CHAPTER 122
Low Back and Neck Pain
Low back and neck pain are among the most common reasons for health care visits. The pain usually results from problems with the spine, including the bones of the spine (vertebrae) and the muscles and ligaments that support it. Occasionally, low back or neck pain results from another disorder, such as a stomach ulcer, pneumonia, premenstrual syndrome, or infection of the prostate gland. Some disorders cause only low back or neck pain. Others can cause both.
Low Back Pain
 Common causes include sprains and strains, osteoarthritis, osteoporosis, a ruptured or herniated disk, fibromyalgia, and, in older people, spinal stenosis.
Common causes include sprains and strains, osteoarthritis, osteoporosis, a ruptured or herniated disk, fibromyalgia, and, in older people, spinal stenosis.
 Pain may be intermittent or constant, superficial or deep, or dull or sharp, depending on the cause.
Pain may be intermittent or constant, superficial or deep, or dull or sharp, depending on the cause.
 Doctors base the diagnosis on symptoms, results of a physical examination, and sometimes x-rays or other imaging tests.
Doctors base the diagnosis on symptoms, results of a physical examination, and sometimes x-rays or other imaging tests.
 Exercising regularly is the best way to prevent low back pain.
Exercising regularly is the best way to prevent low back pain.
 For most low back pain, avoiding activities that stress the back, taking pain relievers, and applying ice or heat are often all that is needed.
For most low back pain, avoiding activities that stress the back, taking pain relievers, and applying ice or heat are often all that is needed.
Low back pain is very common and becomes more common as people age. It is very costly in terms of healthcare payments, disability payments, and missed work. Thus, although low back pain rarely results from life-threatening disorders, it is a significant health problem. However, the number of back injuries in the workplace is decreasing, perhaps because awareness of the problem has increased and preventive measures have improved.
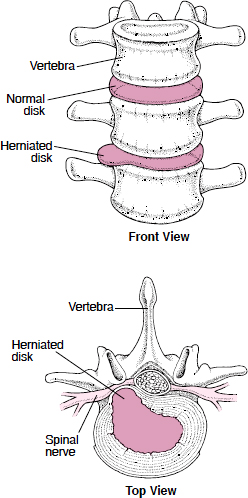
A Herniated Disk
The tough covering of a disk in the spine can tear (rupture), causing pain. The soft, jelly-like interior may then bulge out (herniate) through the covering, causing more pain. Pain occurs because the bulge puts pressure on the spinal nerve root next to it. Sometimes the nerve root becomes inflamed or is damaged.
More than 80% of herniated disks occur in the lower back. They are most common among people aged 30 to 50 years. Between these ages, the covering weakens. The interior, which is under high pressure, may squeeze through a tear or a weakened spot in the covering and bulge out. After age 50, the interior of the disk begins to harden, making a herniation less likely.
A disk may herniate because of a sudden, traumatic injury or repeated minor injuries. Being overweight or lifting heavy objects, particularly lifting incorrectly, increases the risk.
Often, herniated disks cause no symptoms, but they may cause slight to debilitating pain. Movement intensifies the pain.
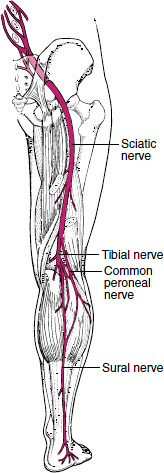
Where the pain occurs depends on which disk is herniated and which spinal nerve root is affected. The pain may be felt along the pathway of the nerve compressed by the herniated disk. For example, a herniated disk commonly causes sciatica—pain along the sciatic nerve.
A herniated disk can also cause numbness and muscle weakness. If the pressure on the nerve root is great, the legs may be paralyzed. If the cauda equina (the bundle of nerves extending from the bottom of the cord) is affected, control of bladder and bowels can be lost. If these serious symptoms develop, medical attention is required immediately.
Most people recover without any treatment, usually within 3 months, but often much faster. Applying cold (such as ice packs) or heat (such as a heating pad) or using over-the-counter analgesics may help relieve the pain. Sometimes surgery to remove part or all the disk and part of a vertebra is necessary. In 10 to 20% of people who have surgery for sciatica due to a herniated disk, another disk ruptures.
The spine (spinal column) consists of the back bones (vertebrae), which are separated and cushioned by shock-absorbing disks made of cartilage. The vertebrae are also covered by a thin layer of cartilage. They are held in place by ligaments and muscles, which include the following:
 Two iliopsoas muscles, which run along both sides of the spine
Two iliopsoas muscles, which run along both sides of the spine
 Two erector spinae muscles, which run along the length of the spine behind it
Two erector spinae muscles, which run along the length of the spine behind it
 Many short paraspinal muscles, which run between the vertebrae
Many short paraspinal muscles, which run between the vertebrae
These muscles help stabilize the spine. The abdominal muscles, which run from the bottom of the rib cage to the pelvis, also help stabilize the spine by supporting the abdominal contents.
Enclosed in the spine is the spinal cord (see page 627 and 793). Along the length of the spinal cord, the spinal nerves emerge through spaces between the vertebrae to connect with nerves throughout the body. The part of the spinal nerve nearest the spinal cord is called the spinal nerve root. Because of their position, spinal nerve roots can be compressed when the spine is injured, resulting in pain.
What Is Sciatica?
The two sciatic nerves are the widest and longest nerves in the body. Each is almost as wide as a finger. On each side of the body, the sciatic nerve runs from the lower spine, behind the hip joint, down the buttock and back of the knee. There the sciatic nerve divides into several branches and continues to the foot. When the sciatic nerve is pinched, inflamed, or damaged, pain—sciatica—may radiate along the length of the sciatic nerve to the foot. Sciatica occurs in about 5% of people who have back pain.
In some people, no cause can be detected. In others, the cause may be a herniated disk, irregular projections of bone due to osteoarthritis, spinal stenosis, or swelling due to a sprained ligament. Rarely, Paget’s disease of bone, nerve damage due to diabetes (diabetic neuropathy), a tumor, or an accumulation of blood (hematoma) or pus (abscess) causes sciatica. Some people seem to be prone to sciatica.
Sciatica usually affects only one side. It may cause a pins-and-needles sensation, a nagging ache, or shooting pain. Numbness may be felt in the leg or foot. Walking, running, climbing stairs, straightening the leg, and sometimes coughing or straining worsens the pain, which is relieved by straightening the back or sitting.
Often, the pain goes away on its own. Resting, sleeping on a firm mattress, taking over-the-counter acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), and applying heat and cold may be sufficient treatment. For many people, sleeping on their side with the knees bent and a pillow between the knees provides relief. Stretching the hamstring muscles gently after warming up may help. Occasionally, other treatments are used. They include anticonvulsants, tricyclic anti-depressants, and, for severe and persistent pain, surgery or corticosteroids.
The lower (lumbar) spine consists of five vertebrae. It connects the chest to the pelvis and legs, providing mobility—for turning, twisting, and bending. It also provides strength—for standing, walking, and lifting. Thus, the lower back is involved in almost all activities of daily living. Low back pain can limit many activities and reduce the quality of life.
Causes
Low back pain has many causes, although often no specific cause can be identified.
Muscle strains and ligament sprains are the most common causes. Strains and sprains may result from lifting, exercising, or moving in an unexpected way (such as when falling or when in a car accident). When due to exercise, injury to the lower back is sometimes called weight lifter’s back (lumbar strain). Weight lifter’s back may be caused not only by snatching a heavy weight from the ground in weight lifting but also by pushing against an opposing lineman in football, suddenly turning to dribble after a rebound in basketball, swinging a bat in baseball, or swinging a club in golf. The lower back is more likely to be injured when a person’s physical conditioning is poor and the supporting muscles of the back are weak. Having poor posture, lifting incorrectly, being overweight, and being tired also contribute.
Osteoarthritis (degenerative arthritis) causes the cartilage that covers and protects the vertebrae to deteriorate. This disorder is thought to be due, at least in part, to the wear and tear of years of use. People who repetitively stress one joint or a group of joints are more likely to develop osteoarthritis. The disks between the vertebrae deteriorate, narrowing the spaces between them and often compressing spinal nerve roots. Irregular projections of bone (spurs) may develop on the vertebrae and compress spinal nerve roots. All of these changes can cause low back pain as well as stiffness.
In osteoporosis, bone density decreases, making the bones more likely to fracture. The vertebrae are particularly susceptible to the effects of osteoporosis. Osteoporosis often results in crush (compression) fractures (which sometimes cause sudden, severe back pain) and compression of spinal nerve roots (which may cause chronic back pain). However, most fractures due to osteoporosis occur in the upper and middle back and cause upper and middle rather than low back pain.
A ruptured or herniated disk can cause low back pain. A disk has a tough covering and a soft, jellylike interior. If a disk is suddenly squeezed by the vertebrae above and below it (as when lifting a heavy object), the covering may tear (rupture), causing pain. The interior of the disk can squeeze through the tear in the covering, so that part of the interior bulges out (herniates). This bulge can compress, irritate, and even damage the spinal nerve root next to it, causing more pain. A ruptured or herniated disk also commonly causes sciatica.
In ankylosing spondylitis, the spine and large joints are inflamed, resulting in stiffness and back pain. This disorder is more common among men, usually starting between the ages of 20 and 40.
Spinal stenosis is narrowing of the spinal canal (the passageway that runs through the center of the spine and contains the spinal cord). It is a common cause of low back pain in older people. Spinal stenosis also develops in middle-aged people who were born with a narrow spinal canal. It is caused by such disorders as osteoarthritis, spondylolisthesis, rheumatoid arthritis, ankylosing spondylitis, and Paget’s disease of the bone. Spinal stenosis may cause sciatica as well as low back pain.
Fibromyalgia is a common cause of low back pain. This disorder causes chronic widespread (diffuse) pain in muscles, tendons, ligaments, and other soft tissues (see page 616). It is most common among women aged 20 to 50.
Referred pain (see box on page 639) sometimes causes low back pain. Referred pain originates in another part of the body, such as the lungs, kidneys, uterus, prostate gland, or organs of the digestive tract but is felt in the lower back. For example, low back pain can be caused by premenstrual syndrome, a prostate infection, pancreatitis, a severe peptic ulcer, an abdominal aortic aneurysm, pelvic inflammatory disease, or ectopic pregnancy.
 Did You Know…
Did You Know…
Strengthening abdominal muscles, as well as back muscles, helps prevent low back pain.
Compression of the spinal cord, a serious disorder, can cause low back pain (see page 799). Compression may result from a severe injury, a herniated disk, accumulation of blood (hematoma), an abscess, or a tumor.
Spondylolisthesis is partial displacement of a vertebra in the lower back. It usually occurs in people who have a birth defect (spondylolysis) that weakens part of the vertebrae. Usually, during adolescence, a minor injury causes a part of the vertebra to fracture. The vertebra then slips forward over the one below it. If it slips far, pain can result.
Other less common causes of low back pain include shingles, cancer that has spread to the spine from other organs (such as the breasts, lungs, prostate gland, or kidneys), bone cancer (multiple myeloma), infections (such as an abscess in the spinal cord or a bone infection), Paget’s disease of bone, and birth defects (such as scoliosis).
Stress may contribute to low back pain, but how it does so is unclear. Heavy physical labor, obesity, smoking, and lack of exercise also contribute to low back pain.
Symptoms
Low back pain varies depending on the cause and type of pain. It may be
 Intermittent or constant
Intermittent or constant
 Superficial or deep
Superficial or deep
 Dull and aching, throbbing, or sharp and stabbing
Dull and aching, throbbing, or sharp and stabbing
Back pain may interfere with sleep.
Types of low back pain include the following: Local Pain: Pain occurs in a specific area of the lower back. It is usually due to sprains and strains. Sudden pain may be felt when the injury occurs. Local pain can often be relieved by changes in position or by light activity followed by stretching. Intense physical activity or prolonged inactivity (such as bed rest) tends to make it worse. Local pain may be constant and aching or, at times, intermittent and sharp. The lower back may be sore when touched. Muscle spasms may occur because the body moves in unusual ways as it tries to avoid the movements that trigger pain. Usually, local pain resolves gradually over days to weeks.
Pain Due to Compression of a Spinal Nerve Root: A nerve root may be compressed by disorders such as a herniated disk, osteoarthritis, spinal stenosis, or Paget’s disease of bone. The pain often occurs within minutes or hours of lifting a very heavy weight, but it may occur spontaneously. It tends to be a dull ache sometimes accompanied by a sharp, intense radiating pain. The pain can radiate to different parts of the body, depending on which nerve root is affected. Commonly, the pain extends from the lower back into the buttock and down the leg past the knee on the affected side, indicating sciatica. Coughing, sneezing, straining, or bending over while keeping the legs straight can trigger the sharp, radiating pain. The pain varies by cause:
 Herniated disk: The pain is worsened by walking a distance.
Herniated disk: The pain is worsened by walking a distance.
 Spinal stenosis: The pain is typically increased by straightening the back (as when walking) and is relieved by bending the spine forward (as when leaning forward).
Spinal stenosis: The pain is typically increased by straightening the back (as when walking) and is relieved by bending the spine forward (as when leaning forward).
 Compression fracture due to osteoporosis: The pain may start suddenly, stay in a particular area of the back, and worsen when a person stands or walks. The area near the fracture may be tender.
Compression fracture due to osteoporosis: The pain may start suddenly, stay in a particular area of the back, and worsen when a person stands or walks. The area near the fracture may be tender.
Usually, the pain and tenderness disappear gradually after a few weeks or months. If pressure on the nerve root is great or if the spinal cord is also compressed, the pain may be accompanied by muscle weakness in the leg, a pins-and-needles sensation, or even loss of sensation and loss of bladder and bowel control.
Referred Pain: Back pain that originates in other organs tends to be deep, aching, constant, and relatively widespread, but it can vary. Typically, movement does not affect it, unlike pain from back disorders, and it may worsen at night.
Other Types: Some disorders cause typical types of pain:
 Infection or cancer: Pain is constant and progressively worsens. It is unrelieved by rest.
Infection or cancer: Pain is constant and progressively worsens. It is unrelieved by rest.
 Ankylosing spondylitis: The pain is accompanied by stiffness that is worse just after a person wakes up.
Ankylosing spondylitis: The pain is accompanied by stiffness that is worse just after a person wakes up.
 Fibromyalgia: Pain occurs throughout the body or moves from part to part. Muscles ache, feel stiff, and may be tender to the touch. The pain may be throbbing, aching, or stabbing. Fibromyalgia is often accompanied by poor sleep.
Fibromyalgia: Pain occurs throughout the body or moves from part to part. Muscles ache, feel stiff, and may be tender to the touch. The pain may be throbbing, aching, or stabbing. Fibromyalgia is often accompanied by poor sleep.
Diagnosis
Doctors ask the person about the pain:
 What the pain is like
What the pain is like
 What relieves or worsens it
What relieves or worsens it
 When and how it started
When and how it started
 Whether other symptoms are also present
Whether other symptoms are also present
Doctors also do a physical examination, focusing on the spine and including evaluation of the nervous system (a neurologic examination). As part of the physical examination, doctors may ask the person to move in certain ways to determine the type of pain. For example, they may ask the person to lie flat, then lift the leg without bending the knee.
With information about the pain, the person’s medical history, and results of a physical examination, doctors may be able to identify the cause. Usually, no other tests are needed because most back pain results from strains and sprains and resolves within 6 weeks. If another cause is suspected or if back pain persists, other tests are often needed.
X-rays of the lower back can help detect degenerative changes due to osteoarthritis, compression fractures due to osteoporosis, and scoliosis. However, magnetic resonance imaging (MRI) or computed tomography (CT) provides clearer images and can confirm or exclude the diagnosis of a herniated disk, spinal stenosis, or cancer. These tests can also indicate whether degenerative changes due to osteoarthritis are responsible for compressing nerves. If compression of the spinal cord is suspected, MRI is done immediately. Rarely, when results of MRI are unclear, myelography (see page 636) with CT is required. Occasionally, electromyography and nerve conduction studies (see page 636) are done to confirm the location of nerve damage.
Prevention
The most effective way to prevent low back pain is to exercise regularly. Aerobic exercise and specific muscle-strengthening and stretching exercises can help.
Aerobic exercise, such as swimming and walking, improves general fitness and generally strengthens muscles. Specific exercises to strengthen and stretch the muscles in the abdomen, buttocks, and back can help stabilize the spine and decrease strain on the disks that cushion the spine and the ligaments that hold it in place.
Muscle-strengthening exercises include pelvic tilts and abdominal curls. Stretching exercises include the sitting leg stretch, knee-to-chest stretch, and hip and quadriceps stretch. Stretching exercises can increase back pain in some people and therefore should be done carefully. As a general rule, any exercise that causes or increases back pain should be stopped. Exercises should be repeated until the muscles feel mildly but not completely fatigued. Breathing during each exercise is important. People who have back pain should consult a doctor before beginning to exercise.
Exercises to Prevent Low Back Pain
Pelvic Tilts
Lie on the back with the knees bent, the heels on the floor, and the weight on the heels. Press the small of the back against the floor, contract the buttocks (raising them about half an inch from the floor), and contract the abdominal muscles. Hold this position for a count of 10. Repeat 20 times.

Abdominal Curls
Lie on the back with the knees bent and feet on the floor. Place the hands across the chest. Contract the abdominal muscles, slowly raising the shoulders about 10 inches from the floor while keeping the head back (the chin should not touch the chest). Then release the abdominal muscles, slowly lowering the shoulders. Do 3 sets of 10.

Knee-to-Chest Stretch
Lie flat on the back. Place both hands behind one knee and bring it to the chest. Hold for a count of 10. Slowly lower that leg and repeat with the other leg. Do this exercise 10 times.

Sitting Leg Stretch
Sit on the floor with the knees straight but slightly flexed (not locked) and the legs as far apart as possible. Place both hands on the same knee. Slowly slide both hands toward the ankle. Stop if pain is felt and go no farther than a position that can be held comfortably for 10 seconds. Slowly return to a sitting position. Repeat with the other leg. Do this exercise 10 times for each leg.

Hip and Quadriceps Stretch
Stand with one foot on the floor and the knee of the other leg bent at about a 90° angle. Grasp the front of the ankle of the bent leg with the hand on the same side. (The other hand may be placed on the back of a chair or on the wall for balance.) Keeping the knees together, press the foot against the hand and away from the body. Hold for a count of 10. Repeat with the other leg. Do this exercise 10 times.

Exercise can also help people maintain bone density and a desirable weight. Thus, exercise may reduce the risk of developing two conditions that can lead to low back pain—osteoporosis and obesity.
Maintaining good posture when standing and sitting reduces stress on the back. Slouching should be avoided. Chair seats can be adjusted to a height that allows the feet to be flat on the floor, with the knees bent up slightly and the lower back flat against the back of the chair. If a chair does not support the lower back, a pillow can be used behind the lower back. Sitting with the feet on the floor rather than with the legs crossed is advised. People should avoid standing or sitting for long periods. If prolonged standing or sitting is unavoidable, changing positions frequently may reduce stress on the back.
Sleeping in a comfortable position on a firm mattress is recommended. Pillows under the waist and head can be used for support by people who sleep on their side, and a pillow under the knees can be used by those who sleep on their back. Pillows under the head should not force the neck to bend too much.
Learning to lift correctly helps prevent back injury. The knees should be bent enough that the arms are level with the object to be lifted. The legs, not the back, should be used to lift. Lifting an object over the head increases the risk of back injury. Heavy objects should be carried close to the body.
Stopping smoking is also recommended.
Treatment
For low back pain that has recently developed, treatment begins with avoiding activities that stress the spine and cause pain—such as lifting heavy objects and bending. Bed rest does not hasten the resolution of the pain, and most experts recommend continued light activity. Bed rest, if required to relieve severe pain, should last no more than 1 or 2 days.
If a specific disorder is causing low back pain, treating that disorder—for example, giving antibiotics to treat a prostate infection—usually relieves the pain.
Over-the-counter or prescription nonsteroidal anti-inflammatory drugs (NSAIDs—see page 644) can be taken to relieve pain and reduce inflammation. If inflammation is not contributing to the pain (and it usually does not), acetaminophen is typically recommended for pain relief instead of an NSAID. Acetaminophen is slightly safer than NSAIDS.
Muscle relaxants, such as carisoprodol, cyclobenzaprine, diazepam, metaxalone, or methocarbamol, are sometimes given to relieve muscle spasms, but their usefulness is controversial. These drugs are not recommended for older people, who are more likely to have side effects.
Application of heat or cold and massage may help (see page 46). Usually, traction is not useful. Spinal manipulation, done by chiropractors or some other doctors (such as osteopathic doctors), may hasten the resolution of pain due to muscle spasm, strains, or sprains. However, it may have risks for people with osteoporosis or a herniated disk. Some reports suggest that acupuncture may have similar benefits, but others suggest little or no benefit.
After the pain has subsided, light activity, as recommended by a doctor or physical therapist, can speed healing and recovery. Specific exercises to strengthen and stretch the back and to strengthen the abdominal muscles are usually recommended to help prevent low back pain from becoming chronic or recurring. Other preventive measures (maintaining good posture, using a firm mattress with appropriately placed pillows, lifting correctly, and stopping smoking) should be continued or started. In response to these measures, most episodes of back pain resolve in several days to 2 weeks. Regardless of treatment, 80 to 90% of such episodes resolve within 6 weeks.
Treatment of Chronic Pain: If low back pain is chronic, additional measures are needed. Aerobic exercise may help, and weight reduction, if necessary, is advised. If the pain is severe, acetaminophen or NSAIDs may not provide sufficient pain relief, and opioid analgesics (see page 642) may be required. If these analgesics are ineffective, other treatments can be considered.
Transcutaneous electrical nerve stimulation (TENS) may be used (see page 648). The TENS device produces a gentle tingling sensation by generating a low oscillating current. A therapist applies the device to the painful area several times a day for 20 minutes to several hours at a time, depending on the severity of the pain. People are sometimes taught to use the device themselves.
Sometimes a corticosteroid (such as dexamethasone or methylprednisolone) plus a local anesthetic (such as lidocaine) is periodically injected into the epidural space—between the spine and the outer layer of tissue covering the spinal cord. These epidural injections are more effective for sciatica than for lumbar spinal stenosis. However, they are usually effective only for several days to weeks. Their main use is to relieve pain enough that an exercise program, which can provide long-term pain relief, can be started.
If a disorder causes severe and constant pain, serious symptoms, or sciatica lasts 6 months or more, surgery may be necessary. If a herniated disk is causing relentless sciatica, weakness, loss of sensation, or loss of bladder and bowel control, surgical removal of the disk (diskectomy) and part of the vertebra (laminectomy) may be necessary. A general anesthetic is usually required. The hospital stay after surgical removal of a disk is usually 1 or 2 days. Often, microsurgical techniques, with a small incision and a local anesthetic, can be used. Hospitalization is not required. However, when the incision is small, the surgeon may not be able to see and therefore may not remove all fragments of the herniated disk. After either procedure, most people can resume all of their activities after a few weeks. More than 90% of people recover fully.
DISORDERS THAT CAUSE ONLY NECK PAIN
For severe spinal stenosis, a large part of the vertebra may be surgically removed to widen the spinal canal. A general anesthetic is usually required. The hospital stay is usually 4 or 5 days. People may need 3 to 4 months before they can resume all of their activities. About two thirds of people have a good or full recovery. For most of the rest, symptoms are prevented from worsening.
When the spine is unstable because of degeneration due to osteoarthritis, vertebrae may be fused together. However, fusion decreases mobility and may put additional stress on the rest of the spine.
Neck Pain
 Neck pain usually results from strains and sprains.
Neck pain usually results from strains and sprains.
 Pain from the neck may shoot down an arm or cause a headache.
Pain from the neck may shoot down an arm or cause a headache.
 Doctors base the diagnosis on symptoms, results of a physical examination, and sometimes x-rays or other imaging tests.
Doctors base the diagnosis on symptoms, results of a physical examination, and sometimes x-rays or other imaging tests.
 Treatment includes taking pain relievers, applying ice or heat, wearing a neck collar, and learning how to stand, sit, and sleep to avoid straining the neck.
Treatment includes taking pain relievers, applying ice or heat, wearing a neck collar, and learning how to stand, sit, and sleep to avoid straining the neck.
The neck’s flexibility makes it susceptible to wear and tear and to injuries that overstretch it, such as whiplash. Also, the neck has the critical job of holding up the head. Poor posture makes that job more difficult. Thus, neck pain, like back pain, is common, and it becomes more common as people age.
The spine contains the spinal cord (see pages 627 and 793). Along the length of the spinal cord, spinal nerves emerge through spaces between the vertebrae to connect with nerves throughout the body. The part of the spinal nerve nearest the spinal cord (spinal nerve root) can be compressed when the spine is injured, resulting in pain. The part of the spine in the neck (cervical spine) consists of seven back bones (vertebrae), which are separated by disks.
The neck also contains muscles and ligaments to support the spine.
Causes
Most of the disorders that can cause low back pain can also cause neck pain, and most involve the spine, the tissues that support it, or both. The most common causes are muscle strains and ligament strains. Other causes include injuries, arthritis, a ruptured or herniated disk, meningitis, and fibromyalgia.
Some disorders cause neck pain but not back pain.
Other disorders that can cause neck pain include a tear in a neck artery’s lining (dissection), a blockage or tumor in the esophagus, infections (such as a bone infection), and inflammation of the esophagus or thyroid gland.
Sometimes neck pain is referred pain (see box on page 639), which originates in another part of the body. Referred neck pain may result from angina or a heart attack.
Symptoms
The neck may be tender, stiff, or both as well as painful. Pain may be worsened by movement. The pain may extend to the shoulders and upper back or may cause a headache. If a nerve is compressed, the pain may shoot down an arm. People may also feel tingling, numbness, or weakness in the arms or sometimes the legs. If the spinal cord is compressed, people may lose control of bladder and bowel functions (incontinence). Other symptoms occur depending on the disorder.
Diagnosis
Doctors can often base the diagnosis on a description of symptoms, risk factors (which may suggest a cause), and results of a physical examination, which includes evaluation of the nervous system (neurologic examination). As part of the physical examination, doctors may move or ask the person to move the neck in all directions to check its range of motion and to determine whether movement makes the pain worse.
X-rays can help identify some disorders, but magnetic resonance imaging (MRI) or computed tomography (CT) may be needed at some point to confirm the diagnosis. If spinal cord compression is suspected, MRI is done immediately. Other tests may also be needed. They include blood tests to check for infection or inflammation and electromyography and nerve conduction studies to determine whether the cause is related to muscles or nerves (see page 636).
Treatment
Treatment depends on the cause. But often, taking over-the-counter analgesics, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can relieve the pain. If inflammation is not contributing to the pain, acetaminophen is usually recommended instead of NSAIDs because it is thought to be safer. Ice or heat may also help (see page 46). People are taught how to stand, sit, and sleep in ways that do not strain the neck.
Doctors may recommend wearing a soft neck collar and using contour pillow for 10 to 14 days to help relieve pain and muscle spasms. People with unstable atlantoaxial subluxation may need to wear a rigid collar. Doctors or physical therapists may also suggest stretching exercises.
If more pain relief is needed, doctors may prescribe analgesics. Muscle relaxants, such as carisoprodol, cyclobenzaprine, diazepam, metaxalone, or methocarbamol, are sometimes used, but their usefulness is controversial. Muscle relaxants are not recommended for older people, who are more likely to have side effects.
For spasmodic torticollis, physical therapy or massage can sometimes temporarily stop the contractions. Drugs (including the anticonvulsant carbamazepine and some mild sedatives such as clonazepam), taken by mouth or injected, can usually relieve the pain. But drugs control contractions in only up to one third of people. If the pain is severe or if posture is distorted, botulinum toxin (a bacterial toxin used to paralyze muscles) may be injected into the affected muscles.
For shingles, antiviral drugs may shorten the duration of the symptoms, and wet compresses on the blisters may help relieve pain.
If the spinal cord or a spinal nerve is compressed or if the neck is unstable, surgery is usually needed.