CHAPTER 101
Foot Problems
Some foot problems start in the foot itself, for example, from a foot injury. Others result from disorders that affect many parts of the body, such as diabetes, gout, or other types of arthritis. Problems can occur in any bone, joint, muscle, tendon, or ligament of the foot. Foot fractures are fairly common (see page 1959). Nail discoloration of the foot should always be evaluated because it may be caused by certain disorders, including a fungal infection (see page 1339).
People who have diabetes or peripheral vascular disease (narrowing of the arteries that carry blood to the legs, arms, and possibly internal organs) should check their feet daily for signs of infection or ulcers and should have a doctor or foot doctor (podiatrist) check their feet at least once a year (see box on page 424).
Many foot disorders are treated by changing a person’s footwear, such as wearing different shoes or using inserts or other devices (called orthotics or orthoses) that change the position or range of movement of the foot and relieve pressure on affected joints. Injections of a local anesthetic can often relieve pain and decrease muscle spasms so that joints can move more easily, and a corticosteroid may also be injected to decrease inflammation. If these treatments are not successful, sometimes surgery is needed to improve joint alignment and function and relieve pain.
Pain in the Ball of the Foot
Pain in the ball of the foot (called metatarsalgia) may have many different causes (including arthritis, poor circulation, pinching of the nerves between the toes, posture problems, and various disorders). However, most often the pain is caused by nerve damage or by an abnormality of the joints nearest the balls of the feet (metatarsal joints). Often, developing one disorder that causes pain in the ball of the foot contributes to development of another disorder that causes pain in the same location.
FREIBERG’S DISEASE
Freiberg’s disease is tissue death (necrosis) of parts of the bones in the ball of the foot, usually the digit next to the big toe (the second metatarsal head).
The cause is injury to the bone, usually in pubertal girls who are growing rapidly or people in whom the bone connected to the base of the big toe is short. In both cases, the metatarsal head can be subjected to repeated stresses.
SPOTLIGHT ON AGING
 With aging, many changes occur in the feet. For instance, there is typically less hair; brown coloration (pigmentation) may occur in spots or patches; and the skin may become dry. The toenails often become thicker and curved, and fungal infections of the nails occur commonly. The feet may actually enlarge in length and width because of changes in the ligaments and joints. A person with these types of changes may need to wear larger shoes. Also, feet can be damaged by a lifetime of ill-fitting shoes.
With aging, many changes occur in the feet. For instance, there is typically less hair; brown coloration (pigmentation) may occur in spots or patches; and the skin may become dry. The toenails often become thicker and curved, and fungal infections of the nails occur commonly. The feet may actually enlarge in length and width because of changes in the ligaments and joints. A person with these types of changes may need to wear larger shoes. Also, feet can be damaged by a lifetime of ill-fitting shoes.
Some Common Foot and Ankle Disorders by Location
Ankle
Tarsal tunnel syndrome
Tibialis posterior tendinosis
Ball of the foot
Interdigital nerve pain (Morton’s neuroma)
Freiberg’s disease
Metatarsal joint pain
Sesamoiditis
Heel (bottom)
Inferior calcaneal bursitis
Plantar fasciosis
Heel (back part)
Achilles tendon enthesopathy
Achilles tendon bursitis
Medial plantar nerve entrapment
Sole
Plantar fibromatosis
Toe
Bunion
Hammer toe
Pain is usually worse when bearing weight, particularly when pushing off of the foot, or when wearing high-heeled shoes. The joint may be swollen and stiff. Doctors examine x-rays to confirm the diagnosis. Pain may be relieved with injections of corticosteroids and by using a splint or cast. Low-heeled shoes or inserts or other devices (orthoses) that change the position or range of movement of the foot and relieve pressure on affected joints are helpful.
DAMAGE TO THE NERVES IN THE FOOT
Irritation or noncancerous (benign) growths of nerves may cause pain in the balls of the feet (interdigital nerve pain).
 Typical symptoms include a mild ache around the third or fourth toe that progresses to a burning or tingling sensation.
Typical symptoms include a mild ache around the third or fourth toe that progresses to a burning or tingling sensation.
 The diagnosis is based on the person’s history and an examination of the foot.
The diagnosis is based on the person’s history and an examination of the foot.
 Injecting a corticosteroid or sometimes applying extreme cold (cryotherapy) can help relieve symptoms.
Injecting a corticosteroid or sometimes applying extreme cold (cryotherapy) can help relieve symptoms.
Causes
The nerves that supply the bottom of the foot and toes (interdigital nerves) travel between the bones of the toes. Pain in the ball of the foot may be caused by irritation of the nerves or by noncancerous growths of nerve tissue (neuromas), usually between the base of the third and fourth toes (Morton’s neuroma), although these growths may occur between any of the toes. Neuromas usually develop in only one foot and are more common among women than men.
Symptoms and Diagnosis
In the early stages, a neuroma may cause only a mild ache around the third or fourth toe, occasionally accompanied by a burning or tingling sensation in the toes, particularly as the disorder progresses. These symptoms are generally more pronounced when a person wears certain types of shoes, especially those that are too narrow for the front part of the foot, including those that are pointed. As the condition progresses, a constant burning sensation may radiate to the tips of the toes, regardless of what shoes are worn. A person may also feel as if a marble or pebble is inside the ball of the foot.
Doctors diagnose the condition by considering the history of the problem and examining the foot. X-rays, magnetic resonance imaging (MRI), and ultrasound cannot accurately identify this disorder but may be helpful in ruling out other disorders that can cause similar symptoms.
Treatment
Injecting the tender spot in the foot with corticosteroids mixed with a local anesthetic and wearing proper shoes and sometimes orthoses may relieve the symptoms. Repeating the injections 2 or 3 times at intervals of 1 or 2 weeks may be necessary. Sometimes cryotherapy (application of intense cold) or injection of alcohol into the neuroma may also relieve pain. If these treatments do not help, surgical removal of the neuroma often relieves the discomfort completely but may cause permanent numbness in the area.
METATARSAL JOINT PAIN
Pain in the joints near the ball of the foot (metatarsophalangeal joint) may originate within the joints themselves.
Causes
Metatarsal joint pain commonly results from misalignment of the joint surfaces, which puts pressure on the joint lining and destroys cartilage in the joints. Mild heat and swelling may develop.
Metatarsophalangeal joint misalignment can also be caused by disorders, such as rheumatoid arthritis, that inflame the joints. In rheumatoid arthritis, hammer toes (see page 611) can develop, which can worsen joint pain and misalignment. Fat tissue, which helps cushion the joints when bearing weight, can be pushed forward under the toes, resulting in a loss of cushioning. This loss of cushioning can also damage the nerves in the ball of the foot.
Metatarsophalangeal joint pain may also result from osteoarthritis or stiffening of the joints of the ball of the foot, most often the joint at the big toe. Most people with these disorders have an abnormal motion of the foot when bearing weight and walking.
Symptoms and Diagnosis
Walking is painful. Over time, pain and stiffening can be disabling.
Doctors usually can diagnose the disorder based on the person’s symptoms and an examination, although testing is done if an infection or arthritis is suspected.
Treatment
Foot orthoses that redistribute body weight away from the most severely affected joints usually provide effective treatment. Occasionally, when these measures are ineffective, surgery is needed.
SESAMOIDITIS
Sesamoiditis is pain around a small bone (the sesamoid) below the metatarsal head where it adjoins the big toe (first metatarsal head).
The cause of sesamoiditis is usually repeated injury. Sometimes the bone is fractured, or the bone or surrounding structures are inflamed. Sesamoiditis is particularly common among dancers, joggers, and those who have high-arched feet or wear high heels.
The pain of sesamoiditis is felt beneath the ball of the foot at the big toe, is usually made worse by walking, and may be worse when wearing certain shoes. The area may be warm or swollen.
The doctor bases the diagnosis on an examination of the foot. The diagnosis may be confirmed by x-rays taken to exclude a fracture of the sesamoid bone.
Simply not wearing shoes that cause pain may be sufficient. If symptoms persist, shoes with a thick sole and low heels, orthoses, or a combination can help by reducing pressure on the sesamoid bone. A non-steroidal anti-inflammatory drug (NSAID) taken by mouth and injections of corticosteroids and a local anesthetic into the affected area can help relieve pain.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome (posterior tibial neuralgia) is pain in the ankle, foot, and toes caused by compression of or damage to the nerve supplying the heel and sole (posterior tibial nerve).
The posterior tibial nerve runs along the back of the calf, through a fibrous canal (tarsal tunnel) near the heel, and into the sole of the foot. When tissues around this nerve become inflamed, they can press on the nerve, causing pain. Disorders that can cause or contribute to tarsal tunnel syndrome include fracture, ankle swelling from heart or kidney failure, an underactive thyroid gland (hypothyroidism), and disorders such as gout or rheumatoid arthritis that inflame the joints.
Pain, the most common symptom of tarsal tunnel syndrome, usually has a burning or tingling quality. It may occur when a person stands, walks, or wears a particular type of shoe. Pain located around the ankle (usually on the inner side) and extending to the toes usually worsens during walking and is relieved by rest. Occasionally, pain also occurs during rest.
To diagnose this condition, a doctor manipulates the affected foot during a physical examination. For example, tapping the injured or compressed area just below the ankle bone often causes tingling, which may extend to the heel, arch, or toes. Nerve conduction studies (see page 636) may be useful to determine the cause or extent of the injury, especially if foot surgery is being considered.
Injections of a mixture of corticosteroids and local anesthetics into the area may relieve pain. Other treatments include wrapping the foot and placing specially constructed devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses) in the shoe to reduce pressure on the nerve within the tarsal tunnel. When other treatments do not relieve the pain, surgery to relieve pressure on the nerve may be necessary.
Medial Plantar Nerve Entrapment
Medial plantar nerve entrapment is compression of a nerve at the inner heel (the medial plantar nerve) that causes pain, numbness, or tingling.
Symptoms include almost constant pain, whether walking or sitting. Just standing is often difficult. Burning, numbness, and tingling, which often occur when nerves are compressed, usually do not occur in medial plantar nerve entrapment.
Doctors base the diagnosis usually on the person’s symptoms and the results of an examination.
Splints and other devices (foot orthoses) that change the position or range of movement of the foot and relieve pressure on affected joints to prevent irritating motion and pressure may help, as may physical therapy and application of extreme cold to the nerve (cryotherapy). If these treatments do not work, injection with an alcohol solution to deaden the nerve or surgery to free the nerve from compressive structures may help relieve pain.
Tibialis Posterior Tendinosis
Tibialis posterior tendinosis is wear and tear of a tendon that passes behind and around the inner ankle.
The usual cause is excessive ongoing strain because of a problem in how the ankle moves. Most often, the problem is that the person’s arch is low and, when walking, the foot tends to turn inward because the person is overweight. Tendon dysfunction may further contribute to flattening of the arch. The tendon may tear completely, sometimes suddenly in a young person.
Early on, people have occasional pain behind the inner ankle. Over time, the pain becomes severe, and swelling occurs. Normal standing and walking become difficult. Standing on the toes is usually painful and may be impossible if the tendon is completely torn.
Doctors can often base the diagnosis on the person’s symptoms and the results of an examination. However, sometimes magnetic resonance imaging (MRI) is necessary to confirm the diagnosis and to see the extent of tendon damage.
Devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses) and ankle braces are usually enough. Complete rupture may require surgery for a person to regain normal function. Surgery is especially important in young active people with tears that develop suddenly.
Plantar Fasciosis
Plantar fasciosis is pain originating from the dense band of tissue called the plantar fascia that extends from the bottom of the heel bone to the base of the toes (ball of the foot).
 The connective tissue between the heel and ball of the foot may become damaged and painful.
The connective tissue between the heel and ball of the foot may become damaged and painful.
 Pain is often worse when first bearing weight and is felt at the heel.
Pain is often worse when first bearing weight and is felt at the heel.
 Stretches, changing footwear, wearing devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses) and splints, and sometimes corticosteroid injections can help.
Stretches, changing footwear, wearing devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses) and splints, and sometimes corticosteroid injections can help.
The plantar fascia connects the bottom of the heel bones to the ball of the foot and is involved in walking and running, giving spring to the step.
Plantar fasciosis is sometimes referred to as plantar fasciitis. However, this term is not correct. The term fasciitis means inflammation of the fascia, but plantar fasciosis is a disorder primarily of repeated stress to the fascia rather than a disorder of inflammation. Other terms used to describe plantar fasciosis include calcaneal enthesopathy and calcaneal spur syndrome (heel spur). However, a heel spur may or may not be present. Often a small tear results from excessive strain placed on the plantar fascia. Plantar fasciosis is one of the most common causes of heel pain.
Plantar fasciosis can develop in those who have sedentary lifestyles, wear high-heeled shoes, have unusually high or low arches in the feet, or have tight calf muscles or a tight Achilles tendon (which attaches the calf muscles to the heel bone). Sedentary people are usually affected when they suddenly increase their level of activity or wear less supportive shoes. Plantar fasciosis is also common among runners and dancers because of the increased stress on the fascia, especially if the person also has poor foot posture. The development of this painful disorder occurs more often in people whose occupations involve standing or walking on hard surfaces for prolonged periods. Disorders that may cause or aggravate plantar fasciosis are obesity, rheumatoid arthritis, and other types of arthritis.
Symptoms
A person with plantar fasciosis may have pain anywhere along the course of the plantar fascia but most commonly where the fascia joins the bottom of the heel bone. The person often feels a great deal of pain after resting, particularly when placing weight on the foot first thing in the morning. The pain temporarily diminishes after the person first walks but may return later in the day. It may also begin when the person walks or runs. In this case, the pain radiates from the bottom of the heel toward the toes. Some people have burning or sticking pain along the inside border of the sole of the foot when walking.
Diagnosis
The doctor may make the diagnosis after examining the foot. Tenderness is evident where the plantar fascia enters the heel bone or at the bottom of the ball of the foot.
X-rays may reveal the presence of a heel spur protruding from the bottom front edge of the heel bone. This heel spur is a growth of extra bone produced over time by a combination of increased strain on the fascia and foot dysfunction. However, people with plantar fasciosis often do not have heel spurs, and most people with heel spurs do not have pain, so the presence of heel spurs does not necessarily confirm plantar fasciosis. Other diagnostic tests, such as magnetic resonance imaging (MRI), are rarely needed.
Treatment
To relieve the stress and pain on the fascia, the person can take shorter steps and avoid walking barefoot. Activities that involve foot impact, such as jogging, should be avoided. The person may need to lose weight. Stretching the calf muscles and foot often accelerates healing. Orthoses placed into well-fitting supportive shoes can help to cushion, elevate, and support the heel.
Other measures that may be needed include use of adhesive strapping or arch-supporting wraps, ice massage, use of nonsteroidal anti-inflammatory drug (NSAIDs), occasional corticosteroid injections into the heel, physical therapy, and splinting at night to stretch the calf muscles and fascia during sleep. Corticosteroid injections should probably not be done more than a few times or else they might make the disorder worse. If these measures do not help sufficiently, a cast may be applied. If symptoms are still bothersome, surgery is very rarely required to attempt to partially release pressure on the fascia and remove any heel spurs.
What Is a heel Spur?
A heel spur is a growth of extra bone on the heel bone (calcaneus). It may form when the plantar fascia, the connective tissue extending from the bottom of the heel bone to the base of the toes, pulls excessively on the heel. The spur may be painful as it develops, but it may become less painful as the foot adjusts to it. Most spurs can be treated without surgery.

Inferior Calcaneal Bursitis
Bursitis is painful inflammation of a bursa (a flat sac containing joint [synovial] fluid that reduces friction in areas where skin, muscles, tendons, and ligaments rub over bones). Bursitis can develop at the bottom of the heel. The heel may throb, particularly when the shoes are removed, and may be slightly warm and swollen. The diagnosis is based on a person’s symptoms and examination results.
This disorder is treated by injecting a local anesthetic/corticosteroid mixture and wearing soft-soled shoes with added protective heel cushion padding.
Achilles Tendon Bursitis
Achilles tendon bursitis is inflammation of the fluid-filled sac (bursa) located either between the skin of the heel and the Achilles tendon (posterior Achilles tendon bursitis) or in front of the attachment of the Achilles tendon to the heel bone (anterior Achilles tendon bursitis, retrocalcaneal bursitis).
 Typical symptoms include swelling and warmth and a tender spot at the back of the heel.
Typical symptoms include swelling and warmth and a tender spot at the back of the heel.
 The diagnosis is based on symptoms, an examination, and sometimes x-rays.
The diagnosis is based on symptoms, an examination, and sometimes x-rays.
 Treatment is aimed at relieving the inflammation and, depending on the location of the Achilles tendon bursitis, eliminating the pressure on the back of the heel.
Treatment is aimed at relieving the inflammation and, depending on the location of the Achilles tendon bursitis, eliminating the pressure on the back of the heel.
The Achilles tendon is the tendon that attaches the calf muscles to the heel bone. Posterior Achilles tendon bursitis is often associated with formation of a bone prominence called Haglund’s deformity or “pump bump” on the heel bone. Anterior Achilles tendon bursitis is also called Albert’s disease or retromalleolar bursitis.
Posterior Achilles tendon bursitis occurs mainly in young women but can develop in men. Walking in a way that repeatedly presses the soft tissue behind the heel against the stiff back support of a shoe can cause or aggravate the bursitis. Shoes that taper sharply inward toward the posterior heel (such as high-heeled shoes) can lead to the development of this bursitis.
Any condition that puts extra strain on the Achilles tendon can cause anterior Achilles tendon bursitis. Injuries to the heel and diseases such as rheumatoid arthritis can also cause it.
Symptoms
When the bursa becomes inflamed after an injury, symptoms usually develop suddenly. When the bursa develops without an injury, symptoms may develop gradually. With both posterior and anterior Achilles tendon bursitis, symptoms usually include swelling and warmth at the back of the heel. A mildly red, swollen, tender spot develops on the back of the heel. When the inflamed bursa enlarges, it appears as a red lump under the skin of the heel and causes pain at and above the heel. If posterior Achilles tendon bursitis becomes chronic, the swelling may become hard, fluid-filled, and red or flesh-colored.
Diagnosis
The diagnosis is based on the symptoms and an examination. For anterior Achilles tendon bursitis, doctors use x-rays to rule out a fracture of the heel bone or damage to the heel bone caused by rheumatoid arthritis or another inflammatory arthritis.
Bursitis in the Heel
Normally, only one bursa is in the heel, between the Achilles tendon and the heel bone (calcaneus). This bursa may become inflamed, swollen, and painful, resulting in anterior Achilles tendon bursitis.
Abnormal pressure and foot dysfunction can cause a protective bursa to form between the Achilles tendon and the skin. This bursa may also become inflamed, swollen, and painful, resulting in posterior Achilles tendon bursitis.

Treatment
With anterior and posterior Achilles tendon bursitis, applying warm or cool compresses to the area and using nonsteroidal anti-inflammatory drugs (NSAIDs) can temporarily relieve the pain and inflammation, as can injections of a mixture of corticosteroids and local anesthetics into the inflamed bursa. The doctor is careful not to inject the mixture into the tendon. After this treatment, the person must rest. When these treatments are not effective, part of the heel bone may need to be surgically removed.
With posterior Achilles tendon bursitis, treatment is aimed at reducing the inflammation and adjusting the foot’s position in the shoe to relieve pressure and motion on the back of the heel. Foam rubber or felt heel pads can be placed in the shoe to eliminate pressure by elevating the heel. Stretching the back part of the shoe or placing padding around the inflamed bursa may help. Sometimes a special shoe, such as a running shoe designed to stabilize the midsole heel, devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses), or both can help to control abnormal foot and heel motion contributing to the posterior heel irritation. Other shoes have padding that reduces irritation to the posterior heel and Achilles tendon.
Achilles Tendon Enthesopathy
Achilles tendon enthesopathy is pain where the Achilles tendon attaches to the back of the heel.
The cause is chronic stretching of the Achilles tendon where it attaches to the heel. Contracted or shortened calf muscles caused by being sedentary and overweight or caused by athletic overuse increase the risk.
People typically feel pain at the back of the heel below the top of the shoe when walking.
The diagnosis is based on a physical examination of the tendon. Manually bending (flexing) the ankle during the examination usually makes the pain worse.
Exercises that stretch the calf muscles for 10 minutes 3 times daily can help. A person can stretch the calf muscle while facing a wall at arms’ length, with the knees straight and the foot bent upward. To minimize stress to the Achilles tendon when walking, the foot and ankle should be moved actively through the ranges of motion for about a minute when rising after long periods of rest. Night splints may also be used to stretch the tendon during sleep and help prevent shortening. Heel lifts should be used temporarily to relieve pain and decrease stress on the tendon while walking.
Corns and Calluses
Corns are hard cone-shaped bumps of skin commonly found on the upper surface of the smaller toes, particularly over a joint. Calluses are somewhat rounded flat thickenings of the skin located on the under-surface of the foot.
Corns and calluses are usually caused by friction and pressure, particularly from tight or ill-fitting shoes. Hammer toe and other toe deformities are often responsible for the development of corns on the top of or at the tip of the toes. Calluses often develop under the ball of the foot because of faulty foot positioning and poor weight distribution. Symptoms include a generalized burning sensation or (at times) severe pain in a specific area. People who have diabetes and a diminished sensation to light touch and protective sensation are at increased risk of developing ulcers and an infection at the site of the callus or corn if left untreated.
Treatment usually requires removal through scraping with a scalpel. After this procedure, padding of various sorts (for example, felt or moleskin) may be applied to remove pressure from the healing area. Devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses) or other inserts that have padding and metatarsal support pads can help to reduce pressure caused by callus build-up under the balls of the feet. Dells, which are holes cut through part of the footwear beneath the area that is painful, can also help reduce pressure and pain.
If the blood supply to the affected area is poor, surgical removal of the dead tissue may not be possible. In this case, special shoes that reduce pressure over the affected area may be necessary.
Bunion
In bunion, the joint of the base of the big toe appears to stick out (becomes prominent).
 Abnormalities in joint position or motion can distort and enlarge or seem to enlarge the joint that connects the big toe with the foot.
Abnormalities in joint position or motion can distort and enlarge or seem to enlarge the joint that connects the big toe with the foot.
 Pain and swelling can affect the inner part of the joint or the entire joint.
Pain and swelling can affect the inner part of the joint or the entire joint.
 Changing shoes, using pads or devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses), or a combination of measures usually helps.
Changing shoes, using pads or devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses), or a combination of measures usually helps.
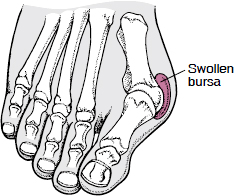
A condition that is often part of the bunion is an abnormal position of the big toe or the bone to which it connects. One such condition is an abnormality in which the joint at the base of the big toe bulges outward from the inner side of the foot and the big toe points inward (toward the smaller toes). This is called hallux valgus. Other factors that contribute may include excessive turning in (pronation) of the ankles and occasionally injury. Osteoarthritis may develop, and bone spurs may form. Osteoarthritis may cause joint scarring, limiting the foot’s range of motion. The joint may swell. A bursa (a painful swelling of the fluid-filled sac) can develop and become swollen and tender if tight shoes are worn.
Symptoms and Diagnosis
The first symptom may be painless enlargement of the joint or pain at the joint when wearing certain shoes. Later symptoms may include increasing enlargement without pain; a painful, warm, red swelling at the inner aspect of the joint; and swelling and pain all around the joint. Joint motion may be restricted.
Hallux Valgus With a Bunion
A hallux valgus is a bulging out of the base of the big toe sideways, away from the foot. The end of the big toe tilts in toward the second toe. A bunion is enlargement of the base of the big toe. A bursa is a painful swelling of the fluid-filled sac at the base of the big toe. A bunion is caused by hallux valgus.
Doctors usually base the diagnosis on symptoms and examination findings. If the diagnosis is uncertain, x-rays are taken. If infection is suspected, doctors withdraw and analyze joint fluid. If multiple joints are affected, tests may be done to diagnose arthritis.
Treatment
Mild discomfort may significantly lessen by wearing shoes with a wide toe box. If not, bunion pads purchased in most pharmacies can shield the painful area. Orthoses can also help redistribute and relieve pressure from the affected joint. If these measures are ineffective or if the person is unwilling to wear large, wide shoes and orthoses because they are unattractive, surgery is considered. Sometimes taking nonsteroidal anti-inflammatory drugs (NSAIDs) or injecting a corticosteroid with or without an anesthetic can help relieve pain and swelling. If the joints are stiff, stretching exercises, which occasionally require injection of a local anesthetic to relieve muscle spasm, can help. Sometimes, surgery to release scar tissue and improve alignment is necessary.
Hammer Toe
Hammer toe is a toe that is in a fixed (rigid) contracted position.
Among the causes of hammer toe are a long metatarsal bone, poor foot posture, rheumatoid arthritis, and years of wearing ill-fitting shoes. Because part of the toe is higher than normal, excessive friction may result, leading to corns and possibly ulcers on the top of the toe. Wearing shoes, particularly shoes with low and narrow toe boxes, may be painful. Doctors treat hammer toe by ensuring that the shoes are comfortable and have a wide enough toe box to avoid further irritation to the toe. Any ulcer or other skin irritation is treated. Toe pads sold in pharmacies also help by shielding the affected toes from the overlying shoe. An operation to straighten the hammer toe may be needed when other treatments do not relieve the pain and disability caused by the rigidly fixed toe.
What Is Hammer Toe?
In hammer toe, the second, third, or fourth toe becomes bent and cannot be straightened without surgery.

Plantar Fibromatosis
Plantar fibromatosis is a noncancerous (benign) growth of connective tissue in the sole (the plantar fascia).
In plantar fibromatosis, bumps develop on the sole and are most obvious when the foot is bent upward against the leg. Most people also have bumps in the palms, usually located at the fourth knuckle.
Treatment is usually not worthwhile unless the bumps become large enough to cause pain when bearing weight. If so, devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses) can help redistribute pressure away from the bumps.