CHAPTER 71
Symptoms and Diagnosis of Lung Disorders
Disorders that affect the lungs and airways are called lung, respiratory, or pulmonary disorders. Depending on the person’s symptoms, a doctor usually recommends various tests to help determine the exact disorder.
Symptoms
Among the most common symptoms of lung disorders are cough, shortness of breath (dyspnea), and wheezing. Less commonly, a blockage in the airways between the mouth and lungs results in a gasping sound when breathing (stridor). Problems in the lungs can also lead to coughing up of blood (hemoptysis), a bluish discoloration of the skin due to a lack of oxygen in the blood (cyanosis), or chest pain. Prolonged lung disease can even produce changes in other parts of the body, including finger clubbing. Some of these symptoms do not always indicate a respiratory problem. Chest pain, for example, may also result from a heart or gastrointestinal disorder, and shortness of breath can be caused by a heart or blood problem.
COUGH
A cough is a sudden, explosive exhalation of air; the function of a cough is to clear material from the airways.
Coughing, a familiar but complicated reflex, is one way in which the lungs and airways are protected. Along with other mechanisms, coughing helps to protect the lungs from particles that have been inhaled. Coughing sometimes brings up sputum (also called phlegm)—a mixture of mucus, debris, and cells expelled by the lungs.
Causes
Coughing occurs when the airways are irritated. Respiratory infections—usually bacterial or viral—irritate the airways and are a common cause of coughing. Allergies can irritate the airways as well. People who smoke often cough. Smoke not only irritates the airways but also damages the cells that line the airways, including the hairlike projections that normally cleanse the airways of debris (cilia). Coughing may also result from postnasal drip, in which nasal secretions drain down the back of the nose into the throat and sometimes into the trachea and other airways, where they produce irritation. Coughing may result from gastroesophageal reflux, in which stomach or esophageal contents flow backward from the esophagus into the trachea and airways, producing irritation. Another cause of cough can be drugs, for example, angiotensin-converting enzyme (ACE) inhibitors (see table on page 340). Narrowing of the airways below the windpipe (bronchoconstriction), foreign bodies, or tumors in the airway can cause cough, wheezing, or both. Bronchoconstriction occurs in asthma, in chronic obstructive pulmonary disease, and heart failure (when fluid accumulates in the lungs).
Coughs vary considerably. A cough may be distressing, especially if coughing episodes are accompanied by chest pain, shortness of breath, blood, or unusually large amounts of or very sticky sputum. However, if coughing increases slowly over decades, as it may in a smoker, the person may hardly be aware of it.
Evaluation
Information about a cough helps a doctor determine its cause. Therefore, a doctor may ask:
 How long has the cough been present?
How long has the cough been present?
 At what time of day does the cough occur?
At what time of day does the cough occur?
 What factors—such as cold air, body position, talking, eating, or drinking—influence the cough?
What factors—such as cold air, body position, talking, eating, or drinking—influence the cough?
 Is the cough accompanied by chest pain, shortness of breath, hoarseness, dizziness, or wheezing?
Is the cough accompanied by chest pain, shortness of breath, hoarseness, dizziness, or wheezing?
 Does the cough bring up sputum or blood?
Does the cough bring up sputum or blood?
 Are there symptoms of another disorder that could cause a cough (for example, gastroesophageal reflux or postnasal drip)?
Are there symptoms of another disorder that could cause a cough (for example, gastroesophageal reflux or postnasal drip)?
 Could a drug be causing the cough?
Could a drug be causing the cough?
 What color is the sputum?
What color is the sputum?
The appearance of the sputum, especially a change in color or consistency, occasionally helps the doctor identify the cause. A yellowish, greenish, or brownish appearance may indicate a bacterial infection. Clear but very sticky (mucoid) sputum is characteristic of asthma. Occasionally, a doctor may use a microscope to examine a sputum sample. Bacteria and white blood cells are additional indications of infection. The presence of a specific type of white blood cell (eosinophil) suggests asthma. A cough may also produce blood, which commonly suggests bronchitis but may also suggest more serious disorders. Usually, a chest x-ray or other tests are done when a person develops a cough that is severe or persistent or has no obvious cause.
Treatment
Because coughing plays an important role in bringing up sputum and clearing the airways, a cough should not be suppressed unless it interferes with sleep. Treating an underlying disorder—such as an infection, fluid in the lungs, or asthma—is more important. For example, antibiotics can be given for an infection, or inhalers can be used for asthma. Depending on the severity of the cough and its cause, a variety of drugs may be used for treatment. When cough results from narrowing of the airways, bronchodilators may provide relief. It is not clear how well other drugs relieve cough.
Antitussive Therapy: Antitussive drugs are given to suppress cough. All opioids are antitussives because they suppress the cough center in the brain. Codeine is the opioid used most often for cough. Codeine may cause nausea, vomiting, and constipation; it may also be addictive. If codeine is taken for a prolonged period, the dose needed to suppress a cough may need to be increased. Opioid cough suppressants can cause drowsiness, particularly when the person also is taking other drugs that reduce concentration (such as alcohol, sedatives, sleep aids, antidepressants, and certain anti-histamines). Opioids are not always safe, and doctors usually reserve them for special situations.
Several non-opioid cough suppressants, such as dextromethorphan and benzonatate, are antitussives that also suppress the cough center in the brain. These drugs, and others, are the active ingredients in many over-the-counter and prescription cough medications. They are not addictive and, when used correctly, produce little drowsiness. In certain people, especially those who are coughing up an abundant amount of sputum, frequent use of these cough suppressants is not recommended.
Steam inhalation, for example from a vaporizer, can help stop a cough by reducing irritation in the throat (pharynx) and airways. The moisture from the steam also loosens secretions, making them easier to cough up. A cool-mist humidifier can achieve the same result. Some doctors believe that drinking sufficient water can produce good hydration and is as effective as steam inhalation for loosening secretions.
Expectorants: Some doctors recommend expectorants (sometimes called mucolytics) to help loosen mucus by making bronchial secretions thinner and easier to cough up, although these drugs do not suppress a cough. It is not clear how effective these drugs are. A saturated solution of potassium iodide may be prescribed. The most commonly used over-the-counter preparations contain guaifenesin or terpin hydrate. A small dose of syrup of ipecac may help in children, especially in those who have croup.
In cystic fibrosis, dornase alfa (inhaled recombinant human deoxyribonuclease I) is used to help thin the pus-filled mucus that results from chronic respiratory infections. Also, inhalation of a saline (salt) solution or use of acetylcysteine (for up to a few days) sometimes helps thin excessively thick and troublesome mucus.
Bronchodilators, Corticosteroids, Antihistamines, and Decongestants: Bronchodilators, such as inhaled albuterol and similar drugs, and inhaled corticosteroids are effective if a cough occurs as a result of airway narrowing (bronchoconstriction), as happens in asthma and chronic obstructive pulmonary disease. Theophylline, which is taken by mouth, is sometimes helpful. Some people who develop wheezing or prolonged cough after viral respiratory infections appear to benefit from short-term use of bronchodilators.
Antihistamines, which dry the respiratory tract, have little or no value in treating a cough, except when it is caused by an upper airway allergy. With coughs from other causes, such as bronchitis, the drying action of antihistamines can be harmful, thickening respiratory secretions and making them difficult to cough up.
Decongestants such as phenylephrine that relieve a stuffy nose are only useful in relieving a cough that is caused by postnasal drip.
DYSPNEA
Dyspnea (shortness of breath) is the unpleasant sensation of difficulty in breathing.
An increase in the rate and depth of breathing occurs normally during exercise and at high altitudes, but the increase seldom causes discomfort. Breathing is also increased at rest in people with many illnesses, whether of the lungs or of other parts of the body. For example, people with a fever generally breathe faster.
With dyspnea, faster breathing is accompanied by the sensation of running out of air. The person feels a sensation of not being able to breathe fast enough or deeply enough. Other sensations include an awareness of increased muscular effort to expand the chest when breathing in or to expel air when breathing out, the uncomfortable sensation that inhaling (inspiration) is urgently needed before exhaling (expiration) is completed, and various sensations often described as tightness in the chest.
Causes
Lung Disorders: People who have lung disorders often experience dyspnea when they physically exert themselves. During exercise, the body makes more carbon dioxide and uses more oxygen. The respiratory center in the brain accelerates breathing when blood levels of oxygen are low or blood levels of carbon dioxide are high. If the heart or lungs are not functioning properly, even a little exertion can lead to dramatic increases in breathing rates and dyspnea. Dyspnea is so unpleasant that the person avoids exertion. As the lung disorder becomes more severe, dyspnea may even occur at rest.
Dyspnea may result from restrictive or obstructive lung disorders. In restrictive lung disorders (such as idiopathic pulmonary fibrosis), lungs become stiff and require increased effort to expand during inhalation. Severe curvature of the spine (scoliosis) also restricts breathing by reducing the movement of the rib cage. In obstructive disorders (such as chronic obstructive pulmonary disease or asthma), resistance to airflow is increased because the airways are narrowed. Because airways widen on inhalation, air can usually be pulled in. However, because airways narrow on exhalation, air cannot be exhaled from the lungs as fast as normal, and breathing becomes labored.
Heart Failure: The heart pumps blood through the lungs. The heart must function properly for the lungs to function normally. If the heart is pumping inadequately (heart failure), fluid may accumulate in the lungs, a condition called pulmonary edema. This condition causes dyspnea that is often accompanied by a feeling of smothering or heaviness in the chest. The fluid accumulation in the lungs may also lead to airway narrowing and wheezing—a condition called cardiac asthma.
Some people with heart failure experience orthopnea, paroxysmal nocturnal dyspnea, or both. Orthopnea is shortness of breath when a person lies down that is relieved by sitting up. Paroxysmal nocturnal dyspnea is a sudden, often terrifying, attack of shortness of breath during sleep. The person awakens gasping and must sit or stand to take a breath. This condition is an extreme form of orthopnea and a sign of severe heart failure (see page 356).
Anemia: Dyspnea can also occur in people who have anemia or blood loss because of a decreased number of red blood cells, which carry oxygen to the tissues. The person breathes rapidly and deeply, in a reflex effort to try to increase the amount of oxygen in the blood.
Other Causes: Someone with severe kidney failure or sudden worsening of diabetes mellitus or someone who has taken certain drugs or poisons feels out of breath and may begin to pant quickly because of an accumulation of a large amount of acids in the blood (a condition called metabolic acidosis). Anemia and heart failure may also contribute to dyspnea in people with kidney failure.
Hyperventilation syndrome causes people to feel that they cannot get enough air, and they breathe heavily and rapidly. This condition is commonly caused by anxiety rather than a physical problem. Many people who experience this syndrome are frightened, may have chest pain, and may believe they are having a heart attack. People may experience a change in consciousness usually described as a feeling that events occurring around them are far away, and they may experience tingling in the hands and feet and around the mouth.
Evaluation and Treatment
Doctors can usually get an idea of what is causing dyspnea from the person’s symptoms and the results of a physical examination. A chest x-ray and measurement of levels of oxygen in the blood with arterial blood gas testing or pulse oximetry help determine the cause. The chest x-ray can show evidence of pneumonia and many other lung abnormalities and can often show evidence of heart failure. A low blood oxygen level usually indicates a heart or lung problem. Pulmonary function testing (see page 454) can measure the degree of restriction or obstruction and the ability of the lungs to transport oxygen from the air to the blood. A lung problem may include both restrictive and obstructive defects as well as abnormal oxygen transport. Other tests may be necessary to diagnose and further evaluate anemia, heart problems, certain specific lung problems, and kidney failure.
Treatment of dyspnea is directed at the cause. People with a low blood oxygen level are given supplemental oxygen using plastic nasal prongs or a plastic mask worn over the face. In severe cases, particularly if a person cannot breathe deeply or rapidly enough, doctors may assist breathing by mechanical ventilation administered through a breathing tube inserted into the trachea or through a tight-fitting face mask.
CHEST PAIN
Chest pain may be described as sharp (possibly knifelike), dull, burning, or squeezing; it may be located in a specific spot on the chest (such as the chest wall) or may be difficult to locate, often feeling like a deep ache. The pain may be constant or intermittent, lasting seconds, minutes, or longer. It may be worsened by breathing, changes in body position, exertion, eating, or other factors.
Pleuritic pain is a sharp pain that is made worse by deep breathing and coughing. Keeping the chest wall still—for example, by holding the side that hurts and avoiding deep breathing or coughing—can reduce the pain. Usually, the site of the pain can be pinpointed, although it may move over time. Pain may occur in the part of the chest supplied by a nerve between the ribs (intercostal nerve). This pain runs from the spine across the back to the chest in a path roughly parallel to a rib, usually affecting an area no wider than two or three ribs.
Causes
Chest pain may arise from structures in the respiratory system, including the pleura (the two-layered membrane covering the lungs). Chest pain can also arise from structures not related to the respiratory system, such as the chest wall, heart, major blood vessels, or esophagus. Some disorders of the heart and major blood vessels are serious; a person may need immediate testing and treatment.
Pleuritic pain often results from inflammation of the pleura (pleurisy). There are many causes of pleuritic pain, including viral and bacterial infections, cancer, and inflammation from disorders that can affect many organs, such as rheumatoid arthritis and systemic lupus erythematosus. Blood clots can travel through the bloodstream to the lungs (pulmonary embolism (see page 488)), lodge in the pulmonary arteries, and cause pleuritic chest pain. Air in the chest cavity (pneumothorax) and inflammation of the membrane surrounding the heart (pericarditis) can also cause chest pain that worsens during deep breathing. Pleural effusion, a fluid buildup in the space between the two layers of pleura (see page 518), may produce pleuritic pain at first, but the pain may subside as accumulating fluid separates the two layers.
Pain arising from other lung disorders (such as a lung abscess or tumor) is usually more difficult to describe than pleuritic pain. The pain is often described as a vague, deep-seated ache in the chest. Almost any disorder that damages the lungs or airways can cause such pain.
Pain originating in the chest wall may worsen with deep breathing or coughing and often is confined to one area in the chest wall, which also feels sore when pressed. The most common causes are chest wall injuries, such as broken ribs and torn or injured muscles located between the ribs (intercostal muscles). Even hard coughing can injure these muscles, causing pain for days or weeks. Pain along the area supplied by an intercostal nerve occurs if the nerve is irritated by a tumor or affected by shingles, which is caused by the varicella-zoster virus. In shingles, pain may occur before the tell-tale rash appears.
Evaluation and Treatment
Characteristics of the pain that a person describes provide clues to help doctors determine the cause. A chest x-ray is usually done. It often reveals the cause of chest pain, particularly pain caused by respiratory system problems. If serious disorders of the heart or major blood vessels are suspected, tests that help diagnose them are done, such as an electrocardiogram (ECG) or blood tests. Treatment is directed at the underlying disorder. Until the underlying disorder is controlled, drugs can relieve pain.
WHEEZING
Wheezing is a whistling, musical sound during breathing resulting from partially obstructed airways.
Wheezing results from an obstruction somewhere in the airways. It may be caused by widespread narrowing of the airways (as in asthma, chronic obstructive pulmonary disease, and some severe allergic reactions), by a local narrowing (as with a tumor), or by a foreign object lodged in an airway. The most common cause of recurrent wheezing is asthma, although many people who have never had asthma wheeze at some time in their lives. Infections such as pneumonia or bronchitis and, in infants, bronchiolitis can sometimes cause wheezing.
A doctor usually is able to detect wheezing by listening with a stethoscope as the person breathes. Loud wheezing can be heard easily, sometimes even without a stethoscope. To hear mild wheezing, the doctor may need to listen with a stethoscope while the person exhales forcefully. A persistent wheeze that occurs in one location in a smoker may be due to lung cancer. If a person develops wheezing suddenly for the first time, a chest x-ray may help in diagnosis. In people with persistent or repeated episodes of wheezing, pulmonary function testing (see page 456) may be needed to help measure the extent of airway narrowing and to assess the benefits of treatment. If doctors suspect a foreign object is lodged in an airway, they can insert a flexible viewing tube (bronchoscope) into the airway to diagnose the problem and remove the object.
Wheezing is relieved with bronchodilators, such as inhaled albuterol. Corticosteroids, taken by mouth for a week or two, can often help relieve an acute episode of wheezing if it is due to asthma or chronic obstructive pulmonary disease.
STRIDOR
Stridor is a gasping sound during inhalation resulting from a partial blockage of the throat (pharynx), voice box (larynx), or windpipe (trachea).
Stridor is usually loud enough to be heard at some distance. The sound is caused by turbulent airflow through a narrowed upper airway. In children, the cause may be croup, an inhaled foreign object, or, rarely, an infection of the epiglottis. In adults, the cause may be a tumor, an abscess, swelling (edema) in the upper airway, or a malfunction of the vocal cords.
Stridor causing dyspnea when the person is at rest is a medical emergency. In such cases, a tube may be inserted through the person’s mouth or nose (tracheal intubation) or by a small surgical incision directly into the trachea (tracheostomy) to allow air to get past the blockage and prevent suffocation. The cause usually becomes clear during tracheal intubation, during which a doctor can see the upper airway directly. If tracheal intubation is not done, the diagnosis is usually determined by inserting a flexible viewing tube through the nose and upper airway (a procedure called nasopharyngeal laryngoscopy).
HEMOPTYSIS
Hemoptysis is the coughing up of blood from the respiratory system.
Although hemoptysis can often be frightening, most causes turn out not to be serious.
Causes
Infection is the most common cause. Sometimes the cause is blood from the nose that has traveled down to the airways and then is coughed up. Unexplained or large amounts of blood in the sputum require evaluation by a doctor.
Tumors, especially those due to lung cancer, account for up to 20% of cases of hemoptysis. Death of lung tissue from blockage of an artery by a blood clot (pulmonary embolism—see page 488) may also cause hemoptysis.
Other causes include high blood pressure in the pulmonary veins, as may occur in heart failure and mitral valve stenosis. Other lung circulation problems, including arteriovenous malformations or inflammatory conditions of the pulmonary blood vessels, may also cause hemoptysis.
Evaluation
If hemoptysis is severe, persistent, or unexplained, a diagnostic evaluation is necessary. Doctors check for lung cancer in smokers older than 40 (and even in younger smokers if the person started smoking in adolescence) who develop hemoptysis, even if the sputum is only blood streaked. A chest x-ray is usually the first test done. A flexible viewing tube (bronchoscope) may be needed to identify the bleeding site. A scan using a radioactive marker (lung perfusion scan (see page 490) or other imaging test may reveal a pulmonary embolism. Despite testing, the cause of hemoptysis is not found in 30 to 40% of cases. When hemoptysis is severe, however, the cause is usually found.
Treatment
Bleeding may produce clots that block the airways and lead to further breathing problems. Therefore, coughing is important to keep the airways clear and should not be suppressed with antitussive drugs.
Hemoptysis is usually mild and usually stops by itself or when the disorder causing the bleeding (for example, heart failure or infection) is successfully treated.
If a large clot blocks a major airway, doctors may have to remove the clot using bronchoscopy. Rarely, hemoptysis is severe or does not stop by itself. If so, a tube may need to be inserted through the mouth or nose into the windpipe or lower into the airways to help keep the airways open. If the source of bleeding is a major blood vessel, a doctor may try to close off the bleeding vessel using a procedure called bronchial artery embolization. Using x-rays for guidance, the doctor passes a catheter into the vessel and then injects a chemical, fragments of a gelatin sponge, or a wire coil to block the blood vessel and thereby stop the bleeding. Sometimes bronchoscopy or surgery may be needed to stop severe or continuing bleeding, or surgery may be needed to remove a diseased portion of the lung. These high-risk procedures are used only as last resorts. If clotting abnormalities are contributing to the bleeding, a transfusion of plasma, clotting factors, or platelets may be needed.
CYANOSIS
Cyanosis is a bluish discoloration of the skin resulting from an inadequate amount of oxygen in the blood.
Cyanosis occurs when oxygen-depleted (also called deoxygenated) blood, which is bluish rather than red, circulates through the skin. Cyanosis can be caused by many types of severe lung or heart disease that produce low levels of oxygen in the blood. It can also result from certain blood vessel and heart malformations that allow blood to flow directly to the heart without ever flowing past the air sacs of the lung (alveoli) where oxygen is extracted from the air. This abnormal blood flow is called a shunt. In a shunt, blood from veins in the body, which is oxygen-depleted, may flow directly into blood vessels returning blood from the lungs to the left side of the heart or directly into the left side of the heart itself. The oxygen-depleted blood then is pumped out to the body, to circulate through the skin and other tissues.
The amount of oxygen in the blood can be estimated by pulse oximetry, in which a sensor is attached to a finger or an earlobe, or it can be measured directly by arterial blood gas analysis (see page 455). Chest x-rays, echocardiography, cardiac catheterization, pulmonary function tests, and sometimes other tests may be needed to determine the cause of decreased oxygen in the blood and the resulting cyanosis.
Oxygen therapy is often the first treatment given, in a similar fashion as for other conditions in which the blood oxygen level is low. Many malformations that cause shunts can be treated with surgery or other procedures.
CLUBBING
Clubbing is an enlargement of the tips of the fingers or toes and a change in the angle where the nails emerge.
Recognizing Finger Clubbing
Finger clubbing is characterized by enlarged fingertips and a loss of the normal angle at the nail bed.

Clubbing occurs when the amount of soft tissue beneath the nail beds increases. Why this increase occurs is not clear but may relate to the levels of proteins that stimulate blood vessel growth. Clubbing seems to occur with some lung disorders (lung cancer, lung abscess, bronchiectasis), but not with others (pneumonia, asthma, chronic obstructive pulmonary disease). Clubbing also occurs with some congenital heart disorders and liver disorders, or in some cases, it may be inherited and not indicate any disorder. Clubbing itself does not need treatment.
Diagnosis
A doctor usually can tell whether a person has a lung or airway disorder based on the medical history and physical examination. Diagnostic procedures are used to confirm the diagnosis, determine the extent and severity of the disorder, and help in planning treatment.
MEDICAL HISTORY AND PHYSICAL EXAMINATION
A doctor first asks the person about symptoms. Chest pain, shortness of breath (dyspnea) either at rest or during exertion, cough, coughing up of sputum or blood (hemoptysis), and wheezing may indicate a lung or airway disorder. Other, more general symptoms, such as fever, weakness, fatigue, or a general feeling of illness or discomfort (malaise), sometimes also reflect a lung or airway disorder.
Next, the doctor asks the person about past infections; previous exposure to chemicals; use of drugs, alcohol, and tobacco; home and work environments; travels; and recreational activities. A doctor asks whether family members have had lung or airway disorders or any other disorders that may affect the lungs or airways (such as clotting and generalized inflammatory disorders). The doctor also asks about other common symptoms, even those that do not seem related to the respiratory system.
During the physical examination, a doctor notes the person’s weight and overall appearance. The person’s general mood and feeling of well-being, which also may be affected by a lung or airway disorder, are also noted. A doctor may ask a person to walk around or climb a flight of stairs to see if either activity causes shortness of breath.
Assessing skin color is important because paleness (pallor) may indicate anemia or poor blood flow, and a bluish discoloration (cyanosis) may indicate an inadequate amount of oxygen in the blood. Fingers are examined for clubbing.
A doctor observes the chest to determine if the breathing rate and movements are normal. Using a stethoscope, a doctor listens to the breath sounds to determine whether airflow is normal or obstructed and whether the lungs contain fluid. By tapping (percussing) the chest, a doctor can often determine if the lungs are filled with air or collapsed and if the space around the lungs contains fluid. In addition to examination of the chest, a complete physical examination may be needed, because disorders of the lungs may affect other parts of the body. Additionally, for some disorders not related to the lungs, the first symptoms may suggest a lung problem. For example, shortness of breath might reflect an abnormality of the kidneys or heart, and pneumonia might reflect an abnormality of the immune system.
PULMONARY FUNCTION TESTING
Pulmonary function tests measure the lungs’ capacity to hold air, to move air in and out, and to exchange oxygen and carbon dioxide. These tests are better at detecting the general type and severity of lung disorder than at defining the specific cause of problems; however, these tests can be used to diagnose some specific disorders, such as asthma.
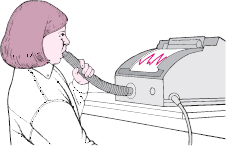
Lung Volume and Flow Rate Measurements: The assessment of a lung disorder often involves testing how much air the lungs can hold as well as how much and how quickly air can be exhaled. These measurements are made with a spirometer, which consists of a mouthpiece and tubing connected to a recording device. The person’s lips should be held tightly around the mouthpiece, and nose clips should be worn to ensure that all the air inhaled or exhaled goes through the mouth. A person inhales deeply, then exhales forcefully as quickly as possible through the tubing while measurements are taken. The volume of air inhaled and exhaled and the length of time each breath takes are recorded and analyzed. Often, the tests are repeated after a person takes a drug that opens the airways of the lungs (bronchodilator).
A simpler device for measuring how quickly air can be exhaled is the small, hand-held peak flow meter. After inhaling deeply, a person blows into this device as hard as possible.
Using a Spirometer
A spirometer consists of a mouthpiece, tubing, and a recording device. To use a spirometer, a person inhales deeply, then exhales vigorously and as quickly as possible through the tubing. The recording device measures the volume of air inhaled or exhaled and the length of time each breath takes.
Lung volume measurements reflect the stiffness or elasticity of the lungs and rib cage as well as the strength of respiratory muscles. The lungs are abnormally stiff in disorders such as pulmonary fibrosis, and the chest wall is abnormally stiff in disorders such as curvature of the spine (scoliosis). Various neuromuscular disorders can cause weakness of the diaphragm and other respiratory muscles, such as myasthenia gravis (see page 818) and Guillain-Barré syndrome (see page 828).
Flow rate measurements reflect the degree of narrowing or obstruction of the airways. The measurements are abnormal in obstructive disorders, such as chronic obstructive pulmonary disease and asthma.
Flow Volume Testing: Most spirometers can continuously display lung volumes and flow rates during a forced breathing maneuver. These flow rates can be particularly helpful in detecting abnormalities that partially block the voice box (larynx) and windpipe (trachea).
Muscle Strength Assessment: The strength of the respiratory muscles can be measured by having the person forcibly inhale and exhale against a pressure gauge. Disorders that weaken the muscles, such as muscular dystrophy and amyotrophic lateral sclerosis (ALS, or Lou Gehrig’s disease), make breathing more difficult and result in low pressures during inhalation and exhalation.
Diffusing Capacity Measurement: A diffusing capacity test can estimate how efficiently oxygen is transferred from the air sacs of the lungs (alveoli) to the bloodstream. Because the diffusing capacity of oxygen is difficult to measure directly, a person inhales a small amount of carbon monoxide, holds the breath for 10 seconds, and then exhales into a carbon monoxide detector.
If the test shows that carbon monoxide is not well absorbed, oxygen will not be exchanged normally between the lungs and the bloodstream either. The diffusing capacity is characteristically abnormal in people with pulmonary fibrosis, in those with disorders affecting the blood vessels of the lungs, and in some people with chronic obstructive pulmonary disease.
Maximal Voluntary Ventilation (MVV): MVV measures a person’s maximum ability to breathe. This test is done in the sitting position. A person is instructed to breathe as rapidly and deeply as possible through a spirometer for a predetermined period of time, usually 15 to 30 seconds. The volume of air moved over that period of time is measured. This test is dependent upon the ability of a person to cooperate but is useful in certain situations.
SLEEP STUDIES
Breathing is usually automatic and controlled by centers in the brain that respond to the levels of oxygen and carbon dioxide in the blood. However, in some people, breathing may stop for prolonged periods, especially during sleep—a condition called sleep apnea (see page 485). The best test for sleep apnea consists of monitoring brain wave activity (with an electroencephalogram, also called an EEG), the oxygen concentration in the blood (with pulse oximetry, which uses a sensor clipped on a finger or an earlobe), the movement of air during breathing (using a device placed in one nostril), chest wall motion, and sometimes other measurements. Combining all these measurements as part of a single test is called a polysomnogram. Because polysomnography is not always available, other tests are sometimes used during sleep to see whether a person has sleep apnea.
ARTERIAL BLOOD GAS ANALYSIS
Arterial blood gas tests measure the levels of oxygen and carbon dioxide in the arterial blood and determine the acidity (pH) of the blood. Taking a sample from an artery requires skill and may cause a few minutes of discomfort. Usually the sample is taken from an artery in the wrist (radial artery). Oxygen, carbon dioxide, and acidity levels are important indicators of lung function because they reflect how well the lungs are getting oxygen into the blood and getting carbon dioxide out of it.
Oxygenation of the blood can be monitored using a sensor placed on a finger or an earlobe—a procedure called pulse oximetry. When a doctor also needs a carbon dioxide or blood acidity measurement (for example, in certain people who are seriously ill), an arterial blood gas measurement is needed.
CHEST IMAGING
Chest x-rays are routinely taken from the back to front. Usually a view from the side is taken also. Chest x-rays provide a good outline of the heart and major blood vessels and usually can reveal a serious disorder in the lungs, the adjacent spaces, or the chest wall, including the ribs. For example, chest x-rays can clearly show most pneumonias, lung tumors, chronic obstructive pulmonary disease, a collapsed lung (atelectasis), and air (pneumothorax) or fluid (pleural effusion) in the pleural space. Although chest x-rays seldom give enough information to determine the exact cause of the abnormality, they can help a doctor determine whether and which other tests are needed to make a diagnosis.
Computed tomography (CT—see page 2037) of the chest provides more detail than a plain x-ray. With CT, a series of x-rays is analyzed by a computer, which then provides several views in different planes, such as longitudinal and cross-sectional views. During CT, a radiopaque dye may be injected into the bloodstream or given by mouth to help clarify certain abnormalities in the chest.
Magnetic resonance imaging (MRI—see page 2040) also produces highly detailed pictures that are especially useful when a doctor suspects blood vessel abnormalities in the chest, such as an aortic aneurysm. Unlike CT, MRI does not use radiation.
Ultrasonography (see page 2044) creates a picture from the reflection of sound waves in the body. Ultrasonography is often used to detect fluid in the pleural space (the space between the two layers of pleura covering the lung and inner chest wall). Ultrasonography can also be used for guidance when using a needle to remove the fluid.
Nuclear lung scanning (see page 2043) is particularly useful in detecting blood clots in the lungs (pulmonary emboli); it also may be used during the preoperative evaluation of people who have lung cancer. This type of imaging uses minute amounts of short-lived radioactive materials to depict the flow of air and blood through the lungs. Usually, the test is done in two stages. In the first stage (lung perfusion scan), a radioactive substance is injected into a vein, and a scanner creates a picture of how it is distributed throughout the blood vessels of the lung. If the perfusion scan is abnormal, a second stage is necessary (lung ventilation scan); the person inhales a radioactive gas, and a scanner creates a picture of how the gas is distributed throughout the lungs.
Pulmonary artery angiography (also called pulmonary artery arteriography) is done by injecting a radiopaque dye into the pulmonary artery and using conventional x-rays to view the dye in the lungs (see page 2036). Angiography is used most often when pulmonary embolism is suspected, usually on the basis of abnormal lung scan results, and is considered the best test for diagnosing or excluding pulmonary embolism. Increasingly, angiography of the pulmonary arteries is being done instead with pictures obtained from a CT scan (CT angiography). CT angiography is less invasive, because in this procedure, radiopaque dye is injected into a small peripheral vein rather than a central pulmonary artery.
Positron emission tomography (PET—see page 2044) scanning may be used when cancer is suspected. This radiographic imaging technique relies on different metabolic rates of malignant (cancerous) compared with benign (noncancerous) tissues. Glucose molecules are combined with a compound that is visible using PET. These molecules are injected intravenously, where they accumulate in rapidly metabolizing tissue (such as in cancerous lymph nodes), making these tissues visible on PET scans. Benign growths usually do not accumulate enough molecules to be visible.
THORACENTESIS
In thoracentesis, fluid that has collected abnormally in the pleural space (pleural effusion—see page 518) is removed. The two principal reasons to perform thoracentesis are to obtain a fluid sample for diagnostic testing or to relieve shortness of breath caused by fluid compressing lung tissue.
During the procedure, the person sits comfortably and leans forward, resting the arms on supports. A small area of skin on the back is cleaned and numbed with a local anesthetic. Then a doctor inserts a needle between two ribs into the chest cavity, but not into the lung, and withdraws some fluid into a syringe. Sometimes the doctor uses ultrasound for guidance (to determine where to insert the needle). The collected fluid is analyzed to assess its chemical makeup and to determine whether bacteria or cancerous cells are present.
If a large volume of fluid has accumulated, it may need to be removed through a plastic catheter and it may be necessary to use a fluid container that is larger than a syringe. The fluid may need to be drained over several days, in which case a larger tube (chest tube or drainage catheter) is left in the chest and suctioned continuously.
The risk of complications during and after thoracentesis is low. A person may feel some pain as the lung fills with air and expands against the chest wall or may feel the need to cough. Also, a person may briefly feel light-headed and short of breath. Other possible complications include puncture of the lung with leakage of air into the pleural space (pneumothorax), bleeding into the pleural space or chest wall, fainting, infection, puncture of the spleen or liver, and, if a large amount of fluid that has been present for weeks to months is withdrawn rapidly, accumulation of fluid within the lung itself (pulmonary edema). A chest x-ray may be performed after the procedure to determine whether any of these complications has occurred.
NEEDLE BIOPSY OF THE PLEURA OR LUNG
If thoracentesis does not uncover the cause of a pleural effusion (a fluid buildup in the space between the two layers of the pleura), a doctor may do a pleural biopsy. First, the skin is cleaned and anesthetized as for thoracentesis. Then using a larger cutting needle, a doctor takes a small sample of tissue from the pleura and sends it to a laboratory to be examined for signs of disorders, such as cancer or tuberculosis. About 80 to 90% of the time, a pleural biopsy is accurate in diagnosing tuberculosis, but it is less accurate for diagnosing cancer and other disorders.
If a tissue specimen needs to be obtained from a lung tumor, a doctor may do a needle biopsy. After anesthetizing the skin, a doctor, often using chest computed tomography (CT) for guidance, directs a biopsy needle into a tumor and obtains cells or a small piece of tissue to be sent to the laboratory for analysis. If a lung infection is suspected, tissue can also be sent for culture (a procedure in which a tissue sample is placed in a container containing nutrients and the container is observed to detect bacterial growth). Complications of pleural and lung biopsies are similar to those for thoracentesis.
BRONCHOSCOPY
Bronchoscopy is a direct visual examination of the voice box (larynx) and airways through a flexible viewing tube (a bronchoscope). A bronchoscope has a light at the end that allows a doctor to look down through the larger airways (bronchi) into the lungs.
A bronchoscope can be used to investigate the source of bleeding in the lungs. If a doctor suspects lung cancer, the airways can be examined and specimens can be taken from any areas that look cancerous. Bronchoscopy can be used for collecting the organisms causing pneumonia that are difficult to collect and identify in other ways. Bronchoscopy is especially helpful for obtaining specimens from the lungs in people who have AIDS and other immune deficiencies. When people have been burned or have inhaled smoke, bronchoscopy helps doctors assess for burns and smoke injury of the larynx and airways. Bronchoscopy can help a doctor treat certain conditions. For example, the bronchoscope can also be used to remove secretions, blood, pus, and foreign bodies; to place drugs in specific areas of the lung; and as a guide over which a tube can be inserted to assist breathing (tracheal intubation).
Understanding Bronchoscopy
To view the airways directly, a doctor passes a flexible bronchoscope through a person’s nostril and down into the airways. The circular inset shows the doctor’s view.
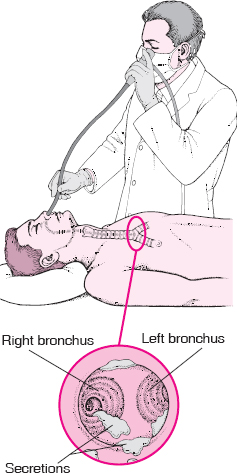
For at least 4 hours before bronchoscopy, the person should not eat or drink. A sedative is often given to ease anxiety, and atropine may be given to reduce the risks of spasm of the voice box and slowing of the heart rate, which sometimes occur during the procedure. The throat and nasal passage are sprayed with an anesthetic, and the bronchoscope is passed through a nostril and into the airways of the lungs.
Bronchoalveolar lavage is a procedure doctors can use to collect specimens from the smaller airways and alveoli that cannot be seen through the bronchoscope. After wedging the bronchoscope into a small airway, a doctor instills salt water (saline) through the instrument. The fluid is then suctioned back into the bronchoscope, bringing cells and any bacteria with it. Examination of the material under the microscope helps in diagnosing infections and cancers. The fluid can also be placed into containers containing special nutrients and left alone for a period of time to see if bacteria grow (culturing), which is a better way to diagnose infections.
Transbronchial lung biopsy involves obtaining a specimen (pieces) of lung tissue by using forceps passed through a bronchoscope. The forceps is threaded through a channel in the bronchoscope into progressively smaller airways until reaching the area of concern. A doctor may use a fluoroscope (an imaging device that uses x-rays to show internal body structures on a screen) for guidance in identifying the area of concern. Such guidance can also decrease the risk of accidentally perforating the lung and causing leakage of air into the pleural space (pneumothorax—see page 520). Although trans-bronchial lung biopsy increases the risk of complications during bronchoscopy, it provides additional diagnostic information and may make major surgery unnecessary.
Transbronchial needle aspiration is sometimes done. In this procedure, a needle is passed through the bronchoscope into the bronchial wall. The needle may be passed through the wall of a large airway under direct visualization or through the wall of a small airway using an x-ray machine for visualization. A doctor may be able to extract cells from suspicious lymph nodes to examine under a microscope.
After bronchoscopy, the person is observed for several hours. If a tissue specimen was removed, a chest x-ray may be taken to check for complications, such as bleeding or leakage of air into the pleural space (pneumothorax).
THORACOSCOPY
Thoracoscopy is the visual examination of the lung surfaces and pleural space through a viewing tube (a thoracoscope). The most common means for obtaining a sample of lung tissue for a biopsy is with a thoracoscope. A thoracoscope also may be used in treating accumulations of fluid in the pleural space (pleural effusions).
The person usually is given general anesthesia for this procedure. Then a surgeon makes up to three small incisions in the chest wall and passes a thoracoscope into the pleural space; this allows air to enter, collapsing the lung. Besides being able to view the lung surface and pleura, a doctor may take samples of tissue for microscopic examination and culture. In certain cases, the doctor may give drugs through the thoracoscope to prevent a reaccumulation of fluid in the pleural space. After the thoracoscope is removed, a chest tube is inserted to remove air that entered the pleural space during the procedure, enabling the collapsed lung to reinflate.
Complications are similar to those for thoracentesis and needle biopsy of the pleura. However, this procedure is more invasive, leaves a small wound, and requires hospitalization.
MEDIASTINOSCOPY
Mediastinoscopy is the direct visual examination of the area of the chest between the two lungs (the mediastinum) through a viewing tube (mediastino-scope). The mediastinum contains the heart, trachea, esophagus, thymus, and lymph nodes. Nearly all mediastinoscopies are used to diagnose the cause of enlarged lymph nodes deep in the chest or to evaluate how far lung cancer has spread before chest surgery (thoracotomy) is done.
Mediastinoscopy is done in an operating room with the person under general anesthesia. A small incision is made in the notch just above the breastbone (sternum). The instrument then is passed down into the chest in front of the windpipe, allowing the doctor to observe the contents of the mediastinum next to the windpipe and to obtain specimens for diagnostic tests if necessary. Complications are similar to those for thoracentesis and needle biopsy of the pleura.
THORACOTOMY
Thoracotomy is an operation in which the chest wall is opened to view the internal chest organs, to obtain samples of tissue for laboratory examination, and to treat disorders of the lungs, heart, or major arteries.
Thoracotomy is a major operation and therefore is used less often than other diagnostic techniques. Thoracotomy is used when procedures such as thoracentesis, bronchoscopy, or mediastinoscopy fail to provide adequate information. The lung problem is identified in more than 90% of people who undergo this operation because the sample site can be seen and selected and because large tissue samples can be taken. Thoracotomy is also often used when cancerous tissue is to be removed from the lung. Thoracotomy allows a surgeon to see and remove all involved tissue.
Thoracotomy requires general anesthesia in an operating room. An incision is made in the chest wall, and tissue samples of the lung are removed for microscopic examination. If specimens are to be taken from areas in both lungs, the breastbone is often split. If necessary, a lung segment, a lung lobe, or an entire lung can be removed.
A chest tube is inserted into the pleural cavity and left in place for 24 to 48 hours afterward. The person usually stays in the hospital for several days. Complications include infection, persistent bleeding, and a persistent leakage of air into the pleural space (pneumothorax).
SUCTIONING
Suctioning is used to obtain secretions and cells from the trachea and large bronchi. It is used to obtain specimens for microscopic examination or culture and to help clear secretions from the airways when cough is inadequate.
One end of a long, flexible, clear plastic tube is attached to a suction pump; the other end is passed through a nostril or the mouth and into the trachea. When the tube is in position, suction is applied in intermittent bursts lasting 2 to 5 seconds. With people who have a tube in the neck that leads to the trachea (tracheostomy) or a tube in the nose or mouth that leads to the trachea (endotracheal tube), the suctioning tube can be inserted directly into the tube that leads to the trachea. Sometimes inserting some salt water into the tube that leads to the trachea eases removal of secretions and cells via suctioning.