CHAPTER 140
Obesity and the Metabolic Syndrome
Obesity
Obesity is the accumulation of excessive body fat.
 Obesity usually results from consuming too many calories and not burning enough calories in physical activity.
Obesity usually results from consuming too many calories and not burning enough calories in physical activity.
 Being obese increases the risk of many disorders, such as diabetes, high blood pressure, heart disease, and certain cancers, and can result in early death.
Being obese increases the risk of many disorders, such as diabetes, high blood pressure, heart disease, and certain cancers, and can result in early death.
 Increasing activity and reducing caloric intake are essential to treating obesity, but some people also need to take drugs.
Increasing activity and reducing caloric intake are essential to treating obesity, but some people also need to take drugs.
 Losing as little of 5 to 10% of body weight can help lessen weight-related problems, such as diabetes, high blood pressure, and high cholesterol levels.
Losing as little of 5 to 10% of body weight can help lessen weight-related problems, such as diabetes, high blood pressure, and high cholesterol levels.
 People who are very obese and who have serious weight-related problems may benefit from weight-loss surgery.
People who are very obese and who have serious weight-related problems may benefit from weight-loss surgery.
The body mass index (BMI) is used to define overweight and obesity. BMI is weight (in kilograms) divided by height (in meters squared). Overweight is usually defined as a BMI of 25 to 29.9. Obesity is defined as a BMI of 30 or higher. Obesity is considered to be severe if BMI is 40 or higher.
Obesity has become increasingly common throughout the world. In the United States, obesity has increased dramatically: 34% of adults are obese, and over 17% of children and adolescents are overweight or obese. Obesity is much easier to prevent than treat. Once people gain excess weight, the body resists losing weight. For example, when people diet or reduce the number of calories they consume, the body compensates by increasing appetite and reducing the number of calories burned during rest.
Causes
Obesity can result from certain disorders, but the increase in obesity results largely from environmental changes that have increased the availability of high-calorie foods and reduced the opportunity for physical activity.
Excess calories are stored in the body as fat. The number of calories needed varies from person to person, depending on age, sex, activity level, and metabolic rate. A person’s resting (basal) metabolic rate—the amount of calories the body burns while at rest—is determined mostly by how much muscle (lean) tissue a person has. The more muscle people have, the higher their metabolic rate.
Physical Inactivity: In developed countries, lack of physical activity contributes greatly to the increase in obesity. Opportunities for physical activity have been engineered away by technological advances, such as elevators, cars, and remote controls. More time is spent doing sedentary activities such as using the computer, watching television, and playing video games. Also, people’s jobs have become more sedentary as office or desk jobs have replaced manual labor. Sedentary people use fewer calories than more active people and thus require fewer calories in the diet. If caloric intake is not reduced accordingly, people gain weight.
Diet: The diet in developed countries is energy dense. That is, it consists of foods that have a large number of calories in a given amount (volume). Foods contain more processed carbohydrates (such as high-fructose corn syrup), more fat, and less fiber. Fats, by nature, are energy dense. A gram of fat has 9 calories, but carbohydrates and proteins have 4 calories per gram.
Convenience foods, such as energy-dense snacks offered at vending machines and fast food restaurants, contribute to the increase in obesity. High-calorie beverages, including soda, juices, coffee drinks, and alcohol, also contribute significantly. For example, a 12-ounce soda or bottle of beer has 150 calories; a 12-ounce coffee beverage or fruit smoothie can have 500 or more calories. An additional 500 calories per day results in a weight gain of 1 pound per week.
Genes: Obesity tends to run in families. However, families share not only genes but also environment, and separating the two influences is difficult. Genes can affect how quickly the body burns calories at rest and during exercise. They can also affect appetite and thus how much food is consumed.
Many genes influence weight, but each gene has only a very small effect. Obesity rarely results when only one gene is abnormal.
Mutations in the following genes are relatively common:
 Gene for the melanocortin 4 receptor: Receptors are structures on the surface of cells that inhibit or produce an action in the cell when certain substances (such as chemical messengers) bind with them. Melanocortin 4 receptors are located mainly in the brain. They help the body regulate its use of energy. A mutation in this gene may account for obesity in 1 to 4% of children.
Gene for the melanocortin 4 receptor: Receptors are structures on the surface of cells that inhibit or produce an action in the cell when certain substances (such as chemical messengers) bind with them. Melanocortin 4 receptors are located mainly in the brain. They help the body regulate its use of energy. A mutation in this gene may account for obesity in 1 to 4% of children.
 Ob gene: This gene controls the production of leptin, a hormone made by fat cells. Leptin travels to the brain and interacts with receptors in the hypothalamus (the part of the brain that helps regulate appetite). The message carried by leptin is to decrease food intake and increase the amount of calories (energy) burned. A mutation in the ob gene prevents leptin production and results in severe obesity in a very small number of children. In these cases, administration of leptin reduces weight to a normal amount.
Ob gene: This gene controls the production of leptin, a hormone made by fat cells. Leptin travels to the brain and interacts with receptors in the hypothalamus (the part of the brain that helps regulate appetite). The message carried by leptin is to decrease food intake and increase the amount of calories (energy) burned. A mutation in the ob gene prevents leptin production and results in severe obesity in a very small number of children. In these cases, administration of leptin reduces weight to a normal amount.
Background: Certain characteristics can increase the risk of becoming overweight or obese. They include the following:
 Certain racial and ethnic backgrounds, such as African Americans, Hispanics, and Pacific Islanders
Certain racial and ethnic backgrounds, such as African Americans, Hispanics, and Pacific Islanders
 A lower socioeconomic group
A lower socioeconomic group
 A lower education level
A lower education level
 Obesity during childhood (see page 1756), which tends to persist into adulthood.
Obesity during childhood (see page 1756), which tends to persist into adulthood.
Pregnancy and Menopause: Gaining weight during pregnancy is normal and necessary. However, pregnancy can be the beginning of weight problems if women do not return to their prepregnancy weight. Having several children close together may com-pound the problem. Breastfeeding can help women return to their prepregnancy weight.
DETERMINING BODY MASS INDEX
After menopause, many women gain weight. This weight gain may result from reduced activity. Hormonal changes may cause fat to be redistributed and accumulate around the waist. Fat in this location increases the risk of health problems (see page 960).
Aging: As people age, body composition may change as muscle tissue decreases. The result is a higher percentage of body fat and a lower basal metabolic rate (because muscle burns more calories).
Lifestyle: Sleep deprivation or lack of sleep (usually considered less than 6 to 8 hours per night) can result in weight gain. Sleeplessness results in hormonal changes that increase appetite and cravings for energy-dense foods.
Stopping smoking usually results in weight gain. Nicotine decreases appetite and increases the metabolic rate. When nicotine is stopped, people may eat more food and their metabolic rate decreases, so that fewer calories are burned. As a result, body weight may increase by 5 to 10%.
Hormones: Hormonal disorders rarely cause obesity. The following are among the most common examples:
 Cushing’s syndrome is caused by excessive levels of cortisol in the body. The syndrome can result from a benign tumor in the pituitary gland (pituitary adenoma) or from a tumor in the adrenal gland or elsewhere, such as in the lungs. Cushing’s syndrome typically causes fat to accumulate in the face, making it look full (called moon face), and behind the neck (called a buffalo hump).
Cushing’s syndrome is caused by excessive levels of cortisol in the body. The syndrome can result from a benign tumor in the pituitary gland (pituitary adenoma) or from a tumor in the adrenal gland or elsewhere, such as in the lungs. Cushing’s syndrome typically causes fat to accumulate in the face, making it look full (called moon face), and behind the neck (called a buffalo hump).
 Polycystic ovary syndrome (see page 1528) affects about 5 to 10% of women. Affected women tend to be overweight or obese. Levels of testosterone and other male hormones are increased, causing fat to accumulate in the waist and abdomen, which is more harmful than the fat that is distributed throughout the body.
Polycystic ovary syndrome (see page 1528) affects about 5 to 10% of women. Affected women tend to be overweight or obese. Levels of testosterone and other male hormones are increased, causing fat to accumulate in the waist and abdomen, which is more harmful than the fat that is distributed throughout the body.
Eating Disorders: Two eating disorders are associated with obesity:
 Binge eating disorder is characterized by binging, by eating large amounts of food during a short amount of time, and usually by a feeling of guilt or remorse or sense of being out of control. Most affected people do not “purge” (for example, by vomiting or using laxatives or diuretics). The disorder is diagnosed when bingeing episodes occur at least twice a week for 6 or more months (see page 879).
Binge eating disorder is characterized by binging, by eating large amounts of food during a short amount of time, and usually by a feeling of guilt or remorse or sense of being out of control. Most affected people do not “purge” (for example, by vomiting or using laxatives or diuretics). The disorder is diagnosed when bingeing episodes occur at least twice a week for 6 or more months (see page 879).
 Night-eating syndrome involves not eating much during the day, consuming a lot of food or calories in the evening, and awakening to eat in the middle of the night.
Night-eating syndrome involves not eating much during the day, consuming a lot of food or calories in the evening, and awakening to eat in the middle of the night.
Drugs: Many drugs used to treat common disorders promote weight gain. These drugs include those used to treat psychiatric disorders including depression, those used to treat seizures, some antihypertensives (such as beta-blockers), corticosteroids, and some drugs used to treat diabetes mellitus.
Symptoms
The most obvious and only true symptom of obesity is a change in overall appearance. However, being obese also increases the risk of many health problems. Virtually every organ system can be affected. These weight-related health problems can cause symptoms, such as shortness of breath, difficulty breathing during activity, snoring, skin abnormalities including acne, and joint and back pain.
Obesity increases the risk of the following:
 High cholesterol levels
High cholesterol levels
 High blood pressure
High blood pressure
 Metabolic syndrome
Metabolic syndrome
 Coronary artery disease
Coronary artery disease
 Heart failure
Heart failure
 Diabetes or a high blood sugar level (insulin resistance or prediabetes)
Diabetes or a high blood sugar level (insulin resistance or prediabetes)
 Cancer of the breast, uterus, ovaries, colon, prostate, kidneys, or pancreas
Cancer of the breast, uterus, ovaries, colon, prostate, kidneys, or pancreas
 Gallstones and other gallbladder disorders
Gallstones and other gallbladder disorders
 A low testosterone level, erectile dysfunction, and reduced fertility in men
A low testosterone level, erectile dysfunction, and reduced fertility in men
 Menstrual disorders, infertility, and increased risk of miscarriage in women
Menstrual disorders, infertility, and increased risk of miscarriage in women
 Skin abnormalities, including acne and facial hair in women
Skin abnormalities, including acne and facial hair in women
 Varicose veins
Varicose veins
 Fatty liver, hepatitis, and cirrhosis
Fatty liver, hepatitis, and cirrhosis
 Blood clots (deep vein thrombosis and pulmonary embolism)
Blood clots (deep vein thrombosis and pulmonary embolism)
 Asthma
Asthma
 Obstructive sleep apnea
Obstructive sleep apnea
 Kidney disorders, including nephrotic syndrome
Kidney disorders, including nephrotic syndrome
 Arthritis, gout, low back pain, and other joint disorders
Arthritis, gout, low back pain, and other joint disorders
 Depression and anxiety
Depression and anxiety
Obesity doubles or triples the risk of early death. The more severe the obesity, the higher the risk. In the United States, 300,000 deaths a year are attributed to obesity.
Diagnosis
Obesity is diagnosed by determining the BMI (see page 952). The BMI does not distinguish between lean and fat tissue. Thus, some people have a high BMI because they have excess muscle (for example, if they are body builders), but they are not considered obese. Conversely, some people have a normal weight but a high percentage of body fat, which is unhealthy. Therefore, body composition, especially percentage of body fat, is also important. Body composition can be measured using dual-energy x-ray absorptiometry (DEXA), which is also used to check for bone loss, or bioelectric impedance, which can be done in a doctor’s office.
Waist circumference is measured. This measurement helps identify and quantify abdominal (visceral) obesity, which is fat that accumulates in the midsection (see page 960). Abdominal obesity is much more harmful than fat that is distributed throughout the body under the skin (subcutaneous fat).
Treatment
The main treatment for obesity is changing lifestyle, which includes changes in diet, increased physical activity, and behavioral modification to help with weight loss and maintenance. Some people may also need to take drugs or to have weight-loss (bariatric) surgery.
Successful weight loss requires motivation and a sense of readiness. People who are most successful have realistic goals and recognize that healthy weight loss can be achieved only with lifelong lifestyle changes rather than a magic bullet or fad diet that cannot be sustained. Seeking the support of health care practitioners such as dieticians or physicians can be beneficial. Programs that require regular contact increase accountability and can increase success rate. Some examples include Overeaters Anonymous (OA), Take Off Pounds Sensibly (TOPS), community-based and work-site programs, and organized commercial programs such as Weight Watchers. Typically, weekly meetings are conducted by counselors and supplemented by instructional and guidance materials.
Dietary Change: Healthy eating for weight loss requires reducing the number of calories consumed and choosing a wide range of foods that provide good nutrition. Reducing the number of calories consumed by 500 to 1,000 calories a day results in weight loss of 1 to 2 pounds per week, which is a healthy rate of weight loss. This approach usually means consuming 1,200 to 1,500 calories a day. Weight can be lost more rapidly with a very low calorie diet, but such diets should be supervised by a doctor. The following changes in diet are recommended:
 Eating 5 or more servings of fruits and vegetables a day
Eating 5 or more servings of fruits and vegetables a day
 Eating lean protein—for example, fish or chicken breast or vegetable protein, such as soy
Eating lean protein—for example, fish or chicken breast or vegetable protein, such as soy
 Switching to no-fat dairy products
Switching to no-fat dairy products
 Eating whole grains
Eating whole grains
 Eliminating high-calorie beverages
Eliminating high-calorie beverages
 Limiting consumption of restaurant and fast food
Limiting consumption of restaurant and fast food
 Switching from harmful fats, such as saturated fat and trans fat, to good fats, such as monoun-saturated fats (found in olive and canola oils) and polyunsaturated fats (in deep-sea fish and vegetable oils) and limiting the amount of fat consumed.
Switching from harmful fats, such as saturated fat and trans fat, to good fats, such as monoun-saturated fats (found in olive and canola oils) and polyunsaturated fats (in deep-sea fish and vegetable oils) and limiting the amount of fat consumed.
Saturated and trans fats not only contribute to weight gain and obesity but can be harmful by leading to abnormal cholesterol levels and an increased risk of coronary artery disease.
Physical Activity: Increasing physical activity is essential to healthy weight loss and weight maintenance. Physical activity includes not only exercise (that is, structured physical activity) but also lifestyle activities, such as taking the stairs instead of the elevator, gardening, and walking instead of driving when possible. Lifestyle activities can burn a considerable number of calories. Also, physical activity helps people maintain weight loss. People who do not exercise while dieting are more likely to regain the weight they lose.
As a general guide, people need to walk at least 150 minutes each week to promote health and to maintain weight. For weight loss, 60 to 90 minutes of physical activity per day is needed. Aerobic exercise, such as jogging, walking briskly (3 to 4 miles an hour), biking, singles tennis, skating, and cross-country skiing, burn more calories than less active exercises (see page 43). For example, vigorous walking burns about 4 calories per minute, so that 1 hour of brisk walking per day burns about 240 calories. Running burns about 6 to 8 calories per minute.
To get the most benefit from exercise, people should do strength training (with weights or another form of resistance) every 48 to 72 hours, about 3 days of the week. Strength training increases the amount of muscle tissue, which increases the metabolic rate, so that the body burns more calories when at rest.
Behavioral Modification: Ultimately, for weight loss to be effective and long-lasting, people must change their behavior. Weight-loss programs that help people change their behavior are the most effective. Some of the skills involved in behavioral modification include problem solving, stress management, and self-monitoring.
 Did You Know…
Did You Know…
Losing as little as 5 to 10% of body weight can greatly reduce weight-related health risks.
Drugs: For people who are obese or overweight and have weight-related disorders, drugs can be useful. Drugs are most effective when used with changes in diet, increased physical activity, and structured programs that include behavioral modification. Some weight-loss drugs are intended to be used for a short time. Others are intended to be used for a long time. Seven weight-loss drugs are currently available by prescription: orlistat, sibutramine, phentermine, benzphetamine, diethylpropion, mazindol, and phendimetrazine.
Orlistat limits the breakdown and absorption of fats in the intestine, producing, in effect, a low-fat diet. It is also currently available over the counter. It can cause bloating, gas and loose stools. Orlistat can interfere with the absorption of the fat-soluble vitamins: A, D, E, and K. If not enough vitamin D is absorbed, some people develop osteoporosis and bone fractures. People who take orlistat should take a vitamin supplement that contains these nutrients. The supplement should be taken at least 2 hours before or after taking orlistat.
SPOTLIGHT ON AGING
 In the United States, the percentage of older people who are obese has been increasing. Obesity in older people is a concern because excess weight increases the risk of certain health problems that tend to become more common as people age: diabetes, cancer, abnormal levels of fats (lipids) in the blood (dyslipidemia), high blood pressure, heart failure, coronary artery disease, and joint disorders.
In the United States, the percentage of older people who are obese has been increasing. Obesity in older people is a concern because excess weight increases the risk of certain health problems that tend to become more common as people age: diabetes, cancer, abnormal levels of fats (lipids) in the blood (dyslipidemia), high blood pressure, heart failure, coronary artery disease, and joint disorders.
Several age-related changes contribute to gaining weight:
 Decreased physical activity: Some reasons for decreased activity are related to aging. They include retirement, loss of capacity for exercise, development of disorders that make movement painful (such as arthritis), and problems with balance. Other factors may also limit physical activity. For example, people may not want to walk because there are no sidewalks, there is too much traffic, or the neighborhood seems unsafe.
Decreased physical activity: Some reasons for decreased activity are related to aging. They include retirement, loss of capacity for exercise, development of disorders that make movement painful (such as arthritis), and problems with balance. Other factors may also limit physical activity. For example, people may not want to walk because there are no sidewalks, there is too much traffic, or the neighborhood seems unsafe.
 Loss of muscle tissue: Muscle tissue is lost partly because levels of growth hormone and sex hormones (estrogen in women and testosterone in men) decrease. But the main reason older people lose lean tissue is physical inactivity. The less muscle tissue people have, the fewer calories their body burns when resting and the easier it is to gain weight.
Loss of muscle tissue: Muscle tissue is lost partly because levels of growth hormone and sex hormones (estrogen in women and testosterone in men) decrease. But the main reason older people lose lean tissue is physical inactivity. The less muscle tissue people have, the fewer calories their body burns when resting and the easier it is to gain weight.
 Increased body fat: When the amount of muscle tissue decreases, the percentage of fat in the body increases. Fat tissue burns fewer calories. Also, the higher percentage of fat means that older people with a normal body mass index (BMI), which is based only on weight and height, may have a higher risk of weight-related health problems than expected. Waist circumference predicts health risks better than BMI in older people.
Increased body fat: When the amount of muscle tissue decreases, the percentage of fat in the body increases. Fat tissue burns fewer calories. Also, the higher percentage of fat means that older people with a normal body mass index (BMI), which is based only on weight and height, may have a higher risk of weight-related health problems than expected. Waist circumference predicts health risks better than BMI in older people.
 Shifting of body fat to the waist: With aging, body fat tends to shift to the waist. Fat that accumulates around the waist and abdomen (as opposed to the hips and thighs) increases the risk of health problems.
Shifting of body fat to the waist: With aging, body fat tends to shift to the waist. Fat that accumulates around the waist and abdomen (as opposed to the hips and thighs) increases the risk of health problems.
Older people are at greater risk of undernutrition than younger people. Therefore, when they try to lose weight, they should be sure to consume a healthy and balanced diet. Whether weight loss in older people has health risks is controversial. Doctors help older people devise weight-loss strategies based on their individual circumstances. Treatment may include diet, exercise, drugs, and surgery. In older people, weight loss is best supervised by a doctor.
Sibutramine, phentermine, benzphetamine, diethylpropion, mazindol, and phendimetrazine are believed to reduce appetite by affecting chemical messengers in the part of the brain that controls appetite. Some of these drugs may also increase the metabolic rate so that more calories are burned.
The combination of fenfluramine and phentermine (often called fen-phen) was the most effective drug treatment. However, fenfluramine was removed from the market because heart valve problems occurred in people who took this combination.
Some nonprescription diet aids, including medicinal herbs, claim to enhance weight loss by increasing metabolism or by increasing a feeling of fullness. These supplements have not been shown to be effective and may contain harmful additives or stimulants, such as ephedra, and should be avoided.
Many new drugs for the treatment of obesity are being developed and will probably change the way obesity is treated in the future.
BARIATRIC SURGERY
Bariatric surgery alters the stomach, intestine, or both to produce weight loss.
In the United States, more than 200,000 people have bariatric surgery each year. This number accounts for almost two thirds of the total number of bariatric procedures done worldwide. These procedures result in substantial weight loss. People may lose half or even more of their excess weight and as much as 80 to 160 pounds. Weight loss is rapid at first, and then slows gradually over a period of about 2 years. Weight loss is often maintained for years. The loss greatly reduces the severity and risk of weight-related medical problems (such as high blood pressure and diabetes). It improves mood, self-esteem, body image, activity level, and ability to work and interact with other people.
When obesity is severe (BMI of more than 40), surgery is the treatment of choice. Surgery is also appropriate when people with a BMI of more than 35 have serious weight-related health problems, such as diabetes, high blood pressure, sleep apnea, or heart failure.
To qualify for surgery, people also need to do the following:
 Understand its risks and effects
Understand its risks and effects
 Be motivated to follow the changes in diet and lifestyle required after surgery
Be motivated to follow the changes in diet and lifestyle required after surgery
 Have tried other methods of losing weight
Have tried other methods of losing weight
 Be physically and mentally able to undergo surgery
Be physically and mentally able to undergo surgery
Whether bariatric surgery is appropriate for people younger than 18 or older than 65 is controversial.
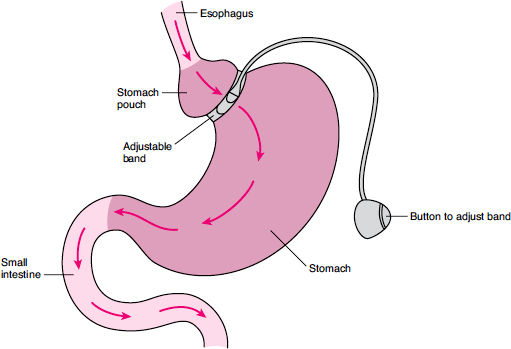
Banding the Stomach
For this procedure, an adjustable band is placed around the upper part of the stomach. It enables people to adjust the size of the passageway for food through the stomach.
After a small incision is made in the abdomen, a viewing tube (laparoscope) is inserted. While looking through the laparoscope, the surgeon places the band around the upper part of the stomach. On the inside of the band is an inflatable ring, which is connected to tubing with a small port at the other end. The port is placed just under the skin. A special needle can be inserted into the port through the skin. The needle is used to insert a salt water (saline) solution into the band or to remove it. Thus, the passageway can be made smaller or larger. When the passageway is smaller, the upper part of the stomach fills faster, causing people to feel “full” more quickly and thus eat less.
Types
Bariatric surgery is often done using a flexible viewing tube (laparoscope) inserted into a small incision (about 1 inch long) just below the navel. This technique is called laparoscopy. Four to six other surgical instruments are then inserted into the abdomen through similar small incisions. Whether laparoscopy can be used depends on the type of procedure and the person’s size. If laparoscopy cannot be used, surgery involves a larger abdominal incision (called open abdominal surgery). Compared with open abdominal surgery, laparoscopy is much less invasive and recovery is much more rapid.
Bariatric surgery may restrict the amount of food people can eat, reduce the amount of food absorbed, or both.
Procedures That Restrict: These procedures include adjustable gastric banding and vertical banded gastroplasty. By restricting the amount of food that people can eat, these procedures make people feel “full” sooner.
Adjustable gastric banding can be done using a laparoscope. A band (sometimes called a lap band) is placed at the upper end of the stomach to divide the stomach into a small upper part and a larger lower part. Food passes through the band on its way to the intestine, but the band slows that passage. Connected to the band is a piece of tubing with a device that allows access at the other end (a port). The port is placed just under the skin so that the tightness of the band can be adjusted after surgery. Fluid can be injected through the port into the band to expand it and make the passageway through the stomach smaller. Or fluid can be removed from the band to shrink it and make the passageway larger. When the passageway is smaller, the upper part of the stomach fills more quickly, sending a message to the brain that the stomach is full. As a result, people eat smaller meals and lose substantial amounts of weight over time.
Bypassing Part of the Digestive Tract
For this procedure, part of the stomach is detached from the rest, creating a small pouch. The pouch is connected to a lower part of the small intestine by a piece of small intestine—an arrangement that resembles a Y. As a result, parts of the stomach and small intestine are bypassed. However, digestive juices (bile acids and pancreatic enzymes) can still mix with food, enabling the body to absorb vitamins and minerals and reducing the risk of nutritional deficiencies.

Vertical banded gastroplasty is no longer commonly done. For this procedure, staples are placed vertically down the stomach along about two thirds of its length. Thus, the top two thirds is divided, with one part smaller than the other. A nonadjustable plastic band is placed at the bottom of the staple line, where the divided parts of the stomach join. Food from the esophagus enters the smaller part, and the band restricts and thus delays the movement of food through the stomach. As a result, people cannot eat as much, and they feel full sooner.
Procedures That Reduce Absorption: These procedures include Roux-en-Y gastric bypass and biliopancreatic diversion with a duodenal switch. These procedures reroute food so that it bypasses parts of the stomach and small intestine, where it is normally absorbed. Thus, less food is absorbed. These procedures also restrict the movement of food through the digestive system.
Roux-en-Y gastric bypass accounts for most of the bariatric procedures in the United States, although banding is becoming more popular. Roux-en-Y gastric bypass can often be done through a laparoscope. The part of the stomach next to the esophagus is detached from the rest, creating a small pouch. As a result, the amount of food that can be eaten at one time is drastically reduced. A section of small intestine is used to connect the pouch to a lower part of the small intestine (this arrangement resembles a Y—hence the name). The opening between them is made narrow to further restrict the movement of food. This connection bypasses the lower part of the stomach and upper part of the small intestine, where much of the absorption occurs. However, it allows digestive juices (bile acids and pancreatic enzymes) to mix with the food. This mixing, which is necessary for food to be absorbed, enables vitamins and minerals to be digested and then absorbed and thus reduces the risk of nutritional deficiencies. Most people stay in the hospital overnight or longer.
For many people who have had a gastric bypass, eating foods high in fat and refined sugar can cause dumping syndrome. Symptoms include indigestion, nausea, diarrhea, abdominal pain, sweating, light-headedness, and weakness. Dumping syndrome occurs when undigested food from the stomach moves into the small intestine too quickly. This syndrome usually stops occurring after a short time.
Biliopancreatic diversion with a duodenal switch is rarely used. Part of the stomach is removed. In contrast to the Roux-en-Y bypass, the part of the stomach that is left connects normally to the esophagus and the small intestine. Also, the valve between the stomach and small intestine is left intact and can function normally. Thus, the stomach empties normally. The small intestine is divided. The part that connects with the stomach (duodenum) is cut and attached to the lower part (ileum), bypassing much of the small intestine. As a result, digestive juices (bile acids and pancreatic enzymes) cannot mix with food as well, and absorption is reduced. Nutritional deficiencies often result.
Evaluation
Before surgery, people are evaluated to determine whether they are able to withstand the stress of surgery. A physical examination and tests are done. Tests may include the following:
 Tests that are routinely done before surgery to check how well vital organs are functioning
Tests that are routinely done before surgery to check how well vital organs are functioning
 Blood tests, including liver function tests, blood sugar levels, and lipid levels (after fasting)
Blood tests, including liver function tests, blood sugar levels, and lipid levels (after fasting)
 Ultrasonography of the abdomen, including the gallbladder
Ultrasonography of the abdomen, including the gallbladder
 Echocardiography (ultrasonography of the heart)
Echocardiography (ultrasonography of the heart)
 Pulmonary function tests
Pulmonary function tests
 Evaluation of the digestive tract (with ultrasonography or endoscopy)
Evaluation of the digestive tract (with ultrasonography or endoscopy)
 Thyroid function tests
Thyroid function tests
 Sleep evaluation (including polysomnography) and testing for sleep apnea
Sleep evaluation (including polysomnography) and testing for sleep apnea
Psychiatric and nutritional evaluations are also done. People should tell their doctor about any drugs or medicinal herbs they are taking. Some drugs, including anticoagulants (such as warfarin) and aspirin, may be stopped before surgery.
After Surgery
After surgery, pain relievers are prescribed.
For the first 2 weeks, the diet is liquids only. People are asked to drink small amounts frequently throughout the day. They should drink as much fluid as prescribed and should take a liquid protein supplement. For the next 2 weeks, people should consume a soft diet. After 4 weeks, they can start eating solid foods. The following can help people avoid digestive problems and discomfort:
 Taking small bites of food
Taking small bites of food
 Chewing food thoroughly
Chewing food thoroughly
 Avoiding high-fat and high-sugar foods, such as “fast food,” cakes, and cookies
Avoiding high-fat and high-sugar foods, such as “fast food,” cakes, and cookies
 Eating only small amounts at each meal
Eating only small amounts at each meal
Usually, people can resume taking their routine drugs after surgery, but tablets may have to be crushed.
People should start walking or doing leg exercises the day after surgery. To avoid blood clots, they should not stay in bed for long periods of time. They can return to their usual activities after about 1 week and to their usual exercises (such as aerobics and strength training) after a few weeks. They should consult their doctor before doing any heavy lifting and manual labor.
Possible Problems: Most people lose their appetite after surgery. People experience pain, and some have nausea and vomiting. Constipation is common. Drinking more fluids and not staying in bed too long at a time can help relieve constipation.
Serious complications, such as problems with the incision, infections, and lung problems, can occur after any operation (see page 2056). In addition, the following complications can occur after bariatric surgery. However, when surgery is done at specialized centers, they occur in fewer than 10% of people. Most can be treated.
After Bariatric Surgery: When to Call the Doctor
After bariatric surgery, some symptoms are common and do not indicate a problem. However, the following symptoms require a call or visit to the doctor:
 Signs of infection at the incision site, such as redness, severe pain, swelling, a bad odor, or oozing
Signs of infection at the incision site, such as redness, severe pain, swelling, a bad odor, or oozing
 Separation of stitched edges of the incision
Separation of stitched edges of the incision
 Continued or increasing abdominal pain
Continued or increasing abdominal pain
 Persistent fever or chills
Persistent fever or chills
 Vomiting
Vomiting
 Persistent bleeding
Persistent bleeding
 Abnormal beating of the heart
Abnormal beating of the heart
 Diarrhea
Diarrhea
 Dark, tarry, foul-smelling stools
Dark, tarry, foul-smelling stools
 Shortness of breath
Shortness of breath
 Sweating
Sweating
 Sudden paleness
Sudden paleness
 Persistent chest pain
Persistent chest pain
 Blockage of the intestine: In about 2 to 4% of people, the intestine becomes blocked because it becomes twisted or scar tissue forms. A blockage can develop weeks to months to years after surgery. Symptoms include severe abdominal pain, nausea, and vomiting.
Blockage of the intestine: In about 2 to 4% of people, the intestine becomes blocked because it becomes twisted or scar tissue forms. A blockage can develop weeks to months to years after surgery. Symptoms include severe abdominal pain, nausea, and vomiting.
 Leakage: In about 1% of people, the new connection between the stomach and intestine leaks. Leakage usually occurs within 2 weeks of surgery. As a result, the stomach’s contents can leak into the abdominal cavity and cause a serious infection (peritonitis). Symptoms include a fast heart rate, abdominal pain, fever, shortness of breath, and a general sick feeling.
Leakage: In about 1% of people, the new connection between the stomach and intestine leaks. Leakage usually occurs within 2 weeks of surgery. As a result, the stomach’s contents can leak into the abdominal cavity and cause a serious infection (peritonitis). Symptoms include a fast heart rate, abdominal pain, fever, shortness of breath, and a general sick feeling.
 Bleeding: Bleeding may occur at the connection between the stomach and intestine, elsewhere in the digestive tract, or in the abdominal cavity. People may vomit blood or have bloody diarrhea or dark, tarry stools.
Bleeding: Bleeding may occur at the connection between the stomach and intestine, elsewhere in the digestive tract, or in the abdominal cavity. People may vomit blood or have bloody diarrhea or dark, tarry stools.
 Gallstones: Many people who successfully follow a diet aimed at quick weight loss develop gallstones. To reduce this risk after bariatric surgery, people are given supplemental bile salts, but these supplements do not always prevent gallstones. About 7% of people who have bariatric surgery need to have their gallbladder removed later.
Gallstones: Many people who successfully follow a diet aimed at quick weight loss develop gallstones. To reduce this risk after bariatric surgery, people are given supplemental bile salts, but these supplements do not always prevent gallstones. About 7% of people who have bariatric surgery need to have their gallbladder removed later.
 Nutritional deficiencies: If people do not make a concentrated effort to eat enough protein, a protein deficiency may develop. Vitamins and minerals (such as vitamins B12 and D, calcium, and iron) may not be absorbed as well after the surgery. Taking supplements, including a multivitamin, can help.
Nutritional deficiencies: If people do not make a concentrated effort to eat enough protein, a protein deficiency may develop. Vitamins and minerals (such as vitamins B12 and D, calcium, and iron) may not be absorbed as well after the surgery. Taking supplements, including a multivitamin, can help.
 Death: Up to 0.5% of people die after surgery. Usually, the cause is a blood clot that travels to the lungs or a severe infection from leakage of one of the connections in the stomach or intestines along with a preexisting heart or lung disorder. Risk is higher for older people and for people who have had open surgery or who are very obese.
Death: Up to 0.5% of people die after surgery. Usually, the cause is a blood clot that travels to the lungs or a severe infection from leakage of one of the connections in the stomach or intestines along with a preexisting heart or lung disorder. Risk is higher for older people and for people who have had open surgery or who are very obese.
Follow Up: Visits to the doctor are scheduled every 4 to 6 weeks during the first several months after surgery—the time when weight loss is most rapid. Then visits are scheduled every 6 to 12 months. Weight and blood pressure are measured, and eating habits are discussed. People should report any problems they are having. Blood tests are done at each visit.
Metabolic Syndrome
Metabolic syndrome (also called syndrome X or insulin resistance syndrome) is characterized by excess abdominal fat, resistance to the effects of insulin (insulin resistance), abnormal levels of fats in the blood, and high blood pressure.
 Excess abdominal fat increases the risk of high blood pressure, coronary artery disease, and type 2 diabetes.
Excess abdominal fat increases the risk of high blood pressure, coronary artery disease, and type 2 diabetes.
 Doctors measure waist circumference, blood pressure, and fasting blood sugar and fat (lipid) levels.
Doctors measure waist circumference, blood pressure, and fasting blood sugar and fat (lipid) levels.
 Changes in eating habits, exercise, behavioral techniques, and drugs may be used to help people lose weight.
Changes in eating habits, exercise, behavioral techniques, and drugs may be used to help people lose weight.
 Diabetes, high blood pressure, and abnormal fat levels are treated.
Diabetes, high blood pressure, and abnormal fat levels are treated.
In developed countries, metabolic syndrome is a serious problem. In the United States, more than 40% of people over 50 may have it. Even children and adolescents can develop metabolic syndrome, but how many have it is unknown.
Metabolic syndrome is more likely to develop when people store excess fat around the abdomen (apple-shaped) rather than around the hips (pear-shaped). The following people tend to store excess fat in the abdomen:
 Most men
Most men
 Women after menopause
Women after menopause
Storing excess fat in the abdomen increases the risk of the following:
 Coronary artery disease
Coronary artery disease
 High blood pressure
High blood pressure
 Type 2 diabetes
Type 2 diabetes
 Abnormal levels of fats (lipids), including cholesterol, in the blood (dyslipidemia)
Abnormal levels of fats (lipids), including cholesterol, in the blood (dyslipidemia)
 Fatty liver
Fatty liver
 Gout
Gout
 Polycystic ovary syndrome (in women)
Polycystic ovary syndrome (in women)
 Chronic kidney disease
Chronic kidney disease
Metabolic syndrome itself causes no symptoms.
Diagnosis
Waist circumference should be measured in all people because even people who are not overweight or appear lean can store excess fat in the abdomen. The greater the waist circumference, the higher the risk of metabolic syndrome and its complications. Risk is substantially increased if waist circumference is more than the following:
 31 inches (80 centimeters) in white or Asian women
31 inches (80 centimeters) in white or Asian women
 37 inches (94 centimeters) in white men
37 inches (94 centimeters) in white men
 33 inches (85 centimeters) in Asian men
33 inches (85 centimeters) in Asian men
If waist circumference is high, doctors should measure blood pressure and blood sugar and fat levels after fasting. These levels are often both abnormal. The metabolic syndrome is diagnosed when the waist circumference is more than 40 inches (102 centimeters) in men or more than 35 inches (88 centimeters) in women (indicating excess fat in the abdomen) and when people have or are being treated for two or more of the following:
 A fasting blood sugar level of more than 100 mg/dL (milligrams per deciliter)
A fasting blood sugar level of more than 100 mg/dL (milligrams per deciliter)
 Blood pressure of more than 130/80 mm Hg (millimeters of mercury)
Blood pressure of more than 130/80 mm Hg (millimeters of mercury)
 A fasting blood triglyceride (a fat) level of more than 150 mg/dL
A fasting blood triglyceride (a fat) level of more than 150 mg/dL
 A high density lipoprotein (HDL—the good) cholesterol level of 40 mg/dL or less for men or 50 mg/dL or less for women
A high density lipoprotein (HDL—the good) cholesterol level of 40 mg/dL or less for men or 50 mg/dL or less for women
Treatment
The initial treatment involves changes in diet and exercise. Each part of the syndrome should also be treated with drugs if necessary. If people have diabetes or a high blood sugar level, drugs that increase the body’s sensitivity to insulin, such as metformin or a thiazolidinedione drug (for example, rosiglitazone or pioglitazone), may help. Also, exercise is important for people with diabetes because it enables the body to use blood sugar more efficiently and can often help lower the blood sugar level. High blood pressure and abnormal fat levels in blood are also treated. Drugs to lower blood pressure (antihypertensives) or to lower lipid levels are used if needed. Other risk factors for coronary artery disease, if present, should be controlled. For example, smokers are advised to stop smoking.