CHAPTER 120
Multiple Sclerosis and Related Disorders
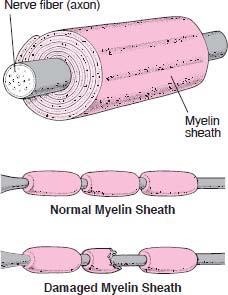
Most nerve fibers inside and outside the brain are wrapped with many layers of tissue composed of a fat (lipoprotein) called myelin. These layers form the myelin sheath. Much like the insulation around an electrical wire, the myelin sheath enables electrical impulses to be conducted along the nerve fiber with speed and accuracy. When the myelin sheath is damaged, nerves do not conduct electrical impulses normally. Sometimes the nerve fibers are also damaged.
Insulating a Nerve Fiber
When babies are born, many of their nerves lack mature myelin sheaths. As a result, their movements are jerky, uncoordinated, and awkward. As myelin sheaths develop, movements become smoother, more purposeful, and more coordinated. Myelin sheaths do not develop normally in children with certain rare hereditary diseases, such as Tay-Sachs disease, Niemann-Pick disease, Gaucher’s disease, and Hurler’s syndrome. These children may have permanent, often extensive, neurologic problems.
In adults, the myelin sheath can be destroyed by stroke, inflammation, immune disorders, metabolic disorders, and nutritional deficiencies (such as a lack of vitamin B12). Such destruction is called demyelination. Poisons, drugs (such as the antibiotic ethambutol), and excessive use of alcohol can damage or destroy the myelin sheath. If the sheath is able to repair and regenerate itself, normal nerve function may return. However, if the sheath is severely damaged, the underlying nerve fiber can die. Because nerve fibers in the central nervous system (brain and spinal cord) rarely regenerate, such damage is irreversible.
Some disorders that cause demyelination affect mainly the central nervous system. Others affect mainly nerves in other parts of the body. Disorders that cause demyelination in the central nervous system and have no known cause are called primary demyelinating disorders. Multiple sclerosis is the most common of these disorders.
Multiple Sclerosis
In multiple sclerosis, patches of myelin and underlying nerve fibers in the eyes, brain, and spinal cord are damaged or destroyed.
 The cause is unknown but may involve an attack by the immune system against the body’s own tissues (autoimmune reaction).
The cause is unknown but may involve an attack by the immune system against the body’s own tissues (autoimmune reaction).
 Usually, periods of relatively good health alternate with episodes of worsening symptoms.
Usually, periods of relatively good health alternate with episodes of worsening symptoms.
 People may have vision problems and abnormal sensations, and movements may be weak and clumsy.
People may have vision problems and abnormal sensations, and movements may be weak and clumsy.
 Usually, doctors base the diagnosis on symptoms and results of a physical examination and magnetic resonance imaging.
Usually, doctors base the diagnosis on symptoms and results of a physical examination and magnetic resonance imaging.
 Treatment includes corticosteroids, drugs that help keep the immune system from attacking the body, and drugs to relieve symptoms.
Treatment includes corticosteroids, drugs that help keep the immune system from attacking the body, and drugs to relieve symptoms.
 Often, the disorder slowly worsens, disabling some people, but life span is unaffected unless the disorder is very severe.
Often, the disorder slowly worsens, disabling some people, but life span is unaffected unless the disorder is very severe.
The term “multiple sclerosis” refers to the many areas of scarring (sclerosis) that result from destruction of the tissues that wrap around nerves (myelin sheath). This destruction is called demyelination. Sometimes the nerve fibers that send messages (axons) are also damaged. Over time, the brain may shrink in size because axons are destroyed.
In the United States, about 400,000 people, mostly young adults, have multiple sclerosis. Most commonly, it begins between the ages of 20 and 40. It is more common among women. Most people have periods of relatively good health (remissions) alternating with periods of worsening symptoms (flare-ups or relapses). Relapses can be mild or debilitating. Recovery during remission is good but incomplete. Thus, the disorder worsens slowly over time.
Causes
The cause is unknown, but a likely explanation is that people are exposed early in life to a virus (possibly a herpesvirus or retrovirus) or some unknown substance that somehow triggers the immune system to attack the body’s own tissues (autoimmune reaction—see page 1124). The autoimmune reaction results in inflammation, destruction of myelin, and damage to the myelin sheath and the underlying nerve fiber.
Heredity seems to have a role in multiple sclerosis. About 5% of people with the disorder have a brother or sister who is affected, and about 15% have a close relative who is affected. Also, multiple sclerosis is more likely to develop in people with certain genetic markers on the surface of their cells called human leukocyte antigens (see page 1099). These markers help the body to distinguish self from nonself and thus know which substances to attack.
Environment also has a role in multiple sclerosis. Where people spend the first 15 years of life affects their chance of developing multiple sclerosis. It occurs in 1 of 2,000 people who grow up in a temperate climate but in only 1 of 10,000 people who grow up in a tropical climate. Multiple sclerosis almost never occurs in people who grow up near the equator. These differences may be related to vitamin D levels. When the skin is exposed to sunlight, the body forms vitamin D. Thus, people who grow up in temperate climates may have a lower vitamin D level. People with a low level of vitamin D are more likely to develop multiple sclerosis. But how vitamin D may protect against the disorder is unknown. The climate in which later years are spent does not change the chances of developing the disorder.
Cigarette smoking also appears to increase the chances of developing the disorder. The reason is unknown.
 Did You Know…
Did You Know…
Nerves are covered with tissues that, like insulation around an electric wire, help the nerve conduct impulses.
Symptoms
Symptoms vary greatly, from person to person and from time to time in one person, depending on which nerve fibers are demyelinated. If nerve fibers that carry sensory information become demyelinated, problems with sensations (sensory symptoms) result. If nerve fibers that carry signals to muscles become demyelinated, problems with movement (motor symptoms) result. Symptoms often come and go, affecting one or several parts of the body. The fluctuating symptoms result from damage to myelin sheaths, followed by repair, followed by more damage. Symptoms may become more severe when people are exposed to high temperatures, such as in very warm weather, a hot bath or shower, or during a fever.
Multiple sclerosis may progress and regress unpredictably. However, there are several patterns of symptoms:
 Relapsing-remitting pattern: Relapses (when symptoms worsen) alternate with remissions (when symptoms are stable). Remissions may last months or years. Relapses can occur spontaneously or can be triggered by an infection such as influenza.
Relapsing-remitting pattern: Relapses (when symptoms worsen) alternate with remissions (when symptoms are stable). Remissions may last months or years. Relapses can occur spontaneously or can be triggered by an infection such as influenza.
 Primary progressive pattern: The disease progresses gradually with no remissions or obvious relapses, although there may be temporary plateaus during which the disease does not progress.
Primary progressive pattern: The disease progresses gradually with no remissions or obvious relapses, although there may be temporary plateaus during which the disease does not progress.
 Secondary progressive pattern: This pattern begins with relapses alternating with remissions, followed by gradual progression of the disease.
Secondary progressive pattern: This pattern begins with relapses alternating with remissions, followed by gradual progression of the disease.
 Progressive relapsing pattern: The disease progresses gradually, but progression is interrupted by sudden relapses. This pattern is rare.
Progressive relapsing pattern: The disease progresses gradually, but progression is interrupted by sudden relapses. This pattern is rare.
COMMON SYMPTOMS OF MULTIPLE SCLEROSIS
| PART OF THE BODY | EXAMPLES |
| Nerves (affecting sensation) |
Numbness Tingling A reduced sense of touch Pain or burning Itching |
| Eyes | Double vision Partial blindness and pain in one eye Dim or blurred vision Inability to see when looking straight ahead Uncoordinated eye movements |
| Genital organs | Difficulty reaching orgasm Lack of sensation in the vagina In men, impotence |
| Muscles and coordination | Weakness and clumsiness Difficulty walking or maintaining balance Tremor Uncoordinated movements Stiffness, unsteadiness, and unusual fatigue |
| Intestine and bladder | Problems controlling urination and bowel movements Constipation |
| Mood | Mood swings Inappropriate elation or giddiness Depression Inability to control emotions (for example, crying or laughing without reason) |
| Brain | Subtle or obvious mental impairment Memory loss Poor judgment Inattention |
| Other | Dizziness or vertigo |
Vague symptoms of demyelination in the brain sometimes begin long before the disorder is diagnosed. For example, tingling, numbness, pain, burning, and itching may occur in the arms, legs, trunk, or face. The sense of touch may be reduced. People may lose strength or dexterity in a leg or hand, which may become stiff.
Vision may become dim or blurred. Mainly, people lose the ability to see when looking straight ahead (central vision). Peripheral (side) vision is less affected. In some people, one eye becomes weaker than the other, causing double vision when looking from one side to the other. This disorder is called internuclear ophthalmoplegia. The stronger eye may move involuntarily, rapidly and repetitively moving in one direction, then slowly drifting back (a symptom called nystagmus). Partial blindness may develop in one eye, and pain occurs when the eye is moved. These symptoms result from inflammation of the optic nerve (optic neuritis). Some people with multiple sclerosis have only optic neuritis.
When the back part of the spinal cord in the neck is affected, bending the neck forward may cause an electrical shock or a tingling sensation that shoots down the back, down both legs, down one arm, or down one side of the body (a response called Lhermitte’s sign). Usually, the sensation lasts only a moment and disappears when the neck is straightened. Often, it is felt as long as the neck remains bent.
As the disorder progresses, movements may become shaky, irregular, and ineffective. People may become partially or completely paralyzed. Weak muscles may contract involuntarily (called spasticity), sometimes causing painful cramps. Muscle weakness and spasticity may interfere with walking, eventually making it impossible, even with a walker or another assistive device. Speech may become slow, slurred, and hesitant.
Late in the disorder, dementia and mania (excessive elation) may develop. The nerves that control urination or bowel movements can be affected, leading to frequent and strong urges to urinate, retention of urine, constipation, and, occasionally, urinary and fecal incontinence. If relapses become more frequent, people become increasingly disabled, sometimes permanently.
Diagnosis
Because symptoms vary widely, doctors may not recognize the disorder in its early stages. Doctors suspect multiple sclerosis in younger people who suddenly develop blurred vision, double vision, or movement problems and abnormal sensations in various unrelated parts of the body. Fluctuating symptoms and a pattern of relapses and remissions support the diagnosis.
When doctors suspect multiple sclerosis, they thoroughly evaluate the nervous system during a physical examination (see page 630). They examine the back of the eye (retina) with an ophthalmoscope (see art on page 1422). The optic disk (the spot where the optic nerve joins the retina) may be inflamed or unusually pale, indicating inflammation of the optic nerve.
Magnetic resonance imaging (MRI) is the best imaging test for detecting multiple sclerosis. It usually detects areas of demyelination in the brain and spinal cord. Before MRI, doctors may inject gadolinium, a paramagnetic contrast agent, into the bloodstream. Gadolinium helps distinguish areas of recent demyelination and active inflammation from areas of long-standing demyelination.
The diagnosis may be clear based on the physical examination and MRI. If not, other tests are done to obtain additional information:
 Spinal tap (lumbar puncture): A sample of cerebrospinal fluid is removed (see page 635). The protein content of the fluid may be higher than normal. The concentration of antibodies may be high, and a specific pattern of antibodies is detected in up to 90% of people with multiple sclerosis.
Spinal tap (lumbar puncture): A sample of cerebrospinal fluid is removed (see page 635). The protein content of the fluid may be higher than normal. The concentration of antibodies may be high, and a specific pattern of antibodies is detected in up to 90% of people with multiple sclerosis.
 Evoked responses: For this test, sensory stimuli, such as flashing lights, are used to activate certain areas of the brain, and the brain’s electrical responses are recorded (see page 636). In people with multiple sclerosis, the brain’s response to stimuli may be slow because signal conduction along demyelinated nerve fibers is impaired. This test can also detect slight damage to the optic nerve.
Evoked responses: For this test, sensory stimuli, such as flashing lights, are used to activate certain areas of the brain, and the brain’s electrical responses are recorded (see page 636). In people with multiple sclerosis, the brain’s response to stimuli may be slow because signal conduction along demyelinated nerve fibers is impaired. This test can also detect slight damage to the optic nerve.
Other tests can help doctors distinguish multiple sclerosis from disorders that cause similar symptoms, such as AIDS, vasculitis, arthritis of the neck, Guillain-Barré syndrome, hereditary ataxias, lupus, Lyme disease, rupture of a spinal disk, syphilis, and a cyst in the spinal cord (syringomyelia). For example, blood tests may be done to rule out Lyme disease, syphilis, and lupus, and imaging tests can help rule out arthritis of the neck, rupture of a spinal disk, and syringomyelia.
Prognosis
What effects multiple sclerosis has and how quickly it progresses vary greatly and unpredictably. Remissions can last months up to 10 years or more. However, some people, particularly men who develop the disorder during middle age, have frequent attacks and are rapidly incapacitated. Nonetheless, about 75% of people who have multiple sclerosis never need a wheelchair, and for about 40%, normal activities are not disrupted. Unless the disorder is very severe, life span is usually unaffected.
 Did You Know…
Did You Know…
Spending the first 15 years of life in a temperate (rather than tropical) climate increases the risk of multiple sclerosis.
Three fourths of people with multiple sclerosis never need a wheelchair.
Treatment
No treatment for multiple sclerosis is uniformly effective. Corticosteroids are most commonly used. They probably work by suppressing the immune system. They are given for short periods to relieve immediate symptoms. For example, prednisone may be taken by mouth, or methylprednisolone may be given intravenously. Although corticosteroids may shorten relapses and slow the progression of multiple sclerosis, they do not stop its progression.
Corticosteroids are rarely used for a long time because they can have many side effects, such as increased susceptibility to infection, diabetes, weight gain, fatigue, decreased bone density (osteoporosis), and ulcers. Corticosteroids are started and stopped as needed.
Other drugs that help keep the immune system from attacking myelin sheaths are usually used. They include the following:
 Interferon-beta injections reduce the frequency of relapses and may help prevent or delay disability.
Interferon-beta injections reduce the frequency of relapses and may help prevent or delay disability.
 Glatiramer acetate injections may have similar benefits for people with early mild multiple sclerosis.
Glatiramer acetate injections may have similar benefits for people with early mild multiple sclerosis.
 Mitoxantrone, a chemotherapy drug, can reduce the frequency of relapses and slow the progression of the disorder. It is given for only up to 2 years and only when other drugs do not work because it can eventually lead to heart damage.
Mitoxantrone, a chemotherapy drug, can reduce the frequency of relapses and slow the progression of the disorder. It is given for only up to 2 years and only when other drugs do not work because it can eventually lead to heart damage.
 Natalizumab is an antibody given intravenously as an infusion once a month. It is more effective than other drugs in reducing the number of relapses and preventing further damage in the brain. However, natalizumab may increase the risk of a rare, fatal infection of the brain and spinal cord (progressive multifocal leukoencephalopathy). Natalizumab is used only by specially trained doctors, and people who take it must be checked periodically for signs of progressive multifocal leukoencephalopathy.
Natalizumab is an antibody given intravenously as an infusion once a month. It is more effective than other drugs in reducing the number of relapses and preventing further damage in the brain. However, natalizumab may increase the risk of a rare, fatal infection of the brain and spinal cord (progressive multifocal leukoencephalopathy). Natalizumab is used only by specially trained doctors, and people who take it must be checked periodically for signs of progressive multifocal leukoencephalopathy.
 Immune globulin, given intravenously once a month, occasionally helps when other drugs have been ineffective.
Immune globulin, given intravenously once a month, occasionally helps when other drugs have been ineffective.
Plasmapheresis is recommended by some experts for severe relapses not controlled by corticosteroids. However, the benefits of plasmapheresis have not been established. For this treatment, blood is withdrawn, abnormal antibodies are removed from it, and the blood is returned to the person (see box on page 1030).
Other drugs can be used to relieve or control specific symptoms:
 Muscle spasms: The muscle relaxants baclofen or tizanidine
Muscle spasms: The muscle relaxants baclofen or tizanidine
 Urinary incontinence: Oxybutynin, bethanechol, or tamsulosin
Urinary incontinence: Oxybutynin, bethanechol, or tamsulosin
 Pain due to abnormalities in nerves: The anticonvulsant gabapentin or sometimes tricyclic antidepressants (such as amitriptyline), the anticonvulsant carbamazepine, or opioids
Pain due to abnormalities in nerves: The anticonvulsant gabapentin or sometimes tricyclic antidepressants (such as amitriptyline), the anticonvulsant carbamazepine, or opioids
 Tremors: The beta-blocker propranolol
Tremors: The beta-blocker propranolol
 Fatigue: Amantadine (used to treat Parkinson’s disease) or, less often, modafinil (used to treat excessive sleepiness)
Fatigue: Amantadine (used to treat Parkinson’s disease) or, less often, modafinil (used to treat excessive sleepiness)
 Depression: Antidepressants such as sertraline or amitriptyline, counseling, or both
Depression: Antidepressants such as sertraline or amitriptyline, counseling, or both
People with multiple sclerosis can often maintain an active lifestyle, although they may tire easily and may not be able to keep up with a demanding schedule. Regular exercise such as riding a stationary bicycle, walking, swimming, or stretching reduces spasticity and helps maintain cardiovascular, muscular, and psychologic health. Physical therapy can help with maintaining balance, the ability to walk, and range of motion and can help reduce spasticity and weakness. People should walk on their own for as long as possible. Doing so improves their quality of life and helps prevent depression. Avoiding high temperatures—for example, by not taking hot baths or showers—can help because heat can worsen symptoms. People who smoke should stop. Taking vitamin D supplements helps prevent osteoporosis or slow its progression and may help slow the progression of multiple sclerosis.
People with urine retention can learn to catheterize themselves and empty the bladder, and those with constipation can take stool softeners or laxatives regularly. People who become weak and unable to move easily may develop pressure sores, so they and their caregivers must take extra care to prevent the sores.
If people are disabled, occupational therapists and social workers can help with rehabilitation.
Other Primary Demyelinating Diseases
Acute Disseminated Encephalomyelitis: Also called parainfectious or postinfectious encephalomyelitis, this rare type of inflammation leads to demyelination of nerves in the brain and spinal cord. (Demyelination is the destruction of the tissues that wrap around nerves, called the myelin sheath.)
This disorder usually develops after a viral infection. Acute disseminated encephalomyelitis is thought to be a misguided immune reaction triggered by the virus. In the United States, this disorder usually results from some types of influenza, hepatitis A or B, or infection with enteroviruses, Epstein-Barr virus, or human immunodeficiency virus (HIV). Measles, chickenpox, and rubella used to be common causes before childhood vaccination became widespread.
Typically, the inflammation develops 1 to 3 weeks after the viral illness begins. It can be treated with corticosteroids given intravenously. Guillain-Barré syndrome (see page 828) seems to be a similar disorder of the peripheral nerves.
Adrenoleukodystrophy and Adrenomyeloneuropathy: Both are rare hereditary metabolic disorders. Adrenoleukodystrophy affects young boys, usually between the ages of 4 and 8. A milder, more slowly developing form of the disorder can begin in adults in their 20s or 30s. Adrenomyeloneuropathy affects adolescent boys.
In these disorders, widespread demyelination is accompanied by adrenal gland dysfunction. Boys have behavioral problems and problems with hearing and vision. Eventually, mental deterioration, involuntary and uncoordinated muscle contractions (spasticity), and blindness occur.
No cure for either disorder is known. Dietary supplements with glycerol trioleate and glycerol trierucate (known as Lorenzo’s oil) have not been shown to slow the progression of the disease. Bone marrow transplantation is an experimental treatment.
Leber’s Hereditary Optic Neuropathy: This disorder causes demyelination leading to partial blindness. The disorder is more common among men. Usually, symptoms begin between the ages of 15 and 35. This disorder is inherited through the mother, and the defective genes seem to be located in mitochondria (structures in cells that provide energy for the cell).
No treatments are available. But limiting consumption of alcohol, which may affect the mitochondria, and not using tobacco products may help.
Tropical Spastic Paraparesis: Also called HTLV-associated myelopathy (see page 806), this disorder causes demyelination in the spinal cord and results from infection with the human T-cell lymphotropic virus (HTLV). The disorder worsens over several years. Gradually, the legs become weak and muscle spasms occur—a condition called spastic weakness. Frequent, strong urges to urinate, urinary incontinence, and bowel dysfunction also develop.
No cure is available, but corticosteroids may help, as may interferon-beta or immune globulin given intravenously (these drugs help prevent the immune system from attacking myelin sheaths). Muscle relaxants such as baclofen or tizanidine help relieve spasms.
Neuromyelitis Optica: Also called Devic disease, this disorder causes symptoms similar to those of multiple sclerosis and used to be considered a variant of multiple sclerosis. However, neuromyelitis optica typically affects only the eyes and the spinal cord, and multiple sclerosis also affects the brain.
Neuromyelitis optica causes inflammation of the optic nerve (optic neuritis). One or both eyes may be affected. The disorder causes episodes of eye pain and dim, blurred, or lost vision. Days to weeks (sometimes years) later, the limbs are affected. People may temporarily lose sensation, and the arms and legs may become weak and sometimes paralyzed. People may be unable to control bladder and bowel function.
In some people, the part of the spinal cord that controls breathing is inflamed, leading to difficulty breathing, which is life threatening.
The disorder progresses differently in each person. As the disorder progresses, people may have brief, frequent, painful muscle spasms. Eventually, blindness, loss of sensation and muscle weakness in the limbs, and bladder and bowel dysfunction may become permanent.
To diagnose the disorder, doctors evaluate the nervous system (neurologic examination) during a physical examination (see page 630). The optic nerve is examined with an ophthalmoscope (see art on page 1422). Tests include magnetic resonance imaging (MRI) and a blood test to detect specific antibodies in people with neuromyelitis optica.
There is no cure. However treatments can stop episodes, control symptoms, and prevent episodes from recurring. A corticosteroid (such as methylprednisolone) and a drug that suppresses the immune system (an immunosuppressant, such as azathioprine) are often used to stop and prevent episodes. Rituximab, a relatively new drug, may be used to reduce the number of abnormal antibodies and to control disorder. Plasma exchange (plasmapheresis) may help people who do not respond to corticosteroids. For this treatment, blood is removed, then abnormal antibodies are removed, and the blood is returned to the person.
Treatment of symptoms is similar to that for multiple sclerosis (see page 791). Baclofen or tizanidine may relieve muscle spasms.