Blind Luck
“You know, Hobbes, some days even my lucky rocket ship underpants don’t help.”
—Bill Watterson, creator of Calvin and Hobbes
There are a lot of factors that determine oral health and oral microbial balance. In this book, we’ve talked about dietary factors such as sugar, refined carbohydrates or packaged foods, plant-based foods, and fiber. Excellent nutrition helps you cultivate a healthy, happy microbiome. I’ve mentioned that saliva flow, small doses of inflammation, and a healthy working immune system keep your mouth healthy. Whether you were born vaginally or by C-section, and if you were breastfed or bottle-fed, will influence your oral microbiome.
Treatments to reign in bacterial overgrowth in your mouth include brushing, flossing, and regular dental cleanings. You can also rebalance your oral microbiome with probiotics, fermented foods, or even antimicrobial herbs to help take the bacteria down a notch before rebuilding.
But what if none of this works?
Old-fashioned blind luck figures into a healthy mouth, too. Chock it up to bad genetics or a bad assortment of bacteria at birth, but some people do all of the right things and still get oral dysbiosis.
An interview with Dr. Mary Ellen Chalmers taught me that doing everything “right” to prevent cavities doesn’t work for everyone. There are people who do everything they should do, like eating a healthy diet, brushing, flossing, and seeing the dentist regularly, but they still get cavities. There are people who eat a lot of sugar and simple carbs, don’t brush regularly, and don’t floss, and they don’t get cavities! The research backs this up. In populations that have a low rate of cavities and do excellent oral hygiene care, still 1 in 5 people gets cavities.163 Oral disease doesn’t just depend on your oral hygiene. It also depends on your genetics, your diet, and other environmental factors.
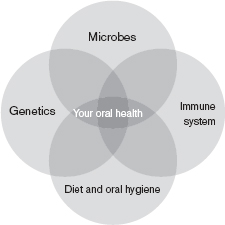
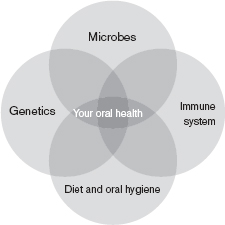
Figure 10.1: Your oral health is the product of interacting forces such as your microbes, your immune system, your environment (such as your diet and oral hygiene), and your genetics.
The Interface of Microbes, Immune Function, and Environment
The oral microbiome is the outcome of a conglomeration of different, interconnected factors. Each of these areas influences, and is influenced by, the others. Your genetics came from your parents and can’t really be changed. They are the blueprints for every cell in your body and for the system as a whole, but without environmental inputs and a microbiome, genes don’t tell us much at all.
As we’ve discussed through this book, you have at least as many bacterial cells in your body as human cells, if not more. They have their own genes. They make proteins and chemicals and waste products that can affect your immune system, your genes, and even your habits or cravings.
Your immune system works closely together with your microbial inhabitants. If your immune system is irritated or overactive, you will have more inflammation and you may lose tissue and bone because of rampant immune attacks. If your immune system is weak, you are more prone to infections.
Your environment includes your diet, your dental hygiene, and your habits, such as smoking. It influences how your genes are translated into real life and how happy or sad your microbiome is. Your environment, such as the choices you make about your diet or smoking, can boost or weaken your immune system.
Genetics, a good microbiome, and a healthy diet will probably help most people avoid oral dysbiosis. Other people will be susceptible to diabetes and periodontal disease because of their genetics, and perhaps a diet of hamburgers, sandwiches, chips, and soda.
There are plenty of areas to work on to heal and repair your oral microbiota. But there is no guarantee that it will work for everyone, 100 percent of the time. Sometimes, it’s just blind luck that gives you a healthy oral microbiome.
Different Oral Microbiomes in One Family
My mom went to a periodontist from the time I can remember. She always said she had “bad teeth.” One dentist attributed it to her mother, who smoked while she was pregnant with my mom. Another dentist blamed her “chalky” enamel on powerful antibiotics she was given as a baby when she had pneumonia. Mom stayed on top of her dental cleanings and dental health, and often had to get root canals and scaling treatments. She flossed every night.
My dad has virtually no issues with his teeth. He goes to the dentist for regular cleanings and also flosses and brushes routinely. He even has all of his wisdom teeth. Like his father, he never needed to remove them because they never gave him trouble. My parents were “health nuts,” so we ate a whole-foods diet growing up that was low in sugar.
My brother and I have relatively good oral health. We had childhood cavities, but not many. However, my sister has struggled with oral health over the years. Like my mom, she is more prone to cavities. She has had trouble with her teeth wearing down.
We were all breastfed, vaginally born babies. We ate similar diets through childhood. I would venture to say we all have a similar oral microbiome since we would have inherited it from our mother and father, and we were living in the same home, eating a similar diet. But at the end of the day, our oral health was not identical. Was there a different genetic predisposition? Were there different microbes at play? Was nutrition or immune function to blame? There is much we don’t yet know about the oral microbiome, and until there is a more scientific explanation, I’ll say that some people have good oral health simply because they are lucky.
There is so much we don’t know and we don’t understand. The study of the oral microbiome is in its infancy. Remember, only 57 percent of the oral microbiome is even named and characterized. I write this chapter to acknowledge and validate the people who struggle with oral disease and dysbiosis even when they have stellar dental hygiene, eat a sugar-free and whole-foods diet, and tend to their nutrition and their microbiomes.
To those people, I would say: While we can’t change our genetics or our pasts, we can change our environment and our microbes. Keep working to promote a healthy microbiome by following the recommendations in Chapter 9. Keep looking for the unique combination of things that work best to optimize your oral health. Find a skillful doctor and dentist who can work with you to find the root causes of your symptoms. Use laboratory testing to establish your baseline and monitor your progress. And look beyond the mouth for disease processes elsewhere in the body that might be draining your system and preventing you from achieving oral health.
Takeaways
• Some people never get cavities; others get cavities no matter how hard they work on dental health.
• Your oral microbiome is a complex outcome of interrelationships between genetics, microbes, environment, and immune function.
• While you can’t change your genetics or your past, you can change your environment and your microbes.