CHAPTER 123
Peripheral Nerve Disorders
The peripheral nervous system refers to the parts of nervous system outside the central nervous system, that is, those outside the brain and spinal cord. The nerves that connect the head, face, eyes, nose, muscles, and ears to the brain (cranial nerves—see page 835) and the nerves that connect the spinal cord to the rest of the body, including the 31 pairs of spinal nerves, are part of the peripheral nervous system. This system also includes more than 100 billion nerve cells that run throughout the body.
Dysfunction of peripheral nerves may result from damage to any part of the nerve:
 Axon (the part that sends messages)
Axon (the part that sends messages)
 Body of the nerve cell
Body of the nerve cell
 Myelin sheath (the membranes that surround the axon, enabling nerve impulses to travel quickly—see art on page 788).
Myelin sheath (the membranes that surround the axon, enabling nerve impulses to travel quickly—see art on page 788).
If motor nerves (which stimulate muscle action) are damaged, muscles may weaken or become paralyzed. If sensory nerves (which carry sensory information) are damaged, abnormal sensations may be felt or sensation may be lost. Some peripheral nerve disorders are progressive and fatal.
Muscle Stimulation Disorders
Muscle stimulation (motor neuron) disorders are characterized by progressive deterioration of the nerves and other structures involved in muscle movement. These disorders develop when motor nerves do not stimulate muscles normally.
 Amyotrophic lateral sclerosis is the most common of these disorders.
Amyotrophic lateral sclerosis is the most common of these disorders.
 Typically, muscles are weak and waste away, and movements become stiff, clumsy, and awkward.
Typically, muscles are weak and waste away, and movements become stiff, clumsy, and awkward.
 Doctors base the diagnosis on results of electromyography, magnetic resonance imaging, and blood tests.
Doctors base the diagnosis on results of electromyography, magnetic resonance imaging, and blood tests.
 There is no specific treatment or cure, but drugs can help lessen symptoms.
There is no specific treatment or cure, but drugs can help lessen symptoms.
For normal muscle function, muscle tissue and nerve connections between the brain and muscle must be normal. In muscle stimulation disorders (motor neuron disorders), motor nerves do not stimulate muscles normally. As a result, muscles weaken, waste away (atrophy), and can become completely paralyzed even though the muscles themselves are not the cause of the problem.
Muscle stimulation disorders include amyotrophic lateral sclerosis (the most common), primary lateral sclerosis, progressive pseudobulbar palsy, progressive muscular atrophy, progressive bulbar palsy, and postpolio syndrome. These disorders are more common among men and usually develop in people who are in their 50s. The cause is usually unknown. About 10% of people who have a muscle stimulation disorder have a hereditary type and thus have family members who also have the disorder.
In all of these disorders, the parts of the nervous system involved in muscle movement—including motor nerves in the spinal cord and in other parts of the body and parts of the brain—progressively deteriorate, causing muscle weakness that can progress to paralysis. However, in each disorder, a different part of the nervous system is affected. Consequently, each disorder has different effects. For example, some affect the mouth and throat first, and others affect a hand or foot first or most severely.
Symptoms
Muscles are affected, but people do not have pain or any changes in sensation. Depression is common.
Amyotrophic Lateral Sclerosis (Lou Gehrig’s Disease): This progressive disorder begins with weakness, often in the hands and less frequently in the feet or mouth and throat. Weakness may progress more on one side of the body than on the other and usually proceeds up the arm or leg. Cramps are also common and may occur before the weakness, but no changes in sensation occur. People may lose weight and feel unusually tired.
Over time, weakness increases. Muscles twitch and become tight, followed by muscle spasms (spasticity). Tremors may appear. Controlling facial expressions may become difficult. Weakening of muscles in the throat may lead to difficulty speaking (dysarthria) and swallowing (dysphagia). Excess saliva is produced, sometimes causing drooling. As the disorder progresses, people may be unable to control emotional responses and may laugh or cry inappropriately.
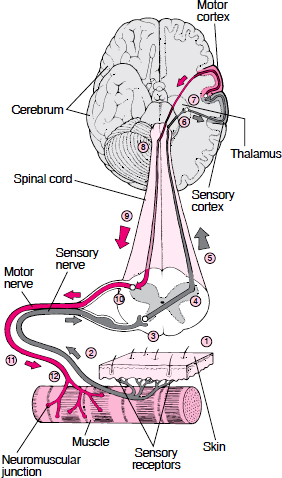
Using the Brain to Move a Muscle
Moving a muscle usually involves communication between the muscle and the brain through nerves. The impetus to move a muscle may originate with the senses. For example, special nerve endings in the skin (sensory receptors) enable people to sense pain, as when they step on a sharp rock, or to sense temperature, as when they pick up a very hot cup of coffee. This information is sent to the brain, and the brain may send a message to the muscle about how to respond. This type of exchange involves two complex nerve pathways: the sensory nerve pathway to the brain and the motor nerve pathway to the muscle.
1. If sensory receptors in the skin detect pain or a change in temperature, they transmit an impulse (signal), which ultimately reaches the brain.
2. The impulse travels along a sensory nerve to the spinal cord.
3. The impulse crosses a synapse (the junction between two nerve cells) between the sensory nerve and a nerve cell in the spinal cord.
4. The impulse crosses from the nerve cell in the spinal cord to the opposite side of the spinal cord.
5. The impulse is sent up the spinal cord and through the brain stem to the thalamus, which is a sensory processing center deep in the brain.
6. The impulse crosses a synapse in the thalamus to nerve fibers that carry the impulse to the sensory cortex of the cerebrum (the area that recieves and interprets information from sensory receptors).
7. The sensory cortex perceives the impulse. A person may then decide to initiate movement, which triggers the motor cortex (the area that plans, controls, and executes voluntary movements) to generate an impulse.
8. The nerve carrying the impulse crosses to the opposite side at the base of the brain.
9. The impulse is sent down the spinal cord.
10. The impulse crosses a synapse between the nerve fibers in the spinal cord and a motor nerve, which is located in the spinal cord.
11. The impulse travels out of the spinal cord along the length of the motor nerve.
12. At the neuromuscular junction, the impulse crosses from the motor nerve to the motor end plate on the muscle, where it stimulates muscle movement.
Eventually, the muscles involved in breathing may weaken, leading to breathing problems. Some people need a ventilator to breathe.
How rapidly amyotrophic lateral sclerosis progresses varies. About 50% of people with the disorder die within 3 years of the first symptoms, 10% live 10 years or more, and a few people survive as long as 30 years.
Primary Lateral Sclerosis and Progressive Pseudobulbar Palsy: These disorders are rare, slowly progressive variants of amyotrophic lateral sclerosis. Primary lateral sclerosis affects mainly the arms and legs, and progressive pseudobulbar palsy affects mainly the muscles of the face, jaw, and throat. In both disorders, severe stiffness accompanies muscle weakness. Emotions may be changeable: People with progressive pseudobulbar palsy may switch from happiness to sadness quickly and without reason. Inappropriate emotional outbursts are common. Many years later, muscles begin to twitch and waste away. The disorders usually progress for several years before total disability results.
Progressive Muscular Atrophy: This disorder can develop at any age. It is similar to amyotrophic lateral sclerosis, but it progresses more slowly, spasticity does not occur, and muscle weakness is less severe. Involuntary contractions or twitching of muscle fibers may be the earliest symptoms. The hands are usually affected first, followed by the arms, shoulders, and legs. Eventually, the whole body is affected. Many people with this disorder survive 25 years or longer.
Progressive Bulbar Palsy: In this disorder, the nerves controlling the muscles of chewing, swallowing, and talking are affected, making these functions increasingly difficult. The voice may have a nasal tone. In some people, emotions are changeable. Because swallowing is difficult, food or saliva is often inhaled (aspirated) into the lungs, causing choking or gagging and increasing the risk of pneumonia. Death, which is often due to pneumonia, usually occurs 1 to 3 years after the disorder begins.
Postpolio Syndrome: In some people who have had polio, muscles may become tired, painful, and weak 15 years or more after recovery from polio. Sometimes muscle tissue also wastes away, suggesting a reactivation of the polio infection. However, in most people who have had polio, such symptoms are not due to postpolio syndrome but to the development of a new disorder, such as diabetes, a slipped (herniated) disk, or osteoarthritis.
Diagnosis
Doctors suspect one of these disorders in adults who have progressive muscle weakness without pain or loss of sensation. Doctors ask people which parts of the body are affected, when the disorder started, what symptoms appeared first, and how the symptoms changed over time. This information gives them clues about the cause of symptoms.
Muscle weakness can have many causes (see table on page 541), so diagnostic tests, such as the following, are needed to help narrow the possibilities:
 Magnetic resonance imaging (MRI) of the brain and sometimes the spinal cord is done to check for abnormalities that may cause similar symptoms.
Magnetic resonance imaging (MRI) of the brain and sometimes the spinal cord is done to check for abnormalities that may cause similar symptoms.
 Electromyography (see page 636), which involves stimulating muscles and recording their electrical activity, can help determine whether the problem is in nerves or muscles.
Electromyography (see page 636), which involves stimulating muscles and recording their electrical activity, can help determine whether the problem is in nerves or muscles.
 Nerve conduction studies, which measures how fast nerves transmit impulses, may also be done. The speed of impulses is not affected until late in these disorders, so if impulses are unexpectedly slow, the cause of symptoms may be another disorder.
Nerve conduction studies, which measures how fast nerves transmit impulses, may also be done. The speed of impulses is not affected until late in these disorders, so if impulses are unexpectedly slow, the cause of symptoms may be another disorder.
 Blood tests are done to check for other disorders (such as infections and metabolic disorders) that do not affect the nerves but can cause weakness.
Blood tests are done to check for other disorders (such as infections and metabolic disorders) that do not affect the nerves but can cause weakness.
Treatment
Muscle stimulation disorders have no specific treatment or cure. Care provided by a team of several types of health care practitioners (multidisciplinary team) helps people cope with progressive disability. Physical therapy helps people maintain muscle strength and helps prevent shortening of muscles (contractures). Nurses or other caregivers must feed people with swallowing difficulties carefully to prevent choking. Some people must be fed through a tube inserted through the abdominal wall into the stomach (gastrostomy tube).
Baclofen may help make muscles less spastic, and phenytoin or quinine may help decrease cramps. Drugs with anticholinergic effects, such as amitriptyline (an antidepressant), may be used because of one of its anticholinergic effects—reducing saliva formation. Amitriptyline or fluvoxamine (also an antidepressant) may help people who have changeable emotions or depression.
In some people with amyotrophic lateral sclerosis, riluzole, a drug that protects nerve cells, can prolong life. It is taken by mouth.
If pain develops as the disorder progresses (for example, it may become painful to sit in one spot without being able to shift position), opioids and benzodiazepines, which are mild sedatives, may be used.
In a few people with progressive bulbar palsy, surgery to improve swallowing helps.
Because amyotrophic lateral sclerosis and progressive bulbar palsy are progressive and incurable, people with one of these disorders are advised to establish advanced directives that specify what kind of care they want at the end of life (see page 69).
Neuromuscular Junction Disorders
Nerves connect with muscles at the neuromuscular junction. There, the ends of nerve fibers connect to special sites on the muscle’s membrane called motor end plates. These plates contain receptors that enable the muscle to respond to acetylcholine, a chemical messenger (neurotransmitter) released by the nerve to transmit a nerve impulse across the neuromuscular junction. After a nerve stimulates a muscle at this junction, an electrical impulse flows through the muscle, causing it to contract.
Overactive Nerves: Tow Syndromes
Sometimes nerves repeatedly send electrical impulses to muscles, resulting in overstimulation. Overstimulation is thought to be a factor in Stiff-person syndrome and Isaac’s syndrome.
Stiff-person syndrome: This syndrome is more common among women and often occurs in people with diabetes or certain kinds of cancer, including Hodgkin lymphoma (Hodgkin’s disease).
The cause may be an autoimmune reaction—when the body produces antibodies that attack its own tissues. Antibodies to an enzyme called glutamic acid decarboxylase are present, but whether they cause the symptoms is unknown.
Muscles of the trunk, abdomen, and legs gradually become stiffer and enlarge. Muscles of the arms, head, and neck are affected less.
The sedative diazepam can consistently relieve the muscle stiffness. Plasmapheresis, in which toxic substances are filtered from the blood, is sometimes tried but often without success. Without treatment, the disorder progresses, leading to disability and stiffness throughout the body.
Isaac’s syndrome: This rare disorder has no known cause. It often occurs in people with cancer.
Muscles, particularly those in the arms and legs, continually twitch, moving like a bag of worms. This symptom is called myokymia. The hands and feet may intermittently have spasms and cramps. Muscle stiffness is common. Sweating may be increased.
Symptoms can be relieved by carbamazepine or phenytoin, both of which are anticonvulsants.
 Did You Know…
Did You Know…
Nerve gases used in chemical warfare interfere with communication between nerves and muscles.
Disorders in which the neuromuscular junction malfunctions include myasthenia gravis, botulism, and Eaton-Lambert syndrome. In addition, many drugs (including very high doses of some antibiotics), certain insecticides (organophosphates), curare (an extract from plants formerly placed on the tip of some poison darts and used to paralyze and kill), and the nerve gases used in chemical warfare can cause the neuromuscular junction to malfunction. Some of these substances prevent the normal breakdown of acetylcholine after the nerve impulse has been transmitted to the muscle.
MYASTHENIA GRAVIS
Myasthenia gravis is an autoimmune disorder that impairs communication between nerves and muscles, resulting in episodes of muscle weakness.
 Myasthenia gravis may result from malfunction of the immune system.
Myasthenia gravis may result from malfunction of the immune system.
 People usually have drooping eyelids and double vision, and muscles become unusually tired and weak after exercise.
People usually have drooping eyelids and double vision, and muscles become unusually tired and weak after exercise.
 Response to a drug given intravenously helps doctors determine whether people may have myasthenia gravis.
Response to a drug given intravenously helps doctors determine whether people may have myasthenia gravis.
 Electromyography, blood tests, and imaging tests are needed to confirm the diagnosis.
Electromyography, blood tests, and imaging tests are needed to confirm the diagnosis.
 Some drugs can improve muscle strength rapidly, and others can slow progression of the disorder.
Some drugs can improve muscle strength rapidly, and others can slow progression of the disorder.
Myasthenia gravis is more common among women. It usually develops in women between the ages of 20 and 40. However, the disorder may affect men or women at any age. Rarely, it begins during childhood.
In myasthenia gravis, the immune system produces antibodies that attack one type of receptor on the muscle side of the neuromuscular junction—the receptors that respond to the neurotransmitter acetylcholine. As a result, communication between the nerve cell and the muscle is disrupted. What causes the body to attack its own acetylcholine receptors—an autoimmune reaction—is unknown. According to one theory, malfunction of the thymus gland may be involved. In the thymus gland, certain cells of the immune system learn how to differentiate between the body and foreign substances. The thymus gland also contains muscle cells (myocytes) with acetyl-choline receptors. For unknown reasons, the thymus gland may instruct the immune system cells to produce antibodies that attack the acetylcholine receptors. People may inherit a predisposition to this autoimmune abnormality. About 65% of people who have myasthenia gravis have an enlarged thymus gland, and about 10% have a tumor of the thymus gland (thymoma). About half of thymomas are cancerous (malignant). Some people with the disorder do not have antibodies to acetylcholine receptors but have antibodies to an enzyme involved in the formation of the neuromuscular junction instead. These people may require different treatment.
The disorder may be triggered by infections, surgery, or use of certain drugs, such as nifedipine or verapamil (used to treat high blood pressure), quinine (used to treat malaria), and procainamide (used to treat abnormal heart rhythms).
Neonatal myasthenia develops in 12% of babies born to women who have myasthenia gravis. Antibodies against acetylcholine receptors, which circulate in the blood, may pass from a pregnant woman through the placenta to the fetus. In such cases, the baby has muscle weakness that disappears several days to a few weeks after birth. The remaining 88% of babies are not affected.
Symptoms
Episodes of worsened symptoms (exacerbations) are common. At other times, symptoms may be minimal or absent.
The most common symptoms are
 Weak, drooping eyelids
Weak, drooping eyelids
 Weak eye muscles, which cause double vision
Weak eye muscles, which cause double vision
 Excessive weakness of affected muscles after they are used
Excessive weakness of affected muscles after they are used
The weakness disappears when the muscles are rested but recurs when they are used again.
In 40% of people with myasthenia gravis, the eye muscles are affected first, but 85% eventually have this problem. In 15% of people, only the eye muscles are affected, but in most people, the whole body is affected. Difficulty speaking and swallowing and weakness of the arms and legs are common. Hand grip may alternate between weak and normal. This fluctuating grip is called milkmaid’s grip. Neck muscles may become weak. Sensation is not affected.
When people with myasthenia gravis use a muscle repetitively, the muscle usually becomes weak. For example, people who once could use a hammer well become weak after hammering for several minutes. However, muscle weakness varies in intensity from hour to hour and from day to day, and the course of the disease varies widely.
About 15% of people have severe episodes (called myasthenia crisis), sometimes triggered by an infection. The arms and legs may become extremely weak, but even then, they do not lose sensation. In some people, the muscles needed for breathing weaken. This condition is life threatening.
Diagnosis
Doctors suspect myasthenia gravis in people with episodes of weakness, especially when the eye or facial muscles are affected or when weakness increases with use of the affected muscles and disappears with rest. Because acetylcholine receptors are damaged, drugs that increase levels of acetylcholine can be used to help confirm the diagnosis. Edrophonium, injected intravenously, is most commonly used. People are asked to exercise the affected muscle until it tires. Then they are given the drug. If it temporarily and quickly improves muscle strength, myasthenia gravis is a possible diagnosis.
Other diagnostic tests are needed to confirm the diagnosis. They include electromyography (stimulating muscles, then recording their electrical activity) and blood tests to detect antibodies to acetylcholine receptors and sometimes the other antibodies present in people with the disorder. Blood tests are also done to check for other disorders. Computed tomography (CT) or magnetic resonance imaging (MRI) of the chest is done to assess the thymus gland and to determine whether a thymoma is present.
Treatment
Drugs may be used to help improve strength quickly or to suppress the autoimmune reaction and slow progression of the disorder.
Drugs that increase the amount of acetylcholine, such as pyridostigmine (taken by mouth), may improve muscle strength. Long-acting capsules are available for nighttime use to help people who experience severe weakness or difficulty swallowing when they awaken in the morning. Doctors must periodically adjust the dose, which may have to be increased during episodes of weakness. However, doses that are too high can cause weakness that is difficult to distinguish from that caused by the disorder. Also, the effectiveness of these drugs may decrease with long-term use. Increasing weakness, which may be due to a decrease in the drug’s effectiveness, must be evaluated by a doctor with expertise in treating myasthenia gravis.
Common side effects of pyridostigmine include abdominal cramps and diarrhea. Drugs that slow the activity of the digestive tract, such as atropine or propantheline, may be needed to counteract these effects.
To suppress the autoimmune reaction, doctors may also prescribe a corticosteroid, such as prednisone, or an immunosuppressant, such as cyclosporine or azathioprine. These drugs are taken by mouth. Most people need to take a corticosteroid indefinitely. When the corticosteroid is started, symptoms may worsen initially, but improvement occurs within a few months. The dose is then reduced to the minimum that is effective. Corticosteroids, when taken for a long time, can have moderate or severe side effects. Thus, azathioprine may be given so that the corticosteroid can be stopped or its dose reduced. With azathioprine, improvement takes about 18 months.
Immune globulin (a solution containing many different antibodies collected from a group of donors) may be given intravenously once a day for 5 days. Over two thirds of people improve in 1 to 2 weeks, and effects may last 1 to 2 months.
When drugs do not provide relief or when a myasthenic crisis occurs, plasmapheresis (see box on page 1030) may be used. In plasmapheresis, toxic substances (in this case, abnormal antibodies) are filtered from the blood.
If a thymoma is present, the thymus gland must be surgically removed to prevent the thymoma from spreading. If no thymoma is present, the benefit of removing the thymus gland is uncertain.
BOTULISM
Botulism is an uncommon, life-threatening poisoning caused by toxins produced by the bacterium Clostridium botulinum.
 Botulism toxins, usually consumed in food, can weaken or paralyze muscles.
Botulism toxins, usually consumed in food, can weaken or paralyze muscles.
 Botulism may begin with dry mouth, double vision, and inability to focus the eyes or with gastric distress.
Botulism may begin with dry mouth, double vision, and inability to focus the eyes or with gastric distress.
 Doctors examine samples of blood, stool, or tissue from the wound, and electromyography may be done.
Doctors examine samples of blood, stool, or tissue from the wound, and electromyography may be done.
 Careful food preparation and storage help prevent botulism.
Careful food preparation and storage help prevent botulism.
 An antitoxin is used to prevent or slow the effects of the toxin.
An antitoxin is used to prevent or slow the effects of the toxin.
Botulism is usually foodborne.
The toxins that cause botulism, which are very potent poisons, can severely impair nerve function. Because these toxins damage nerves, they are called neurotoxins. Botulism toxins paralyze muscles by inhibiting the release of the neurotransmitter acetyl-choline from nerves. In very small doses, the toxin can be used to relieve muscle spasms and to reduce wrinkles.
Causes
The bacterium Clostridium botulinum forms reproductive cells called spores. Like seeds, spores can exist in a dormant state for many years, and they are highly resistant to destruction. When moisture and nutrients are present and oxygen is absent (as in the intestine or sealed jars or cans), the spores start to grow and produce toxins. Some toxins produced by Clostridium botulinum are not destroyed by the intestine’s protective enzymes.
Clostridium botulinum is common in the environment, and spores can be transported by air. Many cases of botulism result from ingesting or inhaling small amounts of soil or dust. Spores can also enter the body through the eyes or a break in the skin.
There are several different forms of botulism.
Foodborne botulism occurs when food contaminated with the toxins is eaten. The most common sources of foodborne botulism are home-canned foods, particularly foods with a low acid content, such as asparagus, green beans, beets, and corn. Other sources include chopped garlic in oil, chili peppers, tomatoes, foil-wrapped baked potatoes that have been left at room temperature too long, and home-canned or fermented fish. However, about 10% of outbreaks result from eating commercially prepared foods, most commonly, vegetables, fish, fruits, and condiments (such as salsa). Less commonly, beef, milk products, pork, poultry, and other foods cause botulism.
Wound botulism occurs when Clostridium botulinum contaminates a wound or is introduced into other tissues. Inside the wound, the bacteria produce toxins that are absorbed into the bloodstream. Injecting drugs with needles that are not sterilized can cause this type of botulism, as can injecting contaminated heroin into a muscle or under the skin (skin popping).
Infant botulism develops in infants who eat food containing spores of the bacteria rather than toxins. The spores then grow in the infant’s intestine, where they produce toxins. The cause of most cases is unknown, but some cases have been linked to the ingestion of honey. Infant botulism occurs most commonly among infants younger than 6 months.
 Did You Know…
Did You Know…
The toxin that causes botulism can be used to treat uncontrollable muscle spasms and to reduce wrinkles.
Injecting illicit drugs increases the risk of botulism.
Symptoms
Symptoms of foodborne botulism develop suddenly, usually 18 to 36 hours after toxins enter the body, although symptoms can start as soon as 4 hours or as late as 8 days after ingesting the toxins. The more toxin ingested, the sooner people become sick. Usually, people who become sick within 24 hours of eating contaminated food are the most severely affected.
The first symptoms of foodborne or wound botulism commonly include dry mouth, double vision, drooping eyelids, and an inability to focus on nearby objects. The pupils of the eyes do not constrict normally when exposed to light during an eye examination. However, in foodborne botulism, the first symptoms are often nausea, vomiting, stomach cramps, and diarrhea. People who have wound botulism do not have any digestive symptoms.
Nerve damage by the toxins affects muscle strength but not sensation. Muscle tone in the face may be lost. Speaking and swallowing become difficult. Because swallowing is difficult, food or saliva is often inhaled (aspirated) into the lungs, causing choking or gagging and increasing the risk of pneumonia. Some people become constipated. The muscles of the arms and legs and the muscles involved in breathing become progressively weaker as symptoms gradually move down the body. Breathing problems may be life threatening. The mind usually remains clear.
In about 90% of infants with infant botulism, constipation is the first symptom. Then the muscles become paralyzed, beginning in the face and head and eventually reaching the arms, legs, and muscles involved in breathing. Eyelids droop, crying is weak, infants are less able to suck, and their face loses its expression. Problems range from being tired and feeding slowly to losing a substantial amount of muscle tone and having difficulty breathing. When infants lose muscle tone, they may feel abnormally limp.
Diagnosis
Doctors suspect botulism based on symptoms. However, other disorders can cause similar symptoms, so additional information is needed.
Electromyography (stimulating muscles and recording their electrical activity—see page 636) may be useful. In most cases of botulism, it shows abnormal muscle responses after electrical stimulation.
For foodborne botulism, a likely food source provides a clue. For example, when botulism occurs in two or more people who ate the same food prepared in the same place, the diagnosis is clearer. The diagnosis is confirmed when the toxins are detected in the blood or when the bacteria are detected in a culture of stool. Toxins may also be identified in food that the person ate.
For wound botulism, doctors ask whether people have had an injury that broke the skin. Doctors may inspect the skin for puncture marks suggesting use of an illicit drug. The diagnosis is confirmed when the toxins are detected in the blood or when the bacteria are detected in a culture of tissue from the wound.
Detecting the bacteria or the toxins in a sample of an infant’s stool confirms the diagnosis of infant botulism.
Sometimes determining whether botulism developed from a wound or from food is impossible.
Prevention
The spores of Clostridium botulinum are highly resistant to heat and may survive boiling for several hours. However, the toxins are readily destroyed by heat. Stored foods can cause botulism if they were inadequately cooked before they were stored. The bacteria can produce some toxins at temperatures as low as 37.4° F (3° C), a typical refrigerator temperature, so refrigerating food does not automatically make it safe.
 Did You Know…
Did You Know…
Infants should not be fed honey.
The following measures can help prevent food-borne botulism:
 Cooking food at 176°F (79.9° C) for 30 minutes, which almost always destroys toxins
Cooking food at 176°F (79.9° C) for 30 minutes, which almost always destroys toxins
 Boiling home-canned food for 10 minutes, which destroys the toxins
Boiling home-canned food for 10 minutes, which destroys the toxins
 Discarding canned foods that are discolored or smell spoiled
Discarding canned foods that are discolored or smell spoiled
 Discarding cans that are swollen or leaking
Discarding cans that are swollen or leaking
 Refrigerating oils infused with garlic or herbs
Refrigerating oils infused with garlic or herbs
 Keeping potatoes that have been baked in aluminum foil hot until served
Keeping potatoes that have been baked in aluminum foil hot until served
 Not feeding children younger than 2 years honey, which may contain Clostridium botulinum spores
Not feeding children younger than 2 years honey, which may contain Clostridium botulinum spores
If people are unsure whether a can should be discarded, they can check it when they start to open it. Before making the first puncture, they can place a few drops of water in the spot to be punctured. If water is expelled rather than sucked into the can when the can is punctured, the can is contaminated and should be discarded.
Any food that may be contaminated should be disposed of carefully. Even tiny amounts of toxins ingested, inhaled, or absorbed through the eye or a break in the skin can cause serious illness. Skin contact should be avoided as much as possible, and hands should be washed immediately after handling the food.
If a wound becomes infected, promptly seeking medical attention can reduce the risk of wound botulism.
Researchers and other people who work with the bacteria or its toxin are immunized.
Treatment
People who may have botulism should go to the hospital immediately. Laboratory tests to confirm the diagnosis are done, but treatment often cannot be delayed until the results are known. To help eliminate any unabsorbed toxin, doctors may give activated charcoal by mouth or through a tube inserted into the stomach.
Vital signs (pulse, breathing rate, blood pressure, and temperature) are measured often. If breathing problems begin, people are transferred to an intensive care unit and may be temporarily placed on a ventilator. Such treatment has reduced the percentage of deaths due to botulism from about 70% in the early 1900s to less than 10%.
A substance that blocks the action of the toxins (antitoxin) is given as soon as possible after botulism has been diagnosed. It is most likely to help if given within 72 hours of when symptoms begin. The antitoxin may slow or stop further physical deterioration, so that the body can heal itself over a period of months. However, the antitoxin cannot undo damage already done. Also, some people have a serious allergic (anaphylactic) reaction to the antitoxin, which is derived from horse serum, or develop serum sickness (see box on page 2018). The antitoxin is not recommended for infant botulism, but use of a botulism immune globulin (derived from the blood of people immunized against botulism) in infants is being studied. People may need to be fed through an intravenous tube. Infants may need to be fed through a thin plastic feeding tube (a nasogastric tube) passed through the nose and down the throat.
Some people who recover from botulism feel tired and are short of breath for years afterward. They may need long-term physical therapy.
EATON-LAMBERT SYNDROME
Eaton-Lambert syndrome is an autoimmune disorder that causes weakness.
Eaton-Lambert syndrome is caused by antibodies that interfere with the release of acetylcholine rather than attack acetylcholine receptors (as occurs in myasthenia gravis—see page 818). Eaton-Lambert syndrome usually precedes, occurs with, or develops after certain cancers, especially lung cancer.
Eaton-Lambert syndrome causes muscle weakness, but persistent use of a muscle causes an increase rather than a decrease in strength (as occurs in myasthenia gravis). People also tire easily. The mouth is dry, the eyelid droops, and the upper arms and thighs are painful. Men may have erectile dysfunction.
Symptoms suggest the diagnosis, but electromyography (stimulating muscles, then recording their electrical activity) is needed to confirm the diagnosis.
Treating cancer, if present, sometimes relieves symptoms due to Eaton-Lambert syndrome. Guanidine, a drug that increases the release of acetylcholine, often lessens symptoms but may inhibit the bone marrow’s production of blood cells and impair liver function. Corticosteroids and plasmapheresis (filtering of toxic substances, including abnormal antibodies, from the blood) help some people.
Plexus Disorders
The networks of interwoven nerve fibers from different spinal nerves (plexuses) may be damaged by injury, tumors, collections of blood, or autoimmune reactions.
 Pain, weakness, and loss of sensation occur in all or part of an arm or a leg.
Pain, weakness, and loss of sensation occur in all or part of an arm or a leg.
 Electromyography and evoked responses help doctors locate the damage, and magnetic resonance imaging helps locate the damage and identify the cause.
Electromyography and evoked responses help doctors locate the damage, and magnetic resonance imaging helps locate the damage and identify the cause.
 Sometimes treating the disorder causing the problem improves nerve function.
Sometimes treating the disorder causing the problem improves nerve function.
A plexus is like an electrical junction box, which distributes wires to different parts of a house. In a plexus, nerve fibers from different spinal nerves (which connect the spinal cord to the rest of the body) are sorted. The fibers are recombined so that all fibers going to a specific body part are put together in one nerve. Damage to nerves in the major plexuses causes problems in the arms or legs that these nerves supply. The major plexuses are the brachial plexus, which is located in the neck and shoulders and distributes nerves throughout the arms, and the lumbosacral plexus, which is located in the lower back and pelvis and distributes nerves to the pelvis and legs.
Causes
The most common causes of damage are physical injury and cancer. An accident that pulls the arm or severely bends the arm at the shoulder may damage the brachial plexus (located near the shoulder). In newborns, the brachial plexus can be damaged during birth if the delivery requires pulling or other maneuvers. A fall can injure the lumbosacral plexus (located near the hip).
A cancer growing in the upper part of the lung can invade and destroy the brachial plexus. Or a cancer of the intestine, bladder, or prostate can invade the lumbosacral plexus. Other masses, such as a noncancerous (benign) tumor, an abscess, or a collection of blood (hematoma), may cause plexus disorders by putting pressure on a plexus.
Radiation therapy for breast cancer or diabetes, which can damage nerves throughout the body, may also damage nerves in a plexus.
Acute brachial neuritis (sudden malfunction of the brachial plexus) is probably caused by an autoimmune reaction—when the body produces antibodies that attack its own tissues. This disorder occurs primarily in men. It typically occurs in young adults but can occur at any age.
Symptoms
Malfunction of the brachial plexus causes pain, weakness, and loss of sensation in an arm. All or part of the arm (such as the forearm or biceps) may be affected. If the cause is an injury, recovery tends to occur slowly, over several months, although some severe injuries cause permanent weakness.
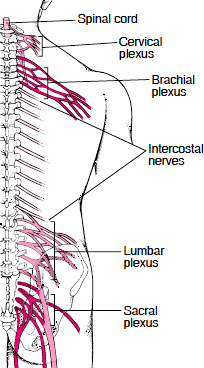
Nerve Junction Boxes: The Plexuses
Much like the electrical junction box in a house, a nerve plexus is a network of interwoven nerves. Nerve fibers from different spinal nerves are sorted and recombined in plexuses, so that all fibers going to a specific body part are put together in one nerve. Four nerve plexuses are located in the trunk of the body:
 The cervical plexus provides nerve connections to the head, neck, and shoulder.
The cervical plexus provides nerve connections to the head, neck, and shoulder.
 The brachial plexus provides connections to the chest, shoulders, upper arms, forearms, and hands.
The brachial plexus provides connections to the chest, shoulders, upper arms, forearms, and hands.
 The lumbar plexus provides connections to the back, abdomen, groin, thighs, knees, and calves.
The lumbar plexus provides connections to the back, abdomen, groin, thighs, knees, and calves.
 The sacral plexus provides connections to the pelvis, buttocks, genitals, thighs, calves, and feet.
The sacral plexus provides connections to the pelvis, buttocks, genitals, thighs, calves, and feet.
Because the lumbar and sacral plexuses are interconnected, they are sometimes referred to as the lumbosacral plexus. The spinal nerves in the chest do not join a plexus. They are the intercostal nerves, which are located between the ribs.
Acute brachial neuritis causes severe pain in the upper arms and shoulders. Usually, the arm becomes weak and reflexes are impaired as the pain resolves. Weakness develops within 3 to 10 days. Then people typically regain their strength over the next few months.
Malfunction of the lumbosacral plexus causes pain in the lower back and leg as well as weakness and loss of sensation in all or part of a leg (such as the foot or calf). Recovery depends on the cause.
Diagnosis
Doctors suspect that a plexus is involved when symptoms are located in a part of the body supplied by a specific plexus. The location of the symptoms indicates which plexus is affected.
Electromyography and nerve conduction studies can also help locate the damage (see page 636). Magnetic resonance imaging (MRI) can help deter-
mine whether a cancer, another mass, or an injury is causing the plexus disorder.
Treatment
Treatment depends on the cause. Cancer near the plexus may be treated with radiation therapy, chemotherapy, or both. Occasionally, a cancer or another mass that is damaging the plexus must be removed surgically.
If diabetes is the cause, controlling blood sugar levels can help.
Doctors sometimes prescribe corticosteroids for acute brachial neuritis and other plexus disorders thought to be caused by an autoimmune reaction, but these drugs have no proven benefit. When an injury is the cause, time for healing may be all that is needed, but sometimes surgery is required.
Thoracic Outlet Syndromes
Thoracic outlet syndromes are a group of disorders caused by pressure on nerves as they pass between the neck and chest. These disorders cause pain and pins-and-needles sensations (paresthesias) in the hand, shoulder, and arm.
 Nerves and blood vessels may be squeezed as they go through the tight passageway from the neck to the chest.
Nerves and blood vessels may be squeezed as they go through the tight passageway from the neck to the chest.
 Pain and a pins-and-needles sensation may begin in the neck and shoulder, then extend down the arm.
Pain and a pins-and-needles sensation may begin in the neck and shoulder, then extend down the arm.
 Various diagnostic tests are done to look for possible causes, but no test can confirm the diagnosis.
Various diagnostic tests are done to look for possible causes, but no test can confirm the diagnosis.
 Physical therapy and exercise usually help relieve symptoms.
Physical therapy and exercise usually help relieve symptoms.
The thoracic outlet is the passageway between the neck and the chest for the esophagus, major blood vessels, trachea, and many nerves. Because this passageway is very crowded, blood vessels or nerves to the arm may be squeezed between a rib and the overlying muscle, resulting in problems. Nonetheless, the exact cause of thoracic outlet disorders is often unclear. Very rarely, the cause is a clear-cut anatomic abnormality, such as an extra little rib in the neck (cervical rib) that puts pressure on an artery or a blockage of one of the subclavian arteries. (The subclavian arteries are located under the collarbone and carry blood to the arms.)
Thoracic outlet syndromes are more common among women and usually develop between age 35 and 55.
Symptoms
Pain and pins-and-needles sensations usually begin in the neck or shoulder, then spread along the inner surface of the arm into the hand and sometimes down the side of the torso.
If pressure is put on one of the subclavian arteries, the hand, arm, and shoulder on the affected side may swell, or the overlying skin may look bluish because the oxygen supply is inadequate (a condition called cyanosis). Sometimes the pressure is severe enough to cause Raynaud’s syndrome, in which the fingers become pale or blue and often numb when exposed to cold. In severe cases, the pressure may cause gangrene in the fingers.
Diagnosis
Doctors base the diagnosis on symptoms and results of a physical examination and several diagnostic tests. Nerve conduction studies and electromyography (see page 636) may detect abnormalities characteristic of thoracic outlet syndrome. Through a stethoscope placed on the collar bone or near the top of the armpit, doctors may hear sounds indicating abnormal blood flow (bruits) in a compressed artery. Angiography of the arteries in the arm (brachial arteries) may be done to detect abnormal blood flow. In this test, x-rays are taken after a dye that is visible on x-rays (radiopaque dye) is injected into the bloodstream. Magnetic resonance imaging (MRI) may be done to look for anatomic abnormalities. However, none of these tests can definitively confirm or rule out the diagnosis of thoracic outlet syndrome.
Treatment
For most people with symptoms of thoracic outlet syndrome, physical therapy and exercise result in improvement. Nonsteroidal anti-inflammatory drugs (NSAIDs) and antidepressants given in low doses may also help.
Surgery may be needed if an anatomic abnormality or blockage of the subclavian artery is confirmed or if symptoms continue to progress. However, because a definitive diagnosis is difficult to make and because symptoms often persist after surgery, most doctors try to avoid surgery.
Mononeuropathy
Mononeuropathy is damage to a single peripheral nerve.
 Pressure on a nerve for a long time can damage it.
Pressure on a nerve for a long time can damage it.
 The affected area may tingle, feel prickly, or be numb, and the affected muscle may be weak.
The affected area may tingle, feel prickly, or be numb, and the affected muscle may be weak.
 Usually, the diagnosis is based on symptoms and results of a physical examination.
Usually, the diagnosis is based on symptoms and results of a physical examination.
 Modifying or stopping the activity that caused the problem and taking pain relievers usually help, but sometimes physical therapy or surgery is needed.
Modifying or stopping the activity that caused the problem and taking pain relievers usually help, but sometimes physical therapy or surgery is needed.
Causes
Physical injury is the most common cause of a mononeuropathy. Injury is commonly caused by the following:
 Prolonged pressure on a nerve that runs close to the surface of the body near a prominent bone, such as a nerve in an elbow, a shoulder, a wrist, or a knee (as may occur during a long, sound sleep, especially in alcoholics)
Prolonged pressure on a nerve that runs close to the surface of the body near a prominent bone, such as a nerve in an elbow, a shoulder, a wrist, or a knee (as may occur during a long, sound sleep, especially in alcoholics)
 Pressure from a misfitting cast or from crutches that fit poorly or that are used incorrectly
Pressure from a misfitting cast or from crutches that fit poorly or that are used incorrectly
 Pressure from staying in a cramped position for a long time, as when gardening or when playing cards with the elbows resting on a table
Pressure from staying in a cramped position for a long time, as when gardening or when playing cards with the elbows resting on a table
Injury may result from pressure that occurs when people cannot move for long periods, as when they are under anesthesia for surgery, are confined to bed (particularly older people), or are paralyzed. Less commonly, injury results from the following:
 Accidents
Accidents
 Prolonged exposure to cold or heat
Prolonged exposure to cold or heat
 Radiation therapy for cancer
Radiation therapy for cancer
 Repeated injuries, such as those due to tight gripping of small tools or to excessive vibration from an air hammer
Repeated injuries, such as those due to tight gripping of small tools or to excessive vibration from an air hammer
 Infections, such as leprosy or Lyme disease
Infections, such as leprosy or Lyme disease
 A collection of blood (hematoma)
A collection of blood (hematoma)
 Cancer, which may directly invade a nerve
Cancer, which may directly invade a nerve
 Some toxic substances and some drugs
Some toxic substances and some drugs
If the pressure on the nerve is mild, people may feel only pins-and needles-sensations without any weakness. For example, people may hit their elbow (funny bone), or a foot may fall asleep. These episodes can be considered temporary mononeuropathies.
Nerves that run close to the body’s surface near a bone are more vulnerable to injury. Examples are the median nerve in the wrist (resulting in carpal tunnel syndrome—see page 601), the ulnar nerve in the elbow, the radial nerve in the upper arm, and the peroneal nerve near the knee.
 Did You Know…
Did You Know…
Using crutches that are the wrong height can damage a nerve and make the hand and wrist weak.
Symptoms
Abnormal sensations, including pins-and-needles or loss of sensation, occur in the area supplied by the injured nerve. Pain and weakness may or may not be present.
Carpal Tunnel Syndrome: The median nerve passes through a narrow passageway at the wrist. Pressure on this nerve causes pain and abnormal sensations in the fingers, the palm side of the hand and wrist, and sometimes the arm and shoulder (see page 601).
Ulnar Nerve Palsy: The ulnar nerve passes close to the surface of the skin at the elbow. The nerve is easily damaged by repeatedly leaning on the elbow or by hitting the elbow (funny bone). Sometimes the nerve is damaged by an abnormal bone growth in the area. Usually, people feel a tingling, pins-and-needles sensation. Ulnar nerve palsy results from more severe injury and makes the muscles in the hand weak. Severe, chronic ulnar nerve palsy can cause muscles to waste away (atrophy), resulting in a clawhand deformity (the fingers are frozen in a bent position because the muscles become tight). Avoiding pressure on the elbow is recommended.
Radial Nerve Palsy: The radial nerve passes along the underside of the bone in the upper arm. Prolonged pressure on this nerve results in radial nerve palsy. This disorder is sometimes called Saturday night palsy because it occurs in people who drink heavily (often during weekends) and then sleep soundly with an arm draped over the back of a chair or under their partner’s head. If crutches fit incorrectly and press on the inside of the arm near the armpit, they can cause this disorder. The nerve damage weakens the wrist and fingers so that the wrist may flop into a bent position with the fingers curved (a condition called wristdrop). Occasionally, the back of the hand may lose feeling. Usually, radial nerve palsy resolves once the pressure is relieved.
When the Foot’s Asleep
A sleeping foot can be considered a temporary neuropathy. The foot falls asleep when pressure is put on the nerve (usually the peroneal nerve but sometimes the sciatic nerve) supplying it. Pressure interferes with the blood supply to the nerve, making the nerve give off abnormal signals (a pins-and-needles sensation), called a paresthesia. Relieving the pressure, for example, by moving around, restores the nerve’s blood supply. As a result, the nerve can function normally, and the pins-and-needles sensation stops.
Peroneal Nerve Palsy: The peroneal nerve passes close to the surface of the skin on the outer, lower part of the knee. Pressure on this nerve results in peroneal nerve palsy. This disorder weakens the muscles that lift the foot, so that the foot cannot be flexed upward (a condition called footdrop). It is most common among thin people who are confined to bed, people who are incorrectly strapped into a wheelchair, and people (especially thin people) who habitually cross their legs for long periods of time. Avoiding pressure on the nerve—for example, by not crossing the legs—usually relieves the symptoms.
Diagnosis
Usually, doctors can diagnose mononeuropathies based on symptoms and results of a physical examination, including feeling (palpating) the affected muscle when it is moving to check for weakness. Sometimes electromyography and nerve conduction studies are done to rule out other possible causes, to determine where the nerve is damaged, or to determine how severe the disorder is.
Treatment
If the cause is a disorder, it is treated. For example, a tumor may be surgically removed.
Usually, when temporary pressure is the cause, the following can help relieve symptoms:
 Resting
Resting
 Not putting pressure on the nerve
Not putting pressure on the nerve
 Placing heat on the affected area
Placing heat on the affected area
 Taking nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, to reduce inflammation
Taking nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, to reduce inflammation
Some people with carpal tunnel syndrome benefit from corticosteroid injections.
Braces or splints are often used to prevent shortening of muscles (contractures) until the symptoms resolve. Surgery may be done to relieve pressure on a nerve if the disorder progresses despite other treatments.
For severe, chronic ulnar nerve palsy, physical therapy helps prevent tightening of muscles. Surgical repair is often unsuccessful.
Multiple Mononeuropathy
Multiple mononeuropathy (mononeuritis multiplex) is the simultaneous malfunction of two or more peripheral nerves in separate areas of the body. It causes abnormal sensations and weakness.
Multiple mononeuropathy typically affects only a few nerves, often in different areas of the body. In contrast, polyneuropathy affects many nerves, usually in about the same areas on both sides of the body. However, if multiple mononeuropathy involves many nerves, it may be difficult to distinguish from polyneuropathy.
Several disorders can cause multiple mononeuropathy, and each disorder produces characteristic symptoms. Diabetes is probably the most common cause, although diabetes more commonly causes polyneuropathy. Other common causes of multiple mononeuropathy include polyarteritis nodosa, lupus (systemic lupus erythematosus), Sjögren’s syndrome, rheumatoid arthritis, sarcoidosis, amyloidosis, and infections (such as Lyme disease and HIV infection). Multiple mononeuropathy may result from direct invasion of the nerve by bacteria, as occurs in leprosy. A disorder may affect the nerves all at once or affect them progressively, a few at a time.
People have pain, weakness, abnormal sensations, or a combination of symptoms in the areas supplied by the affected nerves. Symptoms often begin on one side of the body. When diabetes is the cause, muscles of the eyes and thighs are often affected.
Doctors base the diagnosis on symptoms and results of a physical examination, but electromyography and nerve conduction tests are usually done to confirm the diagnosis.
Treatment depends on the cause.
Polyneuropathy
Polyneuropathy is the simultaneous malfunction of many peripheral nerves throughout the body.
 Infections, toxins, drugs, cancers, nutritional deficiencies, and disorders can cause many peripheral nerves to malfunction.
Infections, toxins, drugs, cancers, nutritional deficiencies, and disorders can cause many peripheral nerves to malfunction.
 Sensation, strength, or both may be impaired, often in the feet or hands before the arms, legs, or trunk.
Sensation, strength, or both may be impaired, often in the feet or hands before the arms, legs, or trunk.
 Doctors base the diagnosis on results of electromyography, nerve conduction studies, and blood and urine tests.
Doctors base the diagnosis on results of electromyography, nerve conduction studies, and blood and urine tests.
 If treating the underlying disorder does not relieve symptoms, physical therapy, drugs, and other measures may help.
If treating the underlying disorder does not relieve symptoms, physical therapy, drugs, and other measures may help.
Polyneuropathy may be acute (beginning suddenly) or chronic (developing gradually, often over months or years).
Causes
Acute polyneuropathy has many causes:
 Infections involving a toxin produced by bacteria, as occurs in diphtheria
Infections involving a toxin produced by bacteria, as occurs in diphtheria
 An autoimmune reaction (when the body attacks its own tissues), as occurs in Guillain-Barré syndrome
An autoimmune reaction (when the body attacks its own tissues), as occurs in Guillain-Barré syndrome
 Toxic substances, including heavy metals such as lead and mercury
Toxic substances, including heavy metals such as lead and mercury
 Drugs, including the anticonvulsant phenytoin, some antibiotics (such as chloramphenicol, nitrofurantoin, and sulfonamides), some chemotherapy drugs (such as vinblastine and vincristine), and some sedatives (such as barbital and hexobarbital)
Drugs, including the anticonvulsant phenytoin, some antibiotics (such as chloramphenicol, nitrofurantoin, and sulfonamides), some chemotherapy drugs (such as vinblastine and vincristine), and some sedatives (such as barbital and hexobarbital)
 Cancer, such as multiple myeloma, which damages nerves by directly invading or putting pressure on them or by triggering an autoimmune reaction
Cancer, such as multiple myeloma, which damages nerves by directly invading or putting pressure on them or by triggering an autoimmune reaction
The cause of chronic polyneuropathy is often unknown. Causes include the following:
 Diabetes
Diabetes
 Excessive use of alcohol
Excessive use of alcohol
 Nutritional deficiencies (such as thiamin deficiency), an uncommon cause in the United States, except among alcoholics who are malnourished
Nutritional deficiencies (such as thiamin deficiency), an uncommon cause in the United States, except among alcoholics who are malnourished
 Anemia due to vitamin B12 deficiency (pernicious anemia)
Anemia due to vitamin B12 deficiency (pernicious anemia)
 An underactive thyroid gland (hypothyroidism)
An underactive thyroid gland (hypothyroidism)
 Liver failure
Liver failure
 Kidney failure
Kidney failure
 Certain cancers, such as lung cancer
Certain cancers, such as lung cancer
 Vitamin B6 (pyridoxine) taken in excessive amounts
Vitamin B6 (pyridoxine) taken in excessive amounts
The most common form of chronic polyneuropathy usually results from poor control of blood sugar levels in people with diabetes (see page 1007) but may result from excessive use of alcohol.
Diabetic neuropathy refers to the several forms of polyneuropathy that diabetes can cause. (Diabetes can also cause mononeuropathy or multiple mononeuropathy, which leads to weakness, typically of the eye or thigh muscles.)
In some people, the cause is hereditary.
Depending on the cause, polyneuropathies may affect motor nerves (which control muscle movement), sensory (which transmit sensory information), cranial nerves (which connect the head, face, eyes, nose, muscles, and ears to the brain), or a combination.
Symptoms
Acute polyneuropathy (for example, as occurs in Guillain-Barré syndrome) begins suddenly in both legs and progresses rapidly upward to the arms. Symptoms include weakness and a pins-and-needles sensation or loss of sensation. The muscles that control breathing may be affected, resulting in respiratory failure.
In the most common form of chronic polyneuropathy, only sensation is affected. Usually, the feet are affected first, but sometimes the hands are. A pins-and-needles sensation, numbness, burning pain, and loss of vibration sense and position sense (knowing where the arms and legs are) are prominent symptoms. Because position sense is lost, walking and even standing become unsteady. Consequently, muscles may not be used. Eventually, they may weaken and waste away.
Diabetic neuropathy commonly causes painful tingling or burning sensations in the hands and feet—a condition called distal polyneuropathy. Pain is often worse at night and may be aggravated by touch or by a change in temperature. People may lose the senses of temperature and pain, so they often burn themselves and develop open sores caused by prolonged pressure or other injuries. Without pain as a warning of too much stress, joints are susceptible to injuries. This type of injury is called Charcot’s joints (see page 572).
Polyneuropathy often affects the nerves of the autonomic nervous system, which controls involuntary functions in the body (such as blood pressure, heart rate, digestion, salivation, and urination). Typical symptoms are constipation, loss of bowel or bladder control (leading to fecal or urinary incontinence), sexual dysfunction, and fluctuating blood pressure—most notably a sudden fall in blood pressure when a person stands up (orthostatic hypotension). The skin may become pale and dry, and sweating may be reduced.
People who have a hereditary form may have hammer toes, high arches, and a curved spine (scoliosis). Abnormalities in sensation and muscle weakness may be mild. Affected people may not notice these symptoms or may consider them unimportant.
How completely people recover depends on the cause of polyneuropathy.
Diagnosis
Doctors usually recognize polyneuropathy by the symptoms. A physical examination and tests such as electromyography and nerve conduction studies (see page 636) can provide additional information about absent or reduced sensation in the feet.
After polyneuropathy is diagnosed, its cause, which may be treatable, must be identified. Doctors ask whether other symptoms are present and how quickly the symptoms developed. Blood and urine tests may detect a disorder that is causing polyneuropathy—for example, diabetes, kidney failure, or an underactive thyroid gland. Infrequently, a nerve biopsy is necessary.
Sometimes polyneuropathy affecting the hands and feet is the first indication that people have diabetes. Sometimes, when extensive testing detects no obvious cause, the cause is an inherited neuropathy that affects other family members so mildly that the disorder was never suspected.
Treatment
Specific treatment depends on the cause, as for the following:
 Excessive amounts of vitamin B6: If the vitamin is stopped, polyneuropathy may resolve.
Excessive amounts of vitamin B6: If the vitamin is stopped, polyneuropathy may resolve.
 Diabetes: Careful control of blood sugar levels may slow progression of the disorder and occasionally relieves symptoms. Transplantation of cells that produce insulin (islet cells—see page 1133), located in the pancreas, sometimes results in a cure.
Diabetes: Careful control of blood sugar levels may slow progression of the disorder and occasionally relieves symptoms. Transplantation of cells that produce insulin (islet cells—see page 1133), located in the pancreas, sometimes results in a cure.
 Multiple myeloma or liver or kidney failure: Treatment of these disorders may result in slow recovery.
Multiple myeloma or liver or kidney failure: Treatment of these disorders may result in slow recovery.
 Cancer: Surgically removing the cancer may be necessary to relieve pressure on the nerve.
Cancer: Surgically removing the cancer may be necessary to relieve pressure on the nerve.
 An underactive thyroid gland: Thyroid hormone is given.
An underactive thyroid gland: Thyroid hormone is given.
 Autoimmune disorders: Treatments include plasmapheresis (filtering of toxic substances, including abnormal antibodies, from the blood), immune globulin given intravenously, corticosteroids, and drugs that suppress the immune system (immunosuppressants).
Autoimmune disorders: Treatments include plasmapheresis (filtering of toxic substances, including abnormal antibodies, from the blood), immune globulin given intravenously, corticosteroids, and drugs that suppress the immune system (immunosuppressants).
If the cause cannot be corrected, treatment focuses on relieving pain and problems related to muscle weakness. Physical therapy sometimes reduces muscle stiffness and can prevent shortening of muscles (contractures). Physical and occupational therapists can recommend useful assistive devices. Some drugs that are usually not considered pain relievers can lessen pain due to nerve damage. They include the antidepressant amitriptyline, the anticonvulsant gabapentin, and mexiletine (used to treat abnormal heart rhythms). Lidocaine, an anesthetic applied as a lotion, an ointment, or a skin patch, may also help.
GUILLAIN-BARRÉ SYNDROME
Guillain-Barré syndrome (acute inflammatory demyelinating polyneuropathy) is a form of polyneuropathy that causes one episode of increasing muscle weakness. The episode lasts 8 weeks or less.
 An autoimmune reaction may damage the myelin sheath around nerves.
An autoimmune reaction may damage the myelin sheath around nerves.
 Usually, weakness begins in both legs and moves up the body.
Usually, weakness begins in both legs and moves up the body.
 Electromyography and nerve conduction studies can help confirm the diagnosis.
Electromyography and nerve conduction studies can help confirm the diagnosis.
 Plasmapheresis or immune globulin given intravenously may speed recovery.
Plasmapheresis or immune globulin given intravenously may speed recovery.
The presumed cause is an autoimmune reaction: The body’s immune system attacks the myelin sheath, which surrounds the axon of many nerves and enables nerve impulses to travel quickly. In about 80% of people with this syndrome, symptoms begin about 5 days to 3 weeks after a mild infection (such as a Campylobacter infection, mononucleosis, or another viral infection), surgery, or an immunization.
Symptoms
Symptoms usually begin in both legs, then progress upward to the arms. Occasionally, symptoms begin in the arms or head and progress downward. Symptoms include weakness and a pins-and-needles sensation or loss of sensation. Weakness is more prominent than abnormal sensation. Reflexes are decreased or absent. In 90% of people who have Guillain-Barré syndrome, weakness is most severe within 3 weeks. In 5 to 10%, the muscles that control breathing become so weak that a ventilator is needed. Because the facial and swallowing muscles become weak, a few people need to be fed intravenously or through a tube placed directly through the abdominal wall into the stomach (gastrostomy tube).
If the disorder is very severe, internal functions controlled by the autonomic nervous system may be impaired. For example, blood pressure may fluctuate widely, heart rhythm may become abnormal, and severe constipation may develop.
In a variant called Miller-Fisher syndrome, only a few symptoms develop: Eye movements become paralyzed, walking becomes difficult, and normal reflexes disappear.
Diagnosis
Doctors suspect the diagnosis based on the pattern of symptoms. Tests are done to confirm the diagnosis. People are usually admitted to the hospital to have the tests because the syndrome can worsen rapidly and impair the muscles involved in breathing.
Analysis of cerebrospinal fluid obtained by a spinal tap (lumbar puncture—see art on page 635), electromyography, nerve conduction studies, and blood tests can help doctors exclude other possible causes of severe weakness, such as transverse myelitis and spinal cord injuries. A combination of high protein levels and no inflammatory cells in the cerebrospinal fluid and characteristic results from electromyography strongly suggest Guillain-Barré syndrome.
Prognosis
Damage stops progressing within 8 weeks. Without treatment, most people improve slowly over several months. However, with early treatment, people can improve very quickly—in days or weeks. About 30% of adults and even more children with the disorder have residual weakness 3 years after the syndrome began. On average, less than 2% of people die.
After improving initially, 3 to 10% of people develop a disorder called chronic inflammatory demyelinating polyneuropathy (see page 829).
Treatment
Guillain-Barré syndrome can worsen rapidly and is a medical emergency. People who develop this syndrome should be hospitalized immediately. Establishing the diagnosis is crucial because the sooner appropriate treatment is started, the better the chance of a good outcome.
In the hospital, people are closely monitored so that breathing can be assisted with a ventilator if necessary. Nurses take precautions to prevent pressure sores and injuries by providing soft mattresses and by turning the people with severe weakness every 2 hours. If weakness is less severe, physical therapy is started to help preserve joint and muscle function. Heat therapy may be used first to relieve pain and thus make physical therapy more comfortable.
Plasmapheresis (filtering of toxic substances, including antibodies to the myelin sheath) from the blood—see box on page 1030) or immune globulin given intravenously is the treatment of choice. These treatments are relatively safe, shorten the hospital stay, speed recover, and reduce the risk of death and permanent disability.
Corticosteroids do not help and may worsen the syndrome.
CHRONIC INFLAMMATORY DEMYELINATING POLYNEUROPATHY
Chronic inflammatory demyelinating polyneuropathy (chronic acquired demyelinating polyneuropathy, or chronic relapsing polyneuropathy) is a form of polyneuropathy that, like Guillain-Barré syndrome, causes increasing muscle weakness, but the weakness lasts longer than 8 weeks.
Chronic inflammatory demyelinating polyneuropathy develops in 3 to 10% of people with Guillain-Barré syndrome.
Weakness and abnormal sensations (numbness and pins-and-needles) last longer than 8 weeks. Weakness can worsen continually or come and go. Reflexes are decreased or absent. In most people with this disorder, blood pressure fluctuates less, abnormal heart rhythms occur less often, and other internal functions are less impaired than in people with Guillain-Barré syndrome. Also, weakness may be more irregular, affecting the two sides of the body differently, and weakness may progress more slowly.
Diagnosis and Treatment
Doctors suspect the diagnosis based on symptoms. Electromyography, nerve conduction studies, and a spinal tap to obtain cerebrospinal fluid are done to confirm the diagnosis. Rarely, a biopsy of the nerve is needed.
Corticosteroids such as prednisone can relieve symptoms. Immunosuppressants such as azathioprine may also be used. However, if chronic inflammatory demyelinating polyneuropathy is severe or progresses rapidly, plasmapheresis or immune globulin given intravenously may be preferred to corticosteroids. People may need treatment for months or years.
Hereditary Neuropathies
Hereditary neuropathies affect the peripheral nerves, causing subtle symptoms that worsen gradually.
Hereditary neuropathies may affect only motor nerves (motor neuropathies), only sensory nerves (sensory neuropathies), or both sensory and motor nerves (sensorimotor neuropathies). Some hereditary neuropathies are relatively common but often are not recognized. Hereditary sensory neuropathies are especially rare. These neuropathies tend to impair the ability to sense pain and temperature.
The genes responsible for many of these neuropathies have been identified. They include some forms of Charcot-Marie-Tooth disease, Refsum’s disease (see box on page 1839), porphyria (see page 975).
Fabry’s disease (see page 1840), and hereditary neuropathy with liability to pressure palsies (see page 830).
CHARCOT-MARIE-TOOTH DISEASE
Charcot-Marie-Tooth disease (peroneal muscular atrophy) is a hereditary neuropathy in which the muscles of the lower legs become weak and waste away (atrophy).
Charcot-Marie-Tooth disease is the most common hereditary neuropathy, affecting 1 of 2,500 people. It is a sensorimotor neuropathy. That is, it affects motor nerves (which stimulate muscle action) and sensory nerves (which carry sensory information).
There are 2 main types and several subtypes of the disease. In some types, axons (the part of the nerve that sends messages) die because the myelin sheath surrounding them is damaged or destroyed (demyelinated). In other types, axons die even though the sheath is not damaged. Most types of the disease are inherited as an autosomal (not sex-linked) dominant trait. That is, only one gene from one parent is required for the disease to develop.
Symptoms
Symptoms vary by type of the disease.
Type 1: Symptoms begin in middle childhood. Weakness begins in the lower legs. It causes an inability to flex the foot (footdrop) and wasting away of the calf muscles (stork leg deformity). Later, hand muscles begin to waste away. The hands and feet become unable to sense vibration, pain, and temperature, and this loss of sensation gradually moves up the limbs.
In milder subtypes of type 1, high arches and hammer toes may be the only symptoms. In one subtype, males have severe symptoms, and females have mild symptoms or may be unaffected.
The disease progresses slowly and does not affect life span.
Type 2: The neuropathy progresses more slowly and causes somewhat similar symptoms, often beginning during the teenage years.
Diagnosis and Treatment
The distribution of weakness, the age at which the disease began, the family history, the presence of foot deformities (high arches and hammer toes), and the results of nerve conduction studies help doctors identify the different types of Charcot-Marie-Tooth disease and distinguish them from other causes of neuropathy. Genetic testing and counseling for Charcot-Marie-Tooth disease is available.
No treatment can stop the progression of the disease. Wearing braces helps correct footdrop, and sometimes orthopedic surgery is needed to stabilize the foot. Physical therapy (to strengthen muscles) and occupational therapy may be helpful.
HEREDITARY NEUROPATHY WITH LIABILITY TO PRESSURE PALSIES
Hereditary neuropathy with liability to pressure palsies is a hereditary disorder in which nerves become very sensitive to pressure, injury, and use.
In this neuropathy, nerves are susceptible to damage resulting from relatively slight pressure or injury or from repetitive use. Usually, this neuropathy starts during adolescence or young adulthood, but it may start at any age. It affects both sexes equally. It is inherited as an autosomal (not sex-linked) dominant trait (see page 12).
Peroneal nerve palsy with footdrop, ulnar nerve palsy, and carpal tunnel syndrome commonly develop. Numbness or weakness occurs periodically in the affected area. Symptoms vary from unnoticeable and mild to severe and incapacitating. Episodes may last several minutes to months.
Doctors may have difficulty diagnosing this neuropathy because the symptoms come and go. Electromyography and genetic testing help establish the diagnosis. Rarely, biopsy of a nerve is required.
Activities that cause symptoms should be avoided or modified. Supports, such as wrist splints and elbow pads, can reduce pressure, prevent reinjury, and allow the nerve to repair itself over time. Rarely, surgery is needed.
About half of the people who have symptoms recover completely within days to months. In people who do not recover completely, symptoms are rarely severe.
Spinal Muscular Atrophies
Spinal muscular atrophies are hereditary disorders in which nerve cells in the spinal cord and brain stem degenerate, causing progressive muscle weakness and wasting.
 These disorders are inherited.
These disorders are inherited.
 The four main types cause various degrees of muscle weakness and wasting.
The four main types cause various degrees of muscle weakness and wasting.
 Depending on the type, people may be confined to a wheelchair, and life span may be shortened.
Depending on the type, people may be confined to a wheelchair, and life span may be shortened.
 The diagnosis, suggested by symptoms, is based on family history, tests of muscle and nerve function, and sometimes blood tests to detect the defective gene.
The diagnosis, suggested by symptoms, is based on family history, tests of muscle and nerve function, and sometimes blood tests to detect the defective gene.
 There is no cure, but physical therapy and use of braces can help.
There is no cure, but physical therapy and use of braces can help.
The disorders are usually inherited as a recessive autosomal (not sex-linked) trait. That is, two genes are required, one from each parent (see page 12). These disorders may also affect the central nervous system. There are four main types of spinal muscular atrophy.
Symptoms
Symptoms of the four main types first appear during infancy and childhood.
In acute (type I) spinal muscular atrophy (Werdnig-Hoffmann disease), muscle weakness is usually apparent at or within a few days of birth. It is virtually always apparent by age 6 months. Infants lack muscle tone and reflexes and have difficulty sucking, swallowing, and eventually breathing. Death occurs in 95% of children within the first year and in all by age 4 years, usually due to respiratory failure.
In children with intermediate (type II) spinal muscular atrophy, weakness typically develops between age 6 and 15 months. Fewer than one fourth of them learn to sit. None can crawl or walk. Muscles are weak, and swallowing may be difficult. Most children are confined to a wheelchair by age 2 to 3 years. The disorder is often fatal in early life, usually because of respiratory problems. But some children survive with permanent weakness that does not continue to worsen. These children often have severe curvature of the spine (scoliosis).
Chronic (type III) spinal muscular atrophy (Wohlfart-Kugelberg-Welander disease) begins in children between age 15 months and 19 years and worsens slowly. Consequently, people with this disorder usually live longer than those with type I or II spinal muscular atrophy. Some of them have a normal life span. Weakness and wasting of muscles begin in the hips and thighs and later spread to the arms, feet, and hands.
Type IV spinal muscular atrophy first appears during adulthood, usually between age 30 and 60 years. Muscles, mainly in the hips, thighs, and shoulders, become weak and waste away.
Diagnosis and Treatment
Doctors usually test for these rare disorders when unexplained weakness and muscle wasting occur in young children. Because these disorders are inherited, a family history may help doctors make the diagnosis. Electromyography and nerve conduction studies (see page 636) help confirm the diagnosis. The specific defective gene has been identified for some of the types and can be detected by blood tests. Occasionally, biopsy of a muscle is done. If there is a family history of one of the disorders, amniocentesis can be done to help determine whether an unborn child has the defective gene.
No specific treatments are available. Physical therapy and wearing braces can sometimes help. Physical and occupational therapists can provide adaptive devices to enable children to feed themselves, write, or use a computer.