 smile in response to your smile
smile in response to your smileChances are there have been plenty of changes around your house in the last month (and we’re not just talking diaper changes). Changes in your baby, as he or she progresses from cute-but-unresponsive blob to an increasingly active and alert tiny person (who sleeps a little less and interacts a little more). And changes in you, as you begin feeling less the bungling beginner and more the (semi-)seasoned veteran. After all, you’ve probably got one-handed diapering down pat, you’re a pro at burping (baby), and you can latch that little mouth onto your breast in your sleep (and often do). Of course, that still doesn’t mean you’re home free. While life with baby may be settling into a somewhat more predictable (though exhausting) routine, crying spells, cradle cap, and diaper contents may still be keeping you guessing (and making frequent calls to the doctor). But as your baby and your parental poise grow, you’ll be better equipped to face those everyday challenges without breaking a sweat. It might also help to keep in mind that you’ll be getting a reward this month for all those sleepless nights: your baby’s first truly social smile!
All babies reach milestones on their own developmental time line. If your baby seems not to have reached one or more of these milestones, rest assured, he or she probably will very soon. Your baby’s rate of development is normal for your baby. Keep in mind, too, that skills babies perform from the tummy position can be mastered only if there’s an opportunity to practice. So make sure your baby spends supervised playtime on his or her belly. If you have concerns about your baby’s development, check with the doctor. Premature infants generally reach milestones later than others of the same birth age, often achieving them closer to their adjusted age (the age they would be if they had been born at term), and sometimes later.
By two months, your baby … should be able to:
 smile in response to your smile
smile in response to your smile
By the end of this month, most babies are able to lift their head to a 45-degree angle.
 respond to a bell in some way, such as startling, crying, quieting
respond to a bell in some way, such as startling, crying, quieting
… will probably be able to:
 vocalize in ways other than crying (e.g., cooing)
vocalize in ways other than crying (e.g., cooing)
 on stomach, lift head 45 degrees
on stomach, lift head 45 degrees
… may even be able to:
 hold head steady when upright
hold head steady when upright
 on stomach, raise chest, supported by arms
on stomach, raise chest, supported by arms
 roll over (one way)
roll over (one way)
 grasp a rattle held to backs or tips of fingers
grasp a rattle held to backs or tips of fingers
 pay attention to an object as small as a raisin (but make sure such objects are kept out of baby’s reach)
pay attention to an object as small as a raisin (but make sure such objects are kept out of baby’s reach)
 reach for an object
reach for an object
 say “Ah-goo” or similar vowelconsonant combination
say “Ah-goo” or similar vowelconsonant combination
… may possibly be able to:
 smile spontaneously
smile spontaneously
 bring both hands together
bring both hands together
 on stomach, lift head 90 degrees
on stomach, lift head 90 degrees
 laugh out loud
laugh out loud
 squeal in delight
squeal in delight
 follow an object held about 6 inches above the baby’s face and moved 180 degrees (from one side to the other), with baby watching all the way
follow an object held about 6 inches above the baby’s face and moved 180 degrees (from one side to the other), with baby watching all the way
Each practitioner will have a personal approach to well-baby checkups. The overall organization of the physical exam, as well as the number and type of assessment techniques used and procedures performed, will also vary with the individual needs of the child. But, in general, you can expect the following at a checkup when your baby is about two months old:
 Questions about how you and baby and the rest of the family are doing at home, and about baby’s eating, sleeping, and general progress. About child care, if you are planning to return to work.
Questions about how you and baby and the rest of the family are doing at home, and about baby’s eating, sleeping, and general progress. About child care, if you are planning to return to work.
 Measurement of baby’s weight, length, and head circumference, and plotting of progress since birth.
Measurement of baby’s weight, length, and head circumference, and plotting of progress since birth.
 Physical exam, including a recheck of any previous problems.
Physical exam, including a recheck of any previous problems.
Even healthy babies spend a lot of time at the doctor’s office. Well-baby checkups, which are scheduled every month or two during the first year, allow the doctor to keep track of your baby’s growth and development, ensuring that everything’s on target. But they’re also the perfect time for you to ask the long list of questions you’ve accumulated since your last visit, and to walk away with a wealth of advice on how to keep your “well baby” well.
To make sure you make the most of a well-baby visit:
 Time it right. When scheduling appointments, try to steer clear of nap time, lunchtime, and any time your baby’s typically fussy. And go for an empty waiting room, avoiding peak hours at the doctor’s office, if possible. Mornings are usually quieter because older children are in school—so, in general, a prelunch appointment will beat the four o’clock rush. And if you feel you’ll need extra time (you have even more questions and concerns than usual), ask for it so it can be scheduled into the visit. That way, you won’t feel quite as hurried.
Time it right. When scheduling appointments, try to steer clear of nap time, lunchtime, and any time your baby’s typically fussy. And go for an empty waiting room, avoiding peak hours at the doctor’s office, if possible. Mornings are usually quieter because older children are in school—so, in general, a prelunch appointment will beat the four o’clock rush. And if you feel you’ll need extra time (you have even more questions and concerns than usual), ask for it so it can be scheduled into the visit. That way, you won’t feel quite as hurried.
 Fill’er up. A hungry patient is a cranky and uncooperative patient. So show up for your well-baby visits with a well-fed baby (once finger foods have been started, you can also bring a snack along for the waiting room). Keep in mind, however, that overfilling the tank just before the appointment may mean baby will be ripe for spitting once the exam begins.
Fill’er up. A hungry patient is a cranky and uncooperative patient. So show up for your well-baby visits with a well-fed baby (once finger foods have been started, you can also bring a snack along for the waiting room). Keep in mind, however, that overfilling the tank just before the appointment may mean baby will be ripe for spitting once the exam begins.
 Dress for undressing success. When choosing baby’s wardrobe for the visit, think easy-on, easy-off. Skip outfits with lots of tiny buttons or snaps that take forever to do and undo, or snug clothes that are difficult to pull on and off. And don’t be too quick to undress; if your baby hates being naked, wait until the exam is about to begin before stripping down.
Dress for undressing success. When choosing baby’s wardrobe for the visit, think easy-on, easy-off. Skip outfits with lots of tiny buttons or snaps that take forever to do and undo, or snug clothes that are difficult to pull on and off. And don’t be too quick to undress; if your baby hates being naked, wait until the exam is about to begin before stripping down.
 Write it down. Remember those two hundred questions you wanted to ask the doctor? You won’t, once you’ve spent twenty minutes in the waiting room and another twenty in the exam room trying to keep your baby (and yourself) calm. So instead of relying on your memory, bring a list you can read off. Pack a pen, too, so you can write down the answers to those questions, plus any other advice and instructions the doctor dispenses. You can also use it to record baby’s height, weight, immunizations received that visit, and so on.
Write it down. Remember those two hundred questions you wanted to ask the doctor? You won’t, once you’ve spent twenty minutes in the waiting room and another twenty in the exam room trying to keep your baby (and yourself) calm. So instead of relying on your memory, bring a list you can read off. Pack a pen, too, so you can write down the answers to those questions, plus any other advice and instructions the doctor dispenses. You can also use it to record baby’s height, weight, immunizations received that visit, and so on.
 Make baby comfortable. Few babies enjoy the poking and prodding of a doctor’s exam—but most enjoy it even less when it takes place on a cold, uncomfortable exam table. Ask the doctor if he or she can perform most of the exam while baby’s on your lap.
Make baby comfortable. Few babies enjoy the poking and prodding of a doctor’s exam—but most enjoy it even less when it takes place on a cold, uncomfortable exam table. Ask the doctor if he or she can perform most of the exam while baby’s on your lap.
 Trust your instincts. Your doctor sees your baby only once a month—you see your baby every day. Which means that you may notice subtle things the doctor doesn’t. If you feel something isn’t right with your child—even if you’re not sure what it is—make sure the doctor knows. Remember, you don’t need a medical degree to be a valuable partner in your baby’s health care. Sometimes the keenest diagnostic tool is a parent’s intuition.
Trust your instincts. Your doctor sees your baby only once a month—you see your baby every day. Which means that you may notice subtle things the doctor doesn’t. If you feel something isn’t right with your child—even if you’re not sure what it is—make sure the doctor knows. Remember, you don’t need a medical degree to be a valuable partner in your baby’s health care. Sometimes the keenest diagnostic tool is a parent’s intuition.
 Developmental assessment. The examiner may actually put baby through a series of “tests” to evaluate head control, hand use, vision, hearing, and social interaction or may simply rely on observation plus your reports on what baby is doing.
Developmental assessment. The examiner may actually put baby through a series of “tests” to evaluate head control, hand use, vision, hearing, and social interaction or may simply rely on observation plus your reports on what baby is doing.
 Immunizations, if baby is in good health and there are no other contraindications. See recommendations, page 226.
Immunizations, if baby is in good health and there are no other contraindications. See recommendations, page 226.
 Guidance about what to expect in the next month in relation to such topics as feeding, sleeping, and development, and advice about infant safety.
Guidance about what to expect in the next month in relation to such topics as feeding, sleeping, and development, and advice about infant safety.
Questions you may want to ask, if the doctor hasn’t already answered them:
 What reactions, if any, can you expect baby to have to the immunizations? How should you treat them? Which reactions should you call about?
What reactions, if any, can you expect baby to have to the immunizations? How should you treat them? Which reactions should you call about?
Also raise concerns that have come up over the past month about baby’s health, feeding issues, or family adjustment. Jot down information and instructions from the doctor. Record all pertinent information (baby’s weight, length, head circumference, birthmarks, immunizations, illnesses, medications given, test results, and so on) in a permanent health record.
Sure, breastfeeding’s ideal—the very best way to feed a baby. But as easy and practical as it is (now that you’ve, hopefully, gotten the hang of it), it does have its limitations, the most significant one being: You can’t breastfeed your baby unless you’re with your baby.
In some cultures, mothers and babies are never farther than a baby sling apart, making round-the-clock Breastfeeding not just doable but incredibly efficient, and making introducing the bottle completely unnecessary. But in our culture, even young babies are often apart from their mothers at a long enough distance and for a long enough time to require one or more supplementary feedings (that is, the replacement of breastfeeding sessions with a bottle of either expressed breast milk or formula).
Not bringing on the bottle? That’s fine too; there’s no rule that says a baby must be introduced to the bottle. There are a number of reasons some mothers choose to keep their babies bottle free:
 They have a baby who rejects the bottle. Mothers who don’t have a compelling reason to supplement may then choose not to push the bottle agenda.
They have a baby who rejects the bottle. Mothers who don’t have a compelling reason to supplement may then choose not to push the bottle agenda.
 Concern that if baby becomes dependent on a bottle, weaning will have to be accomplished twice: first from the breast, then from the bottle. These mothers usually start their babies on a cup as soon as they can sit supported, and use a cup for supplementary feedings of breast milk, and later for other drinks.
Concern that if baby becomes dependent on a bottle, weaning will have to be accomplished twice: first from the breast, then from the bottle. These mothers usually start their babies on a cup as soon as they can sit supported, and use a cup for supplementary feedings of breast milk, and later for other drinks.
MYTH: Supplementing with formula (or adding cereal to a bottle) will help baby sleep through the night.
Reality: Babies sleep through the night when they are developmentally ready to do so. Bringing on bottles of formula or introducing cereal prematurely won’t make that bright day (the one when you’ll wake up realizing you had a full night’s sleep) dawn any faster. Researchers have found no relationship between nighttime food and sleep.
MYTH: Breast milk alone isn’t enough for my baby.
Reality: Exclusively breastfeeding your baby for six months provides him with all the nutrients he needs. After six months, a combo of breast milk and solids can continue nourishing your growing baby well without adding formula.
MYTH: Giving formula to my baby won’t hurt my milk supply.
Reality: Any time you give something other than breast milk to your baby (formula or solid food), your milk supply diminishes. The less breast milk your baby takes, the less milk your breasts make. But waiting until breastfeeding is well established can minimize the effect supplementary bottles of formula have on lactation.
Though plenty of mothers choose not to introduce the bottle at all, and can manage to stick close enough to baby enough of the time that they don’t ever have to, most do introduce a bottle at some point (so they can have an occasional afternoon or evening away from baby, because they’re going back to work, or because the baby is not gaining sufficient weight on breast milk alone, for instance).
Even if you don’t plan on giving bottles regularly, it may be a good idea to express and freeze enough breast milk to fill six bottles—just in case. This will give you a backup supply if you become sick, you’re temporarily taking medication that might pass into your milk, or you’re called out of town unexpectedly. Even if your baby has never taken a bottle, it may be easier for him or her to accept one if it’s filled with familiar breast milk rather than with unfamiliar formula. See page 162 for freezer time limits on breast milk; as batches of the emergency cache expire, you may need to replace them with fresh ones.
Breast milk. Filling a bottle with expressed breast milk is usually uncomplicated (once you’ve mastered the art of pumping) and allows a mother to feed her baby a breast milk–only diet—even when she and baby are apart. (To avoid nipple confusion, wait until breastfeeding is well established before bringing on the bottle; see page 91).
Formula. Supplementing with formula, while obviously as easy as opening a can, may have drawbacks if started too early on in the breastfeeding relationship. When lactation is going well, a bottle of formula can interfere with the breast milk supply and actually create problems where there weren’t any. When lactation isn’t going well, a bottle of formula can make existing problems even worse. Once breastfeeding is well established (usually around six to eight weeks), however, many women find they can successfully combine breastfeeding and formula feeding (see page 90).
Ready to offer that first bottle? If you’re lucky, baby will take to it like an old friend—eagerly latching on and lapping up the contents. Or, maybe more realistically, he or she may take a little time to get warmed up to this unfamiliar food source. Keeping these tips in mind will help win baby over:
 Time it right. Wait until your baby is both hungry (but not frantically so) and in a good mood before attempting to initiate the bottle.
Time it right. Wait until your baby is both hungry (but not frantically so) and in a good mood before attempting to initiate the bottle.
 Hand it over. The first few bottles are more likely to be accepted if they are offered by someone other than you—preferably when you’re not in the same room for baby to complain to. The substitute feeder should cuddle and talk to the baby during the feeding, just as you would when nursing.
Hand it over. The first few bottles are more likely to be accepted if they are offered by someone other than you—preferably when you’re not in the same room for baby to complain to. The substitute feeder should cuddle and talk to the baby during the feeding, just as you would when nursing.
 Keep it covered. If you have to offer that first bottle yourself, it may help to keep your breasts well camouflaged (don’t try to bottle feed braless or in a low-cut blouse; think heavy sweaters instead) and to distract the baby with background music, a toy, or another form of entertainment. Too much distraction, however, and your baby may want to play, not drink.
Keep it covered. If you have to offer that first bottle yourself, it may help to keep your breasts well camouflaged (don’t try to bottle feed braless or in a low-cut blouse; think heavy sweaters instead) and to distract the baby with background music, a toy, or another form of entertainment. Too much distraction, however, and your baby may want to play, not drink.
 Pick the right nipple. If your baby tries out the nipple, then drops it with seeming disapproval, try a different type of nipple or warm it first the next time. For a baby who uses a pacifier, a nipple that is similar in shape may work.
Pick the right nipple. If your baby tries out the nipple, then drops it with seeming disapproval, try a different type of nipple or warm it first the next time. For a baby who uses a pacifier, a nipple that is similar in shape may work.
 Be a sneak. If you’re meeting resistance to the bottle, sneak it in during sleep. Have your bottle giver pick up your sleeping baby and try to give the bottle then. In a few weeks baby may accept the bottle when awake.
Be a sneak. If you’re meeting resistance to the bottle, sneak it in during sleep. Have your bottle giver pick up your sleeping baby and try to give the bottle then. In a few weeks baby may accept the bottle when awake.
Some women choose not to supplement with formula for other reasons, including the desire to breastfeed for the recommended one year or longer (studies show a significant relationship between formula supplementation and early weaning) and to prevent or delay allergy from cow’s milk formula when there’s a family history of allergies.
Don’t have enough expressed milk to make up a complete bottle? No need to throw all that hard work down the drain. Instead, mix formula with the expressed milk to fill the bottle. Less waste—and your baby will be getting enzymes from the breast milk that will help digest the formula better.
When to begin. Some babies have no difficulty switching from breast to bottle and back again right from the start, but most do best with both if the bottle isn’t introduced until at least three weeks, preferably five weeks. Earlier than this, bottle feedings may interfere with the successful establishment of breastfeeding, and babies may experience nipple confusion because dining at breast and bottle call for different sucking techniques. Much later than this, many babies reject rubber nipples in favor of their beloved mama’s familiar fleshy ones.
Occasionally, formula supplementation is recommended because baby isn’t doing well on breast milk alone. This often leaves a mother feeling conflicted. On the one hand, she hears that giving a bottle in such a situation may totally wipe out her chances of breastfeeding successfully; on the other, she’s told by the doctor that if she doesn’t start supplementing her baby’s diet with formula, the health consequences could be serious. The best solution in many such cases is the supplemental nutrition system, shown on page 167, which provides a baby with the formula he or she needs to begin thriving, while stimulating mom’s breasts to produce more breast milk.
How much breast milk or formula to use. One of the beauties of breastfeeding is that baby eats to appetite, not to a specified number of ounces you’re pushing. As soon as you start using a bottle, it’s easy to succumb to the numbers game. Resist. Tell your baby’s care provider (and yourself) to give your baby only as much as he or she wants, with no prodding to finish any particular amount. The average nine-pounder may take as much as 6 ounces at a feeding, or less than 2.
Getting baby used to the bottle. If your schedule will require your regularly missing two feedings during the day, switch to the bottle one feeding at a time, starting at least two weeks before you plan to go back to work. Give your baby a full week to get used to the single bottle feeding before moving on to two. This will help not only baby but also your body adjust gradually, if you are planning to supplement with formula rather than breast milk. The wonderful supply-and-demand mechanism that controls milk production will cut back as you do, making you more comfortable when you’re finally back on the job.
Keeping yourself comfortable. If you plan to give a bottle only occasionally, nursing thoroughly on (or expressing from) both breasts before going out will make fullness and leakage less of a problem. Be sure your baby won’t be fed too close to your return (less than two hours is probably too close) so that if you are uncomfortably full, you can nurse as soon as you get home.
Whether you choose to supplement with breast milk or formula, you should keep in mind that it will probably be necessary for you to express milk if you will be away from your baby for more than three or four hours, to help prevent clogging of milk ducts, leaking, and a diminishing milk supply. The milk can be either collected and saved for future feedings or disposed of.
“My son is five weeks old, and I thought he would be smiling real smiles by now, but he doesn’t seem to be.”
Cheer up. Even some of the happiest babies don’t start true social smiling until six or seven weeks of age. And once they start smiling, some are just naturally more smiley than others. You’ll be able to distinguish the first real smile from those tentative practice ones by the way the baby uses his whole face—not just his mouth. Though babies don’t smile until they’re ready, they’re ready faster when they’re talked to, played with, and cuddled a lot. So smile at your baby and talk to him often, and very soon he’ll be matching you grin for grin.
Think those adorable “ba-ba-ba”s are just baby babble? They’re actually the beginnings of spoken language—baby’s first attempts at figuring out how the other half (the adult half, that is) speaks. But here’s an interesting baby factoid that researchers (who have spent a great deal of time studying what comes out of the mouths of babes) have uncovered: These early articulations of language typically come out of the right side of baby’s mouth (the side controlled by the left side of the brain, the hemisphere that’s in charge of language). When babies babble just for pleasure’s sake (not for language practice), they get the whole mouth moving. When they smile, they apparently use the left side of the mouth (which is mission control for emotions).
But before you try this at home with your baby, here’s something else you need to know: The differences in mouth movements are so subtle that you’d have to have a Ph.D. in linguistics to distinguish a left movement from a right. So leave such analyses to the folks in the lab. Instead, sit back and enjoy all those adorable sounds—no matter which side of baby’s mouth they come out of.
“My six-week-old baby makes a lot of breathy vowel sounds but no consonants at all. Is she on target speechwise?”
With young babies, the “ayes”—and the a’s, e’s, o’s, and u’s—have it. It’s the vowel sounds they make first, somewhere between the first few weeks and the end of the second month. At first the breathy, melodic (and adorable) cooing and throaty gurgles seem totally random, and then you’ll begin to notice they’re directed at you when you talk to your baby, at a stuffed animal who’s sharing her play yard, at a mobile beside her that’s caught her eye, at her own reflection in the crib mirror, or even at a duck on the bumper. These vocal exercises are often practiced as much for her own pleasure as for yours; babies actually seem to love listening to their own voices. In the process, baby is also making verbal experiments and discovering which combinations of throat, tongue, and mouth actions make what sounds.
For mommy and daddy, cooing is a welcome step up from crying on the communication ladder. And it’s just the beginning. Within a few weeks to a few months, baby will begin adding laughing out loud (usually by three and a half months), squealing (by four and a half months), and a few consonants to her repertoire. The range for initiating consonant vocalizations is very broad—some make a few consonant-like sounds in the third month, others not until five or six months, though four months is about average.
When babies begin experimenting with consonants, they usually discover one or two at a time, and repeat the same single combination (ba or ga or da) over and over and over. The next week, they may move on to a new combination, seeming to have forgotten the first. They haven’t, but since their powers of concentration are limited, they usually work on mastering one thing at a time. They also love repetition.
The roads to communication with a baby are endless, and each parent travels some more than others. Here are some you may want to take, now or in the months ahead:
Do a running commentary. Don’t make a move, at least when you’re around your baby, without talking about it. Narrate the dressing process: “Now I’m putting on your diaper … here goes the T-shirt over your head … now I’m buttoning your overalls.” In the kitchen, describe the washing of the dishes, or the process of seasoning the pasta sauce. During the bath, explain about soap and rinsing, and that a shampoo makes the hair shiny and clean. It doesn’t matter that your baby hasn’t the slightest inkling of what you’re talking about. Blow-by-blow descriptions help get you talking and baby listening—thereby starting him or her on the path to understanding.
Ask a lot. Don’t wait until your baby starts having answers to start asking questions. Think of yourself as a reporter, your baby as an intriguing interviewee. The questions can be as varied as your day: “Would you like to wear the red pants or the green overalls?” “Isn’t the sky a beautiful blue today?” “Should I buy green beans or broccoli for dinner?” Pause for an answer (one day your baby will surprise you with one), and then supply the answer yourself, out loud (“Broccoli? Good choice”).
Give baby a chance. Studies show that infants whose parents talk with them rather than at them learn to talk earlier. Give your baby a chance to get in a coo, a gurgle, or a giggle. In your running commentaries, be sure to leave some openings for baby’s comments.
Keep it simple—some of the time. Though right now your baby would probably derive listening pleasure from a dramatic recitation of the Gettysburg Address or an animated assessment of the economy, as he or she gets a bit older, you’ll want to make it easier to pick out individual words. So at least part of the time, make a conscious effort to use simple sentences and phrases: “See the light,” “Bye-bye,” “Baby’s fingers, baby’s toes,” and “Nice doggie.”
Put aside pronouns. It’s difficult for a baby to grasp that “I” or “me” or “you” can be mommy, or daddy, or grandma, or even baby—depending on who’s talking. So most of the time, refer to yourself as “mommy” or “daddy” (or “grandma”) and to your baby by name: “Now Daddy is going to change Amanda’s diaper.”
Raise your pitch. Most babies prefer a high-pitched voice, which may be why women’s voices are usually naturally higher-pitched than men’s, and why most mothers’ (and fathers’) voices climb an octave or two when addressing their infants. Try raising your pitch when talking directly to your baby, and watch the reaction. (A few infants prefer a lower pitch; experiment to see which appeals to yours.)
Bring on the baby talk … or not. If the silly stuff (“Who’s my little bunny-wunny?”) comes naturally to you, babble away in baby talk. If it doesn’t, feel free to skip it (see next page). If you’re big on baby talk, don’t forget to throw some correct, more adult English into your conversations with your infant, too, so that he or she won’t grow up thinking all words end with a y or ie.
Stick to the here and now. Though you can muse about almost anything to your baby, there won’t be any noticeable comprehension for a while. As comprehension does develop, you will want to stick more to what the baby can see or is experiencing at the moment. A young baby doesn’t have a memory for the past or a concept of the future.
Imitate. Babies love the flattery that comes with imitation. When baby coos, coo back; when he or she utters an “Ahh,” utter one, too. Imitation will quickly become a game that you’ll both enjoy, and which will set the foundation for baby’s imitating your language—it will also help build self-esteem (“What I say matters!”).
Set it to music. Don’t worry if you can’t carry a tune—little babies are notoriously undiscriminating when it comes to music. They’ll love what you sing to them whether it’s a current hit, an old favorite from high school, or just some nonsense you’ve set to a familiar tune. If your sensibilities (or your neighbors’) prohibit a song, then singsong will do. Most nursery rhymes entrance even young infants (invest in an edition of Mother Goose if your memory fails you). And accompanying hand gestures, if you know some or can make some up, double the delight. Your baby will quickly let you know which are favorites, and which you’ll be expected to sing over and over—and over—again.
Read aloud. Though at first the words will have no meaning to baby, it’s never too early to begin reading some simple rhyming stories or board books out loud. When you aren’t in the mood for baby talk and crave some adult-level stimulation, share your love of literature (or recipes or gossip or politics) with your little one by reading what you like to read, aloud.
Take your cues from baby. Incessant chatter and song can be tiresome for anyone, even an infant. When your baby becomes inattentive to your wordplay, closes or averts his or her eyes, becomes fussy or cranky, or otherwise indicates the verbal saturation point has been reached, give it a rest.
Following the two-syllable, one-consonant sounds (a-ga, a-ba, a-da) come singsong strings of consonants (da-da-dada-da-da) called “babble,” at six months on the average. By eight months, many babies can produce word-like double consonants (da-da, ma-ma, ha-ha), usually without associating any meaning with them until two or three months later. (To fathers’ delight and mothers’ dismay, dada generally comes before mama.) Mastery of all the consonants doesn’t come until much later, often not until four or five years of age—occasionally even later.
“Our baby doesn’t seem to make the same kind of cooing sounds that his older brother made at six weeks. Should we be concerned?”
Some normal babies develop language skills earlier than average, some later. About 10 percent of babies start cooing before the end of the first month and another 10 percent don’t start until nearly three months, the rest somewhere in between. Some start with strings of consonants before the 4½-month mark; others don’t string consonants until past 8 months. The early verbalizers may end up very strong in language skills (though the evidence isn’t that clear); those who lag far behind, in the lowest 10 percent, may have a physical or developmental problem, but this isn’t clear either. Certainly, it’s too early to be concerned that this might be the case with your baby, since he’s still well within the norm.
If it seems to you over the next several months that your baby consistently, in spite of your encouragement, falls far below the monthly milestones in each chapter, speak to his doctor about your concerns. A hearing evaluation or other tests may be in order. It may turn out that you are so busy that you aren’t really noticing your baby’s vocal achievements (this sometimes happens with second children)—or that everyone else in the household (including his older brother) is making so much noise he can’t get a coo in edgewise. In the less likely case that there actually is a problem, early intervention is often able to remedy it.
“Other parents seem to know how to talk to their babies. But I don’t know what to say to my six-week-old, and when I try, I feel like an absolute idiot. I’m afraid that my inhibitions will slow down his language development.”
They’re tiny. They’re passive. They can’t talk back. And, yet, for many novice mothers and fathers, newborn babies are the most intimidating audience they’ll ever face. The undignified, high-pitched baby talk that seems to come naturally to other parents eludes them, leaving them tonguetied—and feeling guilty over the awkward silence that envelops the nursery.
Though your baby will learn your language even if you never learn his, his speech will develop faster and better if you make a conscious effort at early communication. Babies who aren’t communicated with at all suffer not just in language development but in all areas of growth. But that rarely happens. Even the parent who is bashful about baby talk communicates with his or her baby all day long—while cuddling him, responding to his crying, singing him a lullaby, saying, “It’s time for a walk,” or muttering, “Oh, not the phone again.” Parents teach language when they talk to each other as well as when they talk to their baby; babies pick up almost as much from secondhand dialogue as they do when they’re part of a conversation.
So although it’s not likely that your baby is going to spend the next year in the company of a silent parent, there are ways to expand your baby-word power, even if you’re the kind of adult to whom baby talk doesn’t come naturally. The trick is to start practicing in private, so the embarrassment of gurgling and babbling to your baby in front of other adults won’t cramp your conversation style. If you don’t know where to begin, use the tips on the previous page as a guideline. As you grow more comfortable with baby talk, you’ll likely find yourself slipping into it unawares, even in the company of adults (“Doesn’t that risotto look yummy-yummy for the tum-tummy?”).
“My wife is French, and she wants to speak French to our baby exclusively; I speak English. I think it would be wonderful for our daughter to speak a second language, but wouldn’t it be confusing at this age?”
Because fluency in another language isn’t necessary to function and succeed in most parts of our country (as it is elsewhere), Americans are sadly lagging behind the rest of the world in the ability to converse in anything other than their own native tongue. It’s generally agreed that teaching a child a second language gives her an invaluable skill, and may help her to think in different ways, possibly even improving her future academic performance in other areas. If the language is one that her forebears spoke or some of her relatives speak, it also gives her a significant link with her roots.
There is less agreement on just when to introduce the second language, however. Most experts suggest beginning as soon as a baby is born so that the second language is “acquired” along with the first, not “learned,” as it would be when introduced later. Others believe that this puts the child at a disadvantage in both languages—though probably for only a short time. They generally recommend waiting until a child is two and a half or three before putting on the Berlitz. By this time she usually has a pretty good grasp of English but is still able to pick up a new language easily and naturally.
It’ll probably be almost a year before your baby speaks that first word—two years or more before words are strung into phrases and then sentences, perhaps a year or longer before most of those sentences are easily comprehensible. But long before your baby is communicating verbally, he or she will be communicating in a variety of other ways. In fact, look and listen closely now and you’ll find that your baby’s already trying to speak to you—not in so many words, but in so many behaviors and gestures.
No dictionary of baby communication can tell you what your baby’s saying. Rather, the key to understanding this non-verbal communication is observation—patient, careful observation. Observing your child will speak volumes about his or her personality, preferences, and needs, months before your child can speak at all. For example, does your baby wiggle and fuss uncomfortably when she’s undressed before her bath? That may mean that she dislikes the cold air on her naked body—or just doesn’t like the sensation of being naked at all. Keeping her covered as much as possible before lowering her into the bath will help ease her discomfort.
Or does your baby make coughing sounds around the time he’s ready for a nap? Coughing might be your baby’s way of telling you that he’s getting tired—long before early fatigue melts down into crankiness.
Or does your baby frantically stuff her fist into her mouth when she’s due for a feeding, before she starts wailing loudly? That could be her hunger cue—her first message to you that she’s ready to eat (the second, crying, will make the feeding much more difficult for both of you to accomplish). By observing your baby’s behaviors and gestures, you’ll notice patterns that will start to make sense—and will help you make sense of what baby’s telling you.
And listening to what baby tells you not only makes your job easier (you can provide what baby wants promptly, rather than figuring it out through trial, error, and tears) but also lets your baby know that what he or she has to say matters, an important first step on the road to becoming a confident, secure, successful, and emotionally mature person.
Whether you start now or in a couple of years, there are several approaches to encouraging a child to pick up a second language. One parent can speak English and the other the foreign tongue (as your spouse suggests), or both parents can speak the foreign language (with the expectation the child will pick up English in school and elsewhere), or a grandparent, sitter, or au pair can speak the foreign language and the parents English (usually the least successful of the methods). None of the methods of teaching a second language is particularly successful if the “teacher” isn’t fluent in the language.
Experts recommend you forget about “giving lessons in” a second language and instead immerse your child in it—play games (and, as you child grows, computer games) in it, read books in it (many popular children’s books have been translated from English into other languages), sing songs in it, listen to CDs and watch DVDs in it, visit with friends who are fluent in it, and, if possible, visit places where the language is spoken. Whoever is speaking the second language should speak it exclusively to the child, resisting the temptation to resort to English or to translate if the child seems to be struggling with comprehension. Expect your child to go through some periods of mixing the two languages in the beginning, but, eventually, a separation of the two will occur. During the school years, the child should be taught to read and write in the second language in order for it to take on greater usefulness and significance. If classes aren’t available at school, tutoring or computer-programmed learning may be a good idea.
Your baby won’t remember much, if anything, about the first three years of life, but according to researchers, those three years will have a huge impact on the quality of your child’s life—in some ways more than any of the others that follow.
What makes those first three years—years filled primarily with eating, sleeping, crying, and playing, the years before formal learning even begins—so vital to your child’s ultimate success in school, in a career, in relationships? How can a period of time when your child is so clearly unformed be so critical to the formation of the human being your child will eventually become? The answer is fascinating, complex, and still evolving. Here’s what scientists believe so far.
Research shows that a child’s brain grows to 90 percent of its adult capacity during those first three years—granted, a lot of brain power for someone who can’t yet tie his or her shoes. During these three phenomenal years, brain “wiring” occurs. (“Wiring” is when the crucial connections are made linking brain cells.) By the third birthday, somewhere around one thousand trillion connections will have been made.
With all this activity, however, a child’s brain is very much a work in progress at age three. More connections are made until age ten or eleven, at which point the brain starts specializing for better efficiency, eliminating connections that are rarely used (this pattern continues throughout life, which is why adults end up with only about half the brain connections a three-year-old has). Changes continue to take place well past puberty, with important parts of the brain still continuing to change throughout life.
While your child’s future—like his or her brain—is far from fully cast at age three, it does appear that those early years do form the mold that will shape the person he or she will become. And the greatest influence during those formative years is you. Research shows that the kind of care a child receives during that time determines to a large extent how well those brain connections will be made, how much that little brain will develop, how successful, how content, how confident, and how competent to handle life’s challenges that child will be.
Feeling daunted and overwhelmed by the task that’s been handed you? Don’t be. Most of what any loving parent does intuitively (with no training, without the addition of flash cards or special mind-expanding programs) is exactly what your child—and your child’s brain—needs to develop to his or her greatest potential. Consider:
 Every time you touch, hold, cuddle, hug, or respond to your baby with warm responsive care (all things you do anyway), you’re positively affecting the way your child’s brain forms connections. By reading, talking, singing, making eye contact, or cooing to your baby, you’re helping your baby’s brain reach its full potential. And through your positive parenting, you’ll be teaching your child social and emotional skills that will actually boost your child’s intellectual development as he or she gets older; the more socially and emotionally confident a child is, the more likely that child will be motivated to learn and to take on new challenges with enthusiasm and without fear of failure.
Every time you touch, hold, cuddle, hug, or respond to your baby with warm responsive care (all things you do anyway), you’re positively affecting the way your child’s brain forms connections. By reading, talking, singing, making eye contact, or cooing to your baby, you’re helping your baby’s brain reach its full potential. And through your positive parenting, you’ll be teaching your child social and emotional skills that will actually boost your child’s intellectual development as he or she gets older; the more socially and emotionally confident a child is, the more likely that child will be motivated to learn and to take on new challenges with enthusiasm and without fear of failure.
 Children whose basic needs are met in infancy and early childhood (she’s fed when hungry, changed when wet, held when frightened) develop a sense of trust in others and a high level of self-confidence. Researchers have found that children reared in such nurturing environments have fewer behavioral problems in school later on, and are emotionally more capable of positive social relationships.
Children whose basic needs are met in infancy and early childhood (she’s fed when hungry, changed when wet, held when frightened) develop a sense of trust in others and a high level of self-confidence. Researchers have found that children reared in such nurturing environments have fewer behavioral problems in school later on, and are emotionally more capable of positive social relationships.
 By monitoring and helping to regulate your baby’s impulses and behaviors during the early years (explaining she can’t bite, telling him not to grab a toy), you will eventually teach your child self-control. Setting limits that are fair and age-appropriate and enforcing them consistently will enable your child to be less likely to be anxious, frightened, impulsive, or to rely on violent means to resolve conflicts later on in life, say researchers. He or she will also be more capable of intellectual learning because of the solid emotional foundation you have provided.
By monitoring and helping to regulate your baby’s impulses and behaviors during the early years (explaining she can’t bite, telling him not to grab a toy), you will eventually teach your child self-control. Setting limits that are fair and age-appropriate and enforcing them consistently will enable your child to be less likely to be anxious, frightened, impulsive, or to rely on violent means to resolve conflicts later on in life, say researchers. He or she will also be more capable of intellectual learning because of the solid emotional foundation you have provided.
 Likewise, any caregiver who spends a significant amount of time with your child should provide the same kind of stimulation, the same kind of responsiveness, the same kind of positive discipline. High-quality child care will help ensure that your baby’s brain gets what it needs: lots of nurturing.
Likewise, any caregiver who spends a significant amount of time with your child should provide the same kind of stimulation, the same kind of responsiveness, the same kind of positive discipline. High-quality child care will help ensure that your baby’s brain gets what it needs: lots of nurturing.
 Routine medical care is important, too, ensuring that your child will be screened regularly for any medical or developmental issues that could slow intellectual, social, or emotional growth. It will also allow for early intervention should a problem be uncovered, which could prevent that problem from holding your child back.
Routine medical care is important, too, ensuring that your child will be screened regularly for any medical or developmental issues that could slow intellectual, social, or emotional growth. It will also allow for early intervention should a problem be uncovered, which could prevent that problem from holding your child back.
And here’s probably the most important thing to keep in mind. Helping your child reach his or her potential is different from trying to change the person your child is; encouraging intellectual development is different from pushing it; providing stimulating experiences is different from scheduling in the kind of overload that leads to burnout. It’s easy to avoid crossing that line from just enough parental interaction and involvement to too much by taking your cues from your baby—who, when it comes to getting what he or she needs, can be wise even beyond your years. Watch and listen carefully, and you’ll almost always know what’s best for your child.
“I get together regularly with a parents’ group, and inevitably they all start comparing what their babies have been doing. It makes me crazy—and worried about whether my son is developing fast enough.”
If there’s anything more anxiety provoking than a roomful of pregnant women comparing bellies, it’s a roomful of recently delivered parents comparing babies. Just as no two pregnant bellies are exactly alike, neither are any two babies. Developmental norms (such as those found in each chapter of this book) are useful for comparing your baby to a broad range of normal infants in order to assess her progress and identify any lags. But comparing your baby with someone else’s child, or with an older one of your own, can only result in a lot of unnecessary fears and frustrations. Two perfectly “normal” babies can develop in different areas at completely different clips—one may forge ahead in vocalizing and socializing, another in physical feats, such as turning over. Differences between babies become even more marked as the first year progresses—one baby may crawl very early but not walk until fifteen months, another may never learn to crawl at all but suddenly start taking steps at ten months. Then, too, a parent’s assessment of her baby’s progress is highly subjective—and not always completely accurate. One may not even recognize baby’s frequent coos as the beginnings of language, while another may hear one coo and swear, “He said ‘dada’!”
All of this said, it’s easier to intellectualize that comparing babies isn’t a good idea than to actually stop doing it or avoid those who do. Many compulsive comparers can’t sit within ten feet of another parent-with-baby on a bus, in a doctor’s waiting room, or at the park without launching an assault of outwardly innocent queries that lead to the inevitable comparisons (“What an adorable baby! She’s sitting already? How old is she?”). The best advice, if you can’t completely manage to “mind your own baby,” is to remember how meaningless these comparisons really are. Your baby, like your belly before him, is one of a kind.
“My baby’s pediatrician says that immunization is perfectly safe. But I’ve heard a few stories about serious reactions, and I worry about my daughter getting the shots.”
We live in a society that considers good news to be no news. A story on the positive effects of immunizations cannot compete with one on the extremely rare instances of serious complications associated with them. So it is likely that today’s parents have heard more about the risks of immunization than the benefits. And, yet, as your pediatrician has doubtless told you, for most infants those benefits continue to far outweigh the risks.
Not too many years ago in the United States, the most common causes of infant death were infectious diseases, such as diphtheria, typhoid, and smallpox. Measles and whooping cough were so common that all children were expected to get them, and thousands, especially infants, died or were permanently handicapped by these illnesses. Parents dreaded the coming of summer and the infantile paralysis (polio) epidemics that seemed invariably to arrive with it, killing or disabling thousands of infants and children. Today, smallpox has been virtually eliminated, and diphtheria and typhoid are extremely rare. Only a small percentage of children are stricken with measles or whooping cough each year, and infantile paralysis is a disease parents are not only no longer afraid of, but often aren’t even familiar with. An American baby is now much more likely to die because of not being strapped into a car seat than from a communicable disease. Without a doubt, immunization has made childhood safer for children.
Immunization is based on the fact that exposure to weakened or dead disease-producing microorganisms (in the form of vaccines) or to the poisons (toxins) they produce, rendered harmless by heat or chemical treatment (then called toxoids), will cause an individual to produce the same antibodies that would develop if the person had actually contracted the disease. Armed with the special memory that is unique to the immune system, these antibodies will “recognize” the specific microorganisms, should they attack in the future, and destroy them.
Even the ancients recognized that when people survived a particular disease, they weren’t likely to contract it again, and those who had recovered from the plague were sometimes called upon to care for new victims. Although some societies attempted crude forms of immunization, it wasn’t until Edward Jenner, a Scottish physician, decided to test the old belief that a person who contracted the lesser disease cowpox would never get smallpox, that modern immunization was born. In 1796, Jenner smeared pus from the sores of a milkmaid infected with cowpox on two small cuts in the arm of a healthy eight-year-old boy. The child developed a slight fever a week later, then a couple of small scabs on his arm. When exposed to smallpox later, he remained healthy. He had become immune.
Most worries about immunization—though perfectly understandable—are unfounded. Don’t let the following myths keep you from immunizing your baby:
MYTH: Giving so many shots together isn’t safe.
Reality: Studies have shown that vaccinations are just as safe and effective when given together. There are many combination vaccines that have been used routinely for years (MMR, DTaP). Recently approved and already in use by many doctors is the Pediarix vaccine that combines DTaP, polio, and hep B in a single shot. Researchers are continuing to develop combo vaccines that may become approved for use in the near future. The best part about these combination vaccines: fewer total shots for your baby—something you’re both likely to appreciate.
MYTH: Shots are very painful for a baby.
Reality: The pain of a vaccine is only momentary and, compared to the pain of the serious diseases the immunization is protecting against, insignificant. And there are ways of minimizing the pain your baby feels. Studies show that babies who get shots while they are being held and distracted by their parents cry less, and those who are breastfed immediately before or during the immunization experience less pain. You can also ask your baby’s doctor about giving a sugar solution just before the shot or using an anesthetic cream an hour earlier (which the doctor will have to prescribe).
MYTH: If everyone else’s children are immunized, mine can’t get sick.
Reality: Some parents believe that they don’t have to immunize their own children if everyone else’s children are immunized—since there won’t be any diseases to catch. That theory doesn’t hold up. First of all, there’s the risk that other parents are subscribing to the same myth, which means their children won’t be immunized, either, creating the potential for an outbreak of a preventable disease. Second, unvaccinated children put vaccinated children at risk for the disease as well (vaccines are about 90 percent effective; the high percentage of immunized individuals limits the spread of disease)—so not only might you be hurting your child, you might also be hurting your child’s friends. Third, unvaccinated children can catch whooping cough (pertussis) not only from other unvaccinated children, but also from adults. That’s because the vaccine that protects against it isn’t given after age seven; immunity has largely worn off by adulthood; and the disease, while still highly contagious, is so mild in adults that it’s usually not diagnosed—which means that adults who don’t realize they have whooping cough can inadvertently spread it to babies, who are much more vulnerable to its effects.
MYTH: One vaccine in a series gives a child enough protection.
Reality: Researchers have found that skipping vaccines puts your child at increased risk for contracting the diseases, especially measles and pertussis. So if the recommendations are for a series of four shots, make sure your child receives all the necessary shots so he or she is not left unprotected.
MYTH: Multiple vaccines for such young babies put them at increased risk for other diseases.
Reality: There is no evidence that multiple immunizations increase the risk for diabetes, infectious disease, or other illnesses. Neither is there any evidence to date that there is a connection between multiple vaccines and allergic diseases such as asthma.
The immunization process has come a long way since that early experiment. The first widely administered type of immunization, the smallpox vaccination, was so successful that it is no longer considered necessary. For now, at least, the disease seems to have been eradicated from the entire globe. Plenty of progress has been made with other serious scourges as well, and it’s hoped that immunization will someday wipe out most of them, too.
But while immunization clearly saves thousands of young lives each year, it’s not perfect. Though most children have only a mild reaction to certain vaccines, some become ill, a very few seriously so. Some types of vaccine have been suspected of causing, on rare occasions, permanent damage, even death. Still, the tremendous benefits of protection from serious disease far outweigh the very small risks of immunization for all but high-risk children—clearly making vaccination the very best bet for your baby. And as minimal as the risks are, they can be reduced even further by taking precautions to make sure your baby is safely vaccinated. Here’s how:
 Be sure the doctor gives your baby a thorough checkup before giving a vaccination to be certain no serious illness is developing that is not yet apparent; shots should be postponed when a baby is significantly ill. (A mild illness, such as a cold, is not reason to postpone a shot.)
Be sure the doctor gives your baby a thorough checkup before giving a vaccination to be certain no serious illness is developing that is not yet apparent; shots should be postponed when a baby is significantly ill. (A mild illness, such as a cold, is not reason to postpone a shot.)
 Read the one-page CDC vaccine information statements (VISs) that should be provided by the doctor each time a routine vaccine is given to your child. (The statements are also available on the Web at www.cdc.gov.)
Read the one-page CDC vaccine information statements (VISs) that should be provided by the doctor each time a routine vaccine is given to your child. (The statements are also available on the Web at www.cdc.gov.)
 Observe your baby carefully for 72 hours after the vaccination (especially during the first 48), and report any severe reactions (see page 232) or very unusual behavior to the doctor immediately. Also report any less severe reactions at your next visit.
Observe your baby carefully for 72 hours after the vaccination (especially during the first 48), and report any severe reactions (see page 232) or very unusual behavior to the doctor immediately. Also report any less severe reactions at your next visit.
 Ask the doctor to enter the vaccine manufacturer’s name and the vaccine lot/batch number in your child’s records, along with any reactions you report. Be sure to get a copy of the information for your own records as well. Severe reactions should be reported by the doctor or by you to VAERS (Vaccine Adverse Event Reporting System); www. vaers.org.
Ask the doctor to enter the vaccine manufacturer’s name and the vaccine lot/batch number in your child’s records, along with any reactions you report. Be sure to get a copy of the information for your own records as well. Severe reactions should be reported by the doctor or by you to VAERS (Vaccine Adverse Event Reporting System); www. vaers.org.
 When the next shot is scheduled, remind your baby’s doctor about any previous reactions to the vaccine.
When the next shot is scheduled, remind your baby’s doctor about any previous reactions to the vaccine.
 If you have any fears about vaccine safety, discuss them with your baby’s doctor.
If you have any fears about vaccine safety, discuss them with your baby’s doctor.
It helps to know what the needle that’s headed your baby’s way is loaded with. The following is a guide to immunizations your child will probably receive in the first year and beyond:
Diphtheria, tetanus, acellular pertussis vaccine (DTaP). Immunization against diphtheria, tetanus, and pertussis (whooping cough) is crucial, since all can cause serious illness and death. DTaP (which contains diphtheria and tetanus toxoids and an acellular pertussis vaccine) has fewer serious side effects than the older DTP (which contains a whole-cell pertussis vaccine) and is now the vaccine of choice. Though there were rare reports, not fully substantiated, of a link between the old vaccine and brain damage, there have been no such reports with the new one.
Your child needs five DTaP shots. DTaP is recommended at two, four, and six months, fifteen to eighteen months, and between four and six years.
Up to one-third of children who get DTaP have very mild local reactions where the shot was given, such as tenderness, swelling, or redness, usually within two days of getting the shot. Some children are fussy or will lose their appetite for a few hours or perhaps a day or two. Fever is also a common reaction. These reactions are more likely to occur after the fourth and fifth doses than after the earlier doses. Occasionally, a child will have a more serious side effect, such as a fever of over 104°F. Rarely, a child will cry continuously (for three or more hours) after receiving the DTaP. Even rarer are convulsions, which can result not from the vaccine itself but rather from a high fever accompanying it in a few children (see page 232). Research has shown that any seizures resulting from such vaccine-induced fever do not lead to lasting problems; a suggested link between these seizures and autism has not been found. Research also shows that there is no correlation between the vaccine and a greater risk of SIDS.
In certain circumstances, a doctor may decide to omit the pertussis vaccine (and just administer the DT) if the baby’s previous reactions to DTaP were severe. And a doctor may delay giving the DTaP (or not give it at all) if a child had a severe allergic reaction to the first DTaP dose, a high temperature following the DTaP, or any other severe reaction, including seizures.
Most doctors will postpone the shot for a baby who is significantly sick. Though a few doctors will also delay giving a DTaP (or other) shot because of a mild cold, this isn’t considered necessary—and could result in a child ending up incompletely immunized. After all, many babies who attend day care or who have an older sibling have frequent colds—sometimes one after another during “cold season.” Finding symptom-free windows of opportunity to vaccinate these babies according to schedule often proves impossible. Delaying shots because of mild fevers, ear infection, and most cases of gastrointestinal upset is also not usually considered necessary or wise.
Polio vaccine (IPV). Immunization has virtually eliminated polio (aka infantile paralysis), once a dreaded disease, from the United States. The oral vaccine (OPV), a live vaccine given by mouth, is no longer routinely given because it presented a minuscule risk of paralysis (about 1 in 8.7 million) in vaccinated children. Instead, it has been replaced by the inactivated vaccine (IPV), given by injection.
Children should receive four doses of IPV—the first, at two months; the second, at four months; the third at six to eighteen months; and the fourth, at four to six years—except in special circumstances (such as when traveling to countries where polio is still common, in which case the schedule may be stepped up).
The IPV is not known to produce any side effects except for a little soreness or redness at the site of the injection and the rare allergic reaction. The doctor will likely delay administering the IPV if your child is very ill. A child who had a severe allergic reaction to the first dose generally won’t be given subsequent doses.
Measles, mumps, rubella (MMR). Children get two doses of the MMR, the first between twelve and fifteen months, and the second between ages four and six (though it can be administered anytime as long as it is twenty-eight days after the first). Measles, though often joked about, is in reality a serious disease with sometimes severe, potentially fatal, complications. Rubella, also known as German measles, on the other hand, is often so mild that its symptoms are missed. But because it can cause birth defects in the fetus of an infected pregnant woman, immunization in early childhood is recommended—both to protect the future fetuses of girl babies and to reduce the risk of infected children exposing pregnant women, including their own mothers. Mumps rarely presents a serious problem in childhood, but because it can have severe consequences (such as sterility or deafness) in adulthood, early immunization is recommended.
Reactions to the MMR vaccine are generally very mild and don’t usually occur until a week or two after the shot. About 1 in 5 children will get a rash or slight fever lasting a few days from the measles component. About 1 in 7 will get a rash or some swelling of the neck glands, and 1 in 100, aching or swelling of the joints from the rubella component, sometimes as long as three weeks after the shot. Occasionally, there may be swelling of the salivary glands from the mumps component. Much less common are tingling, numbness, or pain in the hands and feet, all difficult to discern in infants, and allergic reactions. Large studies have not shown a link between the MMR vaccine and autism.
Caution should be taken in administering MMR to a child sick with anything but a mild cold, one with an impaired immune system (from medication, cancer, or another condition), one who has recently had a blood transfusion, one who has a severe allergy to gelatin or the antibiotic neomycin, or one who had a severe allergic reaction after the first dose of MMR.
Varicella vaccine (Var). Varicella, or chicken pox, until recently one of the most common childhood diseases, is usually a mild disease without serious side effects. There can be complications, however, such as Reye’s syndrome and bacterial infections (including group A strep); and the disease can be fatal to high-risk children, such as those with leukemia or immune deficiencies, or those whose mothers were infected with varicella just prior to delivery.
A single dose of varicella vaccine is recommended between twelve and eighteen months. A child who already had chicken pox does not need to get the vaccine. It appears that the vaccine prevents chicken pox in 70 to 90 percent of those who are vaccinated. The small percentage who do get chicken pox after receiving the vaccine usually get a much milder case than if they had not been immunized.
The varicella vaccine is very safe. Rarely, there may be redness or soreness at the site of the injection. Some children also get a mild rash (about five spots) a few weeks after being immunized.
Hemophilus Influenzae b vaccine (Hib). This vaccine is aimed at thwarting the deadly hemophilus influenzae b (Hib) bacteria (which has no relation to influenza, or “flu”) that is the cause of a wide range of very serious infections in infants and young children. Prior to the introduction of the vaccine, Hib was responsible for about 12,000 cases of meningitis in children in the United States annually (5 percent of them fatal) and for nearly all epiglottitis (a potentially fatal infection that obstructs the airways). It was also the leading cause of septicemia (blood infection), cellulitis (skin and connective tissue infection), osteomyelitis (bone infection), and pericarditis (heart membrane infection) in young children.
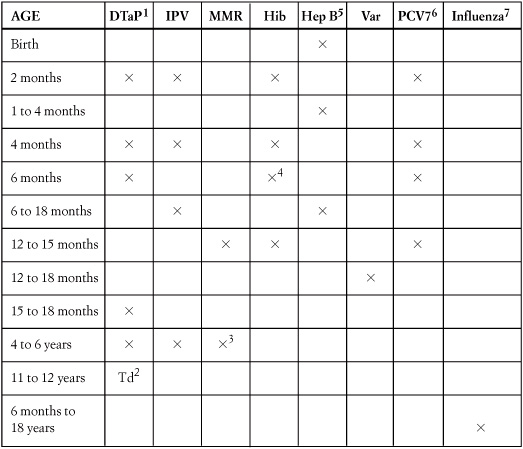
1. The fourth dose of DTaP should be given at least 6 months after the third dose. 2. Subsequent routine Td boosters are recommended every 10 years. 3. May be administered during any visit, provided at least 4 weeks have elapsed since the first dose and that both doses are administered beginning at or after age 12 months. 4. Three Hib conjugate vaccines are licensed for infant use. If PRP-OMP is administered at ages 2 and 4 months, a dose at age 6 months is not required. DTaP/Hib combination products should not be used for primary immunization in infants at ages 2, 4, or 6 months, but can be used as boosters following any Hib vaccine. 5. All infants should receive the first dose of hepatitis B vaccine soon after birth and before hospital discharge (unless the doctor plans on administering the Pediarix combo vaccine at 2 months). The first dose may also be given by age 2 months if the infant’s mother is hep B-negative. Infants born to hepB-positive mothers should receive hepatitis B vaccine and hep B immune globulin (HBIG) within 12 hours of birth, at separate sites. Hepatitis A vaccine is recommended for use in high-risk states and regions (all in the West), and for certain high-risk groups; consult your local public health authority. 6. It is also recommended for certain high-risk children age 24–59 months.7. Influenza vaccine is recommended annually for children over 6 months of age. Children younger than 9 years who are receiving the vaccine for the first time should receive two doses at least 4 weeks apart. Thimerosal has been removed from all vaccines with the exception of the influenza vaccine (which is available without thimerosal).
The Hib vaccine appears to have few, if any, side effects. A very small percentage of children may have fever, redness and/or tenderness on the site of the shot. Your child should get the Hib vaccine at two, four, and six months, with a fourth dose at twelve to fifteen months.
Though severe reactions to immunizations are exceedingly rare, you should call the doctor if your baby experiences any of the following within two days of the shot:
 High fever (over 104°F)
High fever (over 104°F)
 Crying that lasts longer than three hours
Crying that lasts longer than three hours
 Seizures/convulsions (jerking or staring)—usually because of fever and not serious
Seizures/convulsions (jerking or staring)—usually because of fever and not serious
 Seizures or major alterations in consciousness within seven days of shot
Seizures or major alterations in consciousness within seven days of shot
 An allergic reaction (swelling of mouth, face, or throat; breathing difficulties; immediate rash)
An allergic reaction (swelling of mouth, face, or throat; breathing difficulties; immediate rash)
 Listlessness, unresponsiveness, excessive sleepiness
Listlessness, unresponsiveness, excessive sleepiness
Should you note any of the above symptoms following an injection, call the doctor. This is not just for your baby’s sake, but also so that the doctor can report the response to the Vaccine Adverse Events Reporting System. Collection and evaluation of such information may help reduce future risks.
As with other vaccines, Hib vaccine should not be given to a child who is very ill (mild illness isn’t a problem), or who might be allergic to any of the components (check with the doctor).
Hepatitis vaccines. Hepatitis B (hep B), a chronic liver disease, can cause liver failure and liver cancer in future years. Three doses are needed. It is recommended that the vaccine for hepatitis B be given at birth (it may be delayed for premature infants), one to four months, and six to eighteen months. (If the Pediarix combo vaccine is administered, the doses are given at two, four, and six months instead.) Side effects—slight soreness and fussiness—are not common and are short-lived. The vaccine for hepatitis A (hep A), which also affects the liver, is recommended for children over age two living in high-risk states and countries, mostly in the western United States (check with your doctor to see if you are living in a high-risk area).
Pneumococcal conjugate vaccine (PCV7). The pneumococcus bacterium is a major cause of illness among children, responsible for some ear infections, meningitis, pneumonia, blood infections, and other illnesses. Though the PCV vaccine is one of the newer vaccines, large studies and clinical trials have shown that it is extremely effective in preventing the occurrence of certain types of ear infections, meningitis, pneumonia, and other related life-threatening infections. Children should get the vaccine at two, four, and six months, with a booster given at twelve to fifteen months. Side effects, such as low-grade fever or redness and tenderness at the injection site, are occasionally seen and are not harmful.
Influenza. The influenza, or “flu” vaccine is now recommended for all healthy babies between six and twenty-two months old. In the past, it was recommended that only young children at high risk for flu complications receive the vaccine. But studies indicate that even healthy children under age two are at increased risk for hospitalization from flu-related complications. The vaccine is especially important for those at high risk—those with serious heart or lung disease, those with depressed immune systems, asthma, HIV, diabetes, and those with sickle-cell anemia or similar blood diseases. The flu vaccine should not be given to anyone who has had a severe allergic reaction to eggs. High-risk children may, instead, be given antiviral medications to prevent development of influenza. When having your child immunized, ask for a thimerosal-free flu vaccine. (Flu Mist, the nasal spray flu vaccine, is not recommended for children under age five.)
If for some reason any of your baby’s vaccinations are postponed, immunization can pick up where it left off; starting over isn’t necessary. Work with the doctor to get your child caught up as soon as possible.
“I wash my daughter’s hair every day, but I still can’t seem to get rid of the flakes on her scalp.”
Don’t pack away those dark-shouldered outfits yet. Cradle cap, a seborrheic dermatitis of the scalp common in young infants, doesn’t doom your daughter to a lifetime of dandruff. Mild cradle cap, in which greasy surface scales appear on the scalp, often responds well to a brisk massage with mineral oil or petroleum jelly to loosen the scales, followed by a thorough shampoo to remove them and the oil. Tough cases, in which flaking is heavy and/or brownish patches and yellow crustiness are present, may benefit from the daily use of an antiseborrheic shampoo that contains sulfur salicylates, such as Sebulex (make sure you keep it out of baby’s eyes) after the oil treatment. (Some cases are aggravated by the use of such preparations. If your baby’s is, discontinue use and discuss this with the doctor.) Since cradle cap usually worsens when the scalp sweats, keeping it cool and dry may also help—so don’t put a hat on baby unless necessary (such as in the sun or when it’s cold outside), and then remove it when you’re indoors or in a heated car.
When cradle cap is severe, the seborrheic rash may spread to the face, neck, or buttocks. If this occurs, the doctor will probably prescribe a topical ointment.
Occasionally, cradle cap will persist through the first year—and in a few instances, long after a child has graduated from the cradle. Since the condition causes no discomfort and is therefore considered only a cosmetic problem, aggressive therapy (such as use of topical cortisone, which can contain the flaking for a period of time) isn’t usually recommended but is certainly worth discussing with your child’s doctor as a last resort.
“Our son’s feet seem to fold inward. Will they straighten out on their own?”
Your son’s not alone in his stance; most babies appear bowlegged and pigeon-toed. This happens for two reasons—one, because of the normal rotational curve in the legs of a newborn, and, two, because the cramped quarters in the uterus often force one or both feet into odd positions. When baby emerges at birth, after spending several months in that position, the feet are still bent or seem to turn inward.
In the months ahead, as your baby’s feet enjoy their out-of-utero freedom and as he learns to pull up, crawl, and then walk, his feet will begin straightening out. They almost always do so without treatment.
Just to be sure there isn’t another cause of your baby’s foot position, express your concerns at his next well-baby visit. The doctor probably has already checked your baby’s feet for abnormalities, but another check to put your mind at ease won’t hurt. It’s also routine for the doctor to keep an eye on the progress of a baby’s feet to make sure they straighten out as he grows—which they almost certainly will in your son’s case.
In the very unlikely event a baby’s feet don’t appear to be straightening out on their own, casting or special shoes may be recommended at a later date. At just what point treatment is considered will depends on the type of problem and on the doctor’s point of view.
“My son was born with undescended testicles. The doctor said that they would probably descend from the abdomen by the time he was a month or two old, but they haven’t yet.”
The abdomen may seem a strange location for testicles, but it isn’t. The testicles (or testes) in males and the ovaries in females both develop in the fetal abdomen from the same embryonic tissue. The ovaries, of course, stay put. The testes are scheduled to descend down through the inguinal canals in the groin, into the scrotal sac at the base of the penis, somewhere around the eighth month of gestation. But in 3 to 4 percent of full-term boys and about one third of those that are preterm, they don’t make the trip before birth. The result: undescended testicles.
Because of the migratory habits of testicles, it’s not always easy to determine that one hasn’t descended. Normally, the testicles hang away from the body when they are in danger of overheating (protecting the sperm-producing mechanism from temperatures that are too high). But they slip back up into the body when they are chilled (protecting the sperm-producing mechanism from temperatures that are too low) or when they are handled (again protective, to avoid injury). In some boys the testes are particularly sensitive and spend a lot of time sheltered in the body. In most, the left testicle hangs lower than the right, possibly making the right seem undescended (and making a lot of young boys worry). The diagnosis of undescended testicle or testicles is therefore made only when one or both have never been observed to be in the scrotum, not even when the baby is in a warm bath.
An undescended testicle causes no pain or difficulty with urinating, and as your doctor assured you, usually descends on its own. By age one, only three or four boys in a thousand still have un-descended testicles, at which point surgery (a minor procedure) can easily put them in their proper place. Hormone therapy can be tried first, but it isn’t usually successful.
“My son was circumcised as a newborn, and my doctor says he’s developed a penile adhesion. What does that mean?”
Whenever tissues of the body are cut, the edges will stick to the surrounding tissue as it heals. After the foreskin of the penis is removed during a circumcision, the circular edge remaining tends to stick to the penis as it heals. If a significant amount of foreskin remains after the circumcision, it, too, can stick to the penis during the healing process, causing the foreskin to reattach. This penile adhesion is not a problem as long as it’s gently retracted periodically to prevent it from becoming permanently attached. Ask the doctor how you should do this or if it’s really necessary to do at all. When boys, even baby boys, have their normal erections, the sticking skin surfaces are pulled, helping to keep them apart, without any adult intervention. Rarely, if a bridge of skin has permanently attached, a urologist may need to separate the skin and remove the remaining piece of foreskin to prevent the problem from recurring.
“The pediatrician said that my twin boys have inguinal hernias and will have to have surgery. Is this serious?”
A hernia is often thought of as something that develops when a grown man does too much heavy lifting. But even infants too young to lift a finger—never mind a heavy package—aren’t too young to experience a hernia. Hernias are not unusual in newborns, particularly boys, and especially those born prematurely (as twins often are).
In an inguinal hernia, a part of the intestines slips through one of the inguinal canals (the same channels through which the testes descend into the scrotum) and bulge into the groin. The defect is often first noted as a lump in one of the creases where the thigh joins the abdomen, particularly when a baby is crying or very active; it often retracts when he is quiet. When the section of the intestines slips all the way down into the scrotum, it can be seen as an enlargement or swelling in the scrotum, and may be referred to as scrotal hernia.
A hernia doesn’t usually cause any discomfort, and while it must be treated, it isn’t a serious condition and isn’t considered an emergency. Nevertheless, any parent who notices a lump or swelling in their baby’s groin or scrotum should report the finding to the doctor as soon as possible. Doctors usually advise repair as soon as the hernia is diagnosed—assuming the baby is fit for surgery. Such surgery is usually simple and successful, with a very short (sometimes one-day) hospitalization. Only very rarely does an inguinal hernia recur following surgery, though in some children another hernia occurs on the opposite side at a later date.
If a diagnosed infant inguinal hernia is not treated, it can lead to the herniated section becoming “strangulated”—pinched by the muscular lining of the inguinal canal, obstructing blood flow and digestion in the intestines. Vomiting, severe pain, even shock can result. Parents who note a baby suddenly crying in pain, vomiting, and not having bowel movements should call the doctor immediately. If the doctor can’t be reached, the baby should be taken to the nearest emergency room. Elevating the baby’s bottom slightly and applying an ice pack while en route to the ER may help the intestine to retract, but don’t try to push it back in by hand.
“One of my daughter’s nipples sinks in instead of standing out. What’s wrong with it?”
It’s inverted—not at all uncommon in the nipples of infants. Often, a nipple that is inverted at birth corrects itself spontaneously later. If it doesn’t, it won’t be an issue until she’s ready to nurse her own baby, at which point (if necessary, and it likely won’t be) she can take steps to draw the nipple out.
“My little girl hardly ever wants to nurse on my left breast, and it’s shrunken to be considerably smaller than the right.”
Some babies play favorites. It could be that your baby’s more comfortable cradled in your favored, and probably stronger, arm, so she developed a taste for the breast on that side. Or that you often place her on the left breast, so that your right hand is free for eating, holding a book or the phone, or handling other chores, leaving the right breast to dwindle in size and production (or the reverse, if you’re left-handed). Perhaps one breast is the better provider because you favored it early on in the nursing relationship, for any number of reasons—from the location of the cesarean incision pain to the location of the TV set in your bedroom.
Whatever the reason, preferring one breast over the other is a fact of nursing for some babies, and lopsidedness a fact of life for their mothers. Though you might try to increase production on the less favored side by pumping daily and/or starting every feeding with it (if your baby will cooperate), these efforts may not do the trick. In many cases, mothers go through the entire nursing experience with one breast larger than the other (though you’ll probably be the only one who notices the difference). The lopsidedness will diminish after weaning, though a slightly greater-than-normal difference may continue.
Very rarely, a baby rejects a breast because it harbors a developing malignancy. So do mention your baby’s penchant to your doctor.
“We usually carry our son around in a baby carrier. Is this a good idea?”
It’s been a good idea for millennia. Baby carriers and slings—cloth sacks that harness infants to their parents or other caregivers—have, in one form or another, been helping transport babies in other cultures since prehistoric times. There are at least three good reasons. First, babies are usually happy riding in a carrier; they enjoy the steady gentle movement and the closeness to a warm body. Second, babies tend to cry less if they’re carried around a lot—and carrying is made a lot easier with a carrier. And, third, carriers provide parents and other caregivers with the freedom to attend to their daily chores—tote packages, push shopping carts or the vacuum cleaner, make phone calls—while carrying baby.
Different kinds of baby carriers come with different benefits; see a discussion of these on page 60. But if baby carriers are a boon to today’s parents, they can also be a bane if overused or misused. Keep in mind the following when carrying your baby:
Overheating. On a very warm day, even a scantily clothed baby can simmer in a baby carrier—particularly one that encloses the baby’s legs, feet, and head or is made from a heavy fabric such as corduroy. Such overheating can lead to prickly heat and even heat stroke. If you use a carrier in warm weather, in overheated rooms, or on a hot bus or subway (baby carriers should never be used instead of a safety seat in the car), check your baby frequently to be sure he isn’t sweating and his body doesn’t feel warmer than yours. If he does appear to be overheated, remove some clothing or take him out of the carrier completely.
Understimulation. A baby who’s always cooped up in a baby carrier that limits his visual perspective to a chest and, if he looks up, the bottom of a face doesn’t have the opportunity he needs to see the world. This is not a major problem in the first few weeks of life, when a baby’s interest is usually limited to the most basic creature comforts, but it can be now, when he’s ready to expand his horizons. Use a convertible carrier or a sling in which baby can face in for a nap or out for viewing the world, or limit baby’s sojourns to times when he will be sleeping or will be pacified only by being carried and you need your arms for other purposes. At other times, use a stroller or infant seat.
Too much sleeping. Babies who are toted in baby carriers tend to sleep a lot—often a lot more than they need to, with two less-than-desirable results. First, they get used to catnapping on the go (fifteen minutes when you run out to the corner grocery store, twenty when you walk the dog) rather than taking longer naps in their cribs. Second, they may become so well rested during the day that they don’t rest much at night. If your baby immediately falls asleep when placed in a carrier, limit use to make sure he doesn’t nap the day away in it.
Risk of injury. A young infant’s neck isn’t strong enough yet to support his head when he’s jiggled and jostled a lot. Though securing your baby in a baby carrier or sling while you jog may seem like an ideal way of getting your exercise and keeping your baby happy, too, the bouncing could be risky. Instead, strap him in a stroller when you go for a jog. Also be careful to bend at the knees, not the waist, when wearing the carrier—or your baby could slip out.
While judicious use of a baby carrier can make your life easier and your baby’s life happier, he won’t be ready for a back carrier until he can sit by himself.
“Our little girl is adorable, but she seems to cry for the least little reason. If it’s too noisy, or too bright, or even if she’s a little wet. We’re going crazy trying to cope with this. Are we doing something wrong?”
No parent expects to have a challenging child. Pregnant daydreams are pink-and-blue collages of a contented infant who coos, smiles, sleeps peacefully, cries only when she’s hungry, and grows into a sweet-tempered, cooperative child. Bawling, inconsolable babies and kicking, screaming toddlers belong to others—parents who did it all wrong and are paying the price.
And then, for so many parents like you, just weeks after your perfect baby is born, reality does a number on that particular fantasy. Suddenly, it’s your baby who’s crying all the time, who won’t sleep, or who seems perpetually unhappy and dissatisfied no matter what you do. Why shouldn’t you wonder, “What have we done wrong?”
The answer is probably nothing, except perhaps pass on some contributing genes, for a baby’s temperament appears to have much more to do with heredity than environment. How the childhood environment is structured, however, can make a difference as to how inborn temperament affects future development. The child who, with help from mommy and daddy, learns to direct and develop “challenging” inborn personality traits, transforming them from liabilities into assets, can go from impossible problem infant to highly successful adult.
The parental role in this metamorphosis—as in most aspects of a child’s development—is critical. The first step is to identify which of several different types of personalities that have been linked to difficult behavior your own baby displays (some display a combination). Your baby seems to be what is known as a low-sensory-threshold baby. A wet diaper, a starched dress, a high neckline, a bright light, a staticky radio, a scratchy blanket, a cold crib—any or all of these may unduly upset a baby who seems to be extra sensitive to sensory stimulation. In some children, all five senses—hearing, vision, taste, touch, and smell—are very easily overloaded; in others, just one or two. Dealing with the low-sensory-threshold child means trying to keep the general level of unnecessary sensory stimulation down, as well as avoiding those specific things that you notice bother baby, such as:
The active baby. Babies often send the first clue that they’re going to be more active than most right from the uterus; suspicions are confirmed soon after birth when receiving blankets are kicked off, diapering and dressing sessions become wrestling matches, and baby always ends up at the opposite end of the crib after a nap. Active babies are a constant challenge (they sleep less than most, become restless when feeding, can be extremely frustrated until they’re able to be independently mobile, and are always at risk of hurting themselves), but they can also be a joy (they’re usually very alert, interested and interesting, and quick to accomplish). While you don’t want to squelch such a baby’s enthusiasm and adventurous nature, you will want to take special protective precautions as well as learn ways to quiet him or her for eating and sleeping. The following tips should help:
 Use a blanket sleeper in cold weather and lightweight sleepers in cool weather; limit or avoid swaddling.
Use a blanket sleeper in cold weather and lightweight sleepers in cool weather; limit or avoid swaddling.
 Be especially careful never to leave an active baby on a bed, changing table, or any other elevated spot even for a second—they often figure out how to turn over very early, and sometimes just when you least expect it. A restraining strap on the changing table is useful but should not be relied upon if you’re more than a step away.
Be especially careful never to leave an active baby on a bed, changing table, or any other elevated spot even for a second—they often figure out how to turn over very early, and sometimes just when you least expect it. A restraining strap on the changing table is useful but should not be relied upon if you’re more than a step away.
 Adjust the crib mattress to its lowest level as soon as the active baby starts to sit alone for even a few seconds—the next step may be pulling up and over the sides of the crib. Keep all objects a baby might climb on out of crib and play yard.
Adjust the crib mattress to its lowest level as soon as the active baby starts to sit alone for even a few seconds—the next step may be pulling up and over the sides of the crib. Keep all objects a baby might climb on out of crib and play yard.
 Don’t leave an active baby in an infant seat except on the floor—they are often capable of overturning the seat. And of course, baby should always be strapped in.
Don’t leave an active baby in an infant seat except on the floor—they are often capable of overturning the seat. And of course, baby should always be strapped in.
 Learn what slows down your active baby—massage (see page 304), soft music (either your own singing or a CD), a warm bath, or looking at a picture book (though active children may not be ready for this as early as quieter children). Build such quieting activities into your baby’s schedule before feeding and sleeping times.
Learn what slows down your active baby—massage (see page 304), soft music (either your own singing or a CD), a warm bath, or looking at a picture book (though active children may not be ready for this as early as quieter children). Build such quieting activities into your baby’s schedule before feeding and sleeping times.
The irregular baby. At about six to twelve weeks, just when other babies seem to be settling into a schedule and becoming more predictable, these babies seem to become more erratic. Not only don’t they fall into schedules on their own, they aren’t interested in any you may have to offer.
Instead of following such a baby’s lead and letting chaos take over your home life, or taking the reins yourself and imposing a very rigid schedule that is contrary to the infant’s nature, try to find a middle ground. For both your sakes, it’s necessary to put at least a modicum of order in your lives, but try as much as possible to build a schedule around any natural tendencies your baby seems to exhibit. You may have to keep a diary to uncover any hints of a recurring time frame in your child’s days, such as hunger around 11 A.M. every morning or fussiness after 7 P.M. every evening.
Try to counter any unpredictability with predictability. That means trying, as much as possible, to do things at the same times and in the same ways every day. Nurse in the same chair when possible, give baths at the same time each day, always soothe by the same method (rocking or singing or whatever works best). Try scheduling feedings at roughly the same times each day, even if your baby doesn’t seem hungry, and try to stick to the schedule even if he or she is hungry between meals, offering a small snack if necessary. Ease rather than force your baby into more of a structured day. And don’t expect true regularity, just a little less chaos.
Nights with an irregular baby can be torture, mostly because the baby doesn’t usually differentiate them from days. You can try the tips for dealing with night-day differentiation problems (see page 181), but it’s very possible they won’t work for your baby, who may want to stay up throughout the night, at least initially. To survive, mommy and daddy may have to alternate night duty or share split shifts until things get better, which they eventually will if you are persistent and stay cool.
The poor-adaptability or initial-withdrawal baby. These babies consistently reject the unfamiliar—new objects, people, foods. Some are upset by change of any kind, even familiar change such as going from the house to the car. If this sounds like your baby, try setting up a daily schedule with few surprises. Feedings, baths, and naps should take place at the same times and in the same places, with as few departures from routine as possible. Introduce new toys and people (and foods, when baby is ready for them) very gradually. For example, hang a new mobile over the crib for just a minute or two. Remove it and bring it out again in a short while, leaving it up for a few minutes longer. Continue increasing the time of exposure until baby seems ready to accept and enjoy the mobile. Introduce other new toys and objects in the same way. Have new people spend a lot of time just being in the same room with your baby, then talking at a distance, then communicating close up, before they make an attempt at physical contact. Later, when you introduce solids, add new foods very gradually, starting with tiny amounts, and increasing portion size over the span of a week or two. Don’t add another food until the last is well accepted. Try to avoid unnecessary changes when making purchases—a new feeding bottle with a different shape or color, a new gadget on the stroller, a new pacifier. If an item wears out or breaks, try to replace it with an identical or similar model.
The high-intensity baby. You probably noticed it right at the beginning—your baby cried louder than any other child in the hospital nursery. The loud crying and screaming, the kind that can frazzle even the steadiest of nerves, continued when you got home. You can’t flip a switch and turn down the volume on your baby, of course—but turning down the volume of noise and activity in the environment may help tone your child down a bit. Also, you will want to take some purely practical measures to keep the noise from bothering family and neighbors. If possible, soundproof your baby’s room by insulating the walls with insulating board or padding, adding carpeting, curtains, and anything else that will absorb the sound. You can try earplugs, a white-noise machine, a fan or air conditioner to reduce the wear and tear on your ears and nerves without totally blocking out your baby’s cries. As crying lessens in the months ahead, so will this problem, but your child will probably always be louder and more intense than most.
The negative or “unhappy” baby. Instead of smiling and cooing, some babies just seem grumpy all the time. This is no reflection on the parents (unless, of course, they’ve been neglectful), but it can have a profound impact on them. They often find it difficult to love their unhappy babies, and sometimes they even reject them. If nothing seems to satisfy your baby (and no medical explanation is uncovered), then do your best to be loving and caring anyway, secure in the knowledge that one of these days, when your baby learns other ways of expression, the crying and general unhappiness will diminish, though he or she may always be the “serious” type.
 Sound sensitivity. As much as is practical (remember, you still have to live in the house, too) lower the sound level in your home. Keep the radio, stereo, and TV low, adjust the telephone ring to low, and install carpeting and draperies, where possible, to absorb sound. Speak or sing to your baby softly and have others do the same. Be sure any musical or other sound-producing toys aren’t disturbing to baby. If outside noises seem to be a problem, try a white-noise machine or air cleaner in baby’s room to block them out.
Sound sensitivity. As much as is practical (remember, you still have to live in the house, too) lower the sound level in your home. Keep the radio, stereo, and TV low, adjust the telephone ring to low, and install carpeting and draperies, where possible, to absorb sound. Speak or sing to your baby softly and have others do the same. Be sure any musical or other sound-producing toys aren’t disturbing to baby. If outside noises seem to be a problem, try a white-noise machine or air cleaner in baby’s room to block them out.
 Light or visual sensitivity. Use room-darkening shades or drapes so baby can sleep later in the morning and nap during the day, and avoid very bright lights in rooms she frequents. Don’t expose her to too much visual stimulation at once—hang just one toy in the crib, or put just a couple in the play yard at a time. Select toys that are soft and subtle in color and design rather than bright and busy.
Light or visual sensitivity. Use room-darkening shades or drapes so baby can sleep later in the morning and nap during the day, and avoid very bright lights in rooms she frequents. Don’t expose her to too much visual stimulation at once—hang just one toy in the crib, or put just a couple in the play yard at a time. Select toys that are soft and subtle in color and design rather than bright and busy.
 Taste sensitivity. If your baby is breastfed and has a bad day after you eat garlic or onions, consider that the unfamiliar taste of your milk may be the cause; if she’s bottle fed and seems cranky a lot, try switching to a formula with a different taste (ask the doctor for a recommendation). When you introduce solids, recognize the fact that your baby may not relish every taste sensation and may reject strong flavors entirely.
Taste sensitivity. If your baby is breastfed and has a bad day after you eat garlic or onions, consider that the unfamiliar taste of your milk may be the cause; if she’s bottle fed and seems cranky a lot, try switching to a formula with a different taste (ask the doctor for a recommendation). When you introduce solids, recognize the fact that your baby may not relish every taste sensation and may reject strong flavors entirely.
 Touch sensitivity. With this princess-and-the pea-like syndrome, some babies lose their composure as soon as they wet their diapers, become frantic when they’re too warm or dressed in rough fabrics, scream when they’re dunked in the tub or put down on a too-cold mattress or, later, when you tie their shoes over wrinkled socks. So keep clothing comfortable (cotton knits with smooth seams and buttons, snaps, labels, and collars that won’t irritate because of size, shape, or location are ideal), bathwater and room temperatures at levels that keep her happy, and diapers changed frequently.
Touch sensitivity. With this princess-and-the pea-like syndrome, some babies lose their composure as soon as they wet their diapers, become frantic when they’re too warm or dressed in rough fabrics, scream when they’re dunked in the tub or put down on a too-cold mattress or, later, when you tie their shoes over wrinkled socks. So keep clothing comfortable (cotton knits with smooth seams and buttons, snaps, labels, and collars that won’t irritate because of size, shape, or location are ideal), bathwater and room temperatures at levels that keep her happy, and diapers changed frequently.
A small percentage of babies are so oversensitive to touch that they resist being held and cuddled. Don’t over-handle such a baby; do a lot of your caressing and interacting with words and eye contact rather than actual physical touching. When you do hold your baby, learn which way seems least annoying (tight or loose, for example). Observe closely to see what feels good and what doesn’t.
 Smell sensitivity. Unusual odors aren’t likely to bother a very young infant, but some children begin to show a negative reaction to certain scents before the end of the first year. The aroma of frying onions, the smell of a diaper rash medicine, the fragrance of mom’s new perfume or dad’s new aftershave lotion, can all make such a baby restless and unhappy. If your baby seems sensitive to smells, limit strong odors when you can.
Smell sensitivity. Unusual odors aren’t likely to bother a very young infant, but some children begin to show a negative reaction to certain scents before the end of the first year. The aroma of frying onions, the smell of a diaper rash medicine, the fragrance of mom’s new perfume or dad’s new aftershave lotion, can all make such a baby restless and unhappy. If your baby seems sensitive to smells, limit strong odors when you can.
 Stimulation sensitivity. Too much stimulation of any kind seems to trigger trouble for some infants. These babies need to be handled gently and slowly. Loud talk, hurried movements, too many playthings, too many people around, too much activity in a day—these can all be upsetting. To help such a baby sleep better, avoid active play just before bedtime, substituting a soothing, warm bath followed by quiet storytelling or lullabies. Soft recorded music can often help such a baby to settle down, too.
Stimulation sensitivity. Too much stimulation of any kind seems to trigger trouble for some infants. These babies need to be handled gently and slowly. Loud talk, hurried movements, too many playthings, too many people around, too much activity in a day—these can all be upsetting. To help such a baby sleep better, avoid active play just before bedtime, substituting a soothing, warm bath followed by quiet storytelling or lullabies. Soft recorded music can often help such a baby to settle down, too.
Taking the extra steps that keep a very demanding baby happy isn’t easy, but it’s almost always worth the effort. Keep in mind, however, that there will be times when you won’t realistically be able to put baby’s special needs first (baby dislikes bright lights and noise, but you have to take him or her to a family Christmas party with you). That’s fine, too—though you may have to deal with the crying consequences. Keep in mind, also, that most “challenging” symptoms tend to lessen considerably as a child gets older.
Before you decide your baby is one of the challenging ones, however, you should be sure that there isn’t some underlying physical cause of his or her troubling behavior. Describe it to the doctor so that any possible medical explanation—illness or allergy, for example—can be ruled out. Sometimes a baby who seems to be especially demanding is simply colicky, teething, ill, or allergic to her formula. For descriptions of other types of challenging babies, see the box on page 238.
“I know I should put my baby to sleep on his back to protect against SIDS. But he sleeps terribly in that position. Once, when I put him on his tummy to play, he fell asleep and took his longest nap ever. Is it safe to switch?”
Often babies know what’s best for them (as when they stop eating when they’re no longer hungry, or they tune out overly enthusiastic parents when they’ve had too much stimulation). But, unfortunately, not when it comes to sleeping positions. Most babies naturally prefer the tummy position for sleeping; it’s more comfortable, it’s cozier, and it makes them less likely to startle. And for all those reasons, it also ensures longer sleeps and fewer wakings.
But it’s clearly not best for baby. Tummy sleeping is linked to a much higher incidence of SIDS—particularly in babies who are not accustomed to the position (because, like yours, they started out on their backs from birth). Most babies get used to the back position quickly, especially if they’ve never known another sleeping position; others continue to fuss a bit on their backs; and a few, like yours, don’t seem able to settle down for a good night’s sleep when they’re tummy up. Almost all babies would sleep better on their tummies given the chance, which is one of the reasons why scientists believe SIDS is more likely to strike tummy-sleeping babies. Because infants sleep more deeply on their tummies, their arousal responses are muted, preventing them, scientists theorize, from waking up during episodes of sleep apnea and resuming normal breathing patterns.
The first thing you should do is discuss the problem with your pediatrician. He or she might want to look into why your baby dislikes the back position so much. Rarely a baby has a physical or anatomical reason that makes being on his back unusually uncomfortable. Much more likely, your baby just plain doesn’t like the way it feels. If that’s the case, try some of these tips for keeping your baby happy on his back:
 Consider swaddling before bedtime. Research shows that infants who are swaddled before they’re put on their backs sleep more contentedly—and cry less. They’re also less likely to startle and to be woken up by those normal, jerky movements. But don’t swaddle once your baby is active enough to kick off the blanket (loose bedding in the crib poses a safety hazard). Some babies can manage this as early as the second month. Also make sure the room is cool enough when you’re swaddling; overheating is another risk factor for SIDS.
Consider swaddling before bedtime. Research shows that infants who are swaddled before they’re put on their backs sleep more contentedly—and cry less. They’re also less likely to startle and to be woken up by those normal, jerky movements. But don’t swaddle once your baby is active enough to kick off the blanket (loose bedding in the crib poses a safety hazard). Some babies can manage this as early as the second month. Also make sure the room is cool enough when you’re swaddling; overheating is another risk factor for SIDS.
 Prop up the head of the mattress slightly (with a pillow or rolled blanket under the mattress) so baby isn’t flat on his back. This may make him more comfortable. But don’t prop baby with any pillows or other soft bedding inside the crib.
Prop up the head of the mattress slightly (with a pillow or rolled blanket under the mattress) so baby isn’t flat on his back. This may make him more comfortable. But don’t prop baby with any pillows or other soft bedding inside the crib.
 Slowly train your baby to be more comfortable sleeping on his back. If falling asleep in that position is tough for him, try putting him in his infant seat to sleep or rocking him to sleep before transferring him to the crib once he’s asleep (on his back).
Slowly train your baby to be more comfortable sleeping on his back. If falling asleep in that position is tough for him, try putting him in his infant seat to sleep or rocking him to sleep before transferring him to the crib once he’s asleep (on his back).
 Stick with it. Consistency almost always pays off when it comes to babies. Eventually, he’ll probably get used to sleeping on his back.
Stick with it. Consistency almost always pays off when it comes to babies. Eventually, he’ll probably get used to sleeping on his back.
 Check again with the doctor if baby’s still miserable on his back. If nothing you do seems to make your son a happy back-sleeper, the doctor might suggest letting baby sleep on his side, with a wedge that prevents him from rolling onto his stomach (but not his back). While it’s not the recommended sleeping position, it’s still safer than tummy down, and may allow you both to get some sleep.
Check again with the doctor if baby’s still miserable on his back. If nothing you do seems to make your son a happy back-sleeper, the doctor might suggest letting baby sleep on his side, with a wedge that prevents him from rolling onto his stomach (but not his back). While it’s not the recommended sleeping position, it’s still safer than tummy down, and may allow you both to get some sleep.
Once your baby can roll over by himself, chances are he’ll flip over into his preferred sleeping position even when you’ve put him down on his back (see page 355).
In our achievement-oriented society, many parents worry about turning out babies who can keep up with the baby down the street—and they begin worrying early. They worry that if he doesn’t smile by the time he’s four weeks old, he may not get into the right preschool program. They worry that if she hasn’t turned over by two months, she may not make the high school tennis team. Somewhat of an exaggeration? Well, somewhat. In fact, there are parents who worry that unless they do everything right, they won’t be successful in turning the basically unresponsive lump they just delivered into a candidate for an Ivy League sheepskin.
Actually, they have little reason to worry. Babies—even those destined for that coveted sheepskin—develop at different rates, and those who get off to a somewhat slower start often excel later. And parents—even those who are chronically insecure—usually do a thoroughly competent job of stimulating their offspring, often without making a conscious effort.
Yet, as comforting as this knowledge should be, it doesn’t always stop the worry. For many parents, there is the nagging fear that doing what comes naturally when it comes to parenting may not be quite enough. So, if you’d like to check what you’ve already been doing instinctively to see if you’re on the right track, the following tips for creating the right atmosphere for learning and for supplying sensory stimulation should be helpful to you. Also see Making the Most of the First Three Years, pages 224–225.
It’s a lot easier than you might think. Here’s all there is to it:
Love your baby. Nothing helps a baby grow and thrive as much as being loved. A close relationship with a parent, or parents, and/or a substitute parent is crucial for normal development. Love should be unconditional, too—the no-strings-attached variety. It should be communicated as clearly (though it may not come as easily) during a colic bout or a toddler temper tantrum (and, later, during a teenage tempest) as during a moment of angelic behavior.
Relate to your baby. Take every opportunity to talk, sing, or coo to your baby—while you’re changing a diaper, giving a bath, shopping for groceries, or driving the car. These casual but stimulating exchanges go further in making a brighter baby than forcing computer learning programs. And even the most educational toys are useless if baby doesn’t have you (the best of all toys) to play with part of the time. Your goal at this point isn’t to “teach” your baby but to be involved with him or her.
Get to know your baby. Learn what makes your baby happy or miserable, excited or bored, soothed or stimulated—paying more attention to that feedback than to the advice of any book or expert. Gear attempts at stimulation to your unique baby. If loud noises and/or roughhousing upset your child, then entertain with soft sounds and gentle play. If too much excitement makes your baby frantic, limit the length of playtimes and the intensity of activity.
Take the pressure off—and have fun. Learning and development aren’t hastened by pressure, and they may be hindered. Harmful to baby’s self-esteem is the message—no matter how carefully camouflaged—that you’re not satisfied with his or her progress up the developmental ladder. Instead of thinking of the times you spend stimulating your baby as educational sessions, relax and enjoy, for both your sakes.
Give your baby space. Adequate attention is vital; too much can be stifling. Though children need to know that help is available when they need it, they need to learn how to seek it out, too. Your constant hovering will also deprive your baby of the chance to look for and find diversion elsewhere—in the friendly-looking teddy bear who’s sharing the play yard, in the pattern of light cast by the venetian blinds, in his or her own fingers and toes, in the sound of an airplane overhead, a fire engine down the street, the dog barking next door. It may also hamper your baby’s ability to play, learn, and problem-solve independently later on—all important life skills. (Besides, an overly dependent child will make it difficult for you to turn your attention to anything else.) By all means, spend quality time playing with your child. But sometimes just get baby and toy together, and then move off to watch from the sidelines while they get acquainted.
Follow the leader. And make sure your baby, not you, is in the lead. If he or she is fascinated by the mobile, don’t bring out the activity board; instead, focus on the mobile together. Allowing baby to take the wheel once in a while not only enhances learning by taking advantage of the “teachable moment,” but also reinforces baby’s budding sense of self-esteem by communicating that his or her interests are worthy of mommy’s or daddy’s attention.
Let your baby take the lead, too, in deciding when to end a play session—even if it’s before the rattle is grasped. Your baby will tell you, “I’ve had enough,” by turning away, fussing, crying, or otherwise showing disinterest or displeasure. Ignoring the message and pressing on deprives a baby of a sense of control, turns off interest in the subject (at least for a while), and ultimately makes playtime a whole lot less fun for both of you.
Time it right. A baby is always in one of six states of consciousness: deep, or quiet, sleep; light, or active, sleep; drowsiness; active wakefulness with interest in physical activity; fussiness and crying; or quiet wakefulness. It’s during active wakefulness that you can most effectively encourage physical development and during quiet wakefulness that you can best foster other types of learning (see page 120). Also keep in mind that infants have very short attention spans. A baby who turns you off after two minutes of looking at a book isn’t rejecting being read to, but has simply run out of concentration.
Provide positive reinforcement. When your baby starts achieving (when he or she smiles, swats at a rattle, lifts shoulders and arms off the mattress, turns over, or grasps a toy successfully) spur on more efforts with positive reinforcement. Do it with hugs, cheers, applause—whatever is comfortable for you and gets the message across to your baby: “I think you’re terrific.”
Some parents, without ever reading a book about or taking a course in infant stimulation, seem to have an easier time than others initiating learning-playing activities with their babies. And some babies, because they are unusually responsive, are easier to engage in such activities. But any parent-baby team can be successful at learning-playing with a little guidance. The areas to nourish and encourage are:
The sense of taste. Right now you don’t have to go out of your way to stimulate this sense. Your baby’s taste buds are titillated at every meal on breast or bottle. But as baby gets older, “tasting” will become a way of exploring, and everything within reach will end up being mouthed. Resist the temptation to discourage this—except, of course, when what goes into the mouth is toxic, sharp, or small enough to choke on.
The sense of smell. In most environments, the keen smelling apparatus of infants gets plenty of exercise. There’s breast milk, dad’s aftershave, Rover scampering nearby, the flowers on your walk together, the chicken roasting in the oven. Unless your baby shows signs of being overly sensitive to odors, think of the various scents as additional opportunities for your baby to learn about the environment.
The sense of sight. Though it was once believed that babies were largely sightless at birth, it’s now known that they can not only see but can begin learning from what they see right from the start. Through their sense of sight, they learn very quickly to differentiate between objects and human beings (and between one object or human being and another), to interpret body language and other nonverbal cues, and to understand a little bit more every day about the world around them.
Decorate your baby’s room or corner with the goal of supplying stimulating visual surroundings, rather than satisfying your own esthetic. When selecting wallpaper, sheets, wall hangings, toys, or books, keep in mind that babies like sharp contrasts, and that designs that are bold and bright rather than soft and delicate are more appealing (black-and-white and other color-contrasting patterns are favored for the first six weeks or so, pastels and other colors later).
Many objects, toys among them, can stimulate baby visually (but to avoid confusion and overstimulation, provide only one or two at a time during play sessions):
 Mobiles. Figures on a mobile should be fully visible from below (the baby’s perspective), rather than from the side (the adult’s perspective). A mobile should be no more than 12 to 15 inches over the baby’s face, and should be hung to one side or the other of the child’s line of vision, rather than straight above (most babies prefer to gaze toward the right, but observe your child to discover a preference).
Mobiles. Figures on a mobile should be fully visible from below (the baby’s perspective), rather than from the side (the adult’s perspective). A mobile should be no more than 12 to 15 inches over the baby’s face, and should be hung to one side or the other of the child’s line of vision, rather than straight above (most babies prefer to gaze toward the right, but observe your child to discover a preference).
 Other things that move. You can move a rattle or other bright toy across baby’s line of vision to encourage tracking of moving objects. Take a field trip to a pet shop and position baby in front of a fish tank or bird cage to view the action. Or blow bubbles for baby.
Other things that move. You can move a rattle or other bright toy across baby’s line of vision to encourage tracking of moving objects. Take a field trip to a pet shop and position baby in front of a fish tank or bird cage to view the action. Or blow bubbles for baby.
 Stationary objects. Babies spend a lot of time just looking at things. This isn’t idle time, but learning time. Geometric patterns or simple faces in black and white, hand drawn or store-bought, are early favorites—but baby will probably also be fascinated by every-day objects you wouldn’t glance at twice.
Stationary objects. Babies spend a lot of time just looking at things. This isn’t idle time, but learning time. Geometric patterns or simple faces in black and white, hand drawn or store-bought, are early favorites—but baby will probably also be fascinated by every-day objects you wouldn’t glance at twice.
 Mirrors. Mirrors give babies an ever-changing view, and most love them. (They especially enjoy looking at and socializing with the “baby” in the mirror, having no clue yet who that baby is.) Be sure to use safe baby mirrors; hang them on the crib, in the carriage, beside the changing table.
Mirrors. Mirrors give babies an ever-changing view, and most love them. (They especially enjoy looking at and socializing with the “baby” in the mirror, having no clue yet who that baby is.) Be sure to use safe baby mirrors; hang them on the crib, in the carriage, beside the changing table.
 People. Babies delight in looking at faces close up, so you and other family members should spend plenty of time in close proximity to baby. Later, you can also show baby family photos pointing out who’s who.
People. Babies delight in looking at faces close up, so you and other family members should spend plenty of time in close proximity to baby. Later, you can also show baby family photos pointing out who’s who.
 Books. Show baby simple pictures of babies, children, animals, or toys and identify them. The drawings should be clear and sharply defined without a lot of extra (for a baby) detail. Boldly illustrated board books are perfect for this.
Books. Show baby simple pictures of babies, children, animals, or toys and identify them. The drawings should be clear and sharply defined without a lot of extra (for a baby) detail. Boldly illustrated board books are perfect for this.
 The world. Very soon your baby is going to take an interest in seeing beyond that little button nose. Provide plenty of opportunity to see the world—from the stroller, carriage, or car seat, or by carrying your baby face forward. Add commentary, too, pointing out cars, trees, people, and so on. But don’t ramble nonstop during every outing; you’ll become bored, and baby will start tuning you out.
The world. Very soon your baby is going to take an interest in seeing beyond that little button nose. Provide plenty of opportunity to see the world—from the stroller, carriage, or car seat, or by carrying your baby face forward. Add commentary, too, pointing out cars, trees, people, and so on. But don’t ramble nonstop during every outing; you’ll become bored, and baby will start tuning you out.
The sense of hearing. It’s through hearing that infants learn about language, about rhythm, about danger, about emotions and feelings—and about so much else that goes on around them. Auditory stimulation can come from almost any source.
 The human voice. This, of course, is the most significant type of sound in a new infant’s life, so use yours—talk, sing, and babble to your baby. Try lullabies, nursery rhymes, nonsense ditties you create yourself. Imitate animal sounds, especially ones your baby regularly hears, such as the barking of a dog or the meowing of a cat. Most importantly, play back for your baby the sounds he or she makes.
The human voice. This, of course, is the most significant type of sound in a new infant’s life, so use yours—talk, sing, and babble to your baby. Try lullabies, nursery rhymes, nonsense ditties you create yourself. Imitate animal sounds, especially ones your baby regularly hears, such as the barking of a dog or the meowing of a cat. Most importantly, play back for your baby the sounds he or she makes.
Here’s something you need to know before offering a rattle or other toy to your baby: Where you offer it from makes all the difference. A baby won’t reach for an object proffered from the front, only from the side.
 Household sounds. Many young babies are captivated by either soft or lively background music, the hum of the vacuum or the blender, the whistle of the teakettle or the splash of running water, the crinkling of paper, or the tinkling of a bell or wind chime—though they may become fearful of many such sounds later in the first and second years.
Household sounds. Many young babies are captivated by either soft or lively background music, the hum of the vacuum or the blender, the whistle of the teakettle or the splash of running water, the crinkling of paper, or the tinkling of a bell or wind chime—though they may become fearful of many such sounds later in the first and second years.
 Rattles and other toys that make gentle sounds. You don’t have to wait until your baby is able to shake a rattle independently. In the early months, either do the shaking yourself, put the rattle in baby’s hand and help shake it, or attach a wrist rattle. Coordination between vision and hearing will develop as baby learns to turn toward sound.
Rattles and other toys that make gentle sounds. You don’t have to wait until your baby is able to shake a rattle independently. In the early months, either do the shaking yourself, put the rattle in baby’s hand and help shake it, or attach a wrist rattle. Coordination between vision and hearing will develop as baby learns to turn toward sound.
 Music boxes. You’ll be surprised at how quickly your baby will learn to recognize a tune; especially nice are music boxes that have visual appeal, but if one is placed within reach, be sure it doesn’t have small pieces that can be broken off and mouthed by your baby.
Music boxes. You’ll be surprised at how quickly your baby will learn to recognize a tune; especially nice are music boxes that have visual appeal, but if one is placed within reach, be sure it doesn’t have small pieces that can be broken off and mouthed by your baby.
 Musical toys. Toys that make music and also provide visual stimulation and practice with small motor skills (such as a bunny that moves and makes music when baby pulls a string) are particularly good. Avoid toys that make loud noises that can damage hearing, and don’t place even moderately noisy ones right by baby’s ear. Also be sure that the toys are otherwise safe for baby.
Musical toys. Toys that make music and also provide visual stimulation and practice with small motor skills (such as a bunny that moves and makes music when baby pulls a string) are particularly good. Avoid toys that make loud noises that can damage hearing, and don’t place even moderately noisy ones right by baby’s ear. Also be sure that the toys are otherwise safe for baby.
 Children’s tapes and CDs. Try to give them a spin before buying to be sure they’re good listening. Infancy is also an ideal time to start exposing your child to classical music (play it softly during playtime in the crib, or during dinner or bath time), although many babies seem to prefer the livelier rhythms of rock, pop, or country music. Always watch your baby for reactions to music; if he or she seems disturbed by what you’re playing, turn it off. Also, protect your baby’s sense of hearing by keeping the volume down.
Children’s tapes and CDs. Try to give them a spin before buying to be sure they’re good listening. Infancy is also an ideal time to start exposing your child to classical music (play it softly during playtime in the crib, or during dinner or bath time), although many babies seem to prefer the livelier rhythms of rock, pop, or country music. Always watch your baby for reactions to music; if he or she seems disturbed by what you’re playing, turn it off. Also, protect your baby’s sense of hearing by keeping the volume down.
The sense of touch. Touch, though often underrated, is actually one of a baby’s most valuable tools for exploring and learning about the world. It’s through touch that a baby learns the softness of mommy and the relative hardness of daddy, that rubbing a teddy bear feels wonderful, that rubbing a stiff brush doesn’t feel so good, and most important of all, that those who take care of him are loving—a message you send every time you bathe, diaper, feed, hold, or rock your baby.
You can provide more varied touching experiences for your baby with:
 A loving hand. Try to learn how your baby likes to be handled—firmly or lightly, quickly or slowly. Most babies love to be caressed and kissed, to have their tummies tickled or razzed by your lips, to have you blow gently on their fingers or toes. They love the difference between mommy’s touch and daddy’s, the playful way a sibling hugs them and the expert ease with which grandma rocks them.
A loving hand. Try to learn how your baby likes to be handled—firmly or lightly, quickly or slowly. Most babies love to be caressed and kissed, to have their tummies tickled or razzed by your lips, to have you blow gently on their fingers or toes. They love the difference between mommy’s touch and daddy’s, the playful way a sibling hugs them and the expert ease with which grandma rocks them.
 Massage. Preemies who are massaged for at least twenty minutes daily gain weight faster and do better overall than those who aren’t (whether it’s the massage or the fact that they’re handled more is unclear); babies who aren’t touched at all don’t grow at a normal pace. Discover the kind of strokes your baby enjoys most, and avoid those that seem to annoy (see page 304 for tips).
Massage. Preemies who are massaged for at least twenty minutes daily gain weight faster and do better overall than those who aren’t (whether it’s the massage or the fact that they’re handled more is unclear); babies who aren’t touched at all don’t grow at a normal pace. Discover the kind of strokes your baby enjoys most, and avoid those that seem to annoy (see page 304 for tips).
 Textures. Try rubbing a baby’s skin with different textures (satin, terry cloth, velvet, wool, fur, or absorbent cotton) so he or she can get to know how each feels; later encourage independent exploration. Let baby lie tummy down (while supervised only) on surfaces with different textures: the living room carpet, a terry towel, grandma’s faux fur coat, dad’s wool sweater, mom’s corduroy jacket, the marble-topped coffee table—the possibilities are limitless.
Textures. Try rubbing a baby’s skin with different textures (satin, terry cloth, velvet, wool, fur, or absorbent cotton) so he or she can get to know how each feels; later encourage independent exploration. Let baby lie tummy down (while supervised only) on surfaces with different textures: the living room carpet, a terry towel, grandma’s faux fur coat, dad’s wool sweater, mom’s corduroy jacket, the marble-topped coffee table—the possibilities are limitless.
 Playthings with texture. Offer toys that have interesting textures to baby. A plush teddy bear and a coarse-haired stuffed doggy; hard wooden blocks and soft stuffed ones; a rough wooden bowl and a smooth metal one; a silky pillow and a nubby one.
Playthings with texture. Offer toys that have interesting textures to baby. A plush teddy bear and a coarse-haired stuffed doggy; hard wooden blocks and soft stuffed ones; a rough wooden bowl and a smooth metal one; a silky pillow and a nubby one.
Social development. Your baby becomes a social being through watching you, through interacting with you and the rest of the family, and later with others. This isn’t the time to begin teaching your baby how to throw a successful dinner party or make interesting small talk over the canapés, but it is time to begin teaching by example how people should behave toward one another. A few years from now, when your growing child talks to friends, teachers, neighbors, or begins “playing house,” you’ll often hear your example echoed in that tiny voice; hopefully, you’ll be pleased (and not shocked or disappointed) by what you hear.
Toys that help babies with social development are stuffed animals, animal mobiles, and dolls. Though it will be many months before they’ll be able to hug them and play with them, even at this point they can and do begin to socialize with them—just watch an infant converse with animals prancing on the crib bumpers or revolving on a mobile. Later, books and opportunities for make-believe and dress-up play will also help children to develop social skills.
Small motor development. Right now your baby’s hand movements are totally random, but in a couple of months, those tiny hands will move with more purpose and control. You can aid in the development of purposeful movement by giving your baby’s hands plenty of freedom; don’t keep them swaddled or tucked tightly under a blanket (except outdoors in cold weather). Provide a variety of objects that are easy for small hands to pick up and manipulate, that don’t require fine dexterity. And since young babies usually won’t grasp objects that are directly in front of them, offer these objects from the side.
Give your baby ample opportunity for “hands-on” experience with the following:
 Rattles that fit small hands comfortably. Those with two handles or grasping surfaces will eventually allow a baby to pass the rattle from hand to hand, an important skill; those that baby can mouth will help bring relief when teething begins.
Rattles that fit small hands comfortably. Those with two handles or grasping surfaces will eventually allow a baby to pass the rattle from hand to hand, an important skill; those that baby can mouth will help bring relief when teething begins.
 Cradle gyms (they fit across carriage, play yard, or crib) that have a variety of parts for baby to grab hold of, spin, pull, and poke. Beware of those, however, with strings more than 6 inches long, and take down any gym once your baby is able to sit up.
Cradle gyms (they fit across carriage, play yard, or crib) that have a variety of parts for baby to grab hold of, spin, pull, and poke. Beware of those, however, with strings more than 6 inches long, and take down any gym once your baby is able to sit up.
 Activity boards that require a wide range of hand movements to operate. Your baby may not be able to intentionally maneuver the toy for a while, but even a young infant can sometimes set it in motion accidentally. Besides the spinning, dialing, pushing, and pressing skills these toys encourage, they also teach the concept of cause and effect.
Activity boards that require a wide range of hand movements to operate. Your baby may not be able to intentionally maneuver the toy for a while, but even a young infant can sometimes set it in motion accidentally. Besides the spinning, dialing, pushing, and pressing skills these toys encourage, they also teach the concept of cause and effect.
Gross motor development. Putting your baby through the paces of an infant exercise video won’t increase muscular strength or speed motor development. Good motor skills, well-developed bodies, and physical fitness for infants depend instead on the following: good nutrition; good health care (both well baby and sick baby); and plenty of opportunity for self-motivated physical activity. Babies kept cooped up in a swing, baby seat, or ExerSaucer, harnessed in a carriage or stroller, or swaddled in a blanket or bunting will have little opportunity to learn about how their bodies work. Those who are never put down on their tummy for supervised playtime will be slow to learn to lift their head and shoulders or turn over front to back and may never learn to crawl. Change your baby’s position often during the day (propping him up in a sitting position, placing her sometimes on her stomach—supervised—and other times on her back) to maximize the opportunities for physical activity.
Encourage physical development by pulling your baby to a sitting position, letting him or her “fly” (allowing exercise of arms and legs) or “ride” (lying facedown lengthwise on your shins). Motivate rolling over by putting an interesting object to one side as baby lies on his or her back; if baby turns a bit, then give a little help in going all the way. Encourage creeping by letting baby push off against your hands when lying belly down.
Intellectual development. Encouraging the development of all the senses, as well as small and large motor control, will contribute to your baby’s intellectual growth. Talk to your infant a lot, right from the start. Give names to objects, animals, and people your baby sees, point out body parts, explain what you’re doing. Read nursery rhymes and simple stories, showing your baby the illustrations as you go. Expose your child to a variety of settings (the supermarket, a department store, the museum, the park). Travel on buses, in cars, in taxicabs. Even at home, vary your baby’s point of view: Place the baby seat by a window (but only if it has a window guard and only when you’re supervising closely) or in front of a mirror, lay baby in the middle of the living room carpet to survey the action or in the middle of the bed to watch you fold the laundry, or park the stroller in the kitchen while you prepare dinner.
Whatever you do, remember the most important rule of stimulating your baby: The play’s the thing. And the play should be fun.
