How to Treat Special Skin Problems
Where skincare really gets complicated is when you’re dealing with more than one skincare issue. We mentioned in the previous chapter that combination skin, as we define it, is more than just having dry skin in some areas and oily skin in others. As we see it, combination skin can encompass far more. Anytime you’re dealing with more than one skincare concern, we think that’s exactly what combination skin is all about, and why people are so confused about whether this is their skin type or not. In reality, most people have some kind of combination skin because most can have a variety of issues at the same time.
The skin conditions mentioned in this chapter can be present with any number of other skincare problems/concerns. It’s important to realize that the medications or skincare recommendations below will need to be combined with other skincare recommendations in this book as part of a comprehensive daily skincare routine that contains core products suitable for your skin type AND the corresponding products needed to address your skin concerns.
These corresponding products should have textures that work with your skin type; for example, if you have oily skin and brown spots, use a lotion or gel-based skin lightener rather than a skin-lightening cream that’s better suited for dry skin. Treatment products labeled “for all skin types” generally have lighter textures because they are more versatile and easier to combine with other products in your routine.
Rosacea
Rosacea is a chronic, inflammatory skin condition of the face characterized by areas of pink to red color (called flushing) often spread out in a butterfly pattern over the nose and cheeks. In time, rosacea often progresses to the chin and central part of the forehead, too. In the beginning, this flushing can come and go, but over time it becomes increasingly persistent and will eventually stay. For some people, the flushing can be accompanied by bumpy skin, as well as acne breakouts or blackheads and oily or dry skin. Now that’s a dilemma!
Quite typically, rosacea-affected skin starts off being sensitive, but sometimes not. In almost all rosacea cases, skin sensitivity shows up at some point down the road, and tends to progressively worsen without treatment. Often those with rosacea react strongly to internal or external changes in temperature as well as to eating spicy food. Rosacea is a very temperamental, frustrating skin disorder, and it happens to a lot of people! [141]
Rosacea affects primarily adults, usually between the ages of 30 and 60. It affects all segments of the population, but is most common in people with fair skin tones, especially those who tend to blush easily. In fact, depending on whose statistics you want to believe, it can afflict somewhere between 30 and 50 percent of the Caucasian population! Women are diagnosed with rosacea more frequently than men, but men tend to experience more severe symptoms, such as a swollen, distended nose area and more broken capillaries. The diagnosis differential between men and women can be at least partially accounted for because women are more concerned about their skincare problems and are more willing to see dermatologists for treatment than men. Guys, if you think you have rosacea, it’s not something you have to “tough out.” An increasingly red, ruddy complexion can be made better—and it’s not the least bit unmanly to take steps to improve what you don’t like about your skin!
Left untreated, the sensitivity of rosacea-affected skin can go off the charts, reacting to a random mix of stimuli, from the most gentle skincare products to sipping an iced tea.
We mentioned that those with rosacea can also have skin that’s oily or dry (or both), with persistent flaking. The acne-like bumps that tend to accompany rosacea typically don’t respond to over-the-counter or prescription acne treatments; in fact, such products may cause rosacea to become more inflamed and red, either immediately or later on. Adding to these frustrating symptoms is that some people who have rosacea also get acne, and while traditional treatments work to control the acne, they make the redness and sensitivity from rosacea worse, leaving the person feeling torn between not treating the acne so as not to worsen their rosacea, or treating the acne at the expense of making their rosacea worse.
No question—treating rosacea isn’t easy and there’s no known cure, but following the steps we present will get you closer to the beautiful, calm skin you want. First, let’s discuss what causes rosacea, and then, most important, we’ll tell you how to treat it.
What Causes Rosacea?
One of the main reasons there have been such problems finding a cure for rosacea is that no one knows, or at least not everyone agrees on, exactly what causes it. Many researchers think there’s a genetic component to the development of rosacea. Others believe that elevated levels of an inflammatory peptide called cathelicidin or high levels of an enzyme known as KLK5 in the skin’s uppermost layers play a role. [142,143]
Another theory is that a mite commonly found on human skin, Demodex folliculorum, triggers the inflammation that leads to rosacea. Research has shown that those with rosacea tend to have a finer layer of superficial blood vessels in their facial skin, and that these vessels are hypersensitive to internal and external factors. [144,145]
Last, some researchers believe that those with rosacea have a thinner, more delicate surface barrier than normal. Think of the skin’s layers like the layers of an onion: On rosacea skin, the barrier is akin to the onion’s paper-thin skin; on skin without rosacea, there are more layers (literally, thicker skin) offering enhanced barrier protection and, in turn, less reactive, more resilient skin. [146]
Though it’s interesting to know the probable causes of rosacea, it really isn’t helpful because no matter what you believe about the origins of the problem, it will take experimentation to see what skincare routine and what prescription options will reduce and possibly even eliminate your symptoms. It won’t be a cure, so consistency of treatment is vital. The rest of this chapter deals with what you can consider doing and not doing to improve your skin’s condition.
Let’s start with the lifestyle issues that can make rosacea worse. Basically, anything that causes a rush of blood to the face can be an issue. All of the following are triggers.
- Sun exposure.
- Wind.
- Hot climates.
- Heavy or strenuous exercise.
- Emotional stress (or just emotions in general).
- Specific cosmetic ingredients, such as fragrant plant extracts or oils; various forms of mint and citrus; denatured alcohol, and witch hazel.
- Topical steroid creams and other topical medications that can thin the skin.
- Spicy foods, alcohol, coffee, or caffeinated teas, and hot beverages in general.
- Reactions to certain fabrics that might brush against your face, like wool or textured, scratchy-feeling fabrics. [146]
That’s quite the lineup—and it’s not even the entire list. Although some triggers are more obvious than others, it’s hard to know what will spark a rosacea flare-up for you, as it can differ from case to case. What’s on the list above may or may not apply to you and there may be other things that do serve as triggers but that aren’t on our list. The variations of problems someone with rosacea may encounter is one of the stranger aspects of this disorder.
Types of Rosacea
Making rosacea even trickier to address is that it doesn’t manifest itself in just one way; just like there’s more than one type of acne, there’s more than one type of rosacea! In its earliest stages, rosacea can be so subtle and fleeting that many people don’t even know they have it. They tend to think they just have an uneven skin tone or sensitive skin instead of an actual skin disorder. That’s a drawback because the sooner you catch and treat rosacea, the easier it will be to control the symptoms and, more important, to stop its progression!
From subtle beginnings to more advanced cases, here are the four different types of rosacea.
Erythematotelangiectatic: This long and hard-to-pronounce name is the most basic type of rosacea. It’s characterized by flushing and persistent redness, often in a butterfly pattern on a person’s nose, cheeks, forehead, and chin. Blood vessels under the skin may also be visible, and often are referred to as broken capillaries or spider veins. The affected skin may feel warmer to the touch than the surrounding skin, and often reacts strongly to stimuli such as steam from a hot stove or a few sips of red wine. [146,147]
Papulopustular: This form includes bumps and pimple-like eruptions in addition to redness, with some of the bumps becoming infected with acne-causing bacteria. This is what people mean when they say they have acne rosacea. As we stated above, oftentimes, conventional acne treatments only serve to make the redness and extreme sensitivity worse. [146,147]
Phymatous: Most common in men, this type of rosacea involves a thickening of the skin and hyper-growth of facial blood vessels, which can result in a bulbous nose from the excess growth of tissue in this area. Legendary comedian W. C. Fields, famous for his large nose, had this disfiguring type of rosacea. [146,147]
Ocular: This type of rosacea affects the eyes. Symptoms include dry eyes, tearing and burning, a sensation of the eyes feeling gritty, swollen eyelids, recurring sties (an inflammation of the eyelash hair follicle)—and even potential vision loss. Ocular rosacea often exists with another type of rosacea, so you’re battling skin symptoms plus itchy, irritated eyes. If you suspect you have this type of rosacea, consult your dermatologist or ophthalmologist for prescription solutions. There isn’t much that can be done via skincare to control ocular rosacea, though of course avoiding fragrance and irritating ingredients will help. [146,147]
Skincare for Rosacea
Because rosacea is an unpredictable skin disorder, with just about anything capable of setting it off or creating extreme sensitivity, it’s critical to assemble the most gentle skincare routine possible so as not to aggravate matters. All skincare products should be fragrance- and dye-free. “Fragrance-free” means avoiding fragrant plant oils, too, which surprisingly, and disturbingly, often show up in products labeled as being safe for sensitive skin. For example, lavender oil and citrus oils are definite no-nos due to the volatile fragrance components they contain! [148]
A skincare routine for anyone with rosacea must do the following:
- Eliminate irritating or sensitizing ingredients, which may include otherwise benign ingredients not known to be irritating (but they are for your skin).
- Include calming products that reduce redness and soothe skin.
- Improve cell turnover to remove the buildup of dead skin cells.
- Protect from sun damage without causing irritation.
- Fight wrinkles with products containing antioxidants and skin-repairing ingredients.
- Absorb oil if skin is oily, but not to the point where skin becomes dried out.
- Provide a steady stream of barrier-repair ingredients to help skin become more resilient, less reactive, and have a smoother surface. [149,150]
As is true for everyone on the planet, using sunscreen is one of the most important steps in your skincare routine! Unprotected UV exposure makes rosacea worse, so be sure to apply a sunscreen every day that’s rated SPF 30 or higher to keep those damaging rays from harming your delicate skin. [151]
Generally speaking, those with rosacea or sensitive skin should check the ingredient label when selecting a sunscreen. Ideally, you should use only sun-protection products whose active ingredients are titanium dioxide and/or zinc oxide. These mineral sunscreens are gentle and are the least likely to cause a stinging or burning sensation, both of which can worsen the redness and irritation you’re trying to minimize.
When it comes to enjoying time outdoors, don’t forget that sunscreen can’t do it all on its own. Consider sunglasses and wide-brimmed hats to further shield your face from UV radiation.
Here’s a step-by-step routine you can follow to try to get rosacea under control:
- Use an extremely gentle, non-drying, water-soluble cleanser that is appropriate for your skin type. Choose an emollient lotion or cream cleanser if you have dry skin and a thin-textured, gel, foaming, or soft lather cleanser if you have oily or combination skin. No soaps or bar cleansers!
- Soothe and reduce redness with a gentle, fragrance- and alcohol-free toner that’s loaded with anti-irritants and barrier-repair ingredients. This step may seem like extra work, but it can make a HUGE difference in the appearance and comfort of reddened, sensitized skin.
- During the day, apply a sunscreen with SPF 30 or greater whose only active sunscreen ingredients are titanium dioxide and/or zinc oxide, along with healing ingredients such as antioxidants and skin-repairing ingredients. If you have dry skin, choose a more emollient, creamy sunscreen; if you have oily or combination skin a more fluid, lotion texture is optimal. If your combination skin has markedly dry areas, layer a regular cream moisturizer or richer serum underneath your sunscreen only on the dry areas.
- For extra sun protection (and we love extra protection), if you normally wear foundation and pressed powder, select those that have sunscreen. Stick with makeup with sunscreen whose only active ingredients are titanium dioxide and/or zinc oxide as they present little to no risk of irritation. Look for foundation and pressed powder with sunscreen rated SPF 15 or greater, and be sure your daytime moisturizer is rated SPF 30 or greater.
- If you have rosacea with oily or combination skin and breakouts, makeup with sun protection can be the only sunscreen you need (though in that case try to find makeup rated SPF 30). If you have dry skin and rosacea, you can wear a moisturizer with sunscreen under makeup to add a layer of protection or a moisturizer without sunscreen and then the foundation with pressed powder and SPF. There are many foundations and powders with mineral sunscreen actives, so you’ll have plenty of options!
- If you have oily or combination skin, in the evening apply a gel moisturizer or a light serum formulated with antioxidants and skin-repairing ingredients. A serum with retinol is fine because retinol has research showing it helps reduce the inflammatory factors that contribute to rosacea. [152,153] You’ll probably need a separate, more emollient moisturizer for around the eyes because a gel or light serum is usually not enough for that area.If you have normal to dry skin, in the evening use a lotion or cream moisturizer formulated with soothing antioxidants and skin-repairing ingredients. It’s OK if it contains retinol. You can also use a serum over or under your moisturizer for extra hydration, redness reduction, and protection.
- Regardless of your skin type, you’ll want to consider using a BHA (salicylic acid) exfoliant once or twice a day. It takes experimenting to see what strength and frequency of application works best for you. BHA not only exfoliates skin, but also has anti-inflammatory properties that reduce redness and eliminate dry, flaky skin. BHA also works amazingly well if you have rosacea and acne or blackheads!
- Check with your physician to see which prescription medication is best to treat your rosacea. Topical options include MetroGel®, MetroLotion®, Tazorac®, Renova, azelaic acid (brand names Azelex® or Finacea®), brimonidine, doxycycline, isotretinoin, and low-dose minocycline. Oral options include tetracycline and metronidazole. These are considered the most reliably researched medical options. [152,153,154]
All of the topical medications should be applied as directed by your physician. Our strong recommendation is to apply any topical medication in the evening as the last step of your skincare routine, following your cleanser, toner, exfoliant, moisturizer, and/or serum. During the day, apply the topical medication before the sunscreen. Sunscreen is always the last skincare product you apply so as not to dilute its effectiveness.
Products to Eliminate if You Have Rosacea
Aside from what you should use if you have rosacea, it’s critical that you eliminate the parts of your normal skincare routine that increase inflammation and worsen or trigger redness, such as the following.
- Harsh cleansers such as bar soap, bar cleansers, and cleansing scrubs.
- Drying liquid or lotion cleansers. (If your face feels squeaky clean after use, the product is too drying for your skin!)
- Toners with alcohol, witch hazel, rosewater, and fragrance.
- Abrasive scrubs.
- Rough washcloths or facial brushes such as the Clarisonic; the “sensitive” brush head of the Clarisonic is an option, but be aware that even that might cause a reaction.
- At-home facial peels, especially high-strength peels.
- Using too many products at the same time, particularly anti-aging products that contain higher amounts of active ingredients like vitamin C.
- Retinol products, especially high-strength formulas, may be problematic, but retinol products with lower concentrations are usually well tolerated. As mentioned above, some research has shown retinol to be helpful for those with rosacea; however, you’ll want to be cautious with products whose retinol concentration exceeds 0.5%. [150,155]
Prescription Treatments for Rosacea
Because rosacea is a chronic condition with no known cure, you’ll most likely need to see a doctor to get it under control. The reality in most cases is that skincare alone won’t be enough. A good dermatologist should know about the latest prescriptions and in-office treatments and techniques for dealing with rosacea, and can properly diagnose what type you have. Following are a few more details about the variety of medical treatments available for rosacea.
- Oral antibiotics like tetracycline or low-dose doxycycline (brand name: Oracea®) can relieve acne-like pustules and inflammation without aggravating rosacea symptoms. [152,153,154]
- Topical antibiotics, including metronidazole, have been shown to be effective in killing Demodex folliculorum and other microbes that may play a role in rosacea. MetroCream®, MetroGel®, and MetroLotion® contain this active ingredient. Your dermatologist or physician will prescribe based on the texture you prefer, which will be partly based on your skin type (dry, oily, and so on). [153,154,155]
- Prescription-strength azelaic acid (brand names Finacea® or Azelex®) can help reduce lesions and bumps and is also believed to play a role in controlling the inflammatory process that triggers rosacea. [153,154,155]
- Mirvaso® Gel is a prescription product from the Galderma brand (of Cetaphil fame). It’s FDA-approved for treating persistent redness from rosacea. Although how this drug works isn’t exactly clear, researchers believe it constricts the blood vessels that fuel facial redness, with results lasting up to 12 hours. Its chemical name is brimonidine, and, like all topical medications, it has side effects you must discuss with your doctor, particularly if you have circulatory system issues. [153,154,155]
- Beta blockers (prescribed in pill form; typically used to treat heart conditions and high blood pressure) have been shown in some studies to reduce rosacea’s redness. [152]
- The vitamin A drug isotretinoin, both oral and topical, can be effective. Oral isotretinoin was first marketed as the anti-acne drug Accutane, but has been shown to help combat the pustules seen in papulopustular rosacea, although this oral medication typically is a last resort due to its many serious side effects. [156] Topical isotretinoin also has been shown to be effective, with far less severe side effects than the oral version. [154]
- Salicylic acid, also known as beta hydroxy acid (BHA), is not a medical solution, but we feel so strongly about its potential benefit that we include it in this list. Topical salicylic acid in 1% and 2% strengths has anti-inflammatory properties that can potentially reduce redness. It also gently exfoliates rosacea-affected, breakout-prone skin, which can mitigate the flakiness and/or breakouts that can occur with some forms of rosacea. BHA also has antimicrobial properties, and that can be helpful in reducing the microbes that may be associated with rosacea. [31]
Light-Based Treatments for Rosacea
Some of the best and most effective treatments for rosacea involve using light to target the blood vessels that cause the “red mask” and broken capillaries that are the hallmarks of rosacea. Special lasers or intense pulsed light (IPL) machines target capillaries and can diffuse redness in the upper layers of the skin. These light-based treatments cause the walls of blood vessels to heat up, which damages them, causing them to be absorbed by the body as part of its natural defense.
The catch? Repeated treatments (typically 4–6 spaced a few weeks apart) are required for the redness to disappear completely, and most people will need a maintenance treatment at least once per year. These light-based treatments aren’t cheap—they can cost as much as $300 to $700 per treatment, and medical insurance often doesn’t cover the expense (check with your health insurance provider).
Weighing the benefit versus the cost of light-based treatments is obviously a personal decision, but given the potential improvement, both to your skin and your self-esteem, it’s something that should be given consideration. [157,158]
Summing It Up
Although there’s no simple, works-for-everyone solution for rosacea, you can take action and control its most telltale symptoms. Through trial and error, rosacea can be brought under control—no more hiding, no more embarrassment. Male or female, if you have rosacea, see your dermatologist for medical treatments (they will be needed), and keep your skincare routine gentle, gentle, gentle!
RECOMMENDED PRODUCTS FOR ROSACEA:
The products below include various cleansers, toners, moisturizers, and mineral-based sunscreens that we feel strongly are worth trying if you have rosacea. Because rosacea-affected skin can be incredibly finicky and capable of reacting to the most benign formulas, coming up with a definitive list is tricky and, unfortunately, not a sure thing. Therefore, please consider these recommendations knowing that, based on the frustrating nature of rosacea, your skin may respond unfavorably.
Cleansers
- Eucerin Redness Relief Soothing Cleanser ($8.79)
- First Aid Beauty Milk Oil Conditioning Cleanser ($26)
- Neutrogena Ultra Gentle Hydrating Cleanser, Creamy Formula ($8.99)
- Olay Foaming Face Wash, Sensitive Skin ($4.99)
Toners
- Bioelements Calmitude Hydrating Solution ($30)
- Paula’s Choice Resist Advanced Replenishing Toner ($23)
BHA Exfoliants
- Paula’s Choice Skin Perfecting 1% BHA Lotion ($26)
- Paula’s Choice Skin Perfecting 2% BHA Liquid ($28)
- philosophy clear days ahead oil-free salicylic acid acne treatment & moisturizer ($39)
Daytime Moisturizers with SPF
- Exuviance Sheer Daily Protector Sunscreen Broad Spectrum SPF 50 ($42)
- MDSolarSciences Mineral Creme Broad Spectrum SPF 30 UVA/UVB Sunscreen ($30)
- Paula’s Choice Resist Super-Light Daily Wrinkle Defense SPF 30 ($32)
- Paula’s Choice Skin Recovery Daily Moisturizing Lotion SPF 30 ($28)
- Rodan + Fields Soothe Mineral Sunscreen SPF 30 ($41)
Moisturizers and Serums
- Arbonne Calm Gentle Daily Moisturizer ($36)
- Dr. Dennis Gross Skincare Hydration Super Serum Clinical Concentrate Booster ($68)
- Elizabeth Arden Ceramide Capsules Daily Youth Restoring Serum ($74)
- Olay Regenerist Micro-Sculpting Serum, Fragrance-Free ($23.99)
- Paula’s Choice Calm Redness Relief Serum ($32)
- Paula’s Choice Resist Intensive Repair Cream ($32)
- Paula’s Choice Resist Intensive Wrinkle-Repair Retinol Serum ($40)
- Replenix Power of Three Cream ($70)
Brown Spots
Regardless of your ethnic background or skin color, eventually most of us will struggle with some kind of brown or ashen pigmentation problem. The primary, if not exclusive, cause of these spots is sun damage. Skin will either appear lighter or darker than normal in concentrated areas, or you may notice blotchy, uneven patches of brown to gray discoloration or freckling.
No matter when or where these spots show up, chances are good that you want to get rid of them! Brown spots pop up on areas of skin that are always exposed to sun, and even if we try to be diligent about sun protection, years of prior unprotected and prolonged exposure to the sun will add up. But before we discuss treating brown spots, it’s critical to understand more about how they got there in the first place!
What Causes Brown Spots?
Skin pigmentation problems occur because the body produces either too much or not enough melanin. Melanin is the pigment in skin; it’s produced by specific cells known as melanocytes. An enzyme called tyrosinase, which is the catalyst that creates the melanin responsible for the color of our skin, eyes, and hair, triggers it. Excess melanin production is caused primarily by chronic unprotected sun exposure or by hormones (particularly during pregnancy or from taking birth control pills). [159,160]
As far as skin is concerned, depending on how much melanin is present, it provides some amount of sun protection by absorbing the sun’s UV light and functioning as a built-in antioxidant. This explains why darker skin colors are less susceptible to sunburn and to the overall inflammatory, aging effects of sun damage. But, “less susceptible” does not mean “immune from problems.” Also, for those who think getting a tan means you’re getting protection from the melanin changing your skin’s color, you’re not! Tanning is the skin’s response to damage, not a sign you’re getting better protection!
Treating Brown Spots Begins With Sunscreen!
Without question, the first line of defense is sun-smart behavior, which means avoidance or, at the very least, careful exposure to UV light, and daily use (365 days a year) and liberal application (and, when needed, reapplication) of a well-formulated sunscreen. [161,162] Diligent use of a sunscreen alone allows for some repair as well as protection from further sun damage, which is what created the problem in the first place. [163] This is true for everyone!
No other aspect of controlling or reducing skin discolorations is as important as being careful about exposing your skin to the sun and using sunscreen, SPF 30 or greater, that includes the UVA-protecting ingredients of titanium dioxide, zinc oxide, avobenzone, Mexoryl SXTM (ecamsule), or Tinosorb listed as active. Using effective skin-lightening products, exfoliants, peels, or laser treatments without also using a sunscreen will prove a waste of time and money. Sun exposure is one of the primary causes of the skin discoloration disorder melasma, and treatments cannot keep up with the sun’s daily assault on the skin. [164] Before you look at any other option for brown or ashen skin discolorations, start by applying sunscreen and reducing sun exposure. By “reducing exposure,” we don’t mean just spending less time in direct sunlight or tanning only in the early morning hours; it’s about never getting a tan (indoors or out) and taking other precautions such as wearing a hat, sun-protective clothing, and sunglasses—each time, every time, from now on!
Scary but important fact: One bout of unprotected sun exposure can undo months of progress with a skin-lightening product. [165] There’s simply no room for compromise here: Sun protection and skin lighteners are a package deal. When it comes to treating brown spots, one cannot work well without the other—both play critical roles in lightening the brown spots you see now AND preventing those you don’t want to see later! It almost goes without saying, but we’ll say it anyway: No skin-lightening routine will give you the results you want if you continue to get a tan; even “a little sun” can stall or reverse months of progress toward getting you the even skin tone you want. Stated bluntly: Failure to comply here can’t be blamed on the skin-lightening product not working. You have to be willing to commit to avoiding further sun damage.
Skin-Lightening Options
The most successful brown spot treatments use a combination of topical lotions or gels containing melanin-inhibiting ingredients along with a well-formulated sunscreen, and a prescription retinoid (such as Renova or generic versions containing tretinoin, a type of retinoid). [160] Depending on how skin responds to these treatments, exfoliants, either in the form of topical skincare products or chemical peels performed by a physician, can also be included. Then there are lasers or intense pulsed light treatments to enhance the results from topical treatments and, in many cases, pick up where the topical treatments leave off. [166]
Topical hydroquinone is considered the gold standard for reducing or eliminating skin discolorations. [167] Despite the controversy surrounding the hydroquinone* ingredient, topical application has extensive research indicating it is a safe and effective treatment for brown skin discolorations for those with lighter skin tones, and many dermatologists agree. Topical hydroquinone in 2% concentrations from cosmetics companies is available over-the-counter, and 4% concentrations are available by prescription, and are definitely to be considered.
Plant extracts, such as Uva ursi (bearberry) extract, Morus bombycis (mulberry), Morus alba (white mulberry), and Broussonetia papyrifera (paper mulberry), as well as the plant extract arbutin are touted as being natural skin-lightening agents that don’t have the problems (or at least the bad reputation) associated with hydroquinone. Ironically, these plant extracts actually break down into hydroquinone when absorbed into skin, which explains why they have a positive effect on brown discolorations. [168]
*See Chapter 16, Cosmetic Ingredient Dictionary, for information on the controversy surrounding hydroquinone.
Some research has shown that topical azelaic acid in 15% to 20% concentrations is as efficacious as hydroquinone and has a decreased risk of irritation. [169,170] Tretinoin by itself has also been shown to be especially useful in treating hyperpigmentation of sun-damaged skin. Kojic acid, alone or in combination with glycolic acid or hydroquinone, has shown good results due to its inhibitory action on tyrosinase; however, kojic acid has had problems in terms of stability and potential negative effects on skin and is rarely used nowadays. [171]
Several other plant extracts and many types of vitamin C (especially ascorbic acid) also have research showing them to be effective for inhibiting melanin production. [172] All of the above are valid considerations for those who want to avoid hydroquinone, or they can be used with hydroquinone, a combination that could provide even better results!
What to Expect When You Begin Using a Skin Lightener
Of course, the obvious expected (and desired) result from using a skin lightener is for the dark or brown spots to get lighter, right? And, if they fade completely, hey, that’s even better! With once- or twice-daily usage, you can reasonably expect a well-formulated skin-lightening product that contains proven ingredients to progressively lighten your dark spots. But, pack your patience (we know, easier said than done)!
Sadly, the lightening won’t happen overnight, and it’s important to keep that in mind. While we completely understand the desire to see those spots fade NOW, the truth is that it took several years of ongoing daylight exposure for the spots to form deeper in skin and then to show up on the surface. So, it stands to reason these slow-to-form brown spots will require patience and persistence as you wait for them to fade.
Most of us will need to use a lightening product every day, morning and evening, along with daily application of a great sunscreen rated SPF 30 or greater for at least 3 months before we see significant results. Some people do see results sooner, but maximum improvement and continued maintenance is a commitment to using these products regularly. None of these products are a cure.
As stated earlier in this section, but it bears repeating: What you shouldn’t expect from a skin lightener is for it to work if you continue to expose your skin to UV light without sun protection or if you continue to tan, whether from sunlight or, even worse, in a tanning bed. No skin-lightening product will be effective if you’re not willing to protect your skin daily from further UV damage. And, if you want to keep tanning, sorry, a skin lightener won’t work at all—and it’s not because the product is faulty. Sun protection (some dermatologists also stress sun avoidance) is a key part of lightening brown spots and preventing new ones from developing.
To repeat: The bottom line concerning getting rid of brown spots—if you’re not willing to commit to daily sun protection and to not tanning no matter what, there’s no sense in using any skin-lightening product. You’ll be steadily undoing what they’re trying to fix! Two steps forward, one step back isn’t the way to get the best skin of your life—and that’s what we want you to have!
Why You May Need More Than One Skin-Lightening Product
Even if you’re using one of the best skin-lightening products out there and being diligent about daily sun protection, you may not see much, if any, improvement in your dark spots. Why? Simply put, some discolorations are rooted deeper in the skin and, as a result, are much more stubborn and slower to respond to topical treatments.
What to do? Consider seeing a dermatologist for a series of light-emitting or laser treatments; using a prescription product with a higher amount of hydroquinone and/or a retinoid; or having a series of chemical peels—or all of these, spaced out over time. But, before you make an appointment, consider adding a second—or, potentially, a third—lightening product to your routine and see how your brown spots respond after several more weeks (sigh ... see what we mean by needing patience?).
Research has shown that for some people, a combination of active skin-lightening ingredients is needed for optimal results. [173,174] Hydroquinone or vitamin C alone might not be enough, but those two ingredients layered with products that contain other brown spot–fighters (and sunscreen, of course) may be the perfect combination to finally fade those brown spots.
ADDING A SKIN-LIGHTENER TO YOUR ROUTINE
OK, so you’re ready to add a skin-lightening product to your skincare routine. Here’s how to work it in to the skincare routines discussed earlier in this book:
Morning
- Cleanse your face.
- Apply toner (if used; if not, skip to Step 3).
- Apply your AHA or BHA exfoliant.
- Apply the skin-lightening product to the affected areas or all over your face. A lightweight lotion or gel can work for all skin types and layers well with Steps 5 and 6.
- Apply serum. (If you have oily or combination skin you may want to reserve this step for evening only.)
- Apply daytime moisturizer with sunscreen. Eye cream, if used, should be applied before sunscreen unless the eye cream provides sun protection.
Evening
- Cleanse your face.
- Apply toner (if used; if not, skip to Step 3).
- Apply your AHA or BHA exfoliant. If you prefer to apply your exfoliant only in the morning, skip to Step 4.
- Apply the skin-lightening product to the affected areas or all over your face.
- Apply serum and/or a nighttime prescription treatment, such as a retinoid.
- Apply nighttime moisturizer and/or eye cream.
You do not need to wait for the exfoliant to set or dry before you apply the skin lightener, but it’s fine to do so if that’s what you prefer. The same goes for applying serum over the skin lightener and the moisturizer (with or without sunscreen) over the serum.
What if you’re also using a topical anti-acne product? Apply it before the skin lightener, either all over or just to the breakout-prone areas, morning and/or evening—whichever frequency of application you find works best to control your breakouts.
What if you’re using more than one skin-lightening product? Simple: You can apply them in succession. Which one you apply first doesn’t matter, but it helps to go from the lighter texture to the heavier texture; for example, liquid before lotion. It’s also fine to apply one skin lightener in the morning and another one at night. Experiment to find what works best for you. There’s no reason not to go after those brown spots with every potential ingredient proven likely to make a visible difference!
Laser Treatments for Brown Spots
Both ablative and nonablative lasers and light treatments administered by a dermatologist can have a profound positive effect on melasma and brown spots. However, the results are not always consistent, and problems can occur (such as hypo- or hyperpigmentation).
Laser treatments of this kind often are a problem for those with darker skin tones. Nonetheless, when laser treatments work, they can make a remarkable difference in the skin’s appearance, especially when used in combination with the topical treatments previously mentioned. The results from lasers can be amazing and, although expensive, are absolutely worth a try for stubborn discolorations. There are many types of lasers that can be used for this purpose. Which one is optimal for you is best determined by a skilled dermatologist who has a practice that incorporates a variety of different lasers and/or light-emitting devices. Don’t get caught up in a search for the perfect laser for your brown spots; in almost all cases, it’s wasted energy because there usually are several options that might be equally effective. [166]
As effective as laser treatments can be, they’re not cures. If you don’t continue to follow the absolute rules—daily sun protection, use of melanin-inhibiting skincare products or topical medications, and not getting a tan—the brown spots will come back, no question.
Following a great skincare routine as detailed above will be helpful in improving brown skin discolorations, along with keeping it healthy and protected from further UV damage. In terms of inhibiting brown discolorations, the following are the best products we’ve found that contain well-researched ingredients that really can make a difference.
RECOMMENDED PRODUCTS FOR TREATING BROWN SPOTS:
- Alpha Hydrox Spot Light Targeted Skin Lightener ($9.99; hydroquinone)
- Black Opal Even True Tonecorrect Fade Creme ($10.95; hydroquinone)
- Black Opal Tri-Complex Tonecorrect Fade Gel ($12.95; hydroquinone)
- Dr. Dennis Gross Skincare Ferulic Acid & Retinol Brightening Solution ($88; arbutin)
- Olay ProX Even Skin Tone Spot Fading Treatment ($39.99-$44.99; niacinamide)
- Osmotics Lighten FX 3x Dark Spot Remover ($64; arbutin + niacinamide)
- Paula’s Choice Resist Pure Radiance Skin Brightening Treatment ($32; niacinamide + vitamin C)
- Paula’s Choice Resist 25% Vitamin C Spot Treatment ($55; vitamin C)
- Peter Thomas Roth De-Spot Plus ($78; hydroquinone)
Milia/Whiteheads
Milia is the technical term for small, hard, white bumps that are rarely swollen or inflamed, and that don’t change much once they show up—mostly on the face—in just about anyone, including infants, teens, and adults. These frustrating yet benign bumps are incredibly stubborn, and can last for weeks, months, and sometimes longer!
Though milia aren’t harmful in any way, getting rid of them can be tough. There’s a right way and a wrong way to remove them—and the wrong way can damage your skin. Following our recommendations should help you safely get rid of the bumps you have and possibly keep them from ever coming back!
Milia Are NOT Pimples!
If you’ve had milia, you likely wondered if they were some kind of pimple. While many people mistake the tiny, pearl-like bumps for acne, they’re not the same thing. One of the easiest ways to identify milia bumps is by how they feel and look.
Unlike acne, milia are rather firm, and squeezing has little or no impact on them. Also unlike acne, these bumps can show up around the eyes and on parts of the face where there aren’t active oil glands. Milia also don’t have the pain and redness associated with acne nor are they due to inflammatory factors within skin. When a pimple forms, it quickly becomes inflamed, red, and sore; that doesn’t happen with milia. In fact, milia just tend to sit there, minding their own business! [175]
Yellow Bumps Under the Eyes?
If you have yellowish, slight to obvious bumps without a depressed center around your eyes and/or on your eyelids, they aren’t milia (which typically are a translucent flesh to white color). Instead, you may be dealing with a skin growth known as xanthoma. These bumps are common in people who have high cholesterol or high triglyceride levels. See your health care provider for a lipid panel, a test that involves drawing blood to analyze it for the amount of cholesterol and triglycerides that may be causing the bumps. Reducing the health problems associated with xanthoma can reduce the number and size of the bumps. [175]
What Causes Milia?
Milia occur when dead skin cells clump together and get trapped under the skin’s surface, forming small, hard cysts. It’s estimated that nearly 50% of infants in the United States get milia, in part because their young skin is still “learning” to exfoliate. As their skin matures, the milia will disappear on their own, no treatment necessary. Doctors don’t consider infant milia a problem, and rarely prescribe treatment for it. Parents may find the bumps unsightly, but the baby isn’t bothered by them, and they have no impact on the baby’s health. [175]
Adults can get two forms of milia, most often seen on the cheeks and forehead: primary and secondary. Primary is the same type seen in babies, caused by skin cells that build up in the pore lining because they just didn’t shed properly. Secondary milia occur when a skin condition or infection (such as herpes) that leads to blistering actually damages the pore lining. Burns or severe rashes can increase the number of skin cells trapped under the skin’s surface, resulting in milia that form even after the trigger has faded. [175]
Sun damage is a contributing factor to milia because it makes skin rough and leathery, so it’s more difficult for dead cells to rise to the skin’s surface and shed normally. Clogs will ensure milia show up, and as mentioned they tend to stick around. [175]
Many people believe heavy moisturizers, foundations, or makeup in general are responsible for the problem, but that’s highly unlikely. Given that 50% of all babies get milia, and men do as well, it clearly isn’t related to skincare or makeup products. [175] Of course, if you’re still concerned, you can experiment with changing your product selection or application method to see what works for you.
Treating and Preventing Milia
Because milia often go away on their own without treatment, being patient and waiting it out is an option—but waiting is definitely not for everyone!
Because milia form when the skin’s natural exfoliation process malfunctions, using a targeted exfoliating treatment with salicylic acid on a regular basis will immediately improve exfoliation. It may also allow the bump to dissolve on its own (relatively quickly, too) and prevent new ones from forming. [175]
If using a leave-on BHA exfoliant doesn’t help, then you might consider seeing a dermatologist who can tell you which type of milia you have and perhaps even remove them right there in the office. Using a needle or a tiny lancing utensil, a dermatologist can easily remove the milia, leaving very little damage to skin and ensuring a fast healing time. [175]
Skincare for Treating Milia
Although there’s not much you can do to prevent milia, maintaining a suitable skincare routine certainly helps minimize the chance of them appearing. Because deeper or larger milia can be caused by sun damage, always use a daytime moisturizer with SPF 30 or greater to protect your skin every day. This will give those annoying white bumps less of a reason to set up shop on your face!
Milia are a real pain to put up with, but there are things you can do to treat these white bumps. Remember: Patience, daily exfoliation, sun protection, and resisting the temptation to (literally) take matters into your own hands (unless you follow our suggestions) can go a long way toward having clearer, bump-free skin sooner!
Removing Milia at Home
Removing milia at home is not for the faint of heart, or for those who tend to be overly aggressive with their skin. It also isn’t something we encourage, but knowing that some of you will try it anyway, we figured we might as well explain how to do it the right way. Removing milia yourself is not like “popping” a pimple. In Chapter 7, Stop Acne and Breakouts (No Matter Your Age), we explain how popping a pimple the right way (emphasis on the right way) not only gets rid of the unsightly red swelling and white sac, but also reduces the inflammation by releasing the pressure inside, and speeds up healing.
Milia are not pimples; in fact, in many ways they are completely unrelated. Unlike pimples, which for the most part can release somewhat easily on their own, milia actually need to be excised and that is more risky to your skin than popping a pimple, which is why doing it the right way is even more important.
There is only minimal benefit to be gained from removing milia, other than the aesthetics, of course. If aesthetics is important to you, we understand why you want to remove milia, and, just as with pimples, it’s not always realistic to see a physician every time you get one. So, for those of you who aren’t going to spend the money to see a physician to remove milia and are determined to do it yourself, here are the steps you need to take to do it the right way and minimize the risk to skin.
One important caveat: Our strong warning is that if you have many milia all at the same time, as opposed to just one or two that occur intermittently, don’t even begin to do it yourself; it is best to see a physician. The risk of trying to remove lots of them all at once by yourself is just too great. Again, you really could make a mess of things.
Excise means you need to make a tiny tear in skin, directly on top of or near the milia, and then literally lift it out of skin with tweezers or use a comedone extractor with only slight pressure. Here are the steps to follow:
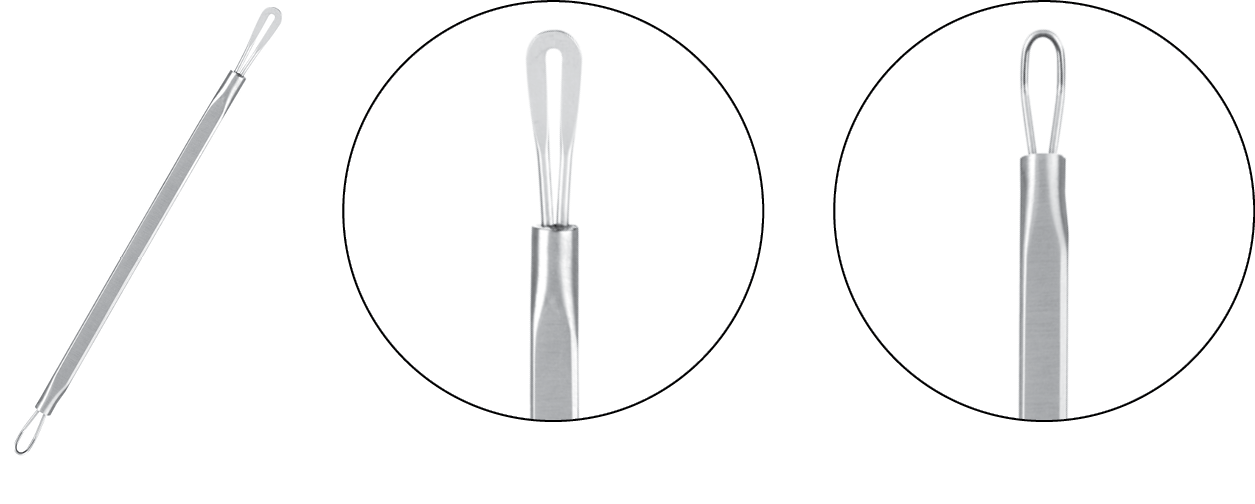
- Make sure you have on hand a sharp needle, very pointed tweezers (flat-ended tweezers will not work!), and/or a comedone extractor. You can buy a comedone extractor from Paula’s Choice or at Sephora. Here’s what it looks like:
- Cleanse your face with a gentle water-soluble cleanser. Use tepid to warm water (not hot or cold, both of which are damaging to skin).
- Before rinsing, lightly massage skin with a soft, wet washcloth or a Clarisonic to remove dead skin cells from the surface to make excision and removing the milia easier. Do NOT over-scrub because that can damage your skin even before you’ve started.
- Dry skin gently. Do not do anything before you’ve dried your skin because skin is more vulnerable to tearing and creating a scab when it is wet.
- Rub the pointed needle, tweezers, and/or comedone extractor with alcohol to prevent infection.
- Then, gently, with either the needle or tweezers, make the teeniest tear in skin, either on top of the milia or right next to it. That should give you enough access to remove the milia.
- If you’ve made the teeny tear next to the milia, then, with very little pressure, use the comedone extractor to gently (and we mean really gently) coax the milia out through the small opening. If you’ve made the teeny tear on top of the milia, use the tweezers to lift it out. That should release the contents.
- Do NOT repeat this process over the same bump more than once or you will damage your skin, so be very, very careful, and go slowly.
- Remember to be gentle and make the teeniest possible tear in skin; the goal is to remove the whitehead without creating a scab or damaging the surrounding skin (scabs are not any better to look at than milia).
- When you’re done, use a cotton swab with hydrogen peroxide or alcohol to disinfect the area. This is the only time we will ever recommend using either of those two skin-damaging products on your face (hydrogen peroxide generates free-radical damage and alcohol causes inflammation).
- You can then follow up with your usual skincare routine.
RECOMMENDED PRODUCTS FOR MILIA:
Other than a skincare routine that’s best for your skin type and other concerns, as we explain in previous chapters, treating milia is really about adding a more potent salicylic acid exfoliant to your routine and using it as a spot treatment. Unfortunately, the list of products that stand a good chance of reducing and potentially eliminating milia is very short, largely because milia are unresponsive to most skincare products.
In our experience, and the experience of others who’ve tried these products, we believe they are among the best options. Once you get your milia under control, you can use other types of exfoliants mentioned throughout this book. Of course, daily sun protection and treating skin gently remain vitally important, but that’s true for everyone!
- Paula’s Choice Resist BHA 9 ($42)
- Paula’s Choice Resist Weekly Retexturizing Treatment 4% BHA ($35)
Sebaceous Hyperplasia
If you have struggled with oily or combination skin for most of your life and are now over the age of 40, you may have noticed a series of small, stubborn, crater-like bumps with a whitish rim popping up randomly on various parts of your face. While these bumps may appear to be a type of blackhead, milia, or breakout, they aren’t. The difference is that these strange spots just don’t go away, no matter what you do. If you’re seeing these spots, chances are you have sebaceous hyperplasia.
What is Sebaceous Hyperplasia?
Sebaceous hyperplasia is the technical name for a benign bump on the skin that forms over time as a result of damage to a pore caused by unknown factors. Randomly, a damaged oil gland (and often more than one) can become enlarged and clogged in a very specific manner, displaying a soft or firm white or yellowish outer rim typically with a tiny to wide depressed center. The depressed center of these bumps is one of the primary ways you can tell you’re dealing with sebaceous hyperplasia, and not with something else such as a whitehead (milia, discussed above) or pimple.
It’s not uncommon to have several of these bumps at once, sometimes spaced apart, but they can be clustered, too. Sebaceous hyperplasia is most often seen on the forehead and central part of the face, but can appear anywhere on the body, especially in areas where the skin has more oil glands. [176]
Cumulative sun damage is considered a co-factor of this condition because sunlight further damages skin and oil glands. [177] That’s one more reason to make sure you’re protecting your skin every day with a well-formulated sunscreen! It’s also typically seen in people who have struggled with oily skin and large pores most of their lives, so getting this problem under control sooner rather than later is also important.
How to Get Rid of Sebaceous Hyperplasia
Treating sebaceous hyperplasia usually requires a visit to the dermatologist, but now there are products available you can use at home to try and get these unsightly bumps under control—at the very least, you’ll achieve noticeable improvement in skin tone and texture!
A dermatologist has several options for treating sebaceous hyperplasia. Before you consider any of them, however, know that, like many other skin disorders, sebaceous hyperplasia cannot be cured, only controlled. The bump can be reduced or eliminated, but the affected oil gland likely will produce a new bump if treatment isn’t maintained, and even then it can recur. Therefore, even if you decide to see a dermatologist for treatment, you’ll want to ensure your at-home skincare routine includes products to keep these bumps at bay, at least to the extent possible from skincare products.
When you visit a dermatologist for sebaceous hyperplasia, he or she may offer the following treatments, alone or in combination:
- Facial peels—This involves using salicylic acid or trichloroacetic acid (TCA).
- Electric needle—This causes the bump to break down and ooze, forming a scab that falls off in a week or so.
- Photodynamic therapy (PDT)—This is a light-emitting treatment where the skin is pre-treated with a special gel that reacts with the light. This option often requires several office visits.
- Liquid nitrogen—This potent option can be effective, but it’s also risky because if it penetrates too deeply, you may be left with a scar or loss of skin pigment.
- Prescription retinoid or azelaic acid—These treatments are intended to reduce the appearance of the lesions, but they won’t eliminate the problem.
- Surgical excision of the bump—This may lead to scarring, but the bump won’t recur in the excised area. This is considered a last-resort option.
- Antiandrogen medication—This reduces testosterone, which may be stimulating enlargement of the oil glands. Examples of these medications are spironolactone or flutamide. This, like surgical excision, is a last resort. [178]
Note: Some sebaceous hyperplasia bumps can resemble a type of skin cancer known as basal cell carcinoma. [179] Your dermatologist will need to examine the area to make an accurate diagnosis. If you’re unsure, don’t assume it’s not skin cancer.
Skincare for Sebaceous Hyperplasia
What about options outside the dermatologist’s office? Although treating sebaceous hyperplasia yourself can be frustrating, and in almost all cases a dermatologist’s care is required, there are a few key products to consider. Chief among them is a product we’re very proud of, one that Paula uses for her sebaceous hyperplasia, and that’s our Resist BHA 9 ($42). This clear, liquid-like solution contains a 9% concentration of salicylic acid. Despite its strength, it’s still extremely gentle due to its time-release formula. Salicylic acid penetrates the oil buildup in the pore lining, increases cell turnover by exfoliating the surface of the skin as well as inside the pore to unclog these bumps, and reduces inflammation, all of which can diminish these bumps. There’s no research directly linking salicylic acid in skincare products to treating sebaceous hyperplasia, but in theory and, as we’ve seen, in practice, it can and often does help a great deal!
You also can consider products that contain lower amounts of salicylic acid, but most cases of sebaceous hyperplasia won’t respond as well to lower strengths; however, they can be extremely beneficial for daily maintenance all over the face. Most people struggling with sebaceous hyperplasia have other bumps and breakouts that can be successfully treated with lower concentrations of salicylic acid.
Other products to consider are those that contain retinol. Research has shown that retinol, which is another name for vitamin A, either in over-the-counter skincare products or in various prescription forms such as Tazorac or Retin-A, can reshape the pore lining and restore more normal pore function and size. Retinol works to control the growth of skin cells that can clog the pore lining, and encourages normal oil production. [95,180]
These factors, plus retinol’s anti-inflammatory action, theoretically make it a powerful option to combine with salicylic acid for treating sebaceous hyperplasia.
Another skincare ingredient that may help improve sebaceous hyperplasia is the B vitamin niacinamide. This cell-communicating ingredient offers multiple benefits to skin, such as reducing inflammation and oil proliferation that accompany sebaceous hyperplasia. [181,182] Products containing salicylic acid, retinol, and niacinamide can be used once or twice daily after cleansing, and may help reduce sebaceous hyperplasia!
What about scrubs? No scrub in the world, regardless of claim or price, can remove these bumps. Sebaceous hyperplasia forms deep within the skin right at the base of the oil gland itself; scrubs simply cannot reach the source of the problem. Warning: Zealously trying to scrub away these bumps can lead to other skin issues, such as dryness, redness, and irritation.
RECOMMENDED PRODUCTS FOR SEBACEOUS HYPERPLASIA:
The list of products that can successfully treat sebaceous hyperplasia is fairly short, largely because most people dealing with sebaceous hyperplasia will require treatment from a dermatologist. These bumps rarely resolve on their own no matter what you use topically. However, skincare can play a role in terms of maintenance and in improving the appearance of sebaceous hyperplasia. The products below are those that can exfoliate inside the pore lining, unclog pores, and influence the pore lining, in the hope that they not only will reduce sebaceous hyperplasia but also prevent, to the extent possible, new bumps from forming.
- Olay Regenerist Regenerating Serum Fragrance-Free ($22.99; contains a high amount of niacinamide)
- Nia24 Skin Strengthening Complex ($93; contains a high amount of niacinamide)
- Paula’s Choice Clinical 1% Retinol Treatment ($55)
- Paula’s Choice Resist BHA 9 ($42; contains 9% salicylic acid)
- Serious Skincare A Force XR Retinol Serum Concentrate ($39.50)
- SkinCeuticals Retinol 1.0 Maximum Strength Refining Night Cream ($70)
- SkinMedica Retinol Complex 0.25 ($60)
- SkinMedica Retinol Complex 0.5 ($75)
Keratosis Pilaris (aka Chicken Skin)
Now let’s leave the face and go on to the body to discuss a very common problem. If you’re seeing large patches of little red or white inflamed bumps on the outside of your upper arms, thighs, or backside, you probably have a skin condition called keratosis pilaris. Also known as KP or as “chicken skin,” this disorder affects 50%–80% of all adolescents and almost half of all adults, though no one knows exactly why this happens or why it’s so prevalent. [183]
KP isn’t a serious or harmful medical condition in the least, but it’s a frustrating and undesirable one nonetheless. For many, these bumps are an embarrassment, and covering them up feels like the only solution. Thankfully, covering up isn’t the only solution. But, as with so many other skin issues, before you understand how to fix the problem, it helps to understand what’s causing it!
What Causes Keratosis Pilaris (KP)?
Research has shown that there’s a genetic component to KP; 50% of those who struggle with it have a family history of it. [184] There are a few different forms of keratosis pilaris. It can range from pink to red bumps on the cheeks (often mistaken for acne) to small, hard red bumps that aren’t irritated to pimple-like bumps that feel rough and coarse but are inflamed and red. Most often, KP shows up on the upper arms and legs.
Regardless of the type, all forms are the result of the buildup of keratin, a hard protein (skin’s surface is made up of cells known as keratinocytes) that protects skin from infection and harmful external substances. The keratin forms a plug that blocks the opening of the hair follicle, resulting in patches of bumpy, often inflamed skin.
Regrettably, there’s no universally accepted treatment for chicken skin, though it’s generally well accepted that unclogging hair follicles and reducing inflammation can make a big difference. [185]
Getting Rid of KP
One of the best ways to get to the root of the problem is to use a beta hydroxy acid (BHA) leave-on exfoliant (active ingredient salicylic acid) that has a pH low enough for exfoliation to occur. [36] BHA is a wonderful multitasker because it penetrates beyond skin’s surface to exfoliate inside the pore lining. It also has antimicrobial properties to kill bacteria that might be making matters worse. Plus, because salicylic acid is related to aspirin (aspirin is acetylsalicylic acid), it acts as an anti-inflammatory agent to reduce the redness that’s often seen with KP.
What about alpha hydroxy acids (AHAs)? AHAs can help exfoliate skin cells, but only at the surface. However, they’re an option for those whose keratosis pilaris does not respond well to BHA treatment. AHAs can be effective when the KP plugs are not very deep, and so the penetrating ability of BHA isn’t quite as necessary. For best results, look for an AHA with glycolic or lactic acid (these may be combined in the same product) at a concentration of 5% or greater.
Because keratosis pilaris is an inflammatory disorder, reducing inflammation is vitally important. (Actually, reducing inflammation is important for skin, period!) You can do this by avoiding bar cleansers and bar soaps, as the ingredients that keep them in their bar form can clog pores and make matters worse. Also, avoid highly fragranced body creams and lotions, whose fragrance can cause irritation and worsen the itching that can accompany KP.
It’s also important not to scrub skin. These bumps can’t be scrubbed away because the problem is deeper than scrubs can reach. Plus, scrubbing only serves to further irritate and inflame skin, making matters worse. Ditch the body scrub and loofah and use gentle cleansers and moisturizers to keep skin smooth. If desired, use a damp cotton washcloth as a mild “scrub,” but be aware that KP itself cannot be scrubbed away, and it’s not the result of skin being dirty.
When it comes to treating KP, ongoing application of such products is required to keep the condition under control. If you stop using them, the condition will eventually return. Some people may find that applying a KP treatment a few times per week will keep the bumps at bay; for others, daily application (once or twice, morning and/or evening) may be needed. As with so many things for your skin, you’ll need to experiment to see which product and what frequency of application works best for you.
Treating KP with Lasers
If topical treatments prove ineffective after a few weeks of daily use, talk to a dermatologist about laser treatments. Several options are available, including photopneumatic therapy (PPx), intense pulsed light (IPL), pulsed dye laser, long-pulsed alexandrite laser, and the Nd:YAG laser. [186,187,188,189]
Laser or light-emitting treatments have an impressive-to-decent track record for improving KP, most notably for reducing its redness and, for those with darker skin tones, the dotted brown spots left behind by the bumps. They also improve skin’s overall surface texture. If topical treatments don’t work (and some cases of KP can be very stubborn), a lot of people find these alternatives are well worth the time and money! In most cases, once your KP is cleared up via laser treatments, you can keep it under control with topical treatments. That’s great, as the ongoing expense of laser treatments adds up!
In terms of skincare, there are only a handful of products we’ve found that contain the types of ingredients that can adequately address the cause and symptoms of KP.
RECOMMENDED PRODUCTS FOR KERATOSIS PILARIS:
Note: All of the products below contain AHA (glycolic or lactic acid) or BHA (salicylic acid) ingredients in a lotion, cream, or wipe form. All are viable options for controlling keratosis pilaris; there isn’t a single “best” option. We encourage you to try more than one to see how your KP responds. Whichever products you choose from the list below, apply at least once daily.
- Alpha Hydrox 12% AHA Silk Wrap Body Lotion ($11.99)
- CeraVe Renewing SA Cream ($21.99; BHA)
- DERMAdoctor KP Duty ($38; AHA)
- Paula’s Choice Clinical KP Treatment Cloths ($32; AHA + BHA)
- Paula’s Choice Resist Skin Revealing Body Lotion 10% AHA ($27)
- Paula’s Choice Resist Weightless Body Treatment with 2% BHA ($25)
Eczema
Eczema (also known as atopic dermatitis) is a general term used to describe a strange variety of skin rashes ranging from small sections of skin that are slightly itchy, dry, and irritated to chronically inflamed, oozing, crusted areas covering the entire body and accompanied by incessant itching. [190] Pardon us for being blunt, but eczema just sucks!
Eczema can have multiple appearances, looking and feeling completely different from person to person. The most common areas for eczema to occur are in the folds of the arms and legs, the back of the neck, back of the hands, tops of the feet, and the wrists. It’s estimated to affect up to 20% of children, and the research on how eczema improves and worsens throughout life is inconclusive—though symptoms do seem to become less intense when a child with eczema reaches adulthood. [191]
What Causes Eczema?
One of the predominant theories is that someone with eczema has a short-circuited immune response, [192] where the skin reacts abnormally when a substance comes in contact with it. In severe cases of eczema, the substance can be as benign as water; for others, the trigger can be anything from clothing, detergents, soaps, grass, food products, allergens (including dust mites), a lack of humidity, or a combination of things. Even more frustrating is that the reaction can be intermittent, with no real rhyme or reason for why or when.
There also appears to be a strong hereditary component to eczema. [193] For example, children whose parents suffer from eczema run an 80% chance of developing it themselves. Further, in both children and adults, stressful situations tend to trigger, prolong, or worsen eczema flare-ups.
Regardless of the source, eczematous skin reacts to a substance or substances or to environmental conditions by spinning out of control and generating mild to severe inflammation, which leads to itching and subsequent scratching that damages skin’s critical barrier function.
Types of Eczema
There are several types and varying degrees of eczema, which, as you can imagine, makes diagnosis and treatment a bit tricky! The following are the most common types of eczema:
Atopic eczema (also referred to as atopic dermatitis): Perhaps the most pernicious and painful type of eczema, it’s characterized by its severity and the intolerable sensation of itching and irritation, leaving skin raw, fissured, and vulnerable to infection. This is the type of eczema that many infants experience between the ages of two and six months. In infants, symptoms appear on the face, scalp, feet, and hands; in older children and into adulthood, symptoms appear in the fold of the arm and behind the knees, though particularly bad outbreaks can appear anywhere on the body.
Allergic contact dermatitis: This specific form of eczema often stems from a subset known as irritant contact dermatitis. It occurs when a specific substance comes in contact with the skin and causes the immune system to overreact. The result is inflamed and sensitized skin. [194] Most typically, allergic contact dermatitis is caused by fragrance, nickel, detergents, wool, grass, citrus, household cleaning products, and vinegar. Once you’ve identified the specific substance, avoiding it often solves the problem.
A subset of allergic contact dermatitis is eyelid dermatitis. Typically mild to moderate redness is present, as well as scaling, flaking, and swollen skin. This is extremely common and almost exclusively affects women in relation to their use of hairstyling products, makeup, and nail polish (even once it dries) when your manicured nails come in contact with the eye area. The best way to solve the problem is to stop using the offending product(s) and find options that don’t trigger a reaction.
Infantile seborrheic eczema: Better known as cradle cap, this form of eczema generally affects only babies and children. [195] The crusty, thick, sometimes reddened lesions may look problematic, but this disorder is rarely itchy or even felt by the child. If you want to treat this, and success is limited, consider a 1% hydrocortisone or a 2% topical ketoconazole cream, which are available from your infant’s pediatrician. [196]
Adult seborrhoeic eczema: This shows up for most people between the ages of 20 and 40, and is estimated to affect 5% of adults. It’s usually seen on the scalp as mild dandruff, but can spread to the face, ears, and chest. The skin becomes red and inflamed and starts to flake. It’s believed to be caused by yeast, but its precise cause remains unclear; stress may be a factor. If the area becomes infected, treatment with an antifungal cream, topical steroid creams, or immunomodulators may be necessary. [197]
Nummular eczema: Typically localized on the legs, nummular eczema is characterized by coin-shaped patches of pink to red skin that may take on an orange cast if crusting or scaling is present. Left untreated, the dry, scaly spots typically darken and thicken. This type of eczema is most common in adolescent girls and in women between the ages of 30 and 60, and the condition tends to occur in winter. [198]
Treating Eczema
There’s no cure for eczema on the horizon, but the good news is that there are a number of treatments that can reduce the symptoms and decrease the level of discomfort. Keep in mind that many people diagnosed with eczema when they are young eventually, for the most part, outgrow it. The primary treatment options for eczema are as follows:
Gentle, effective skincare: The first line of defense is a gentle, fragrance-free skincare routine that prevents or reduces inflammation and keeps skin moist and its barrier intact. [199] Improving the skin’s outer structure by providing it with antioxidants, ingredients that improve the skin’s barrier, anti-irritants, and emollients can have amazing results for most forms of eczema. In fact, it’s been theorized that eczema makes skin more susceptible to oxidative damage, which in turn makes topical application of antioxidants even more important! [200]
Avoid irritants: In addition to using a gentle skincare routine and a well-formulated moisturizer, avoiding things that can trigger skin reactions is also of vital importance. Steering clear of known irritants and prolonged contact with water can be incredibly beneficial. It also helps a great deal to reapply moisturizer within seconds of washing any part of the body, but especially your hands, because soaps and cleansers are notorious for triggering a reaction in those struggling with eczema. [201] Try switching to a creamy, moisturizing body wash (Olay and Dove make good ones) and using that throughout your home as your hand soap. It works beautifully!
Topical steroids: The most typical and successful medications for eczema are prescription-strength topical steroids (cortisone creams such as Eumovate, active ingredient clobetasone butyrate, or various strengths of hydrocortisone). Over-the-counter cortisone creams can be effective for very mild or transient forms of eczema, but if those fail, prescription cortisone creams can save your skin. Although there are no short-term detrimental side effects of using most strengths of cortisone cream, it’s still important to apply it only to the affected areas, and only as needed, because repeated, prolonged application of cortisone creams can cause thinning of the skin, prematurely aging it. [202,203,204]
Oral steroids: In severe cases of eczema, when topical steroids have failed to produce any relief, oral steroids may be prescribed, but only under a doctor’s scrutiny due to the serious side effects associated with this type of medication. [205]
Topical immunomodulators: In 2000 and 2001, Protopic (active ingredient tacrolimus) and Elidel (pimecrolimus) were approved by the FDA as new topical drugs for the treatment of eczema. Not cortisones or steroids, these immunomodulators can regulate the skin’s immune response, which plays a pivotal role in eczema. [206] Regrettably, in March 2005, the FDA announced a public health advisory for Elidel (pimecrolimus) Cream and Protopic (tacrolimus) Ointment “to inform healthcare providers and patients about a potential cancer risk from use of Elidel (pimecrolimus) and Protopic (tacrolimus)…” This risk is uncertain, and more recent studies have refuted it, but the FDA’s precautions still advise that Elidel and Protopic should be used only as labeled, for patients who have failed treatment with other therapies. [207] The topical immunomodulators (pimecrolimus and tacrolimus) don’t present the risk of skin thinning that’s associated with topical corticosteroids.
Phototherapy: Research has shown that exposing skin to controlled wavelengths of UVA or UVB light can help reduce the symptoms of chronic eczema. [208] Under medical supervision, the use of specially designed bulbs can allow affected parts of the body to be exposed to the specific light source. More severe or chronic eczema can be treated with UVA light in combination with a prescription medication called psoralen. Psoralen can be administered either orally or topically, increasing the skin’s sensitivity to light. [209] This treatment is known as PUVA (Psoralen + UVA light) and is administered more often to adults than to infants or children with eczema.
Phototherapy treatments are complicated and expensive. They are administered several times per week over a span of one week to several months at a doctor’s office. As you might have guessed, the risk of accelerated aging of the skin and increased risk of skin cancer from UV radiation therapy can be the same as for sunbathing, so this isn’t an optimal way to treat eczema, as it just replaces one problem (eczema) with another (UV damage). [210]
Non-fragrant oils and dietary changes: Evening primrose oil and borage oil contain gamma linolenic acid, a fatty acid that may play a part in general skin health and that has gained a reputation for reducing the occurrence of eczema when applied topically. Several studies, however, have shown that not to be the case. [211] Nonetheless, if you’re interested in alternative treatments for eczema, this is one you can try with very little risk of adverse effects. Other non-fragrant plant oils, like safflower or jojoba, may also be worth experimenting with, and you can add a few drops of these to your regular body moisturizer, hand cream, or facial moisturizer.
There’s also some research pointing to dietary considerations as a source of reactions. [212] It’s worth experimenting to see if eliminating certain food groups, such as dairy, gluten, processed foods, or nuts, can decrease the severity and/or frequency of eczema outbreaks.
Skincare if you have eczema: From the neck down, treating eczema means being as gentle as you absolutely can, which almost always means avoiding bar soaps and scrubs. Below we list fragrance-free gentle cleansers and body lotions we strongly recommend. If you have eczema on your face, follow our recommendations in the sections that are appropriate for your skin type, also adding products to treat other concerns like rosacea, brown spots, and wrinkles.
Don’t Be Afraid of Cortisone Cream
Whether you have short-term or long-term bouts of eczema, rashes, or any kind of dermatitis, cortisone creams can be your best friend. Topical cortisone creams, which can be either over-the-counter (OTC) or prescription, are known by many names, including corticosteroids, glucocorticosteroids, and steroids. Without question, cortisone creams are truly the “gold standard” for treating eczema. When applied correctly, as directed, they’re completely safe to use, even on children. [213]
We know that our “completely safe” comment may fly in the face of what you’ve heard about topical cortisones—that they’re really terrible for skin—that’s another myth that just isn’t true. [214] In fact, believing this flawed information, and not using cortisone cream when it’s called for, may lead to far more problems for your skin than you can imagine.
We are not saying that there are no risks associated with using cortisone creams, because there are; however, their benefits, when used correctly, will help prevent long-term damage to your skin by interrupting and reducing the cascade of chronic inflammation and itching caused by eczema. Here’s what’s happening:
Depending on the severity of the eczema, your skin can, seemingly for no reason, become red, inflamed, itchy, and flaky, on various areas of the face and body; sometimes accompanied by small sacs filled with fluid. This outbreak causes a great deal of damage to skin, both to the upper and lower layers of skin. More often than not, these eczematous areas are unbearably itchy, so maddening that it triggers uncontrollable and habitual scratching. This scratching further damages skin, causing pain, wounds, and even a risk of infection.
All these symptoms, and your reaction to them (scratching), reduce skin’s ability to heal, cause collagen and elastin to break down, and make the skin more vulnerable to environmental damage, all of which are pro-aging. None of this is desirable, and it’s clearly detrimental to the health of skin, over both the short term and long term. Regrettably, most alternative treatments (that is, those other than cortisone) for moderate to severe eczema are rarely, if ever, successful. They are always worth a try, especially if you have only occasional minor bouts of eczema, but when they fail to do the job, the only real relief will come from applying a cortisone cream that’s appropriate for the type of eczema with which you’re struggling.
So, you’re wondering, what are the risks associated with cortisone creams? The primary risk, and what most people seem to be concerned about, is thinning of the skin. While that is indeed a risk of using cortisone creams it is only a risk from long-term chronic use. Yet, despite this fact, many people fear the thinning of skin will happen immediately and that is not the case.
For many people, cortisone cream is nothing less than a miracle; Paula can personally attest to that, as she’s struggled with eczema to one degree or another for most of her life. Anecdotally, except for the areas where she used it chronically day in and day out for years there have been no negative consequences and the skin in those areas looks completely normal and healthy.
The real story about cortisone is that if it’s used only intermittently for a few days here and there to relieve the symptoms, discomfort, and skin damage eczema can cause then there’s no cause for alarm. Using cortisone creams indefinitely is the problem, not intermittent use to stop the symptoms and reactions so skin can begin to heal.
One strategy is to start with OTC options at your drugstore, but if they don’t work, you may need to see a doctor for prescription-strength versions. In those situations, it’s not uncommon for the doctor to prescribe two or more preparations of different strengths to be used at the same time, but on different parts of the body; for example, a mild cortisone cream for eczema on your face and a moderately strong version for eczema on the thicker skin of your arms or legs. A very strong topical cream is often needed for eczema on the palms and soles of the feet of adults because these areas have thick skin, and eczema in these areas doesn’t respond as well to low-strength cortisone creams.
Topical cortisone creams should be used until the flare-up is completely gone, and then you should stop the treatment and only use it again when another flare-up occurs. Also, it’s best to use the smallest amount possible that reduces the inflammation and itching; applying more won’t make it work any faster or any better. In some cases, it might require treatment for as little as one day; in other cases, it may take up to 14 days to clear a flare-up. If it takes longer, you’ll want to consult your physician. In all cases, apply it only as needed, and keep in mind that the sooner you apply it when you notice a flare-up starting—before it gets bad—reduces the amount of time you’ll need to continue the treatment, and thus limits the potential risk of any skin-thinning.
When you weigh the pros and cons of cortisone creams, the research and results are clear that the damage that results from letting inflamed raw skin linger can be far worse than the effects of intermittent use of a cortisone cream, whether OTC or prescription-only. Don’t let unbalanced, one-sided information prevent you from taking the best possible care of your skin.
RECOMMENDED PRODUCTS FOR ECZEMA:
- Aveeno Daily Moisturizing Body Wash ($8.99)
- Cetaphil Restoraderm Eczema Calming Body Wash ($17.99)
- Cortizone-10 Hydratensive Anti-Itch Lotion for Hands and Body, Healing Natural Aloe Formula ($10.49; this is medicated with 1% hydrocortisone and best for mild eczema)
- Eucerin Eczema Relief Body Crème ($10.49)
- Eucerin Skin Calming Dry Skin Body Wash ($8.79)
- Gold Bond Ultimate Eczema Relief Skin Protectant Cream ($11.99)
- Kate Somerville Eczema Therapy Cream ($48)
- Paula’s Choice Clinical Ultra-Rich Soothing Body Butter ($19)
Scars
Whether from an injury, surgery, or a skin problem such as acne, scars are something almost everyone has to deal with at some point or another. Although unsightly, they’re an amazing example of the miraculous way skin heals itself when injured. Scars may be flat or raised, practically invisible or obvious, but what you do to assist the skin as it heals—and how you treat the scarred area afterward—makes a big difference in how the scar looks. Before you learn how to treat scars, you need to understand how they form, how to care for injured skin to minimize scarring, and what type of scar you’re dealing with.
How Does a Scar Form?
The scar that you see on the skin’s surface is the result of a complex process the skin goes through as it recovers from damage. There are many factors that affect how a wound heals, and the way the wound heals affects how the scar ends up looking. How skin heals and scars varies from person to person, but it also depends on how you care for the wound before the scar is done forming.
The skin goes through three stages of repair before you see a scar. In the first stage, there’s swelling, redness, and some tenderness or pain as a scab begins to form. A scab in and of itself is an amazing part of the healing process and must be protected, but more about that in the next section.
During the next stage, new skin tissue begins to form underneath the scab. The final stage involves rebuilding and reforming the outer and inner layers of skin.
What you do during the first days after getting a wound, what you do after the scab has formed, and what you do when the scab eventually falls off will greatly affect the appearance of the final scar.
Wound Care to Minimize Scars
There’s an easy-to-follow plan to minimize scarring. Although there’s a lot of anecdotal information about specific ingredients (such as aloe and vitamin E) to reduce scars, most of it is not supported by research, and more often than not it’s just a waste of time—time during which you could have used more effective remedies instead. Here’s how to care for a wound to minimize scar formation:
- Allow the wound to “breathe” as much as possible. Do not gunk up the area with creams, oils, or vitamin E from capsules because these substances have occlusive textures that can impede the first stages of healing when skin is trying to repair itself. The fluid that is produced naturally around a wound (known as exudate) is fine by itself for the first few days.
- Don’t soak the wounded area in water or get it wet for extended periods; doing so breaks down the scab and impairs the formation of the new skin below, risking scars that take longer to heal.
- Keep the damaged skin clean using a gentle cleanser, but don’t over-clean or scrub it.
- After cleansing, cover the wound with a thin, light bandage that allows air to circulate.
- You may want to consider a specialty adhesive dressing, such as Nexcare Tegaderm Transparent Dressing or Convatec DuoDERM Extra Thin Dressing. These cost more than standard bandages, but are excellent at keeping wounds moist without letting them get wet.
- If you suspect there’s a risk of infection, consider using an over-the-counter antibacterial liquid such as Bactine Original First Aid Liquid or Band-Aid Antiseptic Wash, Hurt-Free. If the redness increases or if the wound changes color, throbs, or swells, consult a doctor.
- After a day or two, apply a thin layer of a lightweight gel moisturizer or serum loaded with antioxidants (which are brilliant for helping skin heal) and other skin-repairing ingredients.
- If possible, rather than applying sunscreen to the injured area, keep it out of direct sunlight altogether, which means seeking shade or covering it up. Sun exposure makes scarring worse, so protecting the injured area from the sun (as you should be doing for your skin everyday even if you don’t have a wound) is important.
- At night, change the bandage; if the wound is dry or itchy, apply a very thin layer of a lightweight moisturizer or serum, as mentioned above. Keeping wounds moist (but not wet) encourages healing. Tip: A lightweight moisturizer also makes the scab less itchy as it forms, and still allows the skin to breathe!
- Once a scab forms, don’t pick at it or even touch it—ever! Any manipulation or removal is a serious impediment to the healing that is taking place underneath the scab, and can cause scarring that otherwise would not have occurred.
- Do not irritate the skin! Skin’s primary, natural reaction to a wound is inflammation, so anything you do to irritate skin makes matters worse.
- Avoid soaps (they’re too drying), highly fragrant products (whether natural or synthetic, fragrance is a skin irritant), and alcohol, menthol, citrus, eucalyptus, clove, camphor, or any type of mint, all of which increase irritation and make matters worse. [2,5,7]
Types of Scars
Depending on your genetic makeup and the depth and type of tear in your skin, scarring can range from a slightly reddish discoloration to a thick, raised red or dark scar. There are three main types of scars, generally described as flat, indented, or raised.
Flat scars are the most common, and usually occur from everyday injuries or minor burns. Depending on your skin color, flat scars may be pink to red (and eventually fade to very light pink or white) or tan to deep brown or black (eventually becoming lighter).
Note: The flat, pink-to-red or tan-to-brown marks left from a breakout are technically not scars. These marks are known as post-inflammatory hyperpigmentation.
Indented (atrophic) scars often result from cystic acne or a bout with the chickenpox virus. If you’ve ever had a deep, painful breakout or chickenpox, chances are you have at least one of these scars. Other names for indented scars are pockmarks, ice pick scars, and depressed scars. These scars result from the destruction of skin’s underlying support structure, which is why they don’t heal as well as flat or raised scars.
Raised (hypertrophic) scars result from overproduction of collagen in response to injured skin. This type of scarring can result from a slight tear in skin or from a deep wound, and everything in between. Sometimes referred to as keloid scars, they are more common in persons with dark skin. Raised scars flatten over time, but can take years to resolve. We explain how you can help this process along in the next section: Scar Treatments. Stubborn or large/long raised scars may require medical or surgical treatment.
Scar Treatments
Even when you take the proper steps to minimize scarring, once the wound has healed, you’ll likely want to keep treating the scar to make it even less noticeable. You’ll be happy to know there are products and medical procedures that can help—a lot!
Even if you choose to do nothing, a scar continues to heal and change, often for the better part of up to two years after the fact. With ongoing gentle skincare, sun protection, and patience (that’s the hardest part), most scars do improve, becoming less apparent over time. If you don’t want to wait it out, there are some things you can do to treat the scars you have now, as follows:
- Apply a silicone-based gel or scar treatment loaded with skin-healing ingredients and antioxidants such as quercertin. Eight weeks of once- or twice-daily application can make the scar less noticeable, especially if it’s a fresh scar. This type of product shows the best results on flat scars, but also can be helpful on raised and indented scars. Always treat the skin gently and protect the scar with sunscreen rated SPF 30 or greater if it will be exposed to daylight.
- Watch out for scar gels that are little more than silicone, and there are a lot of them out there. Although pure silicone can help heal and reduce scars, silicone alone isn’t all that the skin needs to improve scars. A range of anti-inflammatory, skin-healing, and skin-repairing ingredients will get you much better results because they work with the skin’s natural repair process.
- Raised scars can be flattened to some extent with daily application of a silicone-based scar treatment gel and/or a silicone gel sheet, such as ScarAway Silicone Scar Sheets or Rejuveness Pure Silicone Sheeting (which is reusable). The sheet is worn for 12 to 24 hours at a time for at least three months.
- Indented scars respond best to a series of in-office laser treatments (including Fraxel), dermal fillers, fat grafting, or a combination of these. In extreme cases, surgery may be necessary; there are various methods that your dermatologist can discuss with you. How much an indented scar improves depends on its depth and on how well your skin responds to treatments. Although it’s not realistic to expect 100% improvement, 50% improvement is possible.
What about Mederma for scars? Research on Mederma is conflicting; some research shows that it does work and some shows that it does not work, so the results are mixed. Yes, that’s confusing, but it’s what the science says. In short, Mederma is a product for which you must weigh the pros and cons yourself. [215]
RECOMMENDED SCAR GELS:
- Kate Somerville D-Scar Scar Diminishing Serum ($48)
- Kinerase Scar Healing Therapy ($48)
- Paula’s Choice Clinical Scar-Reducing Serum ($24)
What is Psoriasis?
Psoriasis is a complicated skin disease that is said to affect over 125 million people worldwide. It is a chronic condition resulting from what is thought to be an auto-immune disorder in which skin cells malfunction and reproduce much faster than normal, leaving thickened, raised patches or large areas of red or brown, wet-looking, scaly skin on the face and body.
There are several forms of psoriasis, ranging from mild to severe—and even disabling. Sadly, there is still no cure, but, thankfully, there is an immense amount of research taking place today that is seeking better medical treatments and potential cures. There are many different types of treatments available, ranging from over-the-counter (OTC) options to prescription-only treatments, both topical and oral. Depending on how your skin responds to the treatment, there is a very good chance you will experience improvement for extended periods of time and possibly even keep it that way.
There also are advanced medical options, such as immune-modulating drugs, but they can have long-term risks, which you should discuss with your physician. Experimenting with a variety of options will likely provide the best results, but regardless of what you decide to do, it will require regular and consistent behavior and usage.
Treatment Options for Psoriasis
As mentioned, there are various therapies available to treat psoriasis, and our strong recommendation is to start with those that have the least-serious side effects, such as intermittent use of an OTC topical cortisone cream; vitamin D preparation, both topical and oral; retinoids; salicylic acid (BHA); and topical coal-tar creams, lotions, cleansers, and shampoos. [216,217,218,219,220]
It is important to point out that the vitamin D treatments for psoriasis, both oral and topical, are not the same as the vitamin D supplements you can buy in stores. Calcipotriene is the form of vitamin D used to treat psoriasis, and it has a very different action on skin and the body than the form of vitamin D in supplements (cholecalciferol).
Based on how your skin responds to the above treatment options, you then can decide if you want to consider higher risk treatments, such as UVB therapy. UVB therapy can involve merely exposing your skin to the sun’s UVB rays (daylight) or to UVB emitting devices, or a combination therapy that involves UVB-emitting devices along with topical medications (immune-modulating medications). [221]
Keep in mind that successful treatment often requires a combination of methods. [224] Don’t put off seeing a dermatologist to explore all your options. It is surprising how many people suffer with psoriasis without seeking medical options.
Choosing a Skincare Routine When You Have Psoriasis
Several of the basic principles of skincare we discuss throughout this book apply when you have psoriasis. The exception is if your doctor has prescribed UVB treatment, with sunlight or with UVB therapies, in which case the UVB exposure must be carefully monitored by your physician due to its inherent risks to your health.
Overall, it is vitally important you don’t do anything to irritate your skin, as this will only make matters worse. Avoiding all the things we repeatedly warn against, such as harsh cleansers, abrasive scrubs, hot water, and products with irritating ingredients, especially fragrance (both synthetic and natural), will not only improve how your skin looks and feels, but also help the other treatments you might be using work even better by aiding absorption.
Aside from a gentle, effective, and healing skincare routine, adding skincare products that contain salicylic acid or retinol (vitamin A) to your routine can be helpful in treating psoriasis.
The best skincare routines for those with psoriasis start with a gentle water-soluble cleanser followed by a skin-soothing toner. A leave-on topical salicylic acid (BHA) exfoliant comes next. [223] During the day, follow with a sunscreen, if approved by your dermatologist, and at night, your moisturizer (with or without retinol).
If you are using other topical medications, such as a vitamin D, cortisone, coal-tar, or prescription retinoid cream or lotion, apply them before your sunscreen during the day and before your moisturizer at night. If you are using prescription retinoids, use a moisturizer that does not include retinol.
How Salicylic Acid and Retinoids Help Treat Psoriasis
Salicylic acid is an extremely gentle exfoliant that can soften and remove the layers of scaly, thickened psoriatic lesions. Removing these layers not only improves the appearance of skin, but also allows other topical medications to better penetrate into skin.
In addition, because of salicylic acid’s chemical relationship to aspirin (aspirin is acetylsalicylic acid), it has anti-inflammatory properties, which can reduce the redness associated with psoriasis. Given how salicylic acid functions, a leave-on salicylic acid–based exfoliant (2% to 6% concentration) is considered a viable skincare treatment for psoriasis.
Topical retinoids can significantly benefit psoriasis because of their ability to improve the way skin cells are formed. Prescription forms, like tretinoin Renova or tazarotene, can have impressive results for normalizing new skin cell production.
If you have psoriasis, you still must select skincare products based on your skin type—oily, combination, or dry. Especially important: You must be very careful to use only products that are free of potential irritants. (We are proud to say that Paula’s Choice Skincare is one of the few truly fragrance-free, gentle skincare lines available that also has a wide range of retinol- and salicylic acid–based products.)
The battle against psoriasis is frustrating, and it will take experimentation to find the best options for your skin. Discovering what works best for you will be the result of trying one or more of the treatments we’ve mentioned, either alone or in combination. Experimentation takes patience, and a systematic, ongoing evaluation of how your skin is reacting and of your overall health. Successful treatment, as is true with all chronic skin disorders, requires diligent adherence to the regimen and a realistic understanding of what you can and can’t expect. You also must be aware of the consequences and potential side effects of the various treatment levels.
For more information on the current status of the treatments available for psoriasis, visit the National Psoriasis Foundation (NPF) at www.psoriasis.org.
RECOMMENDED PRODUCTS FOR PSORIASIS:
Cleansers
- Neutrogena Ultra Gentle Hydrating Cleanser, Creamy Formula ($9.49)
- Paula’s Choice Skin Recovery Softening Cream Cleanser ($17)
- The Body Shop Aloe Gentle Facial Wash, for Sensitive Skin ($17)
Toners
- derma e Soothing Toner with Anti-Aging Pycnogenol® ($15.50)
- MD Formulations Moisture Defense Antioxidant Spray ($28)
- Paula’s Choice Resist Advanced Replenishing Toner ($23)
BHA Exfoliants
- Paula’s Choice Resist Weekly Retexturizing Foaming Treatment with 4% BHA ($35)
- Paula’s Choice Skin Perfecting 1% BHA Lotion ($26)
- philosophy clear days ahead oil-free salicylic acid acne treatment and moisturizer ($39)
Daytime Moisturizers with SPF
- MDSolarSciences Mineral Crème Broad Spectrum SPF 30 UVA/UVB Sunscreen ($30)
- Paula’s Choice Skin Recovery Daily Moisturizing Lotion SPF 30 ($28)
- Rodan + Fields SOOTHE Mineral Sunscreen Broad Spectrum SPF 30 ($41)
Moisturizers and Serums
- Josie Maran Cosmetics Pure Argan Milk Intensive Hydrating Treatment ($56)
- Neutrogena Healthy Skin Anti-Wrinkle Cream, Night ($14.99)
- Olay Regenerist Micro-Sculpting Serum, Fragrance-Free ($23.99)
- Paula’s Choice Calm Redness Relief Serum ($32)
- Paula’s Choice Clinical 1% Retinol Treatment ($55)