully to continue to determine its benefit over time. Since the previous edition of this textbook, the indication for bipolar depression has been added and additional cognitive and long-term safety data have become available. No new safety concerns have emerged, and no new data raising efficacy questions have appeared.
References
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision. Washington, DC, American Psychiatric Association, 2000
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Arlington, VA, American Psychiatric Association, 2013
Ballaz SJ, Akil H, Watson SJ: The 5-HT7 receptor: role in novel object discrimination and relation to novelty-seeking behavior. Neuroscience 149(1):192–202, 2007 17869441
Chiu YY, Preskorn S, Sarubbi D, et al: Effect of food on lurasidone absorption. Poster presented at the NCDEU Meeting, Boca Raton, FL, June 14–17, 2010
Citrome L: Lurasidone for schizophrenia: a brief review of a new second-generation antipsychotic. Clin Schizophr Relat Psychoses 4(4):251–257, 2011a 21177242
Citrome L: Lurasidone for schizophrenia: a review of the efficacy and safety profile for this newly approved second-generation antipsychotic. Int J Clin Pract 65(2):189–210, 2011b 21129135
Citrome L, Cucchiaro J, Sarma K, et al: Long-term safety and tolerability of lurasidone in schizophrenia: a 12-month, double-blind, active-controlled study. Int Clin Psychopharmacol 27(3):165–176, 2012 22395527
Enomoto T, Ishibashi T, Tokuda K, et al: Lurasidone reverses MK-801-induced impairment of learning and memory in the Morris water maze and radial-arm maze tests in rats. Behav Brain Res 186(2):197–207, 2008 17881065
Harvey PD: Pharmacological cognitive enhancement in schizophrenia. Neuropsychol Rev 19(3):324–335, 2009 19507034
Harvey PD, McClure MM: Pharmacological approaches to the management of cognitive dysfunction in schizophrenia. Drugs 66(11):1465–1473, 2006 16906778
Harvey PD, Siu CO, Romano S: Randomized, controlled, double-blind, multicenter comparison of the cognitive effects of ziprasidone versus olanzapine in acutely ill inpatients with schizophrenia or schizoaffective disorder. Psychopharmacology (Berl) 172(3):324–332, 2004 14615877
Harvey PD, Ogasa M, Cucchiaro J, et al: Performance and interview-based assessments of cognitive change in a randomized, double-blind comparison of lurasidone vs. ziprasidone. Schizophr Res 127(1–3):188–194, 2011 21277745
Harvey PD, Siu CO, Hsu J, et al: Effect of lurasidone on neurocognitive performance in patients with schizophrenia: a short-term placebo- and active-controlled study followed by a 6-month double-blind extension. Eur Neuropsychopharmacol 23(11):1373–1382, 2013 24035633
Harvey PD, Siu CO, Ogasa M, Loebel A: Effect of lurasidone dose on cognition in patients with schizophrenia: post-hoc analysis of a long-term, double-blind continuation study. Schizophr Res 166(1–3): 334–338, 2015 26117157
Ishibashi T, Horisawa T, Tokuda K, et al: Pharmacological profile of lurasidone, a novel antipsychotic agent with potent 5-hydroxytryptamine 7 (5-HT7) and 5-HT1A receptor activity. J Pharmacol Exp Ther 334(1):171–181, 2010 20404009
Ishiyama T, Tokuda K, Ishibashi T, et al: Lurasidone (SM-13496), a novel atypical antipsychotic drug, reverses MK-801-induced impairment of learning and memory in the rat passive-avoidance test. Eur J Pharmacol 572(2–3):160–170, 2007 17662268
Keefe RS, Poe M, Walker TM, et al: The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. Am J Psychiatry 163(3):426–432, 2006 16513863
Loebel A, Cucchiaro J, Sarma K, et al: Efficacy and safety of lurasidone 80 mg/day and 160 mg/day in the treatment of schizophrenia: a randomized, double-blind, placebo- and active-controlled trial. Schizophr Res 145(1–3):101–109, 2013 23415311
Loebel A, Cucchiaro J, Silva R, et al: Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry 171(2):160–168, 2014a 24170180
Loebel A, Cucchiaro J, Silva R, et al: Lurasidone as adjunctive therapy with lithium or valproate for the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry 171(2):169–177, 2014b 24170221
Loebel AD, Siu CO, Cucchiaro JB, et al: Daytime sleepiness associated with lurasidone and quetiapine XR: results from a randomized double-blind, placebo-controlled trial in patients with schizophrenia. CNS Spectr 19(2):197–205, 2014c 24330860
Mausbach BT, Harvey PD, Goldman SR, et al: Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull 33(6):1364–1372, 2007 17341468
McIntyre RS, Cucchiaro J, Pikalov A, et al: Lurasidone in the treatment of bipolar depression with mixed (subsyndromal hypomanic) features: post hoc analysis of a randomized placebo-controlled trial. J Clin Psychiatry 76(4):398–405, 2015 25844756
Meltzer HY, Cucchiaro J, Silva R, et al: Lurasidone in the treatment of schizophrenia: a randomized, double-blind, placebo- and olanzapine-controlled study. Am J Psychiatry 168(9):957–967, 2011 21676992
Meyer JM, Mao Y, Pikalov A, et al: Weight change during long-term treatment with lurasidone: pooled analysis of studies in patients with schizophrenia. Int Clin Psychopharmacol 30(6):342–350, 2015 26196189
Montgomery SA, Åsberg M: A new depression scale designed to be sensitive to change. Br J Psychiatry 134:382–389, 1979 444788
Nakamura M, Ogasa M, Guarino J, et al: Lurasidone in the treatment of acute schizophrenia: a double-blind, placebo-controlled trial. J Clin Psychiatry 70(6):829–836, 2009 19497249
Nasrallah HA, Silva R, Phillips D, et al: Lurasidone for the treatment of acutely psychotic patients with schizophrenia: a 6-week, randomized, placebo-controlled study. J Psychiatr Res 47(5):670–677, 2013 23421963
Newman-Tancredi A: The importance of 5-HT1A receptor agonism in antipsychotic drug action: rationale and perspectives. Curr Opin Investig Drugs 11(7):802–812, 2010 20571976
Nuechterlein KH, Green MF, Kern RS, et al: The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165(2):203–213, 2008 18172019
Ogasa M, Kimura T, Nakamura M, Guarino J: Lurasidone in the treatment of schizophrenia: a 6-week, placebo-controlled study. Psychopharmacology (Berl) 225(3): 519–530, 2013 22903391
Patterson TL, Goldman S, McKibbin CL, et al: UCSD Performance-based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull 27(2):235–245, 2001 11354591
Pietrzak RH, Olver J, Norman T, et al: A comparison of the CogState Schizophrenia Battery and the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Battery in assessing cognitive impairment in chronic schizophrenia. J Clin Exp Neuropsychol 31(7):848–859, 2009 19142774
Potkin SG, Ogasa M, Cucchiaro J, Loebel A: Double-blind comparison of the safety and efficacy of lurasidone and ziprasidone in clinically stable outpatients with schizophrenia or schizoaffective disorder. Schizophr Res 132(2–3):101–107, 2011 21889878
Sunovion Pharmaceuticals: Latuda (lurasidone HCl) tablets: prescribing information. Revised July 2013. Available at: http://www.latuda.com/LatudaPrescribingInformation.pdf. Accessed September 8, 2015.
Suppes R, Silva R, Cucchiaro J, et al: Lurasidone for the treatment of major depressive disorder with mixed features: a randomized, double-blind, placebo-controlled study. Am J Psychiatry 173(4): 400–407, 2016 26552942
Young RC, Biggs JT, Ziegler VE, Meyer DA: A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133:429–435, 1978 728692